Abstract
Background
Dental caries is a sugar‐dependent disease that damages tooth structure and, due to loss of mineral components, may eventually lead to cavitation. Dental caries is the most prevalent disease worldwide and is considered the most important burden of oral health. Conventional treatment methods (drill and fill) involve the use of rotary burs under local anaesthesia. The need for an electricity supply, expensive handpieces and highly trained dental health personnel may limit access to dental treatment, especially in underdeveloped regions.
To overcome the limitations of conventional restorative treatment, the Atraumatic Restorative Treatment (ART) was developed, mainly for treating caries in children living in under‐served areas of the world where resources and facilities such as electricity and trained manpower are limited. ART is a minimally invasive approach which involves removal of decayed tissue using hand instruments alone, usually without use of anaesthesia and electrically driven equipment, and restoration of the dental cavity with an adhesive material (glass ionomer cement (GIC), composite resins, resin‐modified glass‐ionomer cement (RM‐GICs) and compomers).
Objectives
To assess the effects of Atraumatic Restorative Treatment (ART) compared with conventional treatment for managing dental caries lesions in the primary and permanent teeth of children and adults.
Search methods
Cochrane Oral Health’s Information Specialist searched the following databases: Cochrane Oral Health’s Trials Register (to 22 February 2017), the Cochrane Central Register of Controlled Trials (CENTRAL) (the Cochrane Library, 2017, Issue 1), MEDLINE Ovid (1946 to 22 February 2017), Embase Ovid (1980 to 22 February 2017), LILACS BIREME Virtual Health Library (Latin American and Caribbean Health Science Information database; 1982 to 22 February 2017) and BBO BIREME Virtual Health Library (Bibliografia Brasileira de Odontologia; 1986 to 22 February 2017). The US National Institutes of Health Trials Registry (ClinicalTrials.gov) and the World Health Organization International Clinical Trials Registry Platform were searched for ongoing trials. No restrictions were placed on the language or date of publication when searching the electronic databases.
Selection criteria
We included randomised controlled trials (RCTs) with at least six months' follow‐up that compared the effects of ART with a conventional restorative approach using the same or different restorative dental materials to treat caries lesions.
Data collection and analysis
Two review authors independently screened search results, extracted data from included studies and assessed the risk of bias in those studies. We used standard methodological procedures expected by Cochrane to evaluate risk of bias and synthesise data. Where pooling was appropriate we conducted meta‐analyses using the random‐effects model. We assessed the quality of the evidence using GRADE criteria.
Main results
We included a total of 15 eligible studies randomising 3760 participants in this review. The age of participants across the studies ranged from 3 to 101 years, with a mean of 25.42 years. 48% of participants were male. All included studies were published between 2002 and 2016. Two of the 15 studies declared that the financial support was from companies that manufacture restorative material. Five studies were individually randomised parallel‐group studies; six were cluster‐randomised parallel‐group studies; and four were randomised studies that used a split‐mouth design. Eleven studies evaluated the effects of ART on primary teeth only, and four on permanent teeth. The follow‐up period of the included studies ranged from 6 months to 36 months. We judged all studies to be at high risk of bias.
For the main comparison of ART compared to conventional treatment using the same material: all but two studies used high‐viscosity glass ionomer (H‐GIC) as the restorative material; one study used a composite material; and one study used resin‐modified glass ionomer cement (RM‐GIC)).
Compared to conventional treatment using H‐GIC, ART may increase the risk of restoration failure in the primary dentition, over a follow‐up period from 12 to 24 months (OR 1.60, 95% CI 1.13 to 2.27, five studies; 643 participants analysed; low‐quality evidence). Our confidence in this effect estimate is limited due to serious concerns over risk of performance and attrition bias. For this comparison, ART may reduce pain during procedure compared with conventional treatment (MD ‐0.65, 95% CI ‐1.38 to 0.07; 40 participants analysed; low‐quality evidence)
Comparisons of ART to conventional treatment using composite or RM‐GIC were downgraded to very low quality due to indirectness, imprecision and high risk of performance and attrition bias. Given the very low quality of the evidence from single studies, we are uncertain about the restoration failure of ART compared with conventional treatment using composite over a 24‐month follow‐up period (OR 1.11, 95% CI 0.54 to 2.29; one study; 57 participants) and ART using RM‐GIC in the permanent teeth of older adults with root caries lesions over a six‐month follow‐up period (OR 2.71, 95% CI 0.94 to 7.81; one study; 64 participants).
No studies reported on adverse events or costs.
Authors' conclusions
Low‐quality evidence suggests that ART using H‐GIC may have a higher risk of restoration failure than conventional treatment for caries lesions in primary teeth. The effects of ART using composite and RM‐GIC are uncertain due to the very low quality of the evidence and we cannot rely on the findings. Most studies evaluated the effects of ART on the primary dentition.
Well‐designed RCTs are required that report on restoration failure at clinically meaningful time points, as well as participant‐reported outcomes such as pain and discomfort. Due to the potential confounding effects from the use of different dental materials, a robust body of evidence on the effects of ART compared with conventional treatment using the same restoration material is necessary. We identified four ongoing trials that could provide further insights into this area.
Plain language summary
Atraumatic restorative treatment (hand instruments only) compared with conventional treatment for managing tooth decay
Review question
The aim of this review is to evaluate the effects of a minimally invasive approach, namely Atraumatic Restorative Treatment (ART), for the treatment of tooth decay in children and adults (primary and permanent teeth).
Background
Dental caries (tooth decay) has been considered the most common global disease. Conventional methods (drill and fill) involve the use of electric drills to clear away decayed areas of tooth before filling. Local anaesthetic (painkiller) is normally injected to prevent pain during the procedure. Conventional treatments require highly trained dental health personnel, access to electricity, appropriate tools and are more expensive. These factors may limit access especially in underdeveloped regions of service provision.
Atraumatic Restorative Treatment (ART) is an alternative approach for managing dental decay, which involves removal of decayed tissue using hand instruments alone, usually without the use of anaesthesia (injected painkiller) and electrical equipment.
Study characteristics
This review searched the available evidence that was up to date at 22 February 2017. We found 15 relevant studies including 3760 participants with an average age of 25 years (range 3 to 101) where 48% were male. The follow‐up period in the trials ranged from 6 to 36 months. Two of the 15 studies declared financial support from companies that made tooth‐filling material. In addition, we found four ongoing studies.
Key results
There is low‐quality evidence to suggest that primary teeth treated with the ART approach using high viscosity glass ionomer cement may be more likely than those receiving conventional treatment with the same material to result in restoration failure. In the treatment of primary teeth, ART may reduce pain experience compared with conventional treatment. The evidence available for evaluating the differences between ART and conventional treatments using other restorative materials or in permanent teeth is very low quality so we cannot draw any conclusions. None of the included studies reported on negative side effects or costs.
Quality of the evidence
The available evidence is low‐ to very low‐quality. It is likely that further high‐quality research may change our findings. There are four ongoing studies that may provide more information in the future.
Summary of findings
Background
Description of the condition
Dental caries
Dental caries is a sugar‐dependent disease that damages tooth structure and may result in cavity formation in the hard tissues of the teeth (enamel, dentine and cementum) (Kidd 2005). Dental plaque is a biofilm formed on the tooth surface soon after tooth cleaning. It frequently contains caries‐producing bacteria such as Streptococcus mutans. Such micro‐organisms metabolise dietary sugars and produce acids on the tooth surfaces. The acid production could lead to the diffusion of calcium and phosphate ions and, consequently, demineralisation of enamel (Fejerskov 2004; Kidd 2004). If this process continues, loss of mineral components will eventually lead to cavitation.
Dental caries is the most prevalent disease worldwide (Marcenes 2013). Dental caries and its consequences are considered the most important burden of oral health. They are especially common in sociodemographically disadvantaged groups (Antoft 1999; Ekstrand 2007; Hannigan 2000; Martignon 2010; Petersen 2005; Schwendicke 2015; Sheiham 2010). It affects 60% to 90% of school‐aged children and up to 100% of adults in most countries (Petersen 2005).The resultant pain and discomfort can negatively affect people's quality of life. Furthermore, the management of this condition imposes huge financial burden on society and individuals (Leal 2012).
Description of the intervention
The treatment of dental caries lesions can be either by conventional drill and fill approach, using rotary instruments, or the atraumatic approach, using only hand instruments. Different restorative materials may be used for these two approaches.
Conventional treatments
Conventional methods involve the use of rotary burs, alone or in conjunction with metal hand instruments (Weerheijm 1999). Various dental restorative materials are used, ranging from metal‐based materials such as amalgam, the most popular dental restoration material, especially in the posterior teeth, to tooth‐coloured materials, such as resin composites.
The pain and discomfort associated with conventional cavity preparation methods have resulted in many patients being reluctant to seek dental treatment (Berggren 1984). Local anaesthesia is frequently needed to control the pain associated with cavity preparation. Factors potentially responsible for the discomfort and pain include: the sensitivity of vital dentine; the pressure on the tooth caused by mechanical stimulation of the tooth by rotary devices; bone‐conducted noise and vibration; the high‐pitched noise of the rotary device; and development of high temperatures at the cutting surface (thermal stimulation) (Banerjee 2000). In addition, an important limitation of conventional restorative methods is that they require an electricity supply, expensive handpieces and highly trained dental health personnel. This approach has been shown to have an increased risk of pulp exposure, postoperative pulpal symptoms and the weakening of the tooth as result of more invasive caries removal (Ricketts 2013). These factors limit the use of conventional restorative dentistry in many underdeveloped areas, where facilities and trained human resources are scarce.
Atraumatic treatments
To overcome the limitations of conventional restorative treatment, Atraumatic Restorative Treatment (ART) was developed around 1985, mainly for treating caries in children living in under‐served areas of the world where resources and facilities such as electricity and trained manpower are limited (Frencken 1996). ART is a minimally invasive approach, which involves removal of decayed tissue using hand instruments alone, usually without use of anaesthesia and electrically‐driven equipment, and restoration of the dental cavity with an adhesive material (glass ionomer cement (GIC), composite resins, resin‐modified glass‐ionomer cement (RM‐GICs) and compomers) (Tyas 2000).
Recently, modified ART approaches have been introduced, as opposed to 'true' ART as described above. These modified approaches involve opening the cavity with a drill, cleaning, restoring and finishing with hand instruments, or using alternative restorative materials including amalgam (Monse‐Schneider 2003). Also, some studies applied ART‐type GICs as pit and fissure sealants using different methods such as the press‐finger method (Yip 2002a). These modified ART approaches are not considered to be 'true' ART (Holmgren 2013).
Apart from these modified approaches, the American Academy of Pediatric Dentistry (AAPD) (AAPD 2008‐2009) introduced the Interim Therapeutic Restorations (ITR) approach, which uses almost the same technique as ART, although it may have different therapeutic goals. The ITR procedure involves removal of caries using hand or slow‐speed rotary instruments, as opposed to ART, which uses only hand instruments, followed by restoration with an adhesive restorative material such as self‐setting or resin‐modified glass ionomer cement (RM‐GIC). While ART is recognised as a permanent treatment, the AAPD regards ITR as a provisional technique. The ITR, according to AAPD, may be used "to restore and to prevent dental caries in young patients, uncooperative patients, patients with special health care needs, and situations in which traditional cavity preparation and/or placement of traditional dental restorations are not feasible; it may be used for caries control in children with multiple carious lesions prior to definitive restoration of the teeth" (AAPD 2008‐2009). Based on the AAPD definition, if ITR is applied using hand instruments, and not rotary instruments, it can then be considered as a 'true' ART.
The advantages of ART compared with conventional restorative techniques using dental handpiece and burs include: provision of restorative dental treatment outside the dental surgery setting; a biologically friendly approach; minimal cavity preparations; low costs (Frencken 1999; Mjör 1999; Yip 2001; Yip 2002a); reduced risk for subsequent endodontics and tooth extraction (Anusavice 1999); and lower dental anxiety in children and adults (more 'patient‐friendly') (Mickenautsch 2007; Schriks 2003). These advantages are particularly important in low‐income countries, where electricity supplies are intermittent and people have difficulties accessing dental care. In addition, people who are elderly, medically‐compromised (e.g. HIV infected) or dental phobic can have problems accessing dental care and could benefit from the ART approach (Cole 2000; Honkala 2002; Steele 2007).
Glass‐ionomer cements (GICs) are the predominant restorative materials used for ART (Yip 2001). GIC restorative materials have advantages such as the ability to bond chemically to enamel and dentine, biocompatibility with pulpal tissue and less potential to induce recurrent caries, inhibition of enamel demineralisation, good cavity seal, ease of use, and low costs (Frencken 1996; Van 't Hof 2006). As shown by a recent Cochrane Review, the sealing‐in effect of GICs apart from replacement of damaged tooth tissue, can help with the management of dental carious lesions (Dorri 2015). Although GICs have been the main material used, other adhesive materials include composite resins, RM‐GICs and compomers.
How the intervention might work
As described, ART approach relies on removal of dental caries using hand instruments only, followed by restoration with an adhesive material. The adhesive restorative material prevents diffusion of acids from biofilms into the lesion or mineral out of the lesion, thereby arresting the lesions or reducing their progression. Furthermore, using hand instruments only, minimises iatrogenic damage to the intact tooth substance whilst removing carious tissue.
Why it is important to do this review
Cochrane Oral Health undertook an extensive prioritisation exercise in 2014 to identify a core portfolio of titles that were the most clinically important ones to maintain in the Cochrane Library (Worthington 2015). This review was identified as a priority title by the paediatric dentistry expert panel (Cochrane Oral Health priority review portfolio).
The ART approach seems to be an economic and effective method for improving the oral health not only of people in low‐income countries, but also of those in high‐income countries (Frencken 2004b). It may be considered as a minimally invasive alternative for conventional restorative dental treatment, particularly for Class I (occlusal) single‐surface dental cavities. Because of the advantages claimed for ART, it is important to systematically review the evidence available.
The available systematic reviews on studies comparing the ART approach with conventional approach have limitations including: restricting the search to only one electronic database (MEDLINE) and English language studies (Frencken 2004a; Van 't Hof 2006); not assessing the quality of included studies (Van 't Hof 2006); only including permanent teeth and class I cavities (Frencken 2004a); inconsistency with PRISMA guidelines (Moher 2009) in several areas, such as protocol and registration, risk of bias across studies, reporting of limitations and funding (Frencken 2004a; Mickenautsch 2010; Pettar 2011). We aimed to systematically review randomised controlled trials comparing 'true' ART with conventional restorative approaches.
Objectives
To assess the effects of true Atraumatic Restorative Treatment (ART) compared with conventional treatments for managing dental caries lesions in the primary and permanent teeth of children and adults.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) with at least six months' follow‐up that compared the effects of 'true' ART with a conventional restorative approach using the same or different restorative dental materials. Parallel‐group, split‐mouth and cluster‐study design were eligible for inclusion.
Types of participants
We included dentate participants, regardless of their age and sex, with a history of dental (coronal or root) primary caries lesions extended into enamel and dentine (but not the pulp) and who have undergone restorative treatment using either conventional restorative or true ART approaches. We also considered primary and permanent teeth with single or multiple surface lesions.
Types of interventions
We included adhesive restorative materials, such as GICs with different viscosities or resins, placed with the 'true' ART approach, including ITR with hand instruments, compared with the same or different restorative materials, such as GIC, placed with conventional cavity preparation methods. Only studies using the same restorative material in both arms were considered as key results and the other studies were included for completeness.
We excluded studies on modified ART techniques.
Types of outcome measures
Primary outcomes
Restoration failure, that is, a lost or deficient restoration in the 1) primary dentition, 2) permanent immature dentition, 3) permanent mature dentition
Pain (during and immediately after treatment expressed as intensity of pain or presence or absence of pain)
Secondary outcomes
Adverse events
Secondary caries
Participant experience, for example, satisfaction or quality of life measured by self report, and discomfort, anxiety or stress measured by physiological means or behavioural observation
Costs (direct) ‐ cost of treatment
Costs (indirect) ‐ time off school or work to attend dental visits
Search methods for identification of studies
Electronic searches
Cochrane Oral Health’s Information Specialist conducted systematic searches in the following databases for RCTs and controlled clinical trials. There were no language, publication year or publication status restrictions:
Cochrane Oral Health’s Trials Register (searched 22 February 2017) (Appendix 1);
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 1) in the Cochrane Library (searched 22 February 2017) (Appendix 2);
MEDLINE Ovid (1946 to 22 February 2017) (Appendix 3);
Embase Ovid (1980 to 22 February 2017) (Appendix 4);
LILACS BIREME Virtual Health Library (Latin American and Caribbean Health Science Information database; 1982 to 22 February 2017) (Appendix 5);
BBO BIREME Virtual Health Library (Bibliografia Brasileira de Odontologia; 1986 to 22 February 2017) (Appendix 6).
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, they were combined with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying RCTs and controlled clinical trials as described in the Cochrane Handbook for Systematic Reviews of Interventions Chapter 6 (Lefebvre 2011).
Searching other resources
The following trials registries were searched for ongoing studies:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 22 February 2017) (Appendix 7);
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 22 February 2017) (Appendix 8).
Reference lists
Two review authors independently examined the reference lists of relevant trials in order to identify studies not identified in the previous searches.
Correspondence
We contacted organisations, researchers and experts known to be involved in the field, either by phone, email or in person during scientific events, in an effort to trace unpublished or ongoing studies. We also contacted dental materials and equipment manufacturers to identify any ongoing or unpublished studies.
We did not perform a separate search for adverse effects of interventions used, we considered adverse effects described in included studies only.
Data collection and analysis
Selection of studies
We imported the downloaded set of records from each database to the bibliographic software package Endnote and merged them into one core database to remove duplicate records and to facilitate retrieval of relevant articles. We also obtained potentially relevant reports identified when searching other sources (reference lists of relevant trials, reviews, articles and textbooks). The records located from searching these (non‐electronic) sources were entered manually in Endnote. All records identified by the searches were checked on the basis of title first, then by abstract or keywords or both. Two review authors independently assessed the eligibility of the full text of relevant records (Figure 1).
1.
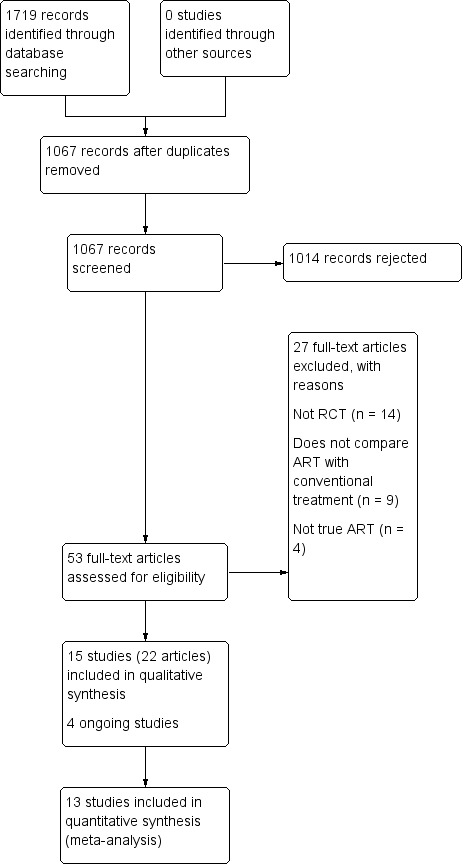
Study flow diagram
One review author (Mojtaba Dorri (MD)) assessed all the references. Two others researchers (Dominic Hurst (DH) and Carlos Zaror (CZ)) assessed the references to establish whether the studies met the inclusion criteria or not, using an inclusion criteria form, which had been prepared previously and pilot tested. We resolved disagreements by discussion. Had resolution not been possible, we would have consulted a third review author (Valeria Marinho (VM)).
