Abstract
Background
Individuals with schizophrenia smoke more heavily than the general population and this contributes to their higher morbidity and mortality from smoking‐related illnesses. It remains unclear what interventions can help them to quit or to reduce smoking.
Objectives
To evaluate the benefits and harms of different treatments for nicotine dependence in schizophrenia.
Search methods
We searched electronic databases including MEDLINE, EMBASE and PsycINFO from inception to October 2012, and the Cochrane Tobacco Addiction Group Specialized Register in November 2012.
Selection criteria
We included randomised trials for smoking cessation or reduction, comparing any pharmacological or non‐pharmacological intervention with placebo or with another therapeutic control in adult smokers with schizophrenia or schizoaffective disorder.
Data collection and analysis
Two reviewers independently assessed the eligibility and quality of trials, as well as extracted data. Outcome measures included smoking abstinence, reduction in the amount smoked and any change in mental state. We extracted abstinence and reduction data at the end of treatment and at least six months after the intervention. We used the most rigorous definition of abstinence or reduction and biochemically validated data where available. We noted any reported adverse events. Where appropriate, we pooled data using a random‐effects model.
Main results
We included 34 trials (16 trials of cessation; nine trials of reduction; one trial of relapse prevention; eight trials that reported smoking outcomes for interventions aimed at other purposes). Seven trials compared bupropion with placebo; meta‐analysis showed that cessation rates after bupropion were significantly higher than placebo at the end of treatment (seven trials, N = 340; risk ratio [RR] 3.03; 95% confidence interval [CI] 1.69 to 5.42) and after six months (five trials, N = 214, RR 2.78; 95% CI 1.02 to 7.58). There were no significant differences in positive, negative and depressive symptoms between bupropion and placebo groups. There were no reports of major adverse events such as seizures with bupropion.
Smoking cessation rates after varenicline were significantly higher than placebo, at the end of treatment (2 trials, N = 137; RR 4.74, 95% CI 1.34 to 16.71). Only one trial reported follow‐up at six months and the CIs were too wide to provide evidence of a sustained effect (one trial, N = 128, RR 5.06, 95% CI 0.67 to 38.24). There were no significant differences in psychiatric symptoms between the varenicline and placebo groups. Nevertheless, there were reports of suicidal ideation and behaviours from two people on varenicline.
Two studies reported that contingent reinforcement (CR) with money may increase smoking abstinence rates and reduce the level of smoking in patients with schizophrenia. However, it is uncertain whether these benefits can be maintained in the longer term. There was no evidence of benefit for the few trials of other pharmacological therapies (including nicotine replacement therapy (NRT)) and psychosocial interventions in helping smokers with schizophrenia to quit or reduce smoking.
Authors' conclusions
Bupropion increases smoking abstinence rates in smokers with schizophrenia, without jeopardizing their mental state. Varenicline may also improve smoking cessation rates in schizophrenia, but its possible psychiatric adverse effects cannot be ruled out. CR may help this group of patients to quit and reduce smoking in the short term. We failed to find convincing evidence that other interventions have a beneficial effect on smoking in schizophrenia.
Keywords: Adult; Humans; Schizophrenia; Smoking Prevention; Antidepressive Agents, Second‐Generation; Antidepressive Agents, Second‐Generation/therapeutic use; Benzazepines; Benzazepines/therapeutic use; Bupropion; Bupropion/therapeutic use; Nicotine; Nicotine/administration & dosage; Nicotinic Agonists; Nicotinic Agonists/therapeutic use; Quinoxalines; Quinoxalines/therapeutic use; Randomized Controlled Trials as Topic; Reinforcement, Psychology; Schizophrenic Psychology; Smoking Cessation; Smoking Cessation/methods; Tobacco Use Cessation Devices; Varenicline
Plain language summary
Are there any effective interventions to help individuals with schizophrenia to quit or to reduce smoking?
People with schizophrenia are very often heavy smokers. It is uncertain whether treatments that have been shown to help other groups of people to quit smoking are also effective for people with schizophrenia. In this review, we analysed studies which investigated a wide variety of interventions. Our results suggested that bupropion (an antidepressant medication previously shown to be effective for smoking cessation) helps patients with schizophrenia to quit smoking. The effect was clear at the end of the treatment and it may also be maintained after six months. Patients who used bupropion in the trials did not experience any major adverse effect and their mental state was stable during the treatment. Another medication, varenicline (a nicotine partial agonist which has been shown to be an effective intervention for smoking cessation in smokers without schizophrenia), also helps individuals with schizophrenia to quit smoking at the end of the treatment. However, this evidence is only based on two studies. We did not have sufficient direct evidence to know whether the benefit of varenicline is maintained for six months or more. In addition, there has been ongoing concern of potential psychiatric adverse events including suicidal ideas and behaviour among smokers who use varenicline. We found that two patients, among 144 who used varenicline, had either suicidal ideas or behaviour. Smokers with schizophrenia who receive money as a reward for quitting may have a higher rate of stopping smoking whilst they get payments. However, there is no evidence that they will remain abstinent after the reward stops. There was too little evidence to show whether other treatments like nicotine replacement therapy and psychosocial interventions are helpful.
Summary of findings
Summary of findings for the main comparison. Applicability in clinical practice ‐ projected numbers of people with schizophrenia per hundred patients treated with smoking cessation therapies (smoking abstinence at the end of the trial and at follow‐up after 6 months).
| Comparison | Smoking abstinence at the end of trial (per 100 patients) | Smoking abstinence at follow‐up after 6 months (per 100 patients) | ||||||||
| Number of trials | Intervention | Control | Difference * | Number needed# | Number of trials | Intervention | Control | Difference * | Number needed# | |
| Bupropion vs. placebo | 7 | 22 | 7 | ↓14 (↓5 to ↓31) |
7 (3 to 20) |
5 | 10 | 4 | ↓7 (0 to ↓24) |
15 (4 to 1350) |
| TNP vs. placebo | Data not combined because of heterogeneity of studies | No trial found | ||||||||
| Varenicline vs. placebo | 2 | 20 | 4 | ↓16 (↓1 to ↓65) |
6 (2 to 71) |
1 | 2 | 0 | ↓2 | # |
| CR + TNP vs. minimal | 1 | 50 | 10 | ↓40 | 3 | No follow‐up data available | ||||
* calculated as absolute risk reduction/increase per 100 people treated, using the rate in control (comparator) arms of trials, with the summary RR applied to calculate the expected absolute risk reduction/ increase for the investigative arms of trials (95% confidence intervals in bracket)
‘ns’ = difference not statistically significant (i.e. summary risk ratio confidence intervals cross 1.00).
# Number needed to be treated with the intervention to cause one person to experience difference in the direction noted. Number needed not given where difference between the intervention and the comparator arm was not significantly different (95% confidence intervals in bracket)
Summary of findings 2. Applicability in clinical practice ‐ smoking reduction at the end of the trial and at follow‐up after 6 months among people with schizophrenia treated with smoking cessation therapies.
|
Comparison (data were from abstinence study) |
Expired CO level at the end of trial (ppm) | Expired CO level at follow‐up after 6 months (ppm) | ||||||
| Number of trials | intervention | control | Difference | Number of trials | Intervention | Control | Difference | |
| Bupropion vs. placebo | 4 | 14.8 | 21.5 | ↓6.8 (↓2.8 to ↓10.8) |
3 | 18.8 | 22.7 | ns |
| TNP vs. placebo | Data not combined because of heterogeneity of studies | No trial found | ||||||
| Varenicline vs. placebo | 1 | #↓11.0 | #↓7.1 | ns | No follow‐up data available | |||
| CR + TNP vs. minimal | 1 | 17.7 | 27.5 | ↓9.8 | No follow‐up data available | |||
‘ns’ = difference not statistically significant
# ‐ these figures represent the mean reduction of expired CO level (in ppm) compared to the baseline level.
Background
Schizophrenia is a chronic and severe mental illness affecting approximately one per cent of the general population (American Psychiatric Association 1994). A meta‐analysis of 42 epidemiological studies across 20 different countries shows that people with schizophrenia have more than five times the odds of current smoking than the general population, and smoking cessation rates are much lower in smokers with schizophrenia compared with the general population (de Leon 2005a). In addition, smokers with schizophrenia smoke more heavily and extract more nicotine from each cigarette (Olincy 1997; Kelly 1999; de Leon 2005a; Williams 2005). People with schizophrenia have a shorter life expectancy than the general population, and chronic cigarette smoking has been suggested as a major contributing factor to higher morbidity and mortality from malignancy and cardiovascular and respiratory diseases in this group of patients, especially in people aged 35 to 54 years. (Brown 2000; Lichtermann 2001; Kelly 2011). Tobacco use among individuals with schizophrenia is financially costly; a study has shown that it consumed 27% of the monthly income of those residing in a high tobacco tax state (Steinberg 2004).
Heavy smoking in patients with schizophrenia has been reported to be associated with more of the positive symptoms of the condition, increased substance misuse, more frequent psychiatric hospitalisation and a higher suicide risk (Goff 1992; Ziedonis 1994; Workgroup on Substance Use Disorders 2006). Tobacco smoking also increases the metabolism of some antipsychotic medications (Desai 2001), and some patients may use tobacco to alleviate the side effects of neuroleptic medications. Individuals with schizophrenia often have impairment in their cognitive function, including difficulty in filtering out unnecessary information (Kumari 2002), secondary to abnormalities in the sensorimotor gating. Cigarette smoking appears to improve sensory gating in patients with schizophrenia (Adler 1998). Hence, patients with schizophrenia may use cigarette smoking to improve their cognitive function. In addition to the cognitive deficits of frontal executive function and in attention among individuals with schizophrenia, depressive symptoms, drug misuse, disorganised thinking and poor task persistence may also explain their lower motivation and greater difficulty for smoking cessation (Culhane 2008; Moss 2009). Patients with schizophrenia may be ambivalent about giving up smoking, as there are few role models of ex‐smokers and less specific support available for quitting smoking. Recent research also showed that they perceived a lower risk to their health associated with smoking when compared to people without schizophrenia (Kelly 2012). Furthermore, smoking is sometimes condoned in mental health settings, and in the past cigarettes were used in token economies to reinforce positive patient behaviour (Gustafson 1992). Smoking has also been recently shown as a possible way for social facilitation and stimulation enhancement among individuals with schizophrenia (Kelly 2012)
Tobacco control specialists and healthcare providers previously have not offered tobacco dependence treatment to patients with schizophrenia, probably secondarily to stigma, lack of information, or perceived hopelessness regarding abstinence (Williams 2006). More recent initiatives have aimed to improve the physical health of those with schizophrenia, and guidelines for cessation interventions for smokers with schizophrenia have now been published (Zwar 2007; Fiore 2008; Dixon 2009; Buchanan 2009).
Smokers with schizophrenia have a more severe nicotine dependence compared to smokers without schizophrenia (de Leon 2005a). Hence, interventions may not be as effective as they have been shown to be in the general population. We also need to consider the safety of these interventions, particularly those involving drug therapy. Some of the pharmacological treatments for nicotine dependence act on neurotransmission. For example, previous smoking cessation guidelines do not recommend the use of bupropion in smokers with schizophrenia, because there may be a theoretical risk of psychotic relapse if bupropion, a dopamine agonist, is used among patients with schizophrenia (Strasser 2001). Some case reports have suggested that varenicline (another medication which has been proven to be effective for smoking cessation in the general population) may exacerbate psychiatric symptoms including psychosis and mood symptoms (Freedman 2007; Liu 2009). Moreover, drug treatment for smoking cessation and reduction may interact with and alter the effectiveness of the antipsychotic medications commonly used among patients with schizophrenia. In addition, nicotine withdrawal can cause symptoms like depression, anxiety and irritability. All these factors may contribute to changes in the mental state of these patients, and the extent of these changes remains unclear. The aim of this review is to summarize existing evidence for different interventions in smoking cessation and reduction for individuals with schizophrenia.
Objectives
This review addressed the following objectives:
To examine the efficacy of different interventions (alone or in combination with other interventions) on smoking cessation in individuals with schizophrenia.
To examine the efficacy of different interventions (alone or in combination with other interventions) on smoking reduction in individuals with schizophrenia.
To assess any harmful effect of different interventions for smoking cessation on the mental state of patients with schizophrenia.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) or quasi‐randomised controlled trials.
Types of participants
We included adult smokers with a current diagnosis of schizophrenia according to the criteria of the International Classification of Diseases (ICD) (World Health Organization 2003) or Diagnostic and Statistical Manual of Mental Disorders (DSM) (American Psychiatric Association 1994). Smokers with a diagnosis of schizoaffective disorder were also included, because certain core symptoms are the same as in schizophrenia. We did not exclude patients with a diagnosis of schizophrenia or schizoaffective disorder who had other substance misuse disorder or additional psychiatric disorders, as individuals with schizophrenia have high prevalence of substance misuse disorders (Dixon 1999). If a study was conducted in a group of participants with mixed psychiatric diagnoses, we included that trial only when separate data for people with schizophrenia or schizoaffective disorder were available. We included people who may or may not have expressed an interest in stopping or reducing smoking. We reported whether or not participants in a study wanted to stop or reduce smoking.
Types of interventions
We included both pharmacological and non‐pharmacological interventions (alone or in combination) specific to smoking cessation or reduction. We included interventions intended for another purpose (e.g. antipsychotics for treating schizophrenia) if smoking abstinence or reduction outcomes were reported. We reported the results of these trials separately and they did not contribute to any meta‐analysis, since they were not designed to test the efficacy of the intervention for smoking cessation or reduction. The control condition could be another intervention (pharmacological or non‐pharmacological), placebo, or usual care.
Types of outcome measures
Primary outcomes
Smoking abstinence at longest follow‐up
The primary outcome was abstinence from smoking assessed at least six months from the start of the intervention, according to the 'Russell Standard' (i.e. a common standard for outcome criteria in smoking cessation trials; West 2005). The United States Department of Health and Human Services (USDHHS) Tobacco Use and Dependence Guideline Panel also suggested a minimum of six months as an adequate period of abstinence to assess treatment differences in the longer term (Fiore 2008). Abstinence could be assessed by self report or with biochemical verification. For data synthesis, we chose the strictest definition of abstinence in each trial, preferring sustained abstinence over point prevalence if both were reported. In studies that used biochemical validation of abstinence, only people whose self reports could be validated were classified as abstinent.
Change in mental state
Change in mental state was measured by change in positive symptoms (e.g. hallucinations, delusions), negative symptoms (e.g. anhedonia, avolition), and depressive symptoms.
Secondary outcomes
Smoking abstinence at the end of the intervention
This was measured as for the primary abstinence outcome.
Reduction of smoking behaviour or dependence
This was assessed at the end of the intervention and during the follow‐up period after the end of the intervention, if data were available. Measures could include any of the following: percentage change in cigarettes per day (CPD) from baseline level; absolute number of cigarettes foregone; incidence of achieving at least a 50% reduction in CPD; reduction of expired carbon monoxide (CO) level; or reduction of scores on scale measures of nicotine dependence (e.g. Fagerström Test for Nicotine Dependence (FTND)).
Other adverse events
We recorded and assessed any other reported adverse events.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Tobacco Addiction Group Specialised Register in November 2012, using the topic‐related free‐text term 'schiz*'. See the Specialised Register section of the Tobacco Addiction Group Module in the Cochrane Library for search strategies for CENTRAL (the Cochrane Central Register of Controlled Trials), MEDLINE, EMBASE, PsycINFO and Web of Science, and dates of searches. CENTRAL was searched in The Cochrane Library 2012 issue 6, using the strategy ((SR‐SCHIZ) and (smoking):ti,ab,kw) AND NOT (SR‐TOBACCO).
In addition, we searched the following electronic databases in October 2012:
MEDLINE, MEDLINE In‐Process & Other Non‐Indexed Citations via OVID (1948 onwards)
EMBASE via OVID (1980 onwards)
PsycINFO via OVID (1806 onwards)
CINAHL Plus with Full Text (1979 onwards)
ISI Web of Science with Conference Proceedings (1900 onwards)
BIOSIS Previews (1969 onwards)
We included all data available up to the last date of search and in any language. We included search terms for schizophrenia, smoking and randomised trials. For schizophrenia, we used the search terms used by the Cochrane Schizophrenia Group. For smoking cessation and reduction, we used search terms defined by the Cochrane Tobacco Addiction Group, with some modification to focus on interventions for both smoking cessation and reduction. To identify randomised trials, we used the search strategies suggested in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Full search strategies for databases are listed in the appendix of this review (Appendix 1; Appendix 2; Appendix 3).
Searching other resources
We checked the reference lists of retrieved studies for additional relevant information. We also searched the following online clinical trials registers to identify potential ongoing and unpublished trials: 1. World Health Organization International Clinical Trials Registry Platform Search Portal (http://apps.who.int/trialsearch); 2. ClinicalTrials.gov register (www.clinicaltrials.gov); 3. The Australian New Zealand Clinical Trials Registry (www.anzctr.org.au); 4. International Standard Randomised Controlled Trial Number Register (www.controlled‐trials.com/isrctn/); 5. UK Clinical Trials Gateway (www.controlled‐trials.com/ukctg/). Where we suspected duplicate reporting of the same trial, we attempted to contact authors for clarification. If duplication was confirmed, we used the full publication together with any other related publications for additional information.
Data collection and analysis
Selection of studies
All of the authors (DTT, MP and ACW) independently screened the titles and abstracts identified by the search, and decided on the possible reports to be included. We obtained and examined full text reports of all potentially relevant trials, to decide whether the studies fulfilled the inclusion criteria. Any disagreement between the authors was resolved through discussion. All studies excluded at this stage are reported in the Characteristics of excluded studies table.
Data extraction and management
Two authors (DTT and MP) independently extracted data from all included trials, with a specifically designed data extraction form. Information extracted included the following:
Methodology ‐ comprising the inclusion and exclusion criteria, method of randomisation and other design features and setting of the trial.
Demographics of participants ‐ including severity of tobacco dependency, concurrent medication used and severity of schizophrenic illness.
Details of the interventions ‐ including any target quit date set.
Outcome measures ‐ including the definition of abstinence and length of follow‐up and measurements used, including any biochemical verification.
We attempted to contact the authors of the reports if there were any uncertainties or possible duplicate reporting of the same patient group, or for clarification of the study design and results. We sought separate data for participants with schizophrenia or schizoaffective disorder in trials that recruited people with a wider range of psychiatric diagnoses. Any disagreement between the authors was resolved through discussions or consultation with another author (ACW).
We categorised trials according to the primary aim of the study (i.e. smoking cessation, smoking reduction, or intervention with other aims). To group trials by category in the Characteristics of excluded studies table, we used the prefixes *, + , and ^ as part of the study identifiers. For each category, we grouped the trials according to the specifics of the intervention.
Assessment of risk of bias in included studies
During data extraction, two authors (DTT and MP) also independently assessed each trial for risk of bias according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We recorded sequence generation during randomisation, concealment of allocation, blinding, completeness of outcome data (including use of intention‐to‐treat (ITT) analysis) and selective outcome reporting for each trial. We also identified other potential sources of bias. We categorised each trial as being at low, uncertain or high risk of bias for each domain, based on the standards described in the Cochrane Handbook for Systematic Reviews of Interventions.
Measures of treatment effect
We calculated summary estimates for the extracted data. Results for dichotomous outcomes were expressed as risk ratios (RR). The RR was calculated as: ((number of participants with the outcome in intervention group / number of participants randomised to intervention group) / (number of participants with the outcome in the control group / number of participants randomised to the control group)). An RR greater than one favoured the intervention group. Results for continuous outcomes were expressed as mean difference (MD) where measured with the same scale, or standardised mean difference (SMD) where measured with different scales. A summary MD or SMD below zero favoured the intervention group in all continuous outcome measures.
Dealing with missing data
We attempted to contact trial authors for any missing data. For data synthesis, where no additional information was forthcoming, we assumed any missing data as failure to achieve the outcome. We also addressed the potential impact of the missing data in the risk of bias table for each study. We did not include trials for meta‐analysis of continuous outcomes if there was no standard deviation (SD) or other estimate of variability available.
Assessment of heterogeneity
We examined statistical heterogeneity among trials with the Cochran Q test and by calculating the I² statistic. The I² statistic describes the percentage of the variability in the summary estimate due to heterogeneity rather than chance (Higgins 2003). Values over 50% suggested moderate heterogeneity and values over 75% suggest substantial heterogeneity.
Assessment of reporting biases
Where appropriate, we assessed potential publication bias with funnel plots of the log risk ratio, mean difference or standardised mean difference.
Data synthesis
Where appropriate, we performed meta‐analysis of the trial data. For abstinence and reduction, we conducted analyses with data from six‐month follow‐up (primary outcome) and from the end of the intervention (secondary outcome). For change in mental state we conducted separate analyses for positive, negative, and depressive symptoms, using data available at the end of the intervention.
For dichotomous outcomes, we calculated the summary estimates using the Mantel‐Haenszel method and reported the 95% confidence intervals (CIs) of the risk ratios. We calculated the summary estimates for continuous outcomes using the inverse variance approach, also with 95% CIs. Change‐from‐baseline measurements and final measurements were combined for continuous outcomes if the mean difference was used to express the summary results, following the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
We pooled data using the random‐effects model, although the fixed‐effect model was also used to ensure robustness of the model chosen and susceptibility to outliers.
Sensitivity analysis
We conducted sensitivity analyses when appropriate, to assess whether the estimate of treatment effect was influenced by various factors, such as location of the trials or publication types etc.
Results
Results
Description of studies
Results of the search
We identified 976 reports from the electronic search of the databases (149 reports from MEDLINE, 477 from EMBASE, 68 from PsycINFO, 6 from CINAHL Plus, 54 from BIOSIS reviews, 105 from ISI Web of Science with Conference Proceedings, and 117 reports from CENTRAL and the Cochrane Tobacco Addiction Group Specialised Register) (Figure 1). We identified eight further trial reports from handsearching and nine ongoing studies from the online clinical trials registers and from handsearching (See Characteristics of ongoing studies). After screening, we reviewed the full text of 103 reports which were considered potentially eligible. We excluded 24 reports of 22 trials after reviewing the full text (See Characteristics of excluded studies). We also contacted the investigators of two trials to clarify the method of treatment allocation, as we had concerns that these two trials were not randomised because of the uneven number of participants among the treatment groups. We have not received any response; see Characteristics of studies awaiting classification.
1.
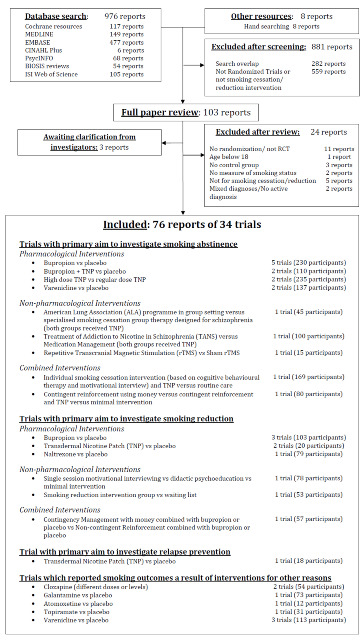
Summary of the process of identifying randomised trials for inclusion
The final review includes 34 trials; see the Characteristics of included studies table. The primary aim of 16 trials was to investigate an intervention for smoking cessation (studies prefixed with an asterisk: *George 2000; *Evins 2001; *George 2002; *Evins 2005; *Baker 2006; *Evins 2007; *Gallagher 2007; *Williams 2007; *George 2008; *Li 2009; *Williams 2010; *Weiner 2011; *Chen 2012; *Weiner 2012; *Williams 2012; *Wing 2012). Nine studies focused on smoking reduction (studies prefixed with a cross; +Hartman 1991; +Dalack 1999; +Steinberg 2003; +Fatemi 2005; +Akbarpour 2010; +Bloch 2010; +Szombathyne 2010; +Tidey 2011; +Gelkopf 2012). One trial investigated the use of nicotine patch for relapse prevention after smoking cessation (^Horst 2005). The remaining eight studies reported outcomes related to smoking abstinence or reduction, but their main aims were to evaluate the effectiveness of interventions for other purposes. These studies are reported separately, and do not contribute data to any meta‐analysis (McEvoy 1995; de Leon 2005b; Kelly 2008; Weinberger 2008; Sacco 2009; Hong 2011; Meszaros 2012; Shim 2012)
Included studies
1. Trials of interventions for smoking cessation, reduction or relapse prevention
Study and participant characteristics
There were 26 trials in this category; most were conducted in the United States and reported in English, apart from *Baker 2006, conducted in Australia; *Wing 2012, conducted in Canada; +Akbarpour 2010, conducted in Iran; +Bloch 2010 and +Gelkopf 2012, conducted in Israel; *Chen 2012 conducted in Taiwan; and *Li 2009, conducted in China and reported in Chinese. Most of the reports were published in journals, except for four trials which were only reported as letters to editors or conference proceedings (+Fatemi 2005; *Williams 2007; +Szombathyne 2010; *Wing 2012). There were three cross‐over studies (+Hartman 1991; +Dalack 1999; +Fatemi 2005) with washout periods from five days to two weeks. The relapse prevention study (^Horst 2005) involved an open‐label phase followed by a randomised controlled trial; in this review we only considered data from the randomised trial phase.
Most trials recruited participants from the community. Four trials (*Chen 2012; *Li 2009; +Akbarpour 2010; +Gelkopf 2012) recruited only smokers in inpatient units, and +Hartman 1991 recruited from hospitals and the community. Two studies did not report details of recruitment (*George 2000; +Steinberg 2003).
Three trials (+Hartman 1991; *Baker 2006; *Gallagher 2007) recruited smokers with mixed psychiatric diagnoses, but data for participants with schizophrenia or schizoaffective disorder were available for separate analysis. A significant number of studies explicitly excluded participants with any active substance misuse other than nicotine (+Dalack 1999; *Evins 2001; *George 2002; *Evins 2005; *Evins 2007; *George 2008; +Akbarpour 2010; +Bloch 2010; +Tidey 2011; *Weiner 2011; +Gelkopf 2012; *Weiner 2012; *Williams 2012; *Wing 2012). +Szombathyne 2010 investigated schizophrenia patients with both nicotine and alcohol dependence.
Sixteen trials explicitly stated that participants had expressed interest in quitting or reducing smoking (*George 2000; *Evins 2001; *George 2002; *Evins 2005; ^Horst 2005; *Baker 2006; *Evins 2007; *Williams 2007; *George 2008; +Bloch 2010; *Williams 2010; +Tidey 2011; +Gelkopf 2012; *Weiner 2012; *Williams 2012; *Wing 2012). +Steinberg 2003 measured changes in quitting motivation after motivational interviewing, where the participants had different levels of interest in quitting smoking at the baseline. Participants in *Chen 2012 also varied in their motivation and readiness to quit smoking. Target quit dates were set in 13 studies (*George 2000; *Evins 2001; *George 2002; *Evins 2005; ^Horst 2005; *Baker 2006; *Evins 2007; *George 2008; *Williams 2010; *Weiner 2011; *Weiner 2012; *Williams 2012; *Wing 2012).
Interventions
We evaluated a range of interventions. Of the studies comparing pharmacotherapy with placebo, the commonest interventions were bupropion (*Evins 2001; *George 2002; *Evins 2005; +Fatemi 2005; *Li 2009; +Akbarpour 2010; +Bloch 2010; *Weiner 2012), transdermal nicotine patch (TNP) (+Hartman 1991; +Dalack 1999; ^Horst 2005) and varenicline (*Weiner 2011; *Williams 2012). +Szombathyne 2010 investigated the effect of naltrexone in smoking and alcohol reduction. Two studies compared the combination of bupropion and TNP, with TNP and placebo (*Evins 2007; *George 2008). Two trials compared the efficacy of different dosages of TNP (*Williams 2007; *Chen 2012) for smoking cessation. Some of the drug therapy studies provided psychosocial interventions to all participants. These psychosocial interventions included group cognitive behavioural therapy (CBT) (*Evins 2001; *Evins 2005; *Evins 2007; +Bloch 2010), group therapy for motivational enhancement, psychoeducation and relapse prevention (*George 2002); group behavioural therapy (*George 2008; *Wing 2012); smoking cessation educational classes along with discussions with health educators (^Horst 2005); group psychoeducation (*Chen 2012); group therapy using the American Cancer Society Fresh Start Program (*Weiner 2012) and individual smoking cessation counselling (*Weiner 2011; *Williams 2012). The duration of drug treatment varied from seven hours (+Hartman 1991) to six months (^Horst 2005).
Five trials predominantly examined the effect of non‐pharmacological interventions. +Steinberg 2003 examined the effect of a single session of motivational interview and compared this with didactic psychoeducation and minimal control intervention. *George 2000 compared the American Lung Association programme in a group setting with a specialised group therapy designed for schizophrenia which had more focus on motivational enhancement, psychoeducation, social skills training and relapse prevention strategy; participants in both groups also received TNP. *Williams 2010 investigated the effect of the Treatment of Addiction to Nicotine in Schizophrenia (TANS) programme (individual 45‐minute weekly sessions for 26 weeks) and compared this with Medication Management (MM) (nine individual 20‐minute sessions over 26 weeks). Participants also received TNP in both groups in this trial. +Gelkopf 2012 in Israel examined the effect of a weekly group session for five weeks, focusing on smoking reduction in a hospital setting. Apart from psychosocial interventions, *Wing 2012 used repetitive transcranial magnetic stimulation (rTMS) to investigate whether this was effective for smoking cessation among individuals with schizophrenia or schizoaffective disorder.
Three other trials investigated the combined effect of pharmacological and psychosocial interventions. In *Baker 2006, a combination of individually administered motivational interviewing with CBT and TNP was compared with routine care. In a three‐arm study, *Gallagher 2007 compared contingent reinforcement (CR) using money, with and without additional TNP, and a self quit control without TNP. In +Tidey 2011, participants were randomised to four different combinations of interventions: bupropion and contingency management (CM); placebo and CM; bupropion and non‐contingent reinforcement (NR); placebo and NR.
