Abstract
Background
Type 2 diabetes is a common and costly chronic disease which is associated with significant premature mortality and morbidity. Although patient education is an integral component of diabetes care, there remain uncertainties regarding the effectiveness of different methods and modes of education.
Objectives
To evaluate the effectiveness of individual patient education on metabolic control, diabetes knowledge and psychosocial outcomes.
Search methods
Multiple electronic bibliographic databases were searched, including The Cochrane Library, MEDLINE, Premedline, ERIC, Biosis, AMED, Psychinfo, EMBASE, CINAHL, APAIS‐health, Australian Medical Index, Web of Science, dissertation abstracts and Biomed Central.
Selection criteria
Randomized controlled and controlled clinical trials which evaluated individual education for adults with type 2 diabetes. The intervention was individual face‐to‐face patient education while control individuals received usual care, routine treatment or group education. Only studies that assessed outcome measures at least six months from baseline were included.
Data collection and analysis
Information was extracted by two reviewers who summarized both study characteristics and outcome statistics. A meta‐analysis using a fixed‐effect model was performed if there were adequate studies with a specified outcome of sufficient homogeneity. For outcomes where there were too few studies or the assessment measurements were not standardized or variable, the results were summarised qualitatively.
Main results
Nine studies involving 1359 participants met the inclusion criteria. Six studies compared individual education to usual care and three compared individual education to group education (361 participants). There were no long‐term studies and overall the quality of the studies was not high. In the six studies comparing individual face‐to‐face education to usual care, individual education did not significantly improve glycaemic control (weighted mean difference (WMD) in HbA1c ‐0.1% (95% confidence interval (CI) ‐0.3 to 0.1, P = 0.33) over a 12 to 18 month period. However, there did appear to be a significant benefit of individual education on glycaemic control in a subgroup analysis of three studies involving participants with a higher mean baseline HbA1c greater than 8% (WMD ‐0.3% (95% CI ‐0.5 to ‐0.1, P = 0.007). In the two studies comparing individual to group education, there was no significant difference in glycaemic control between individual or group education at 12 to 18 months with a WMD in HbA1c of 0.03% (95% CI ‐0.02 to 0.1, P = 0.22). There was no significant difference in the impact of individual versus usual care or group education on body mass index systolic or diastolic blood pressure. There were too few studies to perform a meta‐analysis on the effect of individual education on dietary self management, diabetes knowledge, psychosocial outcomes and smoking habits. No data were available on the other main outcome measures of diabetes complications or health service utilization and cost analysis in these studies.
Authors' conclusions
This systematic review suggests a benefit of individual education on glycaemic control when compared with usual care in a subgroup of those with a baseline HbA1c greater than 8%. However, overall there did not appear to be a significant difference between individual education and usual care. In the small number of studies comparing group and individual education, there was an equal impact on HbA1c at 12 to 18 months. Additional studies are needed to delineate these findings further.
Plain language summary
Individual patient education for people with type 2 diabetes mellitus
Nine studies involving 1359 participants met the inclusion criteria. Six studies compared individual education to usual care and three compared individual education to group education (361 participants). There were no long‐term studies and overall the quality of the studies was not high. Individual face‐to‐face patient education for type 2 diabetes over a six to twelve month period did not significantly improve glycaemic control, body mass index (BMI ‐ measure of overweight; body weight in kilogram divided through squared height in meters, kg/m2), blood pressure or total cholesterol in the short or medium term compared with usual care. However, there did appear to be a significant benefit of individual education on glycaemic control in a subgroup analysis of studies involving participants with a higher baseline HbA1c greater than 8% (that is, too high blood sugar levels over a couple of months or inadequate 'metabolic control'). In the studies comparing individual education to group education, there was no significant difference between individual or group education at 12 to 18 months nor a significant difference in the impact of individual education versus group education on BMI, systolic or diastolic blood pressure.
An exact analysis on dietary self management, diabetes knowledge, psychosocial outcomes and smoking habits could not be performed because there were limited studies and varied measurement tools. However, descriptive evaluation suggested that there was no significant difference in quality of life, self management skills or knowledge between group and individual education. When comparing individual patient education to usual care, the limited number of studies available suggested a positive outcome on self management, smoking and knowledge, however there was conflicting evidence surrounding psychosocial outcomes. No data were available on the other main outcome measures of diabetes complications or health service utilization and cost analysis in these studies.
Background
Description of the condition
Diabetes mellitus is a disorder in the metabolism of blood glucose. It occurs when the body no longer responds effectively to endogenous insulin or when the body's production of insulin is inadequate. This leads to chronic hyperglycaemia (elevated levels of plasma glucose) accompanied by abnormal metabolism of carbohydrate, fat and protein. In the long term, people with diabetes are predisposed to complications which include retinopathy, nephropathy and neuropathy. The risk of cardiovascular disease is also substantially increased. For a detailed overview of diabetes mellitus, please see under 'Additional information' in the information on the Metabolic and Endocrine Disorders Group in The Cochrane Library (see 'About', 'Cochrane Review Group (CRGs)'). For an explanation of methodological terms, see the main glossary in The Cochrane Library.
Type 2 diabetes is one the commonest chronic diseases globally and is closely entwined with the obesity epidemic. The International Diabetes Federation reported an estimate of 194 million people with diabetes in 2003 and predicted that this will increase to 333 million in 2025 (Diabetes Atlas 2005) and similar projections have been made by the World Health Organization (Wild 2004). Most of the increase in diabetes prevalence is predicted to occur in the developing countries where by 2025 more than 75% of the people with diabetes under the age of 65 will reside (King 1998). Hence, in addition to the direct disease costs, diabetes will place an enormous additional burden on these countries through productivity losses. The financial cost of diabetes is immense and increasing. The national costs of diabetes for 2002 in the US is estimated at US$ 92 billion to US$ 132 billion (approx. 72 to 103 billion EUROS) in direct medical expenditure and US$ 40 billion (approx. 31 billion EUROS) for indirect costs and is estimated to increase to US $192 billion (approx. 150 billion EUROS) in 2020 (ADA 2003). Complications are the main driver of all types of diabetes costs increasing the annual cost of diabetes in Australia from US$ 3220 (2523 EUROS) in people without complications to US$ 7715 (6044 EUROS) for people with both microvascular and macrovascular complications. European studies, ie CODE‐2 (Jonsson 2002) and the UK T2ARDIS study (Holmes 2003) showed similar effects with quality of life glycaemic average scores also significantly reduced by complications.
Description of the intervention
These findings demonstrate the high financial burden associated with diabetes and its complications that may, a least in part, be attributable to deficiencies in self management. Education that increases patients' understanding of diabetes can prevent or delay complications and reduce the number and duration of hospitalisations, which in turn can improve quality of life glycaemic. Different methods of teaching people self‐management practices may affect long‐term compliance, relative to many other conditions, the impact of self‐management on diabetes outcomes is important not only to the individual but to the community in the form of health care costs (Glasgow 1999). In the USA it has been found that medical non‐compliance in people with type 2 diabetes imposes a financial burden in the order of 100 billion dollars (approx. 78 billion EUROS) each year (Vermeire 2003). Consequently, patient education is recognized globally as an essential component of diabetes management but its relationship to health outcomes and health service utilization is still not well understood (Corabian 2001; Ellis 2004; Loveman 2008) and reports of its effectiveness are variable (Loveman 2008). Nonetheless, due to the onerous requirements for self‐care that demands multiple daily decisions in order to balance diet, physical activity and medications, it is widely accepted that diabetes education is not only required in the first few months following diagnosis but is an important component of ongoing diabetes care (Loveman 2003). The question, then, is not so much about whether or not people with diabetes should have diabetes education but about which methods and models of education produce the best effect on behaviour change, self management, and physical and psychological outcomes.
An important Health Technology Assessment on patient education for type 2 diabetes by Corabian and Harstall (Corabian 2001) points out that a particular difficulty in assessing educational interventions is the lack of well defined long‐term outcomes, and this is supported by Loveman et al (Loveman 2008). However, since then the American Association of diabetes educators has published criteria for behaviour change as a result of education (AADE 2003) and Australia has developed a national consensus on outcomes and indicators for diabetes patient education (Eigenmann 2007). Patient empowerment, as championed by Funnell 2004 has been gathering popularity as an educational model since the 1980s and has been shown to produce benefits such as improved communication with providers, greater satisfaction with care, improvements in metabolic and psychological outcomes and quality of life. More recent education models such as Diabetes X‐PERT (Deakin 2006) and DESMOND (Davies 2008) are representative of current efforts to better define, structure and evaluate the effect of diabetes education. However, these reports, like the majority of research reports in the peer reviewed literature about diabetes patient education focus on group education. A systematic review by Norris and colleagues (Norris 2001) found evidence that self management training in people with type 2 diabetes was effective. Despite inclusions of some studies assessing individual patient education, the majority of studies included in the review focused on group education. A Cochrane Review by Deakin and colleagues (Deakin 2005) also concluded that adults with type 2 diabetes improved diabetes control and knowledge of diabetes after group‐based training programmes.
Why it is important to do this review
Individual education is a common form of patient education for people with diabetes but, to date, there has been no formal review of the effects of individual patient education on outcomes in people with type 2 diabetes. The availability of this information is critical to informing service and resource allocation decisions relating to individual patient education.
Objectives
To evaluate the effects of individual face‐to‐face patient education.
Methods
Criteria for considering studies for this review
Types of studies
Only randomised controlled trials and controlled clinical trials were included.
Types of participants
Participants were adults diagnosed with type 2 diabetes over the age of 18 years. To be consistent with changes in classification and diagnostic criteria of the disease through the years, the diagnosis should have been established using the standard criteria valid at the time of beginning the study. These diagnostic criteria included those described by the World Health Organisation (WHO 1980; WHO 1985; WHO 1998) and the American Diabetes Association Standards (ADA 1999). The review excluded interventions specific for maturity onset diabetes of the young (MODY) or women with gestational diabetes.
Types of interventions
This review only included studies where individual patient education formed the major component of the intervention. If the study included both individual and group education then it was included only if the individual component was a systematic programme designed for individual education. Studies were restricted to those that reported outcomes at six months from baseline or later.
Individual patient education that met the following criteria:
was specific for people with type 2 diabetes;
was face‐to‐face (not telephone‐ or computer‐based);
education addressed a wide range of self‐management issues and was not limited to particular aspects such as weight management, physical activity or foot care;
aimed to impact on clinical outcomes and/or health service utilisation and costs.
The intervention group was compared with those who received:
group education;
no specific intervention;
usual care (receiving the standard care such as regular follow up with the health provider).