The review authors could read reports in English, Persian, Arabic, Portuguese and Spanish. We identified two papers in Chinese and two papers in Dutch. The papers were translated by two translators who were native speakers and fluent in English. One of the authors (MD) compared two versions. The minor disagreements were resolved by discussion with the translators.
We contacted the authors of any articles we could not classify in order to ascertain if inclusion criteria were met. If we identified more than one publication of a trial, we listed the paper with the primary outcome as the primary reference. Where a trial report thought to be potentially relevant was in a language not known to the review authors, it was translated by a native speaker who was fluent in English.
From all studies meeting the inclusion criteria, we extracted the data and assessed risk of bias. We recorded studies rejected at this or subsequent stages in the ’Characteristics of excluded studies’ tables, along with reasons for exclusion.
Data extraction and management
Two review authors (CZ and MD) independently extracted data from the included studies using a pilot‐tested data‐extraction form. The data were then entered into the Characteristics of excluded studies table in Review Manager 5 (RevMan5) (RevMan 2014) and checked for differences. Any disagreements were resolved through discussion with another review author (Mª José Martínez Zapata (MMZ)) until we reached consensus. We contacted trial authors for clarification or missing information, where there was any uncertainty or data were missing. We treated studies with duplicate publications as a single source of data. Review authors were not blinded to the names of the authors, institutions, journal of publication, or results of the studies.
In the data extraction form, we recorded the following details for each trial: RCT design (e.g. parallel, split‐mouth, cluster); country where the trial took place; setting (e.g. primary or secondary care); funding source; inclusion criteria; exclusion criteria; number of participants randomised and evaluated; baseline number of decayed, missing and filled primary teeth (dmfts)/and permanent teeth (DMFTs); test and control interventions; type and number of operators; primary and secondary outcomes; sample size calculation; duration of follow‐up; any co‐interventions; risk of bias; and any other relevant data. We used the data for each specific time point or time interval separately, as reported in the original studies.
Assessment of risk of bias in included studies
Two review authors (CZ and MD) conducted 'Risk of bias' assessment independently and in duplicate for all the included trials, according to the criteria for assessing risk of bias described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreements were resolved through discussion with another review author (Mª José Martínez Zapata (MMZ)) until we reached a consensus. We contacted trial authors where necessary.
We assessed the risk of bias to be high, unclear or low for seven domains:
Sequence generation: was the method used to generate the allocation sequence appropriate to produce comparable groups? We graded this domain as having a low risk of bias if the authors described a random component in the sequence generation process (e.g. random number table, coin tossing, drawing of lots).
Allocation sequence concealment: was the method used to conceal the allocation sequence appropriate to prevent the allocation being known in advance of, or during, enrolment? We graded this domain as having a low risk of bias if the authors described adequate concealment (e.g. by means of central randomisation, sequentially numbered, opaque envelopes), and graded high risk of bias if inadequate concealment was documented (e.g. alternation, use of case record numbers, dates of birth or day of the week) or if allocation was not concealed.
Blinding of participants and personnel: was knowledge of the allocated intervention adequately prevented during the study? We graded this domain as having a high risk of bias if the study did not use any blinding of participants or operators.
Blinding of outcome assessors: was knowledge of the allocated intervention adequately prevented during the study? We graded this domain as having a high risk of bias if the study did not use any blinding of assessors.
Incomplete outcome data: how complete were the outcome data for the primary outcomes? Did authors report dropout rates and reasons for withdrawals? Did they impute missing data appropriately? We graded this domain as having a low risk of bias if the proportion of the missing outcome data was less than 25% and the groups were balanced in numbers and reasons for dropouts, or if investigators imputed missing data using appropriate methods. If dropout was above 25% and there was no information on reasons for dropouts across groups, but attrition was balanced, we graded the risk of bias as unclear. We graded it as high if the proportion of missing outcome data was over 25% and not balanced between groups.
Selective outcome reporting: did investigators report appropriate outcomes or were key outcomes missing? We graded this domain as having a low risk of bias if authors reported all pre‐specified outcomes. If they did not report prespecified or expected data, we assumed the risk of bias to be high.
Other sources of bias: was the study apparently free of other problems that could put it at a high risk of bias? These include information on the baseline characteristics of the intervention and control groups and the similarity in using co‐interventions between groups. We graded the trials as having a high risk of bias if there were important differences in demographic characteristics or if the groups received different co‐interventions during the trial, or if the statistical analysis was inadequate or inappropriate.
We developed a standardised 'Risk of bias' assessment form and entered data in the 'Risk of bias' tables in RevMan 5 (RevMan 2014).
We summarised the potential risk of bias for each study overall:
low risk of bias: plausible bias not likely to seriously alter the results (if low risk of bias for all items);
unclear risk of bias: plausible bias that raises some doubt about the results (if unclear risk of bias for one or more key items, but none at high risk of bias);
high risk of bias: plausible bias that seriously weakens confidence in the results (if high risk of bias for one or more key items), as described in Section 8.7 of the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 (updated March 2011) (Higgins 2011).
We completed a ’Risk of bias’ table for each included study (see Characteristics of included studies) and presented the results graphically by domain over all studies and by study (Figure 2; Figure 3).
2.
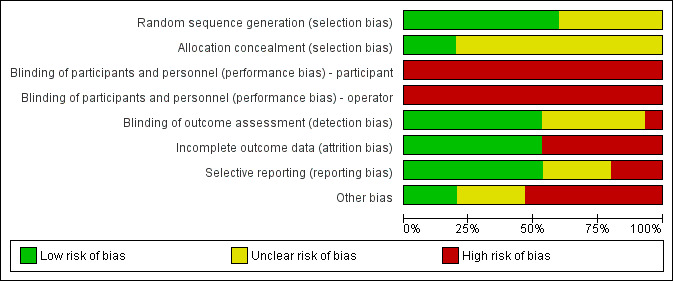
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.
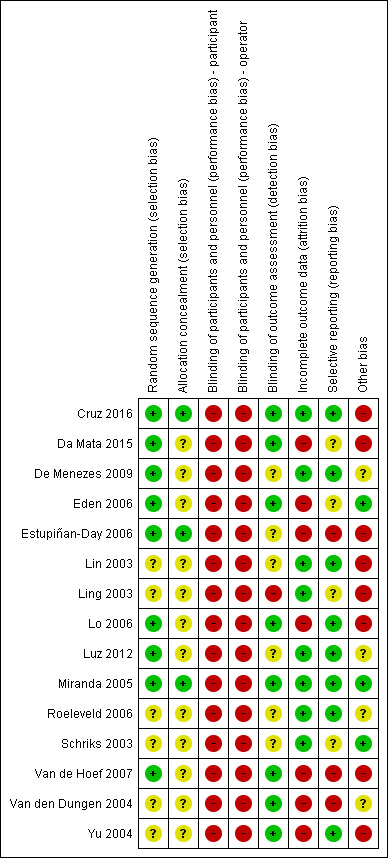
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Measures of treatment effect
We planned to convert data obtained from visual analogue scales and any categorical outcomes into dichotomous data prior to analysis. For continuous data, we planned to calculate mean difference with 95% confidence interval (CI). For each trial, we calculated odds ratios (OR) with 95% CIs for all prespecified dichotomous outcomes.
Unit of analysis issues
In parallel‐group studies, the unit of analysis was the individual. In studies where the unit of randomisation was the individual, but more than one tooth/surface was treated per individual (cluster‐randomised studies), we considered tooth/surface as the unit of analysis and standard errors of the estimates were adjusted taking into account the multiplicity or clustering (Deeks 2011). We considered an intracluster correlation coefficient (ICC) of 0.05, based on published data (Vas 2008).
In split‐mouth studies where two tooth/surfaces are randomised per individual, these pairs are not strictly independent (the unit of analysis is the pair) and therefore, were analysed as 'paired data' (Higgins 2003; Deeks 2011). In these cases, we computed design‐adjusted ORs and standard errors with the Becker‐Balagtas method outlined in Elbourne 2002, assuming a conservative correlation coefficient of 0.05 according to Dorri 2015. We planned to calculate the log odds ratio and standard error separately for each outcome.
In cluster split‐mouth studies, where more than two tooth/surfaces are randomised per individual, the unit of analysis is each pair. We considered these trials as split mouth, analysing the pairs independently, ignoring the clustering effect.
Dealing with missing data
We contacted the study authors where data were missing on the trial characteristics, methodology and/or outcomes. We did not consider missing data as a reason to exclude any of the trials from the review. We had planned to impute missing data, if appropriate. However, we did not carry out data imputation as we assumed all missing data to be at random.
Assessment of heterogeneity
We assessed statistical heterogeneity by examining the characteristics of the studies: the similarity between the types of participants, the interventions and the outcomes as described in Section 9.5 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011).
For this purpose we used the I² statistic (Higgins 2003), which examines the percentage of total variation across studies due to heterogeneity rather than to chance. According to the Cochrane Handbook for Systematic Reviews of Interventions the I2 values are interpreted as follows (Deeks 2011):
0% to 40% might not be important;
30% to 60% may represent moderate heterogeneity;
50% to 90% may represent substantial heterogeneity;
75% to 100% represents considerable heterogeneity.
Assessment of reporting biases
We had planned to assess whether the review was subject to publication bias (or small‐study effects) by using a funnel plot (plots of the effect estimates versus the inverse of their standard errors) (Egger 1997). Asymmetry of the funnel plot may indicate publication bias or other sources of asymmetry including poor methodological quality leading to spuriously inflated effects in smaller studies, true heterogeneity and chance (Sterne 2011). We did not include more than 10 trials in meta‐analysis and therefore, a funnel plot to explore possible publication biases was not indicated. For future updates, if more than 10 trials are included we plan to use a funnel plot to explore publication bias (Egger 1997).
Data synthesis
We pooled only studies that used the same restorative materials in both comparator groups, as different restorative materials require different cavity designs and have different properties that may affect the study outcomes. For example, whilst adhesive restorative materials (e.g. GIC, composite resins) rely on chemical bonding to the tooth for retention, the success of amalgam restoration depends on mechanical retention from the converged cavity walls. This would mean that for an amalgam restoration, following caries removal, the cavity may need to be extended in order to obtain mechanical retention. This may affect the length of procedure, and in turn the patient's experience, and also the restoration survival. In addition GIC releases fluoride that may affect restoration survival.
Our analysis includes data only of those whose results are known, using as a denominator the total number of participants for whom data were recorded for the particular outcome. We expected differences in effect estimates between studies in terms of the number of cavities or surfaces treated per participant and also the duration of follow‐up. Therefore, we applied a random‐effects model for any meta‐analyses (Deeks 2011).
We pooled parallel and split‐mouth data using the generic inverse variance (GIV) (Deeks 2011).
We did not pool data if heterogeneity was over 75%. This was mainly because indicating an average value for the intervention effect when there is a significant inconsistency in the direction of effect may be misleading (Deeks 2011).
We anticipated variation in the timing of endpoints across the studies, both in terms of participant‐reported pain and clinical restoration failure. We included in the meta‐analysis the longest follow‐up reported for each study.
Where studies had multiple intervention or comparator trial arms, we combined summary statistics from all groups where appropriate. We excluded any intervention arms without ART from the meta‐analysis.
The data was analysed using RevMan 5 software (RevMan 2014).
In the event that there were insufficient clinically homogeneous trials for any specific intervention or insufficient study data that could be pooled, a narrative synthesis was presented.
Subgroup analysis and investigation of heterogeneity
We had planned to perform subgroup analysis for dental caries type, as a source of clinical heterogeneity, if sufficient data were available. Therefore, we stratified the analyses in subgroups according to type of cavity surface:
studies reporting on single lesion;
studies reporting on multiple lesions;
studies reporting on single and multiple lesions;
studies where lesion type was not reported;
studies reporting on coronal and root lesion, or on root lesions only.
Sensitivity analysis
We had planned to conduct a sensitivity analysis of the primary outcomes by excluding studies with overall high risk of bias (that is high risk of bias in at least one domain). However, all the included studies were at high risk of bias for at least one domain and therefore, we did not carry out a sensitivity analysis.
Summary of findings
We used GRADEpro GDT software (GRADEpro GDT 2015) to assess the quality of the body of evidence for study outcomes (pain, restoration failure, adverse events) and to develop Table 1, Table 2 and Table 3. The GRADE approach appraises the quality of a body of evidence based on the extent to which one can be confident that an estimate of effect or association reflects the item being assessed. The approach considers evidence from RCTs that do not have serious limitations as 'high' quality. The following factors can decrease the quality of evidence: within‐study limitations (risk of bias), indirectness of the evidence, heterogeneity (inconsistency) in the data, imprecision of effect estimates, and risk of publication bias (Schünemann 2011).
Summary of findings for the main comparison. Atraumatic restorative treatment (ART) using high‐viscosity glass ionomer cement (H‐GIC) compared with conventional restorative treatment using H‐GIC for dental caries.
| Atraumatic restorative treatment (ART) using high‐viscosity glass ionomer cement (H‐GIC) compared with conventional restorative treatment using H‐GIC for dental caries | |||||
|
Patient or population: people with dental caries Settings: community settings and dental clinics Intervention: ART using H‐GIC Comparison: conventional treatment using H‐GIC | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Conventional treatment with H‐GIC | ART with H‐GIC | ||||
|
Restoration failure (primary dentition) at 12 to 24 months |
471 per 1000 | 588 per 1000 (502 to 669) | OR 1.60 (1.13 to 2.27) | 643 participants/846 teeth (5 studies) | ⊕⊕⊝⊝ low1 |
| Pain | Mean pain (primary teeth) was 1.38 (SD 1.21) | Mean pain (primary teeth) was 0.73 (SD 1.14) | MD 0.65 lower (1.38 lower to 0.07 higher) | 40 participants (1 study) | ⊕⊕⊝⊝ low2 |
| Adverse events | ‐ | ‐ | ‐ | ‐ | Not measured |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; OR: odds ratio | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different. Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different. Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||||
1We downgraded the evidence by two levels because of very serious concerns regarding risk of bias: we judged all five studies as high risk of performance bias, three studies as high risk of attrition bias, and two studies as high risk of reporting bias. 2We downgraded the evidence by one level because it is a single study (imprecision) and one level because of serious concern regarding high risk of performance bias.
Summary of findings 2. Atraumatic restorative treatment (ART) using composite resins compared with conventional restorative treatment using composite resins for dental caries.
| Atraumatic restorative treatment (ART) using composite resins compared with conventional restorative treatment using composite resins for dental caries | |||||
|
Patient or population: people with dental caries Settings: community settings and dental clinics Intervention: ART using composite Comparison: conventional treatment using composite | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Conventional treatment | ART | ||||
| Restoration failure (primary dentition) | 362 per 1000 | 387 per 1000 (235 to 565) | OR 1.11 (0.54 to 2.29) | 57 participants/100 teeth (1 study) | ⊕⊝⊝⊝ very low1 |
| Pain | ‐ | ‐ | ‐ | ‐ | Not measured |
| Adverse events | ‐ | ‐ | ‐ | ‐ | Not measured |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different. Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different. Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||||
1We downgraded the evidence by three levels: one level because it is a single study (indirectness) and two levels because of very serious concern regarding the risk of bias (high risk of performance bias and high risk of attrition bias). The result was also very imprecise.
Summary of findings 3. Atraumatic restorative treatment (ART) using resin‐modified glass ionomer cement (RM‐GIC) compared with conventional restorative treatment using RM‐GIC for dental caries.
| Atraumatic restorative treatment (ART) using resin‐modified glass ionomer cement (RM‐GIC) compared with conventional restorative treatment using RM‐GIC for dental caries | |||||
|
Patient or population: people with dental caries Settings: community settings and dental clinics Intervention: ART using RM‐GIC Comparison: conventional treatment using RM‐GIC | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Conventional treatment | ART | ||||
| Restoration failure (primary dentition) | ‐ | ‐ | ‐ | 0 studies | No studies included |
| Restoration failure (permanent teeth) | 75 per 1000 | 180 per 1000 (71 to 388) | OR 2.71 (0.94 to 7.81) | 64 participants/141 teeth (1 study) | ⊕⊝⊝⊝ very low1 |
| Pain | ‐ | ‐ | ‐ | ‐ | Not measured |
| Adverse events | ‐ | ‐ | ‐ | ‐ | Not measured |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different. Low quality: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of effect, but there is a possibility that it is substantially different. Very low quality: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||||
1We downgraded the evidence by one level because it is a single study (indirectness), one level because of concern regarding high risk of performance bias, and one level because the result was imprecise.
Results
Description of studies
Please see Characteristics of included studies; Characteristics of excluded studies; Characteristics of ongoing studies.
Results of the search
The search strategy retrieved 1719 citations (Figure 1). After deleting duplicates and screening titles and abstracts, we evaluated 53 full texts of potentially eligible studies. We excluded 27 studies (Characteristics of excluded studies), and included 22 articles that corresponded to 15 completed RCTs (Cruz 2016; Da Mata 2015; De Menezes 2009; Eden 2006; Estupiñan‐Day 2006; Lin 2003; Ling 2003; Lo 2006; Luz 2012; Miranda 2005; Roeleveld 2006; Schriks 2003; Van de Hoef 2007; Van den Dungen 2004; Yu 2004) (Characteristics of included studies). We also retrieved four ongoing trials (CTRI007332; NCT02562456; NCT02568917; RBR‐4nwmk4) (Characteristics of ongoing studies).
Two studies were in Chinese (Lin 2003; Ling 2003) and two articles were in Dutch (Schriks 2003; Van den Dungen 2004). We contacted two authors in an effort to obtain additional information (Estupiñan‐Day 2006; Eden 2006). Both trial authors responded and answered our questions.
Included studies
We found 15 completed studies, reported in 22 articles, and 4 ongoing studies. Six studies were reported in multiple articles (Da Mata 2015; Eden 2006; Estupiñan‐Day 2006; Schriks 2003; Van de Hoef 2007; Yu 2004). Included studies were published between 2002 and 2016 with a follow‐up period that ranged from 6 to 36 months.
Design
Eleven studies used a parallel‐group design, with six of these using a parallel‐group, cluster‐randomised design. Four studies used a split‐mouth design (Eden 2006; Ling 2003; Miranda 2005; Yu 2004). Only five studies reported a sample size calculation (Da Mata 2015; Eden 2006; Estupiñan‐Day 2006; Lo 2006; Miranda 2005).