Outcomes
Abstinence was defined and measured in 16 trials (*George 2000; *Evins 2001; *George 2002; *Evins 2005; *Baker 2006; *Evins 2007; *Gallagher 2007; *Williams 2007; *George 2008; *Li 2009; *Williams 2010; *Weiner 2011; *Chen 2012; *Weiner 2012; *Williams 2012; *Wing 2012). Three of these studies did not explicitly report whether participants expressed any interest in quitting smoking (*Li 2009; *Weiner 2011; *Chen 2012). Five trials did not report any continuation of follow‐up beyond the end of the intervention; *Williams 2007; *Li 2009; and *Chen 2012 reported abstinence at eight weeks; *Weiner 2011 and *Weiner 2012 after 12 weeks. *Wing 2012 reported abstinence at week 10, i.e. six weeks after the end of the intervention which last for four weeks. The other 10 studies provided results for longer follow‐up, of at least 24 weeks after the start of treatment. All trials except *Li 2009 validated abstinence biochemically. One study reported the rate of relapse to smoking after abstinence (^Horst 2005).
Nine trials only reported smoking reduction as the main outcome measure (+Hartman 1991; +Dalack 1999; +Steinberg 2003; +Fatemi 2005; +Akbarpour 2010; +Bloch 2010; +Szombathyne 2010; +Tidey 2011; +Gelkopf 2012). Most of the studies which measured smoking abstinence also reported some measures of smoking reduction. Self report of reduction in cigarettes per day (CPD) was commonly used as a measure of reduction (+Hartman 1991; +Dalack 1999; *Evins 2001; *George 2002; +Steinberg 2003; *Evins 2005; +Fatemi 2005; *Baker 2006; *Evins 2007; *Gallagher 2007; *Li 2009;+Akbarpour 2010; +Bloch 2010; +Szombathyne 2010; *Williams 2010; +Tidey 2011; +Gelkopf 2012; *Williams 2012). These outcomes were reported after a range of follow‐up periods which varied from two days (+Hartman 1991) to four years (*Baker 2006). Expired carbon monoxide (CO) level reduction was also frequently reported as a measure of smoking reduction (+Dalack 1999; *George 2000; *George 2002; +Steinberg 2003; *Evins 2005; ^Horst 2005; *Gallagher 2007; +Tidey 2011; *Weiner 2011; *Williams 2010; *Weiner 2012; *Wing 2012). Other measures of smoking reduction included plasma cotinine level (*Evins 2001), scale measure of nicotine dependence (e.g. Fagerström Test for Nicotine Dependence (FTND)) (+Steinberg 2003; +Fatemi 2005; *Gallagher 2007; *Li 2009; +Bloch 2010; *Weiner 2012), urine cotinine level (+Fatemi 2005; *Weiner 2012) and salivary cotinine level (*Gallagher 2007).
Most studies reported measures of mental state of the participants (+Dalack 1999;*George 2000; *Evins 2001; *George 2002; *Evins 2005; +Fatemi 2005; *Baker 2006; *Evins 2007; *George 2008; *Li 2009; +Akbarpour 2010; +Bloch 2010; *Williams 2010; +Tidey 2011; *Weiner 2011; *Chen 2012; +Gelkopf 2012; *Weiner 2012; *Williams 2012; *Wing 2012; *Chen 2012).
2. Trials of interventions with primary aim other than smoking cessation, reduction or relapse prevention
Eight trials reported outcomes of smoking behaviour change, but were not originally designed to investigate smoking cessation or reduction (McEvoy 1995; de Leon 2005b; Kelly 2008; Weinberger 2008; Sacco 2009; Hong 2011; Meszaros 2012; Shim 2012). Weinberger 2008 only included participants with schizoaffective disorder, bipolar type. Meszaros 2012 included people with both nicotine and alcohol dependence. Five studies included non‐smokers as participants, and performed separate analyses for those who smoked, in relation to their smoking behaviours (de Leon 2005b; Kelly 2008; Weinberger 2008; Hong 2011; Shim 2012). Although varenicline has been shown to be an effective treatment for smoking cessation in the general population, three studies investigated its possible uses in schizophrenia other than primarily for smoking cessation. Hong 2011 and Shim 2012 examined the effect of varenicline on cognitive function in schizophrenia. Meszaros 2012 investigated the use of varenicline as a treatment for alcohol dependence among individuals with schizophrenia or schizoaffective disorder. Two trials investigated the effect of clozapine in patients with treatment‐resistant schizophrenia (McEvoy 1995; de Leon 2005b). Other interventions included galantamine (Kelly 2008), atomoxetine (Sacco 2009) and topiramate (Weinberger 2008). None of these trials included smoking abstinence as an outcome, but used various methods to measure smoking reduction.
Risk of bias in included studies
1. Trials of interventions for smoking cessation, reduction or relapse prevention
We judged 11 trials to have used an adequate method for generating the randomisation sequence (+Dalack 1999; *Evins 2001; +Steinberg 2003; *Evins 2005; ^Horst 2005; *Baker 2006; *Evins 2007; *Gallagher 2007; *Williams 2010; +Tidey 2011; +Gelkopf 2012). Most of the other studies were classified as unclear because there was no description of the randomisation process and we could not clarify details with the investigators. We obtained additional information on *Li 2009 and +Bloch 2010 (see details in Characteristics of included studies), and judged these two trials as having a high risk of bias.
We judged five studies to have used an adequate method of allocation concealment (+Dalack 1999; *Evins 2001; *Evins 2005; *Evins 2007; *Williams 2010). Other studies did not clearly report the method of allocation concealment and we could not clarify this with the investigators, so the risk of bias was judged to be unclear. Correspondence with *Li 2009, showed that there was no concealment of allocation sequence and hence we judged the study as having a high risk of bias. We had some clarification from *Gallagher 2007 regarding allocation concealment. In their study, allocation was not done centrally and there was a possibility that research staff might know which group the subsequent participant would be assigned to. Hence, we judged that study as having a high risk of bias in allocation concealment. +Bloch 2010 reported that people were randomly allocated based upon their order of arrival and we judged that it was unlikely that allocation concealment was done properly and hence that it had a high risk of bias. We also obtained information from +Gelkopf 2012 regarding their randomisation (see details in Characteristics of included studies), and we believe that it is likely that allocation concealment would be compromised at the very end of the drawing, as the next person's allocation group would become obvious. As a result, we also judged it as high risk of bias.
Adequate blinding to treatment allocation in assessment of outcomes was observed in 10 trials (+Hartman 1991; +Dalack 1999; *Evins 2001; *George 2002; *Evins 2005; +Fatemi 2005; *Evins 2007; +Tidey 2011; *Williams 2012; *Wing 2012). Some studies reported double‐blinding but their reports did not explicitly state who was blinded, and we were not able to clarify this with the investigators (*Williams 2007; *George 2008; *Li 2009; +Akbarpour 2010; +Bloch 2010; +Szombathyne 2010; *Weiner 2011; *Chen 2012: *Weiner 2012). We judged that double‐blinding implied that it was likely that participants and investigators were blinded, but we declared all these studies as having an unclear risk of bias even though it was likely that the possible bias introduced into these studies was minimal. Some studies were assessed to have inadequate blinding. Significant bias could be introduced in these studies without adequate blinding, as self report measures (e.g. self reported reduction of cigarettes used) and subjective assessment (e.g. assessment of psychiatric symptoms) were used for outcome assessments. Three studies did not report any blinding (*George 2000; *Gallagher 2007; +Gelkopf 2012). Only the outcome assessor was blinded in another three studies (+Steinberg 2003; *Baker 2006; *Williams 2010). ^Horst 2005 blinded participants but not the outcome assessor.
There were wide‐ranging variations in how missing outcome data were handled. We judged nine studies as having a low risk of bias secondary to incomplete outcome data (+Dalack 1999; *George 2002; *Baker 2006; *Evins 2007; +Akbarpour 2010; *Weiner 2011; *Chen 2012; +Gelkopf 2012; *Weiner 2012). These studies included all participants who were randomised and used true intention‐to‐treat analysis. Those with missing data were classified either as non‐abstinent or as failing to achieve smoking reduction in these studies (*Baker 2006; *Evins 2007; *Weiner 2012). Some trials used the 'last observation carried forward' approach to handling missing data (+Steinberg 2003; *Gallagher 2007). We had a concern whether this approach was appropriate, as those who were lost to follow‐up may be more likely to relapse, so that the 'last observation carried forward' assumption would probably have overestimated the intervention effect by assuming these participants to have maintained abstinence. Hence, we categorised these trials as having a high risk of bias for incomplete outcome data. In other trials, participants who were randomised were excluded from the analysis for various other reasons. These reasons included dropping out before the start of the intervention (*Evins 2001; *Evins 2005; *George 2008; *Williams 2010; +Tidey 2011; *Williams 2012); the need for dose change for symptom stabilisation or side effects of medications (*George 2000); stopping the intervention during the trial (^Horst 2005; *Li 2009; +Bloch 2010); and lost to follow‐up (+Hartman 1991). We judged all these studies to have a high risk of bias for incomplete outcome data. Three trials did not clearly state how they handled missing outcome data, and were classified as having an unclear risk of bias (+Fatemi 2005; *Williams 2007; +Szombathyne 2010). *Wing 2012 mentioned that an intention‐to‐treat analysis was employed but we could not confirm this. As a result, we classified this trial as at unclear risk of bias.
Three studies did not report all outcome results as predicted in their methods section or in their protocol, and these trials were classified as having a high risk of selective reporting (+Dalack 1999; +Fatemi 2005; *Gallagher 2007).
There were large differences in contact time between the intervention and control groups in a number of trials which examined the effect of non‐pharmacological interventions. *Baker 2006 compared an intervention involving eight hours of individual contact over eight weeks with routine care, which had no extra contact time. *Gallagher 2007 compared three groups; Contingent Reinforcement (CR) with transdermal nicotine patch (TNP), CR only, and self quit without any active intervention. The self quit group had only three visits, but the other two groups had 12 visits for each group. +Steinberg 2003 compared three groups: motivational interview for 40 minutes; didactic psychoeducation for 40 minutes; and minimal intervention for five minutes. In *Williams 2010, the Treatment of Addiction to Nicotine in Schizophrenia (TANS) group received 24 sessions of 45‐minute individual psychological intervention, compared to the Medication Management (MM) group only received nine 20‐minute sessions. +Gelkopf 2012 compared the smoking reduction intervention group which had a weekly one‐hour session for five weeks, with the waiting list which only received one lecture on the dangers of smoking.
There were some other possible biases. Despite randomisation, four studies had statistically significant differences in some characteristics between the intervention and the control groups (*George 2000; *Evins 2005; *Williams 2010; +Tidey 2011). In ^Horst 2005, where the RCT phase followed an earlier open‐label phase, the report did not clearly state whether the two comparison groups were similar in terms of their baseline characteristics. Six trials lacked biochemical validation of smoking status (+Hartman 1991; *Li 2009; +Akbarpour 2010; +Bloch 2010; +Szombathyne 2010; +Gelkopf 2012). Two of the three cross‐over studies had relatively short washout periods, of five days (+Dalack 1999) and one week (+Hartman 1991). In the other cross‐over study (+Fatemi 2005), individual data were not available in the report and it was unclear whether paired analyses were used in the analysis. In those studies which were reported either as 'letters to editors' or as conference proceedings (*Williams 2007; *Weiner 2011; *Wing 2012), there was insufficient information to assess whether any other important bias existed, and we judged them as unclear. *Williams 2012 was sponsored by the drug company that manufactured varenicline, and we judged it as unclear whether any other important bias existed.
2. Trials of interventions with primary aim other than smoking cessation, reduction or relapse prevention
Within this group we only judged two trials to have a low risk of bias in sequence generation (Kelly 2008; Meszaros 2012), and one trial as having a low risk of bias in allocation concealment. Other trials did not explicitly describe the way in which the randomisation sequence was generated, and we could not clarify this with the investigators, so the risks of bias in sequence generation and allocation concealment were rated as unclear. Four trials reported double‐blinding but their reports did not explicitly state who were blinded, and we were not able to clarify this with the investigators (McEvoy 1995; Sacco 2009; Meszaros 2012; Shim 2012). The study by de Leon 2005b excluded four participants from the analysis without stating the reason. Another study used the 'last observation carried forward' method for missing data (Weinberger 2008). In Hong 2011 and Meszaros 2012, there were no intention‐to‐treat analyses and they did not include all people who were randomised in their denominators. Hence, we judged these four trials as having a high risk of bias for incomplete outcome data.
In Kelly 2008 and Weinberger 2008, the results in the reports were subgroup analyses of larger related trials, and some people who smoked were not included in the analysis. The reason for not including these people was unclear, and selection bias might have been introduced. The study by de Leon 2005b reported unequal numbers among the intervention groups and there was no information as to whether these groups were comparable in characteristics and in their baseline cotinine levels. There were also baseline differences between comparison groups in the study by McEvoy 1995. We therefore judged all these trials as having a high risk for other biases.
Effects of interventions
We have grouped the included studies under the following categories: 1. Trials in which the primary aim was smoking cessation; 2. Trials in which the primary aim was smoking reduction; 3. Trials in which the primary aim was relapse prevention; 4. Trials of other interventions which reported smoking outcomes. Within each category, if appropriate, trials were grouped according the principal intervention comparison in each study. For instance, if the main comparison of a study was a drug therapy (even if there was any additional psychosocial intervention for both treatment and placebo groups), the study was grouped under pharmacological interventions. Similarly, if the main comparison of a study was a psychosocial intervention (even if there was any additional drug treatment to all the comparison groups), this was grouped under non‐pharmacological interventions.
1. Trials with a primary aim of smoking abstinence
1.1 Pharmacological intervention ‐ bupropion
Intervention rationale: Bupropion is an atypical antidepressant with both dopaminergic and adrenergic actions. There is robust evidence that bupropion is a safe and effective treatment for nicotine dependence in the general population (Hughes 2007). There is however a theoretical concern about the safety of using bupropion in patients with schizophrenia, as bupropion may precipitate or exacerbate psychosis because of its pharmacodynamic and pharmacokinetic properties. Bupropion and its metabolite inhibit the cytochrome P450 CYP2D6 isoenzyme, and co‐administration of bupropion with drugs that are metabolised by this isoenzyme (including antipsychotic medications such as risperidone, haloperidol) may cause significant drug interactions (GlaxoSmithKline 2008). This, as well as bupropion’s dopaminergic action, may adversely affect the mental state of individuals with schizophrenia. In addition, seizure is a recognised adverse effect of bupropion in the general population, with a rate of between 0.1% and 0.4% (GlaxoSmithKline 2008).
Abstinence outcomes
Seven trials with a total of 340 participants investigated bupropion as an aid for smoking cessation. Five trials (*Evins 2001; *George 2002; *Evins 2005; *Evins 2007; *George 2008) had six‐months follow‐up from the start of bupropion treatment. *Weiner 2012 and these five trials recruited participants who were interested in quitting smoking, and set a target quit date. The study in China by *Li 2009 did not report whether participants had any interest in quitting. At six‐months follow‐up, participants who took bupropion were nearly three times more likely to be abstinent compared to those allocated to placebo, with a lower confidence interval that just excluded one (five trials, N = 214, risk ratio (RR) 2.78, 95% confidence interval (CI) 1.02 to 7.58, I² = 0%; Analysis 1.1; Figure 2). There was no strong evidence for a difference in relative effect between the three trials using bupropion as the sole pharmacotherapy and the two trials using bupropion as an adjunct to transdermal nicotine patch (TNP) (*Evins 2007; *George 2008); confidence intervals were wide in both subgroups. The number of successful quitters was small in all studies. Two trials (*Evins 2001; *Evins 2007) reported data on smoking cessation from a follow‐up of longer than six months: In the two‐year follow‐up report for *Evins 2001, 4 of 18 participants were abstinent, including the only person who was abstinent at the end of the trial. The investigators reported that three of the four abstinent after two years received bupropion slow release (SR) during the trial or during the follow‐up period, and the fourth quit during an extended medical hospitalisation. By the 12‐month follow‐up for *Evins 2007, two more intervention group participants had relapsed. Had the outcome at this point been used in the meta‐analysis, the estimated effect would have been smaller and the confidence intervals for the pooled estimate would have included one (i.e. statistically non‐significant).
1.1. Analysis.
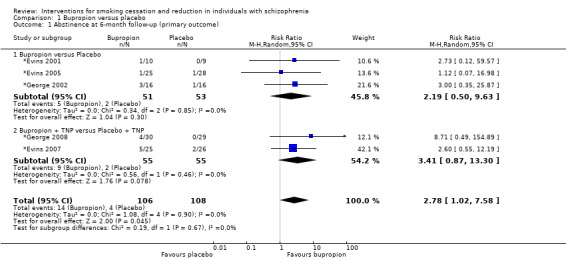
Comparison 1 Bupropion versus placebo, Outcome 1 Abstinence at 6‐month follow‐up (primary outcome).
2.
Bupropion versus placebo: Abstinence at 6‐month follow‐up (primary outcome)
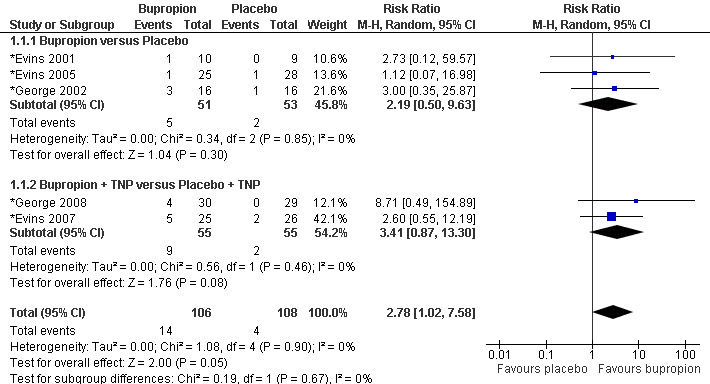
The effect size was similar for the secondary outcome of abstinence at the end of treatment, but the confidence intervals were narrower, reflecting the two additional trials and the larger number of successful short‐term quitters (seven trials, N = 340; RR 3.03, 95% CI 1.69 to 5.42, I² = 0%; Analysis 1.2). Sensitivity analyses detected no important difference in effect from omitting any of the following: one trial was conducted outside the USA and the participants' interests in quitting were uncertain (*Li 2009); or one trial using the lower dose of 150 mg bupropion daily (*Evins 2001), compared with 300 mg daily in other trials.
1.2. Analysis.
Comparison 1 Bupropion versus placebo, Outcome 2 Abstinence at end of treatment (secondary outcome).
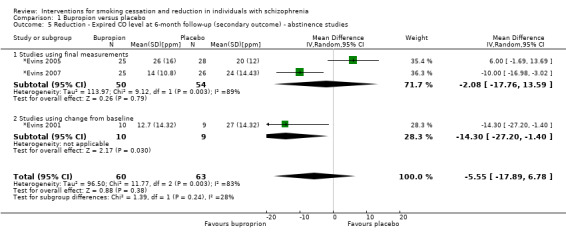
Mental state outcomes
All trials reported the effect of bupropion on the mental state of the participants. Compared with placebo, there was no evidence that bupropion caused any significant deterioration of positive, negative or depressive symptoms in patients with schizophrenia during smoking cessation. Two studies provided sufficient final measurement data for estimation of change of positive symptoms, and one additional study also provided sufficient data to estimate the effect of bupropion on negative and depressive symptoms. There was no evidence that bupropion, compared to control, caused a significant difference in positive symptoms (two trials, N = 85; standardised mean difference (SMD) ‐0.24, 95% CI ‐0.66 to 0.19; I² = 0%), in negative symptoms (three trials, N = 136; SMD ‐0.12, 95% CI ‐0.46 to 0.22; I² = 0%) or depressive symptoms (three trials, N = 136; SMD ‐0.16, 95% CI ‐0.50 to 0.18; I² = 0%) (Analysis 1.3; Figure 3). Other trials also consistently reported that there was no significant difference in these symptoms between the bupropion group and the placebo group after bupropion treatment, but without reporting full data (*George 2008; *Li 2009; *Weiner 2012). In *Evins 2001, bupropion treatment was associated with improvement in negative symptoms and greater stability of psychotic and depressive symptoms, compared to the placebo, during the quit attempt. Three studies also reported the effect of abstinence on the mental state of the participants, and found no effects of smoking abstinence on positive, negative or depressive symptoms (*Evins 2005; *Evins 2007; *George 2008).
1.3. Analysis.
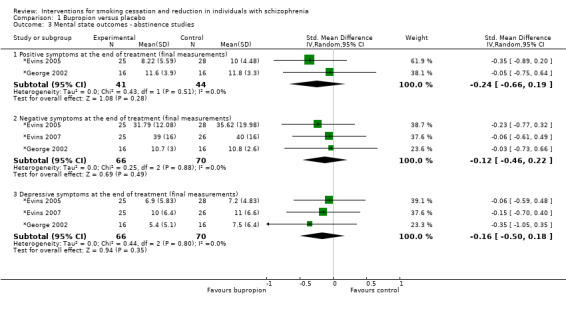
Comparison 1 Bupropion versus placebo, Outcome 3 Mental state outcomes ‐ abstinence studies.
3.
Bupropion versus placebo: Mental state outcomes
Adverse effects
Regarding other adverse effects of bupropion, one participant who took bupropion had a seizure at the end of the trial (*Weiner 2012). However, this patient had a history of polydipsia and was found to have hyponatraemia when he had the seizure. It was likely that the seizure related to polydipsia rather than to bupropion. No seizures were reported in any other trial.
The prevalence of dry mouth was significantly higher in the bupropion group compared to the control group in one study (P < 0.05; *George 2002). The same research group, in a second study (*George 2008), reported significant differences in concentration, jitteriness, light‐headedness, muscle stiffness and frequent nocturnal awakening in the bupropion group. Three of the 59 participants (two in the placebo group and one in the bupropion group) had a psychotic breakdown during that trial, but the authors concluded this was unrelated to bupropion. *Li 2009 reported significantly higher prevalence of insomnia, dry mouth and sweatiness in the bupropion group compared to the control group. Two people from this trial had a recurrence of psychotic symptoms, but the author did not report to which group they had been allocated. One participant in *Evins 2005, randomised to bupropion, had an allergic reaction to the medication. Two participants in *Evins 2007, using bupropion and TNP, dropped out from the trial because of insomnia and dizziness. In *Weiner 2012, they did not find any significant group differences in any of the major adverse events measured by Side Effect Checklists (SEC). The SEC included common bupropion side effects such as restlessness, insomnia, dry mouth and sedation. Five participants from the bupropion group dropped out because of side effects (two people complained of restlessness and increased anxiety in the first week, one complained of worsening of psychosis, one developed a rash at week two, and one developed a seizure, as reported above). The remaining trial reported 'no serious adverse events' (*Evins 2001).
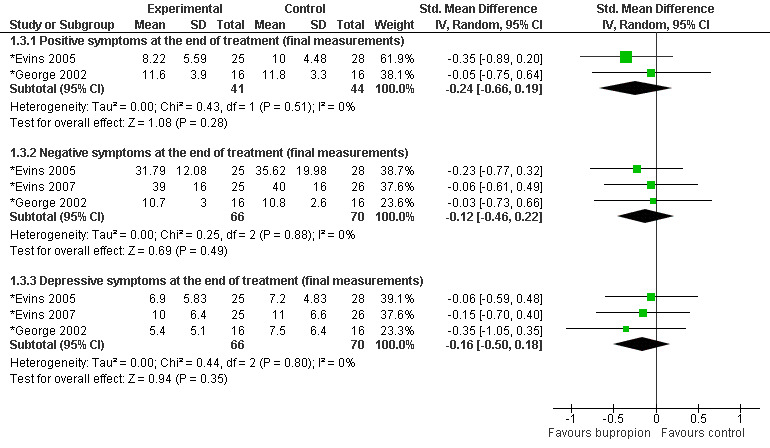
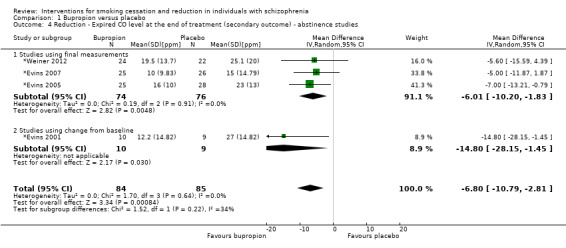
Smoking reduction
Most trials also reported some outcome measures for smoking reduction. However, the data for these outcome measures were probably from the entire sample (i.e. including participants who successfully abstained from smoking and those who continued to smoke). Three trials reported data for smoking reduction measured by expired carbon monoxide (CO) level. At the end of treatment, there was a significant reduction of expired CO in the bupropion group compared to the control group (four trials, N = 169; MD ‐6.80 parts per million (ppm), 95% CI ‐10.79 to ‐2.81 ppm, I² = 0%; Analysis 1.4). *Evins 2001 reported incomplete data for expired CO level and did not contribute to the meta‐analysis, but both favoured bupropion at the end of the treatment. At six months after the start of treatment there was no significant difference in expired CO level (three trials, N = 123; MD ‐5.55 ppm, 95% CI ‐17.89 to 6.78 ppm; Analysis 1.5) but there was substantial heterogeneity among trials (I² = 83%), largely due to one trial in which the average CO level was higher in the bupropion group than the placebo group (*Evins 2005).
1.4. Analysis.
Comparison 1 Bupropion versus placebo, Outcome 4 Reduction ‐ Expired CO level at the end of treatment (secondary outcome) ‐ abstinence studies.
1.5. Analysis.
Comparison 1 Bupropion versus placebo, Outcome 5 Reduction ‐ Expired CO level at 6‐month follow‐up (secondary outcome) ‐ abstinence studies.
Three trials provided data from the entire sample to contribute to a meta‐analysis for smoking reduction measured by cigarettes per day (CPD). At the end of bupropion treatment, there was a significant reduction of CPD in the bupropion group compared to controls (three trials, N = 184; MD ‐10.77, 95% CI ‐16.52 to ‐5.01, I² = 40%; Analysis 1.6). One study reported a separate analysis for participants who had not quit smoking; those who received bupropion had a significant reduction in CPD compared to those who received placebo (*Evins 2005). Another trial, which did not provide raw data for meta‐analysis, also reported a significant reduction in self reported CPD in the bupropion group versus the placebo group (*George 2002). At six months after starting bupropion, two studies provided sufficient data for meta‐analysis. At this point there was no significant difference in the number of CPD between the bupropion and placebo groups (two trials, N = 104; MD 0.40, 95% CI ‐5.72 to 6.53, I² = 0%; Analysis 1.7).
1.6. Analysis.
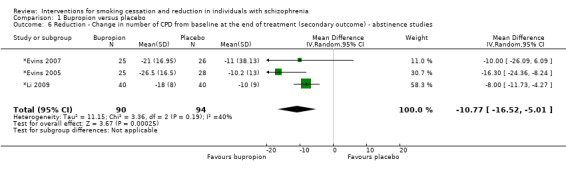
Comparison 1 Bupropion versus placebo, Outcome 6 Reduction ‐ Change in number of CPD from baseline at the end of treatment (secondary outcome) ‐ abstinence studies.
1.7. Analysis.
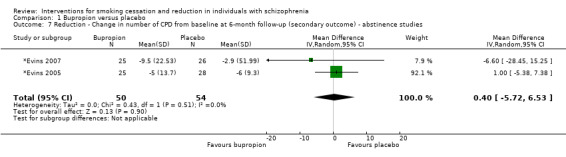
Comparison 1 Bupropion versus placebo, Outcome 7 Reduction ‐ Change in number of CPD from baseline at 6‐month follow‐up (secondary outcome) ‐ abstinence studies.
1.2 Pharmacological intervention ‐ transdermal nicotine patch (TNP)
One trial compared the use of high dose TNP (42 mg) with regular dose TNP (21 mg) in 51 patients with schizophrenia who wanted to quit smoking (*Williams 2007). There was no placebo control group. Seven‐day point prevalence abstinence rates at eight weeks were not significantly different between the high dose group (32%) and the regular dose group (23%). Survival analysis examining time to first relapse back to smoking also did not differ between the two groups. However, the authors reported that tolerability and compliance was good for both groups.
Another trial in Taiwan (*Chen 2012) investigated the effect of different doses of TNP (31.2 mg for the first four weeks, then normal 20.8 mg for the next four weeks, (high dose)), compared 20.8 mg for eight weeks (low dose) among 184 patients with schizophrenia in the chronic wards of two psychiatric hospitals. Their motivation and readiness to stop smoking were variable. Seven‐day abstinence rates at week eight were higher in the low dose compared to the high dose TNP group, although the difference was not significant (low dose: 4.3%; high dose: 1.1%). The investigators reported that the low dose TNP group reduced smoking by three more cigarettes on average, compared to the high dose group, although it is likely that this included people who succeeded in quitting entirely. There were no statistically significant differences between expired CO level and FTND scores between the two groups at the end of the intervention. There were also no significant differences between the two groups in positive and negative symptom scores.
Two other studies examined the effect of TNP together with non‐pharmacological interventions (*Baker 2006; *Gallagher 2007). In *Gallagher 2007, the smoking abstinence rate at the end of the trial (36 weeks) was significantly higher in participants who used TNP compared to those without TNP; both groups also received money as contingent reinforcement. Results of these two studies are summarised in the 'combined interventions' section below.
1.3 Pharmacological intervention ‐ Varenicline
Intervention rationale: Varenicline is a nicotinic acetylcholine α4β2 receptor partial agonist and an α7 full agonist. Varenicline is effective in treating tobacco dependence and its efficacy is probably superior to bupropion (Cahill 2012). The main adverse effect of varenicline is nausea, but this tends to subside over time. There has been concern that varenicline may be associated with psychiatric symptoms including hostility, aggression and suicidal behaviour and psychosis among individuals with and without psychiatric disorders. In February 2008, the US Food and Drug Administration issued a public health advisory, reporting an association between varenicline and an increase in neuropsychiatric adverse events (FDA 2008). This warning continues to be in place after a recent review (FDA 2011).
