Abstract
Background
School tobacco policies (STPs) might prove to be a promising strategy to prevent smoking initiation among adolescents, as there is evidence that the school environment can influence young people to smoke. STPs are cheap, relatively easy to implement and have a wide reach, but it is not clear whether this approach is effective in preventing smoking uptake.
Objectives
To assess the effectiveness of policies aiming to prevent smoking initiation among students by regulating smoking in schools.
Search methods
We searched seven electronic bibliographic databases, including the Cochrane Tobacco Addiction Group specialized register, MEDLINE, EMBASE, PsycINFO and ERIC. We also searched the grey literature and ongoing trials resources. The most recent search was performed in May 2014.
Selection criteria
We included cluster‐randomised controlled trials (c‐RCTs) in which primary and secondary schools were randomised to receive different levels of smoking policy or no intervention. Non‐randomised controlled trials, interrupted time series and controlled before‐after studies would also have been eligible. Cross‐sectional studies were not formally included but we describe their findings and use them to generate hypotheses to inform future research.
Data collection and analysis
We independently assessed studies for inclusion in the review, and present a narrative synthesis, as the studies are too limited in quality to undertake a formal meta‐analysis.
Main results
We found only one study which was eligible for inclusion in the review. It was judged to be at high risk of bias. The study compared two 'middle schools' from two different regions in China. The experimental conditions included the introduction of a tobacco policy, environmental changes, and communication activities, while the control condition was no intervention. After a year's follow‐up the study found no differences in smoking prevalence between intervention and control schools. We also described 24 observational studies, the results of which we considered for hypothesis generation. In these, policy exposure was mainly described using face‐to‐face interviews with school staff members, and the outcome evaluation was performed using self‐administered questionnaires. Most studies reported no differences in students' smoking prevalence between schools with formal STPs when compared with schools without policies. In the majority of studies in schools with highly enforced policies, smoking bans extended to outdoor spaces, involving teachers and including sanctions for transgressions, with assistance to quit for smokers plus support by prevention programmes, there was no significant difference in smoking prevalence when compared to schools adopting weaker or no policies.
Authors' conclusions
Despite a comprehensive literature search, and rigorous evaluation of studies, we found no evidence to support STPs. The absence of reliable evidence for the effectiveness of STPs is a concern in public health. We need well‐designed randomised controlled trials or quasi‐experimental studies to evaluate the effectiveness of school tobacco policies.
Plain language summary
Do school tobacco policies prevent uptake of smoking?
Background: We reviewed the evidence that School tobacco policies (STPs) might prevent smoking initiation among adolescents, as there may be some evidence that the school environment can influence young people to smoke. STP is intended to regulate whether and where pupils can smoke, adult smoking in school, and penalties for pupils caught smoking. We were also interested to know whether specific components of STPs might increase their impact. Components such as a smoking ban for students and/or teachers and their extent, levels of enforcement, monitoring strategies, sanctions for students or teachers found smoking, and the offer of tobacco cessation programmes.
Study characteristics: Our study search was conducted in May 2014. We identified one c‐RCT from China that we judged to be at high risk of bias. We also focussed on 24 observational studies to generate a hypothesis for future research.
Key findings: In the only included c‐RCT with 1807 participants, the intervention did not significantly affect students' smoking behavior. The majority of observational studies reported that schools with highly enforced policies, smoking ban extended to outdoor spaces, involving teachers and including sanctions for transgressions, with assistance to quit for smokers plus support by prevention programmes, did not show a significant difference in smoking prevalence, when compared to schools adopting weaker or no policies.
Quality of the evidence: We found no relevant high‐quality experimental studies. A great limitation within observational studies is the heterogeneity of exposure definitions. There is large variability in policy formats, which can include several different characteristics, which in turn makes comparison difficult. Only a few studies are based on policy definition in written documents, while in the majority the information was obtained by interviewing school heads, teachers or administrators. With regard to analysis methods, some studies did not mention any adjustment for potential confounders and in the others there was a large variability in the factors considered for adjustment. Studies differed in statistical methods employed to examine the relationship between policy and smoking behaviour.
Conclusions: We cannot draw conclusions about the effectiveness of STP from currently available data. Large, possibly multi‐centric studies, employing experimental or a quasi‐experimental design to assess the effectiveness of STPs are needed. Characteristics that could be studied are: degree of formality, participants to which the policy applies, extension of the ban (indoor areas or external school premises), level of enforcement, sanctions for transgression; assistance with smoking cessation and combination with prevention and education activities.
The authors of the review did not receive any external funding or grants to support their research for this review, and have no potential conflicts of interest.
Summary of findings
for the main comparison.
| School tobacco policy compared to no policy | ||||
|
Population: School students Settings: Secondary schools Intervention: School policy Comparison: No policy | ||||
| Outcomes | Effect | No of Participants (studies) | Quality of the evidence (GRADE) | Comments |
| Prevalence of current smokers | No significant difference in prevalence between either pair of schools | 1 c‐RCT with 2 pairs of schools, 1807 students | ⊕⊝⊝⊝ very low1 |
Observational studies also provided limited evidence that school policies affected smoking behaviour. |
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
1 Only one study with small number of clusters judged at high risk of bias.
Background
Description of the condition
Tobacco smoking is an addictive behaviour associated with over five million deaths per year. The World Health Organization projects that the number of deaths per year attributable to tobacco smoking will rise to eight million by 2030. Tobacco use is a major preventable cause of morbidity and mortality, killing an average of one person every six seconds, and is responsible for one in ten adult deaths worldwide (WHO 2012).
Though the majority of smoking‐related deaths are in people aged 35 years or older, the onset of tobacco use occurs primarily in early adolescence, and adolescents are a special target for smoking prevention projects. Trends in youth smoking show a decline during the 1970s and 1980s, and an increase in the 1990s in both the USA and Europe (Warren 2008). A younger age of smoking initiation is associated with smoking more cigarettes per day (Everett 1999) and with a lower cumulative probability of quitting (Chen 1998) than in people who start smoking later on in life. Delaying the onset of smoking may affect the likelihood of becoming addicted to nicotine and smoking heavily.
Schools have been considered an ideal site to deliver tobacco prevention programmes since they universally involve youths across a wide age range, including the ages when most young people initiate smoking. Generally school programmes show relatively weak effects in reducing adolescent smoking, and these modest results have been explained by the strong social influence effect in favour of smoking inside and outside school premises (Friend 2011). Early studies suggested the role of peer and parental smoking as moderators of school‐based effects (Tyas 1998; Faggiano 2010), and perceived smoking by friends has been found to be a stronger predictor of cigarette use than friends' actual use (Iannotti 1992). Some authors have therefore stressed the need to address adolescent smoking at the environmental level (Griesbach 2002; Nakamura 2004).
Although smoking bans in school settings are common worldwide, because of their low enforcement adolescents are still frequently exposed to teachers and other pupils smoking during the school day. In a study conducted in 48 Danish schools, three in five students reported that they had seen or knew of teachers smoking outdoors on the school premises; and most of them reported that they had seen or knew of teachers smoking inside the school building (Poulsen 2002). In the same study, teachers smoking outdoors on school premises were significantly associated with students' smoking behaviour, while exposure to other pupils smoking outdoors was not. Furthermore, it could be argued that students in a school without anti‐tobacco policies would perceive smoking as being acceptable, increasing their risk of taking up the habit.
Description of the intervention
As an intervention, school tobacco policy (STP) is intended to inform whether and where pupils can smoke, to set penalties for pupils caught smoking, and to regulate adult smoking in school (Evans‐Whipp 2004). The primary objectives of this intervention are to prevent or delay tobacco use by youth, and also to reduce the exposure of employees and students to second‐hand smoke.
In many cases the introduction of an STP is combined with other smoking prevention programmes. For example, Ariza 2008 describes a multi‐modal intervention, which includes specific lessons for students and strategies to involve adults in smoking cessation programmes. Policies can vary depending on the extent of the ban, teacher and staff training, and the roles and responsibilities of teachers and staff in policy enforcement. Policy can be governed by a central authority at regional or national level rather than locally, and the mandatory nature of a law may moderate its effect on implementation and impact. Other consequences of STPs have also been observed, e.g. schools which do not accommodate student smoking in a specific area can result in adolescents, sometimes in large groups, leaving school property during school hours to smoke elsewhere (MacBride 2005).
How the intervention might work
From the perspective of social learning theory, the interplay between individual and environment is crucial in developing intentions, expectations and ultimately behaviour (Bandura 1986). Cognitive processes such as perceived health risks or benefits of smoking and perceived availability of tobacco could be involved In smoking behaviour. According to Eccles and Roeser’s ecological perspective (Eccles 1999), factors such as peer and adults' smoking habits influence adolescents’ behaviour in combination with other factors. Therefore STPs, implemented as a part of a comprehensive approach, may affect smoking indirectly by influencing beliefs about acceptability (approval or disapproval) of cigarette smoking by adults and by peers (Lipperman‐Kreda 2009a). According to identity theory, it has been hypothesised that a strong condemnation of smoking by the school communicates to young people that smoking is an unacceptable part of mainstream identities (Lloyd 1998). A further possibility is that STPs strengthen the connection to school among students and staff, as well as school ethos beyond its regulatory content (Fletcher 2008). An STP can also reduce youth smoking by directly limiting smoking opportunities and access to tobacco (Alesci 2003).
The teachers' perceived capacity to act as role models is an important element of the success of this type of intervention. Galaif 1996 found that teachers will comply with a smoking regulation only if they believe that they can directly affect students' smoking behaviour. If students who smoke perceive that it is acceptable for teachers to smoke in school, they are less likely to adhere to school smoking bans. For this reason Trinidad 2005 argues that encouraging teachers not to smoke on school grounds should be considered as a key component of school‐based tobacco prevention programmes; however, conversely smoking bans may encourage teachers to smoke outside school, with the unanticipated result of making teachers who smoke even more visible to students (Wold 2004).
Why it is important to do this review
Implementing STPs was described as a promising strategy to prevent smoking initiation among adolescents(Bowen 1995) However, it is not yet clear whether this approach is effective. It is unclear whether policies contribute to a reduction of youth smoking only when they are included in a comprehensive tobacco control plan at the school level (Lovato 2010a), or whether a policy constitutes a suitable and cost‐effective stand‐alone intervention (Reid 1999). A summary of evidence is critical in order to define which STP elements are effective, and which require further research.
Objectives
To assess the effectiveness of policies aiming to prevent smoking initiation among students by regulating smoking in schools. We addressed the following questions:
Do school tobacco policies (STPs) reduce youth smoking prevalence?
Do school tobacco control policies delay the start of smoking in adolescents?
Do school tobacco control policies reduce the number of cigarettes among smokers?
Which characteristics, if any, of STPs increase their impact.
Methods
Criteria for considering studies for this review
Types of studies
We include cluster‐randomised controlled trials (c‐RCTs) in which schools or classes were randomised to receive different levels of smoking policy or no intervention. As we expected to find a limited number of RCTs, if any, the following prospective designs were also eligible; non‐randomised controlled trials, interrupted time series and controlled before‐after studies. Cross‐sectional studies were not formally included. In the absence of higher quality evidence, their findings were described and used to generate hypotheses for future studies.
Types of participants
Students in primary and secondary schools (10 to 18 years old).
Types of interventions
All written policies that regulate tobacco use inside and/or outside the school property were eligible. We would have classified interventions as partial bans, inside bans and comprehensive policies.
