Abstract
Background
There is evidence that family and friends influence children's decisions to smoke.
Objectives
To assess the effectiveness of interventions to help families stop children starting smoking.
Search methods
We searched 14 electronic bibliographic databases, including the Cochrane Tobacco Addiction Group specialized register, MEDLINE, EMBASE, PsycINFO, CINAHL unpublished material, and key articles' reference lists. We performed free‐text internet searches and targeted searches of appropriate websites, and hand‐searched key journals not available electronically. We consulted authors and experts in the field. The most recent search was 3 April 2014. There were no date or language limitations.
Selection criteria
Randomised controlled trials (RCTs) of interventions with children (aged 5‐12) or adolescents (aged 13‐18) and families to deter tobacco use. The primary outcome was the effect of the intervention on the smoking status of children who reported no use of tobacco at baseline. Included trials had to report outcomes measured at least six months from the start of the intervention.
Data collection and analysis
We reviewed all potentially relevant citations and retrieved the full text to determine whether the study was an RCT and matched our inclusion criteria. Two authors independently extracted study data for each RCT and assessed them for risk of bias. We pooled risk ratios using a Mantel‐Haenszel fixed effect model.
Main results
Twenty‐seven RCTs were included. The interventions were very heterogeneous in the components of the family intervention, the other risk behaviours targeted alongside tobacco, the age of children at baseline and the length of follow‐up. Two interventions were tested by two RCTs, one was tested by three RCTs and the remaining 20 distinct interventions were tested only by one RCT. Twenty‐three interventions were tested in the USA, two in Europe, one in Australia and one in India.
The control conditions fell into two main groups: no intervention or usual care; or school‐based interventions provided to all participants. These two groups of studies were considered separately.
Most studies had a judgement of 'unclear' for at least one risk of bias criteria, so the quality of evidence was downgraded to moderate. Although there was heterogeneity between studies there was little evidence of statistical heterogeneity in the results. We were unable to extract data from all studies in a format that allowed inclusion in a meta‐analysis.
There was moderate quality evidence family‐based interventions had a positive impact on preventing smoking when compared to a no intervention control. Nine studies (4810 participants) reporting smoking uptake amongst baseline non‐smokers could be pooled, but eight studies with about 5000 participants could not be pooled because of insufficient data. The pooled estimate detected a significant reduction in smoking behaviour in the intervention arms (risk ratio [RR] 0.76, 95% confidence interval [CI] 0.68 to 0.84). Most of these studies used intensive interventions. Estimates for the medium and low intensity subgroups were similar but confidence intervals were wide. Two studies in which some of the 4487 participants already had smoking experience at baseline did not detect evidence of effect (RR 1.04, 95% CI 0.93 to 1.17).
Eight RCTs compared a combined family plus school intervention to a school intervention only. Of the three studies with data, two RCTS with outcomes for 2301 baseline never smokers detected evidence of an effect (RR 0.85, 95% CI 0.75 to 0.96) and one study with data for 1096 participants not restricted to never users at baseline also detected a benefit (RR 0.60, 95% CI 0.38 to 0.94). The other five studies with about 18,500 participants did not report data in a format allowing meta‐analysis. One RCT also compared a family intervention to a school 'good behaviour' intervention and did not detect a difference between the two types of programme (RR 1.05, 95% CI 0.80 to 1.38, n = 388).
No studies identified any adverse effects of intervention.
Authors' conclusions
There is moderate quality evidence to suggest that family‐based interventions can have a positive effect on preventing children and adolescents from starting to smoke. There were more studies of high intensity programmes compared to a control group receiving no intervention, than there were for other compairsons. The evidence is therefore strongest for high intensity programmes used independently of school interventions. Programmes typically addressed family functioning, and were introduced when children were between 11 and 14 years old. Based on this moderate quality evidence a family intervention might reduce uptake or experimentation with smoking by between 16 and 32%. However, these findings should be interpreted cautiously because effect estimates could not include data from all studies. Our interpretation is that the common feature of the effective high intensity interventions was encouraging authoritative parenting (which is usually defined as showing strong interest in and care for the adolescent, often with rule setting). This is different from authoritarian parenting (do as I say) or neglectful or unsupervised parenting.
Keywords: Adolescent, Child, Humans, Family, Smoking Prevention, Randomized Controlled Trials as Topic, Smoking, Smoking/psychology
Plain language summary
Do interventions in families prevent children and adolescents from starting to smoke
Review question: This review asks whether family interventions can influence children and adolescents not to smoke, compared to no‐intervention controls or as an add‐on to a school intervention. We particularly focused on children who had never smoked.
Background: Preventing children from starting to smoke is important to avoid a lifetime of addiction, poor health, and social and economic consequences. Family members influence whether children and adolescents smoke. We wanted to know if there is enough evidence to justify funding interventions in families to prevent children starting smoking.
Last search: April 2014.
Study Characteristics: We identified 27 trials; 23 in the USA and one each in Australia, India, the Netherlands, and Norway. The focus varied amongst the studies. Fifteen trials focused on substance use prevention: six focused only on tobacco prevention; one focused on alcohol; one on general substance abuse; three on tobacco, alcohol and marijuana; two on alcohol and tobacco; and two on tobacco and cardiovascular health. Two trials focused on HIV and unsafe sex prevention. Ten trials focused on family functioning, child development and modifying adolescent behaviour. Duration of follow‐up after the intervention was very varied, ranging from 6 months to over 15 years for the studies which intervened with mothers of very young children.
Key Results: Nine trials provided data to compare a family tobacco intervention to no intervention on future smoking behaviour for those who did not smoke at the start of the study. We could not include data from a further eight trials. The results showed a significant benefit of family‐based interventions over the control comparison on preventing experimentation with or taking up regular smoking. Our estimate suggested that family interventions could reduce the number of adolescents who tried smoking at all by between 16 and 32%.
Two trials provided data to compare a combined family plus school intervention to a school intervention and also favoured the family‐based intervention. The estimate suggested that the addition of a family intervention might reduce the onset of smoking by between 4 and 25%. We could not include data from a further five trials.
Our interpretation is that the common feature of the effective interventions was encouraging authoritative parenting (which is usually defined as showing strong interest in and care for the adolescent, often with rule setting). This is different from authoritarian parenting (do as I say) or neglectful or unsupervised parenting.
Quality of the Evidence: Because most of the randomised controlled trials included in the review did not report their methods in sufficient detail to be confident that the results were not biased, we judged the quality of the evidence to be moderate, which means that the estimate of effect is uncertain.
Conclusions: There is moderate quality evidence that family‐based interventions can prevent children and adolescents from starting to smoke. Intensive programs may be more likely to be successful than those of lower intensity. There is also evidence to suggest that adding a family‐based component to a school intervention may be effective. As the interventions and settings in the review differed considerably, it is important that family‐based programmes continue to be evaluated.
Summary of findings
Summary of findings for the main comparison. Family interventions compared to no intervention.
| Family interventions for preventing smoking by children and adolescents | ||||||
|
Patient or population: Children or adolescents at risk for smoking uptake
Intervention: Family intervention Comparison: No intervention control | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Family intervention versus non intervention control group | |||||
| New smoking at follow‐up. Baseline never smokers only | Study population | RR 0.76 (0.68 to 0.84)1 | 48102 (9 studies) | ⊕⊕⊕⊝ Moderate3 | There was no evidence of statistical heterogeneity despite clinical heterogeneity in the characteristics and focus of the interventions, the age range targeted and the duration of follow‐up | |
| 230 per 1000 | 174 per 1000 (156 to 193) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
* Assumed risk based on average for control group participants reached at follow‐up. There was large variation between studies in the rate of new smoking behaviour.
1 RR <1 favours family intervention. 2 Eight studies with about 5,000 participants did not present data in a format that could be used in meta‐analysis. 3 Most studies have low or unclear risk of bias. Downgraded one level.
Summary of findings 2. Family and school intervention compared to school intervention.
| Family and school intervention compared to school intervention only for preventing smoking by children and adolescents | ||||||
|
Patient or population: Children or adolescents at risk for smoking uptake
Intervention: Family intervention in addition to school intervention Comparison: School intervention only | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| School intervention | Family and school intervention | |||||
| New smoking at follow‐up. Baseline never smokers only | 230 per 1000 | 196 per 1000 (172 to 221) | RR 0.85 (0.75 to 0.96)1 | 23012 (2 studies) | ⊕⊕⊕⊝ moderate3 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
* Assumed risk based on same average for control group participants reached at follow‐up as used in Analysis 1. There was large variation between studies in the rate of new smoking behaviour.
1 RR <1 favours family intervention.
2 Five studies with approximately 18,500 participants did not present data in a format that could be used in meta‐analysis, so estimate does not reflect all the evidence. 3 Most studies have low or unclear risk of bias. Downgraded one level.
Background
Tobacco use is the main preventable cause of death and disease worldwide, and the five million deaths annually attributable to tobacco use are predicted to increase to eight million annually by 2030 (Warren 2009). Smoking in adolescence continues to rise in many countries, with 23% of American high school students smoking in 2000, up from 18.5% in 1991 (Johnston 2000). Adult smoking begins in adolescence: in US studies 89% of adult smokers began regular tobacco use by the age of 18 (Bricker 2003). If poorer countries follow the trajectory of the more affluent countries, it is to be expected that 20% to 30% of 13 to 15 year olds may smoke, depending on the culture of the country and the activities of the tobacco companies (Warren 2009). Intervening to prevent smoking uptake during adolescence is critical to slowing or halting the trend towards increased tobacco‐related illness (USDHHS 1994).
A number of reviews, surveys and cohort studies have identified three broad classes of influences for smoking in adolescence: individual characteristics (e.g. gender, concerns with body weight, attitudes to smoking), family factors (parental smoking, number of smokers in the family, parental permissiveness and approval) and peer‐group or friends (number who smoke, academic expectations by friends) (Mayhew 2000). Ethnicity (Proescholdbell 2000), levels of affluence (Jarvis 1997) and level of education also affect smoking, with tertiary education being associated with lower rates of smoking (Chassin 1984; Chassin 1996). In a long‐term cohort study, Jarvis 1997 found that as adolescent smokers moved into young adulthood they were more likely to quit if they assumed adult responsibilities such as marriage and employment.
Parental behaviour also emerges as a significant determinant of adolescent smoking in a number of studies (Mounts 2002). A cohort study nested within the Hutchinson Smoking Prevention Project (Bricker 2003) found that the children of parents who had never smoked were the least likely to smoke (odds reduced by 71% compared with both parents currently smoking), while children of parents who had quit smoking also had reduced odds of smoking themselves (reduced by 39%). Several studies reported that parental advice not to smoke or explicit disapproval of smoking could be effective in young teens (Eisner 1989; Huver 2007; Krosnick 1982; Newman 1989) and in unmarried pregnant teenagers (Hussey 1992). Parenting style and parental restrictions on smoking at home also appeared to have an impact, with permissive home policies increasing the likelihood of experimentation, while authoritative parenting (combining demanding and responsive management of children's behaviour) was the least likely to prompt uptake of smoking (Jackson 1998; Proescholdbell 2000). The influence of friends and peers has also been shown to be associated with smoking behaviour (Krosnick 1982; Simons‐Morton 2002), but smoking uptake is negatively related to perceived social competence and parental monitoring. Smoking is associated with other risk behaviours (DuRant 1999).
There are some non‐modifiable family characteristics that affect the likelihood of smoking. Living in an intact two‐parent family is associated with less smoking by children (Botvin 1993: Covey 1990; Isohanni 1991; Turner 1991) while parental socio‐economic status and education are generally inversely correlated with children's smoking (Tyas 1998). However, Darling 2003 has pointed out that the focus of the literature on predicting the risk of adolescent smoking (which is a continuous process of change) from stable family characteristics such as structure may be one reason why understanding of the developmental processes involved in tobacco initiation is limited.
Further background and theoretical issues concerning adolescent smoking initiation are covered in a companion review of school‐based interventions (Thomas 2013). A Cochrane review of smoking prevention for Indigenous youth identified only two RCTs (Carson 2012). There are also Cochrane reviews of community interventions (Carson 2011) and mentoring to prevent adolescents smoking (Thomas 2011).
Objectives
To assess the effectiveness of interventions to help family members to strengthen non‐smoking attitudes and promote non‐smoking by children or adolescents or their family members.
Methods
Criteria for considering studies for this review
Types of studies
Studies were included in which students and/or family members were randomised to receive interventions or be in the control group, and were excluded if they did not state that allocation to intervention and control groups was randomised. We assessed whether studies used analytic methods appropriate to both the level of allocation and the level of measurement of the outcomes. We excluded those studies that presented only cross‐sectional data that permitted neither individuals nor clusters nor cohorts to be followed to the conclusion of the study.
Types of participants
Children (aged 5 to 12) and adolescents (aged 13 to 18) and family members. The search strategy chosen also located studies that follow these children beyond age 18.
Types of interventions
Interventions with children and family members intended to deter starting to use tobacco. Those with school‐ or community‐based components were included provided the effect of the family‐based intervention could clearly be measured and separated from the wider school‐ or community‐based interventions. Interventions that focused on preventing drug or alcohol use were included if outcomes for tobacco use were reported. The family‐based intervention could include any components to change parenting behaviour, parental or sibling smoking behaviour, or family communication and interaction.
For each study we determined whether during the study the participants received any co‐interventions such as the standard health or tobacco education curriculum taught in the school, or interventions that occurred in their community, and whether the control group received any interventions.
Types of outcome measures
The primary outcome was the effect of the intervention on the smoking status of children who reported no use of tobacco at baseline.
We excluded studies that:
did not assess baseline smoking status in the pre‐test survey;
measured attitudes and intentions to smoke, and did not measure smoking behaviour;
did not allow us to separate the effects of the family intervention from those of other co‐interventions;
focused primarily on cessation rather than prevention; and
did not follow up participants for at least six months from the start of the intervention.
Any measure of smoking behaviour was considered. Studies may use different measures of tobacco use, either frequency (monthly, weekly, daily), or the number of cigarettes smoked, or an index constructed from multiple measures. These measures attempt to capture the trajectories of smoking uptake in which there is a progression from initial experimentation (e.g., once a month in a younger child) to becoming a regular smoker. Not all experimenters make the transition to regular smoking, and interventions that reduce the likelihood of progression may be as useful as those that deter any experimentation. Previous reviews have noted that few studies use biochemical validation (by saliva thiocyanate or cotinine or expired air carbon monoxide levels) of self‐reported tobacco use for inclusion, and we did not require such validation here but recorded its use.
Search methods for identification of studies
We searched the Cochrane Tobacco Addiction Group Specialized Register (compiled by regular searching of electronic databases and specialist conference proceedings), and the Cochrane Central Register of Controlled Trials (CENTRAL). We performed ad hoc searches of the main electronic databases, including MEDLINE, EMBASE, PsycINFO, CINAHL, Web of Science, and ERIC. The MEDLINE search terms are given as an example in Appendix 1. We also searched the 'grey' literature (unpublished reports and conference proceedings), the web sites of relevant organizations, and the reference lists of key articles. Full details of the databases and websites searched are given in Appendix 2. The most recent search was performed on 3 April 2014. At the time of the search the Register included the results of searches of the Cochrane Central Register of Controlled trials (CENTRAL), issue 3, 2014; MEDLINE (via OVID) to update 20140321; EMBASE (via OVID) to week 201413; and PsycINFO (via OVID) to update 20140317. See the Tobacco Addiction Group Module in the Cochrane Library for full search strategies and list of other resources searched.
Data collection and analysis
Selection of studies
We reviewed all the studies retrieved from the literature searches to determine whether they were RCTs, and whether they matched our inclusion criteria. Details of those studies which did not meet the criteria are given in the Table of Excluded Studies, with the reasons for their exclusion.
Data extraction and management
One reviewer (RET) extracted data from the included studies, and the other reviewers (BCT, PB, DLL) independently checked them. We corresponded with authors to clarify study details. Any disagreements were resolved by discussion and consensus. The Co‐ordinating Editor of the Tobacco Addiction Group was available to assist with persistent disagreements.
After entering the studies in the Included Studies Table we noted they varied greatly in intensity. Programe intensity was measured using four dimensions (Baker 2015) and rated High, Medium or Low: Proximity: local [H] – personal (on site, in‐home, face‐to‐face); distant [L] (e.g. mailing, telephone); Direction: programme directed [H] (with consistent prompts and contact, accountability to participate and engage), self‐directed [L] (up to the individual to work through the materials); Exposure period: duration of provision of the intervention and number of components; Unit of delivery: to family in groups [H], individual families [H] or community [L]. Two other aspects were considered: Cost per family to deliver the programme, and Authors' description of intensity, but data were rarely provided. Summary judgments were independently made whether the intervention was high, medium, or low intensity.
Assessment of risk of bias in included studies
Studies were independently assessed by RET, BCT, PB, and DLL for sources of bias that the Cochrane Collaboration Reviewers' Handbook identifies as potential threats to validity.
We also assessed three statistical criteria:
A reported power calculation with attainment of the desired sample size. If a non‐significant result is obtained it may be due either to inadequate sample size or a be a true negative result.
The statistical analysis was deemed appropriate to the unit of randomisation for the family intervention. Intra‐class correlations (ICCs) in smoking behaviour vary by group, school grade, frequency of smoking, gender, ethnicity, and time of school year. ICCs typically inflate the required sample size, and failure to take account of these may lead to inadequate sample size and the risk of drawing false negative conclusions (Type II error) (Dielman 1994; Murray 1990; Murray 1997; Palmer 1998). We considered statistical analysis to be appropriate if the analysis used the same unit as randomisation (for example, if the family intervention was delivered at the level of the school then the school was the unit of analysis), or if other methods were used to account for cluster effects, such as multi‐level modelling.
An intention‐to‐treat analysis.
Data synthesis
Data were extracted from randomised controlled trials that reported smoking prevention (number or percentage of non‐smoking children at baseline that remained non‐smokers at follow‐up) and a minimum follow‐up time of six months. The outcomes used were the proportion prevented from smoking and we used the longest available follow‐up time for the analysis and computed risk ratios. Adjusted risk ratios from cluster‐randomised trials were obtained directly from those trials that reported them. If there is a large degree of heterogeneity in study design, type of outcome measure and statistical reporting, quantitative synthesis is not appropriate. Where trials could be pooled we estimated the effects using a fixed effect (Mantel‐Haenszel) model.
Results
Description of studies
Twenty‐seven trials met the inclusion criteria, of which 12 were randomised controlled trials (RCTs) and 15 were cluster RCTs (C‐RCTs). We identified eight new trials for this update. Full details of included studies are given in the Characteristics of included studies table. We excluded three previously included studies; Knutsen 1991 was excluded as there were no baseline smoking data for children; Nutbeam 1993 was excluded as it was not possible to evaluate the minimal family intervention separately from the school intervention in which it is included; and Salminen 2005 was excluded as, on closer examination, allocation was not randomised. Including these three, we now list 76 excluded studies, details of which can be found in the Characteristics of excluded studies table.
Twenty‐three trials were conducted in the USA and one each in Australia, India, the Netherlands, and Norway.
All RCTs tested a family intervention, though the interventions were heterogeneous. The Family Resource Center intervention was tested in two trials (Connell 2007 and Fosco 2013), the Smoke‐Free Kids programme was also tested in two trials (Hiemstra 2014 and Jackson 2006), and the Strengthening Families Program (SFP 10‐14) was tested in three trials (Spoth 2001, Spoth 2002 and a short version by Riesch 2012). Twenty other interventions were each tested by only one RCT. Interventions typically addressed family functioning in order to prevent multiple risky behaviours including tobacco use and substance abuse. A smaller number focused on tobacco alone, and two (Prado 2007; Wu 2003) primarily addressed HIV and unsafe sex but assessed tobacco use outcomes. Nineteen studies had a control group which offered either no intervention, usual care, or a very minimal intervention such as a leaflet, or used a control that targeted different risk behaviours. Eight studies tested a family intervention as an adjunct to a school‐based prevention programme offered to both intervention and control groups.
In addition to heterogeneity of intervention design, focus, and comparator condition there was also variation in the length of follow‐up, ranging from 6 months to 29 years. Key features of the studies are summarised in the following two tables. Table 3 lists studies that compared a family intervention to no intervention, and Table 4 shows studies that tested a family intervention as an adjunct to a school intervention.
1. Summary of studies of family versus no intervention.
| Study | In MA | Intensity | Focus | Age/ grade at baseline | Duration of follow‐up | Control |
| Cullen 1996 | Y | High | Family functioning | New born | 27‐29 years | No intervention/'usual care' |
| Fosco 2013 | Y | High | Family functioning | 6‐8th grade | 3 years | No intervention/'usual care' |
| Haggerty 2007 | Y | High | Family functioning | 8th grade | 2 years | No intervention/'usual care' |
| Prado 2007 | Y | High | HIV & Unsafe sex | Average age 13 | 3 years | Attention control |
| Spoth 2001 | Y | High | Tobacco, alcohol, marijuana | 6th grade | 6 years | Fact sheets/booklets |
| Storr 2002 | Y | High | Child attention problems | 1st grade | 7 years (8th grade) | No intervention^ |
| Pierce 2008 | Y* | High | Family functioning | 12 years | 6 years (age 18) | No intervention |
| Connell 2007 | N | High | Family functioning | 6th grade | 11 years (age 22) | No intervention |
| Dishion 1995 | N | High | Family functioning | Age 10‐14 | 12 months | Teen focus |
| Fang 2013 | N | High | Substance abuse | Age 10‐14 | 2 years | No intervention/'usual care' |
| Olds 1998 | N | High | Family functioning | New born | 15 years | No intervention/'usual care' |
| Riesch 2012 | N | High | Family functioning | Age 9‐11 | 6 months | No intervention/'usual care' |
| Bauman 2001 | Y | Medium | Tobacco & alcohol | Age 12‐14 | 12 months | No intervention/'usual care' |
| Schinke 2004 | N | Medium | Alcohol | Average age 11.5 | 3 years | No intervention/'usual care' |
| Hiemstra 2014 | Y | Low | Tobacco | Age 9‐11 | 3 years | Fact sheets/booklets |
| Jackson 2006 | Y | Low | Tobacco | 3rd grade | 3 years | Fact sheets/booklets |
| Curry 2003 | Y* | Low | Tobacco | Age 10‐12 | 20 months | No intervention/'usual care' |
| Stevens 2002 | N | Low | Tobacco & Alcohol | Average age 11 | 3 years | Prevention of different risky behaviours |
| Wu 2003 | N | Low | HIV & Unsafe sex | Age 12‐16 | 2 years | Teen only focus |
* Includes baseline smokers
^ Also compared to school programme alone
2. Summary of studies of family & school versus school alone.
| Study | In MA | Intensity | Focus | Age/ grade at baseline | Duration of follow‐up | Control |
| Spoth 2002 | Y | High | Family Functioning | 7th grade | 1 year | School only |
| Guilamo‐Ramos 2010 | Y* | High | Tobacco | 6‐8th grade | 15 months | School only |
| Forman 1990 | N | High | Tobacco, alcohol, marijuana | Average age 15 | 1 year | School only |
| Elder 1996 | N | Medium | Tobacco & cardiovascular | 3rd grade | 3 years | School only |
| Jøsendal 1998 | Y | Low | Tobacco | 13 years | 30 months | School only |
| Ary 1990 | N | Low | Tobacco, alcohol, marijuana | 6‐9th grade | 9‐12 months | School only |
| Biglan 1987 | N | Low | Tobacco | 7‐10th grade | 12 months | School only |
| Reddy 2002 | N | Low | Tobacco & cardiovascular | Age 12 | 1‐8 months | School only |
* Includes baseline smokers
Clustering was controlled for in the following C‐RCTs: Ary 1990; Biglan 1987; Forman 1990; Fosco 2013; Hiemstra 2014; Jackson 2006; Jøsendal 1998; Reddy 2002; Riesch 2012; Spoth 2001; and Spoth 2002. Only three trials provided intraclass correlations (ICCs) (Guilamo‐Ramos 2010 < 0.01, Hiemstra 2014, ICC = "zero" and Wu 2003, ICC = 0.0000). Only one RCT (Dishion 1995) did not control for clustering, and as the ICCs for the three trials which provided them were zero, we did not apply any correction to Dishion 1995. All other trials involved individual interventions with parents or youth and correction for clustering was not required. Ten studies reported good adherence to training (where relevant) and adherence to intervention, 13 reported intermediate levels and four had no evidence about adherence, or evidence of minimal adherence (fidelity and adherence summarised in Table 5). We were unable to extract data from thirteen study reports in a format that could be included in meta‐analysis.
3. Classification of fidelity of training & intervention adherence.
| Study | Fidelity of training/ adherence | Description |
| Bauman 2001 | Good | Provided the consultants to the parents with manualised training throughout the two year programme. "Families who completed the entire program (74%) spent an average total 4 1/2 hours doing the program and parents spent an additional hour talking with the health educator by telephone. The majority of families completed all activities associated with each booklet." |
| Elder 1996 | Good | Provided classroom teachers with 1 or 1.5 training sessions. He found that of the children who began in a school which offered the school + family intervention, 47% attended such a school for the entire period. For the FACTS tobacco curriculum 87% of teachers participated in the classroom sessions, checklists were returned for 96% of classroom sessions, 96% completed the entire lesson and 87% were implemented without modification. For the Family Intervention for tobacco 97% of session‐specific activities were completed, and 78% of adults participated in the home activities. However, only 48% of home team activity cards were returned, 40% of schools participated in 'Great American Smokeout' activities, 33% of schools held assemblies about tobacco and 25% sponsored anti‐tobacco or anti‐drug clubs. |
| Fang 2013 | Good | The intervention was delivered by Internet and fidelity was assured because the computer automatically returned participants to the last place at which they logged off and participants could not log on to the next module until the previous one was completed; only data from participants who answered 3 of 4 fidelity check questions were included. |
| Forman 1990 | Good | All sessions were tape recorded and independent raters achieved intercoder agreement > 90%. In the coping skills training group half of the sessions covered > 80% of the planned activities, the average completion rate across all coping sessions was 74%, 2/3 of the students completed 9 or 10 of the intervention sessions and 92% completed at least 7. In the School‐Plus‐Parent intervention 44% of the students had at least one parent participate in the parent training sessions and of the parents who attended 74% attended at least 4 meetings. |
| Haggerty 2007 | Good | The intervention was self‐administered with telephone support. The mean level of reported completion of the family activities was 81%. On average, family consultants made 16.9 call attempts (resulting in 9.7 completed calls during the 10 weeks) and phone calls lasted about 10.5 minutes/week. in the parent and adolescent format group leaders called families each week to remind them of the upcoming session and 77.9% of families initiated the parent and teen sessions. The mean number of sessions attended was 4.56. Family sessions were led by two workshop leaders with prior experience conducting parent or teen workshops who received 20 hours of training. |
| Hiemstra 2014 | Good | 81% of intervention group children read and completed ⋝ 3 modules and 73% of control families read and completed 3 fact sheets. |
| Riesch 2012 | Good | Students received three 2‐day training sessions. On their checklists more than 90% of the content was consistently covered in the adult groups and 87% in the youth groups. |
| Schinke 2004 | Good | CD‐ROM usage was recorded by code: 95% of youths completed the CD‐ROM in the CD‐ROM intervention group, and 91% in the CD‐ROM + parent intervention group, 83% of parents watched the videotape, 67 % attended the workshop and 79% completed the parent CD‐ROM |
| Spoth 2001 | Good | ISFP intervention: each team of leaders was observed 2‐3 times and there were reliability checks on 50% of family, 30% of youth and 25% of parent sessions (paired observers' scores differed by an average of 10%): coverage of topics was 89% in youth, 87% in family, and 83% in parent sessions. PDFY intervention: each team of group leaders was observed for 2/5 sessions and 50% of these sessions were observed by two observers (average ratings difference 6%) and there was an average 69% coverage of topics. |
| Spoth 2002 | Good | SFP 10‐14 intervention: each team of facilitators was observed on 2‐3 occasions (observers' ratings differed by an average of 2.4%) and average adherence to programme components was 92%. LST intervention: each classroom teacher was observed on 2‐3 occasions (observers' ratings differed by an average 13.6%) and average programme component adherence was 85%. |
| Ary 1990 | Intermediate | Provided teachers with 2‐3 hours of classroom instruction. Surveys of teachers indicated that the control group received 10 sessions of standard tobacco and drug education (with 97% recognizing peer pressures, 97% short‐term effects on the body and brain, 96% long‐term health consequences, 84% decision‐making skills, 72% media pressures, and 67% refusal skills practice), and the intervention schools received a median of 5 sessions of other drug education in addition to PATH. There was no assessment whether the letters to parents were received or read. |
| Connell 2007 | Intermediate | Of the 500 participants, only 115 chose to participate in the Family Check Up. These families received an average 8.9 hours of direct contact with intervention staff. |
| Cullen 1996 | Intermediate | Same general practitioner provided the counselling throughout the intervention, standard questions were used to introduce new ideas but there is no statement that a manualised protocol was followed. |
| Curry 2003 | Intermediate | After 6 months 83% of the parents in the intervention group said they had read the handbook, completed one or more activities and spoken with a counsellor; 51% reported they had watched the videotape and 42% the CDC tape and 47% of the intervention and 45% of the control group children had visited a physician in the previous 6 months. However, of these only 22% in the intervention and 15% in the control group said tobacco use was discussed with the child; and 17% in the intervention and 3% in the control group said the 'Steering Clear' project was discussed. |
| Dishion 1995 | Intermediate | All participants were visited by a therapist at home but there was no process analysis. |
| Fosco 2013 | Intermediate | Of 386 families in the intervention group, 51% received a consultation from a parent consultant and 42% in the full FCU intervention. Of those receiving FCU 78% received additional follow‐up assistance such as parent skills training, education‐related concerns, support in success with homework, attendance and grades, improving school behaviour, and facilitating parent‐teacher communication. Of 180 families, 36% received positive behaviour support, 68% support in limit setting and monitoring skills, 73% support for communication and problem‐solving, 67% school‐related support. Intervention families received an average 94.2 minutes of intervention time |
| Jackson 2006 | Intermediate | Interviews with children were by staff with 2 years experience and 30 hours of training and parent interviews were computer‐assisted by a contracted survey unit. There was no process analysis whether parents received, read and discussed tip sheets, or if the control group received and read the fact sheets. |
| Jøsendal 1998 | Intermediate | A process analysis was conducted but the results were not stated, and there was no process analysis of the intervention variations as time progressed: There were "verbal assurances of compliance from Grade 8 pupils and teachers and Grade 9 pupils." |
| Pierce 2008 | Intermediate | parent counsellors completed 60 hours of training including role playing and tapes were reviewed for fidelity (no statement of fidelity outcomes). |
| Prado 2007 | Intermediate | Facilitators had an average 5 years experience working with low‐income Hispanic immigrant families, were certified in Familias Unidas and PATH, were trained in general group process facilitation and conducted 54 pilot sessions. All sessions were taped. Adherence to Familias Unidas was 3.72/6 and to PATH 3.70/6 (interrater reliability k = .75). |
| Reddy 2002 | Intermediate | There was no process analysis; 2/30 schools had shorter follow‐up; 14/20 schools displayed all 10 posters, 6 displayed 7‐9; 6/20 schools implemented all 20 activities from the teachers' manual, and 8/10 schools in the Family intervention group distributed at least 5 of the 6 booklets. |
| Stevens 2002 | Intermediate | All paediatricians and nurse practitioners received 3 hours of training. After the initial intervention visits 95% of children were seen for subsequent visits, during which prevention messages were documented as delivered in only 47% of the safety intervention and 51% of the alcohol/tobacco intervention practices |
| Storr 2002 | Intermediate | First grade CC and FSP teachers received 60 hours training and certification. In the CC Intervention the implementation mean score was 59.9% and median score 64.4% (range 30‐78%). In the FSP intervention parents attended an average 4/7 and median 5/7 of the core parenting sessions (and 13% attended none). |
| Biglan 1987 | No/minimal evidence | Provided classroom teachers with 2‐3 hours of training. No statement if the parent messages were received or read. |
| Guilamo‐Ramos 2010 | No/minimal evidence | No statement about training or fidelity of implementation. |
| Olds 1998 | No/minimal evidence | Wide ranges in the number of visits (families visited at home received an average of 9 [range 0 ‐16] visits during pregnancy and 23 [range 0 ‐ 59] from birth through the child's 2nd birthday). There was no process analysis of the content of the visits. |
| Wu 2003 | No/minimal evidence | No process analysis. |
We grouped the studies according to the intensity of the family component into three levels of intensity. In the descriptions below, the studies contributed to the comparison between a family intervention and a non intervention or usual care control, unless noted otherwise.