Abstinence outcomes
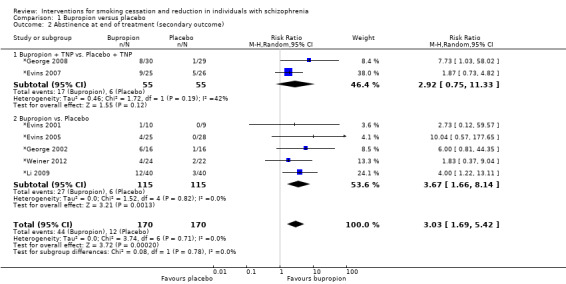
Two trials with a total of 137 participants reported smoking abstinence rates after 12 weeks of treatment with varenicline (*Weiner 2011; *Williams 2012). Both trials set the target quit date (TQD) at around one week after the start of medication. *Williams 2012 also provided data at six‐month follow‐up after starting varenicline. According to this trial, at six‐month follow‐up, participants who took varenicline were around five times as likely to abstain from smoking compared to the placebo group. However, this result did not reach statistical significance and had a wide confidence interval (one trial, N = 128, RR 5.06, 95% CI 0.67 to 38.24, P = 0.12; Analysis 2.1). Both trials contributed data to a meta‐analysis for the secondary outcome of abstinence at the end of treatment. Participants who took varenicline were also nearly five times as likely to abstain from smoking at the end of the treatment, compared to the placebo group (two trials, N = 137, RR 4.74, 95% CI 1.34 to 16.71, I² = 0%; Analysis 2.2; Figure 4). Although the RR reached statistical significance, the confidence interval was wide. A sensitivity analysis omitting *Weiner 2011 (reported as a 'letter to the editor' rather than a full paper), resulted in the RR being reduced to 4.04, just reaching statistical significance (P = 0.05).
2.1. Analysis.
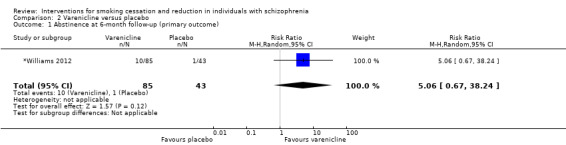
Comparison 2 Varenicline versus placebo, Outcome 1 Abstinence at 6‐month follow‐up (primary outcome).
2.2. Analysis.
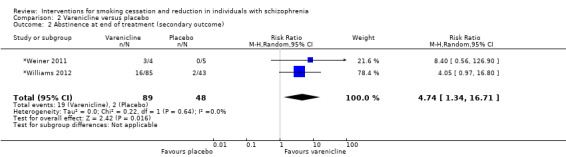
Comparison 2 Varenicline versus placebo, Outcome 2 Abstinence at end of treatment (secondary outcome).
4.
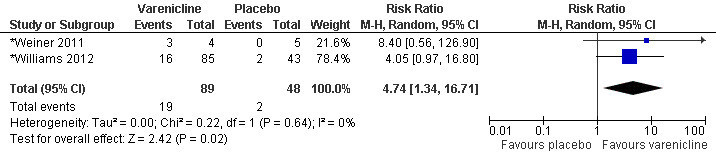
Varenicline versus placebo: Abstinence at the end of treatment (secondary outcome)
Mental state outcomes and other adverse events
Both studies reported that there were no significant differences between the varenicline and placebo groups in positive symptoms during the trial period. *Williams 2012 also did not find any difference between the two groups in negative symptoms throughout the trial, while *Weiner 2011 reported that the two groups did not differ in depressive symptoms.
*Williams 2012 mentioned that there were 13 serious adverse events (SAEs) in 10 participants (nine from the varenicline group and one from the placebo group). In the varenicline group, two patients had three SAEs which were considered to be related to varenicline use. One patient with a history of depression and suicidal ideation, as well as a history of a suicide attempt by overdose, was hospitalised for one day following six days of using varenicline. Another patient with a history of four previous suicide attempts took an overdose and suffered a seizure for which he was hospitalised ('varenicline suicidal patient 1'). No treatment‐related adverse events were reported in the placebo group. One death was reported during the post‐therapy follow‐up period, from accidental drowning 51 days after the last dose of varenicline. The investigators did not consider this to be treatment‐related. They did not find any between‐group differences for other adverse effects, including neuropsychiatric SAEs or study discontinuations. The most common adverse events in the varenicline group were nausea (23.8%), headache (10.7%) and vomiting (10.7%). In *Weiner 2011, no participant reported any suicidal ideation at baseline or throughout the trial. The varenicline group reported worsening of constipation, insomnia and nausea, which have all been noted previously as side effects of varenicline in the general population.
Smoking reduction
*Williams 2012 reported that for non‐abstinent participants, there was a statistically significant reduction of cigarettes per day (CPD) from baseline, in favour of the varenicline group at week 12, who smoked three fewer CPD compared to the placebo group (95% CI 0.4 to 6.1, P = 0.03). The result was no longer significant at week 24. However, non‐abstainers in both groups had reduced levels of expired carbon monoxide (CO) level at week 12, but the difference was not statistically significant (P = 0.11). In *Weiner 2011 from week four onwards the varenicline group showed a significantly greater reduction of expired CO from baseline compared to the placebo group (P = 0.02), although it was unclear whether this result included those who managed to abstain from smoking.
1.4 Non‐pharmacological intervention ‐ American Lung Association (ALA) programme in group setting versus specialised smoking cessation group therapy designed for schizophrenia (both groups receiving transdermal nicotine patch (TNP))
*George 2000 investigated the efficacy of specialised smoking cessation group therapy for patients with schizophrenia, interested in quitting. There was a borderline significant difference in smoking abstinence rate at the end of the trial (based on continuous abstinence in the last four weeks of treatment) between the American Lung Association (ALA) programme group (23.5%), and the specialised group therapy group (32.1%, P = 0.06). However, at six‐month follow‐up, the smoking abstinence rate was significantly higher in the ALA programme group (17.6%) than the specialised group therapy group (10.7%, P < 0.03). There was no statistically significant difference in the expired CO level between the two therapy groups during the course of the trial. There were also no significant differences in psychiatric symptoms or medication side effects between the ALA group and the specialised group therapy group. The authors performed a secondary analysis based on whether the participant received atypical or typical antipsychotic medications. Smoking abstinence rates at the end of the trial and at six‐months follow‐up were significantly higher in the group of patients who receive atypical antipsychotic medications.There was also a significant reduction in expired CO level with TNP in patients treated with atypical antipsychotic medications, compared to those treated with typical antipsychotics.
1.5 Non‐pharmacological intervention ‐ treatment of addiction to nicotine in schizophrenia (TANS) versus medication management (MM) (both groups receiving transdermal nicotine patch (TNP))
*Williams 2010 examined two manualised individual behavioural counselling approaches ‐ treatment of addiction to nicotine in schizophrenia (TANS) and medication management (MM), alongside TNP. There were no statistically significant differences in abstinence rates between the two groups at 12 weeks after the target quit date (TANS: 15.6%; MM: 26.2%, P = 0.22), at six months (TANS: 14%; MM: 16%, P = 0.78) and at 12 months (TANS: 12%; MM: 12%, P = 0.90). There were overall significant reductions of expired CO levels and CPD from baseline in both groups, but there were no differences in CO reduction and reduction of CPD between the two groups. The author also reported that there was a positive association between the percentage of sessions attended and the smoking abstinence rate at 12 weeks, regardless of the treatment conditions.
1.6 Non‐pharmacological intervention ‐ active repetitive transcranial magnetic stimulation (rTMS) versus sham rTMS
Intervention rationale: repetitive transcranial magnetic stimulation (rTMS) is a non‐invasive technique that can induce changes in brain cortical function. High frequency (>1 Hz) rTMS to the dorsolateral prefrontal cortex (DLPFC) has shown potential as a smoking cessation therapy by reducing tobacco craving and consumption in smokers without a psychiatric diagnosis (Eichhammer 2003; Amiaz 2009).
In *Wing 2012, active rTMS (four weeks with five treatments per week) was compared with sham rTMS. Active rTMS did not increase smoking abstinence rates. While it significantly reduced tobacco craving in the first week, active rTMS did not alter craving in the following three weeks.
1.7 Combined interventions ‐ individual smoking cessation intervention (based on cognitive behavioural therapy (CBT) and motivational interview) and transdermal nicotine patch (TNP) versus routine care
*Baker 2006 compared the effect of an individual smoking cessation intervention (based on CBT and motivational interview) and TNP versus routine care in a group of patients with psychotic disorders of mixed diagnoses. All the participants expressed interest in quitting smoking. The authors provided a subgroup analysis of people with a diagnosis of schizophrenia and schizoaffective disorder (N = 169). There were no overall statistically significant differences between the treatment group and the control group in either continuous abstinence or point prevalence abstinence rates at three months, six months, twelve months and four years after the initial assessment (the authors had set the threshold for statistical significance at P < 0.01 to control for multiple comparisons). In terms of smoking reduction, there was a significant difference at three months after the initial assessment, with 42.5% of the treatment group reducing their cigarette consumption by at least 50% relative to baseline, compared with 15.7% of the control group (odds ratio 3.96, 99% CI 1.53 to 10.23, P < 0.001). However, the differences in smoking reduction between the treatment group and the control group were not statistically significant at subsequent follow‐up sessions at six months,12 months and four years after the initial assessment.
1.8 Combined interventions ‐ Contingent reinforcement (CR) using money versus contingent reinforcement and transdermal nicotine patch (TNP) versus minimal intervention
*Gallagher 2007 evaluated the effects of CR using money (with and without additional TNP) compared with minimal intervention in a group of patients with serious mental illnesses. We conducted a subgroup analysis for participants with a diagnosis of schizophrenia or schizoaffective disorder (N = 80). About 32.5% of participants expressed interest in quitting smoking. The abstinence rates at weeks 20 and 36 (the end of the trial) were significant higher in the CR with TNP group, compared with the CR group without TNP (week 20: 56.3% versus 27.8%; week 36: 50% versus 27.8%), and also versus the minimal intervention group (week 20: 10%; week 36: 10%). There was also a significantly larger reduction in Fagerström Test for Nicotine Dependence (FTND) scores in the CR with TNP group both at week 24 and at week 36, compared with the CR group without TNP, and with the minimal intervention group. The CR with TNP group had a significantly lower expired CO level both at week 20 and at week 36 compared to the minimal intervention group. However, there was no significant difference in the expired CO level at either week 20 or week 36 between the CR groups with and without TNP. Number of CPD was lower at week 36 in the CR with TNP group compared to the minimal intervention group, but there was no statistically significant difference at week 20. There was no significant difference in the number of CPD either at week 20 or at week 36 between the CR group and the minimal intervention group, nor between the CR groups with and without TNP.
2. Trials with a primary aim of smoking reduction
2.1 Pharmacological intervention ‐ bupropion
Three trials investigated primarily the effect of bupropion for smoking reduction (+Fatemi 2005; +Akbarpour 2010; +Bloch 2010). +Tidey 2011 investigated the effect of bupropion with contingency management, compared with placebo and non‐contingent reinforcement. Two trials (+Akbarpour 2010; +Bloch 2010) provided data contributing to a meta‐analysis for smoking reduction measured by number of CPD. At the end of about three months of bupropion treatment, there was no significant difference in the number of CPD between the bupropion group and the placebo group (two trials, N = 93; mean difference (MD) ‐2.61, 95% CI ‐7.99 to 2.77, I² = 0%; Analysis 1.8). +Bloch 2010 reported scores measuring positive and negative symptoms before and after the intervention, and analysis showed that there were no significant differences between bupropion and placebo groups for positive and negative symptoms at the end of the treatment. Neither trial reported any other adverse effects related to bupropion.
1.8. Analysis.
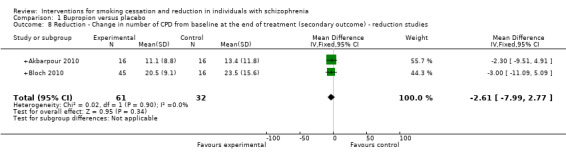
Comparison 1 Bupropion versus placebo, Outcome 8 Reduction ‐ Change in number of CPD from baseline at the end of treatment (secondary outcome) ‐ reduction studies.
In the cross‐over study by +Fatemi 2005, the investigators reported that at the end of the 21‐day active bupropion phase, participants showed a non‐significant trend for reductions in exhaled CO, urine cotinine and urine nicotine and metabolites, compared with the placebo phase. These participants were encouraged to reduce the amount they smoked, rather than to quit entirely. Their results also showed that during the trial, bupropion did not exacerbate positive and negative symptoms in these patients.
In +Tidey 2011, the investigators did not find that the 300 mg dose of bupropion for 22 days reduced smoking, as measured by expired CO level, urinary cotinine level and CPD. The researchers commented that their participants did not actively seek smoking cessation treatment and may have had lower motivation levels compared with other studies. They also reported that bupropion did not increase psychiatric symptoms. In addition, there were no significant differences in adverse events between the bupropion and placebo groups. There were no reports of seizure or of suicidal behaviour in the bupropion group.
2.2 Pharmacological intervention ‐ transdermal nicotine patch
Two cross‐over trials investigated the efficacy of the transdermal nicotine patch (TNP) as a single pharmacotherapy for smoking reduction in schizophrenia. +Dalack 1999 examined the effect of TNP on smoking reduction over 32 hours in 10 participants with schizophrenia who did not express interest in quitting smoking. The expired CO level and CPD were not significantly different whether the participants were using the TNP or placebo. Subgroup analysis suggested that the heaviest smokers (identified by placebo phase nicotine plasma level or expired CO level above group median, i.e. nicotine plasma level > 20.4 ng/ml or expired CO level > 42.5 ppm) had a statistically significant decrease in expired CO level of at least 20%. The author reported that although nicotine levels increased with the TNP, there was no evidence of nicotine toxicity or significant side effects. Psychiatric symptoms did not differ significantly between the TNP phase and the placebo phase. However, there was a statistically significant increase in abnormal involuntary movements with TNP plus smoking, and six out of ten people had more abnormal involuntary movement when using the TNP.
+Hartman 1991 investigated the effect of TNP for seven hours on smoking reduction in a group of 14 people who did not try to stop smoking. We re‐analysed the data for 10 patients with schizophrenia and schizoaffective disorder. These patients smoked significantly fewer cigarettes while receiving nicotine than while receiving placebo (N = 10, mean number of cigarettes with nicotine = 10.5, mean number of cigarettes with placebo = 13.5, t = ‐3.21, df = 9, P < 0.05). There was no biochemical measurement in this trial. The report also noted that only those who smoked at least 12 cigarettes (approximately 1.8/hour) while wearing the placebo patch achieved benefit from the nicotine patch. No participants reported any difference in subjective experience while wearing either patch, nor did they or the observers notice any changes in their mental status.
2.3 Pharmacological intervention ‐ naltrexone
Intervention rationale: naltrexone is an opioid‐receptor antagonist and has been found to be useful as an adjunct in the treatment of alcohol dependence after successful withdrawal. Smoking and alcohol dependence frequently occur together. Quitting drinking may increase the likelihood of successful smoking cessation among individuals with both alcohol and nicotine dependence.
+Szombathyne 2010 investigated naltrexone's efficacy for smoking reduction in patients with schizophrenia who were also dependent on alcohol and nicotine. They did not detect any significant reduction of CPD between the naltrexone and placebo groups. Five per cent of the participants managed to quit smoking at the end of the 12 weeks (abstinence was not clearly defined), and there was no statistically significant difference between naltrexone and placebo for smoking rates. The authors noted that patients who quit drinking successfully during the trial were more likely to quit smoking as well.
2.4 Non‐pharmacological intervention ‐ single session motivational interviewing versus didactic psychoeducation versus minimal intervention
+Steinberg 2003 did not detect a significant reduction in CPD or changes in expired CO level among the three groups, at one week and at one month after the psychosocial intervention. However, a greater proportion of participants receiving the motivational interviewing intervention followed through on a referral for tobacco dependence treatment within one week and one month postintervention, although there was no statistically significant difference among the groups in their motivation to quit smoking. The participants showed mixed levels of interest in quitting smoking.
2.5 Non‐pharmacological intervention ‐ smoking reduction intervention group versus waiting list
+Gelkopf 2012 compared a smoking reduction intervention group with people on a waiting list, measuring by reduction of CPD at three months without biological verification, in a group of chronic inpatients with schizophrenia. They found a significant reduction of CPD in the intervention group compared with the waiting list control group. They also found a significant reduction in the PANSS scores (Positive And Negative Syndrome Scale ‐ a measure of positive and negative symptoms in schizophrenia) in the intervention group compared with the control group.
2.6 Combined Interventions ‐ contingency management with money combined with bupropion or placebo versus non‐contingent reinforcement combined with bupropion or placebo
+Tidey 2011 found a significant reduction in urinary cotinine, expired CO level and CPD in weeks three and four among people who received contingency management with money for 22 days, compared with those who received non‐contingent reinforcement. Bupropion, however, did not increase the efficacy of contingency management.
3. Trials with a primary aim of preventing relapse to smoking
Transdermal nicotine patch
^Horst 2005 reported the relapse rate of recent quitters with schizophrenia who were randomised either to active or placebo TNP for six months. Participants had quit smoking by the end of an open‐label phase during which they had received group support and TNP. A significantly higher proportion of those on placebo (eight out of eight) compared with those on active TNP (three out of nine) relapsed prior to completion of the six‐month period (P < 0.01). There was no report of skin rash for any participants. In addition, the authors did not report any dropouts due to adverse events.
4. Trials of other interventions reporting smoking outcomes
4.1 Clozapine
Intervention rationale: clozapine is an atypical antipsychotic medication with a significant risk of agranulocytosis and seizure. Hence, it is restricted to patients with treatment‐resistant schizophrenia. Previous literature (mainly naturalistic studies or case reports) has suggested that clozapine treatment may be associated with a reduction of smoking in schizophrenia.
We identified two randomised controlled trials (RCTs) (McEvoy 1995 and de Leon 2005b), which examined the effect of different doses or blood levels of clozapine on the mental state of patients with treatment‐resistant schizophrenia. These two trials measured the smoking behaviour of the participants; it was uncertain whether participants had any interest in quitting smoking. McEvoy 1995 investigated the number of cigarettes smoked and expired CO levels in people with different blood levels of clozapine. Participants with a therapeutic plasma level of clozapine (> 200 ng/ml) showed a significant decline of between 25 and 35% in the number of cigarettes smoked and expired CO level. Participants with subtherapeutic clozapine plasma levels (50 ‐ 150 ng/ml) did not show any change in these measures of smoking. However, the authors also recommended a cautious interpretation of the results, as those assigned to subtherapeutic clozapine also had lower CO levels at baseline.
de Leon 2005b used a number of different ways to re‐analyse the data on smoking status from an RCT of different doses of clozapine for 16 weeks. They did not find any evidence in any of their five analyses to support clozapine for reducing smoking. However, the authors stated that they could not rule out a small decrease in smoking in some participants, which did not yield significant changes in total sample mean values.
4.2 Galantamine
Intervention rationale: galantamine is an acetylcholinesterase inhibitor. It has been used as a cognitive enhancing medication for dementia. Recent literature suggests its effect on cognitive enhancement may extend to other mental illnesses like schizophrenia. It also acts as a positive allosteric modulator of nicotine acetylcholine receptors (nAchR), which some research has suggested may help in the management of nicotine dependence.
Kelly 2008 investigated the effect of galantamine on cognitive function among patients with schizophrenia. In a secondary analysis of data from smokers, they did not detect any statistically significant difference in expired CO level before and after 12 weeks of galantamine treatment in participants who received galantamine or placebo. On the contrary, there was a significant and moderate increase in the mean score of FTND in those who took galantamine compared with placebo (effect size of 0.4). These participants had not expressed interest in quitting smoking.
4.3 Atomoxetine
Intervention rationale: atomoxetine is a norepinephrine (noradrenaline) reuptake inhibitor, approved for the treatment of attention deficit hyperactivity disorder (ADHD). Atomoxetine is thought to increase extracellular levels of both norepinephrine and dopamine in the prefrontal cortex, which may help to improve the neurocognitive deficits in patients with schizophrenia. Nicotine may improve selected cognitive deficits in these patients. One theory for the high rates of smoking in schizophrenia is that patients may remediate their neurocognitive deficits by smoking. Hence, there is a suggestion that atomoxetine may moderate nicotine dependence by improving the cognitive function of people with schizophrenia.
Sacco 2009 investigated the effects of atomoxetine on cognitive function and cigarette smoking among people with schizophrenia. They did not detect any statistically significant changes in smoking behaviour, measured by cigarette consumption or expired CO levels in smokers with schizophrenia taking atomoxetine for two weeks, compared with those on placebo. The authors did not report whether or not the participants had any interest in quitting smoking. Atomoxetine was well tolerated and there was no evidence of changes in positive or negative symptoms during the trial.
4.4 Topiramate
Intervention rationale: topiramate is an anticonvulsant which may have clinical benefits as an adjunctive treatment for bipolar disorder. It has been suggested that topiramate may help in treating addictions including nicotine dependence due to its modulation of dopaminergic activity in the cortico‐mesolimbic axis through actions on GABAergic and glutamatergic systems.
Weinberger 2008 reported a secondary analysis of the level of smoking in their trial investigating the efficacy of topiramate as a treatment for schizoaffective disorder (bipolar type). The authors did not detect any significant change in the expired CO level in a subgroup of 24 smokers treated for eight weeks with topiramate or placebo. There were also no significant differences in the reduction of psychiatric symptoms between the topiramate and placebo groups.
4.5 Varenicline (used for reasons apart from smoking cessation or reduction)
Three trials examined the effect of varenicline for purposes other than smoking cessation or reduction. Two studies focused on its effect on cognitive function in people with schizophrenia (Hong 2011; Shim 2012), and the third investigated its use to reduce alcohol dependence in smokers with schizophrenia as a primary outcome (Meszaros 2012).
Hong 2011 used a reduced dose of varenicline (i.e. 0.5 mg twice daily) instead of the usual dose of 1mg twice daily. This trial included both smokers and non‐smokers with schizophrenia, with the smokers expressing no desire to quit. The investigators reported a significant reduction in CPD in those who received varenicline compared with the placebo group (P = 0.04). Expired CO levels were also reduced in the varenicline group compared with the placebo group, but the result did not reach statistical significance (P = 0.21). They also reported that two people who received varenicline and one who received placebo quit smoking by the end of the eight‐week trial. Regarding the mental state of participants and adverse effects, the investigators reported a trend toward reduced psychosis in the varenicline group compared with the placebo group, but this analysis included both smokers and non‐smokers. Nevertheless, they note that there were no differences in treatment effects between smokers and non‐smokers. They did not find any statistically significant differences of negative or depressive symptoms between smokers on varenicline or placebo. Both smoking and non‐smoking participants in the varenicline group reported no increase in suicidal ideation during the trial, nor was there a higher incidence of common side effects compared with the placebo group.
Shim 2012 included both smokers and non‐smokers with schizophrenia in their study investigating the effect of varenicline on cognitive function in individuals with schizophrenia in Korea. They reported that during the eight‐week study, levels of smoking (measured by expired CO levels) in the varenicline group were significantly reduced compared with the placebo group. Regarding mental state and adverse effects, there was no significant change in positive and negative symptoms during varenicline treatment compared with the placebo group. The investigators also reported that no‐one displayed significant depressive symptoms or suicidal ideation. Nausea (30.5% versus 10.3%) and headache (10.2% versus 0%) were significantly higher in the varenicline group compared with the placebo group. However, all the results for mental state and adverse effects included both smokers and non‐smokers, and we were unable to obtain subgroup analyses restricted to smokers from the investigators. Four people (two from each group) were withdrawn from the trial because of worsening of psychotic symptoms, with the investigators commenting that it was not clear if varenicline had caused the deterioration in mental state.
Published as a conference proceeding, Meszaros 2012 reported a study of varenicline for the treatment of alcohol and nicotine dependence in people with schizophrenia. They reported recruitment difficulties; since the beginning of the study in 2008, only 10 patients had been randomised and started on treatment (five each on varenicline and placebo). Four participants (two from each group) had dropped out of the study prior to completion, and two more patients (one from each group) were lost to follow‐up. The study was terminated in 2011. In a personal communication, the authors reported that among the four remaining participants the mean reduction in the number of cigarettes per week was 47 (Standard Deviation 77) in the placebo group and 66 (Standard Deviation 65) in the varenicline group. This difference did not reach statistical significance, and the authors commented that this was probably due to the small sample size. Regarding mental state and adverse events, the investigators found no significant change in positive, negative and general symptoms of schizophrenia during the study. For the people in the varenicline group who did not complete the study, one dropped out because of vomiting, irritability and passive suicidal ideation seven days after starting varenicline ("varenicline suicidal patient 2"). Another dropped out at week four, due to nausea and vomiting. The third was lost to follow‐up as he was incarcerated for violating a restraining order. The investigators also found that nausea, vomiting and abdominal pain was more frequent in the varenicline group. They concluded that varenicline treatment in schizophrenia patients with both smoking and alcohol dependence may be problematic, due to safety concerns and limited tolerability because of gastrointestinal adverse effects.
Discussion
Summary of main results
Interventions used in trials to help smokers with schizophrenia to stop or to reduce smoking are heterogeneous. Table 1 and Table 2 summarize the main results of this review for the most important outcomes. Smokers with schizophrenia who used bupropion to aid smoking cessation were nearly three times as likely as those on placebo to be abstinent at the end of the drug therapy. Although there were fewer trials with follow‐up of six months or longer, the relative effect on abstinence seemed to be sustained at six months, and the results appeared consistent among trials. However, the evidence for sustained abstinence was based on five small trials from just two research groups.
At the end of treatment, smokers with schizophrenia who received bupropion smoked about 11 fewer cigarettes per day (CPD), than those who took placebo. A reduction of expired carbon monoxide (CO) level also occurred in the bupropion group, compared with the placebo group, but was not sustained to six months. The findings for smoking reduction should be interpreted with caution, as these data included the entire sample, combining abstainers and continuing smokers. Hence, the mean reduction included smoking abstinence, as well as reduction in those who did not manage to stop smoking. This explanation may be further supported by the lack of evidence of significant reduction in smoking in those trials aimed primarily at smoking reduction. We found no evidence in support of bupropion as an adjunct to contingency management.
We found no evidence to suggest that smokers with schizophrenia had significant deterioration in positive, negative or depressive symptoms of schizophrenia linked with bupropion. Although some adverse effects of treatment which may be important to patients were noted, there were no serious adverse clinical events such as seizure or suicide. However, the total number of people on bupropion was small (170 in trials for abstinence and 94 in trials for reduction), so there may not be adequate power to test for differences in risks of low event rates, such as seizure; the risk of seizure with bupropion in the general population is between 0.1% and 0.4%.
It was unclear whether transdermal nicotine patch (TNP) helped smoking cessation in this group of patients, as it was tested in only a few trials with small sample sizes. There was some indirect evidence that the abstinence rate was higher in the group with contingency reinforcement with TNP, compared to the group with contingency reinforcement alone (*Gallagher 2007). Some studies showed that TNP may reduce the number of CPD (+Hartman 1991) or the Fagerström Test for Nicotine dependence (FTND) score (*Gallagher 2007), but the available evidence did not show that TNP reduced the expired CO level (+Dalack 1999; *Gallagher 2007). One study showed that TNP may reduce the relapse rate of smoking after smoking abstinence in schizophrenia. Higher doses of TNP did not show any additional benefit in smoking abstinence or preventing relapse after smoking cessation in schizophrenia.
We found some evidence that smokers with schizophrenia who used varenicline for smoking cessation were nearly five times more likely to abstain from smoking at the end of treatment, compared with those who took placebo. However, this evidence was based on only two trials, one of which reported preliminary results with a small number of participants. In addition, there was insufficient evidence from one trial as to whether an effect was sustained at six‐month follow‐up. There was no study investigating the efficacy of varenicline used primarily for smoking reduction. After considering studies for abstinence and studies that examined the effect of varenicline for other non‐smoking purposes, we did not find consistent evidence suggesting that varenicline reduced smoking among people with schizophrenia. Regarding the mental state of the participants, there was no evidence that varenicline caused worsening of positive, negative or depressive symptoms. However, two people out of a total of 144 smokers receiving varenicline reported suicidal ideation or behaviour.
We found no evidence to support the use of naltrexone for smoking reduction in smokers with schizophrenia and alcohol dependence. There were inconclusive findings that the antipsychotic clozapine helped in smoking reduction in people with schizophrenia. There was also no evidence to support the use of galantamine, atomoxetine or topiramate as aids to smoking cessation or to smoking reduction for individuals with schizophrenia.
Regarding non‐pharmacological interventions, there was some evidence to support the use of financial contingency reinforcement (CR) for smoking cessation and reduction in people with schizophrenia. In one study, CR, with and without TNP, increased the abstinence rate for smoking in schizophrenia sufferers at week 20 and week 36. There was also some evidence from two trials that CR, with and without TNP or bupropion, significantly reduced the level of smoking in those with schizophrenia. Nevertheless, there was no evidence that CR produced sustained results for these outcomes once it was withdrawn. In addition, these findings should be treated with caution, as the evidence was based on only two trials.
We found evidence from one small trial that a smoking reduction intervention group, compared to waiting list controls, may reduce the number of CPD in inpatient smokers with schizophrenia who had been in hospital for at least one year. However, there were some concerns with the methodology of this study, and they did not use biological verification. Otherwise, we found no evidence that a single session of motivational interviewing reduced smoking in people with schizophrenia. There was also no evidence that specialised smoking cessation group therapy specifically designed for patients with schizophrenia was more effective for either smoking cessation or reduction, compared with a standard smoking cessation programme. We did not find any evidence to suggest that intensive individual behavioural counselling sessions designed for people with schizophrenia improved smoking cessation or reduction. In addition, repetitive transcranial magnetic stimulation (rTMS) of the dorsolateral prefrontal cortex (DLPFC) did not increase the smoking abstinence rate among smokers with schizophrenia.