We would have included studies of policies aiming to ban drug or alcohol use in addition to smoking if tobacco use outcomes were reported. We would have considered interventions in which an STP was a component of a smoking prevention program only if it was possible to isolate its effect. Studies that compared stronger and weaker policies were eligible. We would have considered whether the implementation of a policy had an impact on its effect.
Types of outcome measures
Primary outcomes
Smoking prevalence among students, measured by individual self‐report. Biochemically validated smoking data, where provided, were used in preference to self‐report. Young people were classified as smokers or non‐smokers in different ways (daily, weekly, monthly, ever, non‐smoker, smokeless tobacco user, smoker). Where multiple definitions were provided, we used the strictest measure given. In studies with multiple follow‐up periods, we would have used data from the longest follow‐up period reported.
Secondary outcomes
1. Actual tobacco use by teachers and school staff. 2. Tobacco use of teachers, school staff, and students as perceived by other students. 3. Compliance with the policy by students, teachers and school staff. 4. Exposure to environmental tobacco smoke.
Search methods for identification of studies
We conducted the most recent search in May 2014.
We searched the following databases:
1. Cochrane Tobacco Addiction Group's Specialised Register 2. Cochrane Central Register of Controlled Trials (CENTRAL) 3. MEDLINE 4. EMBASE 5. PsycINFO 6. ERIC (Educational Resources Information Center) 7. Sociological abstracts (CSA) 8. 'Grey' literature (conference proceedings and unpublished reports) via Google Scholar and dissertation abstracts. 9. Unpublished literature, by searching trial registers (www.clinicaltrials.gov, www.controlled‐trials.com, www.clinicaltrialsregister.eu) and contacting researchers and agencies whom are known to have conducted or sponsored relevant research to identify further studies not found and unpublished reports.
The Tobacco Addiction Group Specialized Register contains reports of controlled trials of interventions for smoking cessation or prevention, evaluations of tobacco control policies, identified from regularly updated highly sensitive searches of CENTRAL, MEDLINE, EMBASE, PsycINFO, and the Science Citation Index. The search strategy for the register used the following topic related terms; (polic* or ban* or restriction* or rule* or environment* or health promoting or smoke‐free) AND (school*) in title, abstract or keyword fields. The search strategies for MEDLINE, EMBASE and PsycINFO combined these topic terms with the smoking and tobacco terms and the study design terms used for the Register searches. The full MEDLINE search strategy can be found in Appendix 1. Searches of ERIC, Sociological Abstracts and other sources combined topic related and smoking related terms.
Searching other resources
We checked cited studies in all studies identified. We did not apply language restrictions. In the case of languages other than English, French, German, Italian, Spanish, Portuguese, Greek, Russian or Swedish, we would have looked for translation facilities within the Cochrane Collaboration.
Data collection and analysis
Selection of studies
All search results were imported into an electronic register. Titles and abstracts were classified according to their relevance to the review. Once bibliographic searches was completed, all retrieved records were assembled in a database and processed in order to de‐duplicate them (i.e., remove duplicate records). Two reviewers (AC, FF) screened all identified studies in the electronic databases. Articles were rejected if the title or abstract was not pertinent to the topic of the review. Any disagreements was resolved between the two reviewers by referring to the full‐text, and by consulting with a third party when necessary (MRG). The same reviewers conducted further screening of the full text of the studies that passed the initial screening stage.
Data extraction and management
Two reviewers (AC, FF) independently extracted data from the selected study using a tailored standardised data extraction form including the following elements:
Country
School level
Participants (demographic information)
Intervention (characteristics of the policy)
Outcomes, and how they are measured
Length of follow‐up from the introduction of the policy
Completeness of follow‐up
Definition of smoking
Any discrepancies were resolved through discussion or, if required, through consultation with a third person (MRG).
Assessment of risk of bias in included studies
Two review authors assessed independently risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011): • adequate sequence generation; • adequate allocation concealment; • blinding of personnel/outcome assessors; • addressing incomplete outcome data; • free of selective outcome reporting; • free of other bias. For each of these domains, risk of bias was judged High, Low, or Unclear Any disagreement was resolved by discussion or by involving a third assessor.
Measures of treatment effect
For dichotomous data, we used the risk ratio (RR) to summarize individual trial outcomes ((number of events in intervention condition/ intervention denominator)/ (number of events in control condition/control denominator)) with 95% confidence intervals. For our primary outcome, the RR was calculated using the student population of the school as the denominator ((number of student smokers in intervention condition/student population in intervention condition)/(number of student smokers in control condition/student population in control condition)). Where the event measured was students classified as smokers, a risk ratio less than one indicated that fewer students were smokers in the intervention group than in the control group. For continuous data, we used the mean difference if outcomes were measured in the same way between trials. We used the standardised mean difference to combine trials that measured the same outcome, but use different methods.
Unit of analysis issues
Though in cluster randomised trials we expected the school (or classes) to be the unit of randomisation, we used the individual as the unit of analysis. We reported adjustments for design effect when provided and dealt with any unit of analysis issues using the guidance in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Dealing with missing data
If the proportion of missing data suggested a risk of bias, the study would have been classified accordingly and included in a sensitivity analysis. Participants who has been missing follow‐up data for our primary outcome would have been counted as smokers in an intention‐to‐treat analysis.
Assessment of heterogeneity
The statistical heterogeneity was to be examined using the I2 statistic. However, this was not necessary as we included only one study.
Assessment of reporting biases
Had we found sufficient studies, we would have tested publication bias using a funnel plot. The relevance of outcomes had been checked to determine if there was any bias in outcome reporting.
Data synthesis
If we had found sufficient studies we would have carried out summary analyses using RevMan 5.1. We would have used the Mantel‐Haenszel fixed‐effect model for meta‐analyses, combining data where trials examined the same intervention and populations and methods were judged sufficiently similar. Where we had suspected clinical or methodological heterogeneity between studies sufficient to suggest that treatment effects may differ between trials, we would have used a random‐effects meta analyses.
Subgroup analysis and investigation of heterogeneity
If relevant studies had been available, we would have conducted subgroup analyses for the following policy characteristics: • ban extended only to school staff versus extended both to staff and students; • only indoor area affected by the ban versus ban extended to outdoor area; • policies enforced by punishment versus policies not enforced by punishment; • policies as stand‐alone interventions versus policies accompanied by educational programmes.
In the presence of substantial heterogeneity, we would have explored the reasons for this, undertaking sensitivity analyses (if there have been sufficient studies to warrant this approach).
Results
Description of studies
Results of the search
Figure 1 shows the study selection process (up to May 2014). Two review authors (AC, FF) independently assessed all the titles and abstracts identified as a result of the comprehensive updated search. Initially 2182 citations were identified in the electronic databases, of which 1702 remained after de‐duplication. No ongoing studies were found in trial registers. We excluded 1553 studies after screening the titles and then 90 after reading the abstracts. At the end of selection process we included one study in this review, which aimed to study the effect of the introduction of smoking policies at school.
1.
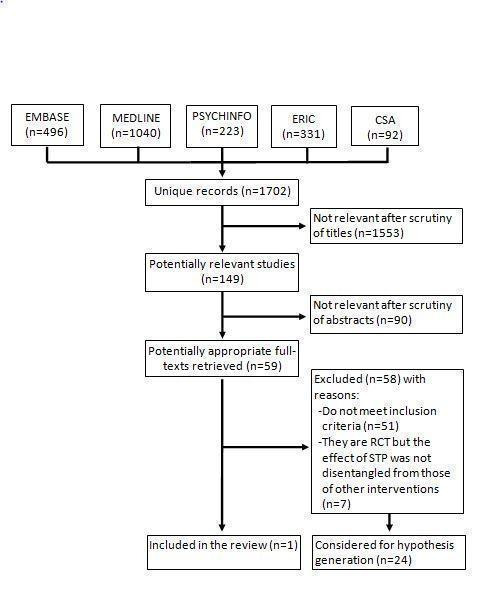
Study flow diagram
Included studies
The included study (Chen 2014) was conducted in 2008 in two Chinese regions and involved two schools in the intervention group and two in the control group. Of a total of 1807 participants aged between 13 and 15 years old, 941 students attended intervention schools and 866 attended control schools. The students were then surveyed a year later about their smoking habits. To assess the frequency of smoking, participants were asked whether they smoked daily, weekly, or were smoking currently. Ever‐smoking was defined as having ever used cigarettes, even one or two times. Characteristics of the intervention were: smoking banned inside the school; peer educators trained to encourage smokers to quit; and brochures about health hazards of smoking distributed among students. The study measured changes in students' smoking behaviour, knowledge and attitudes. The Characteristics of included studies table provides further details on participants, interventions, and outcomes of the study.
Excluded studies
Among the 58 studies that were excluded, 51 were observational and therefore not eligible. Seven studies were randomised controlled trials (RCTs) (Andersen 2012, Elder 1996, De Vries 2006, Gorini 2014, Hamilton 2005, Schofield 2003, Wen 2010), evaluating multi‐modal programmes, but it was not possible to disentangle the effect of STP from those of others interventions, and so they were excluded. Of the 51 observational studies, 27 reported a predictor not suitable for this review (STP not sufficiently specified) or no outcome suitable for the review. The Characteristics of excluded studies table provides details of the respective reasons for excluding each study. The remaining 24 studies reported an effect on students' smoking behaviour and information about the policies' characteristics was collected through interviews with school staff. Even if excluded from the review, they were considered useful for hypothesis generation. All but one were cross sectional studies, while one (Rosendhal 2002) was a cohort study. Twenty‐two studies involved middle or secondary schools, and two were conducted in primary schools (Rosendhal 2002; Huang 2010). Information about the study, characteristics of the policy and main results are summarised in Table 2.