Types of outcome measures
Primary outcomes
metabolic control, measured by glycated haemoglobin A1c (HbA1c);
diabetes complications (eg retinopathy, nephropathy, neuropathy, lower limb amputation, cardiovascular disease);
health service utilisation and health care costs (admission and readmission rates, average length of stay, visits to the general practitioner and the emergency department).
Secondary outcomes
psychosocial outcomes (quality of life, psychological problems such as depression);
diabetes knowledge;
patient self‐care behaviours (dietary habits, physical activity levels) or self management skills (medication administration, use of equipment);
physical measures (body mass index (BMI, kg/m2), weight (kg), blood pressure (systolic and diastolic (mmHg));
metabolic (lipids ‐ total cholesterol (mmol/L), HDL cholesterol (mmol/L), LDL cholesterol (mmol/L), triglycerides (mmol/L)).
Timing of outcome measurement
Outcomes were assessed in the short (6 to 9 months), the medium term (12 to 18 months) and longer term (greater than 18 months).
Search methods for identification of studies
Electronic searches
The following electronic databases were searched from the date on which records began up until April 2007: The Cochrane Library, MEDLINE, Premedline, ERIC, Biosis, AMED, Psychinfo, EMBASE, CINAHL, APAIS‐health, Australian Medical Index, Web of Science, dissertation abstracts and Biomed Central. Studies published in any language were included.
The MEDLINE search strategy can be viewed in Appendix 1. The other databases were searched with a similar strategy adjusted for the particular database.
Data collection and analysis
Selection of studies
Following removal of obviously irrelevant studies, reviews or duplicates by a single reviewer (SD), two independent reviewers (SD, RC) scanned the title and abstract and keywords of every record and retrieved the full text for further assessment when the reference suggested that the study may fit the inclusion criteria. The full text of these studies was analysed and identified as included or excluded independently by three reviewers (SD, RC, SC) based on the above inclusion criteria. Any differences of opinion were discussed and an agreement reached through consensus. In one case the authors were contacted to assist in clarification. Only original published studies were considered.
Data extraction and management
Information was extracted from each reference into a template developed by the authors and presented under Characteristics of included studies. The following information was extracted:
1. Methods: location, method of recruitment including clinical setting, inclusion, exclusion criteria, allocation, blinding, permission, power analysis, intention‐to‐treat. 2. Participants: baseline data, sample size, attrition rate, baseline HbA1c and duration of diabetes. 3. Intervention: description of education given to intervention participants and control participants. 4. Outcome: variables and their measures. 5. Allocation concealment: one of four categories.
Assessment of risk of bias in included studies
Each study was assessed individually for methodological quality and analyzed particularly for potential sources of bias by two reviewers (SD, SC). The following factors were assessed: a) Minimization of selection bias ‐ was there adequate randomization and allocation concealment? b) Minimization of attrition bias ‐ were withdrawals and dropouts completely described and was analysis by intention‐to‐treat? c) Minimization of Detection bias ‐ were outcome assessors blind to the interventions?
The trials were then summarized into three categories as described in Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2005).
A Low risk of bias where all the criteria were met B Moderate risk of bias were one or more criteria were partly met C High risk of bias where one or more criteria were not met
Assessment of heterogeneity
Variation between studies (heterogeneity) was investigated using the I2‐statistic, which describes the percentage of total variation across studies that is due to heterogeneity rather than chance. It allows for calculation and comparison across studies of varying sizes, study types and with varying outcome data (Higgins 2003).
When outcome measurements were not significantly homogeneous for meta‐analysis (such as use of non standardized questionnaires or variable measurement tools) or if there were inadequate number of studies, then they were summarized in a qualitative manner.
Data synthesis
Data were summarized statistically only if there were adequate numbers of studies with sufficient homogeneity and quality. For continuous variables, analysis was based on mean change from baseline and using the weighted mean difference. When standard deviations were not presented they were derived from standard errors, confidence intervals or probability values when available. A meta‐analysis using a fixed‐effect model was performed if there were adequate studies with sufficient homogeneity.
Subgroup analysis and investigation of heterogeneity
Where data were available, subgroup analyses were performed on the effects of individual education and the influences of gender, ethnic background, baseline HbA1c, duration of diabetes and contact time.
Sensitivity analysis
We planned to perform sensitivity analyses in order to explore the influence of the following factors on effect size:
repeating the analysis excluding unpublished studies;
repeating the analysis taking account of study quality, as specified above;
repeating the analysis excluding any very long or large studies to establish how much they dominate the results;
repeating the analysis excluding studies using the following filters: diagnostic criteria, language of publication, source of funding (industry versus other), country.
The robustness of the results was also planned to be tested by repeating the analysis using different measures of effects size (risk difference, odds ratio etc.) and different statistical models (fixed‐ and random‐effects models).
Results
Description of studies
Results of the search
The electronic databases cited above were searched from the date on which records began up until April 2007. Search strategies were designed to capture references that observed any effect of individual patient education as one of the interventions. From the initial search 8235 citations were identified from the following databases, The Cochrane Library (351), MEDLINE (1781), Premedline (203), ERIC (24), Biosis (379), AMED (20), Psychinfo (92), EMBASE (3317), CINAHL (703), APAIS‐health (20), Australian Medical Index (306), Web of science (511), Dissertation abstracts (440) and Biomed central (88). These references were scanned by one reviewer and 7883 were removed because they were obviously irrelevant studies, reviews or duplicates. The search resulted in a total of 352 identified potentially relevant references. The abstracts were studied in detail and full references when necessary by two independent reviewers. Abstracts were required to be translated in four Chinese papers and three Spanish papers. Nine studies completely fulfilled the inclusion criteria ( (see Figure 1 for details of the amended QUOROM (quality of reporting of meta‐analyses) flow‐chart of study selection, Moher 1999). There was consensus among the three reviewers. All publications were in English except for one which was in Spanish (Dalmau 2003) for which data were extracted from translated information.
1.
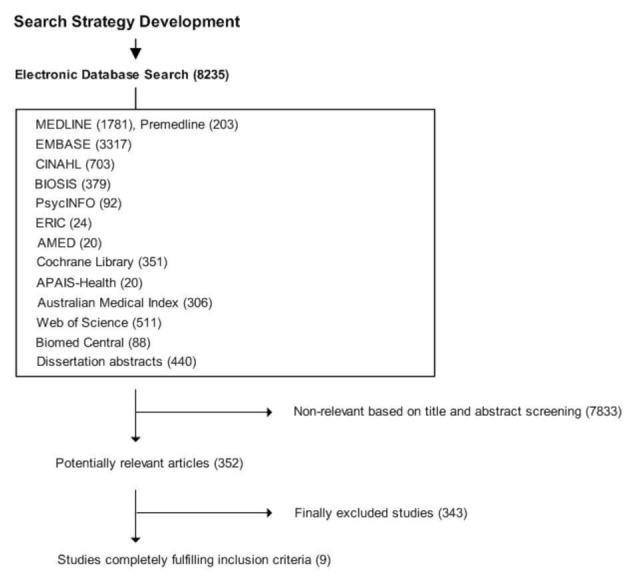
Amended QUOROM (quality of reporting of meta‐analyses) flow‐chart of study selection
The main reasons for exclusion were (see details of excluded studies for further information):
the trial focused on group education or contained components of group education;
was not a randomised or controlled clinical trial;
education was not face‐to‐face;
the study focused on patient participation or case management rather than education;
education was for a specific issue such as foot care, weight loss or physical activity.
Included studies
A total of nine studies met the inclusion criteria. Six compared individual education to usual care (Goudswaard 2004; Hawthorne 1997; Hiss 2001; Ko 2004; Shibayama 2007; Whittemore 2004) and three compared individual education to group education (Campbell 1996; Dalmau 2003; Rickheim 2002). There were no long‐term studies. Three trials were carried out in the United States, one in Australia, one in Spain, one in the Netherlands, one in Japan, one in Hong Kong and one in the United Kingdom. The included studies appeared in the following publications, with frequency shown in brackets.
Atencion Primaria (1)
British Journal of General Practice (1)
Diabetes Care (2)
Diabetes Educator (2)
Diabetes Research and Clinical Practice (1)
Diabetic Medicine (2)
Study Design
All included studies were randomized controlled studies.
Participants
The included studies involved 1359 participants. The smallest study had 53 participants (Whittemore 2004) and the largest study had 376 participants (Hiss 2001). All trials except one (Whittemore 2004) recruited both men and women. The mean age of the participants was between 52 to 65 years. One study focused on education in a migrant population with a low level of literacy (Hawthorne 1997). The duration of diabetes prior to the study was quite variable, with three studies reporting a duration of greater than seven years (Goudswaard 2004; Hiss 2001; Shibayama 2007), four studies where the duration of diabetes was less than three years (Campbell 1996; Dalmau 2003, Rickheim 2002; Whittemore 2004) and two studies where it was not stated (Hawthorne 1997; Ko 2004). The HbA1c level at the commencement of the study was also quite variable ranging from 6.6% to 12.2%. See Characteristics of included studies for further information.
Interventions
The criteria for inclusion demanded that the majority of the intervention involved face‐to‐face education and covered a wide range of diabetes related topics. The content of the education typically covered pathophysiology of diabetes, diabetes control through diet, diabetes control through exercise, compliance with medication, exercise and exercise regimes, glucose self‐monitoring, diabetic complications, foot care, services available, motivation and behavioural strategies. The total face‐to‐face time varied considerably as did the frequency of the sessions and the number of months it was carried over. Most studies involved 2 to 4 hours of face‐to‐face time (Goudswaard 2004 (2.5 hrs), Hiss 2001 (4 hrs), Ko 2004 (2.5 hrs), Shibayama 2007 (3 hrs), Whittemore 2004 (approx. 3 hrs). Two studies contained less 2 hours or less of contact time (Dalmau 2003 (2 hours), Hawthorne 1997 (20 min sessions) and two studies involved greater than five hours of contact time (Campbell 1996 (approx. 7 hrs), Rickheim 2002 (5 to 7 hrs). The majority of the interventions were carried out by diabetes educators and dieticians. One study (Hawthorne 1997) trained a link worker, who had no previous medical background, to carry out the education.
Outcome measures
Only a limited number of outcomes were assessed in these nine studies. The main outcomes common to most studies were glycaemic control and basic physical measures. The studies were too short to assess complications and a cost effectiveness analysis was not covered by any of the studies.
Primary outcomes
metabolic control, measured by glycated haemoglobin A1c (HbA1c): all studies assessed HbA1c;
diabetes complications: none assessed this outcome;
health service utilisation and health care costs: none assessed this outcome.