There were design limitations in most of the included trials. For example, most studies had small numbers of participants and only a few studies reported outcomes beyond the six‐month follow‐up. These factors have limited the validity and precision of the evidence.
Overall completeness and applicability of evidence
In this review, the participants of the included studies were recruited from inpatient units, the community, or from outpatient psychiatric treatment sites, and represent a range of patients with schizophrenia. Interest in quitting smoking varied across sites and studies. As a result, there was significant clinical heterogeneity between the included trials. We therefore considered it was appropriate to perform a meta‐analysis and report the pooled estimates only for studies testing bupropion and varenicline, because they were relatively more homogenous.
Our review includes both pharmacological and non‐pharmacological interventions. For medication treatments, the U.S. Food and Drug Administration (FDA) has approved nicotine replacement therapies (gum, patch, nasal spray, inhaler and lozenge), bupropion, and varenicline as first‐line medications for the treatment of nicotine dependence in the general public. For this review, we found several studies that examined the use of these drug treatments for smoking cessation and reduction in schizophrenia, including those who investigated varenicline for other purposes rather than primarily for smoking cessation or reduction. There are also a number of ongoing studies which investigate the use of varenicline (Evins (NCT00621777); Fatemi (NCT01111149); Smith (NCT00802919)) and hopefully these trials will be able to provide more evidence of the effectiveness of varenicline in the near future. We did not find any studies that examined the effect of other forms of nicotine replacement, such as gum, nasal spray, inhaler and lozenge in people with schizophrenia, but there is an ongoing study which investigates the use of nicotine nasal spray for smoking cessation in people with schizophrenia (Williams (NCT01010477)).
Apart from one trial which investigated the use of naltrexone in smokers with schizophrenia and alcohol dependence, we did not find any trials of other medications that have been investigated for possible efficacy for smoking cessation in the general public, such as clonidine, nortriptyline and selegiline. We also examined the effects of antipsychotics (in particular clozapine) in smoking reduction in those with schizophrenia, as there have been a number of reports about the possible link between antipsychotic use and nicotine dependence in schizophrenia patients (Ereshefsky 1985; McEvoy 1995a). In addition, smokers with schizophrenia may use nicotine to improve their cognitive function (Adler 1998; Sacco 2004). We found studies which examined the effects of medications such as galantamine and atomoxetine for smoking reduction in individuals with schizophrenia. Finally, topiramate modulates dopaminergic activity in the brain through its action on GABAergic and glutamatergic systems, and it has been suggested that topiramate may have an effect on addiction (Johnson 2005). We identified one study which examined its effects on smoking in patients with schizoaffective disorder.
Previous reviews have shown that individual behavioural counselling, group behavioural therapy and telephone counselling are effective interventions to help smokers in the general public to quit smoking (Lancaster 2005a; Stead 2005; Stead 2006). Simple advice from a physician and self help material may also increase smoking cessation rates in the general public (Lancaster 2005b; Stead 2008). Motivational interviewing, especially by primary care physicians and trained practitioners, may also increase the rate of smoking cessation in the general public (Lai 2010). There was no evidence that single session motivational interviewing reduced smoking in people with schizophrenia, or that specialised smoking cessation therapies (group or individual) designed for patients with schizophrenia were superior to non‐specialised therapy. We found no studies comparing group therapy with individual therapy in participants with schizophrenia, nor any studies of telephone counselling, simple advice from a physician, or self help interventions in smoking cessation or reduction in those with schizophrenia. There was no evidence to support the use of active repetitive transcranial magnetic stimulation (rTMS) for smoking cessation in people with schizophrenia.
Interestingly, we found some evidence from two studies with different designs to support the use of money as an incentive to increase abstinence rates and reduce smoking in people with schizophrenia, at the end of the trial. The durations of these two trials was 22 days and 36 weeks respectively, with no follow‐up data after withdrawal of the incentive. A previous review has suggested that incentives do not enhance long‐term cessation rates, and that early success may not be maintained when the rewards are no longer offered (Cahill 2011).
A recent review suggests that combined pharmacotherapy and behavioural support increase smoking cessation success in the general public when compared with a minimal intervention, or with usual care (Stead 2012). We found three trials of combined pharmacological and non‐pharmacological interventions (two with contingent reinforcement and one with an individual counselling intervention). Although both the CR trials showed a higher rate of smoking reduction, with or without smoking cessation, there was no direct conclusive evidence that adding drug treatment (TNP or bupropion) increased the effectiveness of the non‐pharmacological intervention. The other study, examining the effect of an intervention based on cognitive behavioural therapy and motivational interviewing among smokers with schizophrenia, did not demonstrate increased abstinence rates.
In this review, we report smoking reduction as one of the secondary outcomes. Smoking cessation is the recommended method to reduce the harms to smokers (US Department of Health and Human Services 2000). Smoking reduction has been proposed as a non‐cessation method to reduce harm from tobacco. There is evidence to suggest that smokers who are not interested in quitting can make significant reductions in their smoking when they receive appropriate treatment, and that these reductions can be maintained over time (Hughes 2005). One of the concerns over smoking reduction is that it may undermine smokers' motivation to quit smoking, as they may see reduction as an easier alternative to abstinence, and that reduction may be all that they want or are able to achieve. Nevertheless, recent literature has shown that smoking reduction increases the probability of future cessation (Hughes 2006). Individuals with schizophrenia have much lower smoking cessation rates compared with the general population (de Leon 2005a), and smoking reduction may be a step towards cessation. We hypothesize that this step towards accomplishing the task of smoking cessation might increase their self efficacy and make subsequent success more likely. Smoking reduction may also make it easier to quit smoking by reducing the level of nicotine dependence, which is a major barrier to smoking cessation (Shadel 2000).
Most of the trials also provided some information about any potential harmful effects of interventions, in particular on the mental state of the participants. Some medications for smoking cessation are psychotropic themselves (e.g. bupropion), or have been reported to have possible serious neuropsychiatric side effects (e.g. varenicline). It is important to monitor whether these medications have a major impact on mental stability in these patients. Additionally, nicotine withdrawal can cause changes in the mental state, including depression and anxiety (Zwar 2007).
There is some literature reporting interventions which address tobacco addiction at an organization or system level (Lawn 2005; Shmueli 2008; Wye 2009). These interventions may include training of staff to manage tobacco addiction among patients with schizophrenia, and changing psychiatric facilities into smoke‐free settings (Ziedonis 2007). This is particularly important as a number of countries including the UK and the USA have enforced smoking bans in mental health units. However, we did not find any RCTs for these interventions in our search.
Quality of the evidence
For this review, the largest body of evidence was for bupropion, including seven studies and a total of 340 participants in the meta‐analysis. The number of studies was relatively small, and there was no significant heterogeneity between them. In addition, we found some evidence for varenicline from two studies with a total of 137 participants, and no significant heterogeneity between them. There was also some evidence for contingency reinforcement with money from two trials, but their clinical heterogeneity meant that we did not combine the data.
The evidence for the other interventions, including NRT, individual counselling and group therapy, was limited, even though there is good evidence of their benefit for other populations of smokers. Hence, gaps in the evidence for treatments other than bupropion in patients with schizophrenia is probably due to a low number of trials rather than to unpublished studies with negative findings.
The main aim of some included studies was to examine the efficacy of an intervention for other purposes, rather than primarily for smoking cessation or reduction (McEvoy 1995 and de Leon 2005b for clozapine; Kelly 2008 for galantamine; Weinberger 2008 for topiramate; Sacco 2009 for atomoxetine; Hong 2011, Meszaros 2012 and Shim 2012 for varenicline). Apart from Meszaros 2012, all these trials included smokers who were not trying to quit. These studies all reported smoking status as a secondary outcome, with subgroup analyses used in some of them to investigate the effects of the interventions for smokers. In three of the trials, some of the smokers were excluded from the subgroup analyses without justification. The results of these studies should therefore be viewed with caution.
Potential biases in the review process
We have used comprehensive search strategies and wide inclusion criteria, thereby improving the chances of identifying all relevant trials. We obtained reports in any language and unpublished data such as conference abstracts, to reduce potential selection and publication biases. Outcomes had to be at least six months after the intervention and at the end of the intervention, so that the immediate effect and long‐term sustained abstinence could be compared. We conducted sensitivity analyses in the meta‐analysis, and evaluated the robustness of the findings.
There are two issues to consider in this review. Firstly, the number of studies which were included in the meta‐analysis for bupropion and varenicline is relatively small, so we did not produce a funnel plot to explore potential publication bias. We can not exclude the possibility that we may have missed studies with negative results and small sample size. Publication bias can significantly distort the results of a meta‐analysis, especially when the number of studies is relatively small. Secondly, the findings may not apply to all smokers with schizophrenia, as some of the included trials explicitly excluded patients with a diagnosis of both schizophrenia and a co‐morbid substance misuse other than nicotine.
There has been more emphasis recently on the importance of evaluating the potential harms associated with interventions in both clinical trials and systematic reviews (Cuervo 2003; Tunis 2003). This review also examines as one of its outcomes, the effect of different interventions on the mental state of smokers with schizophrenia. This allows us to address the question of whether different interventions can safely be used in this population.
Agreements and disagreements with other studies or reviews
In the Cochrane review of antidepressants for smoking cessation, Hughes 2007 estimated that bupropion increased the odds of quitting smoking after at least six months by approximately 70%, when used as the sole pharmacotherapy (odds ratio (OR) 1.69, 95% confidence interval (CI) 1.53 to 1.85, 36 trials, 11440 participants). It did not detect a significant effect from combining bupropion and nicotine replacement therapy (NRT), compared with NRT alone after six months (OR 1.23, 95% CI 0.67 to 2.26, 6 trials, 1106 participants). Although our pooled estimates suggest that bupropion may have a significant beneficial effect on smoking abstinence in people schizophrenia, neither the subgroup analysis for bupropion alone, or for bupropion and TNP, reached statistical significance.
Cahill 2012 reported that varenicline at standard dose at least doubles the chances of successful smoking cessation after six months or more, compared with placebo (risk ratio (RR) 2.27, 95% CI 2.02 to 2.55, 14 trials, 6166 participants). Lower dose regimens also increased the rate of smoking cessation, while reducing the incidence of adverse events (RR 2.09, 95% CI 1.56 to 2.78, 4 trials, 1272 participants). More participants quit successfully with varenicline than with bupropion (RR 1.52, 95% CI 1.22 to 1.88, 3 trials, 1622 participants). In this review, current evidence from the limited number of studies suggests that varenicline may increase the smoking cessation rate among individuals with schizophrenia in the short term, but the effect did not last in the longer term. Regarding safety, Cahill 2012 reported that possible serious adverse events including significant psychiatric side effects cannot be ruled out on the current evidence. There were a number of studies investigating a possible association between varenicline and suicidality using different data sources and methodology, focusing on studies in the general public (Gunnell 2009; Kasliwal 2009; Harrison‐Woolrych 2011; Moore 2011). These results need to be viewed with caution in view of the difficulties in disentangling treatment‐related events with other potential confounding factors (e.g. psychiatric effects of nicotine withdrawal, increased suicide rates among smokers). In addition, it is essential to remember that these trials routinely excluded participants with psychiatric disorders and/or other alcohol or substance misuse. A recent review of published case reports, case series and prospective studies of the use of varenicline in patients with schizophrenia and schizoaffective disorder suggested that 5% of participants (13 out of 260) experienced the onset or worsening of psychiatric symptoms (Cerimele 2012). Three of the 13 participants experienced a very brief negative effect after one dose of varenicline. They did not find any report of patients with suicidal ideation or suicidal behaviour. However, the authors only included studies published until July 2011, and as a result they missed the two trials which reported two participants with suicidal ideation or behaviours (*Williams 2012; Meszaros 2012) as summarised in this review.
Regarding using contingent reinforcement for smoking cessation, Cahill 2011 concluded that incentives did not enhance long‐term smoking cessation rates among general populations. In addition, early success usually disappeared when rewards were no longer offered, although in one trial of 878 smokers, it achieved high and long‐lasting success rates by giving large cash rewards (up to USD750). Our review found some evidence that contingent reinforcement using money increased the smoking cessation rate, as well as reducing the amount of smoking among people with schizophrenia when the rewards were offered. We did not find any follow‐up data to examine the effect of longer‐term efficacy.
We did not find evidence to support the use of nicotine replacement therapy for smoking cessation or reduction in people with schizophrenia, which does not square with the strong evidence supporting the efficacy of all forms of NRT (Stead 2012b). Neither did higher doses of NRTshow any additional benefit for individuals with schizophrenia who smoke more heavily, compared to the general population. However, there are only a handful of small studies of the use of NRT for smoking cessation in people with schizophrenia, suggesting a lack of research in this area.
The results of this review largely concur with national guidelines, which make some recommendations about the treatment of nicotine dependence in people with schizophrenia. The Clinical Practice Guideline published by the United States Department of Health and Human Services (Fiore 2008) suggests that bupropion and nicotine replacement therapies may be effective for treating smoking in individuals with schizophrenia. Zwar 2007 also makes a similar suggestion for individuals with schizophrenia in the non‐systematically reviewed Australian guidelines on pharmacotherapy for tobacco addiction.
The Schizophrenia Patient Outcomes Research Team (PORT) has also published treatment guidance (Kreyenbuhl 2009). They recommend that those with schizophrenia who want to quit or to reduce cigarette smoking should be offered bupropion SR, 150 mg twice daily, for 10 to 12 weeks, with or without NRT to achieve short‐term abstinence. They also suggest that this pharmacological treatment should be accompanied by a smoking cessation education or support group, although they do not think there is sufficient evidence to recommend a particular psychosocial approach.
Authors' conclusions
Authors' conclusions
Implications for practice.
Our review supports the effectiveness of bupropion for smoking cessation in patients with schizophrenia. The evidence is relatively weak with wide confidence intervals, especially for longer‐term benefit, because of the low number of participants. We found no evidence of any significant deterioration of mental state secondary to use of bupropion in people with schizophrenia. Bupropion use in individuals with schizophrenia did not increase the risk of seizure. The evidence for bupropion as an aid to smoking reduction in people with schizophrenia is inconclusive.
We also found some evidence in support of varenicline for smoking cessation among individuals with schizophrenia. Compared with the bupropion trials, the number of participants is lower and the evidence weaker with wider confidence intervals. There is no evidence at present to suggest that the varenicline's effectiveness will last in the longer term. In addition, although there is no evidence that varenicline worsens symptoms in schizophrenia, there is some concern about serious adverse events such as suicidal ideation or behaviour among schizophrenia patients on varenicline. Based on the current data, we do not think this possibility can be fully ruled out.
There is some evidence that rewards using money may increase smoking cessation and reduction rates among people with schizophrenia. However, we do not find any evidence for a sustained effect, after the rewards are withdrawn. For other drug treatments (including NRT) and psychosocial interventions, we did not find sufficient convincing evidence in to support their use in clinical practice.
Implications for research.
Evidence for the effectiveness of interventions for smoking cessation and reduction in people with schizophrenia is limited to a few small studies without adequate power to detect reasonable treatment effects. Further trials with adequate sample size would be informative. Moreover, reporting of future studies should include more detailed and specific information. Some current reports do not specify whether participants were motivated to quit, which can significantly affect the abstinence rate. It will also be useful to be explicit about reduction rates in reports of trials primarily aimed at abstinence, specifying whether or not they include the entire sample, or only participants who did not quit. It is important that future trials report outcomes beyond the end of treatment, so that longer‐term effects of the intervention can be better evaluated.
In addition, the following areas should be considered for future research:
The safety of varenicline for smoking cessation in people schizophrenia;
The effectiveness of NRT for smoking cessation and reduction, especially with forms other than nicotine patches;
The interaction of antipsychotic medication treatment with smoking behaviour and cessation in people schizophrenia;
The effectiveness of different forms of psychosocial interventions, and the essential component(s) of the intervention;
Any sustained effect on smoking cessation and reduction in contingency reinforcement and other treatments;
The level of treatment compliance for smoking cessation among people with schizophrenia;
The effect of interventions at systematic and policies level (e.g. smoking ban in psychiatric wards) on smoking behaviours in patients with schizophrenia;
How to integrate treatment for smoking cessation into routine psychiatric care;
Economic analysis to address the cost‐effectiveness of different interventions. This would allow the construction of a decision analysis algorithm, which would aid clinicians, patients and policy makers in making evidence‐based treatment decisions.
What's new
| Date | Event | Description |
|---|---|---|
| 10 January 2013 | New search has been performed | Updated with new search; |
| 10 January 2013 | New citation required but conclusions have not changed | New citation version; updated with 14 new included studies; no major changes to conclusion, but with more information on varenicline studies and adverse effects. |
History
Protocol first published: Issue 3, 2008 Review first published: Issue 6, 2010
| Date | Event | Description |
|---|---|---|
| 16 February 2011 | Amended | Date for assessed as up‐to‐date corrected |
| 7 July 2010 | Amended | Graph label corrected |
Notes
The earlier part of this work (bupropion) was presented as a poster at the 17th European Congress of Psychiatry (Lisbon, 2009), and published as a review article in the British Journal of Psychiatry (Tsoi 2010).
Acknowledgements
Our thanks go to John Hughes, Eden Evins and Sumir Punnoose for their comments on the protocol; to Germaine Wong and Dennis Law for their help with data extraction and checking of the Chinese article; to Narelle Willis, Taixiang Wu and Bian Zhao Xiang for their efforts to contact investigators in China and Taiwan; and to all the authors who provided additional data from their studies.
Appendices
Appendix 1. MEDLINE search strategy
1. exp schizophrenia/
2. exp paranoid‐disorders/
3. schizo*.mp.
4. hebephreni*.mp.
5. oligophreni*.mp.
6. Psychotic*.mp.
7. psychosis.mp.
8. psychoses.mp.
9. chronic*.mp.
10. sever*.mp.
11. mental*.mp.
12. ill*.mp.
13. disorder*.mp.
14. ((chronic* or sever*) adj mental* adj (ill* or disorder*)).mp.
15. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 14
16. tardiv*.mp.
17. dyskine*.mp.
18. (tardiv* adj dyskine*).mp.
19. akathisi*.mp.
20. acathisi*.mp.
21. neuroleptic*.mp.
22. malignant.mp.
23. syndrome.mp.
24. 21 and (malignant adj syndrome).mp.
25. movement.mp.
26. disorder*.mp.
27. 21 and 25 and 26
28. parkinsoni*.mp.
29. neuroleptic‐induc*.mp.
30. parkinson's.m_titl.
31. disease.m_titl.
32. (parkinson's adj disease).m_titl.
33. 18 or 19 or 20 or 24 or 27 or 28 or 29
34. 33 not 32
35. exp dyskinesia‐drug‐induced/
36. exp akathisia‐drug‐induced/
37. exp neuroleptic‐malignant‐syndrome/
38. 34 or 35 or 36 or 37
39. 38 or 15
40. smoking cessation.mp.
41. smoking‐cessation/ or tobacco‐use‐disorder/
42. tobacco/
43. nicotine/
44. tobacco, ‐smokeless/
45. exp Smoking/th, pc [Therapy, Prevention & Control]
46. ((quit$ or stop$ or ceas$ or giv$) adj smok$).mp. [mp=title, original title, abstract, name of substance word, subject heading word]
47. tobacco‐smoke‐pollution/
48. 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47
49. smoking/
50. 49 or 48
51. randomised controlled trial.pt.
52. controlled clinical trial.pt.
53. randomized.ab.
54. placebo.ab.
55. clinical trials as topic.sh.
56. randomly.ab.
57. trial.ti.
58. 52 or 53 or 57 or 56 or 51 or 55 or 54
59. (animals not (human and animals)).sh.
60. 58 not 59
61. 60 and 50 and 39
Appendix 2. EMBASE search strategy
1. random$.af.
2. factorial$.af.
3. crossover$.af.
4. cross over$.af.
5. cross‐over$.af.
6. placebo$.af.
7. (doubl$ adj blind$).af.
8. (singl$ adj blind$).af.
9. assign$.af.
10. allocat$.af.
11. volunteer$.af.
12. crossover procedure/
13. double blind procedure/
14. Randomized Controlled Trial/
15. Single Blind Procedure/
16. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
17. smoking cessation.mp.
18. exp smoking cessation/
19. exp smoking‐/
20. ((quit$ or stop$ or ceas$ or giv$ or prevent$) adj smok$).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name]
21. exp passive‐smoking/ or exp smoking‐habit/ or exp cigarette‐smoking/ or exp "smoking‐cessation"/
22. 17 or 18 or 19 or 20 or 21
23. schizo*.mp.
24. Psychotic*.mp.
25. psychosis.mp. or Psychosis/
26. psychoses.mp.
27. 26 or 23 or 25 or 24
28. exp Schizophrenia/
29. exp Psychosis/
30. chronic*.mp.
31. severe*.mp.
32. persistent*.mp.
33. mental*.mp.
34. psychological*.mp.
35. disorder*.mp.
36. ill*.mp.
37. ((chronic* or severe* or persistent*) adj (mental* or psychological*) adj (disorder* or ill*)).mp.
38. "mental‐patient".mp. or exp Mental Patient/
39. tardiv*.mp.
40. dyskine*.mp.
41. (tardiv* adj dyskine*).mp.
42. akathisi*.mp.
43. neuroleptic*.mp.
44. malignant.mp.
45. syndrome.mp.
46. 43 and (malignant adj syndrome).mp.
47. exp Tardive Dyskinesia/
48. exp Akathisia/
49. acathisia.mp.
50. exp Neuroleptic Malignant Syndrome/
51. movement.mp.
52. disorder.mp.
53. 43 and 51 and 52
54. 27 or 28 or 29 or 37 or 38
55. parkinsoni*.mp.
56. neuroleptic‐induced.mp.
57. 41 or 42 or 46 or 47 or 48 or 49 or 50 or 53 or 55 or 56
58. parkinson's.m_titl.
59. 57 not 58
60. 59 or 54
61. 22 and 60 and 16
Appendix 3. PsycINFO search strategy
1. schizo*.mp.
2. hebephreni*.mp.
3. oligophreni*.mp.
4. Psychotic*.mp.
5. psychosis.mp.
6. psychoses.mp.
7. chronic*.mp.
8. sever*.mp.
9. mental*.mp.
10. ill*.mp.
11. disorder*.mp.
12. ((chronic* or sever*) adj mental* adj (ill* or disorder*)).mp.
13. exp schizophrenia/
14. exp psychosis/
15. exp schizoaffective disorder/
16. 1 or 2 or 3 or 4 or 5 or 6 or 12 or 13 or 14 or 15
17. tardiv*.mp.
18. dyskine*.mp.
19. (tardiv* adj dyskine*).mp.
20. akathisi*.mp.
21. acathisi*.mp.
22. neuroleptic*.mp.
23. malignant.mp.
24. syndrome.mp.
25. 22 and (malignant adj syndrome).mp.
26. movement.mp.
27. disorder*.mp.
28. 22 and 26 and 27
29. parkinsoni*.mp.
30. neuroleptic‐induc*.mp.
31. parkinson's.m_titl.
32. disease.m_titl.
33. (parkinson's adj disease).m_titl.
34. 19 or 20 or 21 or 25 or 28 or 29 or 30
35. 34 not 33
36. exp Neuroleptic Malignant Syndrome/
37. exp dyskinesia/
38. exp akathisia/
39. exp parkinsonism‐/
40. 35 or 36 or 37 or 38 or 39
41. 40 or 16
42. smoking cessation.mp. or exp smoking cessation/
43. (antismoking or anti‐smoking).mp.
44. (quit$ or cessat$).mp.
45. (abstin$ or abstain$).mp.
46. (control$ adj smok$).mp. [mp=title, abstract, heading word, table of contents, key concepts]
47. exp behavior modification/
48. 43 or 44 or 45 or 46 or 47
49. tobacco‐smoking/
50. (smok$ or cigar$ or tobacco$).mp.
51. prevention/
52. 49 or 50
53. 48 and 52
54. 51 and 52
55. 42 or 53 or 54
56. randomi*.mp.
57. singl*.mp.
58. doubl*.mp.
59. trebl*.mp.
60. tripl*.mp.
61. blind*.mp.
62. mask*.mp.
63. ((singl* or doubl* or trebl* or tripl*) adj (blind* or mask*)).mp.
64. CLIN*.mp.
65. trial*.mp.
66. (CLIN* adj trial*).mp.
67. placebo*.mp.
68. exp Placebo/
69. crossover.mp.
70. exp Treatment Effectiveness Evaluation/
71. exp mental health program evaluation/
72. random*.mp.
73. assign*.mp.
74. allocat*.mp.
75. (random* adj (assign* or allocat*)).mp.
76. 75 or 71 or 70 or 69 or 68 or 67 or 66 or 63 or 56
77. 76 and 55 and 41
Data and analyses
Comparison 1. Bupropion versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Abstinence at 6‐month follow‐up (primary outcome) | 5 | 214 | Risk Ratio (M‐H, Random, 95% CI) | 2.78 [1.02, 7.58] |
| 1.1 Bupropion versus Placebo | 3 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 2.19 [0.50, 9.63] |
| 1.2 Bupropion + TNP versus Placebo + TNP | 2 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 3.41 [0.87, 13.30] |
| 2 Abstinence at end of treatment (secondary outcome) | 7 | 340 | Risk Ratio (M‐H, Random, 95% CI) | 3.03 [1.69, 5.42] |
| 2.1 Bupropion + TNP vs. Placebo + TNP | 2 | 110 | Risk Ratio (M‐H, Random, 95% CI) | 2.92 [0.75, 11.33] |
| 2.2 Bupropion vs. Placebo | 5 | 230 | Risk Ratio (M‐H, Random, 95% CI) | 3.67 [1.66, 8.14] |
| 3 Mental state outcomes ‐ abstinence studies | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Positive symptoms at the end of treatment (final measurements) | 2 | 85 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.66, 0.19] |
| 3.2 Negative symptoms at the end of treatment (final measurements) | 3 | 136 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.46, 0.22] |
| 3.3 Depressive symptoms at the end of treatment (final measurements) | 3 | 136 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.50, 0.18] |
| 4 Reduction ‐ Expired CO level at the end of treatment (secondary outcome) ‐ abstinence studies | 4 | 169 | Mean Difference (IV, Random, 95% CI) | ‐6.80 [‐10.79, ‐2.81] |
| 4.1 Studies using final measurements | 3 | 150 | Mean Difference (IV, Random, 95% CI) | ‐6.01 [‐10.20, ‐1.83] |
| 4.2 Studies using change from baseline | 1 | 19 | Mean Difference (IV, Random, 95% CI) | ‐14.8 [‐28.15, ‐1.45] |
| 5 Reduction ‐ Expired CO level at 6‐month follow‐up (secondary outcome) ‐ abstinence studies | 3 | 123 | Mean Difference (IV, Random, 95% CI) | ‐5.55 [‐17.89, 6.78] |
| 5.1 Studies using final measurements | 2 | 104 | Mean Difference (IV, Random, 95% CI) | ‐2.08 [‐17.76, 13.59] |
| 5.2 Studies using change from baseline | 1 | 19 | Mean Difference (IV, Random, 95% CI) | ‐14.30 [‐27.20, ‐1.40] |
| 6 Reduction ‐ Change in number of CPD from baseline at the end of treatment (secondary outcome) ‐ abstinence studies | 3 | 184 | Mean Difference (IV, Random, 95% CI) | ‐10.77 [‐16.52, ‐5.01] |
| 7 Reduction ‐ Change in number of CPD from baseline at 6‐month follow‐up (secondary outcome) ‐ abstinence studies | 2 | 104 | Mean Difference (IV, Random, 95% CI) | 0.40 [‐5.72, 6.53] |
| 8 Reduction ‐ Change in number of CPD from baseline at the end of treatment (secondary outcome) ‐ reduction studies | 2 | 93 | Mean Difference (IV, Fixed, 95% CI) | ‐2.61 [‐7.99, 2.77] |
Comparison 2. Varenicline versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Abstinence at 6‐month follow‐up (primary outcome) | 1 | 128 | Risk Ratio (M‐H, Random, 95% CI) | 5.06 [0.67, 38.24] |
| 2 Abstinence at end of treatment (secondary outcome) | 2 | 137 | Risk Ratio (M‐H, Random, 95% CI) | 4.74 [1.34, 16.71] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
*Baker 2006.
| Methods | RCT, Australia. Pts recruited in the community. | |
| Participants | 298 smokers (at least 15 CPD) with ICD‐10 diagnosis of psychotic disorder. Pts who were acutely psychotic, had an acquired cognitive impairment and any medical conditions that would preclude the use of nicotine patch were excluded. All participants interested in quitting; TQD set at wk 3. 156 male, mean age of all 298 pts: 37.2, average CPD 30. 126 had a diagnosis of schizophrenia and 43 a diagnosis of schizoaffective disorder. | |
| Interventions | 1. Individually administered smoking cessation intervention (6 wkly sessions and 2 boosters at wks 8 and 10, 1 hour each): based on motivational interviewing and CBT + TNP (21 mg from wk 3 to 8; 14 mg from week 9 to 10; 7 mg from wk 11 to 12) 2. Routine care Both groups received booklets on smoking cessation. | |
| Outcomes | Abstinence measured at 3, 6, 12 ms and 4 yrs by continuous abstinence from TQD to point of assessment, and 7‐day PPA. Both were self reported and confirmed with expired CO level < 10 ppm. Reduction of smoking measured at 3, 6, 12 ms and 4 yrs by at least 50% reduced CPD. Effects on mental state were measured by BPRS, BDI and STAI. | |
| Source of funding | National Health and Medical Research Council; Rotary; Community Health and Tuberculosis Australia. TNP provided free of charge by GlaxoSmithKline and self help booklets provided at a discounted price by SANE Australia. | |
| Primary aim of the study | Smoking cessation | |
| Notes | Results here only included pts with diagnosis of schizophrenia or schizoaffective disorder; data supplied by authors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Pts drew a sealed envelope from a set in which there was initially an equal distribution of the treatment or control allocations at each site. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Outcome assessors were blinded. However, the experimental design did not allow participants to be blinded and self report was used in both primary and secondary outcome measures. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing data were classified either as non‐abstinent or as a failure to achieve smoking reduction. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | The control group were not comparable to the intervention group in terms of therapy time. In addition, bias may be introduced in definition of abstinence; if the participant reported abstinence but their expired CO level was greater than 10 ppm, the pt was still classified as abstinent. |
*Chen 2012.