1. Characteristics of cross‐sectional studies.
| Nr ref | Study | Participants | Characteristics of the policy | Associations with outcomes |
| 1 | Adams 2009 | 16561 students in grade 7 ‐ 12 (age 12 ‐ 17) attending 20 middle schools and 20 high schools in 24 towns in northern and central Illinois (USA) 2002 ‐ 2005 | STP measured with 2 scales: a) Enforcement (beliefs about the relative problem of youth tobacco use at school, level of active enforcement, strategies employed to enforce the policy, staff and student perceptions about the policy, environmental factors that may be related to tobacco use at school such as assessment of closed vs open campus) b) Comprehensiveness (defined as applicability, restrictions, repercussions, programmes, notification, and evaluation of the written policies) | Enforcement linked to lower odds of smoking (OR 0.83, 95% CI: 0.70 to 0.99) but not with comprehensiveness nor with the interaction between comprehensiveness and enforcement |
| 2 | Barnett 2007 | 763 students (mean age 13) in 50 schools and 762 students (mean age 16) in 57 schools in Quebec (Canada) in 1999. 25 students randomly selected in each school |
STP defined as staff permitted to smoke indoors/outdoors; students permitted to smoke on school ground | Policies permitting students to smoke indoors were not associated with daily smoking among either 13‐ or 16‐year‐old students. Policies permitting staff to smoke outdoors were significantly associated with daily smoking among 13‐year‐old students. Multivariate effect limited to staff smoking outdoors among 13 years girls (OR 4.8, 95% CI: 1.1 to 21.1) |
| 3 | Boris 2009 | 4469 students in grade 9 (mean age 15.4) and 1041 teachers in high schools in Louisiana (USA) in 2004 |
Comparison between schools prohibiting all tobacco use by anyone on the school campus and at all school events (no‐use policy) and schools that allow teachers and other staff to smoke in one 'restricted' area on campus (restricted‐use policy) | No differences in students smoking in the 2 types of schools |
| 4 | Clarke 1994 | 26,429 students from grades 7 ‐ 12 (12 ‐ 18 years) from 351 secondary schools and 347 teachers in Australia in 1990 | All the schools have a smoking policy for students; differences between school about policies' characteristics for teachers and visitors and presence of smoking signs around the school | Smoking prevalence unrelated to staff and visitor smoking policy and presence of smoking signs |
| 5 | Darling 2006 | 26,58 students in grade 10 and 12 (mean age 15) from 63 schools in New Zealand in 2002 |
STP focus categorized as punishment (having sanctions for students who were caught smoking), cessation (having a cessation support), prevention (having included prevention guidelines), comprehensiveness (having communicate students to be smoke‐free and informed the public about the policy); each group of schools was contrasted with the group of schools not having the specific focus | No association between any policy component or intensity with current smoking |
| 6 | Evans‐Whipp 2010 | 3466 students in grade 8 and 10 (age 13 ‐ 15) from 285 schools: 153 (1777 students) in Washington state (USA) and 132 (1689 students) in Victoria state (Australia) in 2003 |
STP components: comprehensiveness (teachers and staff covered by smoking policy; in force on school grounds and during school‐related activities where students are present; extended to visitors) enforcement (policy rated between 'strictly enforced' and 'not at all strictly'), 'harsh' (expulsion, calling the police and out of school suspension) or 'remedial' (referred to a school counsellor or nurse, recommended to participate in an assistance, education, or cessation programme or required to participate in an assistance, education, or cessation program) response for students violating the policy, orientation (emphasizing of total abstinence from drug use and emphasizing harm minimisation) |
No differential effects of policy dimensions on current and daily smoking (between harm minimisation and abstinence policies, and between comprehensive and non‐comprehensive smoking ban) |
| 7 | Galán 2012 | 9127 students attending 4th year of compulsory secondary education (15 ‐ 16 years) from 203 schools in Spain, 2001 ‐ 2005 | Variables taken into account: years before (2001 – 2002) and after (2003, 2004, 2005) the introduction of the law banning smoking at school; characteristics related to the school centre (compliance with the law banning smoking; written reference to smoking control policy in the school regulations; existence of complaints about smoking; undertaking of educational activities regarding smoking prevention) | No differences in smoking prevalence and amount of smoking between the schools that complied with the legislation and those that did not, or with those centres including smoking prevention policies in the school regulation |
| 8 | Hamilton 2003 | 4697 students in grade 9 (mean age 13.6) from 31 schools in Australia in 1999 |
STP components: involvement in school health promotion projects, formation of a school health committee, presence of a health policy and a written drug policy, availability of counselling, education, and discipline strategies used to deal with students caught smoking, quit strategies used to support students and staff who smoke | No association with having a health committee and a drug policy. Counseling, education for students caught smoking associated with lower probability of ever smoking (OR 0.73; 95% CI 0.64 to 0.84) or regular smoking (OR 0.67; 95% CI 0.53 to 0.85) |
| 9 | Huang 2010 | 2350 students from grade 3 ‐ 6 (mean age 10.9) from 26 schools in South Taiwan in 2008 |
STP components: a) Policy status (written/informal/uncertain policy) b) Smoking restrictions (smoking banned completely on school premises/permitted in restricted areas] c) Level of enforcement of smoking restrictions (always/not always) d) Health education related to tobacco, participation in smoke‐free health promotion events, access to cessation programmes and sanctions imposed on students smoking at school |
No association with written policy status or restrictions; Ever‐smoking elevated for students in schools without anti‐tobacco activities or curricula |
| 10 | Kumar 2005 | 35,745 students in grade 8, 10 and 12 (age 13 ‐ 16) in 342 schools of Michigan (USA) in 1999 and 2000 |
STP components: a) Monitoring of students' compliance b) Severity of consequences when students are caught violating the policy c) School policy regulating tobacco use by staff |
Monitoring students' behaviour negatively associated with current daily smoking in middle, but not in high schools. Severity of consequences positively related to smoking in high schools, but no longer after adjustments. Permission for staff to smoke positive predictor of smoking in high schools |
| 11 | Lovato 2007 | 22,318 students in 10 ‐ 11 grade (15 ‐ 19 years old) from 81 schools in Canada |
STP characteristics derived from a) Written policies coded in developing, overseeing and communicating the policy; purpose and goals; prohibition; strength of enforcement; characteristics of enforcement; tobacco use prevention education and assistance to overcome tobacco addictions b) School administrators' interviews on STP implementation c) students' survey on perception of policy enforcement |
Smoking prevalence was only significantly correlated with perception of smoking prevalence, but not with policy. On school property smoking prevalence, but not smoking prevalence related to consistency of enforcement in policy implementation |
| 12 | Lovato 2010a | 27,892 students from grade 5 ‐ 9 (age 10 ‐ 14) from 281 elementary and secondary schools (mean age 16) in 10 Canadian provinces in 2004 ‐ 2005 |
Policy enforcement derived from information about who was involved in policy development, how students were informed, and the nature of enforcement | Purpose and goals clearly stated (OR 0.38; 95% CI 0.15 to 0.95) and presence of an enforcement officer (OR 0.60; 95% CI 0.36 to 0.99) associated with lower probability of being a smoker. Availability of assistance to quit smoking was associated with a higher probability of smoking (OR 2.23; 95% CI 1.12 to 4.45) |
| 13 | Lovato 2010b | 24,474 students in 10 ‐ 11 grade (15 ‐ 19 years old) from 82 randomly sampled secondary schools in 5 Canadian provinces (during the 2003 – 2004 school year) |
School policy intent extracted by examining written documentation on smoking policies. Policy enforcement derived by principals' or teachers' interviews. Tobacco control programmes data derived from a survey completed by school administrators | Strong prohibition in the written policy was associated with a lower probability of smoking (OR 0.92; 95% CI 0.88 to 0.97). Policy enforcement (OR 1.20; 95% CI 1.07 to 1.35) and enforcement officer (OR 1.22; 95% CI 1.04 to 1.43) were associated with higher probabilities of smoking. Focus on preventive programmes was associated with a lower probability of smoking (OR 0.87; 95% CI 0.81 to 0.94) |
| 14 | Moore 2001 | 1375 students in year 11 (aged 15 ‐ 16) from 55 schools in Wales (UK) in 1998 |
STP coded as: 1. Written policy where pupils and teachers were not allowed to smoke anywhere on the school premises 2. No written policies for pupils and teachers and/or teachers allowed to smoke in restricted areas 3. Either no smoking policy for pupils or for teachers. Level of extension of the ban, enforcement |
Weak policy was associated with daily (OR 3.84; 95% CI 1.76 to 8.37) and weekly (OR 2.55; 95% CI 1.26 to 5.15) smoking. Low enforcement associated with daily (OR 1.41; 95% CI 0.96 to 2.07) and weekly (OR 1.32; 95% CI 0.92 to 1.91) smoking for pupils. In logistic regression models the associations remained, even after adjustment for individual‐level variables. Low enforcement for teachers compared to high enforcement was not associated with pupils' daily (OR 1.03; 95% CI 0.66 to 1.59) or weekly (OR 0.86; 95% CI 0.56 to 1.31) smoking |
| 15 | Murnaghan 2007 | 3965 students in grade 12 (mean age 17.6) from 10 schools in Canada, surveyed 1999 ‐ 2001 |
Repeated cross‐sectional with comparison time to assess the effect of implementation of smoking prevention programmes and introduction of STP in a school district. Characteristics of STP not reported | Students exposed to educational and cessation programmes less likely to be occasional smokers rather than non‐smokers (OR 0.42; 95% CI 0.18 to 0.97). Students exposed to STP (OR 1.06; 95% CI 0.67 to 1.68) or the combination of the 2 did not differ from the reference group (OR 0.83; 95% CI 0.61 to 1.12) |
| 16 | Murnaghan 2008 | 4709 students in grade 10 (age 15 – 16) ) from 10 schools in Canada, surveyed 1999 ‐ 2001 |
Repeated cross‐sectional with comparison time to assess the effect of implementation of smoking prevention programmes and introduction of STP in a school district. No report of the characteristics of STP. | STP only associated with non‐significant decrease of occasional smoker vs current non‐smokers (OR 0.72; 95% CI 0.50 to 1.03) and increase of regular smokers vs occasional smokers (OR 1.54; 95% CI 1.04 to 2.29). Smoking prevention only associated with a significant reduction of occasional (OR 0.57; 95% CI 0.44 to 0.75), but not of regular smoking (OR 0.94; 95% CI 0.69 to 1.28). Presence of both activities not associated with students' smoking |
| 17 | Paek 2013 | 983 students in grades 9 and 12 (age 12 ‐ 19) from 14 schools in Michigan (USA) | STP components: types of prohibiting tobacco products, hours of prohibiting tobacco use, places of prohibiting tobacco use, communication of tobacco policy, person in charge of enforcing tobacco policy, designation of a tobacco‐free school zone, anti‐smoking communications, tobacco cessation services, actions taken for students who are caught smoking cigarettes, stringency of tobacco policy enforcement | No association with policy variables after controlling for individual characteristics |
| 18 | Pentz 1989 | 4807 students in grade 7 (mean age 12) in 23 schools in California (USA) in 1986 | STP components: comprehensiveness (presence of formal rule about no smoking on school grounds, near school grounds, closed campus policy, formal health education plan for smoking prevention programming, prevention emphasis, cessation emphasis, punishment emphasis, policy enforcement, time in effect, consequences for violation (7 categories increasing in severity), policy on school ground | Higher number of components and emphasis on prevention rather than cessation associated with statistically non‐significant lower school smoking prevalence both weekly and in last 24 hrs. High punishment emphasis not associated with lower prevalence. More consistent effect obtained on amounts of smoking rather than on prevalence rates in particular, with high emphasis on prevention and low emphasis on cessation |
| 19 | Piontek 2008b | 3364 students (mean age 14.05, range 10 ‐ 21) from 40 schools in Germany |
STP characteristics investigated: a) Extension of smoking ban for students (in school building, on school grounds, or in immediate surroundings) b) Extension of smoking ban for adults (teachers, non‐teaching staff, school visitors in school buildings) c) Monitoring of students’ compliance with the smoking ban (monitored regularly in corridors, rest rooms and on school grounds) d) Sanctions following breaking the smoking rules (different sanction activities) e) Offers of smoking cessation courses f) Smoking prevention activities. Mediating variables: school engagement, attachment to school, risk behaviours, use of substances |
Comprehensive ban for students (OR 0.62; 95% CI 0.42 to 0.92) and presence of evidence‐based prevention programmes (OR 0.62; 95% CI 0.39 to 0.99) associated with lower smoking prevalence. Smoking prevalence not affected by smoking restrictions for adults, sanctions, monitoring of students or availability of smoking cessation |
| 20 | Rosendhal 2002 | (Cohort study) 2883 children recruited in the 5th grade with follow‐up in 6th grade across 213 classes from 91 compulsory schools in Sweden in 1997 |
STP assessed through questions about formal adoption of a local anti‐smoking policy; implementation of a local plan for anti‐tobacco education; ongoing pedagogic activities against tobacco; presence of a smoking room for the staff; and availability of smoking cessation programmes for staff or for students | Having formally adopted a STP is not associated with smoking prevalence (OR 1.06; 95% CI 0.80 to 1.41) |
| 21 | Sabiston 2009 | 24,213 students in grade 10 and 11 (mean age 16) in 81 schools in Canada during 2003 – 2004 school year |
STP reported in written policy (intent) and by administrators' interview. characteristics examined were: participation and communication (excellent if students were involved in the development of the policy, group appointed to oversee the policy, communication to students); stated goals and purpose (excellent if all groups in school were prohibited from all tobacco), strength of enforcement (excellent if verbal and written warnings were delivered to the student and parent/guardian, and sanctions were based on zero tolerance); characteristic of the enforcement (excellent if more than one person/group was designated as ensuring policy enforcement, and the policy outlined clear enforcement strategies), prevention education; availability of cessation programmes, time in effect | Prohibition (OR 0.83; 95% CI 0.72 to 0.95) and availability of cessation assistance (OR 0.74; 95% CI 0.60 to 0.92), but not prevention education (OR 1.23; 95% CI 0.96 to 1.57), linked to lower probability of smoking; length of time a policy was in place associated with a 1% increase in smoking probability per year |
| 22 | Sinha 2004b | 6587 students (age 13 ‐ 15) from 50 State and 50 Federal schools in India in 2000 ‐ 2001 |
Federal schools having STP contrasted to State schools (no STP). STP consists in specific rules and regulations prohibiting use of tobacco and tobacco products on school premises by students, school personnel, parents, and visitors | In State schools there was 5 ‐ 6 times higher prevalence of any tobacco and smokeless tobacco use, 3 ‐ 4 times higher prevalence of any smoking, and 5 ‐ 6 times higher prevalence of cigarette smoking |
| 23 | Wiium 2011a | 1941 students in grades 10 and 11 (age 11 ‐ 16) from 45 schools in Wales (UK) in 2001 ‐ 2002 | STP characteristics examined: policy restriction; formal policy (whether written); staff policy approach (consultative vs prescriptive); dissemination for pupils and staff; sanctions for students (underline health or underline transgression); consistency between policy, environment and school | No association with policy variables after controlling for individual characteristics. The only statistically significant association found was that pupils attending schools that did not disseminate pupil smoking policy in a written document had a greater tendency (OR 2.16; 95% CI 1.13 to 4.10) to smoke daily on school premises than those who attended schools that disseminated policy through a written document |
| 24 | Wiium 2011b | 1404 students (mean age 15) from 73 schools in Norway |
STP characteristics examined the extent to which actions taken by schools (i.e., informing parents of adolescents’ violation of the school tobacco policy, disciplining and counselling adolescents who are caught smoking) changed prevalence | School enforcement of smoking restrictions was not related to adolescent smoking prevalence (OR 1.29; 95% CI 0.80 to 2.05) |
All the studies are cross‐sectional with the exception of Rosendhal 2002 that is a cohort study.