Secondary outcomes
psychosocial outcomes: Campbell 1996; Rickheim 2002; Shibayama 2007; Whittemore 2004,
diabetes knowledge: Campbell 1996; Hawthorne 1997; Rickheim 2002;
patient self‐care behaviours or self management skills : Whittemore 2004; Rickheim 2002;
physical measures (body mass index or blood pressure): Campbell 1996; Dalmau 2003; Hiss 2001; Ko 2004; Rickheim 2002; Shibayama 2007; Whittemore 2004;
metabolic (lipids): Campbell 1996; Dalmau 2003; Hiss 2001; Ko 2004; Shibayama 2007.
Risk of bias in included studies
Blinding
In this type of intervention blinding of participants is not possible. Blinding of physicians was reported in Ko 2004 and Shibayama 2007.
Incomplete outcome data
Loss to follow‐up was quite variable with some studies suffering significant loss to follow‐up. These included Campbell 1996 (64% loss to follow‐up at 12 months) and Rickheim 2002 (46% loss to follow‐up at six months). Those with minimal loss to follow‐up included Ko 2004 (1% loss to follow‐up) and Hawthorne 1997 (5% loss to follow‐up at six months). The other studies had reasonable follow‐up; Dalmau 2003 (14% loss to follow‐up at 12 months), Goudswaard 2004 (14% loss to follow‐up 18 months), Hiss 2001 (16% loss to follow‐up at 12 months), Shibayama 2007 (10% loss to follow‐up at 12 months) and Whittemore 2004 (8% loss to follow‐up at six months).
Other potential sources of bias
Four studies presented a power calculation to detect a difference in HbA1c between the intervention groups (Goudswaard 2004; Hawthorne 1997; Ko 2004 and Shibayama 2007).
Effects of interventions
Data analysis
Mean change from baseline was compared in the short term (6 to 9 months) and medium term (12 to 18 months). No long‐term studies fitted the inclusion criteria. The analysis was divided to compare individual to usual care (Goudswaard 2004; Hawthorne 1997; Hiss 2001; Ko 2004; Shibayama 2007; Whittemore 2004) and individual education to group education (Dalmau 2003; Campbell 1996; Rickheim 2002).
There were four interventions (minimal, extensive group, extensive individual and behavioural) in the study of Campbell 1996. However, as the minimal group was only a six month evaluation it was decided to restrict the analysis to individual versus group education.
When standard deviations were not presented they were derived from standard errors, confidence intervals or probability values when available. These conversion methods to obtain standard deviations of the change from baseline are described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2005).
In some studies, the standard deviation of the change from baseline was unavailable (Goudswaard 2004; Hawthorne 1997; Ko 2004). It was therefore necessary to calculate this using the baseline and final standard deviations with an estimation of the correlation coefficient. There were inadequate data to estimate this from the available studies and therefore an imputed correlation coefficient value of 0.75 was thought to be a reasonable estimate for most outcome variables. A separate analysis using a correlation coefficient of 0.25 was also applied to the analysis of HbA1c as a more conservative estimation of this variable.
Heterogeneity
A χ2‐test for heterogeneity was performed for each outcome using the I2‐statistic and is reported below. The majority of the analyses showed non‐substantial heterogeneity (less than 50%).
Glycated haemoglobin A1c (HbA1c)
All nine studies assessed HbA1c, five studies reported data for 6 to 9 months and seven studies reported 12 to 18 month data.
Individual education versus usual care
Three studies involving 295 participants assessed HbA1c at 6 to 9 months (Goudswaard 2004; Hawthorne 1997; Whittemore 2004). The weighted mean difference (WMD) in HbA1c at 6 to 9 months was ‐0.2% with a trend to favour individual patient education, however this did not reach significance (95% confidence interval (CI) ‐0.5 to 0.03, P = 0.08). Heterogeneity was low (I2 = 15.6%).
Four studies involving 632 participants assessed HbA1c at 12 to 18 months (Goudswaard 2004; Hiss 2001; Ko 2004; Shibayama 2007). There was relatively low heterogeneity (I2 = 30.7%). There was no significant difference in improvement in HbA1c following patient education with the WMD in HbA1c: ‐0.1% (95% CI ‐0.3 to 0.1, P = 0.33).
Changing the correlation coefficient to r = 0.25 did not substantially change the outcome. The WMD in HbA1c at 6 to 9 months was ‐0.3% (95% CI ‐0.7 to 0.2) and 12 to 18 months ‐0.1% (95% CI ‐0.3 to 0.1).
Individual education versus group education
Only two studies looked at individual education versus group education at 6 to 9 months (Campbell 1996; Rickheim 2002) with a total of 148 participants and two studies looked at 12 to 18 months (Campbell 1996; Dalmau 2003) involving 112 participants. At 6 to 9 months HbA1c was reduced by a significantly greater amount from baseline with group education versus individual education with a WMD of 0.8% (95% CI 0.3 to 1.3, P = 0.0007), however there was no significant difference between the interventions at 12 to 18 months with a WMD of 0.03% (95% CI ‐0.02 to 0.1, P = 0.22). There was no heterogeneity between these studies (I2 = 0%).
Using the correlation coefficient of r = 0.25 did not substantially change the outcome with the WMD at 6 to 9 months of 0.8% (95% CI 0.2 to 1.5).
Body mass index (BMI)
Only some studies looked at body mass index (BMI).
Individual education versus usual care
There was only one study which looked at BMI at 6 to 9 months and this study only involved women (Whittemore 2004). Therefore, the analysis focused on 12 months where two studies were available (Ko 2004; Shibayama 2007) involving 312 participants. There was no significant decrease in BMI at 12 to 18 months with a WMD of ‐0.2 BMI units (95% CI ‐1.0 to 0.6, P = 0.62).
Individual education versus group education
Campbell 1996 and Rickheim 2002 contained data on BMI available at 6 to 9 months involving 169 participants and Campbell 1996 and Dalmau 2003 had data at 12 to 18 months involving 123 participants. There was no significant heterogeneity at 6 to 9 months (I2 = 0%) or at 12 to 18 months (I2 = 22.9%). There was no significant difference between individual and group education in reduction in BMI at 6 to 9 months (WMD of ‐0.1 BMI units (95% CI of ‐0.9 to 0.7, P = 0.77) or at 12 to 18 months (‐0.01 BMI units with a 95% CI of ‐0.8 to 0.7, P = 0.98).
Blood Pressure
Individual education versus usual care
Data were available for systolic and diastolic blood pressure at 12 to 18 months for three studies (Hiss 2001; Ko 2004; Shibayama 2007) with 625 and 624 participants, respectively.
Individual education had no significant effect on systolic blood pressure with a WMD of ‐2 mm Hg (95% CI ‐5 to 1, P = 0.19). There was no significant heterogeneity between the studies (I2 = 3.0%).
There was a trend favouring individual education for reduction in diastolic blood pressure with a WMD of ‐2 mm Hg (95% CI ‐3 to 0.00, P = 0.05). There was moderate heterogeneity (I2= 48.4%) between the studies.
Individual education versus group education
Two studies measured systolic and diastolic blood pressure at 12 to 18 months (Campbell 1996; Dalmau 2003). There was no heterogeneity between the studies (I2 = 0%) and no significant difference between individual and group education on reduction in systolic (WMD 4 mm Hg; 95% CI ‐4 to 12, P = 0.33) or diastolic blood pressure (WMD 2 mm Hg; 95% CI ‐4 to 7, P = 0.59).
Cholesterol
Again, only a few studies assessed cholesterol and often measured different subsets such as HDL‐cholesterol or triglycerides. Only total cholesterol had an adequate number of studies at 12 to 18 months and only in the individual education versus usual care analysis.
Individual education versus usual care
Three studies assessed total cholesterol at 12 to 18 months (Hiss 2001; Ko 2004; Shibayama 2007) and involved 627 participants. There was low heterogeneity between the studies (I2 = 25.2%). Individual patient education had no significant effect on total cholesterol compared with usual care with a WMD of ‐0.03 mmol/L (95% CI ‐0.2 to 0.10, P = 0.66).
Individual education versus group education
Only one study (Campbell 1996) assessed total cholesterol which demonstrated no significant difference between individual education and group education in change in total cholesterol over 3, 6 or 12 months.
Smoking
Only two studies reported smoking rates; one comparing individual to usual care (Ko 2004) and the other comparing individual to group education (Dalmau 2003). The study by Ko 2004 had only a small number of smokers in each group and the percentages of smokers were significantly different between the two groups at baseline. There was a significant reduction in the number of participants who quit or reduced the amount of smoking in those receiving individual education versus usual care (16.7% versus 5.7%, P = 0.031). In the Dalmau 2003 study, group education just failed to reach significance in favouring smoking cessation over individual education ( P = 0.05). Again, there were substantial differences in the number of smokers between the groups at baseline (12% in the group with individual education versus 31% of those receiving group education).
Diabetes Knowledge
Only three studies looked at knowledge (Campbell 1996; Hawthorne 1997 and Rickheim 2002) and because they all used different questionnaires to assess knowledge, involved different intervention groups and were of different duration, a meta‐analysis was not performed.
Individual education versus usual care
Hawthorne 1997 found individual education significantly improved all knowledge subsets at six months. For example at six months, 78% of the study group could name one complication of diabetes compared with 18% at the start of the study and there was no significant change in the control group. There was no longer term follow‐up.
Individual education versus group education
Rickheim 2002 used a 14 point knowledge score to assess knowledge at baseline and six months. Both the group and individual intervention groups had significant improvements in knowledge compared to baseline, however there was no significant difference between individual and group education in knowledge scores (P = 0.15). Campbell 1996 used a 15 item diabetes knowledge scale. There was a significant difference between the groups at 6 months (P = 0.000) favouring group education but no significance between group and individual education at 12 months.
Quality of life and psychosocial adjustment
SF‐36 is a global health‐related quality of life instrument measuring quality of life both in both physical and mental components. Shibayama 2007 used a Japanese version of SF‐36 and a Problem Areas in Diabetes Scale (PAID) to assess quality of life and diabetes‐related distress. Whittemore 2004 used the standard PAID survey to assess diabetes‐related distress and the Diabetes Questionnaire (TDQ) to assess how well diabetes was integrated into daily life. Rickheim 2002 included an adjustment to diabetes instrument (ATT19) which measures psychosocial adjustment and attitudes towards diabetes in addition to the SF‐36 scale.
Individual education versus usual care
In the Whittemore 2004 study, women who participated in the individual intervention demonstrated significantly better psychosocial adaptation at six months with less distress (P < 0.01) and better integration (P < 0.03) than women under usual care. In the Shibayama 2007 study there was no significant change in distress scores (PAID scores) or quality of life scores as measured by the Japanese version of SF‐36 over a 12 month period.
Individual education versus group education
In the Rickheim 2002 study there were significant improvements in adjustment as measured by the ATT‐19 survey and quality of life on the SF‐36 mental scale in both individual and group interventions after six months. There was no significant difference between individual and group education.