Funding for the studies was provided by government (Cruz 2016; Da Mata 2015; Lo 2006), foundations (De Menezes 2009; Eden 2006; Estupiñan‐Day 2006; Van de Hoef 2007; Van den Dungen 2004) and pharmaceutical sources or manfacturers(Eden 2006; Roeleveld 2006; Schriks 2003; Yu 2004). Funding was unclear in four studies (Lin 2003; Ling 2003; Luz 2012; Miranda 2005).
Setting
Studies were conducted in China (Lin 2003; Ling 2003; Lo 2006; Yu 2004), Brazil (De Menezes 2009; Luz 2012; Miranda 2005), Indonesia (Schriks 2003; Van den Dungen 2004), and Colombia, Ireland, Turkey, Tanzania and Surinam (Cruz 2016; Da Mata 2015; Eden 2006; Roeleveld 2006; Van de Hoef 2007). There was one international multicentre trial in Ecuador, Panamá and Uruguay (Estupiñan‐Day 2006).
The study setting was dental clinics or hospitals for seven studies (Da Mata 2015; De Menezes 2009; Eden 2006; Ling 2003; Luz 2012; Miranda 2005; Yu 2004); schools for two studies (Estupiñan‐Day 2006; Van den Dungen 2004), and nursing homes for two studies (Cruz 2016; Lo 2006). Four studies did not report the setting (Lin 2003; Roeleveld 2006; Schriks 2003; Van de Hoef 2007).
Participants
Overall, data on 3760 participants and 9944 teeth were included in the review. The studies examined 6347 teeth that were treated using ART and 3204 that received a conventional treatment. One study did not report the teeth treated by group (Van den Dungen 2004).
The mean age of the participants was 25.42 years (ranging from 3 to 101 years). Forty‐eight per cent of participants were male.
Only Eden 2006 reported the baseline dmft index (average number of decayed, missing and filled primary teeth) with a mean dmft of 6.9. Two studies reported a baseline DMFT (average number of decayed, missing and filled permanent teeth) index ranging between 1.0 to 28.54 (Da Mata 2015; Lo 2006).
Eleven trials included only primary teeth, with participants' age ranging from 3 to 13 years (De Menezes 2009; Eden 2006; Lin 2003; Ling 2003; Luz 2012; Miranda 2005; Roeleveld 2006; Schriks 2003; Van de Hoef 2007; Van den Dungen 2004; Yu 2004). Four trials evaluated permanent teeth with participants aged between 7 to 101 years (Cruz 2016; Da Mata 2015; Estupiñan‐Day 2006; Lo 2006).
Interventions
The key results of this review are from the nine included studies that evaluated the effects of ART compared to conventional treatment using the same restorative material in both arms:
seven studies including a total of 1402 participants compared ART using H‐GIC (high viscosity glass ionomer cement) with conventional treatment using H‐GIC in primary teeth (De Menezes 2009; Lin 2003; Roeleveld 2006; Schriks 2003; Van de Hoef 2007; Van den Dungen 2004; Yu 2004);
one study with 160 participants compared ART using composite with conventional treatment using composite in primary teeth (Eden 2006);
one study with 75 participants compared ART using RM‐GIC (resin‐modified glass ionomer cement) with conventional treatment using RM‐GIC in permanent teeth (Cruz 2016).
Five included studies compared ART versus conventional treatment but used different restorative materials in each arm:
one study with 106 participants compared ART using H‐GIC versus conventional treatment using amalgam in primary teeth (Miranda 2005);
one study with 80 participants compared ART using GIC versus conventional treatment using amalgam in primary teeth (Ling 2003) and one study in permanent teeth (1629 participants) (Estupiñan‐Day 2006);
one study with 30 participants compared ART using H‐GIC versus conventional treatment using composite in primary teeth (Luz 2012);
two studies with 210 participants compared ART using H‐GIC versus conventional treatment using RM‐GIC in permanent teeth (Da Mata 2015; Lo 2006).
Only one study used local anaesthesia with an ART group (Van de Hoef 2007). This was a four‐armed study that used local anaesthesia in two of the four arms (one ART and one conventional treatment). Four other studies reported the use of local anaesthesia with conventional treatment (Da Mata 2015; De Menezes 2009; Lo 2006; Luz 2012); five studies reported that it was not used (Eden 2006; Miranda 2005; Roeleveld 2006; Schriks 2003; Yu 2004); and five studies did not report whether or not local anaesthesia was used (Cruz 2016; Estupiñan‐Day 2006; Lin 2003; Ling 2003; Van den Dungen 2004).
Six studies evaluated the effects of ART on multi‐surface caries lesions (Eden 2006; Luz 2012; Roeleveld 2006; Schriks 2003; Van de Hoef 2007; Van den Dungen 2004). Four trials evaluated both single and multi‐surface lesions (Da Mata 2015; De Menezes 2009; Miranda 2005; Yu 2004). Two trials evaluated root lesions (Cruz 2016; Lo 2006). Three studies did not specify cavity type (Estupiñan‐Day 2006; Lin 2003; Ling 2003).
Most studies reported that the interventions were delivered by the dentist or by the dentist and dental students (Schriks 2003; Van de Hoef 2007; Van den Dungen 2004), or by dentists and dental hygienists (Estupiñan‐Day 2006).
Outcomes
Four studies measured pain (De Menezes 2009; Estupiñan‐Day 2006; Luz 2012; Miranda 2005); one study did not report whether anaesthesia was used (Estupiñan‐Day 2006); in two studies, local anaesthesia was given in the conventional treatment arm only (De Menezes 2009; Luz 2012); and the cavity preparation was different in the arms of one study (Miranda 2005).
Restoration failure was assessed in 13 studies (Cruz 2016; Da Mata 2015; Eden 2006; Estupiñan‐Day 2006; Lin 2003; Ling 2003; Lo 2006; Luz 2012; Miranda 2005; Roeleveld 2006; Van de Hoef 2007; Van den Dungen 2004; Yu 2004). We pooled the results of the studies only if the same restorative material was used in the intervention and comparison arms.
None of the studies measured adverse effects.
Secondary/recurrent caries were measured in four studies (Cruz 2016; Miranda 2005; Roeleveld 2006; Yu 2004).
Other aspects of participant experience were measured in four studies: discomfort (Schriks 2003; Van de Hoef 2007); anxiety (Eden 2006); acceptability (Luz 2012); co‐operation (Estupiñan‐Day 2006; Ling 2003).
Two studies assessed cost‐effectiveness (Da Mata 2015; Estupiñan‐Day 2006).
We did not carry out meta‐analysis where different restorative materials were used in trial arms or local anaesthesia was used in only one study arm, as discussed above. In these cases, the data were narratively presented.
Excluded studies
We excluded 27 studies (see Characteristics of excluded studies). The reasons for exclusion were:
did not compare ART with conventional treatment (nine studies);
the ART technique was modified (14 studies);
not randomised (four studies).
Risk of bias in included studies
All studies were judged to be at overall high risk of bias (see Figure 2; Figure 3).
Allocation
Random sequence generation
Of 15 included studies, nine adequately reported the methods used to generate the randomisation sequence, which included computerised sequence generation (Da Mata 2015; De Menezes 2009; Eden 2006; Estupiñan‐Day 2006; Lo 2006; Van de Hoef 2007), ballot box (Luz 2012), or table of random numbers (Cruz 2016; Miranda 2005). We classified the other studies as 'unclear' as authors mentioned that the clinical trial was randomised but did not report further details.
Allocation concealment
Only three studies adequately reported allocation concealment using sealed envelopes (Cruz 2016; Miranda 2005) or centralised assignment (Estupiñan‐Day 2006). In the remaining studies this was not specified and therefore, we classified them as 'unclear'.
Blinding
Blinding of participants and personnel
Given the nature of the intervention, it is not feasible to blind participants and operators to the type of instruments (i.e. manual or rotary) used for restoration. Therefore, both participants and operators were aware of type of intervention.
Blinding of outcome assessors
It is, however, possible to blind outcome assessors to the type of intervention. The outcome assessors were blind in the eight studies that used the same restorative materials for both the intervention and comparison groups. We considered these studies to be at low risk of bias (Cruz 2016; Da Mata 2015; Eden 2006; Lo 2006; Miranda 2005; Van de Hoef 2007; Van den Dungen 2004; Yu 2004). One study reported that assessors were not blind and therefore we rated it as 'high risk' (Ling 2003). Other studies did not report blinding of outcome assessor and were rated as 'unclear'.
Incomplete outcome data
All trials reported if there were any participants who were lost to follow‐up. However, only six studies reported the reasons for dropout (Cruz 2016; Da Mata 2015; Lo 2006; Luz 2012; Miranda 2005; Van de Hoef 2007). We assessed seven studies as 'high risk' of bias because they had losses to follow‐up over 20% (Da Mata 2015: Eden 2006; Estupiñan‐Day 2006; Lo 2006; Van de Hoef 2007; Van den Dungen 2004; Yu 2004), which was higher than had been estimated in the sample size calculation. We assessed the remaining studies as 'low' risk of attrition bias.
Selective reporting
We judged seven studies to be at 'high' or 'unclear' risk of selective reporting bias (Da Mata 2015; Eden 2006; Estupiñan‐Day 2006; Ling 2003; Schriks 2003; Van de Hoef 2007; Van den Dungen 2004). Estupiñan‐Day 2006 did not report the results at three years' follow‐up and Van den Dungen 2004 did not report results at follow‐ups before three years. Other studies reported incomplete data for the follow‐ups.
Other potential sources of bias
We assessed three studies as having no other potential sources of bias (Eden 2006; Miranda 2005; Schriks 2003).
We judged four studies to be 'unclear' as they did not provide information about either important baseline characteristics of the included participants or co‐interventions, or both (De Menezes 2009; Luz 2012; Roeleveld 2006; Van den Dungen 2004).
We assessed eight studies as 'high risk' of other potential sources of bias. In addition to failing to provide information about baseline characteristics, Cruz 2016 did not consider the paired data in their analysis. Lin 2003 and Van de Hoef 2007 did not consider the intracluster coefficient. Ling 2003, Lo 2006 and Yu 2004 did not consider the paired data in their analysis. Da Mata 2015 had an imbalance in DMFT score between groups. Estupiñan‐Day 2006 did not report DMF scores or information about supply of water fluoridation between countries and their analysis did not consider the intracluster correlation coefficient.
Effects of interventions
See: Table 1; Table 2; Table 3
Comparison 1: ART using H‐GIC versus conventional treatment using H‐GIC
Seven studies reported data for this comparison in primary teeth: De Menezes 2009; Lin 2003; Roeleveld 2006; Schriks 2003; Van de Hoef 2007; Van den Dungen 2004; Yu 2004. Data from Schriks 2003 were not useable.
Restoration failure
Five studies, which randomised 959 participants, reported data for restoration failure in the primary dentition with follow‐ups of between 12 and 36 months (Lin 2003; Roeleveld 2006; Van de Hoef 2007; Van den Dungen 2004; Yu 2004). The odd ratios (OR) of restoration failure were 1.60 times higher in the ART arm than in the conventional arm, over a follow‐up period of 12 to 24 months (OR 1.60, 95% CI 1.13 to 2.27; I2 = 0%, 643 participants analysed; Analysis 1.1). The quality of evidence was downgraded by two levels from 'high' to 'low' due to serious concerns regarding risk of performance bias in all five studies, attrition bias in three studies (Yu 2004; Van de Hoef 2007; Van den Dungen 2004), and reporting bias in two studies (Van de Hoef 2007; Van den Dungen 2004) (Analysis 1.1; Figure 4; Table 1).
1.1. Analysis.
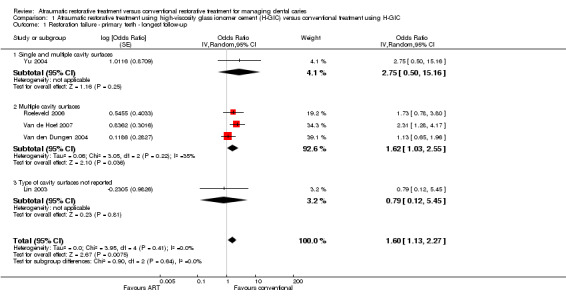
Comparison 1 Atraumatic restorative treatment using high‐viscosity glass ionomer cement (H‐GIC) versus conventional treatment using H‐GIC, Outcome 1 Restoration failure ‐ primary teeth ‐ longest follow‐up.
4.
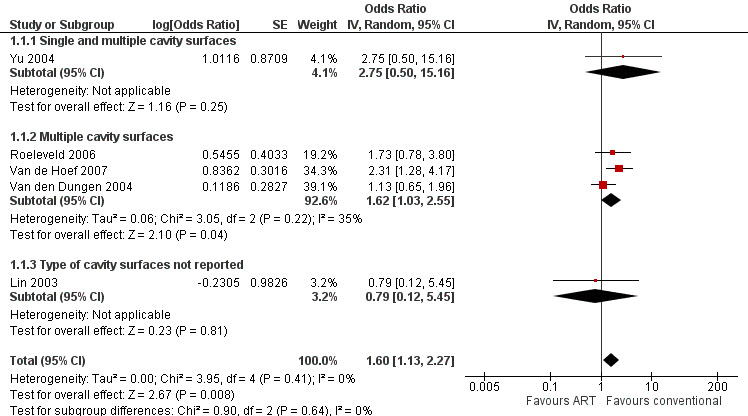
Forest plot of comparison 1. Atraumatic restorative treatment using high‐viscosity glass ionomer cement (H‐GIC) versus conventional treatment using H‐GIC, outcome: 1.1 restoration failure (primary teeth) ‐ longest follow‐up
We carried out subgroup analysis to investigate the impact of cavity type on restoration failure. One study with 27 participants included single and multiple surfaces (Yu 2004). Three studies with 558 participants reported on multiple surfaces only (Roeleveld 2006; Van de Hoef 2007; Van den Dungen 2004). One study with 58 participants did not report the type of cavity treated (Lin 2003). The Chi2 test did not show any evidence of a difference according to cavity type (Chi2 = 0.90, df = 2, P = 0.64, I2 = 0%).
Pain
One study, which randomised 40 participants, reported data for pain in the primary dentition for children aged between four and seven years. ART may reduce the pain during procedure compared with control treatment (MD ‐0.65, 95% CI ‐1.38 to 0.07; 40 participants analysed; Analysis 1.2) (De Menezes 2009). The evidence was downgraded one level because it is a single study (indirectness) and one level because of serious concern regarding high risk of performance bias (Table 1).
1.2. Analysis.
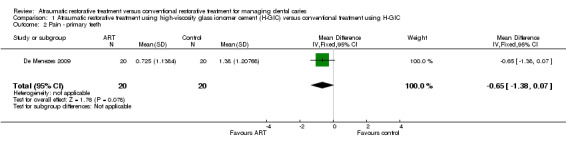
Comparison 1 Atraumatic restorative treatment using high‐viscosity glass ionomer cement (H‐GIC) versus conventional treatment using H‐GIC, Outcome 2 Pain ‐ primary teeth.
Secondary outcomes
Secondary caries
Two studies reported on secondary caries, but this outcome was not reported by trial arm (Yu 2004; Roeleveld 2006).
Participant experience (discomfort)
One study that reported the results of treating multiple lesions in primary dentition, found that the odds of discomfort were reduced with ART in children between six and eight years of age (OR 0.95, 95% CI 0.51 to 1.79; 220 participants analysed; Analysis 1.3) (Van de Hoef 2007). Local anaesthetic was administered in the intervention and comparison groups.
1.3. Analysis.
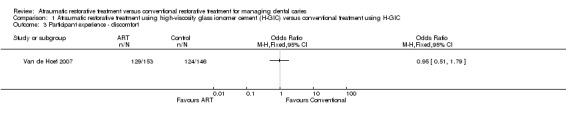
Comparison 1 Atraumatic restorative treatment using high‐viscosity glass ionomer cement (H‐GIC) versus conventional treatment using H‐GIC, Outcome 3 Participant experience ‐ discomfort.
Other outcomes
No studies reported on restoration failure in permanent dentition, adverse events, or costs for this comparison.
Comparison 2: ART using composite versus conventional treatment using composite
Restoration failure
One study, which randomised 160 participants with a mean age of seven years, reported data for restoration failure in multi‐surface lesions of primary dentition with follow‐up at 24 months (Eden 2006). The odds of restoration failure were slightly greater with ART than conventional treatment, however the 95% CI included the possibility that ART both increased the risk of restoration failure and reduced restoration failure, so this result is inconclusive (OR 1.11, 95% CI 0.54 to 2.29, 57 participants analysed; Analysis 2.1). We downgraded the quality of evidence by three levels: one level because the information was based on a single study comprising participants of a very narrow age range (indirectness) and two levels because of very serious concerns regarding risk of bias (high risk of performance bias and attrition bias (103 children (64%) lost to follow‐up at 24 months)) (Table 2).
2.1. Analysis.
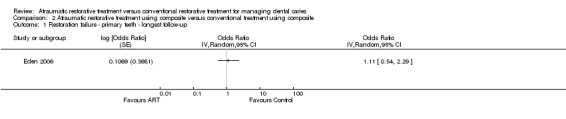
Comparison 2 Atraumatic restorative treatment using composite versus conventional treatment using composite, Outcome 1 Restoration failure ‐ primary teeth ‐ longest follow‐up.
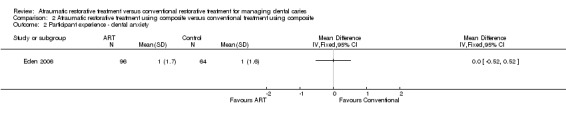
Participant experience (dental anxiety)
Eden 2006 was the only study to report on participant experience (dental anxiety). The authors reported no observed difference in mean dental anxiety as measured by the Venham Picture test (MD 0.00, 95% CI ‐0.52 to 0.52; 57 participants analysed; Analysis 2.2).
2.2. Analysis.
Comparison 2 Atraumatic restorative treatment using composite versus conventional treatment using composite, Outcome 2 Participant experience ‐ dental anxiety.
Other outcomes
No studies reported on pain, restoration failure in the permanent dentition, adverse events, secondary caries, or costs for this comparison.
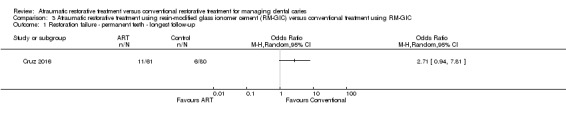
Comparison 3: ART using RM‐GIC versus conventional treatment using RM‐GIC
Restoration failure
One study, which randomised 75 participants with a mean age of 75 years (range 60 to 101 years), reported data for restoration failure in root surfaces of the mature permanent dentition (Cruz 2016). The odds of restoration failure at 24 months' follow‐up were not significantly greater with ART than conventional treatment (OR 2.71, 95% CI 0.94 to 7.81; 64 participants analysed; Analysis 3.1). We downgraded the quality of evidence by three levels: one level as the information was based on a single study comprising older adults only (indirectness), one level because of imprecision and one level because of serious concerns regarding risk of bias (high risk of performance bias (11 adults (15%) lost to follow‐up at six months)) (Table 3).