Risk of bias in included studies
The only study included (Chen 2014), had a small sample size of only 4 schools, a high risk of intraclass correlation, a likely absence of blinding, and lack of information to assess the presence of selective reporting; we judged the risk of bias of this study to be very high. This assessment is summarised in Figure 2.
2.
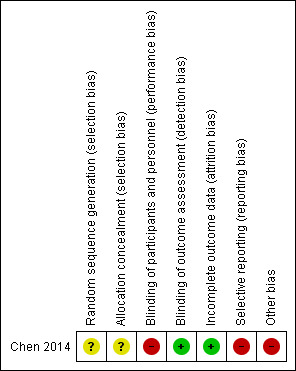
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Effects of interventions
See: Table 1
In Chen 2014 a school tobacco policy (STP) was not significantly associated with all smoking outcomes studied. There weren't substantial differences in the prevalence of current smokers between intervention and control schools in either of the two regions: risk ratio (RR) 0.98 (95% CI 0.71 to 1.4) and RR 1.35 (95% CI 0.57 to 3.2). The study didn't consider other outcomes of interest for this review.
Studies considered for hypothesis generation
Using data from 24 observational studies, we were interested if specific characteristics of STPs were associated with students smoking behaviour. The characteristics analysed were the following:
formally‐adopted STP vs no policy
ban extended outdoor school premises vs internal ban
ban extended to teachers vs teachers' smoking allowed in limited area
STP including (types of) sanctions for transgressors vs including weak or no sanctions
STP including assistance to quit for smokers vs STP without assistance
STP plus prevention components vs STP alone
STP highly enforced vs weakly or not enforced
The mere adoption of an STP did not seem to affect smoking behaviour. Nine studies measured the effects of a formally‐adopted STP on students' smoking. These studies present mixed results, as three studies showed lower prevalence of smoking in schools with STPs, when compared with schools without a formal policy (Lovato 2010b; Moore 2001; Sinha 2004b), while six studies reported no differences (Galán 2012; Hamilton 2003; Huang 2010; Murnaghan 2007; Murnaghan 2008; Rosendhal 2002).
We also analysed the effects of five aspects of policy: extent of a smoking ban, inclusion of teachers' smoking, sanctions for transgression, assistance for smoking cessation, and a ban combined with prevention and education activities. Only a few studies reported results to support the effects of these features.
With respect to the extent of bans, one study detected a difference in students' smoking prevalence, when comparing schools which prohibited students’ smoking on school premises or outdoors, with those which permitted smoking (Piontek 2008b). Three studies found no differences (Barnett 2007; Huang 2010; Pentz 1989); however, of these Pentz 1989 found a difference only in the number of cigarettes smoked.
One policy forbidding teachers to smoke was associated with a decrease in students' daily smoking (Kumar 2005). Prohibition of indoor smoking for teachers was not significantly associated with student smoking, while prohibiting teachers from smoking outdoors was associated only with decreased daily smoking in girls aged 13 years, but not among boys and girls aged 16 years (Barnett 2007). In Boris 2009, Clarke 1994, Piontek 2008b, and Wiium 2011a, comprehensive policies prohibiting teachers from smoking, when compared with those allowing them to smoke in restricted areas, were not related to student smoking.
Nine studies considered the relationship between sanctions for students found smoking and smoking prevalence. Sanctions cited in the STP were not related to smoking prevalence in the majority of the studies (Darling 2006; Pentz 1989; Piontek 2008b; Wiium 2011a). Harsh and remedial penalties (Evans‐Whipp 2010), the severity of sanctions (Kumar 2005; Paek 2013), and sanctions put in place at school and informing parents (Wiium 2011b) were not associated with adolescent smoking. In one study (Hamilton 2003) counselling and education for students caught smoking appeared to be more effective against student smoking than a disciplinary approach alone.
Seven studies considered the effect of assistance with smoking cessation for students. Out of these, only Sabiston 2009 showed a link to a lower probability of smoking. Of the others, five studies did not show a link (Darling 2006; Evans‐Whipp 2010; Lovato 2007; Pentz 1989; Piontek 2008b); in fact Pentz 1989 reported a higher number of cigarettes smoked in schools where cessation support was available. Moreover, Lovato 2010a showed that in schools that mandated cessation programmes students had a higher probability of smoking.
Six studies compared the effect of 'STP only' to 'STP with prevention and education components', but did not find an association with reduction of smoking prevalence (Darling 2006; Lovato 2007; Murnaghan 2007; Murnaghan 2008; Pentz 1989; Sabiston 2009). Pentz 1989 reported lower numbers of cigarettes smoked and lower smoking prevalence (although not statistically significant) in schools with smoking ban policies and smoking prevention programmes.
Eleven of the considered studies focused particularly on the role of policy enforcement. Four studies showed that policy enforcement was linked to lower rates of smoking (Adams 2009; Kumar 2005; Moore 2001; Sabiston 2009). In one study, the data were in favour of schools adopting policy enforcement, but the effect was no longer statistically significant after adjustment for state, gender, age and family socioeconomic status (Evans‐Whipp 2010). The presence of an enforcement officer, but not the strength of the enforcement, was associated with a lower probability of smoking in one study (Lovato 2010a). Smoking prevalence was not related to policy enforcement in two studies (Lovato 2007; Wiium 2011b). One study found no difference in smoking prevalence between schools with a high versus a low degree of monitoring of students’ compliance with the policy (Piontek 2008b). In contrast, Lovato 2010b found that students were more likely to smoke if they attended a school with stronger enforcement of the tobacco policy. Policy enforcement for teachers was not associated with a difference in daily and weekly smoking among students in one study (Moore 2001).
Table 2 shows further details on characteristics, outcomes and results of the considered studies for hypothesis generation, while Table 3 summarizes the effect of policies' characteristics on students' smoking behaviour as reported in the studies.