Self management outcomes
Only two studies looked at some aspect of self management. In the Whittemore 2004 study, women who participated in the individual intervention demonstrated significantly better diet self‐management (P = 0.02) with a trend towards better exercise self‐management (P = 0.13). Rickheim 2002 assessed self‐reported exercise frequency and duration and behavioural goal achievement. There was no significant difference in percent of behavioural goals achieved between the group and individual education groups (P = 0.49) and no affect on self reported physical activity after six months within each group (intervention, P = 0.38; control group P = 0.39) or between the two groups (P = 0.83).
Cost effectiveness
No study carried out a cost effectiveness analysis.
Subgroup analysis
There were inadequate data to perform a subgroup analysis on ethnic background or gender.
Level of baseline HbA1c
An analysis of individual versus usual care in studies where the mean HbA1c at baseline was greater than 8% (Goudswaard 2004; Ko 2004 and Hawthorne 1997), demonstrated that individual education was significantly better at improving HbA1c than usual care with a weighted mean difference of ‐0.3% (95% CI ‐0.5 to ‐0.1, P = 0.007).
Discussion
There were only nine studies that met the fairly strict inclusion criteria and only four that compared individual education to usual care. Many studies were excluded from the review because the intervention involved a combination of group and individual education, the education was not face‐to‐face or it focused on a specific area. The included studies were generally of poor quality with the majority having a high risk of bias. The main shortcomings were the small numbers, high drop out rates, inadequate allocation concealment and lack of intention‐to‐treat analysis.
Individual education versus usual care
Interestingly, individual education when compared to usual care did not have a significant impact on glycaemic control as reflected by glycated haemoglobin A1c (HbA1c) at 6 to 9 months or 12 to 18 months. There are perhaps a number of factors which contributed to this which should be assessed in future studies. Firstly, the face‐to‐face time was fairly limited in most studies with an average of 2 to 4 hours over a six month period. The longest in this group being Hiss 2001 with an average of four hours face‐to‐face time. Secondly, the majority of the intervention was within the first three months (except Shibayama 2007) and in a number of studies there was indeed some evidence of benefit earlier on which however faded over time (Goudswaard 2004; Whittemore 2004). In the meta‐analysis, there was a trend to favour individual patient education at 6 to 9 months, with a weighted mean difference of ‐0.2%, however this did not reach significance (95% CI ‐0.5 to 0.03, P = 0.08). Further studies need to assess whether an intervention over a longer period of time would be more effective. Thirdly, the impact may have been diluted because in some studies there did not appear to be a great difference in the intervention between the individual education and usual care groups. For example, in the study by Shibayama 2007, both groups received monthly reviews by a diabetologist which may explain why the intervention of 25 minutes monthly did not have a substantial impact. Fourthly, the impact may have been diluted by including a high number of participants who had a near normal HbA1c at baseline. In a subgroup analysis focused on studies where participants had an average baseline HbA1c of greater than 8% there was a significant impact of individual education on glycaemic control (P =0.007).
There did not appear to be a significant impact of individual education on body mass index, blood pressure or total cholesterol. However, again there were small numbers and the above considerations should also be applied. Although there were very limited data available, there was a suggestion of benefit of individual education on dietary self management, diabetes knowledge and smoking habits. There was conflicting evidence surrounding psychosocial outcomes with Whittemore 2004 demonstrating a significant improvement in quality of life and adaptation scores at six months in women, in contrast to the study by Shibayama 2007 which showed no evidence of impact on quality of life scores.
Individual versus group education
There were only three studies which compared individual education to group education. Studies which focused on group education were excluded when the control group did not have a structured approach to individual education. Overall the quality of the studies was poor with small numbers and high drop‐out rates (Campbell 1996; Rickheim 2002). In addition, there was a significant difference in the amount of patient contact time. For example, in Campbell 1996, those receiving group education at 12 months had received an average of 21 hours contact time compared to participants who received individual education who received an average of only seven hours contact time. This must be taken into consideration when making conclusions from these studies.
Group education appeared to have a greater impact on glycaemic control than individual education at 6 to 9 months with a weighted mean difference of HbA1c of 0.8% (95% CI 0.3 to 1.3, P = 0.0007), however there was no significant difference between the interventions at 12 to 18 months with a weighted mean difference of 0.03% (95% CI ‐0.02 to 0.1, P = 0.22).
There was no significant difference between the impact of individual education and group education on body mass index, systolic or diastolic blood pressure with both groups having an improvement from baseline during the study.
There was a suggestion in the Dalmau 2003 study that group education may be favoured over individual education for smoking cessation, however this just failed to reach significance ( P = 0.05), and only one study examined this outcome. Diabetes knowledge improved significantly in both group and individual education intervention groups and there was no significant difference between them at six months (Rickheim 2002) or 12 months (Campbell 1996).
There was no significant difference between the effects of individual and group education on quality of life measures as both appeared to have a benefit as measured by the ATT‐19 survey and quality of life on the SF‐36 mental scale (Rickheim 2002). In the same study there was no significant affect on self reported physical activity after six months within each group.
These findings reflect the difficulties of educational research ‐ including the lack of clear definition and documentation of the precise nature, extent and scope of interventions, and the lack of agreed predetermined goal and outcomes of education.
Authors' conclusions
Implications for practice.
This systematic review highlights the benefits of individual education in lowering glycated haemoglobin A1c (HbA1c) in a subgroup of patients with poorer control and a mean baseline HbA1c greater than 8%. There did not appear to be a significant impact of individual education on body mass indexI, blood pressure or total cholesterol, at 12 to 18 months follow‐up. However, in view of the small number of studies and their considerable limitations, further research is needed before any firm conclusions can be made.
There were even smaller number of studies (three) comparing individual face‐to‐face education to group education. Both individual and group education had an equal impact on HbA1c improvement at 12 to 18 months. There were only two studies that looked at other physical measures such as body mass index and blood pressure at 12 to 18 months. There was no significant difference between the impact of individual education and group education on body mass index, systolic or diastolic blood pressure with both groups having an improvement from baseline during the study.
There is no clear evidence in the current literature to assist in recommending either individual or group education over the other. Further high quality research on the effectiveness of different methods and delivery modes of education is urgently needed to guide resource allocation and service configuration for diabetes education programmes.
Implications for research.
As outlined in the discussion, there were considerable limitations in the number and quality of the studies available for this review. Critical assessment of the impact of individual diabetes patient education requires further research based on rigorous methods in high quality studies ‐ including well designed RCTs comparing individual diabetes patient education with group education. Studies with larger numbers, longer duration and well defined, clearly documented interventions are vital to answering the question posed by this review. In particular, more explicitly defined differences between study and control groups in relation to time and duration of face‐to‐face education would reduce the dilutional effects of the intervention.
The participants in the majority of studies on diabetes patient education are recruited from among patients attending hospital based specialist diabetes centres or clinics where multidisciplinary or team care following internationally recommended standards of diabetes care is practised. It is reasonable to assume that this patient population is likely to be in better metabolic control than their counterparts in the community who do not attend such services. The significant benefit of individual education on glycaemic control in a subgroup analysis of three studies involving participants with a higher mean baseline HbA1c greater than 8% may suggest that one of the difficulties in demonstrating benefits of education on clinical parameters of diabetes control relates to the fact that patients recruited to studies of diabetes education are already in reasonable metabolic control. This potential effect requires further exploration.
What's new
| Date | Event | Description |
|---|---|---|
| 7 August 2008 | Amended | Converted to new review format. |
Notes
Conversion from US$ to EUROS was based on 31st Oktober 2008 rates.
Acknowledgements
Cochrane Renal Group Westmead for advice and support. Massimo Porta, MD, PhD, Marina Trento B. ED. SCI. for further clarification of their research groups. Susan Goodall for assistance with study design and protocol development. The contribution of Dr Siva S. Sivarajasingam is also acknowledged.