(a) High Intensity
Connell 2007 compared: (1) the provision of a Family Resource Center in schools with (a) brief consultations with parents; (b) telephone consultations; (c) feedback to parents on their children's behaviour at school; (d) access to videotapes and books; (e) the SHAPe Curriculum for students with 6 lessons (school success, health decisions, building positive peer groups, cycle of respect, coping with stress and anger, and solving problems peacefully), and (2) the Family Resource Center + Family Check Up (interviews exploring parent concerns, assessment including videotaping the family at home, feedback by the therapist using motivational interviewing strategies and exploring interventional services the family could use, which were delivered over two years by therapists). This study could not be included in a meta‐analysis.
Cullen 1996 tested the effect of 20‐30 minute interviews (four annually in the 1st year and two annually for the next four years) by a general practitioner with new mothers to enhance self‐worth, self‐acceptance, foster gentle physical interaction with her child, and adopt a positive attitude to modifying her child's behaviour. Children were followed up as adolescents or young adults.
Dishion 1995 tested "alternative strategies to reduce escalation in problem behaviours among high‐risk young adolescents." Strategeis were to "target parents' use of effective and non‐coercive family management practices (parent focus) and young adolescent's self‐regulation and competence in family and peer environments (teen focus)." Parent sessions focused on four key skills: monitoring; positive reinforcement; limit setting and problem solving. Twelve 90‐minute counselling sessions based on scripted materials and videotapes were tested in four formats: (1) Parent focus: the parent's family management practices and communication skills (monitoring, positive reinforcement, limit setting, and problem solving, with discussion of home practices and demonstration of the skills, with exercises, role‐plays, and discussions); (2) Teen focus: teen self‐regulation and pro‐social behaviour in parental and peer environments (self‐monitoring and tracking, pro‐social goal setting, developing peer environments supportive of pro‐social behaviour; setting limits with friends and problem solving and communication skills with parents and peers); (3) combined parent and teen intervention and (4) self directed change (the six newsletters and five brief videos that accompanied the parent‐ and teen‐interventions). Interventions 1‐3 were classified as high intensity. Results could not be included in a meta‐analysis
Forman 1990 compared (1) a school intervention (10 session small groups with Botvin's Life Skills Training), and (2) the school intervention + a parent intervention (parents participated in five weekly two‐hour sessions to teach parents the coping skills their children were learning in the student groups, teach parents behaviour management skills, and develop a small group support system for parents to encourage each other to take positive, constructive action regarding their adolescents). This study of a family intervention as adjunct to a school intervention could not be included in a meta‐analysis.
Fosco 2013 compared (1) use of Family Resource Center in schools to (2) control (no intervention). A parent consultant was trained in the Family Check‐Up model to facilitate collaboration with parents, identify youth at risk, and refer at‐risk students for counselling. At risk adolescents and families participated in three motivational interviewing sessions to identify family strengths and weaknesses, motivate parents to improve parenting, and to engage in intervention services. Feedback about assessment results provided opportunity to select interventions tailored to unique needs of each family.
Guilamo‐Ramos 2010 compared (1) the Project Towards No Tobacco Use (TNT) risk reduction smoking intervention (10 modules modified for inner city schools and two face‐to‐face sessions of 2.5 hours each addressing: effective listening and tobacco information; course and consequences of tobacco use; self esteem; being true to oneself; changing negative thoughts; effective communication; assertiveness and refusal skills; advertising and social activism), and (2) the "Linking Lives" intervention (consisting of: "Raising Smoke‐Free Kids" (manual of nine short modules, two tobacco‐related homework assignments for parents to use with adolescent); two one‐day sessions (Day 1 discussed module topics, concept parents could make a difference in their adolescent's tobacco‐related behaviour, strategies for effective communication, topics parents might consider discussing in their conversations with their adolescents and the importance of setting limits; Day 2 consisted of two tobacco‐related homework assignments on consequences of smoking and ways to resist peer pressure)). Mothers received two booster calls one and six months after the intervention. This study contributes to the analysis of family interventions used as adjuncts to school interventions.
Haggerty 2007 compared two formats (self‐administered with telephone facilitator support, and a parent and adolescent format) for a seven session "Parents Who Care" programme and control (no treatment). The seven chapters of the workbook were: Relating to your teen; Risks: Identifying and reducing them; Protection: Bonding with your teen to strengthen resilience; Tools: Working with your family to solve problems; Involvement: Allowing everyone to contribute; Policies: Setting family policies on health and safety issues and Supervision: Supervising without invading. In each session parents and adolescents watched a video, practised skills separately and then as families and were asked to continue practice at home.
Olds 1998 provided for infants (1) free sensory and developmental screening performed at 12 and 24 months, with referrals for further evaluation and treatment where necessary, and (2) the same assessments and nurse home visits (nurses taught positive health‐related behaviours, competent care of the child, and personal development for the mother including family planning, educational achievement, and return to the workforce). Children's smoking was assessed at age 15 years. This study could not be included in a meta‐analysis.
Pierce 2008 tested the Parenting to Prevent Problem Behaviors Project, including a self‐help manual (with 12 chapters including building positive behaviours, setting effective limits and relationship building) and a lay facilitator to help participants to work through the manual who followed a computer‐assisted structured counselling script using motivational interviewing and searched the internet and study library for answers to parents' problems. Previously researched information sheets were sent to parents electronically or by mail, and there was a computer‐assisted structured counselling protocol for parents who needed additional help to implement best practices.
Prado 2007 assessed whether providing an intervention to focus on and strengthen Hispanic family‐centred values was required for a substance, sexual behaviour and HIV risk intervention to be effective. He compared: (1) an intervention to improve family functioning to reduce substance use and unsafe sexual behaviour (the Familias Unidas intervention to increase parental involvement, positive parenting and family support in Hispanic families (high intensity) combined with PATH [Parent pre‐adolescent training for HIV prevention]); (2) PATH and an intervention unrelated to parenting (English language lessons); and (3) PATH and a different intervention unrelated to parenting (American Heart Assocation programme).
Riesch 2012 tested a short version of the Strengthening Families Program (SFP 10‐14 ), during which a youth and parent attended the seven‐week, two‐hour‐per‐week programme with videotapes and discussions. This study could not be included in a meta‐analysis.
Spoth 2001 compared two family interventions: (1) the full length SFP 10‐14, now renamed ISF (six two‐hour session and one one‐hour sessions); (2) the Preparing for the Drug‐Free Years Program (five two‐hour sessions) and (3) a control group which received mailed information. The two family interventions are shown separately in the analysis, dividing the control group to avoid double counting
Spoth 2002 tested the SFP programme of seven one‐hour weekly sessions for parents and children to strengthen parental skills in nurturing, setting limits and communication about substances and strengthen children's prosocial and peer resistance skills, and four booster sessions offered one year later. All study participants received the Life Skills Training (LST) intervention at school, so this contributes to the analysis of family interventions used as adjuncts to school intervention.
Storr 2002 compared: (1) the Classroom‐Centered (CC) Intervention (language and mathematics curricula enhanced to encourage skills in critical thinking, composition, listening and comprehension, whole‐class strategies to encourage problem solving by children in group contexts, decrease aggressive behaviour, and encourage time on task, strategies for children not performing adequately; plus teams of children received points for good behaviour and lost points for behaviours such as starting fights ‐ the points could be exchanged for classroom activities, game periods and stickers), and (2) the Family‐School Partnership (FSP) intervention (consisting of multiple components: (a) the 'Parents on Your Side Program' trained teachers to communicate with parents and build partnerships, with a three‐day workshop, training manual and follow‐up supervisory visits; (b) weekly home‐school learning and communicating activities and (c) nine workshops for parents (first two workshops to establish an effective and enduring parent‐staff relationship and facilitate children's learning and behaviour; next five workshops focused on effective disciplinary strategies). This was classified as high intensity for the amount of contact, but there was no description of the amount of tobacco‐focused content. The FSP intervention was also compared to a usual curriculum condition, which is used as the comparator in the family versus no intervention analysis.
(b) Medium intensity
Bauman 2001 tested the Family Matters intervention: four booklets were mailed to participants, and two weeks after each booklet was posted a health educator telephoned a parent, encouraged the participation of all family members in the programme and answered questions.
Elder 1996 compared: (1) a school intervention (15 sessions in third grade about diets healthy for hearts and exercise, 12 in fourth grade about exercise, and 16 about exercise in fifth grade plus eight about tobacco; the tobacco intervention consisted of 'F.A.C.T.S. for 5' (Facts and Activities about Chewing Tobacco and Smoking) with four 50 minutes sessions on: short‐ and long‐term effects of tobacco use; motivations and fallacies about tobacco use; economic costs of tobacco use and the efforts of the tobacco companies to promote use; dangers of passive smoking and being supportive of those who want to quit), as well as a policy component, encouraging the adoption of policies for the school to be tobacco‐free and (2) the school intervention plus a family intervention consisting of a home‐based programme, using 'The Unpuffables' (four sessions with stories about adolescents who combat tobacco use, and games to play with parents) (moderate intensity). This study of a family intervention as adjunct to a school intervention could not be included in a meta‐analysis.
Fang 2013 tested an online nine session (each 35‐45 minutes) substance abuse prevention programme to strengthen the quality of girls' relationships with mothers and increase girls' resilience to resist substance use (consisting of audio, graphics, animation, activities, skill demonstrations, guided rehearsal and immediate feedback).
Schinke 2004 compared a social learning and problem solving curriculum on CD‐ROM (consisting of goal setting, coping, peer pressure, refusal skills, norm correcting, self‐efficacy, problem‐solving (Stop, Options, Decide, Act, Self‐praise), decision‐making, effective communication and time management), and (2) the CD‐ROM + parent intervention (videotape, printed materials on the goals of the youth intervention, showed how parents could help avoid problems with alcohol, and the importance of family rituals, rules and bonding, a two‐hour parent workshop, and a parent CD‐ROM how to reduce youth alcohol use). This study could not be included in a meta‐analysis.
(c) Low intensity (usually written materials or brief contact)
Ary 1990 compared (1) the tobacco social skills Project PATH (Programs to Advance Teen Health), and (2) PATH + parent messages (three mailed brochures to support the classroom messages about refusal skills). This study of a family intervention as adjunct to a school intervention could not be included in a meta‐analysis.
Biglan 1987 compared (1) a programme of information about the health effects and short‐term effects of tobacco, including sensitization to pressures to smoke, training in refusal skills including modelling, rehearsal, reinforcement, practice, video practice, and supporting peers in refusals, and (2) the programme plus four messages mailed to parents following the programme to encourage parents to discuss their views of smoking with their child and set clear rules about smoking. This study of a family intervention as adjunct to a school intervention could not be included in a meta‐analysis.
Curry 2003 tested the 'Steering Clear Project, which included: (a) a 12‐chapter parent handbook, a videotape on the experiences of a former tobacco model, a Centers for Disease Control videotape and a comic book, pen and stickers for the child; (b) two calls from a counsellor; (c) a six‐page newsletter 14 months later; (d) access to a website and (e) prompts to physicians during appointments to encourage families to use the videos and website and talk about staying smoke‐free.
Hiemstra 2014 and Jackson 2006 compared (1) the home‐based Smoke‐Free Kids programme (six printed activity modules containing general communication about smoking, influence of smoking messages, rule setting and non‐smoking agreement, creating a smoke‐free house and environment, and peer influences), and (2) five fact sheets on youth smoking available in the media.
Jøsendal 1998 tested three formats (classroom programme with (1) involvement of parents and teachers, (2) involvement of parents only, or (3) involvement of teachers only) for an eight‐session intervention focused on personal freedom, the freedom to choose, freedom from addiction, making one's own decisions, tobacco‐resistance skills, and the short‐term consequences of smoking. Students brought two brochures home, teachers involved parents in discussions on 'appropriate occasions', and students and parents signed non‐smoking contracts. This study contributes to the analysis of family interventions used as adjuncts to a school intervention.
Reddy 2002 compared (1) the school‐based Project HRIDAY (Health‐Related Information and Dissemination Among Youth), consisting of posters, a booklet on heart health, classroom activities addressing influences to smoke, ways to refuse offers to smoke, and passive smoke, and round table discussions, and (2) HRIDAY plus a family intervention (consisting of six booklets, one of which was about tobacco, brought back to school with parents' signed opinions about the booklets). This study of a family intervention as adjunct to a school intervention could not be included in a meta‐analysis.
Stevens 2002 compared the effect of paediatrician/nurse practitioner advice about (1) alcohol and tobacco and (2) advice about gun safety, bicycle helmets and car seatbelts. Interventions encouraged family communication and rule setting, there was a brochure on effective communication, and children and parents each received 12 quarterly newsletters to reinforce the messages.
Wu 2003 compared (1) Focus on Kids (FOK), an eight session HIV small‐group risk reduction programme focusing on decision making, goal setting, communication, negotiating, and consensual relationships and information regarding safe sex, drugs, alcohol and drug selling, conducted in small groups (5‐10), led by two older peers with no parental involvement, (2) FOK + ImPACT (Informed Parents and Children Together) which included a 20‐minute video about parental monitoring and communicating, role‐playing vignettes in the child's home between the parent and youth with instructor critique and a condom demonstration from the instruction, and (3) FOK + ImPACT + booster sessions at 6 and 10 months. FOK has a minor informational component about tobacco and no family component. ImPACT is 20 minute video followed by role plays between parent and youth but has no tobacco focus. Baseline and 24 months smoking status were measured for all three programmes. We assessed ImPACT as low intensity, without tobacco intervention but with tobacco data collection.
Risk of bias in included studies
Fifty‐two per cent of trials were assessed to be at low risk of selection bias due to the method of randomisation, 44% at unknown risk (because only the words "randomised" were used with no method stated) and 4% at high risk. Eleven per cent of trials were at low risk for allocation concealment, 85% at unknown risk (no statement if performed) and 4% at high risk. Eleven per cent were at low risk for blinding of participants and personnel, 85% at unknown risk (no statement if performed) and 4% at high risk. (Note: It would have not been possible to blind participants to which programme they were in). Twenty‐two per cent of studies were at low risk for blinding of outcome assessment and 78% at unknown risk (no statement if performed). Forty‐one per cent were at low risk for incomplete outcome data, 52% at unknown risk (insufficient information provided to assess if at risk), and 7% at high risk. All were judged to be at low risk for selective reporting (see Figure 1 and Figure 2).
1.
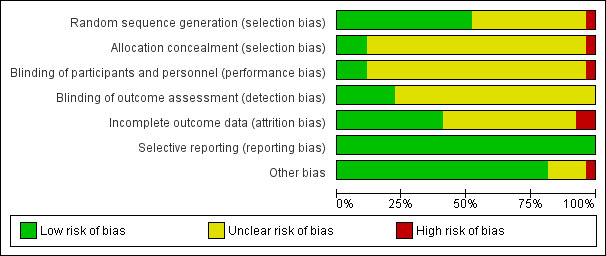
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.
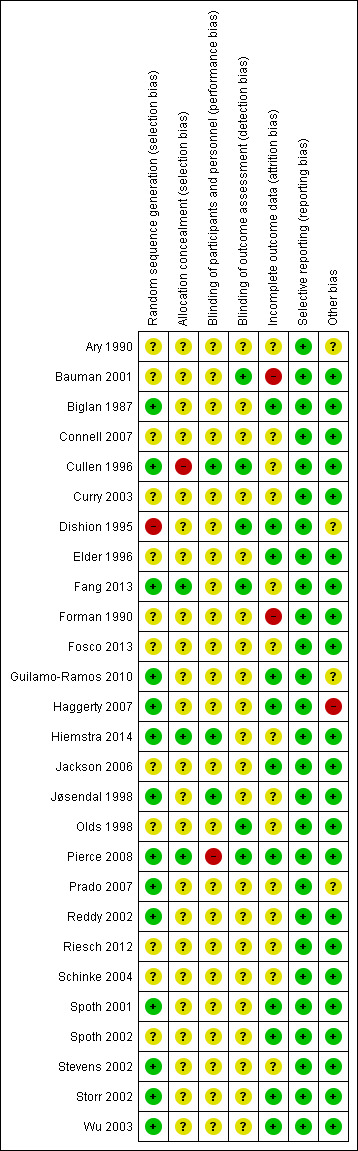
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Effects of interventions
The outcome for all analyses was smoking behaviour at longest follow‐up. Smoking behaviour could include even a puff, or more regular use.
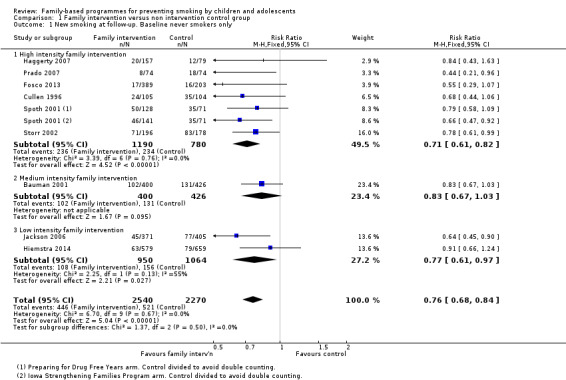
Analysis 1. Family intervention compared to no intervention
Nine studies (4810 participants at follow‐up) reported the impact of a family intervention on smoking uptake for baseline never smokers in a format suitable for meta‐analysis. The pooled estimate detected a reduction in smoking behaviour in the intervention arm (risk ratio [RR] 0.76, 95% confidence interval [CI] 0.68 to 0.84) Figure 3 (Analysis 1.1). When the trials were analysed by intensity of family intervention there was a significant effect in the subgroup of six which used a high intensity intervention (Cullen 1996;Fosco 2013; Haggerty 2007; Prado 2007; Spoth 2001 (two arms: PDFY and ISFP); Storr 2002) (RR 0.71, 95% CI 0.61 to 0.82). Only one study was categorised as using a medium intensity intervention (Bauman 2001). Two used a low intensity intervention (Hiemstra 2014; Jackson 2006) with a RR of 0.77, 95% CI 0.61 to 0.97. Three of the studies individually reported significant effects; Spoth 2001 (using the Iowa Strengthening Families intervention) and Storr 2002 which were high intensity, and Jackson 2006, which was low intensity.
3.
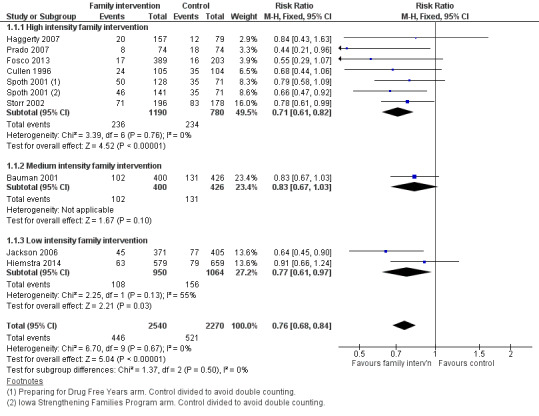
Family intervention versus non intervention control group: New smoking at follow‐up. Baseline never smokers only.
1.1. Analysis.
Comparison 1 Family intervention versus non intervention control group, Outcome 1 New smoking at follow‐up. Baseline never smokers only.
Two studies provided data for meta‐analysis but included some participants who already had experience of smoking at baseline. One used a high intensity family intervention (Pierce 2008) and one a low intensity intervention (Curry 2003). When pooled, these studies (4487 participants) did not detect evidence of any intervention effect (RR 1.04, 95% CI 0.93 to 1.17, Analysis 1.2)
1.2. Analysis.
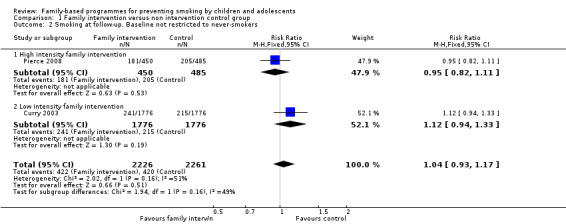
Comparison 1 Family intervention versus non intervention control group, Outcome 2 Smoking at follow‐up. Baseline not restricted to never‐smokers.
Eight studies (approximately 5000 participants) compared a family intervention to control, but did not report outcomes in a format suitable for inclusion in the meta‐analysis. Effects are summarised in Analysis 1.3. Four used a high intensity intervention (Connell 2007; Dishion 1995; Olds 1998; Riesch 2012), two a medium intensity (Fang 2013; Schinke 2004) and two a low intensity intervention (Stevens 2002; Wu 2003). Only one of these studies reported a significant positive effect (Wu 2003); most of the remainder reported non significant effects favouring the intervention.
1.3. Analysis.
Comparison 1 Family intervention versus non intervention control group, Outcome 3 Smoking at follow‐up. Results not in meta‐analysable format.
| Smoking at follow‐up. Results not in meta‐analysable format | ||
|---|---|---|
| Study | Number of participants | Results |
| High intensity family intervention | ||
| Connell 2007 | 998 6th graders allocated. 115/500 intervention received additional Family Check Up component | No overall effect; 'The correlations reveal that, in general, random assignment to the intervention condition was not significantly correlated with problem behaviors over time.' However 'engagement with a family‐centered intervention reduced the risk for problem behaviors from early to late adolescence, including antisocial behavior and tobacco, alcohol and marijuana use.' using CACE modelling to match engagers with similar controls. Treatment predicted significantly less growth in tobacco use, although the intervention effect diminished over time. The effect size for the difference in estimated tobacco use at age 22 for the engagers in the intervention vs. control condition was large (reported in Connell 2009) |
| Dishion 1995 | Pre‐test: 119 families randomly assigned to 4 family therapy treatment groups to "reduce escalation in problem behaviors among high‐risk adolescents" and a control condition, followed for one year | Results reported as Frequency (Log + 1). The F ratios report an N of 140, which includes all intervention groups and the non‐random control and thus the probabilities reported in the text are not reported here. Parent‐only baseline 0.91, 1 year follow‐up 0.63 Teen only Baseline 0.81, 1 year follow‐up 1.66 Parent and teen baseline 0.95, 1 year follow‐up 2.09 Self‐directed baseline 0.75, 1 year follow‐up 1.16. |
| Olds 1998 | 400 pregnant women randomised to different types of antenatal & postnatal support until child's 2nd birthday. Follow‐up at 15 years | No differences reported in amount of cigarette use in past 6 months between any groups |
| Riesch 2012 | 167 parent‐youth dyads recruited from elementary schools in Madison, Wisconsin and Indianapolis, Indiana, and randomised to the Strengthening Families Program 10‐14 (SFP 10‐14) or data collection only | No baseline smoking data. Abstract states: "Youth participation in alcohol, tobacco, and other drugs was very low and did not differ post program." There was attrition in the intervention group from 87 to 63 and in the control from 81 to 66 and post program data for "smoked a cigarette, even a puff" are incomplete. |
| Medium intensity family intervention | ||
| Fang 2013 | Pre‐test: 108; at 2‐years 93 | No evidence of effect: 'The intervention, however, did not exert significant effect on girls’ cigarette use over time.' 30‐day cigarette use, mean (SD): Intervention 0.02 (0.14), Control 1.95 (9.87), p = 0.171 |
| Schinke 2004 | 514 10‐12 year olds | No evidence of additional effect of parent component over CD based intervention. Past 30 day cigarette use CD + parent group; pretest 0.6, 3y 0.8. CD; pretest 0.6, 3y 0.9. Control; pretest 0.7, 3y 1.3; (p < .05 for both intervention groups compared to control) |
| Low intensity family intervention | ||
| Stevens 2002 | 12 paediatric practices in New England approached 4,096 families and recruited 85% (n= 3525) of their 5th and 6th grade children and their parents; 3094 completed the baseline assessment and 2173 (70%) child‐parent pairs completed the 36 month follow‐up. | At baseline 5.4% of children in the alcohol and tobacco intervention and 4.6% in the gun safety, bicycle helmet and set belt use safety intervention group had ever smoked (n.s.). No control group. At 36 months follow‐up there were no significant differences in having ever smoked, OR = 0.97 (95% CI 0.79 to 1.20), P = 0.78. |
| Wu 2003 | 800 African‐American youth 13‐16 years. (1) Focus on Kids (FOK): 8 session (each 1.5 hours) HIV small‐group risk reduction programme on decision making, goal setting, communicating, negotiating, and consensual relationships and information regarding safe sex, drugs, alcohol and drug selling. Conducted in small groups (5‐10), no parent participation. (2) (a) FOK + (b) ImPACT (Informed Parents and Children Together): 20‐min video emphasising concepts of parental monitoring and communicating with 2 instructor‐led role‐playing vignettes between the parent and youth in the child's home. The interventionist critiques the role play according to the main talking points of the videotape and conducts a condom demonstration. (3) (a) FOK + (b) 4 FOK booster sessions at 6m and 10m + (c) + ImPACT Focus on Kids has a minor informational component about tobacco and no family component. ImPACT is 20 minute video followed by role plays between parent and youth, then criticised by interventionist. It has no tobacco focus, but baseline and 24 months smoking were measured for all 3 programmes. ImPACT assessed as low intensity. |
At 24 months the past 6 month smoking rate was significantly lower (P = .003) in the ImPACT family intervention group (+/‐FOK boosters), 12.5%, than the FOK control, 22.7% in the risk reduction intervention (Focus on Kids) is 22.7% and in the combined ImPACT (Informed parents and Children Together) groups is 12.5% Table 1 shows baseline smoking rates for those who remained in the study at 24 months were 27% in the FOK and 23% in the ImPACT group, implying smoking rates decreased for both intervention groups at 24 months (data from Stanton 2004). . |
Analysis 2. Combined family plus school intervention compared to school intervention
Two studies (Jøsendal 1998 and Spoth 2002, 2301 participants at follow‐up) evaluated the effect of a family intervention added to a school‐based intervention and reported suitable data for meta‐analysis. There was evidence of a benefit of the additional intervention over the school component alone (RR 0.85, 95% CI 0.75 to 0.96, Analysis 2.1), with Jøsendal 1998 detecting a significant benefit.