3.1. Analysis.
Comparison 3 Atraumatic restorative treatment using resin‐modified glass ionomer cement (RM‐GIC) versus conventional treatment using RM‐GIC, Outcome 1 Restoration failure ‐ permanent teeth ‐ longest follow‐up.
Secondary caries
One study reported data on secondary caries for this comparison (Cruz 2016). The odds of secondary caries at six months were greater with ART than with conventional treatment (Analysis 3.2).
3.2. Analysis.
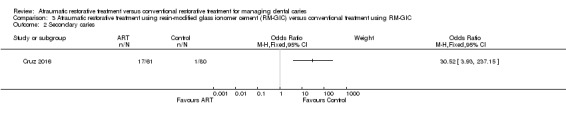
Comparison 3 Atraumatic restorative treatment using resin‐modified glass ionomer cement (RM‐GIC) versus conventional treatment using RM‐GIC, Outcome 2 Secondary caries.
Other outcomes
No studies reported on pain, restoration failure in the primary dentition, adverse events, participant experience, or costs for this comparison.
Comparison 4: ART versus conventional treatment using different restorative materials
Restoration failure
Seven studies used different restorative materials for the intervention and comparator (Da Mata 2015; Estupiñan‐Day 2006; Ling 2003; Lo 2006; Luz 2012; Miranda 2005; Yu 2004) (see Table 4).
1. ART versus conventional treatment studies using different materials in each arm.
| ART with one material versus conventional treatment with another material | |||
| ART material | Conventional treatment material | Outcomes |
Effect estimate OR (95% CI) |
| H‐GIC | Amalgam | Restoration failure ‐primary teeth – 2 studies (Miranda 2005; Yu 2004). Studies reporting on single + multiple lesions | 2.15 (0.73 to 6.35); I2 = 0% |
| Pain (primary dentition) – 1 study (Miranda 2005). Studies reporting on single + multiple lesions | 1.44 (0.45 to 4.60) | ||
| GIC | Amalgam | Restoration failure ‐ primary teeth – 1 study (Ling 2003). Studies reporting on lesion type: not reported | 0.78 (0.30 to 2.02) |
| Restoration failure ‐ permanent, immature teeth – 1 study (Estupiñan‐Day 2006). Studies reporting on lesion type: not reported | 1.71 (1.32 to 2.22) | ||
| Pain ‐ permanent, immature teeth (Estupiñan‐Day 2006) | 0.41 (0.35 to 0.47) | ||
| H‐GIC | Composite and local anaesthetic | Restoration failure ‐ primary teeth – 1 study (Luz 2012). Studies reporting on multiple lesions | 8.00 (1.24 to 51.48) |
| Pain (primary dentition) – 1 study (Luz 2012) | 2.22 (0.51 to 9.61) | ||
| H‐GIC | RM‐GIC and local anaesthetic | Restoration failure ‐ permanent, mature teeth – 2 studies (Da Mata 2015; Lo 2006). Studies reporting on coronal/root caries | 1.46 (0.74 to 2.88); I2 = 0% |
CI: confidence interval; OR: odds ratio
Studies comparing ART using H‐GIC may increase the risk of failure compared with conventional treatment using amalgam in primary teeth (Miranda 2005; Yu 2004).
One study comparing ART using GIC with conventional treatment using amalgam in primary teeth showed that ART may decrease the risk of restoration failure in the primary dentition (Ling 2003). However, in permanent immature teeth, ART resulted in a greater number of failures than conventional treatment (Estupiñan‐Day 2006).
When comparing ART using H‐GIC with conventional treatment using composite in primary teeth, the latter presented significantly fewer failures (Luz 2012).
In root caries of permanent mature teeth, ART with H‐GIC showed greater odds of restoration failure than conventional treatment with RM‐GIC (Da Mata 2015; Lo 2006).
Pain
Of the three studies reporting pain, two RCTs showed increased risk of pain during procedures for participants treated with ART compared with conventional treatment for primary dentition (Luz 2012; Miranda 2005).
One study on permanent immature teeth showed that participants treated with the ART approach presented significantly less pain than the control group (Estupiñan‐Day 2006).
Other outcomes
Ling 2003 assessed participant co‐operation during procedures, showing a co‐operation rate in the ART group significantly higher than in the control group.
No studies reported adverse events, secondary caries, or costs for this comparison.
Discussion
Summary of main results
In total, we included 15 eligible published RCTs in this review, with a total of 3760 participants of whom 48% were men. The mean age of the participants was 25.42 years. The median number of participants per RCT was 291 (range 30 to 2298). Eleven of the trials included primary teeth and four were carried out on permanent teeth. Six studies involved multi‐surface; four involved single and multiple surfaces; two were on root caries and in three trials cavity type was not specified. Most studies used H‐GIC as the restorative material in the ART group; one study used composite resins; and one study used RM‐CGIC. In three studies, the conventional group used amalgam; three studies used RM‐CGIC; two studies used composite resins; and the remaining studies used H‐GIC. We considered the key results to be from the three comparisons that used the same restorative material in both trial arms. The comparison between ART and conventional treatment using different restorative materials was narratively presented.
In primary teeth, there was low‐quality evidence that ART using H‐GIC may increase the risk of restoration failure compared with conventional treatment using H‐GIC. There was low‐quality evidence that ART may reduce pain during the procedure compared with control treatment.
Given the very low‐quality of the evidence from single studies, we are uncertain about the restoration failure of ART compared with conventional treatment using composite over a 24‐month follow‐up period and ART using RM‐GIC in the permanent teeth of older adults with root caries lesions over a six‐month follow‐up period.
None of the included studies reported on adverse effects.
Studies that compared ART with conventional treatment, using different restorative materials in trial arms, did not provide consistent results. The results of these studies for pain were also inconclusive.
Overall completeness and applicability of evidence
Although we included 15 studies in this review, there were only a small number of studies eligible for each comparison.
Only a few studies reported on any of the secondary outcomes.
Only one study that reported on pain was included in the analysis for the pain outcome.
Although the evidence showed that conventional treatment may be more effective than ART technique in primary teeth when the teeth are restored with H‐GIC, these findings should be considered with caution due to the low quality of the evidence. The findings were inconclusive when composite resins or RM‐GIC were used, and applicability to current clinical practice is uncertain due to only one study being included for these comparisons.
There were few available data for secondary caries and participants' experience. No studies reported on adverse events. Only one study reported on the cost of treatment (Da Mata 2015), and concluded that ART was more cost‐effective than conventional treatment for treating older adults. However, these results can only be applied to the healthcare system in Ireland.
In general, the findings of the review should be interpreted with caution because of the high risk of bias in the few studies included and low‐ to very‐low quality of evidence. Clinicians should inform patients of potential pros and cons of each treatment option to enable them to make an informed decision.
Quality of the evidence
We graded the evidence taking into account any limitations in the study design, risk of bias, inconsistency of results, indirectness of evidence, imprecision, presence of publication bias and magnitude of effect estimate.
Evidence on restoration failure was mainly assessed as low‐ to very low‐quality due to high risk of bias and imprecision. High risk of bias was due to performance, attrition, and selective reporting bias. Given that participants and personnel could not be blinded, it was not possible to avoid performance bias. Moreover, the low number of events (i.e. single study) led to additional downgrading for imprecision of the effect estimate.
For the pain outcome, the evidence was of very low quality due to high risk of performance bias and small sample size (i.e. single study).
Potential biases in the review process
We carried out this review according to Cochrane guidelines. We searched a wide range of major electronic databases, without any restriction of language or time. Apart from completed RCTs, we also identified ongoing clinical trials. Where there was uncertainty regarding the studies we contacted the study authors for clarification and further information.
It may be argued that the adjustments to the data made by authors to account for unit of analysis issues could have introduced a risk of bias. We endeavoured to minimise the risk of bias by ensuring that the screening of studies and data extraction were carried out by two authors independently. The data analyses were carried out by two authors and all authors examined the analysis and interpretation of results.
Agreements and disagreements with other studies or reviews
The present review included all available randomised trials comparing ART and conventional treatment in primary and permanent teeth of children and adults. We also identified other systematic reviews on the clinical effectiveness of the ART approach, most of which compared ART to conventional treatment using different restorative materials, mainly amalgam.
Frencken 2004a included only single‐surface ART restorations restored with GIC compared with conventional restorations with amalgam in permanent dentition. They did not show any differences between the two treatments. Mickenautsch 2012 also compared the failure rate in the ART approach versus amalgam fillings in permanent and primary teeth, leaving aside other filling materials. They found no difference between the approaches in both primary and permanent teeth.
Another important difference with some of the existing reviews, such as Frencken 2004a and Van 't Hof 2006 is that we did not introduce any language restrictions and searched a wide range of databases. In our review, we also assessed the quality of the evidence.
Most previous reviews considered survival rate as their only outcome (De Amorin 2012; Frencken 2004a; Van 't Hof 2006), whilst in our review we included a range of primary and secondary outcomes.
Van 't Hof 2006 and De Amorin 2012 assessed the survival of ART restoration using GIC in primary and permanent teeth. Both studies concluded that single‐surface ART restorations using GIC both in primary and permanent dentitions showed higher survival rate compared with multiple‐surface ART restorations.
Pettar 2011 carried out a more comprehensive review to assess the effect of ART on decayed primary and permanent teeth in children between four and 16 years old. It concluded that it was not possible to pool the results due to high clinical heterogeneity. Therefore, it was impossible to get a precise conclusion about the effect of treating childhood caries with ART versus a conventional approach.
Finally, a recent systematic review evaluated the effectiveness of ART in reducing dental anxiety in children with caries lesions in primary teeth compared to conventional treatment (Simon 2017). They concluded that ART was not more beneficial in reducing dental anxiety among paediatric dental patients. We reported a similar finding, although we only included one study for this outcome.
Authors' conclusions
Implications for practice.
The available evidence suggests that atraumatic restorative treatment (ART) using high‐viscosity glass ionomer (H‐GIC) may have a higher risk of restoration failure than conventional treatment for caries lesions in primary teeth, but the evidence is of low‐quality and we cannot rely on the findings. We can draw no conclusions about the effects of ART versus conventional treatment when using resin‐modified glass ionomer (RM‐GIC) or composite because of the very low quality of the evidence.
The low‐ to very low‐quality of the evidence limits the generalisability of these findings. Practitioners and patients should interpret these results with caution. Although there is some evidence in favour of conventional treatment rather than ART in primary teeth, ART may still be considered as a treatment option where access to resources (e.g. dentists, rotary handpieces and electricity) are limited.
Implications for research.
Further well‐designed, adequately powered randomised controlled trials are needed to determine whether the ART approach confers any benefit in terms of success rate or patient experience during treatment in primary and permanent teeth. Future trials should aim to reduce risk of bias and consider potential confounding factors (e.g. type of restoration material, age) in their study designs. Pragmatic, multi‐centre, practice‐based trials, with independent non‐industrial funding could help provide evidence with high validity. Trials should report on time‐ and cost‐related outcomes, participant and operator experience using valid indices.
There are currently four ongoing trials assessing the effectiveness and cost‐effectiveness of ART and their results could provide further insights into this very important area.
What's new
| Date | Event | Description |
|---|---|---|
| 5 March 2018 | Amended | Spelling error in name in Acknowledgements |
Acknowledgements
The review authors would like to thank Cochrane Oral Health and the referees for their comments, support and assistance with conducting this review. We would like to acknowledge Liyuan Ma, Professor Zongdao Shi, Professor Chengge Hua, Dr Fatemeh Mokhtarpour, Professor Bo Su and Frans Banki for their help with translating Chinese and Dutch articles. Thanks are also due to Jo Frecken for providing further details of his study; Anne Littlewood (Cochrane Oral Health) for searching different databases; Marta Roqué‐Figuls (Iberoamerican Cochrane Center) for their contribution in resolving methodological issues; and Dominic Hurst for his contribution in the early stages of this review. We acknowledge those who provided feedback on the review: Helen Worthington, Jan Clarkson, Liz Bickerdike and Ruth Floate; external referees Ivor G. Chestnutt and Margherita Fontana; and Denise Mitchell for copy editing. Last but not least, we would like to thank Laura MacDonald (Cochrane Oral Health) for her generous and continued support throughout this review and, in particular, for facilitating the communication between the review team and Cochrane Oral Health.
Carlos Zaror is a PhD candidate in Methodology of Biomedical Research and Public Health program, Universitat Autònoma de Barcelona (UAB), Barcelona, Spain.
Appendices
Appendix 1. Cochrane Oral Health’s Trials Register search strategy
#1 (cavit* or caries or carious or decay* or lesion* or deminerali* or reminerali*:ti,ab) AND (INREGISTER) #2 (restor* or fill*:ti,ab) AND (INREGISTER) #3 (ultraconservative or "stepwise excavation" or atraumatic or "minimal invasion" or "minimum invasion" or "minim* invasive" or ART:ti,ab) AND (INREGISTER) #4 (cement* or resin* or "glass ionomer" or cemet*:ti,ab) AND (INREGISTER) #5 (seal*:ti,ab) AND (INREGISTER) #6 (#4 and #5) AND (INREGISTER) #7 ((fissure and seal*) or (dental and seal*):ti,ab) AND (INREGISTER) #8 (#3 or #6 or #7) AND (INREGISTER) #9 (#1 and #2 and #8) AND (INREGISTER)
Appendix 2. Cochrane Central Register of Controlled Clinical Trials (CENTRAL) search strategy
#1 MeSH descriptor: [Dental Caries] explode all trees #2 ((teeth near/5 cavit*) or (teeth near/5 caries) or (teeth near/5 carious) or (teeth near/5 decay$) or (teeth near/5 lesion$) or (teeth near/5 deminerali*) or (teeth near/5 reminerali*)) #3 ((tooth near/5 cavit*) or (tooth near/5 caries) or (tooth near/5 carious) or (tooth near/5 decay$) or (tooth near/5 lesion$) or (tooth near/5 deminerali*) or (tooth near/5 reminerali*)) #4 ((dental near/5 cavit*) or (dental near/5 caries) or (dental near/5 carious) or (dental near/5 decay$) or (dental near/5 lesion$) or (dental near/5 deminerali*) or (dental near/5 reminerali*)) #5 ((enamel near/5 cavit*) or (enamel near/5 caries) or (enamel near/5 carious) or (enamel near/5 decay$) or (enamel near/5 lesion$) or (enamel near/5 deminerali*) or (enamel near/5 reminerali*)) #6 ((dentin* near/5 cavit*) or (dentin* near/5 caries) or (dentin* near/5 carious) or (dentin* near/5 decay$) or (dentin* near/5 lesion$) or (dentin* near/5 deminerali*) or (dentin* near/5 reminerali*)) #7 ((root* near/5 cavit*) or (root* near/5 caries) or (root* near/5 carious) or (root* near/5 decay$) or (root* near/5 lesion$) or (root* near/5 deminerali*) or (root* near/5 reminerali*)) #8 MeSH descriptor: [Tooth Demineralization] explode all trees #9 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 #10 [mh ^"Dental restoration, permanent"] #11 [mh ^"Dental restoration, temporary"] #12 (restor* or fill*) #13 (ultraconservative or "stepwise excavation*" or (atraumatic near/6 restor*) or (atraumatic near/6 technique*) or (atraumatic near/6 therap*) or (atraumatic near/6 treat*) or "minimal invasion" or "minimum invasion" or "minim* invasive") #14 ART:ti,ab #15 [mh "Pit and fissure sealants"] #16 ((fissure near/6 seal*) or (dental near/6 seal*)) #17 [mh "Glass ionomer cements"] #18 [mh "Resin cements"] #19 (resin near/6 cement*) #20 (resin near/6 seal*) #21 ("glass ionomer*" or cemet*) #22 #17 or #18 or #19 or #20 or #21 #23 ((dental near/6 seal*) or (fissure near/6 seal*) or (teeth near/6 seal*) or (tooth near/6 seal*)) #24 #22 and #23 #25 #10 or #11 or #12 #26 #13 or #14 or #15 or #16 or #24 #27 #9 and #25 and #26
Appendix 3. MEDLINE Ovid search strategy
exp DENTAL CARIES/
(teeth adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. [mp=title, original title, abstract, name of substance word, subject heading word]
(tooth adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp.
(dental adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp.
(enamel adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp.
(dentin$ adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp.
(root$ adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp.
exp TOOTH DEMINERALIZATION/
or/1‐8
Dental Restoration, Permanent/
Dental Restoration, Temporary/
(restor$ or fill$).mp.
(ultraconservative or "stepwise excavation$" or (atraumatic$ adj6 restor$) or (atraumatic$ adj6 technique$) or (atraumatic$ adj6 therap$) or (atraumatic$ adj6 treat$) or "minimal invasion" or "minimum invasion" or "minim$ invasive").mp.
ART.ab,ti.
exp "Pit and Fissure Sealants"/
((fissure adj6 seal$) or (dental adj6 seal$)).mp.
exp Glass Ionomer Cements/
Resin Cements/
(resin adj6 cement$).mp.
(resin adj6 seal$).mp.
("glass ionomer$" or cemet$).mp.
or/17‐21
((dental adj6 seal$) or (fissure$ adj6 seal$) or (teeth adj6 seal$) or (tooth adj6 seal$)).mp.
22 and 23
10 or 11 or 12
13 or 14 or 15 or 16 or 24
9 and 25 and 26
This subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity‐maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of The Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011](Lefebvre 2011).
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 4. Embase Ovid search strategy
1. exp "DENTAL CARIES"/ 2. (teeth adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 3. (tooth adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 4. (dental adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 5. (enamel adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 6. (dentin$ adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 7. (root$ adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 8. or/1‐7 9. (restor$ or fill$).mp. 10. (ultraconservative or "stepwise excavation$" or (atraumatic$ adj6 restor$) or (atraumatic$ adj6 technique$) or (atraumatic$ adj6 therap$) or (atraumatic$ adj6 treat$) or "minimal invasion" or "minimum invasion" or "minim$ invasive").mp. 11. ART.ab,ti. 12. exp "Fissure sealant"/ 13. ((fissure adj6 seal$) or (dental adj6 seal$)).mp. 14. exp "Glass Ionomer"/ 15. "Resin Cement"/ 16. (resin adj6 cement$).mp. 17. (resin adj6 seal$).mp. 18. ("glass ionomer$" or cemet$).mp. 19. or/14‐18 20. ((dental adj6 seal$) or (fissure$ adj6 seal$) or (teeth adj6 seal$) or (tooth adj6 seal$)).mp. 21. 19 and 20 22. 10 or 11 or 12 or 13 or 21 23. 8 and 9 and 22
This subject search was linked to an adapted version of the Cochrane Embase Project filter for identifying RCTs in Embase Ovid (see http://www.cochranelibrary.com/help/central‐creation‐details.html for information).