Appendices
Appendix 1. Search strategy
| Search terms |
| Unless otherwise stated, search terms are free text terms; MeSH = Medical subject heading (Medline medical index term); exp = exploded MeSH; the dollar sign ($) stands for any character(s); the question mark (?) = to substitute for one or no characters; tw = text word; pt = publication type; sh = MeSH; adj = adjacent. 1. exp Education/ 2. exp Health Education/ 3. exp Health Promotion/ 4. exp Learning/ 5. exp Counseling/ 6. exp Health Behavior/ 7. exp Community health services/ 8. or/1‐7 9. (individual$ or one‐on‐one or one‐to‐one or standard care).tw. 10. (self$ adj6 (care or efficac$ or manag$ or monitor$)).tw. 11. exp Patients/ 12. or/9‐11 13. 8 and 12 14. exp Patient Education/ 15. ((patient$ or adult$ or client$ or participant$ or individual$) adj3 (train$ or educat$ or teach$ or instruct$ or inform or counsel$ or empower$)).tw. 16. 14 or 15 17. 13 or 16 18. exp Diabetes Mellitus, Type 2/ 19. exp Insulin Resistance/ 20. glucose intoleranc$.tw. 21. impaired glucose toleranc$.tw. 22. insulin$ resistanc$.tw. 23. (exp Obesity/ or obes$.tw.) and (Diabetes mellitus/ or diabete$.tw.) 24. (obes$ adj diabet$).tw. 25. dm2.tw. 26. NIDDM.tw. 27. (non insulin$ depend$ or noninsulin$ depend$ or noninsulin?depend$ or non insulin?depend$).tw. 28. ((typ$ 2 or typ$II or typ$ ii) adj diabet$).tw. 29. ((keto?resist$ or non?keto$) adj diabet$).tw. 30. ((adult$ or matur$ or late or slow or stabl$) adj diabet$).tw. 31. (insulin$ defic$ adj relativ$).tw. 32. pluri?metabolic$ syndrom$.tw. 33. or/18‐32 34. exp Diabetes Insipidus/ 35. diabet$ insipidus.tw. 36. 34 or 35 37. 33 not 36 38. 17 and 37 39. randomized‐controlled trial.pt. 40. controlled‐clinical trial.pt. 41. randomized‐controlled‐trials.sh. 42. random allocation.sh. 43. double‐blind method.sh. 44. single‐blind method.sh. 45. or/39‐44 46. animals.sh. 47. humans.sh. 48. 46 not 47 49. 45 not 48 50. clinical trial.pt. 51. exp Clinical Trials/ 52. (clinic$ adj25 trial$).tw. 53. ((singl$ or doubl$ or trebl$ or tripl$) adj (mask$ or blind$)).tw. 54. placebos.sh. 55. placebo$.tw. 56. random$.tw. 57. research design.sh. 58. (latin adj square).tw. 59. or/50‐58 60. 59 not 48 61. 60 not 49 62. exp Evaluation Studies/ 63. follow‐up studies.sh. 64. prospective studies.sh. 65. (control$ or prospectiv$ or volunteer$).tw. 66. cross‐over studies.sh. 67. or/62‐66 68. 67 not 48 69. 68 not (49 or 61) 70. 49 or 61 or 69 71. exp Meta‐Analysis/ 72. exp "Review Literature"/ 73. meta‐analysis.pt. 74. review.pt. 75. or/71‐74 76. letter.pt. 77. comment.pt. 78. editorial.pt. 79. historical‐article.pt. 80. or/76‐79 81. 75 not 80 82. ((systematic$ or quantitativ$ or methodologic$) adj (review$ or overview$)).tw. 83. meta?anal$.tw. 84. (integrativ$ research review$ or research integration$).tw. 85. quantitativ$ synthes$.tw. 86. (pooling$ or pooled analys$ or mantel$ haenszel$).tw. 87. (peto$ or der?simonian$ or fixed effect$ or random effect$).tw. 88. or/82‐87 89. 81 or 88 90. limit 89 to human 91. 70 or 90 92. 38 and 91 |
Data and analyses
Comparison 1. Individual diabetes education programme versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 HbA1c: 6 ‐ 9 months (r = 0.75) | 3 | 295 | Mean Difference (IV, Fixed, 95% CI) | ‐0.23 [‐0.49, 0.03] |
| 1.1 Both Sexes | 2 | 246 | Mean Difference (IV, Fixed, 95% CI) | ‐0.33 [‐0.67, 0.02] |
| 1.2 Women | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐0.1 [‐0.50, 0.30] |
| 2 HbA1c: 12 ‐ 18 months (r = 0.75) | 4 | 632 | Mean Difference (IV, Fixed, 95% CI) | ‐0.08 [‐0.25, 0.08] |
| 3 HbA1c: 6 ‐ 9 months (r = 0.25) | 3 | 295 | Mean Difference (IV, Fixed, 95% CI) | ‐0.26 [‐0.69, 0.16] |
| 3.1 Both Sexes | 2 | 246 | Mean Difference (IV, Fixed, 95% CI) | ‐0.37 [‐0.92, 0.18] |
| 3.2 Women | 1 | 49 | Mean Difference (IV, Fixed, 95% CI) | ‐0.1 [‐0.78, 0.58] |
| 4 HbA1c: 12 ‐ 18 months (r = 0.25) | 4 | 632 | Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.25, 0.14] |
| 5 BMI: 6 ‐ 9 months (r = 0.75) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Women | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 BMI: 12 ‐ 18 months (r = 0.75) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7 Systolic blood pressure: 12 ‐ 18 months (r = 0.75) | 3 | 625 | Mean Difference (IV, Fixed, 95% CI) | ‐1.86 [‐4.68, 0.95] |
| 8 Diastolic blood pressure: 12 ‐ 18 months (r = 0.75) | 3 | 624 | Mean Difference (IV, Fixed, 95% CI) | ‐1.61 [‐3.22, 0.00] |
| 9 Total cholesterol: 12 ‐ 18 months | 3 | 627 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.16, 0.10] |
| 10 Mean baseline HbA1c> 8% | 3 | 424 | Mean Difference (IV, Fixed, 95% CI) | ‐0.31 [‐0.54, ‐0.09] |
1.1. Analysis.
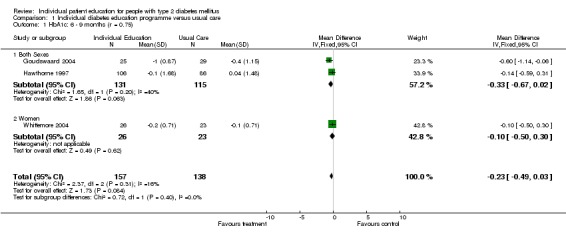
Comparison 1 Individual diabetes education programme versus usual care, Outcome 1 HbA1c: 6 ‐ 9 months (r = 0.75).
1.2. Analysis.
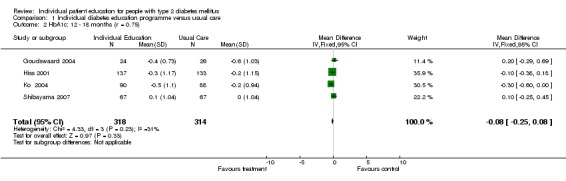
Comparison 1 Individual diabetes education programme versus usual care, Outcome 2 HbA1c: 12 ‐ 18 months (r = 0.75).
1.3. Analysis.
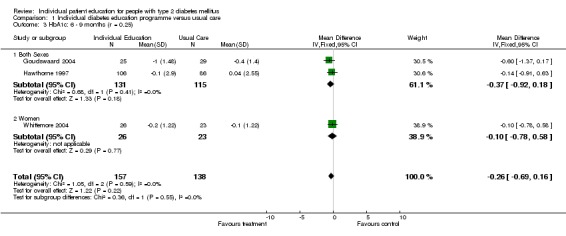
Comparison 1 Individual diabetes education programme versus usual care, Outcome 3 HbA1c: 6 ‐ 9 months (r = 0.25).
1.4. Analysis.

Comparison 1 Individual diabetes education programme versus usual care, Outcome 4 HbA1c: 12 ‐ 18 months (r = 0.25).
1.5. Analysis.
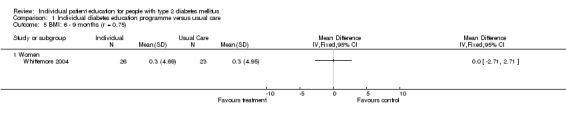
Comparison 1 Individual diabetes education programme versus usual care, Outcome 5 BMI: 6 ‐ 9 months (r = 0.75).
1.6. Analysis.

Comparison 1 Individual diabetes education programme versus usual care, Outcome 6 BMI: 12 ‐ 18 months (r = 0.75).
1.7. Analysis.

Comparison 1 Individual diabetes education programme versus usual care, Outcome 7 Systolic blood pressure: 12 ‐ 18 months (r = 0.75).
1.8. Analysis.

Comparison 1 Individual diabetes education programme versus usual care, Outcome 8 Diastolic blood pressure: 12 ‐ 18 months (r = 0.75).
1.9. Analysis.

Comparison 1 Individual diabetes education programme versus usual care, Outcome 9 Total cholesterol: 12 ‐ 18 months.
1.10. Analysis.
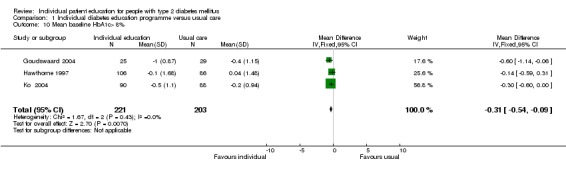
Comparison 1 Individual diabetes education programme versus usual care, Outcome 10 Mean baseline HbA1c> 8%.
Comparison 2. Individual diabetes education programme versus group education programme.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 HbA1c: 6 ‐ 9 months (r = 0.75) | 2 | 148 | Mean Difference (IV, Fixed, 95% CI) | 0.81 [0.34, 1.29] |
| 2 HbA1c: 12 ‐ 18 months | 2 | 112 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.02, 0.08] |
| 3 HbA1c: 6 ‐ 9 months (r = 0.25) | 2 | 148 | Mean Difference (IV, Fixed, 95% CI) | 0.83 [0.19, 1.47] |
| 4 BMI: 6 ‐ 9 months (r = 0.75) | 2 | 169 | Mean Difference (IV, Fixed, 95% CI) | ‐0.11 [‐0.87, 0.65] |
| 5 BMI: 12 ‐ 18 months (r = 0.75) | 2 | 123 | Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.75, 0.73] |
| 6 Systolic blood pressure: 12 ‐ 18 months | 2 | 95 | Mean Difference (IV, Fixed, 95% CI) | 4.12 [‐4.09, 12.32] |
| 7 Diastolic blood pressure: 12 ‐ 18 months (r = 0.75) | 2 | 95 | Mean Difference (IV, Fixed, 95% CI) | 1.52 [‐4.07, 7.11] |
| 8 Total cholesterol: 12 ‐ 18 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
2.1. Analysis.
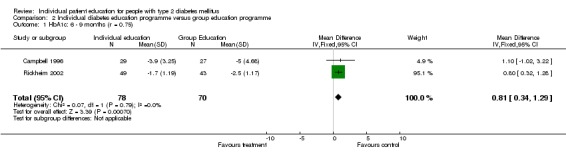
Comparison 2 Individual diabetes education programme versus group education programme, Outcome 1 HbA1c: 6 ‐ 9 months (r = 0.75).
2.2. Analysis.

Comparison 2 Individual diabetes education programme versus group education programme, Outcome 2 HbA1c: 12 ‐ 18 months.
2.3. Analysis.
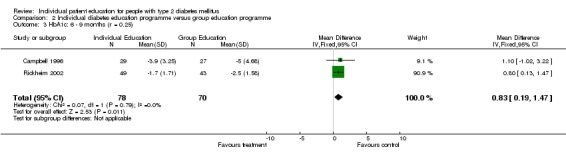
Comparison 2 Individual diabetes education programme versus group education programme, Outcome 3 HbA1c: 6 ‐ 9 months (r = 0.25).
2.4. Analysis.
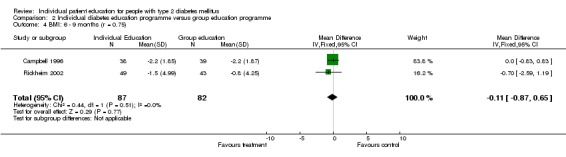
Comparison 2 Individual diabetes education programme versus group education programme, Outcome 4 BMI: 6 ‐ 9 months (r = 0.75).
2.5. Analysis.

Comparison 2 Individual diabetes education programme versus group education programme, Outcome 5 BMI: 12 ‐ 18 months (r = 0.75).
2.6. Analysis.
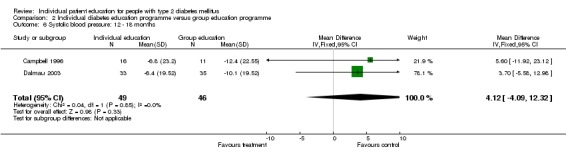
Comparison 2 Individual diabetes education programme versus group education programme, Outcome 6 Systolic blood pressure: 12 ‐ 18 months.
2.7. Analysis.

Comparison 2 Individual diabetes education programme versus group education programme, Outcome 7 Diastolic blood pressure: 12 ‐ 18 months (r = 0.75).