2.1. Analysis.
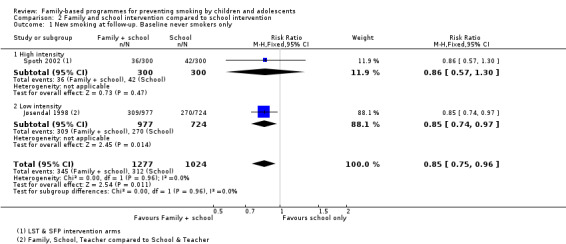
Comparison 2 Family and school intervention compared to school intervention, Outcome 1 New smoking at follow‐up. Baseline never smokers only.
One high intensity intervention study (Guilamo‐Ramos 2010, 1096 participants) provided data for meta‐analysis but included some participants who already had experience of smoking at baseline. There was evidence of a benefit of the additional intervention over the school component alone (RR 0.60, 95% CI 0.38 to 0.94, Analysis 2.2).
2.2. Analysis.
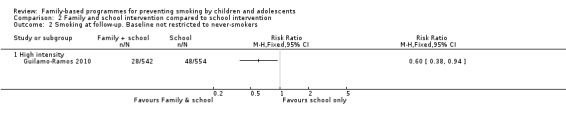
Comparison 2 Family and school intervention compared to school intervention, Outcome 2 Smoking at follow‐up. Baseline not restricted to never‐smokers.
Five studies (approximately 18,500 participants) evaluated the effect of a family intervention added to a school‐based intervention, but did not report outcomes in a format suitable for inclusion in the meta‐analysis. Effects are summarised in Analysis 2.3. One used a high intensity intervention (Forman 1990), one a medium intensity intervention (Elder 1996) and three a low intensity intervention (Ary 1990; Biglan 1987; Reddy 2002). None of these studies reported significant effects.
2.3. Analysis.
Comparison 2 Family and school intervention compared to school intervention, Outcome 3 Smoking at follow‐up. Results not in meta‐analysable format.
| Smoking at follow‐up. Results not in meta‐analysable format | ||
|---|---|---|
| Study | Number of participants | Results |
| High intensity interventions | ||
| Forman 1990 | Baseline: 279 students in 30 schools completed 20 hour training programme and pre and post‐treatment assessment sessions; 201 completed booster and 1 year assessment | At 1 year, no significant differences in mean* cigarette use: School Intervention pretest mean = 2.90, 1 year follow‐up = 3.02 School + parent intervention pretest mean = 2.81, 1 year follow‐up = 2.95 School + parent intervention (parent attended no sessions) pretest mean = 2.84, year follow‐up = 2.81 Control pretest mean 2.83, 1 year follow‐up = 2.93 *Frequency of cigarette use averaged over groups: never = 1, used to but quit = 2, a few a month = 3, a few a week = 4, every day = 5. |
| Medium intensity interventions | ||
| Elder 1996 | Eligibles; all 3rd grade children 1991‐1 (n not stated) . Average of 9087 children evaluated 1992‐1994, and 7,827 at 36 months (at end of 5th grade) of whom 6,527 gave complete information. | At 3 years no significant differences in the percentages in the experimental (4.7%) and control groups (5%) stating that they had ever smoked (OR = 1.01, 95% CI 0.79‐1.30). No evidence provided of any effects from adding the family "Unpuffables" intervention to the school intervention |
| Low intensity interventions | ||
| Ary 1990 | Pre‐test: 7,837 1 year: 6,263 completed assessments at baseline and one year | After 1 year there were no effects of the messages to parents. "The children of parents who received the parent messages as part of the experimental evaluation of this component did not differ significantly in their levels of smoking or smokeless tobacco use from those whose parents did not receive parent messages." |
| Biglan 1987 | Pre‐test:3,387; at one year 2,391 | At 1 year there were no effects of the messages to parents . "The provision of parent messages did not affect outcome". |
| Reddy 2002 | Randomised to Project HRIDAY (Health‐Related Informantion and Dissemination Among Youth) (n = 1439) or to School/Family Intervention (n = 1863) or control. Family intervention consisted of six booklets taken home to parents, only one of which discussed tobacco | At posttest there was no significant difference between the school+family and the school alone condition, although both intervention conditions were significantly different to control (p < .01). ‘The family based program did not appear to significantly add to outcomes’. Mean score at posttest for question ‘Have you ever tried a cigarette/bidi’, 1=Yes. School + Family .0366 (95% CI .0264 to .0504); School .0571 (.0422 to .0768); Control .0937 (.0728 to .1198). Increase in score from pre‐ to posttest was smaller for School + Family than other conditions but CIs wide and no statistical test reported. |
Analysis 3. Other comparisons
One trial (Storr 2002) contributing to Analysis 1 also had a school‐based comparison arm. The family‐school partnership arm and the classroom centred 'Good Behavior Game' arms had similar effects on behaviour (RR 1.05, 95% CI 0.80 to 1.38, n = 388, Analysis 3.1).
3.1. Analysis.
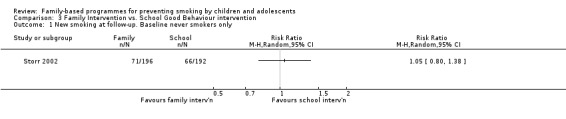
Comparison 3 Family Intervention vs. School Good Behaviour intervention, Outcome 1 New smoking at follow‐up. Baseline never smokers only.
Discussion
Summary of main results
We divided studies into two groups. The first group evaluated family‐based interventions used on their own, compared to a no‐intervention control. The second group evaluated family‐based interventions used as adjuncts to school‐based prevention interventions; these were compared to school‐based interventions alone. Pooling nine trials with baseline never‐smokers (six trials used a high, one a medium and two a low intensity intervention) found fewer participants in the intervention arms began smoking than those in no‐intervention control groups. Pooling two trials with baseline never‐smokers comparing a family intervention plus a school intervention to a school intervention alone (one high and one low intensity) found fewer participants in the combined arms began smoking than those only receiving the school‐based programmes. No study reported any possible harms from the interventions.
Thus, there was moderate quality evidence of benefit for family interventions used on their own, and when used as adjuncts to school interventions. For stand alone interventions, a family intervention might reduce new smoking behaviour, including experimenting or trying 'just a puff', by between 16 and 32%. Based on an average prevalence of new smoking across study control groups of 230 per 1000 this would translate to a reduction to between 156 and 193 per 1000 with the intervention (Table 1). However, the prevalence of new smoking that occurred by the time of follow‐up differed across studies and the absolute effect of an intervention would depend on the setting. For interventions used as adjuncts to school programmes the estimated benefit would be a reduction in new smoking behaviour of between 4 and 25%. Based on the same assumed control group rate of 230 per 1000 this would translate to a reduction in new behaviour to between 172 and 221 per 1000 from the addition of a family component to a school intervention (Table 2).
The common feature of the effective high intensity interventions was encouraging authoritative parenting (interest in and care for the adolescent, often with rule setting). Cullen 1996 used 12 visits by a general practitioner with new mothers to enhance self‐worth, self‐acceptance, foster gentle physical interaction with her child, and adopt a positive attitude to modifying her child's behaviour. Fosco 2013 provided a Family Resource Center in schools and a consultant used motivational interviewing to identify family strengths and weaknesses, motivate parents to improve parenting and engage in intervention services tailored to the unique needs of each family. Haggerty 2007 provided telephone facilitator support as parents and teens worked through a workbook to identify risks and reduce them, bond with the teen, solve family problems, set family policies and supervise without invading. Prado 2007 provided an intervention to strengthen Hispanic family‐centred values and increase parental involvement, positive parenting and family support. Spoth 2001 provided sessions for parents and children to strengthen parental skills in nurturing, setting limits and communication about substances, and strengthen children's prosocial and peer resistance skills. Storr 2002 provided workshops to facilitate children's learning and behaviour and focus on effective disciplinary strategies. In a medium intensity intervention Bauman 2001 sent Family Matters booklets to parents and a health educator telephoned a parent, encouraged the participation of all family members in the programme and answered questions.
The common feature of the effective high intensity interventions used as adjuncts to school interventions was again encouraging authoritative parenting. Guilamo‐Ramos 2010 encouraged parents to think they could make a difference in their adolescent's tobacco‐related behaviour, including strategies for effective communication, topics parents might consider discussing in their conversations with their adolescents, the importance of setting limits, and ways to resist peer pressure. Spoth 2002 encouraged parents to strengthen their skills in nurturing, setting limits and communicating about substances, and strengthen their children's prosocial and peer resistance skills. The classroom intervention in Jøsendal 1998 focused on personal freedom, the freedom to choose, freedom from addiction, and making one's own decisions and the low intensity family component focused on teachers involving parents in discussions and students signing non‐smoking contracts.
Overall completeness and applicability of evidence
The key purpose of the review is to assess whether interventions in families prevent adolescent smoking, and we did find 27 trials that addressed this question. However, only half (fourteen) were meta‐analysable. Twelve of the 13 that were not meta‐analysable found no significant results. The evidence is predominantly from the USA (23 trials), two from Europe, one from India and one from Austaalia. The evidence is thus mainly from one country on one continent. One trial studied children as young as five, and most trials focused on adolescents aged 11‐18. Few studies analysed data separately by gender. We were unable to test whether socio‐economic characteristics may have confounded the results, as there were too few studies and details within the studies to determine whether the effects of the intervention were related to socio‐economic characteristics. However, randomisation should have prevented differential confounding.
Quality of the evidence
The review identified twenty seven studies RCTs involving over 36,000 participants. Many studies were rated as unclear for most risk of bias domains. For this reason we downgraded the quality of evidence for all outcomes to moderate. Only 14 of the studies had outcomes reported in a way that could be extracted for meta‐analysis, and these studies only included about a third of the participants. All but one of the non‐meta‐analysable studies reported non significant effects on tobacco use, but the direction of effect favoured the intervention arm in all cases that gave data. However it is possible that this group of studies had smaller effects than those includable in the meta‐analysis. Although there multiple possible sources of heterogeneity there was little evidence of statistical heterogeneity. Most studies had point estimates indicative of small benefits of interventions.
A limitation may have been combining interventions with differing aims (e.g., tobacco compared to bicycle helmet, gun and seatbelt safety) and that these unrelated aims caused 'noise' which masked the basic message to prevent smoking. It is possible that some of the combination studies might have shown larger effects if they had limited themselves to a strong tobacco intervention.
Unrecorded co‐interventions may have occurred during the study, reducing the apparent effect of the family intervention. Possible co‐interventions could include other mandated school anti‐smoking programmes, social marketing campaigns using mass media, restriction of smoking locations, enforcement of legislation to prohibit the sale and supply of tobacco to those under 18, increasing taxation and cost of cigarettes, and changes in tobacco promotion by tobacco companies. Another possible confounder was the selection of schools because the teachers were enthusiastic, and although the schools may later have been randomised (as in Biglan 1987) the co‐intervention of teacher enthusiasm could augment the effect of the school component. Most of the studies do not report co‐interventions, and if these operated effectively during the study an incremental effect of the family intervention may not have been perceptible.
Potential biases in the review process
There were no limitations of date or language in the literature search, and all titles, abstracts and full‐texts were read independently, and data entered independently by two reviewers. Each study was read on multiple occasions and data verified. We did not receive replies to some of our requests for baseline never‐smoking cohorts from some authors.
The studies span the period 1990‐2014, and trial methodology, analysis and reporting changed over the period. However, some recent studies presented data in non‐metanalysable format.
Agreements and disagreements with other studies or reviews
There are no other systematic reviews focusing on family interventions to prevent smoking. A systematic review (Petrie 2007) identified 16 RCTs, three controlled before and after (CBA) studies and one controlled trial about parenting programmes to prevent tobacco, alcohol or drugs misuse by children under 18 years. They included only seven of the RCTs we identified (Bauman 2001; Forman 1990; Jackson 2006; Jøsendal 1998; Spoth 2001; Spoth 2002; Storr 2002), and our review excluded four of the RCTs they included (Lochman 2002 (because there was no tobacco intervention) and Johnson 1990, Perry 2003 and Severson 1991 (because the effects of the family intervention could not be separated from those of the school intervention). The authors did not conduct a meta‐analysis, but concluded that parenting programmes can be effective in preventing substance use, and noted that more research is needed in this area. A U.S. Preventive Services Task Service review of primary care interventions to prevent adolescent smoking (Patnode 2012) identified some of the family RCTs we identified, and concluded that behaviour‐based prevention interventions could prevent smoking; these findings are not directly comparable with ours due to the wide range of behavioural interventions considered. In general, although parents are important in influencing smoking by children and adolescents, most interventions have focused directly on youth in schools (Thomas 2013) and there are fewer RCTs of family interventions. This may reflect the difficulties of conducting interventions in families.
Previous literature reviews that have not focused on trials have identified the contribution of family, individual and social factors in adolescent smoking, and have also identified several problems in studying how families influence adolescent smoking. Darling 2003 noted three problems in identifying the causes of adolescent smoking: the transitional nature of adolescent smoking, the multiple forms of family structure and influences, and the relationship of families to other developmental processes. Avenevoli 2003 identified 87 studies of the relationship between adolescent and parental or sibling smoking, of which 43 assessed smoking by both parents and siblings. Most studies were of US Caucasian students. The studies lacked standardized instruments, did not measure important confounding and mediating variables (smoking‐specific socialization practices, and the influences of parents on their children's health beliefs, choice of peers, susceptibility to peer pressure, values, and association with peers who smoke), and used cross‐sectional designs. Avenevoli was able to identify only five methodologically rigorous studies, and noted that when effects of parental smoking are found the odds ratios are generally less than 2.0, and the effects are often eliminated when other variables are included in models. Most studies of siblings predict current and life‐time smoking by adolescents. Mayhew 2000 identified 11 cross‐sectional studies and found that adolescent smoking was associated with individual factors (male, Caucasian, positive attitudes to smoking, concerns with body weight, affect regulation, and cigarette availability); family factors (number of family members who smoke, perceptions of parental permissiveness and approval of smoking); and the number of friends in the adolescent's network who smoked, but these cross‐sectional studies are methodologically weak in assessing a developmental process. Mayhew identified 19 prospective studies which aggregated the experimenting, regular and established smokers into one group and identified individual factors (number of cigarette offers, beliefs about the positive functions of smoking, minimization of risks, intentions to smoke, tolerance for deviance and drug use, and high estimates of smoking prevalence); family factors (parents and siblings who smoked, and the level of parental involvement and support); and non‐family factors (number of friends who smoked, approval of smoking by friends, low academic expectations by friends, and a commitment to part‐time work while in school). Nine prospective studies that identified discrete stages of smoking found that smoking by parents, family, and best friend, and school performance were factors that predicted moving from non‐smoking to experimenting; and positive intentions to smoke and lack of commitment not to smoke were related to the transitions between non‐smoking and experimenting and experimenting and regular use. Seven developmental studies which specifically tried to study the development of smoking stages found that for individual factors positive attitudes to smoking predicted high initial rates of smoking and faster rates of smoking; high estimates of the prevalence of tobacco use and alcohol use predicted the transition from trying to experimenting; and marijuana use predicted transitions from non‐smoking to trying, trying to experimenting, and experimenting to regular use. For family factors, having parents who smoked predicted the transition from non‐smoking to experimenting, and parental divorce predicted the transition from non‐smoking to regular smoking. For non‐family factors the number of peers who smoked predicted the transitions from never to trying and from trying to experimenting. Tyas 1998 found that adolescent smokers who begin at younger ages are more likely to become regular smokers and less likely to quit; parental indifference, lack of supervision and lack of knowledge about their children's friends increases the risk of smoking, as does the perception that friends smoke. Participating in sports is associated with lower rates of smoking.
Authors' conclusions
Implications for practice.
The evidence of this review shows that family‐based interventions have the potential to prevent children and adolescents from starting to smoke. There was more evidence that high intensity programmes were likely to be effective because more studies used interventions that were classified as high intensity, but there was not strong evidence of a dose response.
The implications for practice are to choose one of these authoritative parenting interventions most suited to the families who may be involved and the intervention resources available. Given the heterogeneity in the intervention and settings, caution is warranted. When implemented, it may be important monitor both implementation integrity and outcomes.
Implications for research.
The implications for research are to conduct focus groups to assess how the theoretically best grounded interventions with significant results identified in the meta‐analysis could be further improved and then test them head‐to‐head and against a control group. Consortia of researchers could collaborate to test them in fully powered trials with different adolescent and family populations, carefully executed with minimal attrition, maximum programme fidelity and analysed to assess any effects of clustering. The majority of studies were undertaken in the USA and studies in other countries and including their different cultural groups are much needed. The inclusion of an economic evaluation would be useful in understanding the potential cost‐effectiveness of the interventions.
What's new
| Date | Event | Description |
|---|---|---|
| 6 January 2015 | New citation required and conclusions have changed | Eight new RCTs added, three studies in the 2008 version re‐assessed and excluded. Studies that reported data in suitable format now pooled in meta‐analysis, moderate quality evidence of benefit for some subgroups. |
| 6 January 2015 | New search has been performed | Searches updated. All the RCTs in the 2008 version have been re‐assessed and risk of bias tables expanded. Abstract, Plain Language Summary, Results, Conclusions, and Recommendations for Practice and Research sections rewritten, Background updated and Risk of Bias graphs added. |
History
Protocol first published: Issue 4, 2003 Review first published: Issue 1, 2007
| Date | Event | Description |
|---|---|---|
| 12 August 2014 | Amended | Third edition (see "What's new" above). |
| 18 December 2007 | New search has been performed | Updated for 2008 issue 2, with two new included studies (Forman 1990 and Connell 2007) and 14 new excluded trials. Conclusions strengthened but unchanged. |
Notes
None
Acknowledgements
We thank David Olds, Cheryl Perry and Nicholas Ialongo for additional data and clarification Paul Aveyard and Bruce Simons‐Morton for commenting on an earlier version of this review, and Tim Lancaster, Lindsay Stead and Monaz Mehta for excellent editorial support. For this edition of the review we thank Dr. Lin Fang, Dr. John Pierce, Dr. Beth Stormshak and Dr. Sharlene Wolchik (for data for Soper 2010).
Appendices
Appendix 1. MEDLINE search strategy
Term Set #1 adolescen*[Text Word] OR child[Text Word] OR children[Text Word] OR childhood[Text Word] OR juvenile*[Text Word] OR teen*[Text Word] OR youth*[Text Word] OR Adolescent[MESH:NOEXP] OR child[MESH:NOEXP]
Term Set #2 Parents[Mesh] OR parent*[Text Word] OR "family member*"[Text Phrase] OR father*[Text Word] OR mother*[Text Word] OR classroom*[Text Word] OR "elementary school*"[Text Phrase] OR "high school*"[Text Phrase] OR community[Text Word] OR communities[Text Word] OR school*[Text Word] OR home[Text Word] OR "home based"[Text Phrase] OR family[Text Word] OR families[Text Word] OR "community based"[Text Phrase] OR "family based"[Text Phrase] OR family[MESH] OR family therapy[MESH] OR family health[MESH] OR schools[MESH]
Term Set #3 ((cigarette* OR smoking OR tobacco[Text Words]) AND (cessation OR quit* OR stop* OR prevent OR preventing OR prevention OR intervention*[Text Words])) OR Tobacco Use Cessation[MESH] OR tobacco use disorder/prevention and control[Mesh] OR Smoking Cessation[MESH] OR smoking/prevention and control[MESH:NOEXP]
Term Set #4 single blind method[Mesh] OR random allocation[Mesh] OR ((double OR single OR triple OR treble[Text Words]) AND (blind* OR mask*[Text Words])) OR rct*[Text Word] OR (random*[Text Word] AND (trial OR trials OR allocat* OR assign* OR control[Text Words])) OR randomized controlled trials[Mesh] OR double blind method[Mesh] OR randomized controlled trial[Publication Type]
BIBLIOGRAPHIC DATABASES
CBCA Fulltext Education Index CINAHL Cochrane Controlled Trials Register Cochrane Tobacco Addictions Group Register DARE Database of Reviews of Effectiveness EBSCO Sociological Collection EMBASE ERIC (also a grey literature source) MEDLINE PsycINFO Social Sciences Abstracts Sociological Abstracts Web of Science (Science & Social Science Citation Indexes) Wilson Education Fulltext
GREY LITERATURE DATABASES
Australian Policy Online: http://www.apo.org.au/ BioMed Central (online peer reviewed journal articles, incl rcts): http://www.biomedcentral.com/rct/ BioMedNet (conferences reporter): http://news.bmn.com/conferences Campbell Collaboration (systematic reviews of social, psychological and educational interventions): http://www.campbellcollaboration.org/ Canadian Research Index (Government policy & research reports and theses) CABOT Canadian Health Research Database: http://www.mycabot.ca/cgi‐bin/WebObjects/cabot CenterWatch Clinical Trials Listing Service: http://www.centerwatch.com/ Clinicaltrials.gov: http://clinicaltrials.gov/ct/gui/c/b Current Controlled Trials: http://www.controlled‐trials.com/ Digital Dissertations (Doctoral dissertations and master's theses worldwide) EDResearch Online (Australian educational database): http://cunningham.acer.edu.au/dbtw‐wpd/sample/edresearch.htm GrayLit Network (database of U.S. Federal gray literature documents): http://www.osti.gov/graylit/ Health Promotion and Education Database (National Center for Chronic Disease Prevention and Health Promotion): http://outside.cdc.gov:8085/BASIS/ccdchid/web/hes/sf HealthPromis (health promotion database that includes both published and grey literature: http://healthpromis.hda‐online.org.uk/ Health Technology Assessment Database ‐ Univ of York: http://nhscrd.york.ac.uk/ Index to Theses (Grey literature doctoral/masters theses from British and Irish universities) Moving Ideas Electronic Policy Network (Database of policy reports produced by research agencies in the U.S.: http://movingideas.org/ideas/subjects/environment‐1.html National Library of Medicine LocatorPlus (Catalogue of books & reports held by the National Library of Medicine: http://gateway.nlm.nih.gov/gw/Cmd Papers First (Indexes papers given at congresses, conferences, symposia, and meetings) Policy Library (Database of international healthcare, public health and health systems policy reports: http://www.policylibrary.com/health/ Proceedings First (Tables of contents of proceedings from congresses, conferences,expositions, workshops, symposia, and meetings. Social Science Research Network: http://www.SSRN.Com/ Trials Central: http://www.trialscentral.org/ UK National Research Register. Clinical Trials Directory: http://www.update‐software.com/National/ University of Laval E‐Watch Bulletin & database on knowledge utilization: http://kuuc.chair.ulaval.ca/english/index.php U.S. Grey Literature Report: http://www.nyam.org/library/greylit/ U.S. National Technical Information Service (a major source of U.S. grey literature): http://www.ntis.gov/ TRIP Evidence Based Medicine Database: http://www.tripdatabase.com/index.cfm World Health Organization Library Catalogue: http://www.who.int/dsa/ WorldCat (Joint catalogue of materials held by libraries worldwide)
INTERNET SITES
Canadian Organizations: The Alberta Consortium for Health Promotion Research and Education: http://www.health‐in‐action.org/new/Consort/consort.shtml Atlantic Health Promotion Research Centre: http://www.medicine.dal.ca/ahprc/ Canadian Consortium for Health Promotion Research: http://www.utoronto.ca/chp/chp/consort/introe.htm Canadian Institutes of Health Research: http://www.cihr‐irsc.gc.ca/ Canadian Provinical/Territorial Ministries of Health Canadian Public Health Association http://www.cpha.ca/ Health Canada. Health Promotion Online http://www.hc‐sc.gc.ca/english/for_you/hpo/index.html Institute of Health Promotion Research, University of B.C. http://www.ihpr.ubc.ca/ National Clearinghouse on Tobacco and Health http://www.ncth.ca/NCTHweb.nsf Prairie Region Health Promotion Research Centre, University of Saskatchewan http://www.usask.ca/healthsci/che/prhprc/ International Organizations: American Public Health Association http://www.apha.org/ Centers for Disease Control and Prevention http://www.cdc.gov/ Centre for Health Program Evaluation (AU) http://chpe.buseco.monash.edu.au/ Global Tobacco Prevention and Control http://www.cdc.gov/tobacco/global/ International Department of Health Web Sites: Health Promotion HotLinks http://www.web.net/˜stirling/#anchor69179 International Health Promotion Research Links http://www.phs.ki.se/hprin/ International Institute for Health Promotion http://www.american.edu/academic.depts/cas/health/iihp/iihpabout.html Monash University Health Promotion Unit http://www.med.monash.edu.au/healthpromotion/ National Centre for Social Research http://www.scpr.ac.uk/ Stanford Center for Research in Disease Prevention http://prevention.stanford.edu/ World Health Organization http://www.who.int/en/
Appendix 2. Databases and web sites searched
BIBLIOGRAPHIC DATABASES
CBCA Fulltext Education Index CINAHL Cochrane Controlled Trials Register Cochrane Tobacco Addictions Group Register DARE Database of Reviews of Effectiveness EBSCO Sociological Collection EMBASE ERIC (also a grey literature source) MEDLINE PsycINFO Social Sciences Abstracts Sociological Abstracts Web of Science (Science & Social Science Citation Indexes) Wilson Education Fulltext
GREY LITERATURE DATABASES
Australian Policy Online: http://www.apo.org.au/ BioMed Central (online peer reviewed journal articles, incl rcts): http://www.biomedcentral.com/rct/ BioMedNet (conferences reporter): http://news.bmn.com/conferences Campbell Collaboration (systematic reviews of social, psychological and educational interventions): http://www.campbellcollaboration.org/ Canadian Research Index (Government policy & research reports and theses) CABOT Canadian Health Research Database: http://www.mycabot.ca/cgi‐bin/WebObjects/cabot CenterWatch Clinical Trials Listing Service: http://www.centerwatch.com/ Clinicaltrials.gov: http://clinicaltrials.gov/ct/gui/c/b Current Controlled Trials: http://www.controlled‐trials.com/ Digital Dissertations (Doctoral dissertations and master's theses worldwide) EDResearch Online (Australian educational database): http://cunningham.acer.edu.au/dbtw‐wpd/sample/edresearch.htm GrayLit Network (database of U.S. Federal gray literature documents): http://www.osti.gov/graylit/ Health Promotion and Education Database (National Center for Chronic Disease Prevention and Health Promotion): http://outside.cdc.gov:8085/BASIS/ccdchid/web/hes/sf HealthPromis (health promotion database that includes both published and grey literature: http://healthpromis.hda‐online.org.uk/ Health Technology Assessment Database ‐ Univ of York: http://nhscrd.york.ac.uk/ Index to Theses (Grey literature doctoral/masters theses from British and Irish universities) Moving Ideas Electronic Policy Network (Database of policy reports produced by research agencies in the U.S.: http://movingideas.org/ideas/subjects/environment‐1.html National Library of Medicine LocatorPlus (Catalogue of books & reports held by the National Library of Medicine: http://gateway.nlm.nih.gov/gw/Cmd Papers First (Indexes papers given at congresses, conferences, symposia, and meetings) Policy Library (Database of international healthcare, public health and health systems policy reports: http://www.policylibrary.com/health/ Proceedings First (Tables of contents of proceedings from congresses, conferences,expositions, workshops, symposia, and meetings. Social Science Research Network: http://www.SSRN.Com/ Trials Central: http://www.trialscentral.org/ UK National Research Register. Clinical Trials Directory: http://www.update‐software.com/National/ University of Laval E‐Watch Bulletin & database on knowledge utilization: http://kuuc.chair.ulaval.ca/english/index.php U.S. Grey Literature Report: http://www.nyam.org/library/greylit/ U.S. National Technical Information Service (a major source of U.S. grey literature): http://www.ntis.gov/ TRIP Evidence Based Medicine Database: http://www.tripdatabase.com/index.cfm World Health Organization Library Catalogue: http://www.who.int/dsa/ WorldCat (Joint catalogue of materials held by libraries worldwide)
INTERNET SITES
Canadian Organizations: The Alberta Consortium for Health Promotion Research and Education: http://www.health‐in‐action.org/new/Consort/consort.shtml Atlantic Health Promotion Research Centre: http://www.medicine.dal.ca/ahprc/ Canadian Consortium for Health Promotion Research: http://www.utoronto.ca/chp/chp/consort/introe.htm Canadian Institutes of Health Research: http://www.cihr‐irsc.gc.ca/ Canadian Provinical/Territorial Ministries of Health Canadian Public Health Association http://www.cpha.ca/ Health Canada. Health Promotion Online http://www.hc‐sc.gc.ca/english/for_you/hpo/index.html Institute of Health Promotion Research, University of B.C. http://www.ihpr.ubc.ca/ National Clearinghouse on Tobacco and Health http://www.ncth.ca/NCTHweb.nsf Prairie Region Health Promotion Research Centre, University of Saskatchewan http://www.usask.ca/healthsci/che/prhprc/ International Organizations: American Public Health Association http://www.apha.org/ Centers for Disease Control and Prevention http://www.cdc.gov/ Centre for Health Program Evaluation (AU) http://chpe.buseco.monash.edu.au/ Global Tobacco Prevention and Control http://www.cdc.gov/tobacco/global/ International Department of Health Web Sites: Health Promotion HotLinks http://www.web.net/˜stirling/#anchor69179 International Health Promotion Research Links http://www.phs.ki.se/hprin/ International Institute for Health Promotion http://www.american.edu/academic.depts/cas/health/iihp/iihpabout.html Monash University Health Promotion Unit http://www.med.monash.edu.au/healthpromotion/ National Centre for Social Research http://www.scpr.ac.uk/ Stanford Center for Research in Disease Prevention http://prevention.stanford.edu/ World Health Organization http://www.who.int/en/
Data and analyses
Comparison 1. Family intervention versus non intervention control group.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 New smoking at follow‐up. Baseline never smokers only | 9 | 4810 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.68, 0.84] |
| 1.1 High intensity family intervention | 6 | 1970 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.61, 0.82] |
| 1.2 Medium intensity family intervention | 1 | 826 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.67, 1.03] |
| 1.3 Low intensity family intervention | 2 | 2014 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.61, 0.97] |
| 2 Smoking at follow‐up. Baseline not restricted to never‐smokers | 2 | 4487 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.93, 1.17] |
| 2.1 High intensity family intervention | 1 | 935 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.82, 1.11] |
| 2.2 Low intensity family intervention | 1 | 3552 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.94, 1.33] |
| 3 Smoking at follow‐up. Results not in meta‐analysable format | Other data | No numeric data | ||
| 3.1 High intensity family intervention | Other data | No numeric data | ||
| 3.2 Medium intensity family intervention | Other data | No numeric data | ||
| 3.3 Low intensity family intervention | Other data | No numeric data |
Comparison 2. Family and school intervention compared to school intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 New smoking at follow‐up. Baseline never smokers only | 2 | 2301 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.75, 0.96] |
| 1.1 High intensity | 1 | 600 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.57, 1.30] |
| 1.2 Low intensity | 1 | 1701 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.74, 0.97] |
| 2 Smoking at follow‐up. Baseline not restricted to never‐smokers | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 High intensity | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Smoking at follow‐up. Results not in meta‐analysable format | Other data | No numeric data | ||
| 3.1 High intensity interventions | Other data | No numeric data | ||
| 3.2 Medium intensity interventions | Other data | No numeric data | ||
| 3.3 Low intensity interventions | Other data | No numeric data |
Comparison 3. Family Intervention vs. School Good Behaviour intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 New smoking at follow‐up. Baseline never smokers only | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ary 1990.