1. Randomized controlled trial/ 2. Controlled clinical study/ 3. Random$.ti,ab. 4. randomization/ 5. intermethod comparison/ 6. placebo.ti,ab. 7. (compare or compared or comparison).ti. 8. ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 9. (open adj label).ti,ab. 10. ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 11. double blind procedure/ 12. parallel group$1.ti,ab. 13. (crossover or cross over).ti,ab. 14. ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 15. (assigned or allocated).ti,ab. 16. (controlled adj7 (study or design or trial)).ti,ab. 17. (volunteer or volunteers).ti,ab. 18. trial.ti. 19. or/1‐18 20. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 21. 19 not 20
Appendix 5. LILACS BIREME Virtual Health Library search strategy
Mh "Dental caries" or carie$ [Words] and (Mh "Dental Atraumatic Restorative Treatment" or Atraumatic or Atraumático or "Restaurador sem Trauma") [Words]
This subject search was linked to the Brazilian Cochrane Center filter for LILACs BIREME:
((Pt randomized controlled trial OR Pt controlled clinical trial OR Mh randomized controlled trials OR Mh random allocation OR Mh double‐blind method OR Mh single‐blind method) AND NOT (Ct animal AND NOT (Ct human and Ct animal)) OR (Pt clinical trial OR Ex E05.318.760.535$ OR (Tw clin$ AND (Tw trial$ OR Tw ensa$ OR Tw estud$ OR Tw experim$ OR Tw investiga$)) OR ((Tw singl$ OR Tw simple$ OR Tw doubl$ OR Tw doble$ OR Tw duplo$ OR Tw trebl$ OR Tw trip$) AND (Tw blind$ OR Tw cego$ OR Tw ciego$ OR Tw mask$ OR Tw mascar$)) OR Mh placebos OR Tw placebo$ OR (Tw random$ OR Tw randon$ OR Tw casual$ OR Tw acaso$ OR Tw azar OR Tw aleator$) OR Mh research design) AND NOT (Ct animal AND NOT (Ct human and Ct animal)) OR (Ct comparative study OR Ex E05.337$ OR Mh follow‐up studies OR Mh prospective studies OR Tw control$ OR Tw prospectiv$ OR Tw volunt$ OR Tw volunteer$) AND NOT (Ct animal AND NOT (Ct human and Ct animal)))and not (Ct ANIMAL AND NOT (Ct HUMAN and Ct ANIMAL)))
Appendix 6. BBO BIREME Virtual Health Library search strategy
Mh "Dental caries" or carie$ [Words] and (Mh "Dental Atraumatic Restorative Treatment" or Atraumatic or Atraumático or "Restaurador sem Trauma") [Words]
This subject search was linked to the Brazilian Cochrane Center filter for BBO BIREME:
((Pt randomized controlled trial OR Pt controlled clinical trial OR Mh randomized controlled trials OR Mh random allocation OR Mh double‐blind method OR Mh single‐blind method) AND NOT (Ct animal AND NOT (Ct human and Ct animal)) OR (Pt clinical trial OR Ex E05.318.760.535$ OR (Tw clin$ AND (Tw trial$ OR Tw ensa$ OR Tw estud$ OR Tw experim$ OR Tw investiga$)) OR ((Tw singl$ OR Tw simple$ OR Tw doubl$ OR Tw doble$ OR Tw duplo$ OR Tw trebl$ OR Tw trip$) AND (Tw blind$ OR Tw cego$ OR Tw ciego$ OR Tw mask$ OR Tw mascar$)) OR Mh placebos OR Tw placebo$ OR (Tw random$ OR Tw randon$ OR Tw casual$ OR Tw acaso$ OR Tw azar OR Tw aleator$) OR Mh research design) AND NOT (Ct animal AND NOT (Ct human and Ct animal)) OR (Ct comparative study OR Ex E05.337$ OR Mh follow‐up studies OR Mh prospective studies OR Tw control$ OR Tw prospectiv$ OR Tw volunt$ OR Tw volunteer$) AND NOT (Ct animal AND NOT (Ct human and Ct animal)))and not (Ct ANIMAL AND NOT (Ct HUMAN and Ct ANIMAL)))
Appendix 7. US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) search strategy
atraumatic AND caries
Appendix 8. World Health Organization International Clinical Trials Registry Platform search strategy
atraumatic AND caries
Data and analyses
Comparison 1. Atraumatic restorative treatment using high‐viscosity glass ionomer cement (H‐GIC) versus conventional treatment using H‐GIC.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Restoration failure ‐ primary teeth ‐ longest follow‐up | 5 | Odds Ratio (Random, 95% CI) | 1.60 [1.13, 2.27] | |
| 1.1 Single and multiple cavity surfaces | 1 | Odds Ratio (Random, 95% CI) | 2.75 [0.50, 15.16] | |
| 1.2 Multiple cavity surfaces | 3 | Odds Ratio (Random, 95% CI) | 1.62 [1.03, 2.55] | |
| 1.3 Type of cavity surfaces not reported | 1 | Odds Ratio (Random, 95% CI) | 0.79 [0.12, 5.45] | |
| 2 Pain ‐ primary teeth | 1 | 40 | Mean Difference (IV, Fixed, 95% CI) | ‐0.65 [‐1.38, 0.07] |
| 3 Participant experience ‐ discomfort | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 2. Atraumatic restorative treatment using composite versus conventional treatment using composite.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Restoration failure ‐ primary teeth ‐ longest follow‐up | 1 | Odds Ratio (Random, 95% CI) | Totals not selected | |
| 2 Participant experience ‐ dental anxiety | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 3. Atraumatic restorative treatment using resin‐modified glass ionomer cement (RM‐GIC) versus conventional treatment using RM‐GIC.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Restoration failure ‐ permanent teeth ‐ longest follow‐up | 1 | Odds Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Secondary caries | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cruz 2016.
| Methods |
Design: cluster, parallel RCT (a child is a cluster) Number of participants: 75 Setting: nursing home Country: Colombia Unit of randomisation: participant Unit of analysis: tooth Follow‐up: 6 months Dropout: 14.9 % after 6 months |
|
| Participants |
Number randomised: 75 participants; 174 teeth (73 ART group and 101 CT group)
Number analysed: 64 participants/148 teeth
Age mean and SD (range): 74.9 years (60‐101)
Sex: female 36 (48%), male 39 (52%) Average DMFT score: not reported Dentition: permanent Type of caries lesion: root caries Inclusion criteria: root caries defined as the softening of the root dentin to a depth of ≥ 0.5 mm Exclusion criteria: teeth with extraction indication, lesion close to the dental pulp or pain symptomatology |
|
| Interventions | Two treatment arms:
ART was performed using only manual instrumentation to remove decayed tissue. Cotton rolls and a retraction cord were used to obtain relative isolation of the operative field. 2% chlorhexidine (Clorhexol 0.2 g/100 mL; Farpag®, Bogota, Colombia) was applied for 1 min and the cavity was dried and sealed with aglass ionomer cement modified with light‐curing composite resin (Vitremer™®, 3M ESPE, Seefeld, Germany). Interproximal metal and paper strips were used. Conventional technique was performed using a high‐speed handpiece with irrigation and round diamond burs of different diameters. Cavities were restored with RM‐GIC. Use of anaesthesia was not reported in any group. The interventions were conducted by 2 dentists. |
|
| Outcomes |
|
|
| Notes | Funding: COLCIENCIAS for the Young Researcher Scholarship‐Internship Program Trial register number not reported Sample size calculated Intraexaminer and interexaminer reproducibility not assessed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A series of random numbers was used to fabricate sealed envelopes that were only opened for the random allocation of the participants to each working group (ART or conventional technique with rotary instruments)" |
| Allocation concealment (selection bias) | Low risk | Quote: "A series of random numbers was used to fabricate sealed envelopes that were only opened for the random allocation of the participants to each working group (ART or conventional technique with rotary instruments)" |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comment: no information provided, but the participants could tell whether manual or rotary instruments were used |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comment: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "After six months, the condition of the restorations was assessed by two different prosthodontists, without awareness of the technique that was performed in each participant" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "After six months, 64 participants were evaluated (32 men and 32 women) and 26 restorations (14.9%) were lost. Seven participants changed geriatric institutions and were lost to follow‐up, two died, and the two remaining participants were unreachable at the institution during the time of revision” |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes listed in the methods sections were included. |
| Other bias | High risk | Comment: no information provided about baseline characteristics of included participants. The analysis did not consider the pair data. |
Da Mata 2015.
| Methods |
Design: cluster, parallel RCT (a child is a cluster) Number of participants: 107 Setting: dental school/hospital Country: Ireland Unit of randomisation: participant Unit of analysis: tooth Follow‐up: 6, 12 and 24 months Dropout: 15.8% and 33.6% after 12 and 24 months, respectively |
|
| Participants |
Number randomised: 107 (53 ART group and 54 CT group); 99 received the intervention/306 teeth (142 ART and 158 CT)
Number analysed: 71 participants/217 teeth
Age mean and SD (range): 73 years SD = 6.7 (65‐88)
Sex: female 53 (54%), male 46 (46%) Average DMFT score: 25.74 SD = 6.3 ART/28.54 SD = 5.0 CT Dentition: permanent Type of caries lesion: coronal or root caries Inclusion criteria: > 65 years of age, ≥ 1 dentinal carious lesion with no painful symptomatology, ability to perform usual daily dental care activities such as toothbrushing Exclusion criteria: people with carious teeth with a history of pain, with cavities resulting from attrition, erosion or abrasion, with no caries, and with teeth that were periodontally involved |
|
| Interventions | Two treatment arms:
The ART approach consisted of opening of the cavity with a dental enamel hatchet when necessary, removal of soft, completely demineralised carious tissue with excavators, conditioning of the cavity with polyacrylic acid for 20 s, washing and drying with cotton pellets and restoration with a high‐strength glass ionomer cement (GC Fuji IX). The CT procedure consisted of local anaesthesia, use of rotary instruments for access, rotary and hand instruments for removal of all carious tissue, conditioning of the cavity with a polyacrylic acid for 20 seconds, washing and drying with cotton pellets and a resin‐modified glass ionomer (GC Fuji II LC) to restore it. The interventions were conducted by 2 dentists |
|
| Outcomes |
|
|
| Notes | Funding: Irish Health Research Board Trial register number not reported Sample size calculated Interexaminer reproducibility high (kappa = 0.88) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer‐generated randomisation list, provided by a statistician involved in the study" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The allocation sequence was concealed from the primary researcher treating the participants in sequentially numbered, opaque, sealed envelopes" Comment: unclear if the primary researcher is the same person who performed all restorations |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comment: no information provided, but the participants could tell whether manual or rotary instruments were used |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comment: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Restorations were assessed after 6 months and after a year by a calibrated examiner who was not involved in the placement of restorations, and did not know which treatment had been provided for each case" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: loss to follow‐up 33.6% at 24 months |
| Selective reporting (reporting bias) | Unclear risk | Comment: restorations are not reported individually so we do not know how they compared to the overall average. It may have been space limits rather than deliberate selective reporting that is responsible for this. |
| Other bias | High risk | Comment: imbalance in DMFT score between groups |
De Menezes 2009.
| Methods |
Design: parallel RCT Number of participants: 40 Setting: dental clinic Country: Brazil Unit of randomisation: child Unit of analysis: child Follow‐up: just after treatment Dropout: none |
|
| Participants |
Number randomised (participants): 40 (20 ART group and 20 CT group)
Number analysed: 40
Age mean and SD (range): 5.3 years SD = 1.2 (4‐7) Gender: female 19 (47.5%) and male 21 (52.5%) Average DMFT score: not reported Dentition: primary Type of caries lesion: occlusal caries Inclusion criteria: at least one carious lesion involving the occlusal surface of primary molars without pulp involvement and without pain Exclusion criteria: not reported |
|
| Interventions | Two treatment arms:
ART group was treated using hand instruments only. The restorative material used was the H‐GIC, Fuji IX (GC®, Japan). Conventional restorative treatment was performed under local anaesthesia and rubber dam protection using rotary equipment. Cavity cleaning was restricted to removing all carious tissues in enamel and dentine using the drill. The restorative material used was the H‐GIC, Fuji IX (GC®, Japan) The interventions were conducted by 1 dentist |
|
| Outcomes |
|
|
| Notes | Funding: Brazilian Dental Association Trial register number not reported Sample size not calculated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The children were randomly allocated to a test and control group using a series of computer generated random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Comment: not reported |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comment: no information provided, but the participants could tell whether manual or rotary instruments were used |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comment: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no dropouts. All participants assessed |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes listed in the methods sections included |
| Other bias | Unclear risk | Comment: no information provided about baseline characteristics of included participants |
Eden 2006.
| Methods |
Design: cluster, split‐mouth RCT Number of participant: 160 Setting: dental clinic Country: Turkey Unit of randomisation: tooth Unit of analysis: tooth pairs Follow‐up: 6, 12 and 24 months Dropout: 22.5%, 29.4% and 64.4% after 6, 12 and 24 months, respectively |
|
| Participants |
Number randomised (participants): 160 children (96 ART group and 64 CT group)/325 teeth (162 ART and 163 conventional)
Number analysed: 57 children/100 teeth
Age mean and SD (range): 7.0 SD = 0.3
Gender: female 82 (52%), male 75 (48%) Average DMFT score: 6.9 SD = 2.5 Dentition: primary Type of caries lesion: multiple surface caries lesion Inclusion criteria: ≥ 1 bilaterally matched pair of primary molars with class II cavited dentin lesions in different quadrants or jaws and with cavited dentin lesions presenting with an opening wide enough for the smallest excavator (0.9 mm) to penetrate Exclusion criteria: cavities dentin lesions that had pulpal involvement were excluded |
|
| Interventions | Two treatment arms:
The ART procedure consisted of widening the opening in small cavities and removing thin enamel in larger cavity openings with a dental hatchet, until the enamel was free of visible demineralisation. Soft infected dentin was excavated from the cavity walls and floor with spoon excavators. No local anaesthesia was administered. Cavities were restored with composite (Pertac II) The CT procedure consisted of removing carious tissues using a micromotor and a handpiece with diamond and steel burs. The cavity was prepared following the minimal intervention concept. No local anaesthesia was administered. An omni‐matrix and interdental wooden wedges were placed before restoration. The cavities were restored with composite. The interventions were conducted by 3 dentists. |
|
| Outcomes |
|
|
| Notes | Funding: WHO Collaborating Centre of the Radboud University Medical Centre in Nijmegen, The Netherlands, Hu‐Friedy, Germany, and 3M ESPE, Germany Trial register number not reported Sample size not calculated Interexaminer reproducibility moderate (kappa = 0.41) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The cavitied dentin lesions were randomly assigned to the treatment group after stratification for gender, operator, upper/lower jaw, and when needed according to left/right side of the mouth using a validated computer software program (trial Balance)" |
| Allocation concealment (selection bias) | Unclear risk | Comment: not reported |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comment: participants aware of different treatments |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comment: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Two calibrated independent examiners who were blinded to the treatment method provided evaluated the occlusal and approximal parts of the restorations after 6 months, 1 year and 2 years..." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Ten children with 33 restorations were not evaluated at any evaluation time" "The total number of children evaluated after 0.5, 1 and 2 years was 124, 113 and 57, respectively" Comment: loss to follow‐up high at 2 years (64.4%) |
| Selective reporting (reporting bias) | Unclear risk | Comment: some results were reported in another study. Maybe there are other results not reported. |
| Other bias | Low risk | Comment: split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair. |
Estupiñan‐Day 2006.
| Methods |
Design: cluster, parallel RCT Number of participants: 1629 children Setting: community setting Country: Ecuador, Panama and Uruguay Unit of randomisation: child Unit of analysis: tooth Follow‐up: 12, 24 and 36 months Dropout: 15.6% and 51.47% after 12 and 24 months, respectively |
|
| Participants |
Number randomised (participants): 1629 children (868 ART group and 761 CT group)/ 6773 teeth (4976 ART and 1797 conventional)
Number analysed: 3287 teeth
Age mean and SD (range): 7‐9 years
Gender: female 843 (51.38%), male 786 (48.62%) Average DMFT score: not reported Dentition: permanent Type of caries lesion: not reported Inclusion criteria
Exclusion criteria
|
|
| Interventions | The study has 3 arms:
The ART procedure consisted of a manual excavation of dental caries and restoration with glass ionomer. CT with amalgam. No more details Use of anaesthesia was not reported in any group. The interventions were conducted by dentists and dental hygienists. |
|
| Outcomes |
|
|
| Notes | Funding: Inter‐American Development Bank Trial register number not reported Sample size calculated Results at 3 years not reported Interexaminer reproducibility > 0.75 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "In order to ensure balanced treatment groups within the schools, children were randomised in blocks of 4 or 10 depending on the size of the school. Schools with 15 children or fewer and, whenever possible, within a reasonable distance from one another were collapsed. The randomisation was accomplished using a computer‐based (SAS) block randomisation using random number seeds from a random digit table" |
| Allocation concealment (selection bias) | Low risk | Quote: "Assignment for all three countries was done in Washington, DC to ensure consistency" |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comments: no information provided, but the participants could tell whether manual or rotary instruments were used |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comments: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "the PRAT project required its restoration evaluators to be trained and calibrated according to strict standard criteria so that their assessments were reliable and comparable" "At the end of the third year, an external international evaluator will conduct a final evaluation of the condition of restorations performed during the course of the project" Comment: not clear whether the assessments at 1 and 2 years were made by an operator who was not involved in the treatment phase |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comment: loss to follow‐up high at 2 years (51.47%) |
| Selective reporting (reporting bias) | High risk | Comment: results at 3 years not reported |
| Other bias | High risk | Comment: DMF scores not reported. Information about supply of water fluoridation between countries not provided. The analysis did not consider the intracluster correlation coefficient. |
Lin 2003.
| Methods |
Design: cluster, parallel RCT (a child is a cluster) Number of participants: 58 Setting: not reported Country: China Unit of randomisation: child Unit of analysis: tooth Follow‐up: 6, 12 and 24 months Dropout: none |
|
| Participants |
Number randomised (participants): 58 (30 ART group and 28 CT group)/248 teeth (138 ART group and 110 CT group) Number analysed: 58 children/248 teeth Age mean and SD (range): 3‐5 years Gender: female 34 (58,6%), male 24 (41.4%) Average DMFT score: not reported Dentition: primary Type of caries lesion: not reported Inclusion criteria: primary teeth with carious lesion of enamel or dentin Exclusion criteria: not reported |
|
| Interventions | Two treatment arms:
The ART procedure consisted of opening the cavity using enamel hatchet and sharp excavators to remove the caries. Caries was removed from the dentino‐enamel junction using sharp spoon excavators of appropriate size before proceeding on to the floor of the cavity. The glass ionomer silver reinforced restorative was placed in the cavity. In CT caries was removed from the dentino‐enamel junction using high‐speed turbine before proceeding on to the floor of the cavity. The surfaces were then washed with water‐moistened cotton pellets and then blotted dry with fresh cotton pellets. The glass ionomer silver reinforced restorative were placed in the cavity. Use of anaesthesia was not reported in any group. The interventions were conducted by a dentist. |
|
| Outcomes | Success rate was assessed as:
|
|
| Notes | Funding not stated Trial register number not reported Sample size not calculated Intraexaminer reproducibility not assessed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The children were randomly divided into two groups" Comments: method not described. |
| Allocation concealment (selection bias) | Unclear risk | Comments: not reported |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comments: no information provided, but the participants could tell whether manual or rotary instruments were used. |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comments: blinding not possible ‐ operator knew the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comments: not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: no dropouts. All participants were assessed. |
| Selective reporting (reporting bias) | Low risk | Comments: results of all outcomes reported |
| Other bias | High risk | Comments: baseline characteristics and details about co‐interventions were not reported. Analysis did not consider the intracluster correlation coefficient. |
Ling 2003.