2.8. Analysis.
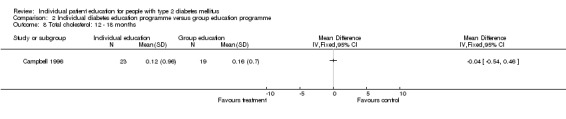
Comparison 2 Individual diabetes education programme versus group education programme, Outcome 8 Total cholesterol: 12 ‐ 18 months.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Campbell 1996.
| Methods | Locale: New South Wales, Australia. Method of recruitment: Patients referred to a Diabetes Education Service (DES). Inclusion/exclusion criteria: Diagnosed with type 2 diabetes, diagnosed for < 5 years, age < 80 yrs, speak, read and understand English, no previous formal instruction on diabetes care, not taking over 75% of the maximum dosage of oral hyopoglycaemic agents and not terminally ill. Randomisation: No details on concealed allocation or method used. Length of follow‐up from start of intervention: 6 and 12 months. Blinding (Investigator (I), Patient (P), Evaluator (E), Analyst (A)): No details given. Power analysis: no Intention to treat: no. Informed consent: yes. Approval: yes | |
| Participants | Socio‐economic background: Not given. Could be judged by referral to the DES. 74% had education up to lower high school. Baseline numbers: Recruited = not given; Eligible= 252; Randomised= 238; Control (Minimal) = 59; Control (Group education) = 65; Intervention (Individual education) = 57; Intervention (Behavioral) = 56. End of study numbers at 6 months: Control (Minimal) = 17; Control (Group education) = 27; Intervention (Individual education) = 29; Intervention (Behavioral) = 43. End of study numbers at 12 months: Control (Group education) = 19; Intervention (Individual education) = 25; Intervention (Behavioral) = 39. Dropout rate: overall at 6 months 53%, at 12 months 35%. Age (mean or range): 58.6 years. Ethnicity: not given. Sex: 52.3 % females. Number of years of diabetes: mean = 0.54 years. Proportion of Type 2: all type 2. Treatment given: 37% on oral hypoglycaemic medication. Average HbA1: Individual 12.2% Group 12.1% | |
| Interventions | The study reported four interventions involving diet, exercise, use of oral hypoglycaemic agents, urine testing, foot care and recommendations to consult opthalmologist and podiatrist. 1. Minimal (Control) ‐ Two (nurse educator and dietician) 1‐ hr sessions. Same topics as intervention groups but in less detail. 2. Group education ‐ Two 1‐hr individual sessions + 3‐day course in small groups + two 2‐hr group follow up at 3 and 9 mo. Also opportunity to attend one 2‐hr lecture. 3. Individual education ‐ Two 1‐hr individual sessions + approx. monthly for 12 months. Same topics but greater details. Opportunity to attend a 2‐hr lecture. 4. Behavioral (Intervention) ‐ series of individual visits by nurse educator + random phone calls by nurse educator. Emphasis on cognitive‐behavioural strategies and cardiovascular risks (diet, exercise and smoking). At 6 months, Extensive and Behavioural were compared with Minimal program as control. For 12‐month comparison, Extensive Group was used as control in this review as there were no outcome reported for Minimal Program. | |
| Outcomes | HbA1, BMI kg/m2; fasting total cholesterol, mmol/l; HDL , mmol/l; cholesterol risk ratio ( total cholesterol /HDL); systolic BP, mmHg; diastolic BP, mmHg; knowledge test (DKN), 15‐point scale; satisfaction ,18 item scale developed by authors. | |
| Notes | Group education had components in individual sessions. Group patients received more overall contact than all other groups. Participants in Minimal program were not measured at 12 months. Therefore for analysis only individual and group were used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Dalmau 2003.
| Methods | Locale: Spain Method of recruitment: Patients from primary care. Inclusion/exclusion criteria: Diagnosed with type 2 diabetes at least six months before the start of trial and had not received group education. Those over 75 years, or having sensory psychological and/or physical deficiencies and those not monitored in primary care were excluded. Randomisation: Unsure of concealment or method used. Length of follow‐up from start of intervention: 12 months. Blinding (Investigator (I), Patient (P), Evaluator (E), Analyst (A)): unsure. Power analysis: unsure. Intention to treat: no. Informed consent: unsure. Approval: unsure. | |
| Participants | Socio‐economic background: Unsure. Baseline numbers: Recruited = 93; Eligible= 79; Randomised= 79; group= 38; Individual = 41. End of study numbers: group= 35; Individual= 33. Dropout rate: 14%. Age: mean = 65 years. Ethnicity: unclear. Sex: 35% males in individual education and 64.7% males in group education Number of years of diabetes: diagnosed at least 6 months prior to study Proportion of Type 2: all. Oral hypoglycaemics: individual 60% and group 51.4% Average HbA1c at baseline: Intervention ‐ 6.6% and group 7.2% | |
| Interventions | Control: Group education. Intervention: Individual education. Each received 3 sessions, seperated by one week, 40 minutes, content the same | |
| Outcomes | HbA1c%; HDL cholesterol, mmol/l; LDL cholesterol, mmol/l; BMI, kg/m2; systolic BP, mmHg; diastolic BP, mmHg; diabetes knowledge. | |
| Notes | There were almost twice as many women in Intervention group compared to that in Control group. Published in Spanish. Data extracted from summary, text and tables. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Goudswaard 2004.
| Methods | Locale: The Netherlands Method of recruitment: Recruited from 57 practices, 78 GPs Inclusion/exclusion criteria: Type 2 diabetes, treated by primary care only, aged less than 76 years, with HbA1c >= 7.0% while taking the maximum feasible dosages of two different oral hypoglycaemic agents. Excluded are those with severe co‐morbidity, not fluent in Dutch, requirement for insulin therapy in the short term on account of severe hyperglycaemic symptoms. Randomisation: By independent trial centre. Method used was computer‐generated random assignment with blocks of 8 patients at a time. Length of follow‐up from start of intervention: 6 and 18 months Blinding (Investigator (I), Patient (P), Evaluator (E), Analyst (A)): Power analysis: yes Intention to treat: yes; missing values represented last previous value. Informed consent: yes Approval: yes | |
| Participants | Socio‐economic background: Participants from all levels of community. Sampling: Recruitment to randomisation =76.3%. Randomisation to completion of trial = 86.2%. Baseline numbers: Recruited = 1810; Eligible = 76; Randomised = 58; Control = 30; Intervention = 28. End of study numbers: Control = 26; Intervention = 24. Dropout rate: 14% Age: average = 60.5 years Ethnicity: Dutch Sex: 52 % females Number of years of diabetes: 7.5 years. Proportion of Type 2: all. Medication: 22% on diet only, 12% on insulin,66% oral hypoglycaemic agents. Average HbA1c ‐ Intervention 8.2%, Control 8.8% | |
| Interventions | Intervention: Collaborative, mixed educational intervention by two diabetes nurses. Focus on diabetes, compliance with medication, importance of physical exercise, losing weight and nutritional advice. 6 sessions during the 6 month period, total contact time of approximately 2.5 hours Control: Usual care by GP. GP instructed not to alter medication unless a patient developed severe hyperglycaemic symptoms |
|
| Outcomes | HbA1c, %. body weight | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Hawthorne 1997.
| Methods | Locale: UK. Method of recruitment: Recruited through Manchester Diabetes Centre or one of 10 mini‐clinics. Inclusion/exclusion criteria: British Pakistanis with Type 2 diabetes. Excluded if enrolled in another study, too ill, if they or spouse had received formal education in the last 6 months Randomisation: Sequential and using concealed envelope and random number generator. Length of follow‐up from start of intervention: 6 months Blinding (Investigator (I), Patient (P), Evaluator (E), Analyst (A)): unclear Power analysis: yes Intention to treat: no Informed consent: yes Approval: yes | |
| Participants | Socio‐economic background: Pakistani migrant and many with little knowledge of English and many illiterate. Baseline numbers: Recruited = na; Eligible= na; Randomised= 201; Control= 112; Intervention = 89. End of study numbers: Control= 86; Intervention= 106. Return to follow‐up rate: 95% Age (mean or range): Intervention 52 years, control 54 years Ethnicity: Pakistani Sex: 46% males in intervention and 47% male in control group Number of years of diabetes: unknown. Proportion of Type 2: all. HbA1c: Intervention 8.4% and control 8.6% | |
| Interventions | Intervention: Face‐to‐face by diabetes nurse using flash cards on various topics (diabetic diet, glucose monitoring and diabetic complications). The educational services were offered in Punjabi or Urudu. 20 minutes with each patient Control: usual care. |
|
| Outcomes | HbA1c, %; knowledge on complications; food knowledge score. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Hiss 2001.
| Methods | Locale: USA. Method of recruitment: Through advertisements and announcement with offer of free & comprehensive diabetes evaluation. Two large and 2 small communities were targeted based on area codes. Inclusion/exclusion criteria: Diagnosed with diabetes Type 2, and those with Type 1 were excluded. Randomisation: No indication of concealed allocation but random number used. Length of follow‐up from start of intervention: 12 months. Blinding (Investigator (I), Patient (P), Evaluator (E), Analyst (A)): not blinded. Power analysis: no Intention to treat: no Informed consent: yes Approval: yes | |
| Participants | Socio‐economic background: Those who responded to the advertisement for the service or incentive or both. Baseline numbers: Recruited = 431; Eligible= 376; Randomised= 376; Control= 190; Intervention = 186. End of study numbers: Control= 156; Intervention= 158. Return to follow‐up rate: 84% Age (mean or range): Control = 64 years; Intervention = 65 years. Ethnicity: not available Sex: Control = 27% and Intervention = 12% females. Number of years of diabetes: Control = 10 years and Intervention = 9 years. Proportion of Type 2: all. Average HbA1c: Intervention 7.7% & control 7.9% | |
| Interventions | Control: usual care. Intervention: Face‐to‐face or via telephone by specialist nurse educator. Approx 4 hours of professional time per patient Individual education and counselling session to encourage the patient to consult physician about identified problem. High risk subsets for each outcome were defined as follows: HbA1c >= 7.5%, cholesterol >= 6.22mmol/l, systolic blood pressure >= 140 mmHg and systolic blood pressure >= 90 mmHg. | |
| Outcomes | HbA1c, %; total cholesterol, mmol/L; diastolic BP, mmHg; systolic BP, mmHg. | |
| Notes | intervention timing not clear; | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Ko 2004.