| Methods | Study design: C‐RCT. Schools matched on urban/rural status, level of tobacco use, ethnicity and school size, then randomised. In the 12 intervention schools, parents randomised to receive (n = 509) or not receive (n = 400) parent messages. No power computation. Analysis: ANCOVA. Total study duration: 1 year |
|
| Participants | Total number: 4891 parents randomised to receive 3 parent messages. At baseline 7837 elementary, middle and high school students provided questionnaire and biochemical data; 6263 of these provided follow‐up data 9‐12 months later. In one school district with 12 schools 509 parents received 3 parent messages and 400 did not and in 2 other school districts 4382 parents received 3 parent messages.. Setting: 22 middle/elementary & 15 high schools from 13 districts in Oregon, USA. Age 6‐11th graders; Gender not stated. |
|
| Interventions | Focus: tobacco, alcohol and marijuana prevention Intervention (1): Project PATH (Programs to Advance Teen Health) Components: At each grade level (a) awareness of social influences to engage in substance use (b) refusal skills training (c) health facts, and (d) contracting not to use cigarettes and other substances. Duration: 25 classroom sessions (5 in each of grades 6 through 10), typically taught over a 1 week period ('focused most heavily on cigarette smoking and smokeless tobacco use, it was designed to deter the use of marijuana and alcohol'). Sessions taught by classroom teachers (who received 2 to 3 hours of training), and in grades 7 and 9 by peers nominated by their classmates. Program different for each grade. Intervention (2): (a) PATH + (b) "Three brochure‐like messages were mailed on separate occasions to parents ... designed to support components of the classroom intervention, including refusal skills, health effects information and commitment not to smoke or chew." (low intensity) (3) Control: typically received 10 classroom sessions of standard tobacco/drug use education. (Outcomes not considered for this review) |
|
| Outcomes | Smoking: Pechacek's self‐reported smoking index to yield an estimate of the no. cigs smoked in last month (composite of no. in last 6m, last month, last week, and last 24 hours): Dichotomised on >1 cig in previous month. Expired air CO tested before survey completion. Follow‐up: 9‐12m after pre‐test. Only results for grades 6‐9 given in Ary 1990 | |
| Notes | Performance bias: No assessment whether letters to parents received or read. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | In 12 intervention schools 509 parents randomly assigned to receive and 400 to not receive messages (imbalanced group numbers) and in the other intervention schools all 4382 parents received messages. Method of randomisation not specified. Schools were blocked on urban/rural status then tobacco and drug use, ethnicity and school size. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information as to whether parents aware of alternate conditions or whether contamination could occur |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information given for receipt of parental messages |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Unclear risk | Family intervention consisted of letters to parents at their homes, so no adjustment for clustering needed for this intervention component. However, no adjustment for clustering in the school intervention |
Bauman 2001.
| Methods | Study design: RCT. 64,811 telephone numbers representative of all telephone numbers in the US; then by random digit dialling found 2,395 (3.7%) where there was a household with an eligible adolescent age 12‐14 and parent pair; then randomised to intervention or control. No power computation. Analysis: GEE Total study duration: follow‐up 12 months after completion of program |
|
| Participants | Total number: Of 2395 eligibles, 1,326 (55%) completed a baseline interview, and of these 549 (46%) began the program, and 407 (34%) completed. Setting: National telephone survey, USA; Age 12‐14; Gender not stated. |
|
| Interventions | Focus: tobacco and alcohol prevention Intervention: The Family Matters intervention: 4 booklets mailed to participants: (a) booklet 1: discuss the consequences to the family of adolescent tobacco or alcohol use; (b) booklet 2: record normal adolescent behaviours, and understand the importance of supervision, support, communication skills, attachment and conflict resolution (c) booklet 3: list parental behaviours that might encourage substance abuse, identify rules that could influence their child's substance use, monitor use, and agree on rules and sanctions for substance use; (d) booklet 4: adults and adolescents to consider what the adolescent could do to resist peer and media pressures to use substances, to practise refusals of tobacco and alcohol, and to watch favourite TV shows together to discuss the messages of the programmes about alcohol and tobacco use. 2 wks after each booklet was posted, a health educator telephoned a parent, encouraged the participation of all family members in the programme, and answered questions; Parent consultants delivered programme and were trained with manual over entire 2 years (moderate intensity). (2) Control; No active programme, only data collection |
|
| Outcomes | One question: 'How much have you ever smoked cigarettes in your life?': Likert‐scale responses collapsed to never‐smoked or had smoked even a puff.
Smokeless tobacco determined by 'Have you ever tried chewing tobacco (such as Redman, Levi Garrett, or Beechnut) or snuff (such as Skoal, Skoal Bandits, or Copenhagen)?'.
Follow‐up at 3m and 12m. "Families who completed the entire program (74% ...) spent an average total 4 1/2 hours doing the program and parents spent an additional hour talking with the health educator by telephone. The majority of families completed all activities associated with each booklet." Data are for baseline never‐smokers (identified from Figure 1) |
|
| Notes | Only cigarette use used in meta‐analysis. Smokeless tobacco use low and did not differ by condition | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "telephone numbers selected to be representative of all telephone numbers in the contiguous states were generated by random‐digit dialling....As baseline interviews were completed, parent–adolescent pairs were matched by date and time of completion and then allocated randomly either to receive Family Matters or to serve as control subjects." Method of randomisation not stated. |
| Allocation concealment (selection bias) | Unclear risk | "As baseline interviews were completed, parent‐adolescent pairs were matched by date and time of completion and then randomly allocated." No details reported who matched pairs. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not possible with this intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Interviewers and health educators were different people, and their interaction was minimized. Interviewers and health educators were blinded from study findings until all data had been collected. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | '86.2% of baseline respondents participated at follow‐up'. 'To assess attrition bias after baseline, we compared respondents who did and did not complete follow‐up interviews... respondents lost to follow‐up were more likely to be baseline users ..'. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | |
Biglan 1987.
| Methods | Study design: C‐RCT. In one school district (6 schools) whole schools assigned to conditions. For the remaining 7 schools, "classes of teachers who agreed teach the experimental curriculum ... were randomly assigned to intervention or control" and 7th grade students were randomly assigned to have parents receive or not receive parent messages. Power computation for parent messages performed but not reported. No power computation for main study. Analysis: factorial analysis of covariance. Separate analyses for those reporting smoking in previous week at baseline and others. A combined within‐ and between‐ schools design was used to investigate contamination effects, classroom unit of analysis, Total study duration: 9‐12 months after initial assessment. |
|
| Participants | Total number. At pre‐test: 3387 in 135 classrooms (4.9% weekly smokers); Setting: 13 middle, junior & high schools, Oregon, USA; Age 7‐10th grades; Gender 51% F; majority white. | |
| Interventions | Focus: Preventing and reducing smoking Intervention (1): Information about health effects and short‐term effects of tobacco; sensitization to pressures to smoke; training in refusal skills including modelling, rehearsal, reinforcement, practice, video practice, and supporting peers in refusals. Duration: 5 sessions; 4 on consecutive days + booster at 2 wks. Providers: regular science or health teachers, trained for 2‐3 hrs. Intervention (2): (a) same as (1) + (b) 7th graders in 6 schools randomised to have 4 messages mailed to their parents following the programme to encourage parents to discuss their views of smoking with their child and set clear rules about smoking (low intensity). (3) Control: no intervention |
|
| Outcomes | Weighted index of self‐reported smoking (Pechacek) based on no. smoked in previous week and yesterday. Nonsmoking=no cigs in previous week. Expired CO measured and saliva collected prior to questionnaire completion. Follow‐up: 9m and 1 yr. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation method not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not possible with this intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessment in class. No statement if assessors blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 18.7% attrition (19.8% in treatment, 24.1% in control, ns); no differential attrition |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | No effects of clustering were detected by the factorial ANOVA, which included grade as one covariate. Students were the unit of analysis for the parent messages |
Connell 2007.
| Methods | Study design: C‐RCT. 998 6th graders randomised to either control or 'universal intervention' classrooms. No power computation. Analysis: "we use CACE [Complier Average Causal Effect] analysis to identify predictors of intervention engagement and to examine the effect of engagement with the selected and indicated levels of ATP [Adolescent Transitions Program] intervention on the development of problem behavior..." Total study duration: 6th grade to age 22 |
|
| Participants | Total number: 998 (all 6th graders in the three middle schools; 498 allocated to control, 500 to intervention, 115 received an additional family intervention). Setting: 3 middle schools in a NW metropolitan area, USA; Age 6th graders; Gender 47.3%F. |
|
| Interventions | Focus: Preventing and reducing smoking and problem behaviour Intervention: Adolescent Transitions Programme. Schools provided with a Family Resource Center (a) brief consultations with parents; (b) telephone consultations; (c) feedback to parents on their childrens' behaviour at school; (d) access to videotapes and books; (e) SHAPe Curriculum for students with 6 lessons (school success, health decisions, building positive peer groups, cycle of respect, coping with stress and anger, and solving problems peacefully. A Family Check Up (FCU) was offered (interview exploring parent concerns, assessment including videotaping family at home, feedback by the therapist using motivational interviewing strategies and exploring interventional services the family could use, which were delivered over two years by therapists). Although all families could receive the FCU, families of high‐risk youths, determined by teacher ratings, were specifically offered the FCU in seventh and eighth grades. The 115 who received this component were designated as "engagers" in the FCU. These families received average 8.9 hours direct contact with intervention staff. (high intensity) Control: no intervention. |
|
| Outcomes | Tobacco from 1 (never) to 6 (more than 20 times) Follow‐up to age 16‐17 in Connell 2007, to age 22 in Connell 2009 | |
| Notes | Connell 2009 reports sub group analysis of 'engagers' matched to control youth using CACE analysis. Data could not be extracted for meta‐analysis, reported narratively. CACE analysis is intended to control for non‐compliance; minimal details are provided; results for tobacco are stated as "significant" but no levels of significance are given or n's |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'Youths were randomly assigned at the individual level to either control (498 youths) or intervention (500 youths) classrooms' no other details provided. "Although all families could receive the Family Check Up, families of high‐risk youths, determined by teacher ratings, were specifically offered the FCU." Method of randomisation not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition 21% by age 18; no analysis if differential attrition occurred |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | |
Cullen 1996.
| Methods | Study design: RCT. 246 newborns 1964‐7 stratified by gender and birth order in their family, then allocated by alternate births to either intervention or control; No power computation. Analysis: tests of proportions using normal approximation to the binomial distribution. Total study duration: 27‐29 years |
|
| Participants | Baseline: cohort of 246 newborns 1964‐7, 124 randomised to intervention, 122 to control. Follow‐up in 1993: 209 (90%) adults aged 27‐29 years; intervention 105, control 104. Setting: alternate births in Busselton Hospital, Busselton, WA, Australia; 53% female at follow‐up. |
|
| Interventions | Focus: prevention of behaviour disorders Intervention: 20‐30 min interviews by GP (4 per yr in 1st yr, 2 per yr for next 4 yrs) with mothers to enhance self‐worth, self‐acceptance, foster gentle physical interaction with child, and adopt a positive attitude to modifying child's behaviour (assessed as high intensity) Control: the study secretary maintained contact with the parents, asked about family events in preceding year and took photos of children at 6 months; No researcher contact with either group 1975‐1993 'other than sporadic visits' to one author as their GP. |
|
| Outcomes | Current smoking (not further defined); Personality, language and learning ability tests at 6 yrs of age. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Alternate allocation by birth in hospital (stratified by gender and position in family). alternate allocation is usually a weak method, but alternate allocation of births may not involve bias as there are no intrinsic characteristics that would cause newborns with specific characteristics to alternate time of birth; |
| Allocation concealment (selection bias) | High risk | 246 families at baseline in 1964‐7 received counselling about child rearing. 209 (90%) of the then newborns were followed up by postal questionnaire as adults aged 27‐29 years in 1993. There is no statement about allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "The original blind nature of this therapeutic trial was maintained for the current study." No statement or process analysis if all GP interviews were conducted and all according to Protocol |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "The original blind nature of this therapeutic trial was maintained for the current study." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 10% attrition; no attrition analysis |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | |
Curry 2003.
| Methods | Study design: RCT. families stratified by child's age, site, and subcohort (assessment or only follow‐up) then randomised to intervention or control. No power computation. Analysis: Chi squared to compare nominal data; t‐tests to compare means on ordinal and interval data; logistic regression for comparisons adjusting for parent baseline survey data, and "tested for effect modification by fitting logistic regression models containing treatment interaction terms." Total study duration: 20 months |
|
| Participants | Total number: Eligibles were 7,337 families with a child 10‐12 yrs identified in the membership files of 2 HMOs in Seattle and Portland; 4,026 [55%] gave consent and 3,563 (88% of enrolled) completed the 20m follow‐up; at the 20m assessment the response rate was 86% in the intervention and 90% in control (P<0.001). Random sample of 12.5% in each group assigned to assessment cohort in which parent and child provided data at baseline, 6,12 and 20 months Setting: Health Maintenance Organisation, Portland, Seattle, USA; Age; 10‐12; Gender 52%F. |
|
| Interventions | Focus: smoking prevention. Intervention: 'Steering Clear Project: (1) intervention: (a) 12‐chapter parent handbook with information and activities to encourage, motivate and reinforce parent‐child communication about tobacco; a videotape on the experiences of a former tobacco model; a CDC videotape; and a comic book, pen and stickers for the child; (b) two calls from a counsellor; (c) a 6‐page newsletter 14m later; (d) access to a website; and (e) physicians were prompted during appointments to encourage families to use the videos and website and talk about staying smoke‐free; trained telephone counsellors. Authors describe programme as 'minimal intensity'. Control: 'usual care'. Exposure to school‐based tobacco prevention curricula; tobacco marketing; and media‐based tobacco prevention messages was assessed at baseline, 6m, 12m, and 20 month follow‐ups. |
|
| Outcomes | Ever smoking and smoking in the past 30 days. Follow‐up at 20m. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not stated; groups were similar at baseline in family characteristics; 2.5% of children in intervention and 0% in control reported smoking in prior 30 days (p = 0.02); |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding of participants not possible. Blinding of personnel not addressed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | at 20m assessment response rate was 86% (I) and 90% (C) (P<0.001); no differential attrition analysis |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Interventions were to individual parents, so no effects of clustering. No other biases ascertained |
Dishion 1995.
| Methods | Study design: RCT. Self‐recruitment through advertisements, then randomly assigned to intervention or control. No power computation. Analysis: MANCOVA.
"Omnibus multivariate effects (within domain) were calculated to determine if outcome variables varied by intervention condition. Significant effects were followed by orthogonal planned contrasts to determine whether any of the three intervention groups ...were more effective." [i.e., clustering was not assessed]. Total study duration: 1 year follow‐up |
|
| Participants | Total number: 158 families recruited into the study after screening, 147 children at 1 year follow‐up (89% child interviews, 84% mother ratings, 88% teacher ratings). Setting: Eugene, Oregon, USA; Age 10‐14, avg, 12; Gender: 47%F. | |
| Interventions | Purpose: "test alternative strategies to reduce escalation in problem behaviours among high‐risk young adolescents." Strategies are to "target parents' use of effective and non‐coercive family management practices (parent focus) and young adolescent's self‐regulation and competence in family and peer environments (teen focus)." Parent sessions focused on 4 key skills; monitoring, positive reinforcement, limit setting and problem solving "All families were initially visited at home by therapists from their group." Interventions 1, 2 & 3 were 12 x 90‐min counselling sessions based on scripted materials and videotapes: Intervention 1: Parent focus (n = 26): the parent's family management practices and communication skills (monitoring, positive reinforcement, limit setting, and problem solving, with discussion of home practices and demonstration of the skills, with exercises, role‐plays, and discussions); Intervention 2 (n =32): Teen focus: teen self‐regulation and pro‐social behaviour in parental and peer environments (self‐monitoring and tracking, pro‐social goal setting, developing peer environments supportive of pro‐social behaviour; setting limits with friends; and problem solving and communication skills with parents and peers); Intervention 3 (n=31): combined parent and teen intervention; (Interventions 1‐3 high intensity) Intervention 4 (n=29): self directed change (the 6 newsletters and 5 brief videos that accompanied the parent‐ and teen‐interventions); (5) Control (n=39): separately recruited by advertisements, no intervention offered. [data not included in this review as non‐random] |
|
| Outcomes | (1) Tobacco use over previous 3m; 'the raw frequencies of use reported over 3 months were transformed (log +1) to yield a distribution for outcome analyses'; (2) expired CO; (3) parent‐child problem solving; (4) parent reports of family conflict; (5) parent reports of child behaviour. Follow‐up at 1 yr. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Method of randomisation not stated; "A cluster sampling approach was used to achieve random assignment. This procedure provided a pre‐established order of assignment of families to each of the four intervention conditions until all conditions were filled. Boys and girls received assignments separately to assure equal distribution of gender across conditions." [The control was described as quasi‐experimental and recruited separately, so any comparison with the control is high risk] |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Biochemical validation used |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition analysis. An inspection of differential dropout of users and nonusers by condition revealed no differences using either parent or child data. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Unclear risk | No analysis for any effects of clustering |
Elder 1996.
| Methods | Study design: C‐RCT. 10 schools at each site randomised to control, 7 to school‐based intervention, 7 to school and family. Analysis: repeated measures ANCOVA, multiple logistic regression to identify predictors of smoking experimentation, school random effect in all analyses, but school effects not stated. Study was not designed to find a difference in smoking prevalence. Total study duration: 3 years |
|
| Participants | Total number: Eligibles: all 3rd grade children 1991‐2 (n not stated). Average of 9087 children evaluated 1992‐1994, and 7827 children at end of 5th grade, of whom 6527 gave complete information. Setting: 96 schools (24 each in Texas, California, Louisiana and Minnesota) USA; Age 3rd grade at baseline; Gender 51% F; Ethnicity, 71% White, 16% Hispanic; 14% African‐Americans. | |
| Interventions | Focus: CATCH trial (Child and Adolescent Trial for Cardiovascular Health). Intervention 1: School intervention, 15 sessions in 3rd grade about diets healthy for hearts and exercise, 12 in 4th grade about exercise, and 16 about exercise in 5th grade plus 8 about tobacco. The tobacco intervention (only offered in 5th grade) was 'F.A.C.T.S. for 5' (Facts and Activities about Chewing Tobacco and Smoking). 4 x 50 min sessions: Session 1: short‐ and long‐term effects of tobacco use; Session 2: motivations and fallacies about tobacco use; Session 3: economic costs of tobacco use and the efforts of the tobacco companies to promote use; Session 4: dangers of passive smoking and being supportive of those who want to quit. Policy component, encouraging the adoption of policies for the school to be tobacco‐free (Minnesota schools already had a policy of 100% smoke‐free schools at all time periods. Intervention 2: (a) School intervention as above, plus (b) Family intervention, Home‐based programme, using 'The Unpuffables' from the ALA: 4 sessions with stories about adolescents who combat tobacco use, and games to play with parents Teachers received 1 or 1 1/2 sessions of training; Control; no statement. |
|
| Outcomes | % of schools with smoke‐free policies; Smoking prevalence. Duration of follow‐up: 3 yrs. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not stated |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not possible to blind participants to intervention. Researcher blinding not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data not available from one school |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | The family component consisted of attending 2 Family Fun Nights, and 15 individual parent and child activity packets to be completed as dyads, so there are no concerns about clustering effects for the principal part of the family programme. |
Fang 2013.
| Methods | Study design: RCT (mother‐daughter dyads). No power computation. Analysis: general linear model repeated‐measure analyses, intention‐to‐treat Total study duration: 2 years |
|
| Participants | Total number: Baseline 206 mother‐daughter dyads eligible, 98 excluded, 108 randomised (56 intervention, 52 control). Setting: recruited from 19 states from social network sites and social service agencies,USA; Age 10‐14; Gender 100%F. |
|
| Interventions | Focus: Substance use and modifying risk and protective factors at individual, family and peer levels Intervention: online 9 session (each 35‐45 minutes) + 1 booster substance abuse prevention programme to strengthen quality of relationships with mothers and increase girls' resilience to resist substance use (audio, graphics, animation, activities, skill demonstrations, guided rehearsal, immediate feedback) (moderate intensity) Control: no intervention |
|
| Outcomes | Number of occasions smoked cigarettes past 30 days Follow‐up: 2 years |
|
| Notes | Fidelity assessment: Computer automatically returned participants to last place they logged off and participants could not log onto next module until previous one completed; only data from participants who answered 3 of 4 fidelity check questions were included. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Assigned by blocked random number sequence using computer random number generator" |
| Allocation concealment (selection bias) | Low risk | "research staff member who was not involved in participant enrolment and intervention assignment generated the sequence using a computer random number generator" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Investgators and recruiting staff were blinded to the assignment procedure" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Of 56 mother‐daughter dyads 54 (96.4%) fully attended 9 session web‐based programme, 50 (89.2%) completed 2 year follow‐up; of 52 control arm dyads 9 lost at 2 year follow‐up; no analysis if differential attrition [outcome data on never smokers provided by Dr Fang via e‐mail] |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | The intervention was online and individual, so no concerns about clustering. No other biases ascertained |
Forman 1990.
| Methods | Study design: C‐RCT. Schools matched on level (middle vs. high school) ethnic composition, % of students receiving free lunches, and school size, and within each cluster randomised to the school intervention, school plus parent intervention or comparison group. No power computation. Analysis: Repeated measures multivariate ANOVA, analysed separately with the school and the individual as unit of analysis (results showed no differences by unit of allocation). Total study duration: 1 year. |
|
| Participants | Total number: Eligibles: 327 students, referred by teachers if had two or more of: high number of disciplinary incidents, low grades, high number of unexcused absences, drug or alcohol use by most friends, drug or alcohol use by family members, low self‐esteem, social withdrawal, or experimental alcohol or drug use; 279 (85%) completed 20 hour training group and pre‐ and post‐assessment sessions; 201 completed booster and assessment at 1 year. Setting: all 30 secondary schools in a SE metropolitan area, USA; Age avg 15 yrs; Gender no statement; Ethniciity 75% White, 24% Black, 1 Hispanic, 3 Other. |
|
| Interventions | Focus: tobacco, alcohol and marijuana prevention Intervention 1: School intervention (10 session small groups with Botvin's Life Skills Training, with 2 hr booster 1 year later). Students learned behavioural self‐management, emotional self‐management, decision‐making, and interpersonal communication and "substance information was addressed." Students provided with handbook with summaries of concepts, facts, and skills discussed during group sessions, material for group exercises, and directions for completing homework assignments. Intervention 2: (a) School intervention + (b) Parent intervention: parents participated in 5 weekly 2‐hr sessions to teach parents the coping skills their children were learning in the student groups, teach parents behaviour management skills, and develop small group support system for parents to encourage each other to take positive, constructive action regarding their adolescents. (high intensity) Control: 10 x 2‐hr sessions in structured small groups with substance abuse programme adapted from that provided by the state drug and alcohol commission |
|
| Outcomes | Lifetime, monthly, weekly and 24‐hr tobacco use; saliva samples were collected but not analysed Follow‐up: 1 year |
|
| Notes | Performance bias: 74% avg completion of coping skills sessions; 44% students in School Plus Parent intervention group had a parent participate in parent training sessions. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "All secondary schools (N = 30) in a seven‐school‐district, two‐county, southeastern metropolitan area were matched into groups of three on the basis of secondary level (middle vs. high school), racial composition, percentage of students receiving free lunch, and school size so that each matched cluster contained schools that were most similar to each other with regard to these characteristics. Within each cluster, schools were randomly assigned to three treatment conditions." No statement of method. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 15%; 279 of 327 students completed the 20 hour training and pre‐and post‐treatment assessment sessions, and of these 200 (72%) completed the booster one year later; no differential attrition analysis |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Clustering assessed with analyses with the individual and the school as unit of analysis, Repeated measures multivariate ANOVA. No other biases ascertained |
Fosco 2013.