| Methods |
Design: split‐mouth RCT Number of participants: 106 Setting: hospital Country: China Unit of randomisation: tooth Unit of analysis: tooth pairs Follow‐up: 6, 12 and 24 months Dropout: none |
|
| Participants |
Number randomised (participants): 106 participants/212 teeth (106 ART group and 106 CT group)
Number analysed: 106 children/212 teeth
Age mean and SD (range): (6‐8 years) Gender: 53 male (50%) and 53 female (50%) Average DMFT score: not reported Dentition: primary Type of caries lesion: not reported Inclusion criteria:
Exclusion criteria:
|
|
| Interventions | Two treatment arms:
For ART group the cavities were filled with FX glass ionomer cement (Japan Co., Ltd), after removing carious tooth tissues and undermined enamel with a sharp excavator. In CT the cavities were filled with silver amalgam (China Iron & Steel Research Institute Group), after removing carious tooth tissues and preparation of cavities with high‐speed turbine drill. Use of anaesthesia was not reported in any group. All interventions were conducted by the same dentist |
|
| Outcomes |
|
|
| Notes | Funding not stated Trial register number not reported Samples size not calculated Intraexaminer reproducibility not assessed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Self‐control method and randomised method were used to allocate teeth into two groups” Comments: method not described |
| Allocation concealment (selection bias) | Unclear risk | Comments: not reported |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comments: participant aware of different treatments |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comments: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: “all the treatments and clinical examinations were done by the same operator” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: all participants were assessed |
| Selective reporting (reporting bias) | Unclear risk | Comments: some outcomes were not reported in the methods section but were shown in the results. |
| Other bias | High risk | Comments: analysis did not consider the paired data |
Lo 2006.
| Methods |
Design: cluster, parallel RCT (an individual is a cluster) Number of participant: 103 Setting: nursing homes Country: China Unit of randomisation: participant Unit of analysis: tooth Follow‐up: 6 and 12 months Dropout: 25.2% after 12 months |
|
| Participants |
Number randomised (participants): 103 participants/162 teeth (78 ART group and 84 CT group) Number analysed: 77 participants/122 teeth Age mean and SD (range): 78.6 years Sex: female 72 (69.9%), male 31 (30.1%) Average DMFT score: 1.0 Dentition: permanent Type of caries lesion: root caries Inclusion criteria: > 60 years of age, having basic self‐care ability, and with root caries lesions ≥ 1 mm in depth Exclusion criteria: lesions involving or judged to be very close to the dental pulp |
|
| Interventions | Two treatment arms:
The ART technique consisted of removing all the soft dentin only with hand instruments. Cotton rolls and gingival retraction cord were used when necessary for field isolation and moisture control. Cavity was conditioned for 10‐15 s. The prepared cavity was restored with a high‐strength chemically cured glass‐ionomer material (Ketac Molar, 3M ESPE, Seefeld, Germany). A clear cellulose matrix was used to build up the contour of the root. CT used local anaesthesia when required. Cotton rolls and gingival retraction cord were used for field isolation and moisture control. Decayed tooth tissues were removed by means of dental burs until the floor and walls of the cavity were found to be hard. The prepared cavity was conditioned with polyacrylic acid for 10‐15 seconds, washed, dried, and restored with a resin modified glass‐ionomer material (Fuji II LC, GC Corporation, Tokyo, Japan) The interventions were conducted by 1 dentist. |
|
| Outcomes |
|
|
| Notes | Funding: Hong Kong Research Grants Council (Ref. HKU 7244/02M) Trial register number: not reported Sample size calculated Intraexaminer reproducibility evaluated but not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We tossed a coin to allocate the selected lesions randomly to receive one of the two study treatments" "For patients who had 2 root‐caries lesions, both types of treatment were provided" "The treatment assignment procedure was repeated if there were more than 2 lesions in a subject" |
| Allocation concealment (selection bias) | Unclear risk | Comments: not reported |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comments: no information provided, but the participants could tell whether manual or rotary instruments were used |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comments: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Restorations was assessed at six‐month intervals by a dentist who was not involved in the provision of the treatments, and who did not know which technique had been used in placing the restoration” “Blindness was possible because tooth‐colored glass‐ionomer material was used in both techniques, and the restorations had similar appearances." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "The reasons for dropout were that the patients had died, were too ill to be examined, or were not at the home on the examination day" Comments: while the causes of dropout are indicated, the loss was high (25%) |
| Selective reporting (reporting bias) | Low risk | Comments: all outcomes listed in the methods sections were included. |
| Other bias | High risk | Comments: the analysis did not consider the paired data. |
Luz 2012.
| Methods |
Design: Parallel RCT Number of participant: 30 Setting: school of dentistry Country: Brazil Unit of randomisation: child Unit of analysis: child Follow‐up: 6 month Dropout: 23.3% after 6 months |
|
| Participants |
Number randomised (participants): 30 children (16 ART group and 14 CT group)
Number analysed: 23 children
Age mean and SD (range): 4‐7 years
Gender: Female 16 (53.3%), male 14 (46.7%) Average DMFT score: not reported Dentition: primary Type of caries lesion: approximal caries lesion Inclusion criteria: children who had at least one approximal active caries lesion in a primary molar and that was accessible to hand instruments. Exclusion criteria: children with spontaneous pain |
|
| Interventions | Two treatment arms:
Children in the ART Group were treated according to ART approach using only hand instruments, no anaesthesia and restorative material was glass ionomer (Ketak‐Molar 3‐M ESPE, St. Paul, Minnesota). Only the demineralised carious tissue and unsupported enamel were removed. Matrix band and wooden wedges were used. Children in CT group were treated with local anaesthesia, rubber dam, rotary instruments and the cavity was filled with composite resin ( Z 350 3‐M ESPE, St. Paul, Minnesota). Only the demineralised carious tissue and unsupported enamel were removed. Matrix band and wooden wedges were used. The interventions were conducted by 1 dentist. |
|
| Outcomes |
|
|
| Notes | Funding not stated Trial register number not reported Sample size not calculated Intraexaminer reproducibility high ‐ kappa > 0.8 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomly assigned to one of the treatment group after stratification for tooth in the upper/lower jaw using a ballot box" |
| Allocation concealment (selection bias) | Unclear risk | Comments: not reported |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comments: no information provided, but the participants could tell whether manual or rotary instruments were used |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comments: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comments: not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: for the outcomes evaluated, all participants were assessed |
| Selective reporting (reporting bias) | Low risk | Comments: all prespecified (primary and secondary) outcomes reported |
| Other bias | Unclear risk | Comments: baseline characteristics and details about co‐interventions not reported |
Miranda 2005.
| Methods |
Design: split‐mouth RCT Number of participant: 80 Setting: dental clinic Country: Brazil Unit of randomisation: tooth Unit of analysis: tooth pairs Follow‐up: 6 and 12 months Dropout: 3.75% after 6 months and 12.5% after 12 months |
|
| Participants |
Number randomised (participants): 80 children/160 teeth (80 ART group and 80 CT group)
Number analysed: 70 children/140 teeth
Age mean and SD (range): 5.71 years (3‐9 years)
Gender: female 33 (41.25%), male 47 (58.75%) Average DMFT score: not reported Dentition: primary Type of caries lesion: single and multiple surface caries lesion Inclusion criteria
Exclusion criteria
|
|
| Interventions | Two treatment arms:
Teeth in the ART group were treated with hand instruments only. The restorative material was glass ionomer (Ketak‐Molar 3‐M ESPE). In CT group, cavities were filled with silver amalgam (SDI), after removing carious tooth tissues and preparation of cavities with high and low‐speed drill. Both treatments were started without use of anaesthesia. The interventions were conducted by 1 dentist |
|
| Outcomes |
|
|
| Notes | Funding not stated Trial register number no reported Sample size calculated Intraexaminer reproducibility not assessed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We used a simple randomised to two treatment cited by Pocock (1993) and a table of random numbers, randomised formed by digits from 0 to 9 in a sequence from right to left and from top to bottom" |
| Allocation concealment (selection bias) | Low risk | Quote: "The concealment was performed through sealed envelopes numbered 1‐100, containing inside cards with corresponding number and an indication of the first treatment, obtained by the method mentioned, being sequentially archived. The listing and envelopes were made by a professional different to the researcher." |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comments: participant aware of different treatments |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comments: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The restorations were evaluated by paediatric dentist who did not perform any treatment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: low dropout rate (12.5%), reasons for missing outcome data unlikely to be related to true outcome |
| Selective reporting (reporting bias) | Low risk | Comments: all prespecified (primary and secondary) outcomes reported |
| Other bias | Low risk | Comments: split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair |
Roeleveld 2006.
| Methods |
Design: parallel RCT Number of participants: 217 Setting: not reported Country: Tanzania Unit of randomisation: child Unit of analysis: child Follow‐up: 7 and 12 months Dropout: 10.1% and 11.1% after 7 and 12 months, respectively |
|
| Participants |
Number randomised (participants): 217 participants in 3 arms (77 ART group, 72 CT group and 68 CarisolvTM group)
Number analysed: 109 children (57 ART and 52 conventional)
Age mean and SD (range): 7.5 years SD = 0.57 (6‐7 years)
Gender: female 123 (56,68%), male 94 (43.32%) Average DMFT score: not reported Dentition: primary Type of caries lesion: multiple‐surface caries lesion Inclusion criteria: ≥ 1 class II cavity in a primary molar, accessible to hand instruments, with an untreated tooth adjacent to cavity, and no pulp exposure Exclusion criteria: not reported |
|
| Interventions | Three treatment arms:
With the ART approach, only hatchets and excavators were used. The CT group was treated by excavation with a stainless steel bur without water cooling (speed: ± 750 rpm). For CarisolvTM group, excavation was performed with special hand instruments after the application of the gel. In all groups a matrix band and wooden wedges were inserted after cleaning the cavity. Cotton wool rolls were used to isolate the cavity so as to prevent contamination with saliva and/or blood. The smear layer was removed from the dentine by conditioning for 15 seconds and rinsed and dried with respectively 3 wet and 3 dry cotton pellets. Hand‐mix GIC (Fuji IX) was placed into the cavity, using the finger press method; Vaseline was applied to the index finger and pressed on for 3 seconds, the finger being removed sideways. No local anaesthesia was used in any group. Interventions were conducted by 4 dentists. |
|
| Outcomes |
|
|
| Notes | Funding: GC Europe provided the GIC; Medi Team provided Carisolv and blunt instruments Trial register number not reported Sample size not calculated Interexaminer reproducibility ranged between 0.66 and 0.84 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “217 children were randomly divided into three groups for treatment with one of three different methods” Comments: insufficient information about the sequence generation process |
| Allocation concealment (selection bias) | Unclear risk | Comments: not reported |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comments: no information provided, but the participants could tell whether manual or rotary instruments were used |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comments: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: “The restorations were evaluated after 7 months (first evaluation) and one year (second evaluation) by 4 final‐year students from The Netherlands” Comments: unclear if different from who was involved in placing them. Blinding would have been possible given that all restorations were GIC. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "There were 193 children present at the second evaluation (t=2), 149 of them could participate in the scoring for success or failure of the restorations." Comments: loss to follow‐up was low at 1 year (12%). Reasons for missing outcomes were not reported. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
| Other bias | Unclear risk | Comments: baseline characteristics and details about co‐interventions not reported |
Schriks 2003.
| Methods |
Design: parallel RCT Number of participants: 403 Setting: not reported Country: Indonesia Unit of randomisation: child Unit of analysis: child Follow‐up: end of treatment Dropout: none |
|
| Participants |
Number randomised (participants): 403 children (202 ART group and 201 CT group)
Number analysed: 403 children
Age mean and SD (range): 6.3 years (4.9‐7.9)
Gender: female 208 (51.6%), male 195 (48.39%) Dentition: primary Type of caries lesion: multiple surface caries lesion Average DMFT score: not reported Inclusion criteria: ≥ 1 multi‐surface cavity in a deciduous molar that was accessible to hand instruments and where no pulp exposure was expected Exclusion criteria: not reported |
|
| Interventions | Two treatment arms:
In ART group, only hand instruments were used, i.e. hatchets and excavators. In CT group, excavation of the demineralised tooth material was carried out by means of stainless steel round burs in a handpiece (750 rpm), without water cooling. In both groups, only the demineralised carious tooth tissue and unsupported enamel were removed. After cleaning the cavity, a matrix band and wooden wedges were applied. Cotton wool rolls were used to isolate the cleaned cavity from contamination with saliva and/or blood. After conditioning the dentin for 15 s, hand‐mix H‐GIC (Chemflex, Dentsply/deTrey) was placed into the cavity in both groups. No local anaesthesia was used in either group. Interventions were conducted by 4 dentists and 1 dental student. |
|
| Outcomes |
|
|
| Notes | Funding: this study was supported by Dentsply/deTrey (UK), ESPE, Dental Union and WOTRO (the Netherlands) Trial register number not reported Sample size not calculated Interexaminer reproducibility was good (kappa = 0.87). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Treatments were allocated randomly" Comments: how this was done not described |
| Allocation concealment (selection bias) | Unclear risk | Comments: not reported |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comments: no information provided, but the participants could tell whether manual or rotary instruments were used |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comments: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: “the Venham score was observed by one of the authors, not participating in the treatments, though aware of the treatment method that was randomly chosen for the child” Comments: this could bias the results, favouring one of the treatment methods. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comments: for the outcomes evaluated all participants were assessed. |
| Selective reporting (reporting bias) | Unclear risk | Comments: all outcomes listed in the methods sections were included, but the results were described incompletely. |
| Other bias | Low risk | Comments: the study appears to be free of other sources of bias. No relations could be found between the treatment and either gender or operator in a number of participants. |
Van de Hoef 2007.
| Methods |
Design: cluster, parallel RCT Number of participant: 299 Setting: not reported Country: Surinam Unit of randomisation: child Unit of analysis: tooth Follow‐up: 6 and 30 months Dropout: 51.7% after 30 months |
|
| Participants |
Number randomised (participants): 299 children (153 ART group and 146 CT group)/408 teeth (205 ART and 203 CT)
Number analysed: 211 teeth
Age mean and SD (range): 7.5 years (6.0‐12.9 years)
Gender: female 155 (51.8%), male 144 (48.2%) Average dmft score: not reported Dentition: primary Type of caries lesion: multiple surface caries lesion Inclusion criteria: schoolchildren in good mental and physical health with ≥ 1 small proximally situated cavity in a primary molar that was accessible to hand instruments from the occlusal surface and where no pulp exposure was expected. The measurements of the cavity had to be < 1 mm mesio‐distally and 2 mm in bucco‐lingual/palatinal direction. The antagonist tooth had to be present. Exclusion criteria: pain, swelling or fistula |
|
| Interventions | The study had four arms:
Children in the ART approach were treated using only hand instruments (i.e. hatchets and spoon excavators) to remove the caries lesions. Participants in the CT group were treated with rotary instruments, i.e. stainless steel round burs in a slow handpiece without water cooling. After access to the cavity was obtained, at first the enamel‐dentine border was cleaned and after that the remaining caries was removed. In both treatments after finishing the preparation a piece of metal matrix band (Matricodent) was applied and fixed with a wooden wedge. In all cases hand‐mixed glass ionomer (Fuji IX, GC Corporation) was used as restoration material. The interventions were conducted by one dentist, one dental student and two hygienists. |
|
| Outcomes |
|
|
| Notes | Funding: Foundation of Youth Dental Care in Paramaribo, Suriname and GC company provided the GIC Trial register number not reported Samples size not calculated Intraexaminer consistency values range from 0.73‐0.84 (Cohen’s kappa) Interexaminer consistency was calculated: 0.72 for the 6‐month evaluation and 0.93 for the evaluation after 30 months. Some of the children received a second restoration placed in another molar. In these cases the same treatment protocol for both restorations was used. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The children were randomly divided into four treatment groups" "The randomization list was obtained by means of SPSS" |
| Allocation concealment (selection bias) | Unclear risk | Comments: not reported |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comments: no information provided, but the participants could tell whether manual or rotary instruments were used |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comments: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The restorations were evaluated by two final‐year dental students of ACTA (who did not perform any treatment)" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "The majority of the dropouts concerned absent patients and shed teeth" Comments: loss to follow‐up close to 50% at 30 months. How many losses due to absence or shedding not reported |
| Selective reporting (reporting bias) | High risk | Comments: discomfort was not reported at all measured times, only during deep excavation and restoration. Not was included a mean of all measured. |
| Other bias | High risk | Comments: baseline characteristics or details about co‐interventions not reported. The analysis did not consider the intra‐cluster correlation coefficient. |
Van den Dungen 2004.
| Methods |
Design: parallel RCT Number of participants: 393 Setting: school Country: Indonesia Unit of randomisation: child Unit of analysis: child Follow‐up: 1.5, 6, 12, 24 and 36 months Dropout: 41.7% after 36 months |
|
| Participants |
Number randomised (participants): 393 children Number analysed: 229 children (116 ART group and 113 CT group) Age mean and SD (range): 6.5 years SD = 0.50 Gender: not reported Average dmft score: not reported Dentition: primary Type of caries lesion: multiple surface caries lesion Inclusion criteria:
Exclusion criteria: not reported |
|
| Interventions | Two treatment arms:
The ART group used hand instruments to remove caries lesion and the cavities were restored with H‐GIC (Chem‐Flex Dentsply/DeTrey). In the CT group, cavities were excavated using a round, stainless steel drill (750 rpm) and restored with H‐GIC (Chem Flex Dentsply/DeTrey). Use of anaesthesia was not reported in any group. Interventions conducted by 2 dentists and 2 dental students |
|
| Outcomes | Succes rate assessed by WHO criteria after 1.5, 6, 12 , 24 and 36 months. Success includes the following scores: 00 and 10. Scores of 11, 12, 13, 20, 21, 30 and 40 are regarded as failures. The scores 50, 60, 70 and 90 are not related to success or failure. | |
| Notes | Funding: The Foundation Backer Dirks Fund provided a grant and Dentsply/DeTrey suggested the material available Trial register number not reported Sample size not calculated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “There were 393 children selected for the study. These were randomly divided into 2 groups and randomly assigned to the four practitioners” Commnents: insufficient information about the sequence generation process |
| Allocation concealment (selection bias) | Unclear risk | Comments: not reported |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comments: no information provided, but the participants could tell whether manual or rotary instruments were used |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comments: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The evaluators were blinded of the method of treatment (ART or conventional)" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comments: loss to follow‐up was high at 3 years (41.7%). Reasons for missing outcomes were not reported. |
| Selective reporting (reporting bias) | High risk | Comments: all outcomes listed in the methods sections were included, but the results were described incompletely. Results before 3 years were not reported. |
| Other bias | Unclear risk | Comments: baseline characteristics and details of co‐interventions not reported |
Yu 2004.