| Methods | Locale: Hong Kong Method of recruitment: from 3 regional diabetic centres in Hong Kong Inclusion/exclusion criteria: HbA1c 8.1 ‐ 11%, age range 35 ‐ 70 years Randomisation: coin tossing Length of follow‐up from start of intervention: 1 year Blinding (Investigator (I), Patient (P), Evaluator (E), Analyst (A)): physicians blinded Power analysis: yes Intention to treat: no Informed consent: not stated Approval: not stated | |
| Participants | Socio‐economic background: Baseline numbers: 90 in each group End of study numbers: 2 control patients defaulted follow‐up Return to follow‐up rate: 99% Age (mean or range): Intervention 55, control 56 years Ethnicity: Chinese Sex: Intervention 48.9% male, control group 38.6% male Number of years of diabetes: not stated Proportion of Type 2: all. Average HbA1c: Intervention 8.6%, control 8.4% | |
| Interventions | Both groups followed up every 10 ‐ 14 weeks Intervention: 5 x 30 minute visits after follow‐up by physicians, by nurse educator, concentrated on CV risk factors Control: same medical care except no nursing reinforcement | |
| Outcomes | fasting glucose, HbA1c, body mass index, waist circumference, blood pressure and lipid profiles | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
Rickheim 2002.
| Methods | Locale: USA. Method of recruitment: Patients referred to Diabetes Centre by primary care provider over a 2‐year period from April 1997 to July 1999. Inclusion/exclusion criteria: Type 2. Newly diagnosed or previously diagnosed but without prior formal diabetes education. Patients treated with medical nutritional therapy and /or medical therapy. Randomisation: randomisation in blocks of 3 patients to Control or Intervention during first year and in the following year, in blocks of 10 patients. Method of concealment or allocation was unclear. Length of follow‐up from start of intervention: 6 months. Blinding (Investigator (I), Patient (P), Evaluator (E), Analyst (A)): all unclear. Power analysis: not presented. Intention to treat: no. Informed consent: yes Approval: yes | |
| Participants | Source of patients: referred by primary care providers. Newly diagnosed diabetes or no history of prior systematic diabetes education Socio‐economic background: not clear. Baseline numbers: Randomised= 170; Control= 87; Intervention = 83. End of study numbers: Control= 43; Intervention= 49. Retention to follow‐up: 54% Age (mean or range): 52.5 years Ethnicity: 93% Caucasians Sex: 66% females Number of years of diabetes: 0.9 years. Proportion of Type 2: All Average HbA1c: Group 9% and individual 8.2% | |
| Interventions | General: Four sessions were given to both groups. 5‐7 hours. Contents covered topics on education including diet, glucose monitoring and foot care. Participants in control groups received in groups of 4 to 8. Individuals in intervention group had shorter sessions to cover the same material. Interventions in both settings emphasized empowering the patient, by increasing knowledge, facilitating self‐management behaviour change | |
| Outcomes | HbA1c, %; weight, kg; BMI, kg/m2; knowledge test (14pts); exercise (times/week); exercise duration (min/week); ATT‐19 ‐ Psychosocial adjustment and attitudes towards diabetes using 19‐point score; SF‐36 mental scale that measured mental health related quality of life; SF‐36 physical scale that measured physical health related quality of life. | |
| Notes | Allocation in blocks of 6 or 10 may be biased. Groups attending clinic may be relatives, friends of similar socio‐economic background. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Shibayama 2007.
| Methods | Locale: Japan Method of recruitment: outpatients of Department of diabetes and Metabolism, University Hospital. Inclusion/exclusion criteria: adults, between ages of 20 ‐ 75, diagnosed with type 2 diabetes; HbA1c between 6.5% and 8.5%, who could not use insulin. Randomisation: randomised but no details on concealment or methods. Length of follow‐up from start of intervention: 1 year Blinding (Investigator (I), Patient (P), Evaluator (E), Analyst (A)): not blinded. Power analysis: yes with 64 patients in each group, there was an 80% power to detect 0.5% difference in the change in HbA1c Intention to treat: no. Informed consent: not stated Approval: Yes | |
| Participants | Socio‐economic background: not stated Baseline numbers: intervention 67 and control 67 End of study numbers at 12 months: intervention 59 control 61 Dropout rate: 10% Age (mean or range): Intervention 61, Control 62 Ethnicity: Japanese Sex: 65% males Number of years of diabetes: mean = intervention 10 years, control 13 years. Proportion of Type 2: all. Treatment given: 89.6% on oral hypoglycaemic medication in intervention and 82.1% in control Average HbA1c: Individual 7.3% Group 7.4% | |
| Interventions | Intervention: received normal medical consultation and one‐to‐one counselling with a certified expert nurse at monthly hospital visits for 1 year. Features are patient participation in goal setting, personalized strategies and goal setting. Control: received usual care by same practitioners at hospital clinic | |
| Outcomes | HbA1c, HRQOL with SF‐36Japanese Version, PAID , cognitive modification (3 items), behavioural modification (1 item) and overall satisfaction with counselling (1 item) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Whittemore 2004.
| Methods | Locale: USA. Method of recruitment: Patients enrolled at single diabetes centre. Inclusion/exclusion criteria: Females, diagnosed with type 2 diabetes; 30 to 70 yrs age; cleared for exercise by primary care provider; had no advanced complications of diabetes; HbA1c >7%; fluent in English and had previously participated in diabetes education. Randomisation: randomised but no details on concealment or methods. Length of follow‐up from start of intervention: 6 months. Blinding (Investigator (I), Patient (P), Evaluator (E), Analyst (A)): all unclear. Power analysis: no. Intention to treat: no. Informed consent: yes. Approval: yes. | |
| Participants | Socio‐economic background: wide cover, low to middle income, mean of 12.6 yrs of education. Baseline numbers: Recruited = 81; Eligible= 53; Randomised= 53; Control= 24; Intervention = 29. End of study numbers: Control= 23; Intervention= 26. Retention to follow‐up rate: 92% Age (mean or range): 57.6 years Ethnicity: 89% white, 11% Hispanic. Sex: all females Number of years of diabetes: 2.7 years. Proportion of Type 2: all. Mean HbA1c 7.7% | |
| Interventions | Control: standard diabetes care at 3 ‐ 4 month intervals. Providers nurse practitioners, internists, endocrinologists and family practice specialists Intervention: Individualised 6 nurse‐coaching sessions over 6 months. Included topics were assessment, education reinforcement (cognitive component), problem solving (behavioural component) and psychosocial support (affective component). | |
| Outcomes | HbA1c, %; BMI, kg/m2; self management on diet, 5‐point scale; self management on exercise, min/mo; distress‐ PAID score; integration ‐ TDQ score., treatment satisfaction DTSQc HbA1c DCA 2000 analyzer |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aas 2005 | Mixed individual and group education sessions |
| Anderson 2005 | Primarily group education |
| Bacardi‐Gascon 2004 | Not a randomised controlled trial/ controlled trial |
| Baradaran 2006 | Primarily group education |
| Baran 1999 | Not a randomised controlled trial/ controlled trial |
| Barcelo 2001 | Mixed type 1/ type 2 |
| Barth 1991 | Primarily group education |
| Bloomgarden 1987 | Primarily group education |
| Bradshaw 2006 | Primarily group education |
| Browning 2003 | Not a randomised controlled trial/ controlled trial |
| Cabrera‐Pivaral 2000 | Primarily group education |
| Chen 2003 | Primarily foot care intervention |
| Cleghorn 2004 | Not a randomised controlled trial/ controlled trial |
| Clifford 2005 | Managed care ‐ pharmacy |
| Cooper 2003 | Primarily group education |
| D'Eramo‐Melkus 1992 | Mixed individual and group education sessions |
| De Weerdt, I., 1991 | Primarily group education |
| Deakin 2006 | Control group non standardized individual education |
| Di Loreto 2003 | Primarily physical activity intervention |
| Dijkstra 2006 | Education of professionals |
| Dongbo 2003 | Primarily group education |
| Donohoe 2000 | Education of professionals |
| Fan 1999 | Mixed individual and group education sessions |
| Fan, M. J., G. 2002 | Not a randomised controlled trial/ controlled trial |
| Fornos 2006 | Managed care ‐ pharmacy |
| Fu 2003 | Primarily group education |
| Fukuda 1999 | Mixed individual and group education sessions |
| Gabbay 2006 | Managed care |
| Gaede 2001 | Mixed individual and group education sessions |
| Gallegos 2006 | Mixed individual and group education sessions |
| Gary 2003 | Managed care |
| Gentile 2004 | Primarily group education |
| Ghosh 2007 | Not randomised controlled trial/ controlled trial |
| Gilliland 2002 | Not a randomised controlled trial/ controlled trial |
| Glasgow | Primarily group education |
| Hae 2005 | Managed care ‐ pharmacy |
| Hajdinjak 2003 | Not a randomised controlled trial/ controlled trial |
| Hanefeld 1991 | Mixed individual and group education sessions |
| Holtrop 2002 | Primarily group education |
| Jayasuriya 2000 | Not a randomised controlled trial/ controlled trial |
| Jones 2003 | Education not face to face |
| Jungmann 1997 | Not a randomised controlled trial/ controlled trial |
| Kirk 2004 | Primarily physical activity intervention |
| Ko, S. H., K. 2007 | Primarily group education |
| Korhonen 1987 | Primarily dietary intervention |
| Kronsbein 1988 | Not a randomised controlled trial/ controlled trial |
| Kulzer 2007 | Mixed individual and group education sessions |
| Laitinen 1993 | Primarily dietary intervention |
| Li 2003 | Mixed individual and group education sessions |
| Li, X., Y. Cao, 2003 | Not a randomised controlled trial/ controlled trial |
| Litzelman 1993 | Not individual education |
| Lorig 2003 | Not specific for diabetes |
| Lou 2006 | Primarily group education |
| Lozano 1999 | Primarily group education |
| Maislos 2004 | Managed care |
| Martinus 2006 | Primarily physical activity intervention |
| Mayer‐Davis 2004 | Mixed individual and group education sessions |
| Mazzuca 1986 | Mixed individual and group education sessions |
| Mshelia 2007 | Mixed individual and group education sessions |
| Neder 2003 | References 'Corbett 2003' which evaluated foot care |
| Odegard 2005 | Managed care ‐ pharmacy |
| Pedersen 2003 | Mixed individual and group education sessions |
| Pennings‐Van 1992 | Primarily group education |
| Philis‐Tsimikas 2004 | Mixed individual and group education sessions |
| Pibernik‐Okanovi2004 | Not a randomised controlled trial/ controlled trial, group education |
| Trento 2001 | Primarily group education |
| Wilson 1987 | Primarily group education |
| Wolf 2004 | Primarily group education |
| Woollard 2003 | Not specific to diabetes |
Contributions of authors
SALLY‐ANNE DUKE: developed the search strategy; co‐selected studies and undertook selection, quality assessment, data extraction, data analysis, and was the primary writer of the final review.
STEPHEN COLAGIURI: advised on design, methods and data analysis, assisted with study selection and reviewed all selected articles
RUTH COLAGIURI: was primarily responible for the protocol, design, co‐selection of all studies and contributed to the writing of the final review.
All three authors were invovled in developing study selection critieria and received and commented on successive drafts of the review.