| Methods | Study design: RCT. No power computation. Analysis: structural equation modelling Mplus 6.1, models estimated using full information maximum likelihood estimation to reduce bias from missing data. Total study duration: 3 years |
|
| Participants | Total number: 593 adolescents and their families (386 intervention, 207 control) Diagnostic criteria: adolescents and families could participate in family resources through school Family Check‐Up programme; Setting: 3 public middle schools in urban area Pacific NW, USA; Age: 6‐8 grade; Gender: intervention 48.2% F, control 49.3 % F; Ethnicity; Intervention 35.8% European American, 17.9% Latino/Hispanic, 15.5% African‐American, 7.5% Asian American, 2.6% American Indian/Native American, 1.8 % Pacific Islander, 18.9% Biracial/mixed ethnicity; control 36.7%, 18.4%, 14.5%, 6.3%, 1.9%, 1.9%, 20.3% |
|
| Interventions | Focus: Behavioural problems (anti‐social behaviour, deviant peer group affiliation, substance use) Intervention: Family resource centre at school. Parent consultant trained in Family Check‐Up model to facilitate collaboration with parents, identify youth at risk, and refer at‐risk students for counselling. At risk adolescents and families participate in 3 motivational interviewing sessions to identify family strengths and weaknesses, motivate parents to improve parenting and to engage in intervention services. Feedback about assessment results provides opportunity to select interventions tailored to unique needs of each family. Of 386 families in intervention group, 51% received consultation from parent consultant, 42% full FCU intervention; of those receiving FCU, 78% received additional follow‐up assistance such as parent skills training, education‐related concerns, support in success with homework, attendance and grades, improving school behaviour, and facilitating parent‐teacher communication. Of 180 families, 36% received positive behaviour support, 68% support in limit setting and monitoring skills, 73% support for communication and problem‐solving, 67% school‐related support. Intervention families received an average 94.2 minutes of intervention time. (assessed as high intensity) Control: no access to Family Check‐Up and its intervention services |
|
| Outcomes | Number of cigarettes previous month Follow‐up: 3 years post intervention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | adolescents "randomly assigned" blocked on school |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Baseline 593 (intervention group 386, control 207). [E‐mail from Dr Stormshak 26 January 2014: Intervention group (compliers baseline 138 never smokers; final evaluation 122 never smokers, 11 smokers) and (non‐compliers baseline 208 never smokers and 3 smokers; final evaluation 130 never smokers and 13 smokers); Control group (compliers baseline 23 never smokers, final evaluation 7 never smokers and 9 smokers) and (non‐compliers baseline 160 never smokers and 3 smokers; final evaluation 126 never smokers and 9 smokers). No differential attrition analysis |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Structural equation modelling assessed any clustering effects. No other biases noted |
Guilamo‐Ramos 2010.
| Methods | Study design: RCT. Analysis; linear regression, logistic regression, odds ratio Total study duration: 15 months |
|
| Participants | Total number: Eligibles 1734 African‐American and Latino mother‐adolescent pairs, children enrolled in grade 6 or 7; 1386 randomised (695 intervention vs. 691 control); at 15 month follow‐up 1,096 included in analysis (542 intervention vs. 554 control). Mothers eligible if they were aged 18 years or older and were primarily responsible for providing care for the target child. Setting: 6 middle schools in the Bronx and Harlem communities of New York, USA; Age: Grades 6‐8; Gender 50.4%F |
|
| Interventions | Purpose: "We evaluated the effectiveness of a parent‐based add‐on component to a school‐based intervention to prevent cigarette smoking among African American and Latino middle school youths." Intervention 1: Project Towards No Tobacco Use (TNT) smoking intervention: 10 modules modified for inner city schools to two face‐to‐face sessions each 2.5 hours (effective listening and tobacco information, course and consequences of tobacco use, self esteem, being true to oneself, changing negative thoughts, effective communication, assertiveness and refusal skills, advertising, and social activism) PLUS the "Linking Lives" intervention (a) "Raising Smoke‐Free Kids" (manual of 9 short modules, two tobacco‐related homework assignments for parents to use with adolescent), (b) two one‐day sessions. Day 1: discussed modules, concept parents could make a difference in their adolescent's tobacco‐related behaviour, strategies for effective communication, topics parents might consider discussing in their conversations with their adolescents, importance of setting limits. Day 2: Tobacco‐related homework assignments: consequences of smoking, and ways to resist peer pressure. Mothers received 2 booster calls 1 & 6 months after the intervention Control: Project Towards No Tobacco Use (TNT) smoking intervention. |
|
| Outcomes | Ever smoking. Analyses include baseline smokers. Total study duration: 15 months: measures at baseline and at 15 months. |
|
| Notes | Research was supported by funding from the Centers for Disease Control and Prevention (CDC; cooperative agreement U87/CCU220155‐3‐0). Odds ratio for ever smoking 0.58 (0.36 to 0.94) based on logistic regression, also reports that 5% TNT‐plus and 10% TNT only reported ever smoking at follow‐up. Numbers quit estimated from these percentages to approximate the reported OR. Power computation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomly assigned by computer." |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement. Not possible to blind participants to intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 22% of those interviewed at baseline did not complete the study. Included in analysis only those who reported data Incomplete data points for participants Analysis if differential attrition could affect outcomes |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Unclear risk | Linear and logistic regression and covariates included grade, but no assessment of clustering. Some contamination of the control was observed, 25% stated they had given their child a handout that had been distributed solely to parents in the TNT plus parent condition. Higher level of contamination then expected, however it does not seem to have been enough to dilute the intervention effect. Smoking behaviour of adolescents was based on self‐reports. |
Haggerty 2007.
| Methods | Study design: RCT. Power computation: No details; sample size in each of the cells prohibited conducting interaction analyses for race×gender×intervention condition. Statistics: repeated measure mixed model regression. Intention‐to‐treat analysis. Total study duration: 2 years. |
|
| Participants | Total number: 331 Grade 8 youth; Self‐Admin & Telephone support (SA): 107 families; Parent and Adolescent Administered (PA) format 118 families; Control: 106 Setting: Grade 8 students, Seattle Public Schools, USA; Age: 13.7 years; Gender 49%F; Ethnicity 168 European‐American; 163 African‐American |
|
| Interventions | Purpose: multifaceted family‐based prevention approach to address common risk and protective factors for initiation into cigarette, alcohol, other drug use or sexual activity, delinquent and violent behaviour so that each teen’s particular vulnerabilities are addressed. Sought to test for overall effects on initiation of problem behaviours in the first 2 years of high school when initiation is likely to occur, but levels are still relatively low. Strategies designed to help families reduce risk factors. Programme teaches families to reduce family management problems by increasing parental supervision and effective consequences for misbehaviour. Intervention 1: Self‐administered with Telephone Support. Video and activities completed within 10 weeks. Written instructions and 62 key activities to complete as a family. Receipt of $100 for completion of program activities. Trained telephone facilitators. Intervention 2: Parent and Adolescent (PA) Format (assessed as high intensity). Met for 7 consecutive weeks, sessions conducted once per week over 7 weeks in middle school. 1,3 & 7 session 2.5 h long, remaining 2 h. Group and home practice exercises, video segments and workbook. Reimbursement provided for Childcare and transportation Receipt of $100 for participation. Trained leaders Program workbook (common to both): Chapter One Roles: Relating to your teen; Chapter Two Risks: Identifying and reducing them; Chapter Three Protection: Bonding with your teen to strengthen resilience; Chapter Four Tools: Working with your family to solve problems; Chapter Five Involvement: Allowing everyone to contribute; Chapter Six Policies: Setting family policies on health and safety issues; Chapter Seven Supervision: Supervising without invading. (3) Control: No treatment follow‐up only Integrity of Intervention: Self‐administered with telephone support: Mean level of reported completion of the family activities was 81%. On average, family consultants made 16.9 call attempts resulting in 9.7 completed calls during the 10 weeks; phone calls lasted about 10.5 min per week. Families received up to $100 for their completion of program activities. Parent and Adolescent (PA) Format: Group leaders called families each week to remind them of the upcoming session. Of the 118 families assigned to the PA condition, 92 (77.9%) initiated the parent and teen sessions. The mean number of sessions attended was 4.56. Family sessions were led by two workshop leaders with prior experience conducting parent or teen workshops, and received 20 h of training. |
|
| Outcomes | Initiation of cigarette use from post‐test to 24 month follow‐up Sex, Alcohol, Marijuna, other illegal drugs also assessed. | |
| Notes | Grant # R01‐DA121645‐05 from the National Institute on Drug Abuse. Results from both formats of programme combined and compared to control |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “Participating families were stratified on race and gender”. The unit of assignment was the family, not school or neighborhood.” Authors stated: “Comparisons at baseline revealed no significant differences on demographic characteristics or outcome variables by intervention condition. indicating the integrity of randomisation.” |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition of participants: 331 baseline, 313 at post‐tests, 306 at 1 year, 304 at 2 years = 92%. "No significant differences between attriters and attriters on key outcomes .. Among both child outcome and demographic measures, there was no evidence of differential attrition." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | High risk | The interventions were self‐administered, so there is no concern for clustering. Selection bias: Consent rates were higher for Afro American families (55%) than for European American families (40%). Of those who refused, 53% completed a refusal survey which suggested that those who declined participation were significantly more educated and were more likely to be married and to be European American than parents who consented. |
Hiemstra 2014.
| Methods | Study design: C‐RCT. Power computation: 428 per condition to detect 10% absolute difference in initiation of smoking over 36 months alpha = 0,.05, 2 tailed, power = 80% Analysis: logistic regression to assess baseline covariates; intention to treat, missing data replaced by multiple imputations; outcome differences between conditions by chi‐squared; ICCs zero so no adjustment for school effect Total study duration: 36 months |
|
| Participants | Total number: 1478 children and mothers (728 intervention, 750 control); then those who had already puffed a cigarette (80) were excluded from analysis, leaving 1398 never‐smoking children. [630 of 1347 school boards were willing to give recruitment letters to children to pass to parents] Setting: 418 schools, Netherlands; Age: 9‐11; Gender: Intervention 56.6% F; control 48.7% F |
|
| Interventions | Purpose: to prevent smoking initiation Intervention: "Smoke‐Free Kids" programme: 5 printed activity modules + booster (general communication about smoking, influence of smoking messages, rule setting and non‐smoking agreement, creating smoke free house and environment, peer influence). Booster module 12 months after baseline. (assessed as low intensity). Control: "Factsheets provided information on youth smoking and directed parents' attention towards macro‐level variables relevant to youth smoking." |
|
| Outcomes | Outcome measured: 1 = never smoked to 9 once daily, dichotomised to 0 and 1 (any smoking) Follow‐up: 36 months after intervention |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Independent statistician using SPSS |
| Allocation concealment (selection bias) | Low risk | Independent statistician using SPSS |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "Participants were blind to randomisation." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 1398 baseline never smokers; 1238 completers at 36 months (89%); no differential attrition analysis |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Intention‐to‐treat analysis. Intraclass correlation (ICC) = 0, so no concern for clustering. |
Jackson 2006.
| Methods | Study design: RCT. Parent‐child dyads randomised to experimental or control group. No power computation. Analysis: intention to treat; X2 to test for attrition bias; logistic regression to test whether the programme affected initiation of smoking | |
| Participants | Total number: 1147 parents who smoked and had a 3rd grade child submitted consent forms; 135 not contactable; 125 not eligible; 887 parent‐child (3rd grader) dyads completed baseline assessment, 776 (89%) completed 3 year assessment. Setting: 28 school districts in N. Carolina, S. Carolina and Colorado, USA; Age; 3rd grade; Gender 53%F |
|
| Interventions | Focus: tobacco prevention Intervention (n = 371): "Smoke Free Kids" programme: 6 guides mailed to home (5 at 2 week intervals, one after 1 year) with tips on parenting skills; newsletters; gifts to participating children (low intensity) Control (n = 405): 5 fact sheets about tobacco mailed to home. |
|
| Outcomes | Ever having puffed on a cigarette Follow‐up: 3 years |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "parent‐offspring pairs randomly assigned." Method not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 873 parent‐child dyads completed baseline interviews and randomised; 776 (89%) children completed interview 3 years later. "There was no association between attrition and demographic attributes." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | No assessment of any clustering effects. No other biases ascertained |
Jøsendal 1998.
| Methods | Study design: C‐RCT. Power computation: power 80% alpha = 0.05 required n = 757 in each group, with sample sizes achieved. Analysis: no adjustment for clustering in Jøsendal (1998), but multilevel multiple logistic regression for changes in smoking rates allowed for clustering and adjusting for gender and baseline smoking for 3 yr follow‐up (Jøsendal 2005) Total study duration: 3 years |
|
| Participants | Total number; National representative sample of every 11th school by ascending postal code: 99 schools, 195 classes, 4441 students (grade 7), of whom 4215 provided written consent. 2230 in relevant arms. Programme administered by classroom teachers. Setting: 195 classes in 99 schools, Norway; Age, 13; Gender no statement. |
|
| Interventions | Focus: Tobacco Intervention 1: Model programme: 8‐session Be smokeFREE intervention focused on personal freedom, the freedom to choose, freedom from addiction, making one's own decisions, tobacco‐resistance skills, and the short‐term consequences of smoking. The classroom teachers received 2 days training, detailed programme manuals to secure fidelity, and filled in a questionnaire after each lesson to evaluate programme fidelity. Students brought 2 brochures home; teachers involved parents in discussions on 'appropriate occasions', and students and parents signed non‐smoking contracts. Parental component assessed as low intensity Intervention 2: Same school programme without parental involvement Intervention 3: Same school and parent programme, teachers not trained Control; Usual smoking & health classes (Intervention 3 and control do not contribute to this review) |
|
| Outcomes | Daily, weekly, <weekly smoking, and non‐smoking. Follow‐up at 6m, 18m, 30m. Longest follow‐up used here. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Schools were chosen as sampling units and as units for allocation to groups. Schools were drawn from a list containing all Norwegian schools in order of ascending zip‐code. Control schools were first selected (every nth school, starting with a randomly selected number between 1 and n), then the first three following schools with a similar number of students (± 10%) on the school list were chosen". Clusters: Schools Cluster constraints: Not stated. Baseline comparability: Not stated. |
| Allocation concealment (selection bias) | Unclear risk | No statement. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Process analysis conducted but results not stated; also, the programme was varied and no process analysis of the variations as time progressed: Verbal assurances of compliance from Grade 8 pupils and teachers and Grade 9 pupils. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | After 30 months, 11.2% attrition in intervention (all 3 arms) and 5.8% in control. "...smokers were more likely to drop out than non‐smokers. This tendency was slightly stronger in the comparison group than the intervention group. Due to this, a separate survey of approximately 100 students who dropped out of the project was conducted approximately three years after the intervention had been finished (data not shown). Results from this survey showed that more smokers had left the comparison group than the model intervention group." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Effects of clustering assessed by multilevel modelling. No other biases ascertained |
Olds 1998.
| Methods | Study Design: RCT, women stratified by socio‐demographic characteristics and randomly assigned to one of four interventions or control. Analysis: intention to treat. General linear model and adjustment for covariates (maternal age, maternal education, locus of control, support from partner, maternal employment status, paternal .public assistance status). Total study duration: 15 years |
|
| Participants | Total number: 500 consecutive pregnant women with no previous live births recruited. Abstract and text says 400 newborns enrolled (but intervention groups total to 390) of whom 315 followed to age 15 if "mother and child were still alive and the family had not refused participation.'. Setting: semi‐rural community (Chemung County) in NY State, USA; Diagnostic criteria: Women "actively recruited" from free antepartum clinic if no previous live births, < 25 weeks pregnant, 19 years, unmarried or of low socioeconomic status; also enrolled if no previous live births but without these risk factors (85% of sample were young, unmarried or of low socioeconomic status) Diagnostic criteria: children of participants in a randomised trial of 400 consecutive primiparous pregnant women, 85% <19, or unmarried or low SES. 89% white. Age (315 adolescents followed up at 15 yrs of age); Gender no statement. |
|
| Interventions | Focus: Effect of prenatal and early childhood nurse visits on children's antisocial behaviour Intervention 1 (n=94): Free sensory and developmental screening at 12m and 24m, with referrals for further evaluation and treatment where necessary; Intervention 2 (n=90): As (1), + free taxi transport for pre‐natal and well‐child care until child was 2; Intervention 3 (n=100): as (2), + nurse home visits during the pregnancy; Intervention 4 (n=116) as (3), + nurse home visits until child's 2nd birthday. The nurses taught positive health‐related behaviours; competent care of the child, and personal development for the mother (family planning, educational achievement, and return to the workforce). |
|
| Outcomes | Cigarettes smoked/day in the preceding 6m. Groups 1 and 2 combined as comparison, since no differences between them. Follow‐up at 15 yrs. | |
| Notes | Performance bias: wide ranges in the number of visits (families visited at home received an average of 9 (range 0 ‐16) visits during pregnancy and 23 (range 0 ‐ 59) from birth through child's 2nd birthday); no process analysis of the content of the visits. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants randomised by selecting treatment assignment from decks of cards composed to ensure proportional treatment assignment within stratification blocks based upon women's race, marital status, and geographic region of residence at registration. To ensure balanced subclasses during the 2.5‐yr recruitment phases, card decks were periodically reconstituted to over‐represent treatment conditions that had smaller numbers of subjects; groups were similar at baseline and at 15 yrs; |
| Allocation concealment (selection bias) | Unclear risk | Not clear that assignment was fixed once women selected card. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Persons involved in data gathering were blinded to the women's treatment conditions." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "500 consecutive pregnant women with no previous live births were recruited, and 400 were enrolled. A total of 315 adolescent offspring participated in a follow‐up study when they were 15 years old." "intention to treat approach." No statement if differential attrition occurred. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Home visitation by nurses, then follow‐up interviews conducted with adolescents and mothers/guardians so no concerns for clustering. No other biases identified |
Pierce 2008.
| Methods | Study design: RCT. Power computation: sample to test whether encouraging parents to maintain best parenting practices is associated with reduction of target behaviours by age 18 will have 80% power to detect 25% effect size (allowing for 6% loss/year), and 30% effect size (allowing for loss of 12%/year). Sample was recruited by random digit dialling commencing May‐August 2003. Baseline equivalence: equivalent on all variables related to smoking outcomes. Analysis: logistic regression, using maximum likelihood framework adjusting for baseline covariates known to be predictors of study outcome and loss to follow‐up. Study duration: "Six adolescent and four parent interviews are completed with each participating family from baseline through age 18 years of the target adolescent." Eligibility was "families had an eldest child between the ages of 10‐13 years." Screening and enrolment were conducted by the survey firm between May 2003 and October 2004. Interviews were conducted quarterly. The authors provided us with data from waves 1 and waves 2‐6 combined. |
|
| Participants | Total number: From random sample of 57,000 households enumerated, 4781 identified with oldest child 10‐13 years, letters sent to 3079 (64%) who provided an address, mailings sent to "systematic" sub‐sample of 220 each month August 2003 through October 2004; unable to reach 1006 (non‐response to 18 callbacks or disconnected phone), 819 outside eligibility range (e.g., adolescent already 14 years), unable to complete both parent and child interviews with 218 families, Baseline: final enrolment 1036 families (36%), 514 intervention, 522 control; sample compared to US Census Bureau 2001/2 slightly under‐sampled Hispanic (sample 16%, census 18%) and slightly over‐sampled Caucasians (69%, census 65%) and African‐Americans (18%, census 16%) Setting: national sample of households, USA Diagnostic criteria: Households with eldest child 10‐13 years Age at baseline 12 years: Gender; 49%F |
|
| Interventions | Purpose: "Parenting to Prevent Problem Behaviors Project" Intervention: (a) Training phase to ensure all participants would have similar best‐parenting practices knowledge base: self‐help manual (12 chapters with 3 modules: building positive behaviours, setting effective limits, and relationship building). A lay facilitator called to help participants to work through the manual, (b) Implementation phase to ensure best parenting habits maintained in face of situational stressors: lay facilitator phoned at 3 months and followed a computer‐assisted structured counselling script to identify 10 major issues with teen on substance use, antisocial behaviour and moodiness, and use of best parenting practices using motivational interviewing. Facilitator also searched Internet and study library for answers to parents' problems, and previously researched information sheets sent to parents electronically or by mail; computer‐assisted structured counselling protocol for parents who needed additional help to implement best practices; family management questionnaire. Parent counsellors completed 60 hours training including role playing. Tapes were reviewed for fidelity (no statement of fidelity outcomes). Control: no‐contact |
|
| Outcomes | Tobacco use assessed by 15 questions from national and state telephone surveys. Categorised as Committed Never, Susceptible, Ever experimented, Smoked in past 90 days Six telephone interviews with adolescent and four with parents from baseline through 18 years by trained assessor blinded to study group |
|
| Notes | Trainers received 60 hours training with role‐playing and case management reviews with clinical psychologist, and tapes reviewed for fidelity Results not yet published. E‐mail 24 February 2014 from Dr. John Pierce, who kindly computed outcome data through waves 2‐6. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator and permuted block design to allocate to intervention and control by region of country, parental smoking, child smoking risk and hours out at night |
| Allocation concealment (selection bias) | Low risk | No statement, but random number generator described above |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Trainers had to know that they were counselling the intervention group |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Six telephone interviews with adolescent and four with parents from baseline through 18 years by trained assessor blinded to study group" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | (e‐mail from Dr. Pierce 24 Feb 2014): 1036 smokers (Intervention 514, control 522) at baseline including ever smokers. 64 (12.5%) intervention, 37 (7.1%) control missing for waves 2‐6. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Intervention self‐help at home so no concern for clustering. No other biases noted |
Prado 2007.
| Methods | Study Design: RCT. Power computation: "with 80% power, 240 participants were required across the 3 study conditions to detect an Intervention x Time effect size equivalent to d=.28." Analysis: Growth curve modelling. Total study duration: 36 months (2 cohorts: May 2001‐July 2004 and May 2002‐July 2005); Interval between intervention and outcome measure: 6, 12 (post‐intervention), 24 and 36 months |
|
| Participants | Total number: 266 (128 boys, 138 girls) and their primary caregivers (34 men, 232 women) Setting: 3 middle schools in Miami, Florida, USA Diagnostic criteria: Children entering grade 8 in next school year and attending one of the three participating schools, at least one parent born in a Spanish‐speaking country in the Americas, adolescent living with a primary caregiver who is participating in the study, neither students nor family member ever hospitalised for psychiatric condition, the family would reside in Miami for the 1st year of the study and South Florida for the duration of the study, and the primary caregiver was available to attend weekly evening meetings. Age: avg age 13; Gender: 52%F; Caregivers mean age 41. |
|
| Interventions | Purpose: "Consistent with Hispanic cultural expectations, Familias Unidas places parents in positions of leadership and expertise and builds on pan‐Hispanic values, such as primacy of family, sanctity of parental authority, and roles of parents as the family's leaders and educators." "It was therefore important to test whether the efficacy of PATH in preventing substance use and unsafe sex in Hispanic adolescents depends on whether it is embedded within a family‐strengthening intervention." Goal: To "investigate whether Familias Unidas + PATH [Parent pre‐adolescent training for HIV prevention] would be efficacious relative to two control conditions in preventing substance use and unsafe sexual behaviour in Hispanic adolescents and improving family functioning.........[and] "examine whether and to what extent improvements in family functioning would mediate the effects of intervention condition on substance use and unsafe sexual behavior" Intervention 1: Familias Unidas + PATH (15 group sessions, 8 family visits and 2 parent‐adolescent circles). (high intensity) Control 1: ESOL (English for Speakers of Other Languages) + PATH (8 ESOL classes, 6 group sessions, 2 family visits) Control 2: ESOL + HEART (American Heart Association HeartPower! for Hispanics) (8 ESOL classes, 7 group sessions) Familias Unidas "strives to increase parental involvement, positive parenting, and family support in Hispanic families" as "essential to promoting positive adolescent development and to preventing substance use and unsafe sex". Intervention included family visits focused on parents and parent‐adolescent facilitated discussion circles. Facilitators had average 5 years experience working with low‐ income Hispanic immigrant families, certified in Familias Unidas and PATH, trained in general group process facilitation and conducted 54 pilot sessions. All sessions taped. Adherence to Familias Unidas 3.72/6, PATH 3.70/6, interrater reliability k = .75 |
|
| Outcomes | Outcome measured: 90 day cigarette use "Growth curve analyses indicated significant differences in past 90 day cigarette use between Familias Unidas + PATH and ESOL +PATH (z=3.25, p<.002, d=0.54) as well as between Familias Unidas + PATH and ESOL + HEART (z=2.66, p<.008, d=0.80). A total of "1.4% of the adolescents in Familias Unidas + PATH reported smoking in the 90 days prior to assessment, compared to 10% in ESOL + PATH and 14.3% in ESOL + HEART." Time points from the study that are considered in the review or measured or reported in the study: baseline, 6, 12 (post‐intervention), 24 and 36 months |
|
| Notes | Funding: National Institute of Mental Health Grant MH63402, National Institute on Drug Abuse Grant 19101 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation: The research coordinator randomised participants to one of three conditions using an urn randomisation (Wei & Lachin, 1988) computer program that balanced on the following adolescent characteristics: gender; years in the United States (i.e., 0–3, 3–10, or more than 10); having initiated substance use (yes, no); and having initiated (yes, no) oral, vaginal, or anal sex. |
| Allocation concealment (selection bias) | Unclear risk | "The research coordinator randomised participants to one of the three conditions using an urn randomisation..." Unclear whether there was a strategy to conceal the sequence |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding was only undertaken in the process evaluation, not in the measurement of outcome. Measures were by self‐report |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding was only undertaken in the process evaluation, not in the measurement of outcome. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unidas + Path baseline 91, 71 completed 36 month assessment; ESOL + PATH 84 and 70; ESOL + HEART 91 and 70; no statement of differential analysis of attrition; "intent‐to‐treat design, such that participants continued to be assessed at each time point, whether or not they had dropped out of the intervention." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Unclear risk | The total intervention differed between the three groups by intention: "In the Familias Unidas + PATH condition, there were 15 group sessions, 8 family visits, and 2 parent‐adolescent circles. In the ESOL + PATH condition there were 8 ESOL classes, 6 group sessions, and 2 family visits. In the ESOL + HEART condition, there were 8 ESOL classes and 7 group sessions." CACE analysis. No assessment of clustering effects for group sessions. No other biases ascertained. |
Reddy 2002.
| Methods | Study Design: C‐RCT. Schools blocked on type (private, government) and gender (males only, females only, and co‐educational) and randomised by coin toss. No power computation. Analysis: F‐tests and t‐tests to assess for baseline differences between intervention groups. Mixed effects regression. Individual student survey data could not be matched from pre‐to post‐test, but school populations 'fairly stable during the study period'. Total study duration: Intervention lasted for 1 school yr (September‐June); Follow‐up 1‐8m post‐intervention. |
|
| Participants | Total Number: At baseline, 5752 students, 5043 (88%) provided consent, 4776 (83%) participated in the baseline survey
Setting: 30 elementary schools in New Delhi, India Age: aged 12 (7th grade); Gender: 49.5%F. |
|
| Interventions | Project HRIDAY [Health‐Related Information and Dissemination Among Youth]: reduction in cardiovascular risk factors (diet, physical activity, tobacco use) 1. School Intervention (10 schools, n=1439): (a) 10 posters in schools on cardiovascular health, (b) distribution of the HRIDAY project booklet with information on heart health, (c) classroom activities selected by teachers from a list of 20 [including 3 on influences to smoke, ways to refuse offers to smoke, and passive smoke], (d) round table discussions on food policy and nutrition, (e) invitation to sign a petition requesting a ban on tobacco advertising to be presented to the Prime Minister of India. 2. School/Family intervention (10 schools, n= 1863): as (1), + 6 booklets (1 on tobacco use, the rest on dietary patterns and exercise) taken home by pupils, and brought back parents' signed opinions about the booklets. (low intensity) 3. Control (10 schools, n=1474): Usual curriculum teachers and selected peer leaders received training (duration not stated). | |
| Outcomes | Ever use of cigarette or bidi, and likelihood of tobacco use when adult. Knowledge of and attitudes to smoking also surveyed. | |
| Notes | Performance bias: no process analysis; 2/30 schools had shorter follow‐up; 14/20 schools displayed all 10 posters, 6 displayed 7‐9; 6/20 schools implemented all 20 activities from the teachers' manual; 8/10 schools in Family intervention group distributed at least 5 of the 6 booklets. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The 30 schools in the study were representative of all schools in the urban area of New Delhi and were randomly selected from a sampling frame of all New Delhi schools (Government vs Private, same sex vs. coed)." Randomisation by coin toss (e‐mail from Dr. Cheryl Perry) Clusters: schools. Cluster constraint: blocked on type (private, government) and gender (males only, females only, and co‐educational). Baseline comparability: groups equivalent at baseline. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Present after 1yr: 4452 (77% of eligible students); no attrition analysis; no linkage of pre‐ and post student responses. (e‐mail from Dr. Cheryl Perry states there was insufficient funding for process evaluation and assessment of attrition). |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | e‐mail from Dr. Cheryl Perry states there was adjustment for clustering, No other biases ascertained |
Riesch 2012.