| Methods |
Design: cluster split‐mouth RCT Number of participants: 60 Setting: school dental clinic Country: China Unit of randomisation: tooth Unit of analysis: tooth pairs Follow‐up: 6, 12 and 24 months Dropout: 33.3% and 55% after 12 and 24 months |
|
| Participants |
Number randomised (participants): 60 children/167 teeth (72 ART group and 95 CT group)
Number analysed: 27 child/69 teeth
Age mean and SD (range): 7.4 SD 1.24 (7‐9 years)
Gender: female 33 (55%), male 27 (45%) Average dmft score: not reported Dentition: primary Type of caries lesion: simple and multiple surface caries lesion Inclusion criteria: healthy children with ≥ 1 pair of primary molars with caries lesions of similar size and class Exclusion criteria: not reported |
|
| Interventions | Study has 9 arms:
The ART cavity preparation method followed the directions given in the ART technique manual, ensuring removal of all softened carious dentin at the dentinoenamel junction. Strong, unsupported enamel cusps were left intact where access for caries removal was deemed satisfactory. Bases were not used with any of the restorations. The cavities for CT were prepared with conventional rotatory instruments. The cavities were not used with any of the restorations. The GICs were coated with a varnish after placement, and the amalgam restorations were left unpolished. No local anaesthesia was used in either group. The interventions were conducted by 2 dentists. |
|
| Outcomes |
|
|
| Notes | Funding: supply of commercial materials and some financial assistance was provided by ESPE Dental Medizin GmbH and by GC International Corp Trial register number not reported Sample size not calculated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Treatments were assigned randomly to one of nine groups” Comments: how this was done is not described. |
| Allocation concealment (selection bias) | Unclear risk | Comments: not reported |
| Blinding of participants and personnel (performance bias) ‐ participant | High risk | Comments: participants aware of different treatments |
| Blinding of participants and personnel (performance bias) ‐ operator All outcomes | High risk | Comments: blinding not possible ‐ operator knew the intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The assessment were recorded by a researcher who did not performed any treatment" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Comments: loss to follow‐up was high at 2 years (55%). |
| Selective reporting (reporting bias) | Low risk | Comments: all prespecified outcomes reported |
| Other bias | High risk | Comments: the analysis did not consider the paired data. |
ART: atraumatic restorative treatment; CPI: Community Periodontal Index; CT: conventional treatment; dmft: decayed, missing and filled primary teeth); DMFT: decayed, missing and filled permanent teeth; GIC: glass ionomer cement; H‐GIC: high‐viscosity glass ionomer cement; RCT: randomised controlled trial; RM‐GIC: resin‐modified glass‐ionomer cement; USPHS: US Public Health Service
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Andrade 2010 | Compares ART with chemomechanical caries removal (Papacarie) |
| Barata 2007 | Compares ART with chemomechanical caries removal (Carisolv) |
| Barata 2008 | Compares ART with chemomechanical caries removal (Carisolv) |
| Caro 2012 | ART technique was modified with Papacarie |
| De Amorim 2014 | Not an RCT |
| De Menezes 2011 | Not an RCT. Only the schools that received experimental group were randomised. CT group was not randomised. |
| Frencken 1994 | Not an RCT. One village received ART, a second village was treated with amalgam and a third village was the control. |
| Frencken 2006 | Not an RCT. The electricity failed on a number of days and the principal investigator decided that all children, who had been bussed to the WHO Centre for treatment, would be treated using the ART approach. |
| Hilgert 2014 | Not RCT |
| Hu 2005 | Not RCT |
| Hui‐min 2005 | Compares ART with different GICs |
| Ibiyemi 2011 | Does not compare ART with conventional treatment |
| ISRCTN76299321 | Not an RCT |
| Kalf‐Scholte 2003 | No randomisation between CT and ART, only between materials used for ART |
| Mandari 2001 | Modified ART, using hand instruments and a caries‐removal solution (Caridex) |
| McComb 2002 | Does not compare ART with CT. Compares different materials |
| Menezes 2006 | Does not compare ART with CT. Compares two types of GICs |
| Mickenautsch 2007 | Not an RCT |
| Mizuno 2011 | Compares ART with chemomechanical caries removal (Papacarie) |
| NCT02234609 | Modified ART. Not an RCT |
| NCT02274142 | Does not compare ART with conventional treatment. Compares different GICs |
| NTR4400 | Not an RCT |
| Phantumvanit 1996 | Not an RCT. One village received ART and those in the other village received CT |
| Phonghanyudh 2012 | Modified ART; this involved accessing caries using high speed to break enamel |
| Rahimtoola 2002 | Not an RCT. Two operators did not strictly follow the randomisation procedure for the selection of the treatment technique. |
| Taifour 2002 | Not an RCT. The electricity failed on a number of days and the principal investigator decided that all children, who had been bussed to the WHO Centre for treatment, would be treated using the ART approach. |
| Yip 2002b | Not an RCT |
ART: atraumatic restorative treatment; CT: conventional treatment; GIC: glass ionomer cement; RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
CTRI007332.
| Trial name or title | Comparison of efficacy and acceptability of caries removal methods ‐ a randomized controlled clinical trial |
| Methods | Design: RCT Country: India |
| Participants |
Inclusion criteria
Exclusion criteria
|
| Interventions | The study has three arms
|
| Outcomes | Primary outcomes
Secondary outcomes
|
| Starting date | December 2015 |
| Contact information | DR SS Hiremath, hiremath29@gmail.com |
| Notes |
NCT02562456.
| Trial name or title | Cost‐efficacy between ART and composite resin restorations in primary molars |
| Methods | Design: parallel RCT, single‐blind Country: Brazil |
| Participants |
Inclusion criteria
Exclusion criteria
|
| Interventions | Two treatment arms:
|
| Outcomes | Primary outcome
Secondary outcome
|
| Starting date | October 2015 |
| Contact information | Daniela P Raggio, PhD danielar@usp.br |
| Notes |
NCT02568917.
| Trial name or title | Effectiveness of ART and conventional treatment ‐ practice‐based clinical trial |
| Methods | Design: parallel RCT, single blind Country: Brazil |
| Participants |
Inclusion criteria
Exclusion criteria
|
| Interventions | Two treatment arms:
|
| Outcomes | Primary outcome
Secondary outcome
|
| Starting date | January 2016 |
| Contact information | Professor Daniela P Raggio danielar@usp.br |
| Notes |
RBR‐4nwmk4.
| Trial name or title | Evaluation of atraumatic restorative treatment (ART) in the family health strategy of Teresina, Piauí |
| Methods | Design: parallel RCT, double blind Country: Brazil |
| Participants |
Inclusion criteria
Exclusion criteria
|
| Interventions | Two treatment arms: Group 1: ART using H‐GIC Group 2: CT using H‐GIC |
| Outcomes | Primary outcome
Secondary outcome
|
| Starting date | September 2015 |
| Contact information | Marcoeli Silva De Moura. Universidade Federal Do Piauí. marcoeli‐moura@uol.com.br |
| Notes | Funding: Fundação de Amparo a Pesquisa do Estado do Piauí ‐ FAPEPI |
ART: atraumatic restorative treatment; CT: conventional treatment; GIC: glass ionomer cement; H‐GIC: high‐viscosity glass ionomer cement; RCT: randomised controlled trial; RM‐GIC: resin‐modified glass‐ionomer cement
Differences between protocol and review
The 'Objectives' section was expanded to better describe the objectives of this review for the readers.
We had planned to include both RCTs and quasi‐RCTs in this review. However, we decided to exclude quasi‐RCTs to improve the internal validity of findings.
In the protocol it was not clear whether we would include studies using different restorative materials in study arms. We clarified in the 'Types of interventions section' that studies using the same and different materials in study arms would be included in the review, but only studies using the same restorative material in both arms would be pooled in the meta‐analysis.
We had planned to search IndMED (India), Chinese BiomedicalLiterature Database (CBM) (in Chinese), Grey literature databases such as SIGLE (1980 to present). In the full review, Cochrane Oral Health amended the list of databases and added the following: Meta Register of Controlled Trials (to 6 July 2015), ClinicalTrials.gov (to 22 February 2017), WHO International Clinical Trials Registry Platform (to 22 February 2017).
Following consultation with Cochrane Oral Health, we decided to reduce the large list of secondary outcomes and to prioritise only the clinically relevant outcomes.
To pool parallel and split‐mouth data, we used the generic inverse variance method (GIV) and therefore, we calculated the OR rather than RR.
Contributions of authors
Mojtaba Dorri (MD) ‐ drafting of the protocol, designing a search strategy, screening search results, selection of studies, writing to authors of papers for additional information, quality assessment, data extraction, drafting the final review, updating the review. María José Martinez‐Zapata ‐ selection of studies, quality assessment, data extraction, carrying out the analysis, drafting the final review, updating the review. Tanya Walsh ‐ data extraction, carrying out the analysis, interpreting the analysis, drafting the final review, updating the review. Valeria Marinho (VM) ‐ drafting of the protocol, selection of studies, interpreting the analysis, drafting the final review, updating the review. Aubrey Sheiham (AS) ‐ drafted the protocol, designed a search strategy, and selected studies. Aubrey made a very important contribution to this review. He passed away in 2015. Carlos Zaror (CZ) ‐ screening search results, selection of studies, writing to authors of papers for additional information, quality assessment, data extraction, carrying out the analysis, drafting the final review, updating the review.
Sources of support
Internal sources
The University of Manchester, Manchester Academic Health Sciences Centre (MAHSC), UK NIHR Manchester Biomedical Research Centre, UK.
External sources
-
CONICYT Higher educational program. Government of Chile, Chile.
Project number 80140042
-
Instituto de Salud Carlos III, Spain.
- Dr. Mª José Martinez Zapata is funded by a Miguel Servet research contract from the Instituto de Salud Carlos III and European Social Fund (Investing in Your Future) (CP15/00116)
-
Naitonal Institute for Health Research (NIHR), UK.
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Oral Health. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health
-
Cochrane Oral Health Global Alliance, Other.
The production of Cochrane Oral Health reviews has been supported financially by our Global Alliance since 2011 (Cochrane Oral Health Global Alliance partners). Contributors over the past year have been: British Association for the Study of Community Dentistry, UK; British Society of Paediatric Dentistry, UK; the Canadian Dental Hygienists Association, Canada; Centre for Dental Education and Research at All India Institute of Medical Sciences, India; National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; NHS Education for Scotland, UK; Swiss Society for Endondontology, Switzerland
Declarations of interest
Mojtaba Dorri: none known. Maria José Martinez‐Zapata: none known. Tanya Walsh: none known. Dr Walsh is an Editor with Cochrane Oral Health. Valeria CC Marinho: none known. Aubrey Sheiham: deceased. Declaration of interest from protocol: 'none known'. Carlos Zaror: none known.
Deceased November 2015
Edited (no change to conclusions)
References
References to studies included in this review
Cruz 2016 {published data only}
- Cruz A, Marín D. Clinical outcome of root caries restorations using ART and rotary techniques in institutionalized elders. Brazilian Oral Research 2016;30(1):1‐8. [DOI] [PubMed] [Google Scholar]
Da Mata 2015 {published data only}
- Mata C, Allen PF, Cronin M, O'Mahony D, McKenna G, Woods N. Cost‐effectiveness of ART restorations in elderly adults: a randomized clinical trial. Community Dentistry and Oral Epidemiology 2014;42(1):79‐87. [DOI] [PubMed] [Google Scholar]
- Mata C, Allen PF, McKenna G, Cronin M, O'Mahony D, Woods N. Two‐year survival of ART restorations placed in elderly patients: A randomised controlled clinical trial. Journa of Dentistry 2015;43(4):405‐11. [DOI] [PubMed] [Google Scholar]
De Menezes 2009 {published data only}
- Menezes DM, Leal SC, Frencken FE. Self‐report of pain in children treated according to the atraumatic restorative treatment and the conventional restorative treatment‐‐a pilot study. Journal of Clinical Pediatric Dentistry 2009;34(2):151‐6. [DOI] [PubMed] [Google Scholar]
Eden 2006 {published data only}
- Eden E, Topaloglu‐Ak A, Frencken JE, Van't Hof M. Survival of self‐etch adhesive Class II composite restorations using ART and conventional cavity preparations in primary molars. American Journal of Dentistry 2006;19(6):359‐63. [PubMed] [Google Scholar]
- Topaloglu‐Ak A, Eden E, Frencken JE. Perceived dental anxiety among schoolchildren treated through three caries removal approaches. Journal of Applied Oral Science 2007;15(3):235‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Estupiñan‐Day 2006 {published data only}
- Estupiñan‐Day S, Milner T, Tellez M. Oral health of low income children: procedures for atraumatic restorative treatment (PRAT). Pan American Health Organization 2006. [DOI] [PubMed]
- Estupiñán‐Day S, Tellez M, Kaur S, Milner T, Solari A. Managing dental caries with atraumatic restorative treatment in children: successful experience in three Latin American countries. Revista Panamericana de Salud Publica 2013;33(4):237‐43. [DOI] [PubMed] [Google Scholar]
Lin 2003 {published data only}
- Lin XP, Guo L, An LX. The clinical effect of ART and psychological guidance in treatment of carious deciduous teeth in preschool children. Shanghai Kou Qiang Yi Xue 2003;12(4):313‐4. [PubMed] [Google Scholar]
Ling 2003 {published data only}
- Ling L, Wang X. Evaluation of effects of Atraumatic Restorative Treatment and cooperation degree in primary teeth. Stomatology 2003;23(5):290‐91. [Google Scholar]
Lo 2006 {published data only}
- Lo EC, Luo Y, Tan HP, Dyson JE, Corbet EF. ART and conventional root restorations in elders after 12 months. Journal of Dental Research 2006;85(10):929‐32. [DOI] [PubMed] [Google Scholar]
Luz 2012 {published data only}
- Luz P, Barata J, Meller C, Slavutsky S, Araujo F. ART acceptability in children: a randomized clinical trial. Revista da Faculdade de Odontologia de Porto Alegre 2012;53(1):27‐31. [Google Scholar]
Miranda 2005 {published data only}
- Miranda L. Randomized controlled clinical study comparing atraumatic restorative treatment with conventional amalgam treatment in primary molars: evaluation after 6 and 12 months [Estudo clínico randomizado e controlado comparando o tratamento restaurador atraumático ao convencional com amálgama em molares decíduos: avaliação após 6 e 12 meses] [Thesis].. Rio de Janeiro (Brazil): Faculdade de Odontologia, Universidade do Estado do Rio de Janeiro, 2005. [Google Scholar]
Roeleveld 2006 {published data only}
- Mhaville RJ, Amerongen WE, Mandari GJ. Residual caries and marginal integrity in relation to Class II glass ionomer restorations in primary molars. European Archives of Paediatric Dentistry 2006;7(2):81‐4. [DOI] [PubMed] [Google Scholar]
- Roeleveld AC, Amerongen WE, Mandari GJ. Influence of residual caries and cervical gaps on the survival rate of Class II glass ionomer restorations. European Archives of Paediatric Dentistry 2006;7(2):85‐91. [DOI] [PubMed] [Google Scholar]
Schriks 2003 {published data only}
- Schriks MCM, Amerongen WE. Atraumatic perspectives of ART: psychological and physiological aspects of treatment with and without rotary instruments. Community Dentistry and Oral Epidemiology 2003;31:15‐20. [DOI] [PubMed] [Google Scholar]
- Gemert‐Schriks MC. Discomfort during atraumatic restorative treatment (ART) versus conventional restorative treatment [Ongemak tijdens atraumatic restorative treatment (ART) versus conventionel ebehandel methode]. Ned Tijdschr Tandheelkd 2007;114(5):213‐7. [PubMed] [Google Scholar]
Van de Hoef 2007 {published data only}
- Bochove JA, Amerongen WE. The influence of restorative treatment approaches and the use of local analgesia, on the children’s discomfort. European Archives of Paediatric Dentistry 2006;7(1):11‐6. [DOI] [PubMed] [Google Scholar]
- Hoef N, Amerongen E. Influence of local anaesthesia on the quality of class II glass ionomer restorations. International Journal of Paediatric Dentistry 2007;17(4):239‐47. [DOI] [PubMed] [Google Scholar]
Van den Dungen 2004 {published data only}
- Dungen GM, Huddleston Slater AE, Amerongen WE. ART or conventional restorations? A final evaluation of proximal restorations in deciduous molars [Art Of Conventioneel? Onderzoeksresultaten Van Proximale Restauraties In Tijdelijke Molaren]. Ned Tijdschr Tandheelkd 2004;111(9):345‐9. [PubMed] [Google Scholar]
Yu 2004 {published data only}
- Yip HK, Smales RJ, Yu C, Gao XJ, Deng DM. Comparison of atraumatic restorative treatment and conventional cavity preparations for glass‐ionomer restorations in primary molars: one‐year results. Quintessence International 2002;33:17‐21. [PubMed] [Google Scholar]
- Yu C, Gao XJ, Deng DM, Yip HK, Smales RJ. Survival of glass ionomer restorations placed in primary molars using atraumatic restorative treatment (ART) and conventional cavity preparations: 2‐year results. International Dental Journal 2004;54(1):42‐6. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Andrade 2010 {published data only}
- Andrade P. Atraumatic and chemical‐mechanical methods: a controlled clinical trial of caries progression [Métodos atraumáticos e químico‐mecãnico: um ensaio clínico controlado de progressão de cárie]. Thesis.
Barata 2007 {published data only}
- Barata T. Clinical evaluation of two minimally invasive methods: chemi‐mechanical and mechanical [Avaliação clínica de dois métodos minimamente invasivos: químico‐mecânico e mecânico]. Thesis. Faculdade de Odontologia de Bauru, Universidade de São Paulo. 2007.