2. Summary of comparisons.
| Characteristics of the policy | Studies (Refs) | N. participants (country) | Age of participants |
Results (*=statistically significant) ORs and RRs need a 95% CI |
| Formally‐adopted STP vs no policy | ||||
| Favours policy (3) | Lovato 2010b | 24,474 (Canada) | 15 ‐ 19 years | OR 0.92* current smoker (last 30 days) |
| Moore 2001 | 1375 (UK) | 15 ‐ 16 years | OR 0.26* daily smoker | |
| Sinha 2004b | 6587 (India) | 13 ‐ 15 years | OR 0.2* current smoker | |
| Total: 32, 436 | ||||
| No difference (6) | Galán 2012 | 9127 (Spain) | 15 ‐ 16 years | OR 0.96 current smoker |
| Hamilton 2003 | 4697 (Australia) | 13.6 mean age | OR 0.82 regular smoker | |
| Huang 2010 | 2350 (Taiwan) | 10.9 mean age | No differences (values not reported) | |
| Murnaghan 2007 | 3965 (Canada) | 17.6 mean age | OR 1.06 occasional smoker | |
| Murnaghan 2008 | 4709 (Canada) | 15 ‐ 16 years | OR 0.72 occasional smoker | |
| Rosendhal 2002 | 2883 (Sweden) | 10 ‐ 11 years | RR 1.06 ever smoker | |
| Total: 27,731 | ||||
| Ban extended outdoor school premises vs internal ban | ||||
| Favours policy (1) | Piontek 2008b | 2818 (Germany) | 10 ‐ 21 years | OR 0.62* current smoker (last 30 days) |
| Total: 2818 | ||||
| No difference (3) | Barnett 2007 | 762 (Canada) | 13 ‐ 16 years | 20.8% (school with outdoor ban) vs 23.6% (school without outdoor ban) daily smoker prevalence |
| Huang 2010 | 2350 (Taiwan) | 10.9 mean age | No differences (values not reported) | |
| Pentz 1989 | 4807 (USA) | 12 ‐ 13 years | 4.93% (schools with comprehensive STP) vs 5.60% weekly smoker | |
| Total: 7919 | ||||
| Ban extended to teachers vs teachers' smoking allowed in limited area | ||||
| Favours policy (2) | Barnett 2007 | 395 (Canada) | 13 mean age | OR 0.2* (staff cannot smoke outdoors) daily smoker among 13 years (girls) |
| Kumar 2005 | 35,745 (USA) | 13 ‐ 16 years | OR 1.24 daily smoker in middle schools and OR 0.82 in high schools | |
| Total: 36,140 | ||||
| No difference (5) | Barnett 2007 | 1130 (Canada) | 13 ‐ 16 years | 23.3% (staff can smoke outdoors) vs 22.8% (staff cannot smoke outdoors) daily smokers among 13 years (boys) and 16 years (P = ns) |
| Boris 2009 | 4469 (USA) | 15.4 mean age | 24.6% (staff cannot smoke) vs. 25.2% (staff can smoke in restricted area) 30‐day cigarette smoking prevalence (P = ns) | |
| Clarke 1994 | 26,429 (Australia) | 12 ‐ 18 years | 27.2% (staff not allowed to smoke) vs 30.9% (no restrictions) weekly smokers among grade 11 and 12 (P < 1) | |
| Piontek 2008b | 2818 (Germany) | 10 ‐ 21 years | ß coefficient –0.06 current smoker | |
| Wiium 2011a | 1941 (UK) | 11 ‐ 16 years | 16.4% (staff not allowed to smoke) vs 18.6% (restricted area) daily smokers | |
| Total: 36,787 | ||||
| STP highly enforced vs weakly or not enforced | ||||
| Favours policy (4) | Adams 2009 | 16,561 (USA) | 12 ‐ 17 years | OR 0.83* current smoker (last 30 days) |
| Kumar 2005 | 35,745 (USA) | 13 ‐ 16 years | OR 0.81* daily smoker in middle school, OR 1.03 in high school | |
| Moore 2001 | 1375 (UK) | 15 ‐ 16 years | OR 0.65* daily smoker | |
| Sabiston 2009 | 24,213 (Canada) | 16 mean age | OR 0.90* current smoker (last 30 days) | |
| Total: 77,894 | ||||
| No difference (5) | Evans‐Whipp 2010 | 3466 (USA and Australia) | 13 ‐ 15 years | OR 0.78 current smoker (last 30 days) |
| Lovato 2007 | 22,318 (Canada) | 15 ‐ 19 years | OR 1.11 smoking prevalence | |
| Lovato 2010a | 27,892 (Canada) | 10 ‐ 14 years | RR 1.63 current smoker (last 30 days) | |
| Piontek 2008b | 2818 (Germany) | 10 ‐ 21 years | ß coefficient 0.25 current smoker | |
| Wiium 2011b | 1404 (Norway) | 16 mean age | OR 1.29 daily smoker | |
| Total: 57,898 | ||||
| Favours controls (1) | Lovato 2010b | 24,474 Canada | 15 ‐ 19 years | OR 1.20* current smoker |
| Total: 24,474 | ||||
| STP including (types of) sanctions for transgressors vs including weak or no sanctions | ||||
| Favours counselling and education for students vs disciplinary approach only (1) | Hamilton 2003 | 4697 Australia | 13.6 mean age | OR 0.67* regular smoker |
| Total: 4697 | ||||
| No difference (8) | Darling 2006 | 2658 (New Zealand) | 15 mean age | RR 0.89 daily smoker in school with sanctions included in the policy |
| Evans‐Whipp 2010 | 3466 (USA and Australia) | 13 ‐ 15 years | OR 0.99 current smoker (last 30 days) | |
| Kumar 2005 | 35,745 (USA) | 13 ‐ 16 years | OR 0.98 daily smoker in middle school, OR 1.01 in high school | |
| Paek 2013 | 983 (USA) | 12 ‐ 19 years | ß coefficient −0.02 current smoker (last 30 days) | |
| Pentz 1989 | 4807 (USA) | 12 ‐ 13 years | 4.91% weekly smokers in school with high punishment emphasis vs 5.38% in school with low punishment emphasis | |
| Piontek 2008b | 2818 (Germany) | 10 ‐ 21 years | ß coefficient 0.10 current smoker with punishment emphasis | |
| Wiium 2011a | 1941 (UK) | 11 ‐ 16 years | 18.1% (sanctions tending to health) vs 15.7% (sanctions tending to discipline) daily smokers | |
| Wiium 2011b | 1404 Norway | 15 years | OR 0.65 daily smoker when pupils were disciplined at school vs other forms, OR 2.90 daily smoker when parents were informed vs other forms | |
| Total: 53,822 | ||||
| STP including assistance to quit for smokers vs STP without assistance | ||||
| Favours policy (1) | Sabiston 2009 | 24,213 (Canada) | 16 mean age | OR 0.74* current smoker (last 30 days) |
| Total: 24,213 | ||||
| No difference (5) | Darling 2006 | 2658 (New Zealand) | 15 mean age | RR 1.17 daily smoker |
| Evans‐Whipp 2010 | 3466 (USA and Australia) | 13 ‐ 15 years | OR 1.15 current smoker (last 30 days) | |
| Lovato 2007 | 22,318 (Canada) | 15 ‐ 19 years | No differences in smoking prevalence | |
| Pentz 1989 | 4807 (USA) | 12 ‐ 13 years | 5.29% (high cessation emphasis) vs 4.72% (low cessation emphasis) weekly smokers | |
| Piontek 2008b | 2818 (Germany) | 10 ‐ 21 years | ß coefficient 0.32 current smoker when cessation programme is offered | |
| Total: 36,067 | ||||
| Favours controls (1) | Lovato 2010a | 27,892 Canada | 10 ‐ 14 years | RR 2.23* current smoker (last 30 days) |
| Total: 27,892 | ||||
| STP plus prevention components vs STP alone | ||||
| No difference (6) | Darling 2006 | 2658 (New Zealand) | 15 mean age | RR 1.17 daily smoker |
| Lovato 2007 | 22,318 (Canada) | 15 ‐ 19 years | No differences in smoking prevalence | |
| Murnaghan 2007 | 3965 (Canada) | 17.6 mean age | OR 0.83 occasional smoker | |
| Murnaghan 2008 | 4709 (Canada) | 15 ‐ 16 years | OR 1.54 occasional smoker | |
| Pentz 1989 | 4807 (USA) | 12 ‐ 13 years | 4.31% (high prevention emphasis) vs 5.77% (low prevention emphasis) weekly smokers | |
| Sabiston 2009 | 24,213 (Canada) | 16 mean age | OR 1.10 current smoker (last 30 days) | |
| total: 62,670 |
OR: odds ratio RR: risk ratio
Discussion
Summary of main results
The results of this review are limited by the number of studies identified and the low methodological quality of the only one we included, Chen 2014, which showed no significant differences for students' smoking behaviours between schools with and without a STP. Furthermore, the study was judged as having high risk of bias. For this reason at present there is insufficient evidence that STPs are effective for the reduction of smoking initiation among young people. Through a systematic search of observational studies, we also identified some studies exploring different aspects of STP. Specific characteristics like enforcement, extended outdoor bans, strict surveillance measures, assistance to quit smoking, formal adoption of a STP and inclusion of prevention or education activities were not found to be associated with a decreased likelihood of smoking. These results questioned the effectiveness of STPs, but, given the very low quality of the evidence, in the absence of large and rigorous intervention studies, they should be considered in order to orient future research on this topic. The review didn't include studies that addressed whether STPs are able to reduce the start of smoking in adolescents or reduce the number of cigarettes among smokers.
Quality of the evidence
It is important to consider that the main conclusion of this review is based only on one randomised controlled trial (RCT) at high risk of bias. This is because the included study did not describe the randomisation method for the schools and did not provide information on allocation concealment, which may introduce significant selection bias. On the other hand the number of dropouts and participants lost to follow‐up were very low. Given the characteristics of the assessed intervention, it is important to note that it was not feasible to blind the participants or the school personnel. The investigators measuring the outcomes could have been blinded, but this was not reported in the included study. Insufficient details were provided on variables used In the statistical analysis for the adjustment for possible confounders.
We have also analysed some observational studies, which in turn have important limitations, apart from their study design. One important issue is the heterogeneity of exposure definition. There is large variability in policy formats, and these can include several different characteristics, which make comparisons difficult. Only a few studies are based on policy definition in written documents. Policy information obtained by interviewing school principals, school administrators or teachers might overstate the extent of the STP, and frequently it is not possible to differentiate the contribution of the STP from that of other school interventions. Descriptive terms, like 'enforcement' or 'comprehensiveness', were used in different and incompatible ways, with specific policy characteristics being differently defined. This was true of smoking prevention programmes, availability of cessation support, and the sanctions for violations. The outcome variables were heterogeneous, and the age range between studies was variable. Since age is a major determinant of the prevalence of tobacco use, with a doubling of the initiation rates between early and middle adolescence (DiFranza 2007), discrepancies between studies should always be interpreted with respect to age distribution. With regard to analysis methods, some studies did not mention any adjustment for potential confounders (Clarke 1994; Darling 2006; Sinha 2004b; Wiium 2011b) and in general there is large variability in the factors considered for adjustment.
Agreements and disagreements with other studies or reviews
Five RCTs excluded from this review (Elder 1996; De Vries 2006; Hamilton 2005; Schofield 2003; Wen 2010), as it was not possible to differentiate the effect of smoking policy from other interventions, were included in another Cochrane review (Thomas 2013). A recent Cochrane review (Langford 2014) aimed to assess the impact of the Health Promoting School framework on several health behaviours; four (De Vries 2006; Hamilton 2005; Schofield 2003; Wen 2010) of 14 studies included for evaluating the effect on smoking behaviour were also considered in this review, but excluded for the reason mentioned above. The conclusions of the present work largely agree with those produced in a previous systematic review (Galanti 2014). Other reviews on STP have previously been published. A review conducted with the scope of identifying which school characteristics are responsible for the variation in smoking prevalence found weak associations between some aspects of STPs and smoking (Aveyard 2004). A narrative review on the impact of school drug policies on youth substance use concluded that more comprehensive and strictly enforced policies are associated with less smoking, but may also displace the behaviour from school grounds to off‐school premises (Evans‐Whipp 2004). A non‐systematic review of school contextual effects on students' behavioural outcomes showed how in schools without STPs, smoking was more prevalent among pupils (Sellström 2006), but no detailed description of the characteristics of the policies was provided.
Authors' conclusions
Implications for practice.
Despite a comprehensive search of the literature evaluating the effectiveness of school policies for preventing smoking among young people, we did not find any evidence of an effect. This is mainly explained by the absence of rigorous studies. Whlie this finding suggests that STP is an ineffective stand‐alone intervention, we believe that the theoretical basis of this intervention (Wilson 2012) should be tested under the control of well designed studies.
Implications for research.
Large, possibly multi‐centric studies, employing an experimental or a quasi‐experimental design, are needed to assess the effectiveness of this intervention.
Future research in this area must be rigorously designed and evaluated. Design issues of particular importance include the following:
A cluster‐randomised study design, with a sufficient number of clusters (schools) in each comparison group. When new national smoking bans outside schools are enforced, researchers could take the chance to evaluate their impact by the adoption of study designs such as interrupted time series.
The intervention should be accurately and objectively described, in particular the rules of the policy, the persons involved, the penalties for the infringement of rules, and the process of enforcement.
Outcome variables should be standard and validated where possible, and should include process as well as behavioural change data.
Information relating to context (e.g. social, political and cultural factors) should also be collected and factored into the analysis.
Several STP components can play an essential role in contributing to policy effectiveness; the most important ones suggested by this review are:
degree of formality: form of statements of the policy (whether written or other);
participants to which the policy applies (students, staff, visitors/guests);
extent of the ban (in all indoor areas or on external school premises);
level of enforcement including: rules for surveillance and for referral of smoking ban infringements; definition of the person responsible for policy evaluation and review; agenda for periodic evaluation and policy review;
sanctions for transgression;
assistance with smoking cessation;
combination with prevention and education activities.
What's new
| Date | Event | Description |
|---|---|---|
| 9 February 2016 | Amended | External source of support added |
Acknowledgements
The authors would like to thank the editorial staff of the Cochrane Tobacco Addiction Review Group for running the search strategy and for their advice and support during the review process.
Appendices
Appendix 1. MEDLINE search strategy
1 RANDOMIZED‐CONTROLLED‐TRIAL.pt.
2 CONTROLLED‐CLINICAL‐TRIAL.pt.
3 CLINICAL‐TRIAL.pt.
4 Meta analysis.pt.
5 exp Clinical Trial/
6 Random‐Allocation/
7 randomized‐controlled trials/
8 double‐blind‐method/
9 single‐blind‐method/
10 placebos/
11 Research‐Design/
12 ((clin$ adj5 trial$) or placebo$ or random$).ti,ab.