| Methods | Study design; RCT. Parent‐child dyad (schools only used to recruit dyads). No power computation: "We reasoned from past studies that approximately 20% of invited families would respond. An average of 60 children was enrolled in the fifth grade at each elementary school. To attain the 150 dyads expected as part of the SAMHSA contract, we needed to include a minimum of 13 schools. We randomly selected 17 schools from the high and low minority enrolment schools." Intention‐to‐treat. Analysis: “a clustered randomized trial, the data included multilevel or hierarchically structured samples. Adult–youth dyads were clustered within each school. A two‐level regression model was used (Rasbash, Charlton, Browne, Healy, & Cameron, 2009) with a dummy variable for treatment effects to avoid underestimating standard errors of regression coefficients from fitting a model that did not recognize clustering. Baseline measures were used as covariates in each analysis. The model for assessing change was a multilevel model for fixed‐occasion repeated outcomes (Goldstein, 1995; Yang, Health, & Goldstein, 2000).” Total study duration: Study was conducted from April 2003 through December 2005 (10 weeks for the intervention, then Interval between intervention and when outcome was measured, 6 months to Post 2 follow‐up). |
|
| Participants | Total number: From 16 randomly selected schools recruited 167 parent youth dyads (86 intervention; 81 from comparison). Recruitment: In Madison, 396 letters of invitation were sent; 66 parents indicated an interest in enrolling by telephone, return of a form to the school, or e mail; 57 were eligible for the study; and 55 consented to participate, for an enrolment rate of 14%. In Indianapolis, 520 letters of invitation were sent; 148 parents responded as interested in enrolling by telephone, return of a form to the school, or e‐mail; 140 were eligible for the study; and 112 consented to participate, for an enrolment rate of 22%. Of those eligible, reasons for not enrolling were lack of time or unwillingness to make the commitment to study procedures. Setting: 2 Midwestern cities (Madison, Wisconsin; Indianapolis, Indiana), USA. Gender: Youth 50% female. Adults: 91% intervention & 88% control female, tended to be educated beyond high school, employed, and married. Age: youth 9 to 11 (avg 10.8 years); Adults were in their late thirties. Ethnicity: 55% in the intervention African American and 56% in the control. Consent: No details of informed consent process ‐ “consented to participate” |
|
| Interventions | Purpose: Assessing the short version of the Strengthening Families Program (SFP 10‐14), a major revision of the 14 session SFP. Based on the Bio‐psychosocial Vulnerability Model. Designed to reduce risk factors and build family capacity and coping skills to access and use resources within their school and community to achieve child socialization goals. (1) Intervention: Youth and one parent attended the 7‐week, 2‐hr‐per‐week program together at community locations in the evenings or weekends in each city. Didactic content was presented by videotape, discussion sessions were timed, and the curriculum was detailed carefully in a manual that contained all the required handouts. In each session youth and parents or legal guardians were separated for the first hour to work on goal‐oriented, developmentally appropriate activities and dyads were reunited in the second hour for family‐oriented activities. (high intensity) (2) Control: Minimal contact comparison condition. Comparison group families participated only in the data collection procedures. No comparison families reported participation in another family skill building or parenting program. Integrity of Intervention: Used bachelor’s prepared or university students who were trained to facilitate the SFP 10‐14. Trainers from the Iowa State University Extension conducted 2‐day sessions on three separate occasions. Analyses of the checklists, more than 90% of the content was consistently covered in the adult groups and 87% for the youth groups. Analysis made by intensity of the intervention (partial dose/reduced completion). |
|
| Outcomes | "Smoked a cigarette‐ even 1 puff" | |
| Notes | A paradoxical result was: “significant outcomes among youth who received a partial dose were in the direction opposite than expected, that is, youth who received a partial dose perceived their communication with their father as statistically significantly less open at Post 2 and their involvement in the family as statistically significantly less at Post 1 than youth in the comparison condition.” The work was supported by the Substance Abuse and Mental Health Services Administration (UD1 SPO‐9460,Susan K. Riesch Project, Director and Janie Canty‐Mtichell Project Co‐Director). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Schools were randomly assigned to the intervention or comparison conditions. Schools served only as a recruitment site for adult‐youth dyads.” Method not described. Separate randomisation for 7 schools with "predominantly high" and 9 schools with "predominantly low" minority involvement. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No description of blinding. Unlikely blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description of blinding. Unlikely blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Baseline: 167 adult‐youth dyads. Retention strategies employed: Families participating in both study conditions received three newsletters directed toward games, activities, and issues of interest to parents and children. Cash or gift cards rewards provided on completion of surveys: $10, $15, and $20 for youth and $20, $30, and $40 for adults at Times 1, 2, and 3, respectively. 35 families withdrew between baseline and Post 2. "No significant differences among sociodemographic characteristics were found between those who completed the study and those who did not at each site." which would place the study at low risk of bias. Participation in the ATOD data collection was low. For the question at follow‐up about "smoked even a puff," 63 in the Intervention and 66 in the Comparison group provided an answer, and only 47 in the Intervention and 51 in the Control group provided an answer whether they had “smoked a whole cigarette.” These data did not provide sufficient numbers for modelling. The low rate of ATOD data collection and no comment whether differential attrition in data collection places the study at unclear risk of bias |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Clustering effects assessed by multilevel modelling. No other biases ascertained |
Schinke 2004.
| Methods | Study design: RCT. No power computation. Analysis: MANOVA, youths did the CD‐ROMs individually so no adjustment for clustering needed Total study duration: 3 years (Follow‐up at 1, 2, 3 years) |
|
| Participants | Total number: Baseline: 514 youths
Setting: Recruited from 43 community agencies in New York City, New Jersey and Delaware, USA. Diagnostic criteria: youth attending community agencies Age: avg 11.5 years; Gender: 51.4%F. |
|
| Interventions | Focus: Alcohol reduction Intervention (1): Social learning and Problem solving using CD‐ROM: ten 45 minute sessions on goal setting, coping, peer pressure, refusal skills, norm correcting, self‐efficacy, problem‐solving (Stop, Options, Decide, Act, Self‐praise), decison‐making, effective communication, and time management, Intervention (2): CD‐ROM + Parent intervention: (a) parents received a 30 minute videotape with printed materials on the goals of the youth intervention, showed how parents could help avoid problems with alcohol, and the importance of family rituals, rules and bonding (b) 2 hour parent workshop; (c) parent CD‐ROM how to reduce youth alcohol use (3) Control: (no further description) |
|
| Outcomes | Number of cigarettes in the last 30 days | |
| Notes | Performance bias: minimal risk: usage of CD‐ROMs was recorded by a code; 95% of youths completed the CD‐ROM in the CD‐ROM intervention group, and 91% in the CD‐ROM + parent intervention group; 83% of parents watched the videotape; 67% attended the workshop, and 79% completed the parent CD‐ROM. Detection bias: research assistants administered questionnaires individually by phone; | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomly within strata, sites were divided among three study groups: CD‐ROM intervention, CD‐ROM plus parent intervention and control." (no statement of method) |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Attrition CD‐ROM intervention 7.9%, CD‐ROM plus parent intervention 11.8% and control 6.7%. No differences in pretest scores. No differential attrition analysis |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Intervention delivered by CD‐ROM so no concern for clustering. No other biases identified |
Spoth 2001.
| Methods | Study design: C‐RCT. Schools blocked on size and proportion in lower income households, then randomly assigned to one of 3 groups. No power computation. Analysis: multilevel mixed model ANCOVA; dichotomous outcomes by z tests; groups were equivalent at baseline and multilevel analyses with logistic growth curve techniques controlled for the effects of clustering; for 4 and 6 yr follow‐up growth curve analysis was used; Total study duration: grade 6 to age 21 |
|
| Participants | Total number: Baseline: 1,309 eligible families (index child in 6th grade); 6th graders, age 11, 55% F; of the 309 eligible families 667 (51%) completed the pretest [238 ISF, 221 PDFY, 208 Control];
6th grade posttest 188,177,186; 7th grade follow‐up 161, 155, 156; 8th grade follow‐up 152, 145, 141; 10 grade follow‐up 152, 144, 151; 12th grade follow‐up 151, 157, 149; age 21 follow‐up 170, 161, 152): at 10th grade follow‐up at age 15 447 (67%); and 373 families (56%) completed all 5 data assessments across 4 years; Setting: 33 rural schools in 19 contiguous counties in Iowa, USA. Schools were selected on basis of school lunch eligibility program (15% or more of families eligible for free or reduced cost lunch) and community size (8,500 or less) Diagnostic criteria: Criteria were for schools (15% or more of district families eligible for free or reduced‐cost lunches) Age: grade 6; gender: not stated. |
|
| Interventions | Focus: tobacco, alcohol, marijuana prevention Intervention (1): Iowa Strengthening Families Program (ISFP, subsequently called "Iowa Strengthening Families Program for Parents and Youth") (11 schools, n=117): 7‐session programme (1 hour separate training for parent and child, second hour is a family session), and the 7th session is a one hour family session. Parents taught to clarify expectations, use appropriate discipline, manage strong emotions regarding their child, effectively communicate with their child; Children's sessions paralleled the parents' sessions but added peer resistance and peer relationship skills training. In the family sessions family members practised conflict resolution and communication skills and engaged in activities to increase family cohesiveness and positive involvement of the child in the family. (high intensity); Each team of leaders observed 2‐3 times; reliability checks on 50% of family sessions, 30% of youth sessions and 25% of parent (paired observers differed by average of 10%); coverage of topics 89% in youth, 87% in family, and 83% in parent sessions Intervention (2): Preparing for the Drug‐Free Years Program (PDFY, subsequently called "Guiding Good Choices") (11 schools, n=124): Five 2‐ hour sessions, with 4 parents‐only sessions: parents instructed on risk factors for substance abuse, developing clear guidelines on substance‐related behaviours, enhancing parent‐child bonding, monitoring compliance with their guidelines and providing appropriate consequences, managing anger and family conflict; and enhancing positive child involvement in family tasks; 1 child session instructed in peer resistance skills. (high intensity) Each team of group leaders observed for 2 of the 5 sessions; 50% of sessions observed by two observers (average difference on ratings 6%); average 69% coverage. (3) Control (11 schools, n=208): 4 mailed booklets (physical and emotional changes in adolescence, and parent‐child relationships). |
|
| Outcomes | Past year cigarette frequency on 7 point scale from 1 = not at all to 7 "about 2 packs/day" [also assessed were: Ever smoked, ever used chewing tobacco, cigarettes/day, and no. of times chewed tobacco in the past month]. Follow‐up at 4 yrs and 6 yrs. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Schools were blocked on the proportion of students who resided in lower income households and on school size. Within blocks, each school was randomly assigned to one of the three experimental conditions... Random assignment was computer‐generated by a data‐analyst..." Clusters: schools; Cluster constraint: blocked on the proportion of students who resided in lower income households and on school size Baseline comparability: no differences (Spoth 2001, Guyll 2004) |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1,309 eligible families recruited, and 667 (51%) completed pretest. Although only 447 (67%) remained at 4 years, there was no differential attrition across groups; a multiple imputation Monte Carlo software programme (NORM) showed that attrition did not affect the findings; there was also no differential attrition after 6 years (Spoth 2004) |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Performance bias: minimal risk: (a) for ISFP programme, 94% of attending families were represented by 1 family member in 5 or more sessions, and all key programme concepts were covered; (b) for PDFY programme all teams covered all key concepts, and completed 69% of the detailed tasks in the group leaders' manual. 93% of families attended at least 4/5 sessions. 87% of activities covered in the family sessions, 83% in the parent sessions, and 89% in the youth sessions |
Spoth 2002.
| Methods | Study design: C‐RCT, randomised block design. Analysis: multilevel analyses of covariance (hierarchical linear modelling) , with school as a random effect and dual biological parent families as a covariate (only significant difference between groups at baseline). Allocation was at the school level and multilevel analysis controlled for the effects of clustering. Repeated measures with linear slope contrasts. Intent‐to‐treat analysis. No power computation. Post‐test measures used as baseline. Total duration of study: 5 1/2 years | |
| Participants | Total number: 1677 7th graders randomly assigned and 1664 completed pretest. Setting: 36 rural schools in 22 contiguous counties in Iowa, USA (selected from 43 eligible schools, those selected were those with 20% of more of households eligible for free or reduced cost lunches, all middle grades taught at one location, and school district enrolment < 1200); Age: 7th graders; Gender 47%F; 96% white. |
|
| Interventions | Focus: family‐ and school‐based competency training to prevent uptake of alcohol, tobacco and marijuana. Intervention (1): Strengthening Families Program for Parents and Youth 10‐14 (SFP 10‐14): revision of the Iowa Strengthening Families Program; 7 1‐hr weekly sessions for parents and children to strengthen parental skills in nurturing, setting limits and communication about substances, and strengthen children's prosocial and peer resistance skills. 4 booster sessions offered 1 yr later. Each team of facilitators observed on 2‐3 occasions; observers differed by average 2.4%; average adherence 92% (high intensity) Intervention (2): Life Skills Training (LST): 15 x 45‐min classes + homework to provide knowledge about substance abuse, and promote youth skills in social resistance, self‐management and general social skills, using coaching, facilitating, role modelling, feedback and reinforcement. 5 booster sessions in 8th grade. Each classroom teacher observed on 2‐3 occasions; observers differed by average 13.6%; average adherence 85% 12 schools received LST (n=621), 12 received LST + SFP 10‐14 (n=549). (3) Control (n=494): no statement if received any anti‐tobacco intervention. | |
| Outcomes | Self‐reported never smoking at 1 yr after post‐test assessment; 'bogus pipeline' CO monitoring at all assessments (i.e. data collected but not assessed, to encourage honest reporting) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Within each school, children and teachers were randomly assigned to one of two intervention or control classrooms." (an e‐mail from Dr. Ialongo states that a SAS programme generated the class lists and randomly assigned students; that children and teachers were randomly assigned to 1st grade within each of the 9 participating schools; and that there was balancing for gender and kindergarten teacher ratings of aggressive disruptive behaviour and academic readiness). Baseline comparability: Children in control group somewhat less likely to be male, and African American, more likely to be from 2 parent households, teacher ratings of problem behaviour higher in CC group; these differences were statistically adjusted in the analyses. Clusters were classrooms and cluster constraints were: "A randomised block design was employed, with each of the nine schools serving as a blocking factor..." "Criteria for selection of the initial pool of schools were: 20% or more of households in the school district within 185% of the federal poverty level; community size (school district enrolment under 1,200, and all middle school grades (6‐8) taught at one location... After we matched the schools and randomly assigned them to conditions..." (Spoth 2002); "... experimental assignment, which was guided by a randomised block design. Based on school‐level risk measures calculated from data collected through a prospective telephone survey of randomly selected parents of eligible children, the schools were split into 12 matched sets of three." (Spoth 2008). Baseline comparability: groups equivalent at baseline on smoking |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "No significant Dropout x Condition interactions for pre‐to posttesting or from posttesting to the follow‐up assessment, for any outcome or socio‐demographic measure." Spoth 2002 (used "listwide deletion of missing data"): totals: baseline 1664, posttest 1563, 1 yr follow‐up in 8th grade 1372 (LST pretest 621, posttest 583, 1 yr follow‐up 503) (LST+SFP: pretest 549, posttest 517, 1 yr follow‐up 453) (Control: pretest 494, posttest 463, 1 yr follow‐up 416); Trudeau 2003 ‐ same data. Spoth 2008: (used multiple imputation for missing data, so N's larger than for Spoth 2002): totals: baseline 1677, posttest 1690, 1 yr follow‐up 1633; 12 th grade follow‐up 1237) (LST pretest 622, posttest 618, 1 yr follow‐up 583, 12th grade 428)(LST+SFP: pretest 543, posttest 554, 1 yr follow‐up 539, 12 th grade follow‐up 450), (control: pretest 489, posttest 496, 1 yr follow‐up 488, 2th grade follow‐up 347), ("undetermined" pretest 23, 8th grade 23, 12th grade 12). No differential drop out between groups Expired air samples were collected but not analysed |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Performance bias: adherence to the SFP programme was 92%, and to the LST programme 85%. Of the students who participated, the percentages attending 50% or more of the lessons were 100% for the LST programme + 100% for the boosters; 90% for the SFP 10‐14 programme + 89% for the boosters. |
Stevens 2002.
| Methods | Study design: RCT. Practices matched by size and randomised within each pair using computer‐generated random numbers. Two intervention arms, no usual‐care control group. No power computation. Analysis: Chi squared and t tests to check for baseline differences, baseline factors potentially related to outcomes controlled for by logistic regression analyses. | |
| Participants | Total number: 4096 families approached by participating primary care physicians; 3525 (86%) agreed to participate; 3094 (77%) 5th and 6th graders and their parents completed the baseline assessment; 2183 36 month follow‐up (71% of those completing baseline questionnaire) Setting: 12 primary care paediatric practices in Massachusetts, New Hampshire and Vermont, USA; Age avg 11; Gender 48% F; 5% ever smokers at baseline |
|
| Interventions | Focus: Dartmouth Prevention Cohort Study: prevention of risky adolescent behaviours (smoking , drinking) and bicycle helmet use, gun storage and seatbelt use, by office‐based paediatric interventions. Intervention (1): Clinician advice about alcohol and tobacco. (low intensity). Intervention (2): Clinician advice about gun safety, bicycle helmets and car seatbelts. Pediatricians and nurse practitioners received 3 hr training session. All the practice staff encouraged family communication and rule setting about the issues. Families received a brochure on effective communication and pens, card games or fridge magnets to reinforce the message; children and parents each received 12 quarterly newsletters to reinforce the messages. The practices received a monthly message based on chart audits, phone calls and visits from the research co‐ordinator. Paediatrician, parent and child signed a contract committing family to discuss the issues at home and to develop a policy about the relevant behaviours. Families received a follow‐up signed letter from clinician, and a fridge magnet to 'post' the policy document. |
|
| Outcomes | Ever smoking at 12m, 24m, 36m follow‐up, on 2183 child‐parent pairs. | |
| Notes | Performance bias: minimal risk: High level of process evaluation by research staff. After the initial intervention visits 95% of children were seen for subsequent visits, during which prevention messages were delivered in only 47% of the practices allocated to the safety intervention and 51% of those allocated to the alcohol/tobacco intervention. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 12 paediatric practices paired by practice size and computer assigned randomly within pairs |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Baseline 3,525 5th/6th grade children and parents. 36 month follow‐up on 2,183 child parent pairs. Monthly and end of project chart audits of at least 10% of charts to check number of encounters recorded. Parens and children surveyed whether they had read newspapers, liked them, and found them useful. No statement if differential attrition or implementation. 99% of charts labelled with project sticker, 95% of children had been seen for an office visit, and in 51% of the tobacco/alcohol arm and 47% of safety arm visits prevention message was documented |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Individual counselling by paediatrician or nurses so no concern for clustering. No other biases identified |
Storr 2002.
| Methods | Study design: C‐RCT, schools as blocks, pupils randomly assigned within each school. Power computation: estimated that 150 children per group would be needed. With an average 30% cumulative risk of initiating smoking, between‐group relative risk of initiating smoking is 1.75; and alpha 0.05, 2‐tailed for 80% power. Analysis: Life table and survival analysis to compare risk of starting to smoke across study groups. Cox regression model for time to event data to estimate effect of interventions. Statistical adjustment for baseline covariates with Cox regression models. Intention to treat analysis. Discrete Time Survival Analyses. No adjustment for clustering for CC data, no need for clustering adjustment for individual FSP data., Total study duration: 7 years |
|
| Participants | Total number: Baseline: 678 first graders Setting: 9 public primary schools in Baltimore. Maryland, USA. Age avg 5.7 yrs; Gender 53% M; 86% African‐American. |
|
| Interventions | (1): Classroom‐Centered (CC) Intervention (n=230): 'Universal Preventive intervention' targeting attention problems, aggressive & shy behaviour (a) language and mathematics curricula enhanced to encourage skills in critical thinking, composition, listening and comprehension; (b) whole‐class strategies to encourage problem solving by children in group contexts, decrease aggressive behaviour, and encourage time on task; (c) strategies for children not performing adequately. Teams of children received points for good behaviour and lost points for behaviours such as starting fights; the points could be exchanged for classroom activities, game periods and stickers. CC implementation mean score 59.9%, median score 64.4% (range 30‐78%)
Intervention (2): Family‐School Partnership (FSP) intervention (n=229): (a) the 'Parents on Your Side Program' trained teachers to communicate with parents and build partnerships, with 3‐day workshop, training manual and follow‐up supervisory visits; (b) weekly home‐school learning and communicating activities; (c) 9 workshops for parents (first two workshops to establish an effective and enduring parent‐staff relationship and facilitate children's learning and behaviour; next 5 workshops focused on effective disciplinary strategies). (although high intensity for contact, is assessed as moderate intensity as no description of tobacco‐focused content). Parents attended average 4/7, median 5/7 core parenting sessions, 13% attended none. First grade CC and FSP teachers received 60 hours training and certification. (3) Control group (n=219): usual curriculum and parent‐teacher communications. |
|
| Outcomes | Self‐reported smoking assessed 7 years after initiation of project, when they were 13 years of age; time to initiation of smoking (longest follow‐up reported in Furr‐Holden 2004) | |
| Notes | Performance bias: implementation scores for the CC intervention averaged 60% (range 30 to 78%); 7/9 CC teachers implemented > 50% of the Protocol. Parents in the FSP intervention attended an average of 4/7 sessions (range 13% attended no workshops, 35% attended 6/7). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Within each school, children and teachers were randomly assigned to one of two intervention or control classrooms." (an e‐mail from Dr. Ialongo states that an SAS programme generated the class lists and randomly assigned students; that children and teachers were randomly assigned to 1st grade within each of the 9 participating schools; and that there was balancing for gender and kindergarten teacher ratings of aggressive disruptive behaviour and academic readiness). Clusters: classrooms; Cluster constraints: "A randomised block design was employed, with each of the nine schools serving as a blocking factor..." Baseline comparability: Children in control group somewhat less likely to be male, and African American, more likely to be from 2 parent households, teacher ratings of problem behaviour higher in CC group; these differences were statistically adjusted in the analyses. |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No statement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Storr 2002 (Figure 1): Of the 678 pupils who entered Grade 1, 549 at 6 year (7th grade) follow‐up (189 CC, 192 FS, 168 control); Furr‐Holden 2004 reported ‐ "At follow‐up, 5, 6, 7 years after randomisation (sixth through eighth grades), approximately 84% (566/678) of the sample was available." No differential attrition among groups across baseline characteristics or smoking status. |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Generalized Estimating Equations assessed for clustering. No other biases ascertained |
Wu 2003.
| Methods | Study design: C‐RCT, randomised at level of site. Analysis: Chi squared and Kruskal‐Wallis tests to assess baseline equivalence of demographic characteristics. General linear modelling for differences in behaviour and perceptions among intervention groups. Independent sample t tests corrected for ICCs for each behaviour to adjust for clustering. No power computation. Total study duration: 24 months |
|
| Participants | Total number; 817 African‐American youths Setting: 35 low income housing developments, community and recreation centres in Baltimore, Maryland, USA. Diagnostic criteria: Housing development tenant association members and recreation centre staff recruited "eligible" youth and parents Age 12‐16 years (median 14 years); Gender 58% F. |
|
| Interventions | Focus: Effect of adding parental monitoring and booster sessions to small‐group risk reduction interventions for adolescents. Intervention (1): Focus on Kids (FOK), (n = 321): 8 session (each 1.5 hours) HIV small‐group risk reduction programme on decision making, goal setting, communicating, negotiating, and consensual relationships and information regarding safe sex, drugs, alcohol and drug selling. Conducted in small groups (5‐10), led by 2 older peers, with games, discussions, homework assignments and videotapes. Intervention (2): (n = 258) (a) FOK + (b) ImPACT (Informed Parents and Children Together): 20‐min video emphasising concepts of parental monitoring and communicating with 2 instructor‐led role‐playing vignettes between the parent and youth in the child's home. The interventionist critiques the role play according to the main talking points of the videotape and conducts a condom demonstration. Intervention (3): (n= 238) (a) FOK + (b) 4 FOK booster sessions at 6m and 10m + (c) + ImPACT Focus on Kids has a minor informational component about tobacco and no family component. ImPACT is 20 minute video followed by role plays between parent and youth, then criticised by interventionist. It has no tobacco focus, but baseline and 24 months smoking were measured for all 3 programmes. ImPACT assessed as low intensity. |
|
| Outcomes | Cigarette use: self‐reported smoking in last 6m (not further defined) measured as 0 = no, 1 = yes Other outcomes: sexual intercourse; unprotected sex; alcohol, drugs, selling or delivering drugs; carrying a knife, fighting, beating someone up, or intention to take a risk. Assessment on Parent Adolescent Communication Scale Follow‐up at 6m,12m, 24m (Reported in Stanton 2004). |
|
| Notes | Performance bias: no process analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised using random number table. "Intervention groups were similar for sex and age at baseline." |
| Allocation concealment (selection bias) | Unclear risk | No statement |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No statement |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "Questionnaires administered orally and visually by computer." No statement about blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Baseline: 817 youths 12‐16 years (Intervention 1 = 321; Intervention 2 = 496). Of 496 intervention, 238 randomised to receive booster session, 238 no booster. At 12 months follow‐up Intervention 1 = 243, Intervention 2 = 337. Stanton 2004: "...the baseline demographic and risk‐protective behaviours of youths absent at 24 months were comparable across intervention groups. That is, despite the dropout rate, the baseline risk profile remained equivalent across intervention groups." |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Other bias | Low risk | Informed Parents and Children Together (ImPACT) is delivered as videotape then interactive role playing between parent and youth, so no concern for clustering for the family component. The Focus on Kids (FOK) component was delivered in groups. All outcomes adjusted for clustering. ICC for tobacco = 0.0000. No other biases identified |
ALA: American Lung Association CDC: Centers for Disease Control CO: carbon monoxide C: control
cig.: cigarette F: female GEE: Generalized Estimating Equations GP: general practitioner HDL: high density lipid HMO: Health Maintenance Organization I: intervention m: month M: male no.: number SES: socio‐economic status
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abdullah 2005 | RCT; but intervention is to help parents of young children stop smoking; no assessment of children's smoking |
| Albrecht 2006 | RCT; tobacco outcomes; no prevention, only cessation |
| Allendorf 1985 | RCT; parent intervention, but no outcome data on tobacco |
| Ariza 2008 | Not RCT; cannot separate effects of family intervention |
| Beatty 2008 | Study did not assess smoking status |
| Biglan 2000 | Family intervention not separately analysable |
| Broning 2014 | RCT; tobacco use results not reported |
| Brotman 2008 | RCT; no tobacco intervention or outcomes |
| Byrnes 2010 | RCT; family and tobacco intervention; no tobacco outcomes |
| Charlier 2009 | Not RCT, no tobacco outcomes |
| Cohen 1989 | Effects of parental interventions cannot be separated from school interventions |
| Cohen 1995 | RCT; Only 6% of families began the intervention |
| Cruz 2009 | Not RCT; tobacco intervention; cannot separate effect of parental component |
| DeGarmo 2009 | RCT. Not possible to separate family and school effects in the school‐based "Linking the Interests of Families and Teachers Multimodal Preventive Intervention." |
| Eckenrode 2010 | Intervention was delivered to mothers during the first 2 years after birth only |
| Ellickson 2003 | Effects of parental interventions cannot be separated from school interventions |
| Faggiano 2008 | RCT; school based; no family intervention |
| Flay 1988 | Family intervention not separately analysable |
| Glover 2009 | Not RCT |
| Gordon 2008 | Family intervention effects not separately analysed |
| Hahn 2007 | RCT; parent intervention; Babies, hence no tobacco outcomes. |
| Hansen 1987 | Family intervention not separately analysable |
| Hansen 1991 | Cannot separate effects of parent interview homework from schools intervention |
| Hawkins 1999 | Not RCT (CCT). New for 2008 update. |
| Hawkins 2009 | RCT, Tobacco outcomes, community intervention; cannot separate effects of family component on tobacco outcomes |
| Horn 2007 | RCT; smoking cessation. New for 2008 update. |
| Jackson 1994 | Survey, not RCT |
| Johnson 1990 | RCT; tobacco outcomes; cannot separate effects of family intervention from school intervention. New for 2008 update. |
| Jowers 2007 | RCT; Keep A Clear Mind programme; no tobacco outcomes |
| Knutsen 1991 | Fathers were randomised, and children with them. No baseline smoking data for children |
| Komro 2008 | RCT; schools, no specific tobacco intervention; tobacco, alcohol and marijuana outcomes combined; no reply to e‐mail to authors 13 December 2013 asking if could provide separate tobacco outcomes |
| Kristjansson 2010 | Not RCT; National community‐wide intervention programme, no family intervention; tobacco outcomes, assessed by a series of national surveys. |
| Krohn 1983 | Survey, not RCT |
| Kumpfer 2012 | Not RCT |
| Litrownik 2000 | RCT; pre‐ and post ‐assessment at 8 weeks. Follow‐up not long enough |
| Lochman 2002 | RCT; family intervention; no tobacco outcomes. New for 2008 update. |
| Moncher 1994 | RCT; cannot separate outcomes of family from community intervention |
| Nilsson 2006 | RCT; tobacco intervention; cannot separate effect of parents in the "Tobacco Free Duo" as adolescents could be linked with school staff, a parent or a significant other adult |
| Nutbeam 1993 | Excluded from 2015 update. Not possible to separate the effects of the minimal family intervention from the school intervention. The second school intervention had different components so cannot be used as a non‐family control. |
| O'Byrne 2002 | Survey, not RCT |
| Olds 2010 | Intervention was delivered to mothers during the first 2 years of birth only. Smoking not measured in children |
| Parsai 2009 | RCT; secondary analysis of RCT, tobacco outcomes; parental monitoring was not randomly allocated but used as an analytic variable |
| Patten 2006 | RCT, cessation |
| Pentz 1989 | Not RCT (CBA) |
| Pentz 2013 | RCT; adolescents; tobacco is included in substance use outcome measure; no reply to e‐mail 13 December 2013 to authors requesting separate outcome data for tobacco |
| Perry 1990 | Not an RCT |
| Perry 2003 | RCT; D.A.R.E. Plus program consists of: (a) 4 session classroom program "On the Verge," (b) home team activities with parents, (c) theatre productions in classrooms, (d) 3 postcards to students, and (e) 10 postcards to parents. Cannot separate effects of parental from school components. |
| Perry 2009 | RCT; tobacco intervention; cannot separate effects of family intervention |
| Piper 2000 | No parental intervention |
| Ramchand 2006 | Not RCT (follow‐up of cohort); tobacco outcomes; no family intervention. New for 2008 update. |
| Rohrbach 1994 | RCT; Cannot separate out effect of parental intervention from school intervention |
| Rohrbach 2002 | Parents not randomly assigned to experimental control groups |
| Rosati 2012 | No tobacco outcomes |
| Salminen 2005 | Not an RCT. "the members of the ethics committee felt that the randomization of the high‐risk families into an intervention and a control group would be unethical." "this lack of randomization is a drawback of the study," |
| Schinke 1988 | RCT; cannot separate outcomes of family from community intervention |
| Schinke 2000 | RCT; cannot separate outcomes of family from community intervention |
| Schinke 2009 | RCT; family intervention; no tobacco intervention or outcomes |
| Severson 1991 | Effects of quiz given to parents by students, and messages mailed to parents cannot be separated from the school intervention |
| Simons‐Morton 2005 | RCT; but cannot separate effects of parent component |
| Soper 2010 | RCT; e‐mail from Dr. Wolchik indicated smoking status not ascertained at baseline; RCT randomised families to: (1) Mother program (MP) n = 81; Program for mothers: strategies to improve mother‐child relationship quality, effective discipline, interparental conflict, father‐child contact; Program for children: active coping, avoidant coping, coping efficacy, negative errors, quality of mother‐child relationship (2) Mother program plus Child Coping program (MPCP) n =83; MP program plus: books and syllabi related to coping with divorce (3) Control: Literature Comparison condition n = 76 |
| Spoth 2007 | RCT; tobacco outcomes; cannot separate effects of family from school interventions. E mail to Dr. Spoth 13 December 2013 enquiring if could obtain data before school intervention was commenced and no reply. |
| Stevens 1993 | Not RCT (CBA) |
| Tang 1997 | Not RCT (CBA) |
| Tingen 2006 | Not an RCT; cannot separate effects of family component from Georgia Quit Line telephone help line |
| Vartiainen 2007 | RCT; cannot separate effects of family intervention from schools intervention. |
| Vitória 2011 | Tobacco outcomes but cannot separate effects of family intervention. Design: authors state "A quasi‐experimental study was then conducted, randomly selecting areas (groups of neighbouring cities) to define control and intervention conditions. A total of two areas with comparable sociogeographic characteristics were established, although physically separated from each other to prevent results from being contaminated. In these areas, there were 64 schools, all invited to participate. Through random selection, the southern area became the control condition (11 schools from the counties of Moita, Seixal and Barreiro) and the northern area became the intervention condition (14 schools from the counties of Loures and Odivelas). ... All 7th grade classes of these 25 schools participated." |
| Wakschlag 2011 | Not RCT: observational substudy of the large “Social Emotional Contexts of Adolescent Smoking Patterns” longitudinal study of 1,263 youth |
| Wen 2007 | Not RCT; intervention is to reduce parental smoking |
| Werch 1991 | RCT; did not measure children's smoking behaviour, only intentions to smoke |
| Werch 2005 | RCT; but no family intervention: the flyer mailed to the home did not involve the parents or other family members explicitly, and the effects of the flyer cannot be separated from the individual counselling in school |
| Werch 2010 | RCT; tobacco intervention and outcomes; only 3 month follow‐up |
| Wilson 2012 | Parents provided consent, only family involvement is discussing Fruit & Vegetable preparation |
| Wilson 2013 | Interviews with 17 mothers in Scotland about reducing second‐hand smoke at home |
| Yilmaz 2013 | RCT; physician intervention with families to create smoke‐free house; urinary cotinine levels measured after 12 months |
| Young 1996 | RCT; did not measure children's smoking behaviour, only intentions to smoke |
| Zavela 2004 | Not an RCT; cannot separate effect of family intervention |
CBA: controlled before and after
Differences between protocol and review
None
Contributions of authors
RET conceived and designed the review. RET, PB, BCT and DL checked titles and abstracts for inclusion, retrieved studies and extracted data. Lindsay Stead performed multiple searches. RET performed the data analyses and wrote the text. All authors contributed to the content of the review.