| Methods | RCT, Taiwan. Pts were long stay inpatients and study was conducted in hospital setting. | |
| Participants | 184 "regular daily smokers" with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. All pts were long‐stay patients in two psychiatric hospitals (average term of current hospitalisation 8.8 yrs). Exclusion criteria included acute exacerbation of psychosis that was required transfer to acute ward, as well as severe respiratory and heart disease. Interests in quitting smoking varied among pts. No TQD set. 171 male; mean age 45.2; average CPD 13. 141 participants with a diagnosis of schizophrenia; 68% on typical antipsychotic medications. |
|
| Interventions | 1. Low dose TNP (20.8 mg) for 8 wks 2. High dose TNP (31.2 mg for 4 wks, then 20.8 mg for next 4 wks) Both groups received 6 sessions of smoking cessation group psychoeducation (20 minutes each; 2 sessions per wk) after starting TNP |
|
| Outcomes | Abstinence measured as self report 7‐day PPA at wk 8 (verified by expired CO level < 10ppm) Reduction of smoking measured by reduction of CPD, expired CO level and FTND scores at baseline, wk 5 (CPD only) and wk 8. Effects on mental state measured by PANSS. Parkinsonism symptoms measured by SAS. |
|
| Source of funding | National Health Bureau, Department of Health, Taiwan | |
| Primary aim of the study | Smoking cessation (although investigators state that smoking reduction is their primary outcome, because of very low % of pts achieved smoking cessation in their pilot study) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Reported double‐blind, but unclear who were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Included every pt who had been randomised in the analyses. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | Low risk | Nothing stated |
*Evins 2001.
| Methods | RCT, USA. Pts recruited from the community. | |
| Participants | 19 smokers (at least half a pack of CPD) with DSM‐IV diagnosis of schizophrenia. All pts were on stable dose of antipsychotic medications for at least 4 wks. Patients excluded if co‐morbid substance abuse, bulimia, a history of seizure disorder or current major depressive episode. All pts were interested in quitting; TQD set between wks 3 and 4. 11 male; mean age 44.1; 16 white; average CPD 34. 8 pts were on clozapine and 7 on typical antipsychotic. Average length of illness 12 yrs. | |
| Interventions | 1. Bupropion 150 mg/day for 12 wks 2. Placebo for 12 wks Both groups received 9 wkly 1‐hour sessions of group CBT. | |
| Outcomes | PPA measured at wks 12 and 24 (self report verified by expired CO level < 9 ppm or serum cotinine < 14 ng/ml). A follow‐up study also reported abstinence after 2 yrs. Reduction of smoking measured by serum cotinine, and ≥ 50% reduction in CPD verified with a 30% reduction of expired CO level. Measurements at baseline, wks 12 and 24. Effects on mental state measured by BPRS, SANS and HAM‐D. Parkinsonism symptoms measured by SAS and AIMS. | |
| Source of funding | NIDA & NARSAD. GlaxoSmithKline provided medications including placebo. | |
| Primary aim of the study | Smoking cessation | |
| Notes | Two‐yr follow‐up data were also available. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation sequence was generated by a computer programme. |
| Allocation concealment (selection bias) | Low risk | Randomisation was performed at the research pharmacy which was separated from the main research personnel. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Pts, outcome assessors and investigators were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 1/19 dropped out prior to start of medication and was not included in the analysis. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | Low risk | Nothing stated |
*Evins 2005.
| Methods | RCT, USA. Pts recruited from the community. | |
| Participants | 57 smokers (at least 10 CPD) with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder, depressed type. All pts were on antipsychotic medication for more than 30 days and had stable psychiatric symptoms. Pts excluded with substance use disorder (other than nicotine or caffeine) within 6 ms, or with a history of seizure disorder, bulimia, mania or current major depressive episode. All pts were interested in quitting; TQD set at wk 3. 39 male; mean age 45.7; average CPD 30. 12 pts were on clozapine, 5 on typical antipsychotic. | |
| Interventions | 1. Bupropion 300 mg/day for 12 wks (150 mg/day for first wk) 2. Placebo for 12 wks Both groups received 12 wkly 1‐hour sessions of group CBT. | |
| Outcomes | 7‐day PPA and 4‐wk CA at wks 12 and 24 (self report verified by expired CO level < 9 ppm). Reduction measured by expired CO level and number of cigarettes smoked. Measurements at baseline, wks 12, 14, 18 and 24. Effects on mental state measured by PANSS, SANS, HAM‐D and HAM‐A. Parkinsonism symptoms measured by SAS and AIMS. | |
| Source of funding | NIDA & NARSAD. GlaxoSmithKline provided medications. | |
| Primary aim of the study | Smoking cessation | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Generated by a computer program. |
| Allocation concealment (selection bias) | Low risk | Randomisation was performed at the research pharmacy which was separated from the main research personnel. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Nothing stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Nothing stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | More clozapine‐treated pts were randomised to the placebo group (1/25 versus 11/28). |
*Evins 2007.
| Methods | RCT, USA. Pts recruited from the community. | |
| Participants | 51 smokers (at least 10 CPD for past yr) with DSM‐IV diagnosis of schizophrenia. All pts were on antipsychotic medication for > 30 days and had stable psychiatric symptoms. Patients excluded with substance use disorder (other than nicotine or caffeine) within 6 ms, or with a history of seizure disorder, bulimia, mania or current major depressive episode. All pts were interested in quitting; TQD set at wk 4. Gender distribution uncertain; mean age 44.2; average CPD 26. 16 pts were on clozapine. | |
| Interventions | 1. Bupropion SR 300 mg/day for 12 wks. (150 mg/day for first 7 days) 2. Placebo for 12 wks Both groups received: (1) 12 wkly 1‐hour sessions of group CBT; (2) TNP (from wk 4) 21 mg/day for 4 wks, then 14 mg/day for 2 wks, 7 mg/day for 2 wks + up to 18 mg per day nicotine gum as required. | |
| Outcomes | CA at wks 8, 12, 24 and 52 (defined by meeting 7‐day PPA by self report every assessment after TQD at the time point , verified by expired CO level ≤ 8 ppm). Reduction measured by number of cigarettes smoked. Measurement at baseline, wk 12 and 24. Effects on mental state measured by PANSS, SANS, HAM‐D and STAI. Parkinsonism symptoms measured by SAS and AIMS. | |
| Source of funding | Massachusetts Department of Mental Health Federal Block Grant. GlaxoSmithKline provided medications including placebo. | |
| Primary aim of the study | Smoking cessation | |
| Notes | 6‐m abstinence used in meta‐analysis for comparability with other trials. 2 pts in the intervention group relapsed by 1 yr | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Generated by a computer program. |
| Allocation concealment (selection bias) | Low risk | Randomisation was performed at the research pharmacy which was separated from the main research personnel. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Pts, investigators and outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 5/25 (bupropion) and 8/26 (control) lost in follow‐up. Dropouts were considered smokers. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | Low risk | Nothing stated |
*Gallagher 2007.
| Methods | RCT, USA. Pts recruited from the community and study conducted in a clinic. | |
| Participants | 181 participants (60 pts in each arm, 1 died shortly after enrolment because of lung cancer) with DSM‐IV Axis 1 diagnosis of psychotic spectrum or affective disorders. At least 10 CPD and smoked regularly for > 3 yrs. CO level ≥ 10 ppm after at least 15 minutes smoke‐free at baseline visit. Pts with co‐morbid substance misuse disorder were not excluded. No TQD set. 80 had a diagnosis of schizophrenia or schizoaffective disorder. 50/80 were male; mean age 42.3; 71.2% white, 20% Hispanic, 8.8% black; average CPD 29. 32.5% wanted to cut down or quit smoking. 47.5% had co‐morbid diagnosis of substance misuse. 40% had diagnosis of schizophrenia. | |
| Interventions | 1. CR with money for 36 wks (up to USD480) if pts abstained from smoking. Pts did not receive CR at the visit if they relapsed but they would be able to resume receiving CR if they abstained again. 2. CR with money for 36 wks (as above) + TNP (dose varies between pts) for first 16 wks 3. Controls (no active intervention ‐ just attended assessment) Significant support was provided to ensure adherence for all three groups, including reminder phone calls and outreach, provision of bus pass to attend appointments. | |
| Outcomes | Abstinence at wks 20 and 36 (defined as expired CO level ≤ 10 ppm or salivary cotinine level ≤ 15 ng/ml). Reduction measured by expired CO level, FTND score, salivary cotinine level and number of CPD. Measurements were taken at baseline and various points including wks 20 and 36. Effects on mental state measured by BSI. | |
| Source of funding | Arizona Disease Control Research Commission | |
| Primary aim of the study | Smoking cessation | |
| Notes | Results in this review only include pts with diagnosis of schizophrenia or schizoaffective disorder; data supplied by authors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Generated by a computer random number generator. |
| Allocation concealment (selection bias) | High risk | A list of random numbers was used to allocate the participants by the research staff. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Nothing stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Nothing stated |
| Selective reporting (reporting bias) | High risk | Only a few outcome measures were reported. |
| Other bias | High risk | The interventions were not comparable: the self quit group had only 3 visits, compared to 12 visits in the other two groups. |
*George 2000.
| Methods | RCT, USA. Setting unclear. | |
| Participants | 45 smokers with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. FTND score at least 5. All pts were interested in quitting; TQD set at wk 3. 30 males; mean age 39.7; 28 participants were white, 13 black, 4 Hispanic; average CPD 30. 19 had a diagnosis of schizophrenia. Mean daily dose of antipsychotics (chlorpromazine equivalence) 612.3 mg. 18 pts were on atypical antipsychotics. | |
| Interventions | 1. American Lung Association (ALA) programme wkly for 10 wks (60 minutes each session): first 7 wks behavioural group therapy + final 3 wks supportive group counselling 2. Specialised group therapy designed for pts with schizophrenia, wkly for 10 wks (60 minutes each session): first 3 wks motivational enhancement therapy + last 7 wks psychoeducation, social skills training and relapse prevention strategy. Both groups also received TNP (21 mg/day for first 6 wks then 14 mg/day for another 2 wks and 7 mg/day for final 2 wks) | |
| Outcomes | Abstinence at wk 10 (end of therapy) and at 6 ms follow‐up (defined as continuous abstinence for last 4 wks ‐ by self report of cigarette use and verified by expired CO level <10 ppm). Reduction measured by expired CO level; measurements at baseline and wkly for 12 wks. Effects on mental state measured by PANSS and BDI. Parkinsonism symptoms measured by Webster Extrapyramidal symptoms scale and AIMS. | |
| Source of funding | NIMDA, NARSAD & VISN 1 Mental Illness Research Education and Clinical Centre grant from Department of Veteran Affairs, USA | |
| Primary aim of the study | Smoking cessation | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Mentioned block randomisation but unclear how the allocation sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | Baseline difference between two groups: specialised group therapy had significantly more pts with schizoaffective disorder and pts in that group also had a significantly lower negative syndrome score; the ALA group had significantly more pts prescribed atypical antipsychotics. |
*George 2002.
| Methods | RCT, USA. Pts recruited from the community. | |
| Participants | 32 smokers with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. All pts were clinically stable on psychotic or affective symptoms. They also fulfilled the following criteria: (1) FTND score ≥ 5; (2) expired CO level ≥10ppm; (3) plasma cotinine level ≥150 ng/ml. Pts were excluded if they had (1) history of epilepsy or seizure; (2) history of alcohol or drug abuse 6 ms before the study; (3) a change of dose of antipsychotic for symptom control or side effect in the past 6 ms. All pts were interested in quitting; TQD set at wk 3. 18 males; mean age 43.2; 20 white, 11 black; average CPD 24. 20 had a diagnosis of schizophrenia. 22 were on atypical antipsychotics. Mean daily dose of antipsychotics (chlorpromazine equivalence) 757 mg. | |
| Interventions | 1. Bupropion 300 mg/day for 10 wks (150 mg/day for first 3 days) 2. Placebo for 10 wks Both groups received 10 wkly 1‐hour sessions of group therapy for motivational enhancement, psychoeducation and relapse prevention. | |
| Outcomes | Abstinence at wk 10 and 6 m follow‐up (defined as 7‐day PPA verified by expired CO level < 10 ppm) Reduction of smoking measured by expired CO level and self report number of CPD. Effects on mental state measured by PANSS and BDI. Parkinsonism symptoms measured by Webster Extrapyramidal symptoms scale and AIMS. | |
| Source of funding | NIMDA, NARSAD & VISN 1 Mental Illness Research Education and Clinical Centre grant from Department of Veteran Affairs, USA | |
| Primary aim of the study | Smoking cessation | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | Low risk | Not stated |
*George 2008.
| Methods | RCT, USA. Pts recruited from the community. | |
| Participants | 59 smokers (at least 10 CPD and expired CO > 10 ppm) with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. All pts were clinically stable and on a stable dose of antipsychotic for at least 1 m before randomisation. Pts with alcohol or substance misuse or dependence 3 m before study were excluded. Pts also did not have any history of seizure disorder. All pts were interested in quitting; TQD set at day 15. 35 males; mean age 40.3; 28 white, 26 black, 4 Hispanics; average CPD 23. 32 had a diagnosis of schizophrenia. 9 pts were on clozapine and 13 pts were on typical antipsychotic. | |
| Interventions | 1. Bupropion 300 mg/day for 10 wks (150 mg/day for first 3 days) 2. Placebo for 10 wks Both groups received 10 wkly 50‐minute sessions of group behavioural therapy and TNP (21 mg per 24 hours) from day 15 to day 70. | |
| Outcomes | Abstinence was measured by self report as 7‐day PPA at day 70, CA for last 4 wks of trial (day 43 to day 70) and 6 ms post TQD. Abstinence was verified by expired CO level < 10ppm. Reduction was not reported. Effects on mental state were measured by PANSS, BDI and HAM‐D. | |
| Source of funding | NIDA & NARSAD | |
| Primary aim of the study | Smoking cessation | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | Low risk | Not stated |
*Li 2009.
| Methods | RCT, China. Pts recruited from a psychiatric inpatient unit. | |
| Participants | 80 smokers with DSM‐IV diagnosis of schizophrenia and nicotine dependence. All pts smoked at least 10 CPD for minimum of 1 yr. Their BPRS scores were ≤ 35 and CGI ≤ 3. Pts excluded with history of epilepsy, unstable physical problem, alcohol or other substance dependence and prominent psychotic symptoms. Pts' interest in quitting smoking and TQD information were not mentioned in the report. All pts were men. Mean age 38.0. Average number of CPD 30 and average yrs of smoking 17. |
|
| Interventions | 1. Bupropion 75 mg twice a day for 1 wk then 150 mg twice a day for remaining 3 wks 2. Placebo for 4 wks No other intervention for both groups. | |
| Outcomes | Abstinence defined as self reported CA for past wks at wk 1, 2, 4 and 8. There was no biological verification. Reduction measured by reduction in CPD and reduction of scores on scale measure of nicotine dependence. Effects on mental state measured by BPRS. | |
| Source of funding | Not reported | |
| Primary aim of the study | Smoking cessation | |
| Notes | Article in Chinese. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | The report mentioned the use of random number table. However, we have contacted the investigators to clarify the exact method of sequence generation. They told us that they used a random number table from a statistics textbook and five investigators were given copies of this random number table. When a participant was included, the investigators selected a random number from the table. From the description, our opinion was that the investigators did not use the random number table properly. |
| Allocation concealment (selection bias) | High risk | From our correspondence with the investigators as above, there was no concealment of allocation sequence. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | No biochemical verification of smoking status. |
*Weiner 2011.
| Methods | RCT, USA. Pts recruited from the community. | |
| Participants | 9 smokers (at least 10 CPD for a yr and FTND score ≥ 4) with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. All pts were clinically stable and on a stable dose of antipsychotic for at least 1 m before randomisation. Pts excluded with substance misuse (apart from tobacco) in the last 3 ms or dependence in the last 6 ms before study. Pts also excluded if they (1) had any lifetime history of suicide attempt; (2) had psychiatric hospitalisation within the past 6 ms; (3) had suicidal ideation or were currently depressed; (4) were taking bupropion. Pts' interest in quitting was not mentioned in the report; TQD set at the end of the third counselling session (after wk 1 visit) Demographics of participants were not reported. All pts were on second generation antipsychotic medications. | |
| Interventions | 1. Varenicline 1mg twice daily for 12 wks 2. Placebo for 12 wks Both groups received individual smoking cessation counselling based on the American Lung Association Freedom from Smoking Program. All pts had 2 sessions of counselling before starting study medication. | |
| Outcomes | Abstinence was defined as expired CO < 10ppm at each of the last 4 visits at wk 12. Reduction measured by reduction of the expired CO level. Effects of mental state measured by BPRS (positive symptoms and anxiety/depressive symptoms) and CDSS. |
|
| Source of funding | NIDA | |
| Primary aim of the study | Smoking cessation | |
| Notes | The report is a letter to the editors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information |
| Other bias | Unclear risk | Insufficient information |
*Weiner 2012.
| Methods | RCT, USA. Pts recruited from the community. | |
| Participants | 46 smokers (at least 10 CPD) with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. All pts had FTND score ≥4 and no change in their usual medication regimen. Pts were excluded with current depressive episode, substance misuse other than nicotine in the past 3 ms, substance dependence other than nicotine in the past 6 ms, or neurological diagnosis or unstable medical condition.
All pts were interested in decreasing smoking. TQD set at 2 wks after start of bupropion.
37 males; mean age 48.7. 69.6% white. Baseline mean expired CO level 26.5ppm. 28 pts were on second generation antipsychotic medications, another 13 on clozapine; others were on first generation antipsychotic. |
|
| Interventions | 1. Bupropion 300 mg/day for 12 wks (wks 2 to14) 2. Placebo for 12 wks Both groups received 9 wkly sessions of group therapy according to American Cancer Society Fresh Start Program (modified for people with schizophrenia) | |
| Outcomes | Abstinence defined as expired CO level < 10ppm for at least 4 study visits during treatment phase (sustained abstinence) Reduction measured by expired CO level, FTND score and urine cotinine level. Effects on mental state measured by BRPS and SANS. Motor side effects were monitored by SAS. Pts also underwent neuropsychological measures. | |
| Source of funding | VA Capitol Network (VISN 5) Mental Illness Research, Education and Clinical Centre | |
| Primary aim of the study | Smoking cessation | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | Low risk | Not stated |
*Williams 2007.
| Methods | RCT, USA. Pts recruited from the community. | |
| Participants | 51 smokers with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. All pts were stable on antipsychotic medications. pts who took bupropion or clonidine were excluded. All pts interested in quitting. No TQD set. Baseline characteristics not reported. | |
| Interventions | 1. TNP 42 mg daily for 8 wks 2. TNP 21 mg daily for 8 wks No other additional intervention for all groups. | |
| Outcomes | Abstinence measured at wk 8 by self report of 7‐day PPA and verified by expired CO < 8ppm. Reduction was not reported. Effects on mental state were not reported. | |
| Source of funding | NIDA, New Jersey Department of Health and Senior Services | |
| Primary aim of the study | Smoking cessation | |
| Notes | Conference proceeding only. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | According to protocol, only outcome measure was CA from smoking, reported in the conference proceeding. |
| Other bias | Unclear risk | Insufficient information. |
*Williams 2010.
| Methods | RCT. USA. Pts recruited in the community. | |
| Participants | 100 smokers (at least 10 CPD) with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. All pts took atypical antipsychotic medications for at least 1 m before the trial. Pts excluded whose MMSE < 22, or concurrent use of clonidine, bupropion, NRT, nortriptyline or other tobacco products (e.g. cigar, smokeless tobacco). All pts were willing to quit smoking. TQD set at wk 5 from the start of trial. 55 males; mean age 45.2. 65.5% white. There was a statistically significant difference in baseline CO level between 2 groups. |
|
| Interventions | 1. TANS: 24 individual sessions of 45 minutes psychological intervention over 26 wks (motivational interviewing, social skills training, use of NRT, relapse prevention technique) 2. MM: 9 individual sessions of 20 minutes psychological intervention over 26 wks (medication compliance, education about NRT) Both groups also received TNP for 16 wks after quit date (21 mg for 12 wks then 14 mg for remaining 4 wks) | |
| Outcomes | Abstinencemeasured as PPA by self report and verified by expired CO < 10ppm (TQD, 12, 26 wks and 1 yr after TQD). Reduction measured by reduction in expired CO level and CPD. Effects on mental state measured by PANSS and BDI. Therapeutic relationship was also monitored by Working Alliance Inventory (WAI). | |
| Source of funding | NIDA | |
| Primary aim of the study | Smoking cessation | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adaptive urn randomisation procedure used. |
| Allocation concealment (selection bias) | Low risk | See above |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | Baseline difference between two groups in CO level. The interventions were not comparable as they differed by therapy time. |
*Williams 2012.
| Methods | RCT, USA & Canada. Pts recruited from the community. | |
| Participants | 128 smokers (aged 18 to 75) with DSM‐IV TR diagnosis of schizophrenia or schizoaffective disorder. All pts smoked at least 15 CPD and scored at least 7 on the baseline motivation to quit score of the contemplation ladder. Pts did not have any acute exacerbation of psychiatric symptoms, nor psychiatric hospitalisation for the last 6 ms. Their PANSS score was below 70. Female pts consented for birth control if at child bearing age. Pts with the following conditions were excluded: (1) serious suicidal ideation or behaviour; (2) history of drug or alcohol abuse or dependence; (3) clinically significant cardiovascular or cerebrovascular disease in the last 6 ms; (4) any other unstable medical conditions; (5) previous use of varenicline; (6) uncontrolled hypertension; (7) body mass index <15 or >38; (8) use of other smoking cessation aids; (9) use of another investigational drug within 30 days of baseline visit; (10) use of marijuana or other non‐cigarette tobacco products. All pts were interested in quitting smoking. TQD set as 8 days after baseline visit. 98 males; mean age 41.1; 75 white; 38 African American; 6 Asians and 8 other racial group. Average CPD 23. 91 had a diagnosis of schizophrenia. 109 pts were on atypical antipsychotic. |
|
| Interventions | 1. Varenicline (0.5mg daily for 3 days then twice daily for 4 days then 1mg twice daily) for 12 wks 2. Placebo for 12 wks Both groups received wkly counselling (less than 30 minutes) | |
| Outcomes | Abstinence measured at wk 4, wk 12 and wk 24 (defined as 7‐day point prevalence of abstinence, verified by CO ≤ 10 ppm) Reduction of smoking measured by incidence of achieving 50% or greater reduction from baseline in mean CPD over the past 7 days at wk 12 and 24, as well as change of mean CPD over the previous 7 days at wks 12 and 24. Effects on mental state measured by PANSS, SAS, Columbia Suicide Severity Rating Scale (C‐SSRS) and Cinical Global Impression (CGI). |
|
| Source of funding | Sponsored by Pfizer (manufacturer of varenicline) | |
| Primary aim of the study | Smoking cessation | |
| Notes | Varenicline: Placebo in 2:1 ratio. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | Unclear risk | Sponsored by drug company |
*Wing 2012.
| Methods | RCT, Canada. Pts recruited from community | |
| Participants | 15 smokers (at least 10 CPD, baseline CO level ≥ 10ppm and a FTND score of at least 4) with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. Exclusion criteria included: (1) substance abuse or dependence in the past 3 ms; (2) current use of tobacco pharmacotherapies; (3) intolerance to TNP; (4) on high dose benzodiazepines; (5) seizure disorder; (6) metallic implant; (7) psychiatric or medical instability (e.g. PANSS score >70 or change in antipsychotic medications in the previous m); (8) pregnancy. All participants are willing to quit smoking in the next 30 days. TQD set at wk 3. Demographics of pts were not reported. |
|
| Interventions | 1. Active Repetitive Trancranial Magnetic Stimulation (rTMS) ‐ bilateral to dorsolateral prefrontal cortex (five times per wk for 4 wks) 2. Sham rTMS All pts also receive TNP (21mg/24 hour) and wkly group behavioural therapy (psychoeducation, social skills training and relapse‐prevention skills training) for smoking cession from wk 3 to wk 9. |
|
| Outcomes | Abstinence measured at wk 10 (7‐day point prevalence), as assessed by self reported smoking abstinence and expired CO level <10ppm. Reduction measured by expired CO level. Effects on mental state measured by PANSS. |
|
| Source of funding | Canadian Institue for Health Research, Canandian Tobacco Control Research Initiative, Centre for Addiction and Mental Health | |
| Primary aim of the study | Smoking cessation | |
| Notes | Letters to editors and conference proceedings. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | Unclear risk | Insufficient information to assess whether an important risk of bias exists. |
+Akbarpour 2010.
| Methods | RCT, Iran. Pts recruited from a psychiatric in‐patient unit. | |
| Participants | 32 smokers with DSM‐IV TR diagnosis of schizophrenia and all smoked cigarettes within 12 ms prior to initial interview. Pts were excluded if (1) contraindicated to bupropion including seizure disorder, current or prior diagnosis of bulimia or anorexia nervosa; (2) serious comorbid psychiatric illness including major depression; (3) recent history of alcohol use within the last 3 ms; (4) history of allergy to bupropion. Pts' interest in quitting smoking and whether a TQD was set were not mentioned in the report. All pts were men. Mean age 47.4. Average number of CPD 14. No information regarding psychiatric medications. |
|
| Interventions | 1. Bupropion 150mg daily for 3 days then 300mg daily for total 8 wks 2. Placebo for 8 wks No other addition intervention for both groups. | |
| Outcomes | Abstinence was not defined or measured. Reduction of smoking was measured by number of cigarettes smoked (mean number of smoked CPD was recorded immediately before and at the end of treatment). No biological verification. Effects on mental state measured by MMSE. | |
| Source of funding | Not reported | |
| Primary aim of the study | Smoking reduction (although it was reported as smoking abstinence) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | No biochemical verification of smoking status |
+Bloch 2010.
| Methods | RCT. Israel. Pts were recruited from the community. | |
| Participants | 61 smokers with DSM‐IV TR diagnosis of schizophrenia or schizoaffective disorder. All pts were between 18 and 70 yrs old, clinically stable as judged by their psychiatrists, and were on a stable dose of antipsychotic medication for at least 1 m. They scored at least 5 on a motivation for smoking cessation analogue scale (i.e. strong desire to quit smoking or at least reduce significantly the number of CPD). Any pts with co‐morbid Axis 1 psychiatric diagnosis were excluded. No TQD set. 46 males; mean age 41.6; 37 Jews and 24 Arabs; average CPD 41. 41 pts with diagnosis of schizophrenia; 19 with diagnosis of schizoaffective disorder. Unclear about psychiatric medications. |
|
| Interventions | 1. Bupropion 150mg daily for 3 days then 300mg daily for total 14 wks 2. Placebo for 14 wks Both groups received 15 sessions of group CBT. | |
| Outcomes | Abstinence was not defined or measured. Reduction of smoking was measured by reduction of CPD and FTND scores at wk 7 and 14. No biological verification. Effects on mental state measured by PANSS, BPRS. | |
| Source of funding | NARSAD, Phillip Morris USA and Phillip Morris International | |
| Primary aim of the study | Smoking Reduction and identify the role serotonin transporter polymorphism on smoking behaviour in schizophrenia | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Pts were randomly allocated based upon order of arrival to either the treatment or placebo group at a rate of 2:1 ratio. |
| Allocation concealment (selection bias) | High risk | Unlikely that allocation concealment was done properly if pts were allocated based upon order of arrival. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | No biochemical verification of smoking status. |
+Dalack 1999.
| Methods | Cross‐over study, USA. Pts recruited from the community but stayed in hospital during study. | |
| Participants | 10 pts with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. Moderate to severe nicotine addiction (≥20 CPD). No current non‐nicotine substance use disorder (confirmed by urine toxicology). Stable on antipsychotic medication for at least 3 ms. Pts had not expressed interest in quitting smoking. No TQD set. All males; mean age 42.1; 8 Caucasian; average CPD 35; average number of yrs smoking 26. 4 pts on clozapine. 6 pts with diagnosis of schizophrenia. Average length of illness 23 yrs. | |
| Interventions | TNP (22mg per 24 hours) versus placebo patch for 32 hours (Day 1 and Day 2). Washout period for the next 5 days. Cross‐over to the other intervention for 32 hours. No other addition intervention for both groups. | |
| Outcomes | Abstinence was not defined or measured. Reduction of smoking was measured by number of cigarettes smoked during the hospital stay and expired CO level. Measurements taken at baseline, the end of Day 1 and Day 2 (both wks). Effects on mental state measured by BPRS, SANS, HAM‐D. Parkinsonism symptoms measured by SAS and AIMS. | |
| Source of funding | Research Advisory Group, Department of Veterans Affairs | |
| Primary aim of the study | Smoking reduction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number generator was used to generate sequence. |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally at pharmacy. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | High risk | Only some of the outcomes were reported in the reports. |
| Other bias | High risk | Cross‐over study with short washout period. |
+Fatemi 2005.
| Methods | Cross‐over study, USA. Pts recruited from the community. | |
| Participants | 10 smokers with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. Pts encouraged to reduce their smoking, rather than to quit. No TQD set. Demographics for smokers were not reported. | |
| Interventions | Bupropion (dose uncertain) vs. placebo for 21 days. Washout period for 1 wk afterwards. Cross‐over to the other intervention for another 21 days. No other addition intervention for both groups. | |
| Outcomes | Abstinence was not defined or measured. Reduction of smoking measured by number of cigarettes smoked, expired CO level, FTND, urine cotinine, urine nicotine and metabolites. Measurements taken at baseline and at the end of 21 days (for both interventions). Effects on mental state measured by BPRS, PANSS, SAPS, SANS, HAM‐D and BDI. Parkinsonism symptoms measured by SAS and AIMS. | |
| Source of funding | NIH | |
| Primary aim of the study | Smoking reduction | |
| Notes | The report is a letter to the editors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | High risk | Only the results of some of the outcome measures were reported. |
| Other bias | High risk | Cross‐over design but uncertain about whether paired analyses were used or not. First period data were not available. |
+Gelkopf 2012.