Barata 2008 {published data only}
- Barata TJ, Bresciani E, Mattos MC, Lauris JR, Ericson D, Navarro MF. Comparison of two minimally invasive methods on the longevity of glass ionomer cement restorations: short‐term results of a pilot study. Journal of Applied Oral Science 2008;16(2):155‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Caro 2012 {published data only}
- Caro T, Aguilar A, Saavedra J, Alfaya T, França C, Fernandes K, et al. Comparison of operative time, costs, and self‐reported pain in children treated with atraumatic restorative treatment and conventional restorative treatment. Clinical and Experimental Medical Letters 2012;53(4):159‐63. [Google Scholar]
De Amorim 2014 {published data only}
- Amorim RG, Leal SC, Mulder J, Creugers NH, Frencken JE. Amalgam and ART restorations in children: a controlled clinical trial. Clinical Oral Investigations 2014;18(1):117‐24. [DOI] [PubMed] [Google Scholar]
De Menezes 2011 {published data only}
- Menezes Abreu DM, Leal SC, Mulder J, Frencken JE. Dental anxiety in 6‐7‐year‐old children treated in accordance with conventional restorative treatment, ART and ultra‐conservative treatment protocols. Acta Odontologica Scandinavica 2011;69(6):410‐6. [DOI] [PubMed] [Google Scholar]
- Menezes Abreu DM, Leal SC, Mulder J, Frencken JE. Pain experience after conventional, atraumatic, and ultraconservative restorative treatments in 6‐ to 7‐yr‐old children. European Journal of Oral Sciences 2011;119(2):163‐8. [DOI] [PubMed] [Google Scholar]
Frencken 1994 {published data only}
- Frencken JE, Songpaisan Y, Phantumvanit P, Pilot T. An atraumatic restorative treatment (ART) technique: evaluation after one year. International Dental Journal 1994;44(5):460‐4. [PubMed] [Google Scholar]
Frencken 2006 {published data only}
- Frencken JE, Taifour D, 't Hof MA. Survival of ART and amalgam restorations in permanent teeth of children after 6.3 years. Journal of Dental Research 2006;85(7):622‐6. [DOI] [PubMed] [Google Scholar]
- Frencken JE, Van't Hof MA, Taifour D, Al‐Zaher I. Effectiveness of ART and traditional amalgam approach in restoring single‐surface cavities in posterior teeth of permanent dentitions in school children after 6.3 years. Community Dentistry and Oral Epidemiology 2007;35(3):207‐14. [DOI] [PubMed] [Google Scholar]
- Taifour D, Frencken JE, Beiruti N, Van´t Hof MA, Truin Gj, Palenstein WH. Comparison between restorations in the permanent dentition produced by hand and rotary instrumentation – survival after 3 years. Community Dentistry and Oral Epidemiology 2003;31(2):122‐8. [DOI] [PubMed] [Google Scholar]
Hilgert 2014 {published data only}
- Hilgert L, Amorin R, Leal S, Mulder J, Creugers N, Frencken J. Is high‐viscosity glass‐ionomer‐cement a successor to amalgam for treating primary molars?. Dental Materials 2014;30:1172–8. [DOI] [PubMed] [Google Scholar]
Hu 2005 {published data only}
- Hu JY, Chen XC, Li YQ, Smales RJ, Yip KH. Radiation‐induced root surface caries restored with glass‐ionomer cement placed in conventional and ART cavity preparations: results at two years. Australian Dental Journal 2005;50(3):186‐90. [DOI] [PubMed] [Google Scholar]
Hui‐min 2005 {published data only}
- Hui‐min L, Zheng‐hong D. Clinical observation of using different material in the elderly decayed tooth ART technique. Practical Clinical Medicine 2005;6:105‐7. [Google Scholar]
Ibiyemi 2011 {published data only}
- Ibiyemi O, Bankole OO, Oke GA. Survival rates of two atraumatic restorative treatment (ART) types in occlusal carious permanent teeth after two years. African Journal of Medicine and Medical Sciences 2011;40(2):127‐34. [PubMed] [Google Scholar]
ISRCTN76299321 {published data only}
- ISRCTN76299321. Atraumatic restorative treatment for caries in the Elderly ‐ a study to assess a novel approach for the prevention of root caries. isrctn.com/ISRCTN30662154 2013.
Kalf‐Scholte 2003 {published data only}
- Kalf‐Scholte SM, Amerongen WE, Smith AJ, Haastrecht HJ. Atraumatic restorative treatment (ART): a three‐year clinical study in Malawi‐‐comparison of conventional amalgam and ART restorations. Journal of Public Health Dentistry 2003;63(2):99‐103. [DOI] [PubMed] [Google Scholar]
Mandari 2001 {published data only}
- Mandari GJ, Frencken JE, Van't Hof MA. Six‐year success rates of occlusal amalgam and glass‐ionomer restorations placed using three minimal intervention approaches. Caries Research 2003;37(4):246‐53. [DOI] [PubMed] [Google Scholar]
- Mandari GJ1, Truin GJ, Van't Hof MA, Frencken JE. Effectiveness of three minimal intervention approaches for managing dental caries: survival of restorations after 2 years. Caries Research 2001;35(2):90‐4. [DOI] [PubMed] [Google Scholar]
McComb 2002 {published data only}
- McComb D, Erickson RL, Maxymiw WG, Wood RE. A clinical comparison of glass ionomer, resin‐modified glass ionomer and resin composite restorations in the treatment of cervical caries in xerostomic head and neck radiation patients. Operative Dentistry 2002;27(5):430‐7. [PubMed] [Google Scholar]
Menezes 2006 {published data only}
- Menezes JP, Rosenblatt A, Medeiros E. Clinical evaluation of atraumatic restorations in primary molars: a comparison between 2 glass ionomer cements. Journal of Dentistry for Children 2006;73(2):91‐7. [PubMed] [Google Scholar]
Mickenautsch 2007 {published data only}
- Mickenautsch S, Frencken JE, Van't HM. Atraumatic restorative treatment and dental anxiety in outpatients attending public oral health clinics in South Africa. Journal of Public Health Dentistry 2007;67(3):179‐84. [DOI] [PubMed] [Google Scholar]
Mizuno 2011 {published data only}
- Mizuno D, Guedes C, Hermida L, Motta L, Santos E, Bussadori S. Clinical and radiographic analysis of the chemical‐mechanical caries removal and ART: a pilot study [Análisis clínico y radiográfico de las técnicas ART y remoción químico‐mecánica de caries: estudio piloto]. Odontoestomatología 2011;13(18):29‐35. [Google Scholar]
NCT02234609 {published data only}
- NCT02234609. Effectiveness of modified class IV atraumatic restorative treatment. clinicaltrials.gov/show/NCT02234609 2014.
NCT02274142 {published data only}
- NCT02274142. Randomized clinical trial, double‐blinded on ART restorations. clinicaltrials.gov/show/NCT02274142.
NTR4400 {unpublished data only}
- NTR4400. Hand instruments are better accepted than rotary instrumentation for restoring tooth cavities in people with disabilities. www.trialregister.nl/trialreg/admin/rctview.asp?TC=4400.
Phantumvanit 1996 {published data only}
- Phantumvanit P, Songpaisan Y, Pilot T, Frencken JE. Atraumatic restorative treatment (ART): a three‐year community field trial in Thailand‐‐survival of one‐surface restorations in the permanent dentition. Journal of Public Health Dentistry 1996;56(3 Spec No):141‐5. [DOI] [PubMed] [Google Scholar]
Phonghanyudh 2012 {published data only}
- Phonghanyudh A, Phantumvanit P, Songpaisan Y, Petersen PE. Clinical evaluation of three caries removal approaches in primary teeth: a randomised controlled trial. Community Dental Health 2012;29(2):173‐8. [PubMed] [Google Scholar]
Rahimtoola 2002 {published data only}
- Rahimtoola 2002. Comparison of two tooth‐saving preparation techniques for one‐surface cavities. ASDC Journal of Dentistry for Children 2002;69(1):16‐26. [PubMed] [Google Scholar]
- Rahimtoola S, Amerongen E, Maher R, Groen H. Pain related to different ways of minimal intervention in the treatment of small caries lesions. ASDC Journal of Dentistry for Children 2000;67(2):123‐7. [PubMed] [Google Scholar]
- Amerongen WE, Rahimtoola S. Is ART really atraumatic?. Community Dentistry and Oral Epidemiology 1999;27:41‐5. [DOI] [PubMed] [Google Scholar]
Taifour 2002 {published data only}
- Taifour D, Frencken JE, Beiruti N, Vant´t Hof MA, Truin GJ. Effectiveness of glass–ionomer (ART) and amalgam restorations in the deciduous dentitions: results after 3 years. Caries Research 2002;36:437‐44. [DOI] [PubMed] [Google Scholar]
Yip 2002b {published data only}
- Yip KH, Smales RJ, Gao W, Peng D. The effects of two cavity preparation methods on the longevity of glass ionomer cement restorations: an evaluation after 12 months. Journal of the American Dental Association 2002;133(6):744‐51. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
CTRI007332 {published data only}
- CTRI007332. Comparison of efficacy and acceptability of caries removal methods ‐ a randomized controlled clinical trial. ctri.nic.in/Clinicaltrials/advsearch.php.
NCT02562456 {published data only}
- NCT02562456. Cost‐efficacy between ART and composite resin restorations in primary molars. clinicaltrials.gov/show/NCT02562456.
NCT02568917 {published data only}
- NCT02568917. Effectiveness of ART and conventional treatment ‐ practice‐based clinical trial. clinicaltrials.gov/show/NCT02568917.
RBR‐4nwmk4 {published data only}
- RBR‐4nwmk4. Evaluation of atraumatic restorative treatment (ART) in the family health strategy of Teresina, Piauí. www.ensaiosclinicos.gov.br/rg/RBR‐4nwmk4/ 2016.
Additional references
AAPD 2008‐2009
- American Academy of Pediatric Dentistry Council on Clinical Affairs. Policy on interim therapeutic restorations (ITR). Pediatric Dentistry 2008‐2009;30(7 Suppl):38‐9. [PubMed] [Google Scholar]
Antoft 1999
- Antoft P, Rambusch E, Antoft B, Christensen HW. Caries experience, dental health behaviour and social status: three comparative surveys among Danish military recruits in 1972, 1982 and 1993. Community Dental Health 1999;16(2):80‐4. [PubMed] [Google Scholar]
Anusavice 1999
- Anusavice KJ. Does ART have a place in preservative dentistry?. Community Dentistry and Oral Epidemiology 1999;27(6):442‐8. [DOI] [PubMed] [Google Scholar]
Banerjee 2000
- Banerjee A, Watson TF, Kidd EA. Dentine caries excavation: a review of current clinical techniques. British Dental Journal 2000;188(9):476‐82. [DOI] [PubMed] [Google Scholar]
Berggren 1984
- Berggren U, Meynert G. Dental fear and avoidance: causes, symptoms, and consequences. Journal of the American Dental Association 1984;109(2):247‐51. [DOI] [PubMed] [Google Scholar]
Cole 2000
- Cole BO, Welbury RR. The atraumatic restorative treatment (ART) technique: does it have a place in everyday practice?. Dental Update 2000;27(3):118‐20, 122‐3. [DOI] [PubMed] [Google Scholar]
De Amorin 2012
- Amorim R, Leal S, Frencken J. Survival of atraumatic restorative treatment (ART) sealants and restorations: a meta‐analysis. Clinical Oral Investigation 2012;16:429‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Dorri 2015
- Dorri M, Dunne SM, Walsh T, Schwendicke F. Micro‐invasive interventions for managing proximal dental decay in primary and permanent teeth. Cochrane Database of Systematic Reviews 2015, Issue 11. [DOI: 10.1002/14651858.CD010431.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ekstrand 2007
- Ekstrand KR, Martignon S, Christiansen ME. Frequency and distribution patterns of sealants among 15‐year‐olds in Denmark in 2003. Community Dental Health 2007;24(1):26‐30. [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta‐analyses involving cross over trials: methodological issues. International Journal of Epidemiology 2002;31(1):140‐9. [DOI] [PubMed] [Google Scholar]
Fejerskov 2004
- Fejerskov O. Changing paradigms in concepts on dental caries: consequences for oral health care. Caries Research 2004;38:182‐91. [DOI] [PubMed] [Google Scholar]
Frencken 1996
- Frencken JE, Pilot T, Songpaisan Y, Phantumvanit P. Atraumatic restorative treatment (ART): rationale, technique, and development. Journal of Public Health Dentistry 1996;56(3 Spec No):135‐40, 161‐3. [DOI] [PubMed] [Google Scholar]
Frencken 1999
- Frencken JE, Holmgren CJ. How effective is ART in the management of dental caries?. Community Dentistry and Oral Epidemiology 1999;27(6):423‐30. [DOI] [PubMed] [Google Scholar]
Frencken 2004a
- Frencken JE, 't Hof MA, Amerongen WE, Holmgren CJ. Effectiveness of single‐surface ART restorations in the permanent dentition: a meta‐analysis. Journal of Dental Research 2004;83(2):120‐3. [DOI] [PubMed] [Google Scholar]
Frencken 2004b
- Frencken JE, Holmgren CJ. ART: a minimal intervention approach to manage dental caries. Dental Update 2004;31(5):295‐8, 301. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- McMaster University (developed by Evidence Prime). GRADEpro GDT. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015.
Hannigan 2000
- Hannigan A, O’Mullane DM, Barry D, Schäfer F, Roberts AJ. A caries susceptibility classification of tooth surfaces by survival time. Caries Research 2000;34(2):103‐8. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from: handbook.cochrane.org.
Holmgren 2013
- Holmgren CJ, Roux D, Doméjean S. Minimal intervention dentistry: part 5. Atraumatic restorative treatment (ART) a minimum intervention and minimally invasive approach for the management of dental caries. British Dental Journal 2013;214(1):11‐18. [DOI] [PubMed] [Google Scholar]
Honkala 2002
- Honkala S, Honkala E. Atraumatic dental treatment among Finnish elderly persons. Journal of Oral Rehabilitation 2002;29(5):435‐40. [DOI] [PubMed] [Google Scholar]
Kidd 2004
- Kidd EAM, Fejerskov O. What constitutes dental caries? Histopathology of carious enamel and dentin related to the action of cariogenic biofilms. Journal of Dental Research 2004;83:C35‐8. [DOI] [PubMed] [Google Scholar]
Kidd 2005
- Kidd EAM. Essentials of Dental Caries: The Disease and Its Management. 3rd Edition. London: Wright, 2005. [Google Scholar]
Leal 2012
- Leal SC, Bronkhorst EM, Fan M, Frencken JE. Untreated cavitated dentine lesions: impact on children’s quality of life. Caries Research 2012;46(2):102‐6. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Marcenes 2013
- Marcenes W, Kassebaum NJ, Bernabé E, Flaxman A, Naghavi M, Lopez A, et al. Global burden of oral conditions in 1990‐2010: a systematic analysis. Journal of Dental Research 2013;92(7):592‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martignon 2010
- Martignon S, Tellez M, Santamaría RM, Gomez J, Ekstrand KR. Sealing distal proximal caries lesions in first primary molars: efficacy after 2.5 years. Caries Research 2010;44(6):562‐70. [DOI] [PubMed] [Google Scholar]
Mickenautsch 2010
- Mickenautsch S, Yengopal V, Banerjee A. Atraumatic restorative treatment versus amalgam restoration longevity: a systematic review. Clinical Oral Investigations 2010;14(3):233‐40. [DOI] [PubMed] [Google Scholar]
Mickenautsch 2012
- Mickenautsch S, Yengopal V. Failure rate of atraumatic restorative treatment using high‐viscosity glass‐ionomer cement compared to that of conventional amalgam restorative treatment in primary and permanent teeth: a systematic review update. Journal of Minimum Intervention in Dentistry 2012;5:63‐124. [Google Scholar]
Mjör 1999
- Mjör IA, Gordan VV. A review of atraumatic restorative treatment (ART). International Dental Journal 1999;49(3):127‐31. [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta‐Analyses: The PRISMA Statement. PLoS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
Monse‐Schneider 2003
- Monse‐Schneider B, Heinrich‐Weltzien R, Schug D, Sheiham A, Borutta A. Assessment of manual restorative treatment (MRT) with amalgam in high‐caries Filipino children: results after 2 years. Community Dentistry and Oral Epidemiology 2003;31(2):129‐35. [DOI] [PubMed] [Google Scholar]
Petersen 2005
- Petersen PE, Bourgeois D, Ogawa H, Estupinan‐Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bulletin of the World Health Organization 2005;83(9):661‐9. [PMC free article] [PubMed] [Google Scholar]
Pettar 2011
- Pettar M, Jin Z, Tai‐xiang W, Memetimin N, Zhen‐hua L. Atraumatic restorative treatment versus conventional restorative treatment for childhood caries: a systematic review. Chinese Journal of Evidence‐Based Medicine 2011;11(4):413‐8. [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Ricketts 2013
- Ricketts D, Lamont T, Innes NPT, Kidd E, Clarkson JE. Operative caries management in adults and children. Cochrane Database of Systematic Reviews 2013, Issue 3. [DOI: 10.1002/14651858.CD003808.pub3] [DOI] [PubMed] [Google Scholar]
Schwendicke 2015
- Schwendicke F, Dörfer C, Schlattmann P, Foster Page L, Thomson M, Paris S. Socioeconomic inequality and caries: a systematic review and meta‐analysis. Journal of Dental Research 2015;94(1):10‐18. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Sheiham 2010
- Sheiham A, Sabbah W. Using universal patterns of caries for planning and evaluating dental care. Caries Research 2010;44(2):141‐50. [DOI] [PubMed] [Google Scholar]
Simon 2017
- Simon AK, Bhumika TV, Nair NS. Does atraumatic restorative treatment reduce dental anxiety in children? A systematic review and meta‑analysis. European Journal of Dentistry 2017;9(2):304‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Steele 2007
- Steele J. ART for treating root caries in older people: is the atraumatic restorative technique an effective method of treating root caries in older people?. Evidence‐Based Dentistry 2007;8:5‐6. [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D (editors). Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Tyas 2000
- Tyas MJ, Anusavice KJ, Frencken JE, Mount GJ. Minimal intervention dentistry‐‐a review. FDI Commission Project 1‐97. International Dental Journal 2000;50(1):1‐12. [DOI] [PubMed] [Google Scholar]
Van 't Hof 2006
- 't Hof MA, Frencken JE, Palenstein Helderman WH, Holmgren CJ. The atraumatic restorative treatment (ART) approach for managing dental caries: a meta‐analysis. International Dental Journal 2006;56(6):345‐51. [DOI] [PubMed] [Google Scholar]
Vas 2008
- Vas J, Modesto M, Mendez C, Perea‐Milla E, Aguilar I, Carrasco‐Lozano JM, et al. Effectiveness of acupuncture, special dressings and simple, low‐adherence dressings for healing venous leg ulcers in primary healthcare: study protocol for a cluster‐randomized open‐labelled trial. BMC Complementary and Alternative Medicine 2008;8:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Weerheijm 1999
- Weerheijm KL, Groen HJ. The residual caries dilemma. Community Dentistry and Oral Epidemiology 1999;27(6):436‐41. [DOI] [PubMed] [Google Scholar]
Worthington 2015
- Worthington H, Clarkson J, Weldon J. Priority oral health research identification for clinical decision‐making. Evidence‐based Dentistry 2015;16(3):69‐71. [DOI] [PubMed] [Google Scholar]
Yip 2001
- Yip HK, Smales RJ, Ngo HC, Tay FR, Chu FC. Selection of restorative materials for the atraumatic restorative treatment (ART) approach: a review. Special Care in Dentistry 2001;21(6):216‐21. [DOI] [PubMed] [Google Scholar]
Yip 2002a
- Yip HK, Smales RJ. Glass ionomer cements used as fissure sealants with the atraumatic restorative treatment (ART) approach: review of literature. International Dental Journal 2002;52(2):67‐70. [DOI] [PubMed] [Google Scholar]