Declarations of interest
None to declare
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Ary 1990 {published data only}
- Ary DV, Biglan A, Glasgow E, Zoref L. The efficacy of social‐influence prevention programs versus "standard care": Are new initiatives needed?. Journal of Behavioral Medicine 1990;13:281‐96. [DOI] [PubMed] [Google Scholar]
Bauman 2001 {published data only}
- Bauman KE, Ennett ST, Foshee VA, Pemberton M, King TS, Koch GG. Influence of a family program on adolescent smoking and drinking prevalence. Prevention Science 2002;3(1):35‐42. [DOI] [PubMed] [Google Scholar]
- Bauman KE, Ennett ST, Foshee VA, Pemberton M, King TS, Koch GG. Influence of a family‐directed program on adolescent cigarette and alcohol cessation. Prevention Science 2000;1(4):227‐37. [DOI] [PubMed] [Google Scholar]
- Bauman KE, Foshee VA, Ennett ST, Pemberton M, Hicks KA, King TS, et al. The influence of a family program on adolescent tobacco and alcohol use. American Journal of Public Health 2001;91(4):604‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ennett ST, Bauman KE, Pemberton M, Foshee VA, Chuang Y‐C, King TS, et al. Mediation in a family‐directed program for prevention of adolescent tobacco and alcohol use. Preventive Medicine 2001;33:333‐46. [DOI] [PubMed] [Google Scholar]
Biglan 1987 {published data only}
- Biglan A, Glasgow RE, Ary DV, Thompson R, Severson H, Lichtenstein E, et al. How generalizable are the effects of smoking prevention programs? Refusal skills training and parent messages in a teacher‐administered program. Journal of Behavioral Medicine 1987;10(6):613‐28. [DOI] [PubMed] [Google Scholar]
Connell 2007 {published data only}
- Connell AM. Employing complier average causal effect analytic methods to examine effects of randomized encouragement trials. The American Journal of Drug and Alcohol Abuse 2009;35(4):253‐259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell AM, Dishion TJ, Yasui M, Kavanagh K. An adaptive approach to intervention: Linking engagement in family‐centered intervention to reductions in adolescent problem behavior. Journal of Consulting and Clinical Psychology 2007;75(4):568‐79. [DOI] [PubMed] [Google Scholar]
Cullen 1996 {published data only}
- Cullen KJ, Cullen AM. Long‐term follow‐up of the Busselton six‐year controlled trial of prevention of children's behavior disorders. Journal of Pediatrics 1996;129:136‐9. [DOI] [PubMed] [Google Scholar]
Curry 2003 {published data only}
- Curry SJ, Hollis J, Bush T, Polen M, Ludman EJ, Grothaus L, et al. A randomized trial of a family‐based smoking prevention intervention in managed care. Preventive Medicine 2003;37(6):617‐26. [DOI] [PubMed] [Google Scholar]
Dishion 1995 {published data only}
- Dishion TJ, Andrews DW. Preventing escalation in problem behaviors with high‐risk young adolescents: immediate and 1‐year outcomes. Journal of Consulting and Clinical Psychology 1995;63(4):538‐48. [DOI] [PubMed] [Google Scholar]
- Poulin F, Dishion TJ, Kavanagh, Kiesner J. The prevention of behaviour problems in adolescence: the Adolescence Transition Program [La prévention des problèmes de comportement à l'adolescence: Le Adolescent Transition Program]. Criminologie 1998;31(1):67‐85. [Google Scholar]
Elder 1996 {published data only}
- Elder JP, Perry CL, Stone EJ, Johnson CC, Yang M, Edmundson EW, et al. Tobacco use measurement, prediction, and intervention in elementary schools in four states: The CATCH study. Preventive Medicine 1996;25:486‐94. [DOI] [PubMed] [Google Scholar]
- Johnson CC, Osganian SK, Budman SB, Lytle LA, Barrera EP, Bonura SR, et al. CATCH: family process evaluation in a multicenter trial. Health Education Quarterly 1994;Suppl 2:S91‐106. [DOI] [PubMed] [Google Scholar]
- Perry CL, Parcel GS, Stone E, Nader PR, McKinlay SM, Luepker RV, et al. The Child and Adolescent Trial for Cardiovascular Health (CATCH): Overview of the intervention program and evaluation methods. Cardiovascular Risk Factors 1992;2(1):36‐44. [Google Scholar]
Fang 2013 {published and unpublished data}
- Fang L, Schinke SP. Alcohol use among Asian American adolescent girls: The impact of psychological and family factors. Journal of Ethnicity in Substance Abuse 2011;10:275‐294. [DOI] [PubMed] [Google Scholar]
- Fang L, Schinke SP. Two‐year outcomes of a randomized, family‐based substance use prevention trial for Asian American adolescent girls. Psychology of Addictive Behaviors 2013;27(3):788‐798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang L, Schinke SP, Cole KCA. Preventing substance use among early Asian‐American adolescent girls: Initial evaluation of a web‐based mother‐daughter program. Journal of Adolescent Health 2010;47:529‐532. [DOI] [PMC free article] [PubMed] [Google Scholar]
Forman 1990 {published data only}
- Forman SG, Linney JA, Brondino MJ. Effects of coping skills training on adolescents at risk for substance use. Psychology of Addictive Behaviors 1990;4(2):67‐76. [Google Scholar]
Fosco 2013 {published and unpublished data}
- Fosco GM, Frank JL, Stormshak EA, Dishion TJ. Opening the "Black Box": Family Check‐Up intervention effects on self‐regulation that prevents growth in problem behavior and substance use. Journal of School Psychology 2013;51:455‐468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stormshak EA, Connell AM, Véronneau M‐H, Myers MW, Dishion TJ, Kavanagh K, et al. An ecological approach to promoting early adolescent mental health and social adaptation: Family‐centered intervention in public middle schools. Child Development 2011;82(1):209‐225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stormshak EA, Fosco GM, Dishion TJ. Implementing interventions with families in schools to increase youth school engagement: The Family Check‐Up model. School Mental Health 2010;2(2):82‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guilamo‐Ramos 2010 {published data only}
- Guilamo‐Ramos V, Jaccard J, Dittus P, Gonzalez B, Bouris A, Banspach S. The Linking Lives health education program: a randomized clinical trial of a parent‐based tobacco use prevention program for African American and Latino youths. American Journal of Public Health 2010;100(9):1641‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haggerty 2007 {published data only}
- Haggerty KP, Skinner ML, MacKenzie EP, Catalano RF. A randomized trial of Parents Who Care: Effects on key outcomes at 24‐month follow‐up. Prevention Science 2007;8:249‐60. [DOI] [PubMed] [Google Scholar]
Hiemstra 2014 {published data only}
- Hiemstra M, Otten R, Schayck OCP, Engels RCME. Smoking‐specific communication and children's smoking onset: An extension of the theory of planned behavior. Psychology & Health 2013;27(9):1100‐1117. [DOI] [PubMed] [Google Scholar]
- Hiemstra M, Ringlever L, Otten R, Schayck OCP, Engels RCME. Short‐term effects of a home‐based smoking prevention program on antismoking socialization and smoking‐related cognitions: A cluster randomized controlled trial.. European Addiction Research 2013;19:128‐140. [DOI] [PubMed] [Google Scholar]
- Hiemstra M, Ringlever L, Otten R, Schayck OCP, Jackson C, Engels RCME. Long‐term effects of a home‐based smoking prevention program on smoking initiation: A cluster randomized controlled trial. Preventive Medicine 2014;60:65‐70. [DOI] [PubMed] [Google Scholar]
- Hiemstra M, Ringlever L. Otten R, Jackson C, Schayck OCP, Engels RCME. Efficacy of smoking prevention program `Smoke‐free Kids`: study protocol of a randomized controlled trial. BMC Public Health 2009;9:477. [DOI: 10.1186/1471-2458-9-477] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jackson 2006 {published data only}
- Jackson C, Dickinson D. Can parents who smoke socialise their children against smoking? Results from the Smoke‐free Kids intervention trial. Tobacco Control 2003;12(1):52‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson C, Dickinson D. Enabling parents who smoke to prevent their children from initiating smoking. Results from a 3‐year intervention evaluation. Archives of Pediatric and Adolescent Medicine 2006;160:56‐62. [DOI] [PubMed] [Google Scholar]
Jøsendal 1998 {published data only}
- Jøsendal O, Aarø LE, Bergh I. Effects of a school‐based smoking prevention program among subgroups of adolescents. Health Education Research 1998;13:215‐24. [DOI] [PubMed] [Google Scholar]
- Jøsendal O, Aarø LE, Torsheim T, Rasbash. Evaluation of the school‐based smoking‐prevention program "Be smokeFree". Scandinavian Journal of Psychology 2005;46:189‐99. [DOI] [PubMed] [Google Scholar]
Olds 1998 {published data only}
- Olds DL, Henderson Jr CR, Cole R, Eckenrode J, Kitzman H, Luckey D, et al. Long‐term effects of nurse home visitation on children's criminal and antisocial behavior: 15‐year follow‐up of a randomized controlled trial. JAMA 1998;280(14):1238‐44. [DOI] [PubMed] [Google Scholar]
Pierce 2008 {published and unpublished data}
- Pierce JP, James LE, Messer K, Myers MG, Williams RE, Trinidad DR. Telephone counseling to implement best parenting practices to prevent adolescent problem behaviors. Contemporary Clinical Trials 2008;29:324‐334. [DOI] [PMC free article] [PubMed] [Google Scholar]
Prado 2007 {published data only}
- Prado G, Pantin H, Briones E, Schwartz SJ, Feaster D, Huang S, et al. A randomized controlled trial of a parent‐centered intervention in preventing substance use and HIV risk behaviors in Hispanic adolescents. Journal of Consulting and Clinical Psychology 2007;75(6):914‐926. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reddy 2002 {published data only}
- Reddy KS, Arora M, Perry CL, Nair B, Kohli A, Lytle LA, et al. Tobacco and alcohol use outcomes of a school‐based intervention in New Delhi. American Journal of Health Behavior 2002;26(3):173‐81. [DOI] [PubMed] [Google Scholar]
Riesch 2012 {published data only}
- Riesch SK, Brown RL, Anderson LS, Wang K, Canty‐Mitchell J, Johnson DL. Strengthening Families Program (10‐14) effects on the family environment. Western Journal of Nursing Research 2012;34:340‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schinke 2004 {published data only}
- Schinke SP, Schwinn TM, Noia J, Cole KC. Reducing the risks of alcohol use among urban youth: three‐year effects of a computer‐based intervention with and without parent involvement. Journal of Studies in Alcohol 2004;65:443‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Spoth 2001 {published data only}
- Guyll M, Spoth RL, Chao W, Wickrama KAS, Russell D. Family‐focused preventive interventions: Evaluating parental risk moderation of substance use trajectories. Journal of Family Psychology 2004;18(2):293‐301. [DOI] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C, Azevedo K. Brief family intervention effects on adolescent substance initiation: School‐level growth curve analyses 6 years following baseline. Journal of Counseling and Clinical Psychology 2004;72:535‐42. [DOI] [PubMed] [Google Scholar]
- Spoth R, Reyes ML, Redmond C, Shin C. Assessing a public health approach to delay onset and progression of adolescent substance use: Latent transition and log‐linear analyses of longitudinal family preventive intervention outcomes. Journal of Consulting and Clinical Psychology 1999;67(5):619‐30. [DOI] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Guyll M, Shin C, Redmond C. Universal intervention effects on substance use among young adults mediated by delayed adolescent substance initiation. Journal of Consulting and Clinical Psychology 2009;77(4):620‐632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth RL, Redmond C, Shin C. Randomized trial of brief family interventions for general populations: adolescent substance use outcomes 4 years following baseline. Journal of Consulting and Clinical Psychology 2001;69(4):627‐42. [DOI] [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Randall GK. Longitudinal effects of a universal family‐focused intervention on growth patterns of adolescent internalizing symptoms and polysubstance use: Gender comparisons. Journal of Youth and Adolescence 2007;36:725‐740. [Google Scholar]
Spoth 2002 {published data only}
- Spoth R, Randall GK, Shin C, Redmond C. Randomized study of combined universal family and school preventive interventions: Patterns of long‐term effects on initiation, regular use, and weekly drunkenness. Psychology of Addictive Behaviors 2005;19(4):372‐381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth RL, Randall GK, Trudeau L, Shin C, Redmond C. Substance use outcomes 5½ years past baseline for partnership‐based,family‐school preventive interventions. Drug and Alcohol Dependence 2008;96:57‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth RL, Redmond C, Trudeau L, Shin C. Longitudinal substance initiation outcomes for a universal preventive intervention combining family and school programs. Psychology of Addictive Behaviors 2002;16(2):129‐34. [PubMed] [Google Scholar]
- Trudeau L, Spoth R, Lillehoj C, Redmond C, Wickrama KAS. Effects of a Preventive Intervention on Adolescent Substance Use Initiation, Expectancies, and Refusal Intentions. Prevention Science 2003;4(2):109‐122. [DOI] [PubMed] [Google Scholar]
Stevens 2002 {published data only}
- Jones DJ, Olson AL, Forehand R, Gaffney CA, Zens MS, Bau JJ. A family‐focused randomized controlled trial to prevent adolescent alcohol and tobacco use: The moderating roles of positive parenting and adolescent gender. Behavior Therapy 2005;36:347‐355. [Google Scholar]
- Stevens MM, Olson AL, Gaffney CA, Tosteson TD, Mott LA, Starr P. A pediatric, practice‐based, randomized trial of drinking and smoking prevention and bicycle helmet, gun, and seatbelt safety promotion. Pediatrics 2002;109(3):490‐7. [DOI] [PubMed] [Google Scholar]
Storr 2002 {published data only}
- Furr‐Holden CDM, Ialongo NS, Anthony JC, Petras H, Kellam SG. Developmentally inspired drug prevention: middle school outcomes in a school‐based randomized prevention trial. Drug and Alcohol Dependence 2004;73:149‐58. [DOI] [PubMed] [Google Scholar]
- Ialongo N, Poduska J, Werthamer L, Kellam S. The distal impact of preventive interventions on conduct problems and disorder in early adolescence. Journal of Emotional Behavior Disorders 2001;9:146‐160. [Google Scholar]
- Ialongo NS, Werthamer L, Kellam SG. Proximal impact of two first‐grade preventive interventions on the early risk behaviors for later substance abuse, depression and antisocial behavior. American Journal of Community Psychology 1999;27(5):599‐641. [DOI] [PubMed] [Google Scholar]
- Storr CL, Ialongo NS, Kellam SG, Anthony JC. A randomized controlled trial of two primary school intervention strategies to prevent early onset tobacco smoking. Drug and Alcohol Dependence 2002;66(1):51‐60. [DOI] [PubMed] [Google Scholar]
- Wang Y, Browne DC, Petras H, Stuart EA, Wagner FA, Lambert SF, et al. Depressed mood and the effect of two universal first grade interventions on survival to the first cigarette smoked among urban youth. Drug and Alcohol Dependence 2009;100:194‐203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Storr CL, Green KM, Zhu S, Stuart EA, Lynne‐Landsman SD, et al. The effect of two elementary school‐based prevention interventions on being offered tobacco and the transition to smoking. Drugs and Alcohol Dependence 2012;120:202‐208. [DOI: 10.1016/j.drugalcdep.2011.07.022] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2003 {published data only}
- Stanton B, Cole M, Galbraith J, Li X, Pendleton S, Cottrel L, et al. Randomized trial of a parent intervention: parents can make a difference in long‐term adolescent risk behaviors, perceptions, and knowledge. Archives of Pediatrics and Adolescent Medicine 2004;158:947‐55. [DOI] [PubMed] [Google Scholar]
- Wu Y, Stanton BF, Galbraith J, Kaljee L, Cottrell L, Li X. Sustaining and broadening intervention impact: a longitudinal randomized trial of 3 adolescent risk reduction approaches. Pediatrics 2003;111(1):e32‐e36. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Abdullah 2005 {published and unpublished data}
- Abdullah ASM, Lam TH, Mak YW, Loke AY. A randomized controlled trial of a smoking cessation intervention on parents of young children ‐ a preliminary report [POS2‐011]. Society for Research on Nicotine and Tobacco 10th Annual Meeting, Feb 18‐21, Phoenix Arizona. 2004.