| Methods | RCT, Israel. Pts recruited from a psychiatric in‐patient unit. | |
| Participants | 53 smokers with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder (at least for 5 yrs). All pts were between 18 and 65 of age and was admitted to hospital for at least a yr. They expressed interest in participating a smoking reduction programme. They smoked at least 7 cigarettes daily for > 6 ms (self report). They also met the criteria of nicotine dependence based on FTND. All pts were treated with antipsychotic medications. Exclusion criteria included significant physical illness, organic brain damage, mental retardation and diagnosis of alcohol or drug abuse or dependence. TQD not set. 28.6% of pts were women. Mean age 46.3. Average number of CPD 21. No information regarding psychiatric medications. |
|
| Interventions | 1. Smoking reduction intervention group (wkly 1‐hour session for 5 wks, delivered by 2 hospital staff) 2. Waiting list (one lecture on danger of smoking) Both groups did not receive any other smoking reduction intervention. | |
| Outcomes | Abstinence was not defined or measured. Reduction of smoking was measured by reduction of CPD at 3 ms. No biological verification. Effects on mental state measured by PANSS, HAM‐D. | |
| Source of funding | Not reported | |
| Primary aim of the study | Smoking reduction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Information provided from author regarding randomisation: investigators decided beforehand to have 18 individuals in the control group and 35 in the intervention group. They cut out 53 slips of paper each named 0 (control) or 1 (study). The investigators then took the list of participant and starting alphabetically took the slips of paper out of a box for each client. |
| Allocation concealment (selection bias) | High risk | See above. With the method described above, it is likely that towards the very end of the drawing, it would become obvious what the next person was likely to get. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | Possible contamination between the intervention group and the waiting list group, as they are inpatient in the same hospital. No biochemical verification of smoking status. The interventions were not comparable as they differed significantly in therapy time. |
+Hartman 1991.
| Methods | Cross‐over study, USA. Pts were recruited from both inpatients and outpatients. | |
| Participants | 14 smokers with mixed psychiatric diagnoses and smoked at least 10 cigarettes daily. Pts did not have any other current substance use. Pts were not interested in quitting and no TQD was set. All males; mean age 40.9; 4 white, 7 black, 2 Asian, 1 Hispanic. Average CPD 23. Average yrs of smoking 19. 8 had a diagnosis of schizophrenia and 2 a diagnosis of schizoaffective disorder. | |
| Interventions | TNP (8mg) vs. placebo patch for 7 hours (Day 1). Pts stayed for the next 2 entire days in the clinic for observation of smoking behaviour (although unlimited amount of pts' preferred brand of cigarettes were only provided during the 7 hours on patch). Cross‐over to the other intervention one wk later. No other additional intervention for both groups. | |
| Outcomes | Abstinence was not defined or measured. Reduction of smoking measured by collection of cigarette butts in pts' own container (collection of cigarette butts was observed). Effects on mental state were not measured. | |
| Source of funding | Not reported | |
| Primary aim of the study | Smoking reduction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | No biological verification of smoking status. Cross‐over design with short washout period. |
+Steinberg 2003.
| Methods | RCT, USA. Setting unclear. | |
| Participants | 78 smokers (at least 10 CPD) with diagnosis of schizophrenia or schizoaffective disorder. 53% of pts also had a history of substance use disorder. Interest in quitting smoking varied among individuals. No TQD set. 53 males; mean age 43.8; 60 Caucasians, 11 African Americans, 4 Africans, 3 Hispanic, 1 Asian; average CPD 27. 40 had a diagnosis of schizophrenia. Average length of illness was 20.8 yrs. | |
| Interventions | 1. Motivational Interview for 40 minutes (a single session) 2. Didactic psychoeducation based on ALA brochure for 40 minutes (a single session) 3. Minimal control intervention for 5 minutes (a single session) No other additional intervention for all groups. | |
| Outcomes | Abstinence not defined or measured. Reduction of smoking measured by number of cigarettes smoked, expired CO level and FTND scores. Measurements taken at baseline, one wk and 1 m after intervention. Effects on mental state not measured. | |
| Source of funding | National Cancer Institute Grant, NIDA and Centre for Substance Abuse Treatment Grant. | |
| Primary aim of the study | Smoking reduction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Mentioned randomisation in a ratio of 5:5:2 and the allocation sequence was generated by computer. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | The minimal control intervention group was not comparable to the other two interventions. |
+Szombathyne 2010.
| Methods | RCT, USA. Pts recruited from the community. | |
| Participants | 79 smokers with a diagnosis of schizophrenia or schizoaffective disorder. All pts also had combined nicotine and alcohol dependence. Demographics of participants unclear. Uncertain whether pts have interest in quitting smoking or TQD set. | |
| Interventions | 1. Naltrexone (oral ‐ 100mg on Mondays and Wednesdays, 150mg on Fridays) for 12 wks 2. Placebo for 12 wks Both groups also received wkly motivational enhancement therapy addressing alcohol use. |
|
| Outcomes | Abstinence not defined or measured. Reduction of smoking measured by number of cigarettes smoked. No biological verification. Measurements were taken at baseline, wk 12. Effects on mental state not measured. | |
| Source of funding | NIAAA, NARSAD, the World's Leading Charity Dedicated to Mental Health Research | |
| Primary aim of the study | Smoking reduction in patients with alcohol dependence and schizophrenia | |
| Notes | Conference proceeding only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to assess whether an important risk of bias exists. |
| Other bias | High risk | No biochemical verification of smoking status. |
+Tidey 2011.
| Methods | RCT, USA. Pts recruited from the community. | |
| Participants | 57 smokers (at least 20 CPD, FTND ≥6) with DSM‐IV TR diagnosis of schizophrenia or schizoaffective disorder. All pts were clinically stable on psychoactive medications for at least 2 ms. They also scored at least 4 for the Contemplation Ladder. Exclusion criteria included pregnancy, positive breath alcohol level or positive urine toxicology, medication or medical condition contraindicated the use of bupropion and high psychiatric symptom severity (i.e. ≥6 in items at BPRS).
No TQD set.
37 males; mean age 45.1; 39 white, 8 African Americans, 5 other races; average CPD 27. Pts were on a variety of antipsychotic medications. |
|
| Interventions | 4 groups:
|
|
| Outcomes | Abstinence not defined or measured. Reduction of smoking measured by reduction of number of cigarettes smoked, expired CO level and urinary cotinine level. Measurements taken at baseline, wk 2, 3 and 4. Effects on mental state measured by PANSS. Extrapyramidal side effects measured by UPDRS, AIM. Nicotine withdrawal measured by Minnesota Nicotine Withdrawal Scale (MNWS). Cigarette craving measured by Questionnaire on Smoking Urges‐brief form (QSU‐brief). | |
| Source of funding | NIH | |
| Primary aim of the study | Smoking reduction | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Tossing of coin. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | Significant differences among group on PANSS positive and negative symptoms score. |
^Horst 2005.
| Methods | Open‐label phase study followed by RCT, USA. Pts recruited from the community. | |
| Participants | 50 smokers with diagnosis of schizophrenia or schizoaffective disorder entered the open label phase. They had stable symptoms for the last 2 ms and used tobacco daily. All pts interested in quitting; TQD set. 18 pts entered the RCT phase as they fulfilled the following criteria: (1) agreed to set a quit date within 2 wks; (2) reduced their tobacco use by 75% after 60 days from the start of the open‐label phase; (3) quit smoking 100% after 90 days from the start of the open‐label phase. For all pts in the open‐label phase, 26 were men; mean age was 42.5; average pack‐yrs 39.9. | |
| Interventions | 1. TNP (Nicoderm CQ) for 6 ms (Dose ranged from 14 mg to 63 mg daily, according to pts' cotinine saliva levels. The dose was fixed throughout 6 ms) 2. Placebo patch for 6 ms. All pts received biweekly educational smoking cessation classes and motivational discussions with health educator. | |
| Outcomes | Relapse to smoking ‐ defined by expired CO level greater than 10 ppm for 2 consecutive wks. Abstinence not defined or measured. Reduction of smoking measured by expired CO level. Measurements taken at baseline, every 2 wks and at the final session. Effects on mental state not measured. | |
| Source of funding | American Legacy Foundation & Via Christi Foundation. SmithKlineBeecham provided placebo patches. | |
| Primary aim of the study | Relapse prevention after smoking cessation. | |
| Notes | Only the data from the RCT were included in this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin flip by blinded third party. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | Unclear risk | Uncertain whether there were any baseline differences for the two groups in the RCT phase |
de Leon 2005b.
| Methods | RCT, USA. Pts were in‐patients and study was conducted in hospital setting. | |
| Participants | 50 pts with DSM‐IIIR diagnosis of schizophrenia. All were treatment resistant (not responded at least 3 antipsychotics ‐ each antipsychotic was prescribed for at least 6 wks and at CPZ equivalent dose of above 1000 mg daily). CGI at least moderately ill and BPRS‐Anchored scores ≥ 45. Only 42 participants who were daily smokers were included in the analysis. Of these 42 pts, 2 withdrew before completing clozapine trial and another 2 did not provide sufficient cotinine measures. Interest in quitting smoking was uncertain. No TQD set. Demographics for smokers not reported. Average CPD 19. | |
| Interventions | 1. Clozapine 100mg daily 2. Clozapine 300mg daily 3. Clozapine 600mg daily Duration of clozapine: 16 wks. No other additional intervention for both groups. All pts were switched to haloperidol for 4 wks and then had a washout period for 1 wk before clozapine. | |
| Outcomes | Abstinence not defined or measured. Reduction of smoking measured by plasma cotinine; measurements at baseline and between 13th and 15th wks. Effects on mental state measured by BPRS‐Anchored, SANS and CGI. | |
| Source of funding | NIMH, NARSAD, Universidad Nacional (Medellin, Colombia). Novartis Research Institute provided free medication. | |
| Primary aim of the study | Efftect of different doses of clozapine on mental state. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | Unequal numbers in the three intervention groups and uncertain whether these three groups were comparable in characteristics and also baseline cotinine level. |
Hong 2011.
| Methods | RCT, USA. Pts recruited from the community. | |
| Participants | 69 pts (43 smokers) with a diagnosis of schizophrenia or schizoaffective disorder. All received antipsychotic medications and they were clinically stable for at least 4 wks. Aged between 18 and 60. Exclusion criteria included: (1) pts were undergoing smoking cessation therapy; (2) major medical conditions; (3) atrioventricular block as identified by ECG; (4) renal insufficiency. Interest in quitting smoking is not required. No TQD set. Among 43 smokers, 27 were males. Mean age 42.2. Average CPD 18. |
|
| Interventions | 1. Varenicline 0.5mg daily for 1 wk then 0.5mg twice daily for 7 wks (total 8 wks) 2. Placebo for 8 wks Both groups did not receive any additional intervention. |
|
| Outcomes | Abstinence not defined or measured. Reduction of smoking measured by reduction of CPD and reduction of the expired CO level. Measurement taken at wk 1, 2, 4, 6, 8 and 10. Effects on mental state measured by BPRS, SANS, HAM‐D and CGI. | |
| Source of funding | Stanley Medical Research Institute, NIH, Neurophysiology Core of the University of Maryland General Clincial Research Centre | |
| Primary aim of the study | Effect of varenicline on neurobiological and cognitive biomarkers in schizophrenia | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | Low risk | |
Kelly 2008.
| Methods | RCT, USA. Pts recruited from both inpatients and outpatients. | |
| Participants | 86 pts with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. All were treated by antipsychotics except clozapine. Pts were not on anticholingeric medications and with SAS score ≤4. Pts with DSM‐IV diagnosis of alcohol or substance misuse or dependence (except nicotine) were excluded. 73 Pts smoked (defined as baseline expired CO level ≥8 ppm). Only 41 pts had at least 1 follow up measurement and were included in the analysis. Among these 41 pts, 39 were men; mean age 47.5; 14 white, 28 black. Pts not interested in quitting; no TQD. |
|
| Interventions | 1. Galantamine for 12 wks (up to 24 mg/day) 2. Placebo for 12 wks No other additional intervention for both groups. | |
| Outcomes | Abstinence not defined or measured. Reduction of smoking measured by expired CO level and FTND scores. Measurements taken at baseline and every 2 wks till wk 12. Effects on mental state measured by BPRS, SANS and CGI. Parkinsonism symptoms measured by SAS and AIMS. | |
| Source of funding | VA Capital Network (VISN 5) Mental Illness, Research, Education and Clinical Centre, Stanley Medical Research Institute and NIMH. Ortho McNeil Neurologics supplied medications. | |
| Primary aim of the study | Effect of galantamine on cognitive function. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random sequence was generated by computer. |
| Allocation concealment (selection bias) | Low risk | Allocation was performed centrally at the research pharmacy. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | Subgroup analysis of another trial with significant number of smokers not included in the analysis. |
McEvoy 1995.
| Methods | RCT, USA. Pts were chronically hospitalised patients. | |
| Participants | 12 smokers with DSM‐IIIR diagnosis of chronic schizophrenia. All pts had persistent psychopathology despite extended course of typical antipsychotics. Interest in quitting smoking was uncertain. No TQD set. 8 males; mean age 34; average CPD 7. Average length of illness 16 yrs. | |
| Interventions | 1. Low clozapine (dose varied but plasma clozapine level 50‐150ng/ml) for 12 wks 2. Medium clozapine (plasma level 200‐300 ng/ml) for 12 wks 3. High clozapine (plasma level 350‐450 ng/ml) for 12 wks No other additional intervention for all groups. | |
| Outcomes | Abstinence was not defined or measured. Reduction of smoking measured by number of cigarettes smoked and expired CO level. Measurements taken at baseline and wk 12. Effects on mental state measured by BPRS and CGI. | |
| Source of funding | Not reported | |
| Primary aim of the study | Efftect of different doses of clozapine on mental state | |
| Notes | Pts were allowed free access to cigarettes for 120 minutes only. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | Potential baseline difference between groups: the low clozapine group had lower baseline expired CO level. |
Meszaros 2012.
| Methods | RCT, USA. Pts recruited from the community. | |
| Participants | 10 smokers (aged 18 to 69, at least 20 CPD over the 7 days prior to intake) with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. Pts took antipsychotic medication for at least 4 wks, and with a current DSM‐IV diagnosis of nicotine dependence and alcohol dependence. Exclusion criteria included: (1) unable to give informed consent; (2) currently receiving any pharmacological smoking cessation treatment including bupropion; (3) currently taking naltrexone, Campral or Anatabuse; (4) history of suicide attempt in the past yr; (5) suicidal ideation at baseline; (6) female of childbearing potential without contraception; (7) pregnancy; (8) unstable medical or psychiatric disorder; (9) positive urine drug screen for cocaine, opioids or amphetamine at baseline, or current DSM‐IV diagnosis of cocaine, opioid or cannabis dependence (1 m prior to enrolment). Pts expressed desire to cut down or quit smoking and drinking. No TQD set. Demographics of participants were not reported. |
|
| Interventions | 1. Varenicline 0.5mg daily for first 3 days, then 0.5mg twice daily for 4 days, then 1mg bd for 7 wks (i.e. total 8 wks) 2. Placebo (matched in appearance) for 8 wks Both groups received (1) voucher‐based incentives contingent on attendance; (2) manual based individual wkly motivational interviewing sessions every wk for up to 30 minutes each, focusing on increasing motivation to reduce or quit smoking and drinking. |
|
| Outcomes | Abstinence was not defined or measured. Reduction measured by reduction of CPD and expired CO level at the end of the treatment phase (wk 8). Efffect on mental state measured by PANSS. |
|
| Source of funding | NARSAD | |
| Primary aim of the study | Effect of varenicline on alcohol dependence (as primary outcome according to protocol) | |
| Notes | Conference proceedings only but we obtained further information from the investigators. The study terminated because of slow recruitment and high drop out rate. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation schedule provided by biostatistician. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | High risk | Only reported CPD but not expired CO level |
| Other bias | Unclear risk | Insufficient information to assess whether an important risk of bias exists. |
Sacco 2009.
| Methods | RCT, conducted in the USA. Settings unclear. | |
| Participants | 12 smokers with DSM‐IV diagnosis of schizophrenia. Demographics of participants unclear. Uncertain whether pts have interest in quitting smoking. No TQD set. | |
| Interventions | 1. Atomoxetine 40mg daily for 2 wks 2. Atomoxetine 80mg daily for 2 wks 3. Placebo for 2 wks No other additional intervention for all groups. | |
| Outcomes | Abstinence not defined or measured. Reduction of smoking measured by number of cigarettes smoked and expired CO level. Measurements were taken at baseline, day 8 and day 15. Effects of mental state were measured by PANSS. | |
| Source of funding | NARSAD & NIDA. | |
| Primary aim of the study | Effect of atomoxetine on mental state. | |
| Notes | The report is a letter to the editors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | High risk | Only report part of the results. |
| Other bias | Unclear risk | Insufficient information to assess whether an important risk of bias exists |
Shim 2012.
| Methods | RCT, Korea. Setting unclear. | |
| Participants | 120 pts (60 smokers and 60 non‐smokers) with DSM‐IV diagnosis of schizophrenia, aged between 18 and 60. All pts scored less than 75 in PANSS total score for at least 3 ms before the study. For smokers, they smoked at least 10 CPD for more than 1 yr. Exclusion criteria included: (1) serious or unstable medical disorder within previous 6 ms; (2) other DSM‐IV Axis 1 diagnosis; (3) substance abuse or dependence (except nicotine) in the last 12 ms before study; (4) pregnant or breast feeding; (5) high risk of suicide clinically; (6) use of any form of NRT or other tobacco products; (7) history of taking clozapine. Interest in quitting or reducing smoking uncertain. No TQD set. Among smokers, 55 male. Mean age 41.3. All Koreans. Average CPD 14. Average length of illness 15.1 yrs. Pts were on various antipsychotic medications. Fixed dose of psychotropic medications throughout the study in both groups. |
|
| Interventions | 1. Varenicline 0.5mg daily for day 1 to 3, then 0.5mg twice daily for day 4 to 7 then 1mg twice daily for wk 2 to 8. 2. Placebo for 8 wks No other additional interventions for both groups. |
|
| Outcomes | Abstinence not defined or measured. Reduction of smoking measured by number of cigarettes smoked and expired CO level. Measurements were taken at baseline, wk 1, 2, 4 and 8. Effects of mental state were measured by PANSS, SANS, HAM‐D, CGI. Extrapyramidal side effects measured by SAS and Barnes Akathsia Rating Scale. | |
| Source of funding | Stanley Medical Research Institue | |
| Primary aim of the study | Effects of varenicline on cognitive function in schizophrenia | |
| Notes | Subgroup demographic data (smokers vs non‐smokers) from supplementary data via journal website | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | Low risk | |
Weinberger 2008.
| Methods | RCT, USA. Pts recruited from both inpatients and outpatients. | |
| Participants | 48 pts with DSM‐IV TR diagnosis of schizoaffective disorder, bipolar type. All pts had a PANSS score at least 60 and a CGI score at least 4. Pts were on a stable dose of lithium and/or valproate for at least 2 wks before the study. Pts with alcohol or marijuana dependence or other substance misuse were excluded. Pts did not have an interest in quitting smoking. No TQD set. 31 daily smokers but only 24 participants (daily smoker and baseline expired CO level ≥ 10 ppm) were included in the data analysis. Among these 24 pts; 12 males; 13 whites, 10 African Americans; mean age uncertain; average CPD 20. | |
| Interventions | 1. Topiramate (dose variable from 100mg to 400mg daily) for 8 wks (after titration of dose) 2. Placebo for 8 wks No other additional intervention for all groups. | |
| Outcomes | Abstinence not defined or measured. Reduction of smoking measured by expired CO level. Measurements at baseline, wk 4 and wk 8. Effects of mental state measured by PANSS, MADRS, YMRS and CGI. | |
| Source of funding | NIDA & Ortho McNeil Neurologics (funded the medications and study) | |
| Primary aim of the study | Effect of topiramate on mental state. | |
| Notes | The report is a letter to the editors. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Mentioned randomisation in a ratio of 2:1 (favouring topiramate) but unclear how the allocation sequence was generated. |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment in the reports. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not stated |
| Selective reporting (reporting bias) | Low risk | All expected outcomes |
| Other bias | High risk | Only 24 participants were analysed although there were 31 smokers. |
AIMS: Abnormal Involuntary Movement Scale BDI: Beck Depression Inventory BPRS: Brief Psychiatric Rating Scale BSI: Brief Symptoms Inventory CA: continuous abstinence CBT: cognitive behavioural therapy CGI: Clinical Global Impression CO: carbon monoxide CPD: cigarettes per day DSMIV: Diagnostic and Statistical Manual of Mental Disorders 4th Edition FTND: Fagerström Test for Nicotine Dependence HAM‐D: Hamilton Depression Rating Scale ICD: International Classification of Diseases m(s): month(s) MM: medical management MMSE: Mini‐Mental State Examination NRT: nicotine replacement therapy PANSS: Positive and Negative Syndrome Scale PPA: point prevalence abstinence Pt(s): participant(s) RCT: randomised controlled trial SANS: Scale for the Assessment of Negative Symptoms SAPS: Scale for the Assessment of Positive Symptoms SAS: Simpson Agnus Scale STAI: State and Trait Anxiety Inventory TANS: Treatment of Addiction to Nicotine in Schizophrenia TNP: transdermal nicotine patch TQD: target quit date
wk(s): week(s)
YMRS: Young Mania Rating Scale
yr(s): year(s)
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Allen 2011 | The main purpose of this study is to investigate the effect of nicotine replacement therapy on agitation in smokers with schizophrenia. There was no report on smoking status. |
| Arbour‐Nicitopoulos 2011a | No measures of cigarette consumption or smoking status. Only reported measure for cigarette craving and mood changes. |
| Arbour‐Nicitopoulos 2011b | Qualitative study ‐ not RCT |
| Aubin 2012 | General review ‐ not RCT |
| Baker 2010 | General review ‐ not RCT |
| Banham 2010 | Systematic review ‐ not RCT |
| Brown 2003 | Pts aged below 18 |
| Brunette 2011 | No randomisation but allocated intervention according to location of hospital |
| Bryant 2011 | Systematic review ‐ not RCT |
| Dutra 2012 | No comparison group |
| Kisely 2006 | Before and after study without randomisation |
| McClure 2010 | Participants did not have an active diagnosis of schizophrenia during the trial |
| McEvoy 1999 | Before and after study without randomisation |
| McKee 2009 | The primary purpose of the study was to utilize mecamylamine as a mechanistic probe because of its ability to increase smoking behaviour. |
| Morris 2011 | Mixed psychiatric diagnoses and subgroup data was not available |
| Pachas 2012 | Before and after study without randomisation |
| Roll 1998 | Before and after study without randomisation |
| Shiina 2010 | Main aim of the study is to investigate the effect of tropisetron on cognitive function of patients with schizophrenia. No comparison between tropisetron and placebo group regarding effect of tropisetron on smoking status. |
| Tidey 2002 | Before and after study without randomisation |
| Tidey 2012 | Main aim of study is to investigate the separate and combined effect of acute nicotine replacement and sensorimotor smoking replacement (in the form of Very Low Nicotine Content cigarettes) on cigarette craving, withdrawal symptoms and usual brand smoking in schizophrenia and non‐schizophrenia smokers. Intervention only lasted for 25 hours. |
| Weiner 2001 | No comparison group |
| Wells 2003 | No measures of cigarette consumption or smoking status. Only reported measure for motivation to quit smoking. |
Characteristics of studies awaiting assessment [ordered by study ID]
Chen 2002.
| Methods | Controlled trial, conducted in Taiwan. Pts were recruited from a day‐care ward in a psychiatric hospital. |
| Participants | 65 pts with DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. All pts smoked more than 20 cigarettes daily and are willing to stay for 60 minutes for participating in the smoking cessation group. Pts with acute confusion, violent behaviours or did not attend more than half of the sessions were excluded from the study. Interest in quitting smoking was uncertain. No target quit date set. 60 pts were men. Mean age 40.1. |
| Interventions |
No other addition intervention for all groups. |
| Outcomes | Self report seven‐day point abstinence measured at 1 wk after participating in the smoking cessation programme (i.e. wk 5) and wk 8. No biochemical verification. Reduction of smoking was not reported. Effects of mental state were not reported. |
| Notes | Attempts through different means have been made to contact the authors to clarify method of randomisation (it mentions in the report that pts were randomly assigned to the two groups. However, the allocation was uneven: 23 in the experimental group and 42 in the control group). So far, there is no response from the authors. |
Chou 2004.
| Methods | Controlled trial, conducted in Taiwan. Pts were recruited from a day‐care ward in a psychiatric hospital. |
| Participants | 68 pts with diagnosis of schizophrenia. All pts smoked at least 15 CPD for minimum of 1 yr. Pts with history of using NRT within 6 ms before study enrolment and any current use of other smoking cessation treatments were excluded. Interest in quitting smoking was uncertain. No target quit date set. 61 participants were men. Mean age 38.6. Average number of CPD 23. |
| Interventions |
No other addition intervention for all groups. |
| Outcomes | Abstinence was defined as expired CO level <10ppm and measured as self reported continuous prevalence at the end of TNP treatment (i.e. wk 8) and 3‐m follow‐up. Reduction of smoking was measured by expired CO level and FTND score. Measurements were taken at baseline, wkly for first 4 wks, wk 8 and 3‐m follow‐up. Effects on mental state were measured by BRPS and HAS. |
| Notes | Attempts through different means have been made to contact the authors to clarify method of randomisation (it mentions in the report that pts were randomly assigned to the two groups, matched by the CO level. However, the allocation was uneven: 26 in the experimental group and 42 in the control group). So far, there is no response from the authors. |
Characteristics of ongoing studies [ordered by study ID]
Baker(ACTRN1260900103927).
| Trial name or title | Healthy lifestyle intervention for cardiovascular disease risk reduction among smokers with psychotic disorders |
| Methods | RCT. Study is conducted in Australia. |
| Participants | Adult smokers (at least 15 CPD) with a diagnosis of a psychotic disorder or bipolar disorder. All pts take antipsychotic medication as prescribed for at least 2 ms. Exclusion criteria: (1) non‐English speaking; (2) organic brain damage; (3) medical condition that would preclude NRT; (4) actively suicidal or acutely unwell. |
| Interventions |
|
| Outcomes | Continuous and point prevalence of abstinence (confirmed by expired CO level} and self reported number of CPD at wk 15, as well as 12, 18, 24, 30 and 36 ms after initial assessment |
| Starting date | July 2009 |
| Contact information | Amanda Baker (amanda.bake@newcastle.edu.au) |
| Notes | Includes pts with mental illness other than schizophrenia |
Dixon (NCT00960375).
| Trial name or title | Smoking Cessation for Veterans with Severe and Persistent Mental Illness |
| Methods | RCT. Study is conducted at multi‐sites in Washington DC and Maryland, USA. |
| Participants | Adult smokers (at least 10 CPD or FTND score 5 or more) with DSM‐IV diagnosis of severe and persistent mental illness including a diagnosis of a psychotic disorder (schizophrenia, affective psychoses, other psychotic diagnoses and major depression with psychotic features). Exclusion criteria: (1) current alcohol or substance dependence (other than nicotine); (2) documented history of severe neurological disorder or severe head trauma with loss of consciousness; (3) severe or profound mental retardation by chart review. |
| Interventions |
|
| Outcomes | Smoking reduction measured by expired CO level and self reported abstinence from tobacco (abstinence was not defined) |
| Starting date | April 2010 |
| Contact information | Wendy Potts (wendy.potts@va.gov) |
| Notes | Principal Investigator: Lisa Dixon (ldixon@psych.umaryland.edu). Includes pts with mental illness other than schizophrenia |
Evins (NCT00621777).
| Trial name or title | A study of Varenicline for Prevention of Relapse to Smoking in Patients with Schizophrenia or Bipolar disorder (SCRP) |
| Methods | RCT. Study is conducted at multi‐sites in Massachusetts, Michigan, Minnesota and New Hampshire, USA. |
| Participants | Adult smokers (at least 10 CPD and expired CO level > 9ppm) with DSM‐IV diagnosis of schizophrenia, schizoaffective disorder or bipolar disorder. All pts are willing to quit smoking and set a quit date within 2 to 3 wks. Exclusion criteria: (1) diagnosis of dementia, neurodegenerative disease or organic mental disorder; (2) substance use disorder other than nicotine or caffeine in the last 6 ms; (3) major depressive disorder within the last 6 ms; (4) serious unstable medical illness; (5) elevated liver function tests over twice normal; (6) estimated creatinine clearance <40ml/min; (7) use other tobacco products apart from cigarettes (e.g. cigar, pipe); (8) current suicidal or homicidal ideation. |
| Interventions |
Both groups also receive 13‐session wkly CBT programme for smoking cessation. Those pts who have been abstinent for more than 2 wks at the last 4 wks of 12‐wk treatment will enter a 40‐wk relapse prevention programme. They will again be randomised to receive Varenicline or placebo in addition to CBT for relapse prevention. |
| Outcomes | Abstinence is measured by the seven‐day point prevalence abstinence rate at the end of the relapse prevention phase at wk 53. Safety and tolerability of extended duration pharmacotherapy when added to antipsychotic medications in schizophrenia patients who have recently quit smoking is also examined. |
| Starting date | February 2008 |
| Contact information | Gladys N Pachas (gpachas1@partners.org) |
| Notes | Principal Investigator: A. Eden Evins, Massachusetts General Hospital. Includes pts with mental illness other than schizophrenia. |
Fatemi (NCT01111149).