13 ((singl$ or doubl$ or trebl$ or tripl$) adj5 (blind$ or mask$)).ti,ab.
14 (volunteer$ or prospectiv$).ti,ab.
15 exp Follow‐Up‐Studies/
16 exp Retrospective‐Studies/
17 exp Prospective‐Studies/
18 exp Evaluation‐Studies/ or Program‐Evaluation.mp.
19 exp Cross‐Sectional‐Studies/
20 exp Behavior‐therapy/
21 exp Health‐Promotion/
22 exp Community‐Health‐Services/
23 exp Health‐Education/
24 exp Health‐Behavior/
25 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24
26 smoking cessation.mp. or exp Smoking Cessation/
27 "Tobacco‐Use‐Cessation"/
28 "Tobacco‐Use‐Disorder"/
29 Tobacco‐Smokeless/
30 exp Tobacco‐Smoke‐Pollution/
31 exp Tobacco‐/
32 exp Nicotine‐/ (19782)
33 ((quit$ or stop$ or ceas$ or giv$) adj5 smoking).ti,ab.
34 exp Smoking/pc, th [Prevention & Control, Therapy]
35 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 [A category smoking terms]
36 exp Smoking/ not 35 [B category smoking terms]
37 1 or 2 or 3 [Likely CT design terms; RCTs, CCTs, Clinical trials]
38 35 and 25 [A category smoking+all design terms]
39 35 and 37 [A category smoking terms+likely CT design terms]
40 (animals not humans).sh. [used with 'not' to exclude animal studies for each subset]
41 ((26 or 27 or 28 or 29) and REVIEW.pt.) not 38 [Set 4: Core smoking related reviews only]
42 36 and 25 [B category smoking+all design terms]
43 (42 and 37) not 40 [Set 3: B smoking terms, likely CT design terms, human only]
44 38 not 39 not 40 [Set 2: A smoking terms, not core CT terms, human only]
45 (35 and 37) not 40 [Set 1: A smoking terms, likely CT design terms, human only]
46 (36 and 25) not 40 not 43 [Set 4: B smoking terms, not core CT terms]
47 (polic* or ban* or restriction* or rule* or environment*).mp.
48 school*.mp.
49 47 and 48 [Topic related terms]
50 45 and 49 [Topic + A smoking terms & core CT terms SET 1]
51 44 and 49 [Topic + A smoking terms & wide design terms SET 2]
52 43 and 49 [Topic + B smoking terms & core CT termsSET 3]
53 46 and 49 [Topic + B smoking terms & wide design terms SET 4]
Lines 1 to 24 identify controlled trials and other types of programme evaluations, as used to identify reports of studies for the Tobacco Addiction Group Specialised Register. Lines 26 to 34 identify reports related to smoking and tobacco control. Lines 47 and 48 identify reports relevant to the topic of this review. Sets 1 to 4 will be screened for the review, Sets 1 and 2 are expected to be the most likely to contain relevant reports, and Set 4 to be unlikely to identify any.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Chen 2014.
| Methods | Cluster‐RCT at level of school | |
| Participants | Country: China (Linzhi, Tibet and Guangzhou, Guangdong Province) School type: Middle Target group: Grades 6 and 7 (13 ‐ 15 yrs) Number of intervention schools: 1 in Linzhi and 1 in Guangzhou Number of control schools: 1 in Linzhi and 1 in Guangzhou Number of participants: 941 in intervention schools and 866 in control schools | |
| Interventions |
Start date: 2008
Duration: 1 year
Comparators: No intervention Health Policies in School: A tobacco control committee headed by the principal was established; regulations on smoking were made at the beginning of the study Health Environment in school: No‐smoking signs were placed in the school yards. Peer education was conducted to help smokers to quit smoking. Teachers were required not to smoke in front of students. Personal Health Skills: Brochures of health hazards of smoking and .blackboard newsletter, posters and publicity pictures were disseminated. Smoking‐related health education lectures were given. Students participated in smoking cessation‐related activities including essay competitions, signing a non‐smoking pledge, Additional components: No‐Tobacco‐Day theme activities, self‐producing newspaper competition and logo design contests. |
|
| Outcomes |
Primary outcomes: Ever smoking, daily smoking, weekly smoking, current smoking. Secondary outcomes: Smoking‐related knowledge and smoking‐related attitudes |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided on random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No details provided on allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unlikely that participants could have been adequately blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes were self‐reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates were very low; correspondence rate from matched questionnaires between the two surveys was 99.6% in Linzhi and 99.4% in Guangzhou |
| Selective reporting (reporting bias) | High risk | No protocol available |
| Other bias | High risk | selection bias: unclear sample procedure and no citation of stratified sampling |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adams 2009 | Cross‐sectional study; considered for hypothesis generation |
| Aldinger 2008 | Inappropriate outcomes (no association with smoking behaviour) |
| Andersen 2012 | RCT; not possible to isolate the predictor |
| Ariza 2008 | Not possible to isolate the predictor |
| Baillie 2008 | Inappropriate outcomes (no association with smoking behaviour) |
| Barnett 2007 | Cross‐sectional study; considered for hypothesis generation |
| Boris 2009 | Cross‐sectional study; considered for hypothesis generation |
| Clarke 1994 | Cross‐sectional study; considered for hypothesis generation |
| Darling 2003 | Inappropriate outcomes (no association with smoking behaviour) |
| Darling 2006 | Cross‐sectional study; considered for hypothesis generation |
| De Vries 2003 | RCT; not possible to isolate the predictor (see De Vries 2006) |
| De Vries 2006 | RCT; not possible to isolate the predictor |
| Elder 1996 | RCT; not possible to isolate the predictor |
| Evans‐Whipp 2007 | Inappropriate outcome (students' smoking based on observation) |
| Evans‐Whipp 2010 | Cross‐sectional study; considered for hypothesis generation |
| Galán 2012 | Cross‐sectional study; considered for hypothesis generation |
| Garcìa‐Vàzquez 2009 | Not possible to isolate the predictor |
| Gorini 2014 | RCT; not possible to isolate the predictor |
| Griesbach 2002 | Inappropriate outcome (pupils' perception of teacher and student smoking) |
| Hamilton 2003 | Cross‐sectional study; considered for hypothesis generation |
| Hamilton 2005 | RCT; not possible to isolate the predictor |
| Huang 2010 | Cross‐sectional study; considered for hypothesis generation |
| Johnson 2009 | Not possible to isolate the predictor |
| Kumar 2005 | Cross‐sectional study; considered for hypothesis generation |
| Labiris 2005 | Not possible to isolate the predictor |
| Lipperman‐Kreda 2009a | Inappropriate predictor's measure (policy reported by students) |
| Lipperman‐Kreda 2009b | Inappropriate predictor's measure (policy reported by students) |
| Lovato 2007 | Cross‐sectional study; considered for hypothesis generation |
| Lovato 2010a | Cross‐sectional study; considered for hypothesis generation |
| Lovato 2010b | Cross‐sectional study; considered for hypothesis generation |
| Maes 2003 | Inappropriate predictor |
| Moon 1999 | Not possible to isolate the predictor |
| Moore 2001 | Cross‐sectional study; considered for hypothesis generation |
| Murnaghan 2007 | Repeated cross‐sectional study. Considered for hypothesis generation |
| Murnaghan 2008 | Repeated cross‐sectional study. Considered for hypothesis generation |
| Murnaghan 2009 | Not possible to isolate the predictor |
| Novak 2001 | Inappropriate predictor |
| O'Brien 2010 | Inappropriate predictor |
| Paek 2013 | Cross‐sectional study; considered for hypothesis generation |
| Pentz 1989 | Cross‐sectional study; considered for hypothesis generation |
| Pinilla 2002 | Inappropriate predictor's measure (policy reported by students) |
| Piontek 2008a | Inappropriate predictor's measure (policy reported by students) |
| Piontek 2008b | Cross‐sectional study; considered for hypothesis generation |
| Poulin 2007 | Inappropriate predictor's measure (policy reported by students) |
| Reitsma 2004 | Inappropriate predictor's measure (policy reported by students) |
| Rosendhal 2002 | Cohort study. Considered for hypothesis generation |
| Roski 1997 | Inappropriate outcomes (no association with smoking behaviour) |
| Sabiston 2009 | Cross‐sectional study; considered for hypothesis generation |
| Schofield 2003 | RCT; not possible to isolate the predictor |
| Sinha 2004a | Inappropriate predictor |
| Sinha 2004b | Cross‐sectional study; considered for hypothesis generation |
| Trinidad 2005 | Inappropriate outcomes |
| Wakefield 2000 | Inappropriate predictor's measure (policy reported by students) |
| Watts 2010 | Inappropriate predictor's measure (policy reported by students) |
| Wen 2010 | RCT; not possible to isolate the predictor |
| Wiium 2011a | Cross‐sectional study; considered for hypothesis generation |
| Wiium 2011b | Cross‐sectional study; considered for hypothesis generation |
| Wold 2004 | Inappropriate outcomes |
| Østhus 2007 | Inappropriate predictor's measure (policy reported by students) |
| Øverland 2010 | Inappropriate predictor's measure (policy reported by students) |
Differences between protocol and review
Background section has been summarised from the original protocol. List of eligible study designs now uses EPOC recommended terminology.
Contributions of authors
AC was involved in coordinating the review, developing the protocol, extracting data, conducting the analysis and co‐wrote and edited the review.
MRG was involved in developing the protocol and co‐wrote the review.
LG, DB and SB were involved in conducting the analysis and co‐wrote the review.
FF was involved in coordinating the review, developing the protocol, extracting data and co‐wrote and edited the review.
Sources of support
Internal sources
No sources of support supplied
External sources
-
European Community’s Seventh Framework Programme (FP7/2007‐2013), under Grant Agreement n. 266813‐Addictions and Lifestyle in Contemporary Europe‐Reframing Addictions Project (ALICE RAP), Other.
Participant organizations in ALICE RAP can be seen at http://www.alicerap.eu/about‐alice‐rap/partners.html. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Declarations of interest
AC, MRG, LG, DB, SB and FF have no potential conflict of interest.
Edited (no change to conclusions)
References
References to studies included in this review
Chen 2014 {published data only}
- Chen L, Chen Y, Hao Y, Gu J, Guo Y, Ling W. Effectiveness of school‐based smoking intervention in middle school students of Linzhi Tibetan and Guangzhou Han ethnicity in China. Addictive Behaviors 2014;39(1):189‐95. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Adams 2009 {published data only}
- Adams ML, Jason LA, Pokorny S, Hunt Y. The relationship between school policies and youth tobacco use. Journal of School Health 2009;79(1):17‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aldinger 2008 {published data only}
- Aldinger C, Zhang X, Liu L, Pan X, Yu S, Jones J, et al. Changes in attitudes, knowledge and behavior associated with implementing a comprehensive school health program in a province of China. Health Education Research 2008;Vol.23(6):1049–67. [DOI] [PubMed] [Google Scholar]
Andersen 2012 {published data only}
- Andersen A, Krolner RS, Nielsen L, Thygesen LC, Due P. Prevention of smoking among adolescents: First year results from the cluster randomised X:IT trial. European Journal of Epidemiology. Conference: IEA‐EEF European Congress of Epidemiology 2012: Epidemiology for a Fair and Healthy Society; Porto, Portugal. September. 2012.