- Abdullah ASM, Mak YW, Loke AY, Lam T‐H. Smoking cessation intervention in parents of young children: a randomised controlled trial. Addiction 2005;100:1731‐1740. [DOI] [PubMed] [Google Scholar]
Albrecht 2006 {published data only}
- Albrecht SA, Caruthers D, Patrick T, Reynolds M, Salamie D, Higgins LW, et al. A randomized controlled trial of a smoking cessation intervention for pregnant adolescents. Nursing Research 2006;55(6):402‐10. [DOI] [PubMed] [Google Scholar]
Allendorf 1985 {published data only}
- Allendorf S, Sunseri AJ, Cullinan J, Oman JK. Student heart health knowledge, smoking attitudes, and self‐ esteem. Journal of School Health 1985;55(5):196‐9. [DOI] [PubMed] [Google Scholar]
Ariza 2008 {published data only}
- Ariza C, Nebot M, Tomas Z, Gimenez E, Valmayor S, Tarilonte V, et al. Longitudinal effects of the European smoking prevention framework approach (ESFA) project in Spanish adolescents. European Journal of Public Health 2008;18(5):491‐497. [DOI] [PubMed] [Google Scholar]
Beatty 2008 {published data only}
- Beatty SE, Cross DS, Shaw TM. The impact of a parent‐directed intervention on parent‐child communication about tobacco and alcohol. Drug and Alcohol Review 2008;27(6):591‐601. [DOI] [PubMed] [Google Scholar]
Biglan 2000 {published data only}
- Biglan A, Ary DV, Smolkowski K, Duncan T, Black C. A randomised controlled trial of a community intervention to prevent adolescent tobacco use. Tobacco Control 2000;9:24‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Broning 2014 {published data only}
- Bröning S, Sack P‐M, Thomsen M, Stolle M, Wendell A, Stappenbeck J, Thomasius R. Implementing and evaluating the German adaptation of the “Strengthening Families Program 10 ‐ 14“– a randomized‐controlled multicentre study. BMC Public Health 2014;14:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brotman 2008 {published data only}
- Brotman LM, Gouley KK, Huang KY, Rosenfelt A, O'Neal C, Klein RG, et al. Preventive intervention for preschoolers at high risk for antisocial behavior: Long‐term effects on child physical aggression and parenting practices. Journal of Clinical Child and Adolescent Psychology 2008;37(2):386‐96. [DOI] [PubMed] [Google Scholar]
Byrnes 2010 {published data only}
- Byrnes HF, Miller BA, Aalborg AE, Plasencia AV, Keagy CD. Implementation fidelity in adolescent family‐based prevention programs: relationship to family engagement. Health Education Research 2010;25(4):531‐541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrnes HF, Miller BA, Laborde N. A comparison of maternal outcomes from an alcohol, tobacco, and other drug prevention program for mothers choosing an intervention versus being randomized. Health Education & Behavior 2013;40(2):206‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Charlier 2009 {published data only}
- Charlier N. Glover M. Robertson J. Keeping Kids Smokefree: lessons learned on community participation. Health Education Research 2009;24(6):949‐56. [DOI] [PubMed] [Google Scholar]
Cohen 1989 {published data only}
- Cohen RY, Felix MR, Brownell KD. The role of parents and older peers in school‐based cardiovascular prevention programs: implications for program development. Health Education Quarterly 1989;16(2):245‐53. [DOI] [PubMed] [Google Scholar]
Cohen 1995 {published data only}
- Cohen DA, Rice JC. A parent‐targeted intervention for adolescent substance use prevention ‐ lessons learned. Evaluation Review 1995;19(2):159‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cruz 2009 {published data only}
- Cruz GG, Ferrero MB, Coca IA, Maderuelo JA, García MT. Program for the prevention of smoking in secondary school students. Archivos de Bronconeumología 2009;45(1):16‐23. [DOI] [PubMed] [Google Scholar]
DeGarmo 2009 {published data only}
- DeGarmo DS, Eddy JM, Reid JB, Fetrow RA. Evaluating mediators of the impact of the Linking the Interests of Families and Teachers (LIFT) multimodal preventive intervention on substance use initiation and growth across adolescence. Prevention Science 2009;10(3):208‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eckenrode 2010 {published data only}
- Eckenrode J, Campa M, Luckey DW, Henderson CR, Cole R, Kitzman H, et al. Long‐term effects of prenatal and infancy nurse home visitation on the life course of youths: 19‐year follow‐up of a randomized trial. Archives of Pediatrics & Adolescent Medicine 2010;164:9‐15. [DOI] [PubMed] [Google Scholar]
Ellickson 2003 {published data only}
- Ellickson PL, McCaffrey DF, Ghosh‐Dastidar B, Longshore DL. New inroads in preventing adolescent drug use: results from a large‐scale trial of project ALERT in middle schools. American Journal of Public Health 2003;93(11):1830‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Faggiano 2008 {published data only}
- Faggiano F, Galanti MR, Bohrn K, Burkhart G, Vigna‐Taglianti F, Cuomo L, et al. The effectiveness of a school‐based substance abuse prevention program: EU‐Dap cluster randomized controlled trial. Preventive Medicine 2008;47:537‐543. [DOI] [PubMed] [Google Scholar]
- Faggiano F, Richardson C, Bohrn K, Galanti MR, EU‐Dap Study Group. A cluster randomized controlled trial of school‐based prevention of tobacco,alcohol and drug use: The EU‐Dap design and study population. Preventive Medicine 2007;44:170‐173. [DOI] [PubMed] [Google Scholar]
- Faggiano F, Vigna‐Tagliantia F, Burkhart G, Bohrn K, Cuomo L, Gregori D, et al. The effectiveness of a school‐based substance abuse prevention program:18‐Month follow‐up of the EU‐Dap cluster randomized controlled trial. Drug and Alcohol Dependence 2010;108:56‐64. [DOI] [PubMed] [Google Scholar]
- Kreeft P, Wiborg G, Galanti MR, Siliquini R, Bohrn K, Scatigna M, et al. ‘Unplugged’: a new European school programme against substance abuse. Drugs: education, prevention and policy 2009;16(2):167‐181. [Google Scholar]
- Vigna‐Taglianti F, Vadrucci S, Faggiano F, Burkhart G, Siliquini R, Galanti MR. Is universal prevention against youths' substance misuse really universal? Gender‐specific effects in the EU‐Dap school‐based prevention trial. Journal of Epidemiology and Community Health 2009;63(9):722‐728. [DOI] [PubMed] [Google Scholar]
Flay 1988 {published data only}
- Flay BR, Brannon BR, Johnson CA, Hanson WB, Ulene AL, Whitney‐Saltiel DA, et al. The television school and family smoking prevention and cessation project. I. Theoretical basis and program development. Preventive Medicine 1988;17:585‐607. [DOI] [PubMed] [Google Scholar]
Glover 2009 {published data only}
- Glover M, Scragg R, Nosa V, Bullen C, McCool J, Kira A. Keeping Kids Smokefree: rationale, design, and implementation of a community, school, and family‐based intervention to modify behaviors related to smoking among Maori and Pacific Island children in New Zealand. International Quarterly of Community Health Education 2009‐2010;30(3):205‐222. [DOI] [PubMed] [Google Scholar]
Gordon 2008 {published data only}
- Gordon J, Biglan A, Smolkowski K. The impact on tobacco use of branded youth anti‐tobacco activities and family communications about tobacco. Prevention Science 2008;9(2):73‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hahn 2007 {published data only}
- Hahn EJ, Hall LA, Rayens MK, Myers AV, Bonnel G. School‐ and home‐based drug prevention: Environmental, parent, and child risk reduction. Drugs: Education, Prevention and Policy 2007;14(4):319‐31. [Google Scholar]
Hansen 1987 {published data only}
- Hansen WB, Malotte CK, Fielding JE. Tobacco and alcohol prevention: Preliminary results of a four‐year study. Adolescent Psychiatry 1987;14:556‐75. [PubMed] [Google Scholar]
Hansen 1991 {published data only}
- Hansen WB, Graham JW. Preventing alcohol, marijuana, and cigarette use among adolescents: peer pressure resistance training versus establishing conservative norms. Preventive Medicine 1991;20(3):414‐30. [DOI] [PubMed] [Google Scholar]
Hawkins 1999 {published data only}
- Hawkins J, Catalano R, Kosterman R, Abbott R, Hill KG. Preventing adolescent health‐risk behaviors by strengthening protection during childhood. Archives of Pediatrics & Adolescent Medicine 1999;153(3):226‐34. [DOI] [PubMed] [Google Scholar]
Hawkins 2009 {published data only}
- Hawkins JD, Oesterle S, Brown EC, Arthur MW, Abott RD, Catalano RF Archives of Pediatric, Adolescent Medicine 2009. 163(9):789‐798. Youth problem behaviors 8 years after implementing the Communities That Care system. A community‐randomized trial. JAMA Pediatrics 2014;168(2):122‐129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins JD, Oesterle S, Brown EC, Arthur MW, Abott RD, Fagan AA, et al. Results of a type 2 translational research trial to prevent adolescent drug use and delinquency: a test of Communities That Care. Archives of Pediatric and Adolescent Medicine 2009;163(9):789‐798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins JD, Oesterle S, Brown EC, Monahan KC, Abbott RD, Arthur MW, et al. Sustained decreases in risk exposure and youth problem behaviors after installation of the Communities That Care prevention system in a randomized trial. Archives of Pediatrics & Adolescent Medicine 2012;166(2):141‐148. [DOI] [PMC free article] [PubMed] [Google Scholar]
Horn 2007 {published data only}
- Horn K, Dino G, Hamilton C, Noerachmanto N. Efficacy of an emergency department‐based motivational teenage smoking intervention. Preventing Chronic Disease 2007;4(1):1‐12 www.cdc.gov/pcd/issues/2007/jan/06_0021.htm. [PMC free article] [PubMed] [Google Scholar]
Jackson 1994 {published data only}
- Jackson C, Bee‐Gates DJ, Henrisen L. Authoritative parenting, child competencies, and initiation of cigarette smoking. Health Education Quarterly 1994;21(1):103‐16. [DOI] [PubMed] [Google Scholar]
Johnson 1990 {published data only}
- Johnson CA, Pentz MA, Weber MD, Dwyer JH, Baer N, MacKinnon DP, et al. Relative effectiveness of comprehensive community programming for drug abuse prevention with high‐risk and low‐risk adolescents. Journal of Consulting and Clinical Psychology 1990;58(4):447‐56. [DOI] [PubMed] [Google Scholar]
Jowers 2007 {published data only}
- Jowers KL, Bradshaw CP, Gately S. Taking school‐based substance abuse prevention to scale: District‐wide implementation of Keep A Clear Mind. Journal of Alcohol and Drug Education 2007;51(3):73‐91. [Google Scholar]
Knutsen 1991 {published data only}
- Knutsen SF, Knutsen R. The Tromso survey: The family intervention study ‐ the effect of intervention on some coronary risk factors and dietary habits, a 6‐year follow‐up. Preventive Medicine 1991;20(2):197‐212. [DOI] [PubMed] [Google Scholar]
Komro 2008 {published and unpublished data}
- Komro KA, Perry CL, Veblen‐Mortenson S, Farbakhsh K, Toomey TL, Stigler MH, et al. Outcomes from a randomized controlled trial of a multi‐component alcohol use preventive intervention for urban youth: Project Northland Chicago. Addiction 2008;103:606‐618. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kristjansson 2010 {published data only}
- Kristjansson AL, James JE, Allegrante JP, Sigfusdottir ID, Helgason AR. Adolescent substance use, parental monitoring, and leisure‐time activities: 12‐year outcomes of primary prevention in Iceland. Preventive Medicine 2010;51(2):168‐171. [DOI] [PubMed] [Google Scholar]
Krohn 1983 {published data only}
- Krohn MD, Massey JL, Skinner WF, Lauer RM. Social bonding theory and adolescent cigarette smoking: Longitudinal analysis. Journal of Health and Social Behavior 1983;24:337‐49. [PubMed] [Google Scholar]
Kumpfer 2012 {published data only}
- Kumpfer XL, Xie J, O'Driscoll R. Effectiveness of a culturally adapted strengthening families program 12‐16 years for high risk Irish families. Child & Youth Care Forum 2012;41(2):173‐195. [Google Scholar]
Litrownik 2000 {published data only}
- Litrownik AJ, Elder JP, Campbell NR, Ayala GX, Slymen DJ, Parra MD, et al. Evaluation of a tobacco and alcohol use prevention program for Hispanic migrant adolescents: promoting the protective factor of parent‐child communication. Preventive Medicine 2000;31(2):124‐33. [DOI] [PubMed] [Google Scholar]
Lochman 2002 {published data only}
- Lochman JE, Wells KC. Contextual social‐cognitive mediators and child outcome: A test of the theoretical model in the Coping Power program. Developmental Psychopathology 2002;14:945‐67. [DOI] [PubMed] [Google Scholar]
- Lochman JE, Wells KC. Effectiveness of the Coping Power program and of classroom intervention with aggressive children. Behavior Therapy 2003;34:493‐515. [Google Scholar]
- Lochman JE, Wells KC. The Coping Power program for preadolescent aggressive boys and their parents. Outcome effects at the 1‐year follow‐up. Journal of Consulting and Clinical Psychology 2004;72(4):571‐8. [DOI] [PubMed] [Google Scholar]
- Lochman JE, Wells KC. The Coping Power program in the middle‐school transition: Universal and indicated prevention effects. Psychology of Addictive Behavior 2002;16(4S):S40‐S54. [DOI] [PubMed] [Google Scholar]
Moncher 1994 {published data only}
- Moncher M, Schinke SP. Group intervention to prevent tobacco use among Native American youth. Special Issue: Empirical research on the outcomes of social work with groups. Research on Social Work Practice 1994;4(2):160‐71. [Google Scholar]
Nilsson 2006 {published data only}
- Nilsson M, Stenlund H, Bergström E, Weinehall L, Janlert U. It Takes Two: Reducing adolescent smoking uptake through sustainable adolescent–adult partnership. Journal of Adolescent Health 2006;39:880‐886. [DOI] [PubMed] [Google Scholar]
Nutbeam 1993 {published data only}
- Nutbeam D, Macaskill P, Smith C, Simpson JM, Catford J. Evaluation of two school smoking education programmes under normal classroom conditions. BMJ 1993;306:102‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Byrne 2002 {published data only}
- O'Byrne KK, Haddock K, Poston WSC. Parenting style and adolescent smoking. Journal of Adolescent Health 2002;30:418‐25. [DOI] [PubMed] [Google Scholar]
Olds 2010 {published data only}
- Olds DL, Kitzman HJ, Cole RE, Hanks CA, Arcoleo KJ, Anson EA, et al. Enduring effects of prenatal and infancy home visiting by nurses on maternal life course and government spending: follow‐up of a randomized trial among children at age 12 years. Archives of Pediatrics & Adolescent Medicine 2010;164:419‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Parsai 2009 {published data only}
- Parsai M, Voisine S, Marsiglia FF, Kulis S, Nieri T. The protective and risk effects of parents and peers on substance use, attitudes, and behaviors of Mexican and Mexican American female and male adolescents. Youth & Society 2009;40(3):353‐376. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patten 2006 {published data only}
- Patten CA, Croghan IT, Meis TM, Decker PA, Pingree S, Colligan RC, et al. Randomized clinical trial of an internet‐based versus brief office intervention for adolescent smoking cessation. Patient Education and Counseling 2006;64:249‐58. [DOI] [PubMed] [Google Scholar]
Pentz 1989 {published data only}
- Pentz MA, Johnson A, Dwyer JH, MacKinnon DM, Hansen WB, Flay BR. A comprehensive community approach to adolescent drug abuse prevention: effects on cardiovascular disease risk behaviors. Annals of Medicine 1989;21:219‐22. [DOI] [PubMed] [Google Scholar]
Pentz 2013 {published and unpublished data}
- Pentz MA, Riggs NR. Longitudinal relationships of executive cognitive function and parent influence to child substance use and physical activity. Prevention Science 2013;14:229‐237. [DOI] [PubMed] [Google Scholar]
Perry 1990 {published data only}
- Perry CL, Pirie P, Holder W, Halper A, Dudovitz B. Parent involvement in cigarette smoking prevention: Two pilot evaluations of the "Unpuffables Program". Journal of School Health 1990;60(9):443‐7. [DOI] [PubMed] [Google Scholar]
Perry 2003 {published data only}
- Perry CL, Komro KA, Veblen‐Mortenson S, Bosma LM, Farbakhsh K, Munson KA, et al. A randomized controlled trial of the middle and junior high school D.A.R.E. and D.A.R.E. plus programs. Archives of Pediatric and Adolescent Medicine 2003;157:178‐184. [DOI] [PubMed] [Google Scholar]
Perry 2009 {published data only}
- Perry CL, Stigler MH, Arora M, Reddy KS. Preventing tobacco use among young people in India: Project MYTRI. American Journal of Public Health 2009;99(5):899‐906. [DOI] [PMC free article] [PubMed] [Google Scholar]
Piper 2000 {published data only}
- Piper DL, Moberg P, King MJ. The HEALTHY FOR LIFE Project: behavioural outcomes. The Journal of Primary Prevention 2000;21(1):47‐73. [Google Scholar]
Ramchand 2006 {published data only}
- Ramchand R. Adolescent work experiences and drug involvement in an urban environment. Ph.D. Dissertation Johns Hopkins University 2006; Vol. UMI Microform 3213788.
Rohrbach 1994 {published data only}
- Rohrbach LA, Hodgson CS, Flay BR, Hansen WB, Pentz MA. Parental participation in drug abuse prevention: results from the Midwestern Prevention Project. Journal of Research on Adolescence 1994;4(2):295‐317. [Google Scholar]
Rohrbach 2002 {published data only}
- Rohrbach LA, Howard‐Pitney B, Unger JB, Dent CW, Howard KA, Boley T, et al. Independent evaluation of the California Tobacco Control Program: relationships between program exposure and outcomes, 1996‐1998. American Journal of Public Health 2002;92(6):975‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosati 2012 {published data only}
- Rosati MJ, Cupp PK, Chookhare W, Miller BA, Byrnes HF, Fongkaew W. Successful implementation of Thai Family Matters: strategies and implications. Health Promotion Practice 2012;13:355‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Salminen 2005 {published data only}
- Salminen M, Vahlberg T, Ojanlatva A, Kivelä S‐L. Effects of a controlled family‐based health education/counseling intervention. American Journal of Health Behavior 2005;29(5):395‐406. [DOI] [PubMed] [Google Scholar]
Schinke 1988 {published data only}
- Schinke SP, Orlandi MA, Botvin GJ, Gilchrist LD, Trimble JE, Locklear VS. Preventing substance abuse among American‐Indian adolescents: A bicultural competence skills approach. Journal of Counseling Psychology 1988;35(1):87‐90. [PMC free article] [PubMed] [Google Scholar]
Schinke 2000 {published data only}
- Schinke SP, Tepavac L, Cole KC. Preventing substance use among Native American youth: Three‐year results. Addictive Behaviors 2000;25(3):387‐97. [DOI] [PubMed] [Google Scholar]
Schinke 2009 {published data only}
- Schinke SP, Cole KCA, Fang L. Gender‐specific intervention to reduce underage drinking among early adolescent girls: a test of a computer‐mediated, mother‐daughter program. Journal of Studies on Alcohol & Drugs 2009;70(1):70‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schinke SP, Fang L, Cole KC. Preventing substance use among adolescent girls: 1‐year outcomes of a computerized, mother‐daughter program. Preventive Medicine 2009;34(9):1060‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Severson 1991 {published data only}
- Severson HH, Glasgow R, Wirt R, Brozovsky P, Zoref L, Black C, et al. Preventing the use of smokeless tobacco and cigarettes by teens; results of a classroom intervention. Health Education Research 1991;6(1):109‐20. [Google Scholar]
Simons‐Morton 2005 {published data only}
- Simons‐Morton B, Haynie D, Saylor K, Crump AD, Chen R. The effects of the Going Places program on early adolescent substance use and antisocial behavior. Prevention Science 2005;6(3):187‐197. [DOI] [PubMed] [Google Scholar]
Soper 2010 {published data only}
- Soper AC, Wolchik SA, Tein J‐Y, Sandler IN. Mediation of a preventive intervention's 6‐year effects on health risk behaviors. Psychology of Addictive Behaviors 2010;24(2):300‐310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolchik SA, Sandler IN, Millsap RE, Plummer B, Greene SM, Anderson ER, et al. Six‐year follow‐up of a randomized, controlled trial of preventive interventions for children of divorce. Journal of the American Medical Association 2002;28:1‐8. [DOI] [PubMed] [Google Scholar]
- Zhou Q, Sandler IN, Millsap R, Wolchik SA, Dawson‐McClure S. Mother‐child relationship quality and effective discipline in mediators of the 6‐year effects of the New Beginnings Program for children from divorced families. Journal of Consulting and Clinical Psychology 2008;76:579‐594. [DOI] [PMC free article] [PubMed] [Google Scholar]
Spoth 2007 {published data only}
- Greenberg MT, Feinberg ME, Meyer‐Chilenski S, Spoth R, Redmond, C. Community and team member factors that influence the early phase functioning of community prevention teams: the PROSPER Project. Journal of Primary Prevention 2007;28:485‐504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redmond C, Spoth R, Shin C, Schainker LM, Greenberg MT, Feinberg ME. Long‐term protective factor outcomes of evidence‐based interventions implemented by community teams through a community‐university partnership. Journal of Primary Prevention 2009;30:513‐530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Greenberg M, Bierman K, Redmond C. PROSPER community‐university partnership model for public education systems: capacity‐building for evidence‐based, competence‐building prevention. Prevention Science 2004;5:31‐9. [DOI] [PubMed] [Google Scholar]
- Spoth R, Redmond C, Shin C, Greenberg M, Clair S, Feinberg M. Substance‐use outcomes at 18 month past baseline. The PROSPER community‐university Partnership Trial. American Journal of Preventive Medicine 2007;32(5):395‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stevens 1993 {published data only}
- Stevens MM, Freeman DH, Mott LA, Youells FE, Linsey SC. Smokeless tobacco use among children: the New Hampshire study. American Journal of Preventive Medicine 1993;9:160‐6. [PubMed] [Google Scholar]
Tang 1997 {published data only}
- Tang KC, Rissel C, Bauman A, Fay J, Porter S, Dawes A, et al. Evaluation of Kickbutts ‐ a school and community‐based smoking prevention program among a sample of year 7 and 8 students. Health Promotion Journal of Australia 1997;7:122‐7. [Google Scholar]
Tingen 2006 {published data only}
- Tingen MS, Waller JL, Smith TM, Baker RR, Reyes J, Treiber FA. Tobacco prevention in children and cessation in family members. J Am Acad Nurse Practitioners 2006;18:169‐179. [DOI] [PubMed] [Google Scholar]
Vartiainen 2007 {published data only}
- Vartiainen E, Rennanen M, Kaukkala A, Dijk F, Lehtavuori R, Vries H. The effects of a three‐year smoking prevention programme in secondary schools in Helsinki. European Journal of Public Health 2007;17(3):249‐56. [DOI] [PubMed] [Google Scholar]
Vitória 2011 {published data only}
- Vitória, PD, Silva, SA, Vries H. Longitudinal evaluation of a smoking prevention program for adolescents [Avaliação longitudinal de programa de prevenção do tabagismo para adolescentes]. Revista Saúde Pública 2011;45(2):344‐354. [DOI] [PubMed] [Google Scholar]
Wakschlag 2011 {published data only}
- Wakschlag LS, Metzger A, Darfler A, Ho J, Mermelstein R, Rathouz PJ. The Family Talk About Smoking (FTAS) paradigm: New directions for assessing parent–teen communications about smoking. Nicotine & Tobacco Research 2011;13:103‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wen 2007 {published data only}
- Wen XZ, Chen WQ, Lu CY, Liang CH, Zhang CX, Han K, et al. Process evaluation on a health promotion model regarding smoking prevention among Chinese secondary school students. Zhonghua Liu Xing Bing Xue Za Zhi 2007;28(3):224‐8. [PubMed] [Google Scholar]
Werch 1991 {published data only}
- Werch CE, Young M, Clark M, Garrett C, Hooks S, Kersten C. Effects of a take‐home drug prevention program on drug‐related communication and beliefs of parents and children. Journal of School Health 1991;61(8):346‐50. [DOI] [PubMed] [Google Scholar]
- Young M, Kersten C, Werch C. Evaluation of a parent child drug education program. Journal of Drug Education 1996;26(1):57‐68. [DOI] [PubMed] [Google Scholar]
Werch 2005 {published data only}
- Werch C, Moore MJ, DiClemente CC, Bledsoe R, Jobli E. A multihealth intervention integrating physical activity and substance use prevention for adolescents. Prevention Science 2005;6(3):213‐226. [DOI] [PubMed] [Google Scholar]
Werch 2010 {published data only}
- Werch CEC, Bian H, Diclemente CC, Moore MJ, Thombs D, Ames SC, et al. A brief image‐based prevention intervention for adolescents. Psychology of Addictive Behaviors 2010;24(1):170‐175. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2012 {published data only}
- Wilson DB, Jones RM, McClish D, Westerberg AL, Danish S. Fruit and vegetable intake among rural youth following a school‐based randomized controlled trial. Preventive Medicine 2012;54:150‐6. [DOI] [PubMed] [Google Scholar]
Wilson 2013 {published data only}
- Wilson IS, Ritchie D, Amos A, Shaw A, O'Donnell R, Mills LM, et al. 'I'm not doing this for me': mothers' accounts of creating smoke‐free homes. Health Education Research 2013;28(1):165‐78. [DOI] [PubMed] [Google Scholar]
Yilmaz 2013 {published data only}
- Yilmaz G, Caylan N, Karacan CD. Brief intervention to preteens and adolescents to create smoke‐free homes and cotinine results: a randomized trial. Journal of Tropical Pediatrics 2013;59(5):365‐71. [DOI] [PubMed] [Google Scholar]
Young 1996 {published data only}
- Young M, Kersten C, Werch C. Evaluation of a parent child drug education program. Journal of Drug Education 1996;26(1):49‐56. [DOI] [PubMed] [Google Scholar]
Zavela 2004 {published data only}
- Zavela KJ, Battistich V, Gosselink CA, Dean BJ. Say Yes First: Follow up of a five‐year rural drug prevention program. Journal of Drug Education 2004;34(1):73‐88. [DOI] [PubMed] [Google Scholar]
Additional references
Avenevoli 2003
- Avenevoli S, Merikangas KR. Familial influences on adolescent smoking. Addiction 2003;98 Suppl 1:1‐20. [DOI] [PubMed] [Google Scholar]
Baker 2015
- Baker PRA, Francis DP, Soares J, Weightman AL, Foster C. Community wide interventions for increasing physical activity. Cochrane Database of Systematic Reviews 2015, Issue 1. [DOI: 10.1002/14651858.CD008366.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Botvin 1993
- Botvin GJ, Baker E, Botvin EM, Dusenbury L, Cardwell J, Diaz T. Factors promoting cigarette smoking among Black youth: a causal modeling approach. Addictive Behaviors 1993;18:397‐405. [DOI] [PubMed] [Google Scholar]
Bricker 2003
- Bricker JB, Leroux BG, Petersen AV Jr, Kealey KA, Sarason IG, Anderson MR, et al. Nine‐year prospective relationship between parental smoking cessation and children's daily smoking. Addiction 2003;98:585‐93. [DOI] [PubMed] [Google Scholar]
Carson 2011
- Carson KV, Brinn MP, Labiszewski NA, Esterman AJ, Chang AB, Smith BJ. Community interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD001291.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carson 2012
- Carson KV, Brinn MP, Labiszewski NA, Peters M, Chang AB, Veale A, et al. Interventions for tobacco use prevention in Indigenous youth. Cochrane Database of Systematic Reviews 2012, Issue 8. [DOI: 10.1002/14651858.CD009325.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
Chassin 1984
- Chassin L, Presson CC. Predicting the onset of cigarette smoking in adolescents: A longitudinal study. Journal of Applied Social Psychology 1984;14(3):224‐43. [Google Scholar]
Chassin 1996
- Chassin L, Presson CC, Rose JS, Sherman SJ. The natural history of cigarette smoking from adolescence to adulthood: demographic predictors of continuity and change. Health Psychology 1996;15:478‐84. [DOI] [PubMed] [Google Scholar]
Covey 1990
- Covey LS, Tam D. Deprssive mood, the single‐parent home, and adolescent cigarette smoking. American Journal of Public Health 1990;80:1330‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Darling 2003
- Darling N, Cumsille P. Theory, measurement, and methods in the study of family influences on adolescent smoking. Addiction 2003;98 Suppl 1:21‐36. [DOI] [PubMed] [Google Scholar]
Dielman 1994
- Dielman TE. Correction for the design effect in school‐based substance use and abuse prevention research: Sample size requirements and analysis considerations. NIDA Research Monographs. Vol. 139, Washington, D.C: National Institute of Drug Addiction, 1994:115‐26. [PubMed] [Google Scholar]
DuRant 1999
- DuRant RH, Smith JA, Kreiter SR, Krowchuk DP. The relationship between early age of onset of initial substance use and engaging in multiple health risk behaviors among young adolescents. Archives of Pediatrics & Adolescent Medicine 1999;153(3):286‐91. [DOI] [PubMed] [Google Scholar]
Eisner 1989
- Eisner JR, Morgan M, Gammage P, Gray E. Adolescent smoking: Attitudes, norms and parental influence. British Journal of Social Psychology 1989;28:193‐202. [DOI] [PubMed] [Google Scholar]
Hussey 1992
- Hussey JM, Gilchrist LD, Gillmore MR, Lohr MR. Factors related to cigarette smoking during adolescent pregnancy. Journal of Youth and Adolescence 1992;21(4):409‐20. [DOI] [PubMed] [Google Scholar]
Huver 2007
- Huver RME, Engels RCME, Vries H. Are anti‐smoking parenting practices related to adolescent smoking cognitions and behavior?. Health Education Research 2007;21(1):66‐77. [DOI] [PubMed] [Google Scholar]
Isohanni 1991
- Isohanni M, Moilanen I, Rantakallio P. Determinants of teenage smoking, with reference to non‐standard family background. British Journal of Addictions 1991;86:391‐8. [DOI] [PubMed] [Google Scholar]
Jackson 1998
- Jackson C, Henriksen L, Foshee VA. The authoritative parenting index: predicting health risk behaviors among children and adolescents. Health Education & Behavior 1998;25(3):319‐37. [DOI] [PubMed] [Google Scholar]
Jarvis 1997
- Jarvis MJ. Patterns and predictors of smoking cessation in the general population. In: Bolliger CT, Fagerstroem KT editor(s). The tobacco epidemic. Progress in respiratory research no. 28. Basel: Karger, 1997:151‐64. [Google Scholar]
Johnston 2000
- Johnston LD, O'Malley PM, Bachman JG. The monitoring the future national survey results on adolescent drug use: overview of key findings, 1999. NIH Publ No. 00‐4690. Rockville, MD: National Institute of Drug Abuse, 2000:48. [NIH Publ No. 00‐4690] [Google Scholar]
Krosnick 1982
- Krosnick JA, Judd CM. Transitions in social influence at adolescence: Who induces cigarette smoking?. Developmental Psychology 1982;18(1):359‐68. [Google Scholar]
Mayhew 2000
- Mayhew KP, Flay BR, Mott JA. Stages in the development of adolescent smoking. Drug and Alcohol Dependence 2000;59 Suppl 1:61‐81. [DOI] [PubMed] [Google Scholar]
Mounts 2002
- Mounts NS. Parental management of adolescent peer relationships in context: the role of parenting style. Journal of Family Psychology 2002;16:58‐69. [DOI] [PubMed] [Google Scholar]
Murray 1990
- Murray DM, Hannan PJ. Planning for the appropriate analysis in school‐based drug‐use prevention studies. Journal of Consulting and Clinical Psychology 1990;58(4):458‐68. [DOI] [PubMed] [Google Scholar]
Murray 1997
- Murray DM, Short BJ. Intraclass correlation among measures related to tobacco use by adolescents: Estimates, correlates, and applications in intervention studies. Addictive Behaviors 1997;22(1):1‐12. [DOI] [PubMed] [Google Scholar]
Newman 1989
- Newman IM, Ward JM. The influence of parental attitude and behavior on early adolescent cigarette smoking. Journal of School Health 1989;59(4):150‐2. [DOI] [PubMed] [Google Scholar]
Palmer 1998
- Palmer RF, Graham JW, White EL, Hansen WB. Applying multilevel analytic strategies in adolescent substance use prevention research. Preventive Medicine 1998;27:328‐36. [DOI] [PubMed] [Google Scholar]
Patnode 2012
- Patnode CD, O'Connor E, Whitlock EP, Perdue LA, Soh C. Primary Care Relevant Interventions for Tobacco Use Prevention and Cessation in Children and Adolescents: A Systematic Evidence Review for the U.S. Preventive Services Task Force. Rockville, MD, USA: Agency for Healthcare Research and Quality (Internet File) December 2012. [PubMed]
Petrie 2007
- Petrie J, Bunn F, Byrne G. Parenting programmes for preventing tobacco, alcohol or drugs misuse in children <18: a systematic review. Health Education Research 2007;22(2):177‐91. [DOI] [PubMed] [Google Scholar]
Proescholdbell 2000
- Proescholdbell RJ, Chassin L, MacKinnon DP. Home smoking restrictions and adolescent smoking. Nicotine & Tobacco Research 2000;2(2):159‐67. [DOI] [PubMed] [Google Scholar]
Simons‐Morton 2002
- Simons‐Morton BG. Prospective analysis of peer and parent influences on smoking initiation among early adolescents. Prevention Science 2002;3:275‐83. [DOI] [PubMed] [Google Scholar]
Thomas 2011
- Thomas RE, Lorenzetti D, Spragins W. Mentoring adolescents to prevent drug and alcohol use. Cochrane Database of Systematic Reviews 2011, Issue 11. [DOI: 10.1002/14651858.CD007381.pub2] [DOI] [PubMed] [Google Scholar]
Thomas 2013
- Thomas RE, McLellan J, Perera R. School‐based programmes for preventing smoking. Cochrane Database of Systematic Reviews 2013, Issue 4. [DOI: 10.1002/14651858.CD001293.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Turner 1991
- Turner RA, Irwin JE Jr. Family structure, family processes, and experimenting with substances during adolescence. Journal of Research in Adolescence 1991;1:93‐106. [Google Scholar]
Tyas 1998
- Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tobacco Control 1998;7:409‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
USDHHS 1994
- US Department of Health and Human Services. Report of the Surgeon General.. Preventing tobacco use among young people: a report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Disease Prevention and Health Promotion, Office on Smoking and Health, 1994. [Google Scholar]
Warren 2009
- Warren CW, Lea V, Lee J, Jones NR, Asma S, McKenna M. Change in tobacco use among 13−15 year olds between 1999 and 2008: findings from the Global Youth Tobacco Survey. Global Health Promotion 2009;16:38. [DOI: 10.1177/1757975909342192] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Thomas 2003
- Thomas RE, Baker P, Lorenzetti D. Family‐based programmes for preventing smoking by children and adolescents. Cochrane Database of Systematic Reviews 2003, Issue 4. [DOI: 10.1002/14651858.CD004493] [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2007
- Thomas RE, Baker P, Lorenzetti D. Family‐based programmes for preventing smoking by children and adolescents. Cochrane Database of Systematic Reviews 2007, Issue 1. [DOI: 10.1002/14651858.CD004493.pub2] [DOI] [PubMed] [Google Scholar]