| Trial name or title | Varenicline and Smoking Cessation in Schizophrenia (VSCS) |
| Methods | RCT. Study is conducted in Minnesota, USA. |
| Participants | Adult smokers (at least 10 CPD) with a DSM‐IV diagnosis of schizophrenia or schizoaffective disorder. All pts are motivated to quit smoking and with stabilized psychotic symptoms. Exclusion criteria: (1) serious cardiac, renal, hypertensive, pulmonary, endocrine, or neurological disorder; (2) seizure disorder, recent withdrawal from alcohol or anxiolytics; (3) history of bulimia nervosa, anorexia nervosa, or dementia; (4) history of depression, panic, or bipolar disorders; (5) pregnancy or lactation; (6) prior use of varenicline or bupropion within 3 ms prior to initiation of study; (7) current use of other smoking cessation treatments; (8) regular use of non‐cigarette tobacco products (more than once a wk); (9) history of substance abuse (alcohol or non‐nicotine containing drugs) in the preceding 6 ms; (10) patients with suicidal ideations or plans; (11) florid psychosis or increasing psychosis following varenicline or bupropion treatment; (12) history or current alcohol dependence; (13) current use of monoamine oxidase inhibitor. |
| Interventions |
|
| Outcomes | Abstinence is measured by self report and verified by exhaled CO level and blood/urine tests for nicotine and its metabolites. Smoking reduction is measured by 50% or greater reduction in self reported CPD and a 30% or greater reduction in CO and cotinine levels. Mental state and side effects (including suicidality and abnormal movements) are also measured regularly. |
| Starting date | December 2009 |
| Contact information | S Hossein Fatemi, University of Minnesota |
| Notes |
Josiassen (NCT00231101).
| Trial name or title | Quetiapine Decreases Smoking in Patients With Chronic Schizophrenia |
| Methods | RCT. Study is conducted in Pennsylvania, USA. Both in‐patients and out‐patients are recruited. |
| Participants | Adult smokers (at least one pack of CPD) with DSM‐IV diagnosis of schizophrenia (all subtype including schizoaffective disorder). The participants also show a less‐than‐optimal clinical response to an adequate course of risperidone. Exclusion criteria: (1) treatment refractory schizophrenia (as defined by treatment failure with 3 different antipsychotics of adequate duration in a sufficient dose); (2) significant extra‐pyramidal side effects or akathisia; (3) significant cardiac disease or unstable blood pressure; (4) history of seizures or significant neurological disease; (5) active drug or alcohol addiction in the past 3 ms; (6) pregnancy or breastfeeding; (7) serious suicidal risk. |
| Interventions |
No other additional interventions for both groups. |
| Outcomes | Abstinence is not measured. Smoking reduction is measured by changes of FTND scores, expired CO level and blood levels of cotinine. Mental state is monitored by PANSS, SANS and CGI. |
| Starting date | January 2004 |
| Contact information | Richard C Josiassen (richardjosiassen@noyesfoundation.net) |
| Notes |
Saxon (NCT00508560).
| Trial name or title | Contingency Management for Smoking Cessation Among Veterans With Psychotic Disorders |
| Methods | RCT. Study is conducted in the USA. |
| Participants | Adult smokers (at least 5 or more CPD for at least 16 of the past 30 days prior to study screening) with a diagnosis of schizophrenia or any other psychotic disorder (including bipolar disorder with psychotic features, major depression with psychotic features). All pts indicate willingness to attend smoking cessation group therapy. Exclusion criteria: (1) any current substance dependence disorder except nicotine dependence; (2) imminent risk for suicide or violence; (3) severe psychiatric symptoms or psychosocial instability; (4) gross cognitive impairment. |
| Interventions |
|
| Outcomes | Abstinence is measure by 7 and 30‐day point prevalence and continuous abstinence from quit date. Smoking reduction is measured by change in CPD. |
| Starting date | July 2007 |
| Contact information | Michelle Esterberg (michelle.esterberg@va.gov) |
| Notes | Principal Investigator: Andrew J. Saxon (VA Puget Sound Health Care System). Includes pts with mental illness other than schizophrenia. |
Smith (NCT00802919).
| Trial name or title | Varenicline for Cognitive Deficits and Cigarette Smoking in Schizophrenia ‐ Efficacy and Predictors |
| Methods | RCT. Study is conducted in New York, USA and in Israel. |
| Participants | Adult smokers with diagnosis of schizophrenia or schizoaffective disorder. Participants are taking antipsychotic medication. Exclusion criteria: (1) significant cardiac disease or past history of stroke; (2) history of using varenicline with serious side effects; (3) suicide attempt or serious suicidal ideation in the past yr; (4) pregnant or breastfeeding; (5) significant renal impairment; (6) baseline HDRS score > 20. |
| Interventions |
|
| Outcomes | Abstinence is not measured. Smoking reduction is measured by cotinine level. Mental state is monitored with PANSS and CDSS. |
| Starting date | September 2008 |
| Contact information | Robert C Smith(rsmith@nki.rfmh.org) |
| Notes |
Stockings 2011.
| Trial name or title | A randomised controlled trial linking mental health inpatients to community smoking cessation supports: A study protocol |
| Methods | RCT. Study is conducted in a large regional inpatient mental health facility located in New South Wales, Australia. |
| Participants | Adult smokers (self report of being a current or occasional smoker). All participants are inpatients in a mental health unit. Exclusion criteria: (1) not having a current contact telephone number or address; (2) non‐English speaking; (3) current physical or mental wellbeing is judged by clinical staff to be too unstable to participate. |
| Interventions |
|
| Outcomes | Primary outcome is smoking reduction as measured by CPD at 1 wk, 2 ms, 4 ms and 6 ms post discharge. Secondary outcome is self reported abstinence from smoking (5% of pts who abstain are verified with expired CO level) |
| Starting date | June 2009 |
| Contact information | Jenny Bowman (jenny.bowman@newcastle.edu.au) |
| Notes | ACTRN12609000465257. Includes pts with mental illness other than schizophrenia |
Williams (NCT01010477).
| Trial name or title | Trial of Nicotine Nasal Spray as an Aid for Smoking Cessation in Schizophrenia |
| Methods | RCT. Study is conducted in the USA. |
| Participants | Adult smokers with DSM‐IV diagnosis of schizophrenia. Participants smoke at least 10 CPD and have an expired CO level >9ppm. They are also motivated to quit smoking and on atypical antipsychotic medication for at least 1 m. Exclusion criteria: (1) current suicidal risk; (2) psychiatric hospitalisation in the last 30 days; (3) unable to read or understand questionnaires in English; (4) pregnant or lactating; (5) regular use of non‐cigarette forms of tobacco; (6) Mini‐mental state examination score <22 |
| Interventions |
Both group will also receive behavioural intervention |
| Outcomes | Abstinence is defined as self report of no tobacco use for 4 wks, confirmed by exhaled CO level <10ppm during these period. Abstience will be assessed at wk 5, wk 12, wk 20, wk 26 and wk 52. |
| Starting date | August 2009 |
| Contact information | Mia H Zimmermann (hanosma@umdnj.edu) |
| Notes | Principlal Investigator: Jill M Williams, University of Medicine and Dentistry, New Jersey |
Differences between protocol and review
1. We widened the inclusion criteria in two ways: a) To include patients with schizoaffective disorder, since individuals with this diagnosis share certain core symptoms with patients with schizophrenia. b) To include trials of interventions for other purposes that reported smoking‐related outcomes, if the trials met the study and participant inclusion criteria. Trials which tested an intervention for another primary purpose were reported separately and did not contribute to any meta‐analysis.
2. We changed the primary outcome measure to abstinence from smoking, assessed at least six months from the start of the intervention, to be consistent with other reviews by the Cochrane Tobacco Addiction Group, and the 'Russell Standard'. We reported smoking abstinence at the end of the trial and smoking reduction as secondary outcomes.
Contributions of authors
DTT and ACW conceived and designed the review. DTT conducted the search. DTT, ACW and MP screened retrieved papers. DTT and MP extracted data from the papers, with contribution from ACW to resolve disagreement. DTT entered the data into RevMan 5 and performed data analysis. DTT wrote the review with input from MP and ACW.
Sources of support
Internal sources
Nottinghamshire Healthcare NHS Trust, UK.
Division of Psychiatry, University of Nottingham, UK.
Academic Clinical Psychiatry, University of Sheffield, UK.
School of Public Health, University of Sydney, Australia.
External sources
NHS National Institute for Health Research, UK.
Declarations of interest
None known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
^Horst 2005 {published data only}
- Horst W, Klein MW, Williams D, Werder SF. Extended use of nicotine replacement therapy to maintain smoking cessation in persons with schizophrenia. Neuropsychiatric Disease and Treatment 2005;1(4):349‐55. [PMC free article] [PubMed] [Google Scholar]
*Baker 2006 {published and unpublished data}
- Baker A, Richmond R, Haile M, Lewin TJ, Carr VJ, Taylor RL, et al. A randomized controlled trial of a smoking cessation intervention among people with a psychotic disorder. American Journal of Psychiatry 2006;163:1934‐42. [DOI] [PubMed] [Google Scholar]
- Baker A, Richmond R, Haile M, Lewin TJ, Carr VJ, Taylor RL, et al. Characteristics of smokers with a psychotic disorder and implications for smoking interventions. Psychiatry Research 2007;150:141‐152. [DOI] [PubMed] [Google Scholar]
- Baker A, Richmond R, Lewin TJ, Kay‐Lambkin F. Cigarette smoking and psychosis: naturalistic follow up 4 years after an intervention trial. Australian and New Zealand Journal of Psychiatry 2010; Vol. 44, issue 4:342‐50. [DOI] [PubMed]
- Richmond RL, Baker A, Haile M, Carr V, Lewin T, Wilhelm K, et al. Intervention for tobacco dependence among people with a psychotic illness: RCT with one year outcome. Nicotine & Tobacco Research 2005;7(4):681. [Google Scholar]
*Chen 2012 {published data only}
- Chen H‐K, Lan T‐H, Wu B‐J. A double‐blind randomized clinical trial of different doses of transdermal nicotine patch for smoking reduction and cessation in long‐term hospitalised schizophrenic patients. European Archives of Psychiatry and Clinical Neuroscience 2012;epub:doi: 10.1007/s00406‐012‐0338‐3. [DOI] [PubMed] [Google Scholar]
*Evins 2001 {published and unpublished data}
- Evins A, Cather C, Goff DC, Rigotti NA. Increased smoking cessation and reduction: Two years following a smoking cessation trial in patients with schizophrenia. Conference Abstract of Society for Research on Nicotine and Tobacco 9th Annual Meeting: New Orleans, Louisiana, USA. 2003.
- Evins A, Mays VK, Rigotti NA, Tisdale T, Cather C, Goff DC. A pilot trial of bupropion added to cognitive behavioral therapy for smoking cessation in schizophrenia. Nicotine & Tobacco Research 2001;3(4):397‐403. [DOI] [PubMed] [Google Scholar]
- Evins AE, Cather C, Rigotti NA, Freudenreich O, Henderson DC, Olm‐Shipman CM, et al. Two‐year follow‐up of a smoking cessation trial in patients with schizophrenia: increased rates of smoking cessation and reduction. Journal of Clinical Psychiatry 2004;65(3):307‐11. [DOI] [PubMed] [Google Scholar]
- Evins AE, Mays VK, Rigotti NA, Tisdale T, Daigle A, Goff DC. Reduction In tobacco use in schizophrenia with bupropion SR and Cognitive Behavioral Therapy. Conference abstract of Society for Research on Nicotine and Tobacco 6th Annual Meeting: Arlington, Virginia, USA. 2000.
*Evins 2005 {published and unpublished data}
- Evins A, Cather C, Deckersbach T, Freudenreich O, Culhane MA, Olm‐Shipman CM, et al. A double‐blind placebo‐controlled trial of bupropion Sustained‐Release for smoking cessation in schizophrenia. Journal of Clinical Psychopharmacology 2005;25(3):218‐25. [DOI] [PubMed] [Google Scholar]
- Evins A, Deckersbach T, Cather C, Freudenreich O, Culhane MA, Henderson DC, et al. Independent effects of tobacco abstinence and bupropion on cognitive function in schizophrenia. Journal of Clinical Psychiatry 2005;66(9):1184‐90. [DOI] [PubMed] [Google Scholar]
- Evins AE, Cather C, Culhane M, Freudenreich O, Rigotti NA, Goff DC. Smoking cessation in schizophrenia: A double blind placebo controlled trial of bupropion SR added to cognitive behavioral therapy. Biological Psychiatry 2004;55:226S. [Google Scholar]
- Evins AE, Cather C, Goff DC, Olm‐Shipman C, Rigotti NA. A placebo controlled trial of bupropion SR for smoking cessation in schizophrenia (POS3‐49). Conference abstract of Society for Research on Nicotine and Tobacco 9th Annual Meeting: New Orleans, Louisiana, USA. 2003.
- Evins EA, Goff DC, Shipman CO, Rigotti NA, Cather C. A controlled trial of bupropion SR for smoking cessation in patients with schizophrenia. Conference abstract of 156th Annual Meeting of the American Psychiatric Association: San Francisco, USA. 2003.
*Evins 2007 {published and unpublished data}
- Evins A, Cather C, Culhane MA, Birnbaum A, Horowitz J, Hsieh E, et al. A 12‐week double‐blind, placebo‐controlled study of bupropion SR added to high‐dose dual nicotine replacement therapy for smoking cessation or reduction in schizophrenia. Journal of Clinical Psychopharmacology 2007;27(4):380‐6. [DOI] [PubMed] [Google Scholar]
- Evins AE, Cather C, Culhane M, Birnbaum AS, Horowitz J, Hsieh E, et al. A placebo‐controlled study of bupropion SR added to high dose nicotine replacement therapy for smoking cessation or reduction in schizophrenia (POS2‐104). Conference abstract of Society for Research on Nicotine and Tobacco 12th Annual Meeting: Orlando, Florida, USA. 2006.
*Gallagher 2007 {published and unpublished data}
- Gallagher SM, Penn PE, Schindler E. Smoking cessation in persons with schizophrenia and other serious mental illness (PA1‐5). Conference abstract of Society for Research on Nicotine and Tobacco 12th Annual Meeting: Orlando, Florida, USA. 2006.
- Gallagher SM, Penn PE, Schindler E, Layne W. A comparison of smoking cessation treatments for persons with schizophrenia and other serious mental illnesses. Journal of Psychoactive Drugs 2007;39(4):487‐97. [DOI] [PubMed] [Google Scholar]
*George 2000 {published data only}
- George TP, Hitsman B, Papandonatos GD, Sacco KA, Vessicchio JC, Dudas M, et al. Predictors of smoking cessation in schizophrenia: Analysis of data from three sequential controlled clinical trials. Neuropsychopharmacology 2004;29 Suppl 1:S103. [Google Scholar]
- George TP, Ziedonis DM, Feingold A, Pepper W, Satterburg CA, Winkel J, et al. Nicotine transdermal patch and atypical antipsychotic medications for smoking cessation in schizophrenia. American Journal of Psychiatry 2000;157:1835‐42. [DOI] [PubMed] [Google Scholar]
- Sacco KA, Hitsman B, Papandonatos GD, Vessicchio JC, Dudas MM, Termine A, et al. Predictors of smoking cessation in schizophrenia: analysis of data from three sequential controlled clinical trials (PA5‐3). Conference abstract of the Society for Research on Nicotine and Tobacco 10th Annual Meeting: Phoenix, Arizona, USA. 2004.
*George 2002 {published data only}
- George TP, Hitsman B, Papandonatos GD, Sacco KA, Vessicchio JC, Dudas M, et al. Predictors of smoking cessation in schizophrenia: Analysis of data from three sequential controlled clinical trials. Neuropsychopharmacology 2004;29 Suppl 1:S103. [Google Scholar]
- George TP, Vessicchio JC, Termine A, Bregartner TA, Feingold A, Rounsaville BJ, et al. A placebo controlled trial of bupropion for smoking cessation in schizophrenia. Biological Psychiatry 2002;52(1):53‐61. [DOI] [PubMed] [Google Scholar]
- Sacco KA, Hitsman B, Papandonatos GD, Vessicchio JC, Dudas MM, Termine A, et al. Predictors of smoking cessation in schizophrenia: analysis of data from three sequential controlled clinical trials (PA5‐3). Conference abstract of the Society for Research on Nicotine and Tobacco 10th Annual Meeting: Phoenix, Arizona, USA. 2004.
- Vessicchio JC, Termine A, Bregartner TA, George TP. Bupropion versus placebo for smoking cessation in schizophrenia. Conference abstract of the College on Problems of Drug Dependence 64th Anuual Scientific Meeting: Quebec, Canada. 2002.
*George 2008 {published data only}
- George TP, Hitsman B, Papandonatos GD, Sacco KA, Vessicchio JC, Dudas M, et al. Predictors of smoking cessation in schizophrenia: Analysis of data from three sequential controlled clinical trials. Neuropsychopharmacology 2004;29 Suppl. 1:S103. [Google Scholar]
- George TP, Vessicchio J, Allen T, Weinberger A, Sacco KA. A randomized, double‐blind, placebo‐controlled trial of sustained‐release bupropion combined with transdermal nicotine patch for smoking cessation in schizophrenia: Neuropsychological predictors of treatment outcome. Neuropsychopharmacology 2006;31 Suppl. 1:S254‐5. [Google Scholar]
- George TP, Vessicchio JC, Sacco KA, Weinberger AH, Dudas MM, Allen TM, et al. A placebo‐controlled trial of bupropion combined with nicotine patch for smoking cessation in schizophrenia. Biological Psychiatry 2008;63:1092‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George TP, Vessicchio JC, Weinberger AH, Sacco KA. Sustained‐release bupropion combined with transdermal nicotine patch for smoking cessation in schizophrenia (SYM11C). Conference abstract of the Society for Research on Nicotine and Tobacco 13th Annual Meeting: Austin, Texas, USA. 2007.
- Sacco KA, Hitsman B, Papandonatos GD, Vessicchio JC, Dudas MM, Termine A, et al. Predictors of smoking cessation in schizophrenia: analysis of data from three sequential controlled clinical trials (PA5‐3). Conference abstract of the Society for Research on Nicotine and Tobacco 10th Annual Meeting: Phoenix, Arizona, USA. 2004.
*Li 2009 {published and unpublished data}
- Li Jun, Zhang Tian‐liang, Wang Bin, Li Xian‐wei. An efficacy analysis of bupropion for smoking cessation in schizophrenia. Zhongguo Xinyao yu Linchuang Zazhi 2009;28(3):231‐4. [Google Scholar]
*Weiner 2011 {published data only}
- Weiner E. Comparison of Varenicline and Placebo for Smoking Cessation in Schizophrenia. www.clinicaltrials.gov/ct2/show/NCT00554840 (accessed on 31/03/2010).
- Weiner E, Buchholz A, Coffay A, Liu F, McMahon RP, Buchanan RW, et al. Varenicline for smoking cessation in people with schizophrenia: a double blind randomized pilot study. Schizophrenia Research 2011;129(1):94‐5. [; 6459] [DOI] [PMC free article] [PubMed] [Google Scholar]
*Weiner 2012 {published data only}
- Weiner E, Ball MP, Buchanan R, Gold JM. A comparison of Bupropion SR and Placebo for Smoking Cessation. Conference abstract of the International Congress on Schizophrenia Research: Colorado Springs, Colorado, USA. 2007.
- Weiner E, Ball MP, Buchholz AS, Gold JM, Evins AE, McMahon RP, et al. Bupropion sustained release added to group support for smoking cessation in schizophrenia: a new randomized trial and a meta‐analysis. Journal of Clinical Psychiatry. United States, 2012; Vol. 73, issue 1:95‐102. [] [DOI] [PubMed]
- Weiner E, Buchanan R, Gold J, Ball P, Bennett M. A comparison of bupropion SR and placebo for smoking cessation in schizophrenia. Schizophrenia Research 2003;60:305‐6. [Google Scholar]
*Williams 2007 {published data only}
- Williams JM, Gandhi KK, Foulds J, Steinberg M, Lou S, Masumova F, et al. No advantage for high dose compared to regular dose nicotine patch on short‐term abstinence rates in schizophrenia (PA2‐3). Conference abstract of the Society for Research on Nicotine and Tobacco 13th Annual Meeting: Austin, Texas, USA. 2007.
*Williams 2010 {published data only}
- Steinberg ML, Williams J. Psychosocial Treatments for Individuals with Schizophrenia and Tobacco Dependence. Journal of Dual Diagnosis 2007;3(3/4):99‐112. [Google Scholar]
- Williams JM, Steinberg ML, Zimmermann MH, Gandhi KK, Stipelman B, Budsock PD, et al. Comparison of two intensities of tobacco dependence counselling in schizophrenia and schizoaffective disorder. Journal of Substance Abuse Treatment 2010; Vol. 38, issue 4:384‐93. [] [DOI] [PMC free article] [PubMed]
- Ziedonis D, Williams J, Zimmermann M, Krejci J, Steinbery M, Foulds J, Violette N, Agatep B, Sawh L, Gaffney J. Behavioral Therapy Development for Smokers with Schizophrenia. Conference abstract of the 13th World Conference on Tobacco OR Health: Washington DC, USA. 2006.
*Williams 2012 {published data only}
- Pfizer. Smoking Cessation Study for Patients With Schizophrenia or Schizoaffective Disorder. www.clinicaltrials.gov/ct2/show/NCT00644969 (accessed on 31/03/2010).
- Williams JM, Anthenelli RM, Morris CD, Treadow J, Thompson JR, Yunis C, et al. A randomized, double‐blind, placebo‐controlled study evaluating the safety and efficacy of varenicline for smoking cessation in patients with schizophrenia or schizoaffective disorder. Journal of Clinical Psychiatry. United States, 2012; Vol. 73, issue 5:654‐60. [] [DOI] [PubMed]
*Wing 2012 {published data only}
- George T. rTMS Effects on Smoking Cessation and Cognition in Schizophrenia. www.clinicaltrials.gov/ct2/show/NCT00736710 (accessed on 31/03/2010).
- Wing V C, Bacher I, Daskalakis Z J, George T. A preliminary study of repetitive transcranial magnetic stimulation for smoking cessation in schizophrenia. Neuropsychopharmacology (Conference Proceedings of 49th Annual Conference of the American College of Neuropsychopharmacology, ACNP, 5/12/2010‐9/12/2010 Miami Beach, FL United States). 2010; Vol. 35:S163.
- Wing Victoria C, Bacher Ingrid, Wu Becky S, Daskalakis Zafiris J, George Tony P. High frequency repetitive transcranial magnetic stimulation reduces tobacco craving in schizophrenia. Schizophrenia Research 2012;139(1‐3):264‐6. [DOI] [PubMed] [Google Scholar]
+Akbarpour 2010 {published data only}
- Akbarpour F, Rezaei O, Khodaie‐Ardakani MR, Sheikhvatan M, Goodarzi H, Dolatshahi B. A double‐blind placebo‐controlled trial of bupropion for smoking abstinence and cognition improvement in schizophrenia. Minerva Psichiatrica 2010; Vol. 51, issue 4:263‐9. []
+Bloch 2010 {published data only}
+Dalack 1999 {published and unpublished data}
- Dalack GW, Becks L, Hill E, Pomerleau O, Meador‐Woodruff JH. Nicotine Withdrawal and Replacement in Schizophrenia. Conference abstract from the 150th Annual Meeting of the American Psychiatric Association: San Diego, California, USA. 1997.
- Dalack GW, Becks L, Hill E, Pomerleau O, Meador‐Woodruff JH. The effects of treated and untreated nicotine withdrawal on smokers with schizophrenia. Schizophrenia Research (conference abstract from the 6th International Congress on Schizophrenia Research, Colorado Springs, Colorado, USA). 1997; Vol. 24:63.
- Dalack GW, Becks L, Hill E, Pomerleau OF, Meador‐Woodruff JH. Nicotine withdrawal and psychiatric symptoms in cigarette smokers with schizophrenia. Neuropsychopharmacology 1999;21:195‐202. [DOI] [PubMed] [Google Scholar]
- Dalack GW, Meador‐Woodruff JH. Acute feasibility and safety of a smoking reduction strategy for smokers with schizophrenia. Nicotine & Tobacco Research 1999;1(1):53‐7. [DOI] [PubMed] [Google Scholar]
- Dalack GW, Meador‐Woodruff JH. The Nicotine Patch, Smoking and Schizophrenia. Conference abstract from the 150th Annual Meeting of the American Psychiatric Association: San Diego, California, USA. 1997.
+Fatemi 2005 {published data only}
- Fatemi S, Stary J, Hatsukami D, Murphy S. A double‐blind placebo‐controlled cross over trial of bupropion in smoking reduction in schizophrenia [Letter to the Editor]. Schizophrenia Research 2005;76(2‐3):353‐6. [DOI] [PubMed] [Google Scholar]
+Gelkopf 2012 {published and unpublished data}
- Gelkopf M, Noam S, Rudinski D, Lerner A, Behrbalk P, Bleich A, et al. Nonmedication smoking reduction program for inpatients with chronic schizophrenia: a randomized control design study. Journal of Nervous and Mental Disease. United States: Lippincott Williams and Wilkins (351 West Camden Street, Baltimore MD 21201‐2436, United States), 2012; Vol. 200, issue 2:142‐6. [] [DOI] [PubMed]
+Hartman 1991 {published data only}
- Hartman N, Leong GB, Glynn SM, Wilkins JN, Jarvik ME. Transdermal nicotine and smoking behavior in psychiatric patients. American Journal of Psychiatry 1991;148(3):374‐5. [DOI] [PubMed] [Google Scholar]
+Steinberg 2003 {published and unpublished data}
- Steinberg ML. Engaging smokers with schizophrenia in treatment for tobacco dependence: A brief motivational interviewing intervention. Dissertation Abstracts International: Section B: The Sciences and Engineering 2003; Vol. 64, issue 3‐B:1508.
- Steinberg ML, Ziedonis DM, Krejci JA, Brandon TH. Motivational interviewing with personalized feedback: a brief intervention for motivating smokers with schizophrenia to seek treatment for tobacco dependence. Journal of Consulting & Clinical Psychology 2004;72(4):723‐8. [DOI] [PubMed] [Google Scholar]
+Szombathyne 2010 {published data only}
- Szombathyne‐Meszaros Z, Dimmock J A, Ploutz‐Snyder R, Batki S L. Oral naltrexone treatment for alcohol dependence in schizophrenia is not effective for smoking cessation. Alcoholism: Clinical and Experimental Research 2010;34(6):176A. [Google Scholar]
+Tidey 2011 {published and unpublished data}
- Tidey JW. Contingent Incentives Plus Bupropion for Smoking in People With Schizophrenia. www.clinicaltrials.gov/ct2/show/NCT00136760 (accessed on 31/03/2010).
- Tidey JW, Rohsenow DJ, Kaplan GB, Swift RM, Reid N. Effects of contingency management and bupropion on cigarette smoking in smokers with schizophrenia. Psychopharmacology 2011; Vol. 217, issue 2:279‐87. [] [DOI] [PMC free article] [PubMed]
de Leon 2005b {published and unpublished data}
- Simpson GM, Josiassen RC, Stanilla JK, Leon J, Nair C, Abraham G, et al. Double‐blind study of clozapine dose response in chronic schizophrenia. American Journal of Psychiatry 1999;156:1744‐50. [DOI] [PubMed] [Google Scholar]
- Leon J, Diaz FJ, Josiassen RC, Cooper TB, Simpson GM. Does clozapine decrease smoking?. Progress in Neuro‐Psychopharmacology & Biological Psychiatry 2005;29(5):757‐62. [DOI] [PubMed] [Google Scholar]
Hong 2011 {published data only}
- Hong E. Moderate Dose Varenicline Treatment on Neurobiological and Cognitive Biomarkers in Schizophrenia Smokers and Non‐smokers. Neuropsychopharmacology (Conference proceedings of the 50th Annual Meeting of the American College of Neuropsychopharmacology 4/12/11 to 8/12/11, ACNP Waikoloa, HI United States). 2011; Vol. 36:S97‐S98.
- Hong LE, Thaker GK, McMahon RP, Summerfelt A, RachBeisel J, Fuller RL, Wonodi I, Buchanan RW, Myers C, Heishman SJ, Yang J, Nye Adrienne. Effects of moderate‐dose treatment with varenicline on neurobiological and cognitive biomarkers in smokers and nonsmokers with schizophrenia or schizoaffective disorder. Archives of General Psychiatry 2011;68(12):1195‐1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kelly 2008 {published and unpublished data}
- Buchanan RW, Conley RR, Dickinson D, Ball MP, Feldman S, Gold J, et al. Galantamine for the treatment of cognitive impairments in people with schizophrenia. American Journal of Psychiatry 2008;165:82‐9. [DOI] [PubMed] [Google Scholar]
- Kelly DL, McMahon RP, Weiner E, Boggs DL, Dickinson D, Conley RR, et al. Lack of beneficial galantamine effect for smoking behavior: a double‐blind randomized trial in people with schizophrenia. Schizophrenia Research 2008;103(1‐3):161‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
McEvoy 1995 {published data only}
- McEvoy J, Freudenreich O, McGee M, VanderZwaag C, Levin E, Rose J. Clozapine decreases smoking in patients with chronic schizophrenia. Biological Psychiatry 1995;37(8):550‐2. [DOI] [PubMed] [Google Scholar]
Meszaros 2012 {published and unpublished data}
- Meszaros ZS. Varenicline Treatment in Alcohol and Nicotine Dependent Patients With Schizophrenia. www.clinicaltrials.gov/ct2/show/NCT00727103 (accessed on 31/03/2010).