Ariza 2008 {published data only}
- Ariza C, Nebot M, Tomás Z, Giménez E, Valmayor S, Tarilonte V, et al. Longitudinal effects of the European smoking prevention framework approach (ESFA) project in Spanish adolescents. European Journal of Public Health 2008;18(5):491–7. [DOI] [PubMed] [Google Scholar]
Baillie 2008 {published data only}
- Baillie LE, Lovato CY, Taylor E, Rutherford MB, Smith M. The pit and the pendulum: the impact on teen smokers of including a designated smoking area in school tobacco control policy. Health Education Research 2008;23(6):1008–15. [DOI] [PubMed] [Google Scholar]
Barnett 2007 {published data only}
- Barnett TA, Gauvin L, Lambert M, O’Loughlin J, Paradis G, McGrath JJ. The influence of school smoking policies on student tobacco use. Archives of Pediatrics & Adolescent Medicine 2007;161(9):842‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boris 2009 {published data only}
- Boris NW, Johnson CC, Huang S, Myers L, Andrew K, Webber LS. Targeting school tobacco policy: lessons from the Acadiana Coalition of Teens Against Tobacco (ACTT). Health Promotion Practice 2009;10(4):549‐56. [DOI] [PubMed] [Google Scholar]
Clarke 1994 {published data only}
- Clarke V, White V, Hill D, Borland R. School structural and policy variables associated with student smoking. Tobacco Control 1994;3(4):339‐46. [Google Scholar]
Darling 2003 {published data only}
- Darling H, Reeder A. Smoke‐free schools? Results of a secondary school smoking policies survey 2002. New Zealand Medical Journal 2003;116(1180):U560. [PubMed] [Google Scholar]
Darling 2006 {published data only}
- Darling H, Reeder AI, Williams S, McGee R. Is there a relation between school smoking policies and youth cigarette smoking knowledge and behaviours?. Health Education Research 2006;21(1):108–15. [DOI] [PubMed] [Google Scholar]
De Vries 2003 {published data only}
- Vries H, Mudde A, Kremers S, Wetzels J, Uiters E, Ariza C, et al. The European Smoking Prevention Framework Approach (ESFA): short‐term effects. Health Education Research 2003;18(6):649‐63. [DOI] [PubMed] [Google Scholar]
De Vries 2006 {published data only}
- Vries H, Dijk F, Wetzels J, Mudde A, Kremers S, Ariza C, et al. The European Smoking prevention Framework Approach (ESFA): effects after 24 and 30 months. Health Education Research 2006;21(1):116‐32. [DOI] [PubMed] [Google Scholar]
Elder 1996 {published data only}
- Elder JP, Perry CL, Stone EJ, Johnson CC, Yang M, Edmundson EW, et al. Tobacco use measurement, prediction, and intervention in elementary schools in four states: The CATCH Study. Preventive Medicine 1996;25(4):486‐94. [DOI] [PubMed] [Google Scholar]
Evans‐Whipp 2007 {published data only}
- Evans‐Whipp TJ, Bond L, Toumbourou JW, Catalano RF. School, parent, and student perspectives of school drug policies. Journal of School Health 2007;77(3):138‐46. [DOI] [PubMed] [Google Scholar]
Evans‐Whipp 2010 {published data only}
- Evans‐Whipp TJ, Bond L, Ukoumunne OC, Toumbourou JW, Catalano RF. The impact of school tobacco policies on student smoking in Washington State, United States and Victoria, Australia. International Journal of Environmental Research and Public Health 2010;7(3):698‐710. [DOI] [PMC free article] [PubMed] [Google Scholar]
Galán 2012 {published data only}
- Galán I, Díez‐Gañán L, Gandarillas A, Mata N, Cantero JL, Durbán M. Effect of a smoking ban and school‐based prevention and control policies on adolescent smoking in Spain: a multilevel analysis. Prevention Science 2012;13(6):574–83. [DOI] [PubMed] [Google Scholar]
Garcìa‐Vàzquez 2009 {published data only}
- García‐Vázquez J, Arbesú Fernández E, Rodríguez Vigil L, Alvarez Iglesias G, Fernández Rodríguez S, Mosquera Tenreiro C. Evaluation of a school based intervention to promote smokefree areas [Evaluaciòn de una intervenciòn de promociòn de espacios sin humo en el àmbito educativo]. Gaceta Sanitaria 2009;23(1):23–8. [DOI] [PubMed] [Google Scholar]
Gorini 2014 {published data only}
- Gorini G, Carreras G, Bosi S, Tamelli M, Monti C, Storani S, et al. Effectiveness of a school‐based multi‐component smoking prevention intervention: the LdP cluster randomized controlled trial. Preventive Medicine 2014;61:6‐13. [DOI] [PubMed] [Google Scholar]
Griesbach 2002 {published data only}
- Griesbach D, Inchley J, Currie C. More than words? The status and impact of smoking policies in Scottish schools. Health Promotion International 2002;17(1):31‐41. [DOI] [PubMed] [Google Scholar]
Hamilton 2003 {published data only}
- Hamilton G, Cross D, Lower T, Resnicow K, Williams P. School policy: What helps to reduce teenage smoking?. Nicotine & Tobacco Research 2003;5(4):507–13. [DOI] [PubMed] [Google Scholar]
Hamilton 2005 {published data only}
- Hamilton G, Cross D, Resnicow K, Hall M. A school‐based harm minimization smoking intervention trial: outcome results.. Addiction 2005;100(5):689‐700. [DOI] [PubMed] [Google Scholar]
Huang 2010 {published data only}
- Huang HL, Chen FL, Hsu CC, Yen YY, Chen T, Huang CM, et al. A multilevel‐based study of school policy for tobacco control in relation to cigarette smoking among children in elementary schools: gender differences. Health Educ Res 2010;25(3):451‐63. [DOI] [PubMed] [Google Scholar]
Johnson 2009 {published data only}
- Johnson CC, Myers L, Webber LS, Boris NW, He H, Brewer D. A school‐based environmental intervention to reduce smoking among high school students: the Acadiana Coalition of Teens against Tobacco (ACTT). International Journal of Environmental Research and Public Health 2009;6(4):1298‐316. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kumar 2005 {published data only}
- Kumar R, O'Malley PM, Johnston LD. School tobacco control policies related to students' smoking and attitudes toward smoking: national survey results, 1999‐2000. Health Education & Behavior 2005;32(6):780‐94. [DOI] [PubMed] [Google Scholar]
Labiris 2005 {published data only}
- Labiris G, Voutsinas A, Niakas D. Preliminary evaluation of the school‐smoking‐prevention policy in Greece. European Journal of Public Health 2005;15(3):329‐30. [DOI] [PubMed] [Google Scholar]
Lipperman‐Kreda 2009a {published data only}
- Lipperman‐Kreda S, Paschall MJ, Grube JW. Perceived enforcement of school tobacco policy and adolescents' cigarette smoking. Preventive Medicine 2009;48(6):562‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lipperman‐Kreda 2009b {published data only}
- Lipperman‐Kreda S, Grube JW. Students' perception of community disapproval, perceived enforcement of school antismoking policies, personal beliefs, and their cigarette smoking behaviors: results from a structural equation modelling analysis. Nicotine & Tobacco Research 2009;11(5):531‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lovato 2007 {published data only}
- Lovato CY, Sabiston CM, Hadd V, Nykiforuk CI, Campbell HS. The impact of school smoking policies and student perceptions of enforcement on school smoking prevalence and location of smoking. Health Education Research 2007;22(6):782‐93. [DOI] [PubMed] [Google Scholar]
Lovato 2010a {published data only}
- Lovato CY, Pullman AW, Halpin P, Zeisser C, Nykiforuk CI, Best F, et al. The influence of school policies on smoking prevalence among students in grades 5‐9, Canada, 2004‐2005. Preventing Chronic Disease 2010;7(6):A129. [PMC free article] [PubMed] [Google Scholar]
Lovato 2010b {published data only}
- Lovato CY, Zeisser C, Campbell HS, Watts AW, Halpin P, Thompson M, et al. Adolescent smoking: effect of school and community characteristics. American Journal of Preventive Medicine 2010;39(6):507‐14. [DOI] [PubMed] [Google Scholar]
Maes 2003 {published data only}
- Maes L, Lievens J. Can the school make a difference? Amultilevel analysis of adolescent risk and health behaviour. Social Science & Medicine 2003;56(3):517‐29. [DOI] [PubMed] [Google Scholar]
Moon 1999 {published data only}
- Moon AM, Mullee MA, Rogers L, Thompson RL, Speller V, Roderick P. Helping schools to become health‐promoting environments—an evaluation of the Wessex Healthy Schools Award. Health Promotion International 1999;14(2):111‐22. [Google Scholar]
Moore 2001 {published data only}
- Moore L, Roberts C, Tudor‐Smith C. School smoking policies and smoking prevalence among adolescents: multilevel analysis of cross‐sectional data from Wales. Tobacco Control 2001;10(2):117‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murnaghan 2007 {published data only}
- Murnaghan DA, Sihvonen M, Leatherdale ST, Kekki P. The relationship between school‐based smoking policies and prevention programs on smoking behavior among grade 12 students in Prince Edward Island: a multilevel analysis. Preventive Medicine 2007;44(4):317‐22. [DOI] [PubMed] [Google Scholar]
Murnaghan 2008 {published data only}
- Murnaghan DA, Leatherdale ST, Sihvonen M, Kekki P. A multilevel analysis examining the association between school‐based smoking policies, prevention programs and youth smoking behavior: evaluating a provincial tobacco control strategy. Health Education Research 2008;23(6):1016‐28. [DOI] [PubMed] [Google Scholar]
Murnaghan 2009 {published data only}
- Murnaghan DA, Leatherdale ST, Sihvonen M, Kekki P. School‐based tobacco‐control programming and student smoking behaviour.. Chronic Dis Can 2009;29(4):169‐77. [PubMed] [Google Scholar]
Novak 2001 {published data only}
- Novak SP, Clayton RR. The influence of school environment and self‐regulation on transitions between stages of cigarette smoking: a multilevel analysis. Health Psychology 2001;20(3):196‐207. [PubMed] [Google Scholar]
O'Brien 2010 {published data only}
- O'Brien LM, Polacsek M, Macdonald PB, Ellis J, Berry S, Martin M. Impact of a school health coordinator intervention on health‐related school policies and student behavior. Journal of School Health 2010;80(4):176‐85. [DOI] [PubMed] [Google Scholar]
Paek 2013 {published data only}
- Paek HJ, Hove T, Oh HJ. Multilevel analysis of the impact of school‐level tobacco policies on adolescent smoking: the case of Michigan. Journal of School Health 2013;83(10):679‐89. [DOI] [PubMed] [Google Scholar]
Pentz 1989 {published data only}
- Pentz MA, Brannon BR, Charlin VL, Barrett EJ, MacKinnon DP, Flay BR. The power of policy: the relationship of smoking policy to adolescent smoking. American Journal of Public Health 1989;79(7):857‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pinilla 2002 {published data only}
- Pinilla J, González B, Barber P, Santana Y. Smoking in young adolescents: an approach with multilevel discrete choice models. Journal of Epidemiology and Community Health 2002;56(3):227‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Piontek 2008a {published data only}
- Piontek D, Buehler A, Rudolph U, Metz K, Kroeger C, Gradl S, et al. Social contexts in adolescent smoking: does school policy matter?. Health Education Research 2008;23(6):1029‐38. [DOI] [PubMed] [Google Scholar]
Piontek 2008b {published data only}