- Meszaros ZS, Abdul‐Malak Y, Dimmock J A, Wang D, Batki S L. Varenicline treatment of alcohol and nicotine dependence in schizophrenia: Problems encountered in a pilot trial. American Journal on Addictions (Conference Proceedings of 22nd Annual Meeting and Symposium of the American Academy of Addiction Psychiatry, AAAP 8/12/2011‐11/12/2011, Scottsdale, AZ United States). 2012; Vol. 21, issue 4:393‐4.
Sacco 2009 {published data only}
Shim 2012 {published data only}
- Shim J C, Jung D U, Jung S S, Seo Y S, Cho D M, Lee J H, et al. Adjunctive Varenicline Treatment with Antipsychotic Medications for Cognitive Impairments in People with Schizophrenia: A Randomized Double‐Blind Placebo‐Controlled Trial. Neuropsychopharmacology 2012;37(3):660‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shim JC, Jung D, Oh M, Kong B, Ha T, Cho D, et al. Varenicline treatment for smoking cessation in people with schizophrenia: A randomized double‐blind placebo‐controlled trial. Schizophrenia Bulletin. 2011; Vol. 37:320‐1. []
Weinberger 2008 {published and unpublished data}
- Chengappa KNR, Kupfer DJ, Parepally H, John V, Basu R, Buttenfield J, et al. A placebo‐controlled, random‐assignment, parallel‐group pilot study of adjunctive topiramate for patients with schizoaffective disorder, bipolar type. Bipolar Disorder 2007;9(6):609‐17. [DOI] [PubMed] [Google Scholar]
- Weinberger AH, George TP, Perkins KA, Chengappa KNR. Effects of topiramate on smoking in patients with schizoaffective disorder, bipolar type. Journal of Clinical Psychopharmacology 2008;28(2):247‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger AH, George TP, Perkins KA, Chengappa KNR. Effects of topiramate on smoking patients with schizoaffective disorder, bipolar type: Response to Khazaal and Zullino. Journal of Clinical Psychopharmacology 2009;29:193‐194. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Allen 2011 {published data only}
- Allen MH, Debanné M, Lazignac C, Adam E, Dickinson LM, Damsa C. Effect of nicotine replacement therapy on agitation in smokers with schizophrenia: a double‐blind, randomized, placebo‐controlled study. American Journal of Psychiatry 2011;168(4):395‐9. [DOI] [PubMed] [Google Scholar]
- Damsa C, Lazignac C, Adam E, Virgillito S, Allen MH. Effect of nicotine replacement on agitation and aggression in smokers with schizophrenia: a double blind, randomized placebo controlled pilot study. Proceedings of the 162nd Annual Meeting of the American Psychiatric Association; 2009 May 16 21; San Francisco , CA. 2009. [; 30292]
Arbour‐Nicitopoulos 2011a {published data only}
- Arbour‐Nicitopoulos K P, Faulkner G E, Cohn T A, Selby P. Smoking Cessation in Women With Severe Mental Illness: Exploring the Role of Exercise as an Adjunct Treatment. Archives of Psychiatric Nursing 2011;25(1):43‐52. [DOI] [PubMed] [Google Scholar]
Arbour‐Nicitopoulos 2011b {published data only}
- Arbour‐Nicitopoulos K P, Faulkner G E, Hsin A, Selby P. A pilot study examining the acute effects of exercise on cigarette cravings and affect among individuals with serious mental illness. Mental Health and Physical Activity 2011;4(2):89‐94. [Google Scholar]
Aubin 2012 {published data only}
Baker 2010 {published data only}
- Baker Amanda L, Lubman Dan I, Hides Leanne. Smoking and schizophrenia: Treatment approaches within primary care. Primary Psychiatry 2010;17(1):49‐54. [Google Scholar]
Banham 2010 {published data only}
- Banham Lindsay, Gilbody Simon. Smoking cessation in severe mental illness: What works?. Addiction 2010;105(7):1176‐89. [DOI] [PubMed] [Google Scholar]
Brown 2003 {published data only}
- Brown RA, Ramsey SE, Strong DR, Myers MG, Kahler CW, Lejuez CW, et al. Effects of motivational interviewing on smoking cessation in adolescents with psychiatric disorders. Tobacco Control 2003;12 Suppl 4:iv3‐iv10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brunette 2011 {published data only}
- Brunette M F, Ferron J C, McHugo G J, Davis K E, Devitt T S, Wilkness S M, et al. An Electronic Decision Support System to Motivate People With Severe Mental Illnesses to Quit Smoking. Psychiatric Services 2011;62(4):360‐6. [DOI] [PubMed] [Google Scholar]
Bryant 2011 {published data only}
- Bryant J, Bonevski B, Paul C, McElduff P, Attia J. A systematic review and meta‐analysis of the effectiveness of behavioural smoking cessation interventions in selected disadvantaged groups. Addiction 2011;106 (9):1568‐85. [DOI] [PubMed] [Google Scholar]
Dutra 2012 {published data only}
- Dutra SJ, Stoeckel LE, Carlini SV, Pizzagalli DA, Evins AE. Varenicline as a smoking cessation aid in schizophrenia patients: Effects on smoking behavior and reward sensitivity. Biological Psychiatry 2011; Vol. 69, issue 9 SUPPL. 1:280S. [] [DOI] [PMC free article] [PubMed]
- Dutra Sunny J, Stoeckel Luke E, Carlini Sara V, Pizzagalli Diego A, Evins AE, Dutra SJ, et al. Varenicline as a smoking cessation aid in schizophrenia: Effects on smoking behavior and reward sensitivity. Psychopharmacology 2012; Vol. 219, issue 1:25‐34. [] [DOI] [PMC free article] [PubMed]
Kisely 2006 {published data only}
- Kisely SR, Preston NJ. A Group Intervention which assists patients with dual diagnosis reduce their tobacco use. In: Abelian ME editor(s). Trends in psychotherapy research. Hauppauge, NY: Nova Science Publishers, 2006:141‐59. [Google Scholar]
McClure 2010 {published data only}
- McClure J B, Swan G E, Catz S L, Jack L, Javitz H, McAfee T, et al. Smoking outcome by psychiatric history after behavioral and varenicline treatment. Journal of Substance Abuse Treatment 2010;38(4):394‐402. [DOI] [PMC free article] [PubMed] [Google Scholar]
McEvoy 1999 {published data only}
- McEvoy JP, Freudenreich O, Wilson WH. Smoking and therapeutic response to clozapine in patients with schizophrenia. Biological Psychiatry 1999;46:125‐9. [DOI] [PubMed] [Google Scholar]
McKee 2009 {published data only}
- McKee SA, Weinberger AH, Harrison ELR, Coppola S, George TP. Effects of the nicotinic receptor antagonist mecamylamine on ad‐lib smoking behaviour, topography, and nicotine levels in smokers with and without schizophrenia: a preliminary study. Schizophrenia Research 2009;115:317‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morris 2011 {published data only}
- Morris C D, Waxmonsky J A, May M G, Tinkelman D G, Dickinson M, Giese A A, et al. Smoking reduction for persons with mental illnesses: 6‐month results from community‐based interventions. Community Mental Health Journal 2011;47(6):694‐702. [DOI] [PubMed] [Google Scholar]
Pachas 2012 {published data only}
- Pachas G N, Cather C, Pratt S I, Hoeppner B, Nino J, Carlini S V, et al. Varenicline for Smoking Cessation in Schizophrenia: Safety and Effectiveness in a 12‐Week Open‐Label Trial. Journal of Dual Diagnosis 2012;8(2):117‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roll 1998 {published data only}
- Roll JM, Higgins ST, Steingard S, McGinley M. Use of monetary reinforcement to reduce the cigarette smoking of persons with schizophrenia: a feasibility study. Experimental & Clinical Psychopharmacology 1998;6(2):157‐61. [DOI] [PubMed] [Google Scholar]
Shiina 2010 {published data only}
- Shiina A, Shirayama Y, Niitsu T, Hashimoto T, Yoshida T, Hasegawa T, et al. A randomised, double‐blind, placebo‐controlled trial of tropisetron in patients with schizophrenia. Annals of General Psychiatry 2010;9:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tidey 2002 {published data only}
- Tidey JW, O'Neill SC, Higgins ST. Contingent monetary reinforcement of smoking reductions, with and without transdermal nicotine, in outpatients with schizophrenia. Experimental & Clinical Psychopharmacology 2002;10(3):241‐7. [DOI] [PubMed] [Google Scholar]
Tidey 2012 {published data only}
- Tidey JW, Rohsenow DJ, Kaplan GB, Swift RM, Ahnallen CG. Separate and Combined Effects of Very Low Nicotine Cigarettes and Nicotine. Nicotine & Tobacco Research 2012; Vol. epub. [] [DOI] [PMC free article] [PubMed]
Weiner 2001 {published data only}
- Weiner E, Ball MP, Summerfelt A, Gold J, Buchanan RW. Effects of sustained‐release bupropion and supportive group therapy on cigarette consumption in patients with schizophrenia. American Journal of Psychiatry 2001;158(4):635‐7. [DOI] [PubMed] [Google Scholar]
Wells 2003 {published data only}
- Wells ME. Increasing motivation to stop smoking among persons with schizophrenia and other chronic mental illnesses. Dissertation Abstracts International: Section B: The Sciences and Engineering 2003; Vol. 63, issue 8‐B.
References to studies awaiting assessment
Chen 2002 {published data only}
- Chen R, Ku C, Chou K, Shen C. The impact of smoking cessation programs on schizophrenic patients' smoking behaviors [abstract]. American Journal of Respiratory and Critical Care Medicine 2002;165(8 Suppl):A309. [Google Scholar]
- Chen R, Ku C‐H, Lu R‐B, Chou K‐R. The impact of smoking cessation programs on smoking‐related health belief and rate of quit‐smoking among schizophrenic patients. Journal of Medical Sciences 2002;22(5):215‐20. [Google Scholar]
Chou 2004 {published data only}
- Chou KR, Chen R, Lee JF, Ku CH, Lu RB. The effectiveness of nicotine‐patch therapy for smoking cessation in patients with schizophrenia. International Journal of Nursing Studies 2004;41(3):321‐30. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Baker(ACTRN1260900103927) {published data only}
- Baker A. Healthy lifestyle intervention for cardiovascular disease risk reduction among smokers with psychotic disorders. www.anzctr.org.au/trial_view.aspx?ID=308232 (accessed on 11/4/2010).
- Baker A L, Kay‐Lambkin F J, Richmond R, Filia S, Castle D, Williams J, et al. Healthy lifestyle intervention for people with severe mental disorders. Mental Health and Substance Use: Dual Diagnosis 2010;4 (2):144‐57. [Google Scholar]
- Baker A, Kay‐Lambkin FJ, Richmond R, Filia S, Castle D, Williams J, et al. Study protocol: a randomised controlled trial investigating the effect of a healthy lifestyle intervention for people with severe mental disorders. BMC Public Health 2011; Vol. 11, issue 1:10. [DOI] [PMC free article] [PubMed]
- Filia S, Baker A, Richmond R, Kay‐Lambkin F, Castle D, Williams J, et al. Randomised controlled trial of a healthy lifestyles intervention to reduce cardiovascular disease (CVD) risk among smokers with psychosis: Interim results. Australian and New Zealand Journal of Psychiatry 2010;44:A31‐A32. [] [Google Scholar]
Dixon (NCT00960375) {published data only}
- Dixon L B, Potts W. Smoking cessation for veterans with severe and persistent mental illness. www.clinicaltrials.gov/ct2/show/NCT00960375 (accessed on 20/7/12).
Evins (NCT00621777) {published data only}
- Evins AE. A study of Varenicline for Prevention of Relapse to Smoking in Patients with Schizophrenia or Bipolar Disorder (SCRP). www.clinicaltrials.gov/ct2/show/NCT00621777 (accessed on 12/11/2012).
Fatemi (NCT01111149) {published data only}
- Fatemi SH. Varenicline and smoking cessation in schizophrenia (VSCS). http://www.clinicaltrials.gov/ct2/show/NCT01111149 (accessed on 20/7/12).
Josiassen (NCT00231101) {published data only}
- Josiassen RJ. Quetiapine Decreases Smoking in Patients With Chronic Schizophrenia. www.clinicaltrials.gov/ct2/show/NCT00231101 (accessed on 31/03/2010).
Saxon (NCT00508560) {published data only}
- Saxon AJ. Contingency Management for Smoking Cessation Among Veterans With Psychotic Disorders. www.clinicaltrials.gov/ct2/show/NCT00508560 (accessed on 12/11/2012).
Smith (NCT00802919) {published data only}
- Smith RC. Varenicline for Cognitive Deficits and Cigarette Smoking in Schizophrenia ‐ Efficacy and Predictors. www.clinicaltrials.gov/ct2/show/NCT00802919 (accessed on 12/11/2012).
Stockings 2011 {published data only}
- The effect of an integrated smoking care program on the reduction and abstinence of smoking in mental health inpatients following discharge from hospital. http://www.anzctr.org.au/trial_view.aspx?ID=83938 (accessed on 16/11/2012).
- Stockings EA, Bowman JA, Wiggers J, Baker AL, Terry M, Clancy R, et al. A randomised controlled trial linking mental health inpatients to community smoking cessation supports: a study protocol. BMC Public Health 2011;11:570. [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams (NCT01010477) {published data only}
- Trial of Nicotine Nasal Spray as an Aid for Smoking Cessation in Schizophrenia. http://www.clinicaltrials.gov/ct2/show/NCT01010477 (accessed on 12/11/2012).
Additional references
Adler 1998
- Adler LE, Olincy A, Waldo M, Harris JG, Griffith J, Stevens K, et al. Schizophrenia, sensory gating, and nicotinic receptors. Schizophrenia Bulletin 1998;24(2):189‐202. [DOI] [PubMed] [Google Scholar]
American Psychiatric Association 1994
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorder. 4th Edition. Washington, DC: American Psychiatric Association, 1994. [Google Scholar]
Amiaz 2009
- Amiaz R, Levy D, Vainiger D, Grunhaus L, Zangen A. Repeated high‐frequency transcranial magnetic stimulation over the dorsolateral prefrontal cortex reduces cigarette craving and consumption. Addiction 2009;104(4):653‐660. [DOI] [PubMed] [Google Scholar]
Brown 2000
- Brown S, Inskip H, Barraclough B. Causes of the excess mortality of schizophrenia. British Journal of Psychiatry 2000;177:212‐7. [DOI] [PubMed] [Google Scholar]
Buchanan 2009
- Buchanan RW, Kreyenbuhl J, Kelly DL, Noel JM, Boggs DL, Fischer BA, et al. The 2009 Schizophrenia PORT Psychopharmacological Treatment Recommendations and Summary Statements. Schizophrenia Bulletin 2010;36(1):71‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cahill 2011
- Cahill K, Perera R. Competitions and incentives for smoking cessation. Cochrane Database of Systematic Reviews 2011, Issue 4. [DOI: 10.1002/14651858.CD004307.pub4] [DOI] [PubMed] [Google Scholar]
Cahill 2012
- Cahill K, Stead LF, Lancaster T. Nicotine receptor partial agonists for smoking cessation. Cochrane Database of Systematic Reviews 2012, Issue 4. [DOI: 10.1002/14651858.CD006103.pub6] [DOI] [PubMed] [Google Scholar]
Cerimele 2012
- Cerimele JM, Durango A. Does Varenicline Worsen Psychiatric Symptoms in Patients With Schizophrenia or Schizoaffective Disorder? A Review of Published Studies. Journal of Clinical Psychiatry 2012;73(8):e1039‐1047. [DOI] [PubMed] [Google Scholar]
Cuervo 2003
- Cuervo LG, Clarke M. Balancing benefits and harms in health care. British Medical Journal 2003;327(7406):65‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Culhane 2008
- Culhane MA, Schoenfeld DA, Barr RS, Cather C, Deckersbach T, Freudenreich O, et al. Predictors of early abstinence in smokers with schizophrenia. Journal of Clinical Psychiatry 2008;69(11):1743‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
de Leon 2005a
- Leon J, Diaz FJ. A meta‐analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophrenia Research 2005;76(2/3):135‐57. [DOI] [PubMed] [Google Scholar]
Desai 2001
- Desai HD, Seabolt J, Jann MW. Smoking in patients receiving psychotropic medications: A pharmacokinetic perspective. CNS Drugs 2001;15(6):469‐94. [DOI] [PubMed] [Google Scholar]
Dixon 1999
- Dixon L. Dual diagnosis of substance abuse in schizophrenia: prevalence and impact on outcomes. Schizophrenia Research 1999;35 Suppl:S93‐S100. [DOI] [PubMed] [Google Scholar]
Dixon 2009
- Dixon L, Perkins D, Calmes C. Guideline Watch (September 2009): Practice Guideline for the Treatment of Patients with Schizophrenia. American Psychiatric Publishing, 2009. [Google Scholar]
Eichhammer 2003
- Eichhammer P, Johann M, Kharraz A, Binder H, Pittrow D, Wodarz N, Hajak G. High‐frequency repetitive transcranial magnetic stimulation decreases cigarette smoking. Journal of Clinical Psychiatry 2003;64(8):951‐953. [DOI] [PubMed] [Google Scholar]
Ereshefsky 1985
- Ereshefsky L, Jann MW, Saklad SR, Davis CM, Richards AL, Burch NR. Effects of smoking on fluphenazine clearance in psychiatric inpatients. Biological Psychiatry 1985;20:329‐332. [DOI] [PubMed] [Google Scholar]
FDA 2008
- US Food, Drug Administration. Public Health Advisory: Important Information on Chantix (varenicline). http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/PublicHealthAdvisories/ucm051136.htm (accessed on 30/11/12).
FDA 2011
- US Food, Drug Administration. [FDA drug safety communication: safety review update of Chantix (varenicline) and risk of neuropsychiatric adverse events.]. http://www.fda.gov/Drugs/DrugSafety/ucm276737.htm (accessed 30/11/2012) October 2011.
Fiore 2008
- Fiore M, Jaén C, Baker T, Bailey W, Benowitz NL, Curry S, et al. Treating tobacco use and dependence: 2008 Update ‐ Clinical Practice Guideline. United States Department of Health and Human Services, 2008. [Google Scholar]
Freedman 2007
- Freedman R. Exacerbation of schizophrenia by varenicline. American Journal of Psychiatry 2007;164:1269. [DOI] [PubMed] [Google Scholar]
GlaxoSmithKline 2008
- Prescribing Information (Wellbutrin XL ‐ bupropion hydrochloride extended‐release tablets). http://us.gsk.com/products/assets/us_wellbutrinXL.pdf 2008.
Goff 1992
- Goff DC, Henderson DC, Amico E. Cigarette smoking in schizophrenia: Relaitonship to psychopathology and medication side effects. American Journal of Psychiatry 1992;149(9):1189‐94. [DOI] [PubMed] [Google Scholar]
Gunnell 2009
- Gunnell D, Irvine D, Wise L, Davies C, Martin RM. Varenicline and suicidal behaviour: a cohort study based on data from the General Practice Research Database. British Medical Journal 2009;339:b3805. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gustafson 1992
- Gustafson R. Operant conditioning of activities of daily living on a psychogeriatric ward: A simple method. Psychological Reports 1992;70:603‐7. [DOI] [PubMed] [Google Scholar]
Harrison‐Woolrych 2011
- Harrison‐Woolrych M, Ashton J. Psychiatric adverse events associated with varenicline: an intensive postmarketing prospective cohort study in New Zealand. Drug Safety 2011;34(9):763‐772. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. British Medical Journal 2003;7414:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011 [Computer program]
- Higgins JPT, Green S [eds]. Cochrane Handbook for Systematic Reviews of Interventions,5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011.
Hughes 2005
- Hughes JR, Carpenter MJ. The feasibility of smoking reduction: an update. Addiction 2005;100:1074‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hughes 2006
- Hughes JR, Carpenter MJ. Does smoking reduction increase future cessation and decrease disease risk? A qualitative review. Nicotine & Tobacco Research 2006;8(6):739‐49. [DOI] [PubMed] [Google Scholar]
Hughes 2007
- Hughes JR, Stead LF, Lancaster T. Antidepressants for smoking cessation. Cochrane Database of Systematic Reviews 2007, Issue 1. [DOI: 10.1002/14651858.CD000031.pub3] [DOI] [PubMed] [Google Scholar]
Johnson 2005
- Johnson BA. Recent advances in the development of treatments for alcohol and cocaine dependence: focus on topiramate and other modulators of GABA or glutamate function. CNS Drugs 2005;19:873‐896. [DOI] [PubMed] [Google Scholar]
Kasliwal 2009
- Kasliwal R, Wilton LV, Shakir SA. Safety and drug utilization profile of varenicline as used in general practice in England: interim results from a prescription‐event monitoring study. Drug Safety 2009;32(6):499‐507. [DOI] [PubMed] [Google Scholar]
Kelly 1999
- Kelly C, McCreadie RG. Smoking habits, current symptoms, and premorbid characteristics of schizophrenic patients in Nithsdale, Scotland. American Journal of Psychiatry 1999;156(11):1751‐7. [DOI] [PubMed] [Google Scholar]
Kelly 2011
- Kelly DL, McMahon RP, Wehring HJ, Liu F, Mackowick KM, Boggs DL, Warren KR, Feldman S, Shim J‐C, Love RC, Dixon L. Cigarette Smoking and Mortality Risk in People with Schizophrenia. Schizophrenia Bulletin 2011;37(4):832‐838. [DOI: 10.1093/schbul/sbp152] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kelly 2012
- Kelly DL, Raley HG, Lo S, Wright K, Liu F, McMahon RP, Moolchan ET, Feldman S, Richardson CM, Wehring HJ, Heishman SJ. Perception of Smoking Risks and Motivatin to Quit Among Nontreatment‐Seeking Smokers With and Without Schizophrenia. Schizophrenia Bulletin 2012;38(3):543‐551. [DOI: 10.1093/schbul/sbq124] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kreyenbuhl 2009
- Kreyenbuhl J, Buchanan RW, Dickerson FB, Dixon LB. The Schizophrenia Patient Outcomes Research Team (PORT): Updated Treatment Recommendations 2009. Schizophrenia Bulletin 2010;36(1):94‐103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kumari 2002
- Kumari V, Sharma T. Effects of typical and atypical antipsychotics on prepulse inhibition in schizophrenia: A critical evaluation of current evidence and directions for future research. Psychopharmacology 2002;162(2):97‐101. [DOI] [PubMed] [Google Scholar]
Lai 2010
- Lai DTC, Cahill K, Qin Y, Tang J‐L. Motivational interviewing for smoking cessation. Cochrane Database of Systematic Reviews 2010, Issue 1 10.1002/14651858.CD006936.pub2. [DOI: 10.1002/14651858.CD006936.pub2] [DOI] [PubMed] [Google Scholar]
Lancaster 2005a
- Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD001292.pub2] [DOI] [PubMed] [Google Scholar]
Lancaster 2005b
- Lancaster T, Stead LF. Self‐help interventions for smoking cessation. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD001118.pub2] [DOI] [PubMed] [Google Scholar]
Lawn 2005
- Lawn S, Pols R. Smoking bans in psychiatric inpatient settings? A review of the research. The Australian & New Zealand Journal of Psychiatry 2005;39(10):866‐85. [DOI] [PubMed] [Google Scholar]
Lichtermann 2001
- Lichtermann D, Ekelund J, Pukkala E, Tanskanen A, Lonnqvist J. Incidence of cancer among persons with schizophrenia and their relatives. Archives of General Psychiatry 2001;58(6):573‐8. [DOI] [PubMed] [Google Scholar]
Liu 2009
- Liu ME, Tsai SJ, Yang ST. Varenicline‐induced mixed mood and psychotic episode in a patient with Schizoaffective Disorder. CNS Spectrum 2009;14:346. [DOI] [PubMed] [Google Scholar]
McEvoy 1995a
- McEvoy JP, Freudenreich O, Levin ED, Rose JE. Haloperidol increases smoking inpatients with schizophrenia. Psychopharmacology 1995;119(1):124‐126. [DOI] [PubMed] [Google Scholar]
Moore 2011
- Moore TJ, Furberg CD, Glenmullen J, Maltsberger JT, Singh S. Suicidal behaviour and depression in smoking cessation treatments. PLoS ONE 2011;6(11):e27016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moss 2009
- Moss TG, Sacco KA, Allen TM, Weinberger AH, Vessicchio JC, George TP. Prefrontal cognitive dysfunction is associated with tobacco dependence treatment failure in smokers with schizophrenia. Drug and Alcohol Dependence 2009;104(1‐2):94‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Olincy 1997
- Olincy A, Young DA, Freedman R. Increased levels of the nicotine metabolite cotinine in schizophrenic smokers compared to other smokers. Biological Psychiatry 1997;42(1):1‐5. [DOI] [PubMed] [Google Scholar]
Sacco 2004
- Sacco KA, Bannon KL, George TP. Nicotinic receptor mechanisms and cognition in normal states and neuropsychiatric disorders. Journal of Psychopharmacology 2004;18(4):457‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shadel 2000
- Shadel WG, Shiffman S, Niaura R, Nichter M, Abrams DB. Current models of nicotine dependence: What is known and what is needed to advance understanding of tobacco etiology among youth. Drug and Alcohol Dependence 2000;59 Suppl 1:S9‐22. [DOI] [PubMed] [Google Scholar]
Shmueli 2008
- Shmueli D, Fletcher L, Hall SE, Hall SM, Prochaska JJ. Changes in psychiatric patients' thoughts about quitting smoking during a smoke‐free hospitalization. Nicotine & Tobacco Research 2008;10(5):875‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stead 2005
- Stead LF, Lancaster T. Group behaviour therapy programmes for smoking cessation. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD001007.pub2] [DOI] [PubMed] [Google Scholar]
Stead 2006
- Stead LF, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD002850.pub2] [DOI] [PubMed] [Google Scholar]
Stead 2008
- Stead LF, Bergson G, Lancaster T. Physician advice for smoking cessation. Cochrane Database of Systematic Reviews 2008, Issue 2. [DOI: 10.1002/14651858.CD000165.pub3] [DOI] [PubMed] [Google Scholar]
Stead 2012
- Stead LF, Lancaster T. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database of Systematic Reviews 2012, Issue 10. [DOI: 10.1002/14651858.CD008286.pub2] [DOI] [PubMed] [Google Scholar]
Stead 2012b
- Stead LF, Perera R, Bullen C, Mant D, Hartmann‐Boyce J, Cahill K, Lancaster T. Nicotine replacement therapy for smoking cessation. Cochrane Database of Systematic Reviews 2012, Issue 11. [DOI: 10.1002/14651858.CD000146.pub4] [DOI] [PubMed] [Google Scholar]
Steinberg 2004
- Steinberg ML, Williams JM, Ziedonis DM. Financial implications of cigarette smoking among individuals with schizophrenia. Tobacco Control 2004;13(2):206. [PMC free article] [PubMed] [Google Scholar]
Strasser 2001
- Strasser K. Smoking Reduction and Cessation for People with Schizophrenia: Guidelines for General Practitioners. Smoking Reduction and Cessation for People with Schizophrenia:Guidelines for General Practitioners. SANE Australia & Department of Psychiatry, University of Melbourne, 2001. [Google Scholar]
Tunis 2003
- Tunis SR, Stryer DB, Clancy CM. Practical clinical trials: increasing the value of clinical research for decision making in clinical and health policy. Journal of American Medical Association 2003;290(12):1624‐32. [DOI] [PubMed] [Google Scholar]
US Department of Health and Human Services 2000
- US Department of Health and Human Services. Reducing Tobacco Use. A Report of the US Surgeon General. Atlanta, GA: Office of Smoking and Health, 2000. [Google Scholar]
West 2005
- West R, Hajek P, Stead L, Stapleton J. Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction 2005;100(3):299‐303. [DOI] [PubMed] [Google Scholar]
Williams 2005
- Williams JM, Ziedonis DM, Abanyie F, Steinberg ML, Foulds J, Benowitz NL. Increased nicotine and cotinine levels in smokers with schizophrenia and schizoaffective disorder is not a metabolic effect. Schizophrenia Research 2005;79(2‐3):323‐35. [DOI] [PubMed] [Google Scholar]
Williams 2006
- Williams JM, Ziedonis DM. Snuffing out tobacco dependence. Ten reasons behavioral health providers need to be involved. Behavioral Healthcare 2006;26(5):27‐31. [PubMed] [Google Scholar]
Workgroup on Substance Use Disorders 2006
- Workgroup on Substance Use Disorders, American Psychiatric Association Steering Committee on Practice Guidelines. Practice Guideline for the Treatment of Patients With Substance Use Disorders. 2nd Edition. American Psychiatric Association, 2006. [Google Scholar]
World Health Organization 2003
- World Health Organization. International Classification of Diseases. 10th Edition. WHO, 2003. [Google Scholar]
Wye 2009
- Wye PM, Bowman JA, Wiggers JH, Baker A, Knight J, Carr VJ, et al. Smoking restrictions and treatment for smoking: policies and procedures in psychiatric inpatient units in Australia. Psychiatric Service 2009;60(1):100‐7. [DOI] [PubMed] [Google Scholar]
Ziedonis 1994
- Ziedonis D, Kosten TR, Glazer WM, Frances RJ. Nicotine dependence and schizophrenia. Hospital and Community Psychiatry 1994;45(3):204‐6. [DOI] [PubMed] [Google Scholar]
Ziedonis 2007
- Ziedonis D, Parks J, Zimmermann MH, McCabe P. Program and System Level Interventions to Address Tobacco Amongst Individuals with Schizophrenia. Journal of Dual Diagnosis 2007;3(3/4):151‐175. [Google Scholar]
Zwar 2007
- Zwar N, Richmond R, Borland R, Peters M, Stilman S, Litt J, et al. Smoking cessation pharmacotherapy: an update for health professionals. Royal Australian College of General Practitioners, 2007. [Google Scholar]
References to other published versions of this review
Tsoi 2010
- Tsoi DT, Porwal M, Webster AC. Efficacy and safety of bupropion for smoking cessation and reduction in schizophrenia: systematic review and meta‐analysis. British Journal of Psychiatry 2010;196:346‐353. [DOI] [PubMed] [Google Scholar]