- Piontek D, Buehler A, Donath C, Floeter S, Rudolph U, Metz K, Gradl S, Kroeger C. School Context Variables and Students’Smoking. Eur Addict Res 2008;14(1):53‐60. [DOI] [PubMed] [Google Scholar]
Poulin 2007 {published data only}
- Poulin CC. School smoking bans: do they help/do they harm?. Drug and Alcohol Review 2007;26(6):615‐24. [DOI] [PubMed] [Google Scholar]
Reitsma 2004 {published data only}
- Reitsma AH, Manske S. Smoking in Ontario schools: does policy make a difference?. Canadian Journal of Public Health 2004;95(3):214‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosendhal 2002 {published data only}
- Rosendahl KI, Galanti MR, Gilljam H, Bremberg S, Ahlbom A. School and class environments are differently linked to future smoking among preadolescents. Preventive Medicine 2002;34(6):649–54. [DOI] [PubMed] [Google Scholar]
Roski 1997 {published data only}
- Roski J, Perry CL, McGovern PG, Williams CL, Farbakhsh K, Veblen‐Mortenson S. School and community influences on adolescent alcohol and drug use. Health Education Research 1997;12(2):255‐66. [DOI] [PubMed] [Google Scholar]
Sabiston 2009 {published data only}
- Sabiston CM, Lovato CY, Ahmed R, Pullman AW, Hadd V, Campbell HS, et al. School smoking policy characteristics and individual perceptions of the school tobacco context: are they linked to students' smoking status?. Journal of Youth and Adolescence 2009;38(10):1374‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schofield 2003 {published data only}
- Schofield MJ, Lynagh M, Mishra G. Evaluation of a Health Promoting Schools program to reduce smoking in Australian secondary schools.. Health Education Research 2003;18(6):678‐92. [DOI] [PubMed] [Google Scholar]
Sinha 2004a {published data only}
- Sinha DN, Gupta PC, Warren CW, Asma S. Effect of school policy on tobacco use by school personnel in Bihar, India. Journal of School Health 2004;74(1):3‐5. [DOI] [PubMed] [Google Scholar]
Sinha 2004b {published data only}
- Sinha DN, Gupta PC, Warren CW, Asma S. School policy and tobacco use by students in Bihar, India. Indian Journal of Public Health 2004;48(3):118‐22. [PubMed] [Google Scholar]
Trinidad 2005 {published data only}
- Trinidad DR, Gilpin EA, Pierce JP. Compliance and support for smoke‐free school policies. Health Education Research 2005;20(4):466‐75. [DOI] [PubMed] [Google Scholar]
Wakefield 2000 {published data only}
- Wakefield MA, Chaloupka FJ, Kaufman NJ, Orleans CT, Barker DC, Ruel EE. Effect of restrictions on smoking at home, at school, and in public places on teenage smoking: cross sectional study. BMJ 2000;321(7257):333‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Watts 2010 {published data only}
- Watts AW, Lovato CY, Card A, Manske SR. Do students' perceptions of school smoking policies influence where students smoke?: Canada's Youth Smoking Survey. Cancer Causes & Control 2010;21(12):2085‐92. [DOI] [PubMed] [Google Scholar]
Wen 2010 {published data only}
- Wen X, Chen W, Gans KM, Colby SM, Lu C, Liang C, et al. Two‐year effects of a school‐based prevention programme on adolescent cigarette smoking in Guangzhou, China: a cluster randomized trial. International Journal of Epidemiology 2010;39(3):860‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wiium 2011a {published data only}
- Wiium N, Burgess S, Moore L. Brief report: multilevel analysis of school smoking policy and pupil smoking behaviour in Wales. Journal of Adolescence 2011;34(2):385‐9. [DOI] [PubMed] [Google Scholar]
Wiium 2011b {published data only}
- Wiium N, Wold B. Actions taken by schools when tobacco policies are violated: associations with adolescent smoking prevalence. Scandinavian Journal of Psychology 2011;25(2):494‐501. [DOI] [PubMed] [Google Scholar]
Wold 2004 {published data only}
- Wold B, Torsheim T, Currie C, Roberts C. National and school policies on restrictions of teacher smoking: a multilevel analysis of student exposure to teacher smoking in seven European countries. Health Education Research 2004;19(3):217‐26. [DOI] [PubMed] [Google Scholar]
Østhus 2007 {published data only}
- Østhus S, Pape H, Lund KE. Smoking restrictions and smoking prevalence in high schools [Røykerestriksjonerog røykevaner i videregående skole]. Tidsskr Nor Laegeforen 2007;127(9):1192‐4. [PubMed] [Google Scholar]
Øverland 2010 {published data only}
- Øverland S, Aarø LE, Lindbak RL. Associations between schools' tobacco restrictions and adolescents' use of tobacco. Health Education Research 2010;25(5):748‐56. [DOI] [PubMed] [Google Scholar]
Additional references
Alesci 2003
- Alesci NL, Forster JL, Blaine T. Smoking visibility, perceived acceptability, and frequency in various locations among youth and adults. Preventive Medicine 2003;36(3):272–81. [DOI] [PubMed] [Google Scholar]
Aveyard 2004
- Aveyard P, Markham WA, Cheng KK. A methodological and substantive review of the evidence that schools cause pupils to smoke. Social Science & Medicine 2004;58(11):2253‐65. [DOI] [PubMed] [Google Scholar]
Bandura 1986
- Bandura A. Social Foundations of Thought and Action. New York: Prentice‐Hall, 1986. [Google Scholar]
Bowen 1995
- Bowen DJ, Kinne S, Orlandi M. School policy in COMMIT: a promising strategy to reduce smoking by youth. Journal of School Health 1995;65(4):140‐4. [DOI] [PubMed] [Google Scholar]
Chen 1998
- Chen J, Millar WJ. Age of smoking initiation: implications for quitting. Health Reports 1998;9(4):39‐46. [PubMed] [Google Scholar]
DiFranza 2007
- DiFranza JR, Savageau JA, Fletcher K, O'Loughlin J, Pbert L, Ockene JK, et al. Symptoms of tobacco dependence after brief intermittent use: the Development and Assessment of Nicotine Dependence in Youth‐2 study. Archives of Pediatrics & Adolescent Medicine 2007;161(7):704‐10. [DOI] [PubMed] [Google Scholar]
Eccles 1999
- Eccles JS, Roeser R. School and community influences on human development. In: Bornstein M, Lamb M editor(s). Developmental Psychology: An Advanced Textbook. 4th Edition. Mahwah, NJ: Lawrence Erlbaum, 1999:503‐4. [Google Scholar]
Evans‐Whipp 2004
- Evans‐Whipp TJ, Beyers JM, Lloyd S, Lafazia AN, Toumbourou JW, Arthur MW, et al. A review of school drug policies and their impact on youth substance use. Health Promotion International 2004;19(2):227‐34. [DOI] [PubMed] [Google Scholar]
Everett 1999
- Everett SA, Warren CW, Sharp D, Kann L, Husten CG, Crossett LS. Initiation of cigarette smoking and subsequent smoking behaviour among U.S. high school students. Preventive Medicine 1999;29(5):327‐33. [DOI] [PubMed] [Google Scholar]
Faggiano 2010
- Faggiano F, Vigna‐Taglianti F, Burkhart G, Bohrn K, Cuomo L, Gregori D, et al. The effectiveness of a school‐based substance abuse prevention program: 18‐month follow‐up of the EU‐Dap cluster randomized controlled trial. Drug and Alcohol Dependendence 2010;108(1‐2):56‐64. [DOI] [PubMed] [Google Scholar]
Fletcher 2008
- Fletcher A, Bonell C, Hargreaves J. School effects on young people's drug use: a systematic review of intervention and observational studies. Journal of Adolescent Health 2008;42(3):209‐20. [DOI] [PubMed] [Google Scholar]
Friend 2011
- Friend KB, Lipperman‐Kreda S, Grube JW. The impact of local U.S. tobacco policies on youth tobacco use: A critical review. Open Journal of Preventive Medicine 2011;1(2):34‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Galaif 1996
- Galaif ER, Sussman S, Bundek N. The relations of school staff smokers’ attitudes about modelling smoking behaviour in students and their receptivity to no‐smoking policy. Journal of Drug Education 1996;26(4):313‐22. [DOI] [PubMed] [Google Scholar]
Galanti 2014
- Galanti MR, Coppo A, Jonsson E, Bremberg S, Faggiano F. Anti‐tobacco policy in schools: upcoming preventive strategy or prevention myth? A review of 31 studies. Tobacco Control 2014;23(4):295‐301. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S. Cochrane Handbook for SystematicReviews of Interventions Version 5.1.0. The Cochrane Collaboration 2011. [Google Scholar]
Iannotti 1992
- Iannotti RJ, Bush PJ. Perceived vs. actual friends’ use of alcohol, cigarettes, marijuana, and cocaine: which has the most influence?. Journal of Youth and Adolescence 1992;21(3):375–89. [DOI] [PubMed] [Google Scholar]
Langford 2014
- Langford R, Bonell CP, Jones HE, Pouliou T, Murphy SM, Waters E, et al. The WHO Health Promoting School framework for improving the health and well‐being of students and their academic achievement. Cochrane Database of Systematic Reviews 2014, Issue 4. [DOI: 10.1002/14651858.CD008958.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lloyd 1998
- Lloyd B, Lucas K, Holland J, McGrellis S, Arnold S. Smoking in Adolescence: Images and Identities. New York: Routledge, 1998. [Google Scholar]
MacBride 2005
- MacBride M. School Smoking Policy. Discussion Paper Prepared for Tobacco Control Program. Victoria, Canada: BC Ministry of Health, 2005. [Google Scholar]
Nakamura 2004
- Nakamura M, Kitayama N, Inoue M. Smoke free schools. Japanese Journal of School Health 2004;45:502‐4. [Google Scholar]
Poulsen 2002
- Poulsen LH, Osler M, Roberts C, Due P, Damsgaard MT, Holstein BE. Exposure to teachers smoking and adolescent smoking behaviour: analysis of cross sectional data from Denmark. Tobacco Control 2002;11(3):246‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reid 1999
- Reid D. Failure of an intervention to stop teenagers smoking. BMJ 1999;319(7215):934‐935. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sellström 2006
- Sellström E, Bremberg S. Is there a "school effect" on pupil outcomes? A review of multilevel studies. Journal of Epidemiology and Community Health. 2006;60(2):149‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2013
- Thomas RE, McLellan J, Perera R. School‐based programmes for preventing smoking. Cochrane Database of Systematic Reviews 2013, Issue 4. [DOI: 10.1002/14651858.CD001293.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tyas 1998
- Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tobacco Control 1998;7(4):409‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Warren 2008
- Warren CW, Jones NR, Peruga A, Chauvin J, Baptiste JP, Costa de Silva V. Global youth tobacco surveillance 2000‐2007. MMWR Surveillance Summaries 2008;57(1):1–28. [PubMed] [Google Scholar]
WHO 2012
- World Health Organization Tobacco Free Initiative. Tobacco Facts. www.who.int/tobacco/mpower/tobacco_facts/en/index.html (accessed May 2012).
Wilson 2012
- Wilson LM, Avila Tang E, Chander G, Hutton HE, Odelola OA, Elf JL, et al. Impact of tobacco control interventions on smoking initiation, cessation, and prevalence: a systematic review. Journal of Environmental Public Health 2012;2012:961724. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Coppo 2012
- Coppo A, Galanti MR, Buscemi D, Giordano L, Faggiano F. School policies for preventing smoking among young people. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD009990] [DOI] [PMC free article] [PubMed] [Google Scholar]