Sources of support
Internal sources
Austrailian Department of Health and Ageing via the Australasian Cochrane Centre, Not specified.
External sources
No sources of support supplied
Declarations of interest
None known
New
References
References to studies included in this review
Campbell 1996 {published data only}
- Campbell E M, Redman S, Moffitt PS, Sanson‐Fisher RW. The relative effectiveness of educational and behavioral instruction programs for patients with NIDDM: a randomized trial. Diabetes Educator 1996;22(4):379‐86. [DOI] [PubMed] [Google Scholar]
Dalmau 2003 {published data only}
- Dalmau Llorca MR, Garcia Bernal G, Aguilar Martin C, Palau Galindo A. [Group versus individual education for type‐2 diabetes patients]. Atencion Primaria 2003;32(1):36‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goudswaard 2004 {published data only}
- Goudswaard AN, Stolk RP, Zuithoff NP, Valk HW, Rutten GE. Long‐term effects of self‐management education for patients with Type 2 diabetes taking maximal oral hypoglycaemic therapy: a randomized trial in primary care. Diabetic Medicine 2004;21(5):491‐6. [DOI] [PubMed] [Google Scholar]
Hawthorne 1997 {published data only}
- Hawthorne K, Tomlinson S. One‐to‐one teaching with pictures‐ flashcard health education for Bristish Asians with diabetes. British Journal of General Practice 1997;47:301‐304. [PMC free article] [PubMed] [Google Scholar]
Hiss 2001 {published data only}
- Hiss RG, Lou Gillard M, Armbruster BA, McClure LA. Comprehensive evaluation of community‐based diabetic patients: Effect of feedback to patients and their physicians: A randomized controlled trial. Diabetes Care 2001;24(4):690‐4. [DOI] [PubMed] [Google Scholar]
Ko 2004 {published data only}
- Ko GTC, Li JKY, Kan ECY, Lo MKW. Effects of a structured health education programme by a diabetic education nurse on cardiovascular risk factors in Chinese Type 2 diabetic patients: a 1‐year prospective randomized study. Diabetic Medicine 2004;21:1274‐1279. [DOI] [PubMed] [Google Scholar]
Rickheim 2002 {published data only}
- Rickheim PL, Weaver TW, Flader JL, Kendall DM. Assessment of group versus individual diabetes education: a randomized study. Diabetes Care 2002;25(2):269‐74. [DOI] [PubMed] [Google Scholar]
Shibayama 2007 {published data only}
- Shibayama T, Kobayashi K, Takano A, Kadowaki T, Kazuma K. Effectiveness of lifestyle counseling by certified expert nurse of Japan for non‐insulin‐treated diabetic outpatients: A 1‐year randomized controlled trial. Diabetes Research and Clinical Practice 2007;76:265‐268. [DOI] [PubMed] [Google Scholar]
Whittemore 2004 {published data only}
- Whittemore R, Melkus GD, Sullivan A, Grey M. A nurse‐coaching intervention for women with type 2 diabetes. Diabetes Educator 2004;30(5):795‐804. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Aas 2005 {published data only}
- Aas, A M, I. Bergstad, et al. An intensified lifestyle intervention programme may be superior to insulin treatment in poorly controlled Type 2 diabetic patients on oral hypoglycaemic agents: results of a feasibility study. Diabetic Medicine 2005;22(3):316‐322. [DOI] [PubMed] [Google Scholar]
Anderson 2005 {published data only}
- Anderson, R M, M. M. Funnell, et al. Evaluating a problem‐based empowerment program for African Americans with diabetes: results of a randomized controlled trial. Ethnicity and Disease 2005;15(4):671‐8. [PubMed] [Google Scholar]
Bacardi‐Gascon 2004 {published data only}
- Bacardi‐Gascon, M, P. Rosales‐Garay, et al. Effect of Diabetes Intervention Programs on Physical Activity among Migrant Mexican Women with Type 2 Diabetes. Diabetes Care 2004;27(2):616. [DOI] [PubMed] [Google Scholar]
Baradaran 2006 {published data only}
- Baradaran, H R, R. P. Knill‐Jones, et al. A controlled trial of the effectiveness of a diabetes education programme in a multi‐ethnic community in Glasgow [ISRCTN28317455]. BMC Public Health 2006;6:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baran 1999 {published data only}
- Baran, R W, K. Crumlish, et al. Improving outcomes of community‐dwelling older patients with diabetes through pharmacist counseling. American Journal of Health‐System Pharmacy 1999;56(15):1535‐1539. [DOI] [PubMed] [Google Scholar]
Barcelo 2001 {published data only}
- Barcelo, A, S. Robles, et al. An intervention to improve diabetes control in Chile. [Spanish]. Revista Panamericana de Salud Publica/Pan American Journal of Public Health. 2001;10(5):328‐333. [PubMed] [Google Scholar]
Barth 1991 {published data only}
- Barth, R, L. V. Campbell, et al. Intensive education improves knowledge, compliance, and foot problems in type 2 diabetes,. Diabetic Medicine. 1991;8(2):111‐117. [DOI] [PubMed] [Google Scholar]
Bloomgarden 1987 {published data only}
- Bloomgarden, Z T, W. Karmally, et al. Randomized, controlled trial of diabetic patient education: Improved knowledge without improved metabolic status,. Diabetes Care 1987;10(3):263‐272. [DOI] [PubMed] [Google Scholar]
Bradshaw 2006 {published data only}
- Bradshaw, B G. The efficacy of a resiliency training program in adults with type 2 diabetes mellitus. Thesis Univeristy of Utah 2006.
Browning 2003 {published data only}
- Browning, C J, S. A. Thomas. Six‐month outcome data for the Good Life Club project: an outcomes study of diabetes self‐management.. Special Issue: The Management of Chronic Disease in Primary Care Settings 2003; Vol. 9:192‐198.
Cabrera‐Pivaral 2000 {published data only}
- Cabrera‐Pivaral, C E, G. Gonzalez‐Perez, et al. Effects of behavior‐modifying education in the metabolic profile of the type 2 diabetes mellitus patient. Journal of Diabetes & its Complications 2000;14(6):322‐6. [DOI] [PubMed] [Google Scholar]
Chen 2003 {published data only}
- Chen, Y S, W. C. Xu, et al. Significance of reinforcing management on limb salvage therapy in patients at high risk for diabetic foot. [Chinese],. Zhongguo Linchuang Kangfu 2003;7(18):2556‐2557. [Google Scholar]
Cleghorn 2004 {published data only}
- Cleghorn, G D, M. Nguyen, et al. Practice‐based interventions to improve health care for Latinos with diabetes. Ethnicity & Disease Summer 2004;1:117‐121. [PubMed] [Google Scholar]
Clifford 2005 {published data only}
- Clifford, R M, W. A. Davis, et al. Effect of a pharmaceutical care program on vascular risk factors in type 2 diabetes: the Fremantle Diabetes Study. Diabetes Care 2005;28(4):771‐6. [DOI] [PubMed] [Google Scholar]
Cooper 2003 {published data only}
- Cooper, H, K. Booth, et al. Using combined research methods for exploring diabetes patient education. Patient Education & Counseling 2003;51(1):45‐52. [DOI] [PubMed] [Google Scholar]
D'Eramo‐Melkus 1992 {published data only}
- D'Eramo‐Melkus, G A, J. Wylie‐Rosett, et al. Metabolic impact of education in NIDDM. Diabetes Care 1992;15(7):864‐9. [DOI] [PubMed] [Google Scholar]
De Weerdt, I., 1991 {published data only}
- De Weerdt, I, A. P. Visser, et al. Randomized controlled multicentre evaluation of an education programme for insulin‐treated diabetic patients: Effects on metabolic control, quality of life, and costs of therapy,. Diabetic Medicine. 1991;8(4):338‐345. [DOI] [PubMed] [Google Scholar]
Deakin 2006 {published data only}
- Deakin, T A, J. E. Cade, et al. Structured patient education: the Diabetes X‐PERT Programme makes a difference. Diabetic Medicine 2006;23(9):944‐954. [DOI] [PubMed] [Google Scholar]
Di Loreto 2003 {published data only}
- Di Loreto, C, C. Fanelli, et al. Validation of a counseling strategy to promote the adoption and the maintenance of physical activity by type 2 diabetic subjects. Diabetes Care 2003;26(2):404‐8. [DOI] [PubMed] [Google Scholar]
Dijkstra 2006 {published data only}
- Dijkstra, R F, L. W. Niessen, et al. Patient‐centred and professional‐directed implementation strategies for diabetes guidelines: A cluster‐randomized trial‐based cost‐effectiveness analysis,. Diabetic Medicine 2006;23(2):164‐170. [DOI] [PubMed] [Google Scholar]
Dongbo 2003 {published data only}
- Dongbo, F, F. Hua, et al. Implementation and quantitative evaluation of chronic disease self‐management programme in Shanghai, China: Randomized controlled trial,. Bulletin of the World Health Organization 2003;81(3):174‐182. [PMC free article] [PubMed] [Google Scholar]
Donohoe 2000 {published data only}
- Donohoe, E, J. A. Fletton, et al. Improving foot care for people with diabetes mellitus ‐ A randomized controlled trial of an integrated care approach,. Diabetic Medicine 2000;17(8):581‐587. [DOI] [PubMed] [Google Scholar]
Fan 1999 {published data only}
- Fan, L, J. Zhu, et al. Effect of diabetic education on patients' knowledge and self‐management ability [Chinese]. Hong Kong Nursing Journal 1999;35(2):15‐8. [Google Scholar]
Fan, M. J., G. 2002 {published data only}
- Fan, M J, G. H. Wu, et al. Effect evaluation of health education in 80 cases of type 2 diabetes,. Zhongguo Linchuang Kangfu 2002;6(21):3298. [Google Scholar]
Fornos 2006 {published data only}
- Fornos, J A, N. F. Andres, et al. A pharmacotherapy follow‐up program in patients with type‐2 diabetes in community pharmacies in Spain. Pharmacy World & Science 2006;28(2):65‐72. [DOI] [PubMed] [Google Scholar]
Fu 2003 {published data only}
- Fu, D, H. Fu, et al. Implementation and quantitative evaluation of chronic disease self‐management programme in Shanghai, China: Randomized controlled trial. Bulletin of the World Health Organization 2003;81(3):174‐182. [PMC free article] [PubMed] [Google Scholar]
Fukuda 1999 {published data only}
- Fukuda H, M. Evaluation of a diabetes patient education program consisting of a three‐day hospitalization and a six‐month follow‐up by telephone counseling for mild type 2 diabetes and IGT. Environmental Health & Preventive Medicine 1999;4(3):122‐129. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gabbay 2006 {published data only}
- Gabbay, R A, I. Lendel, et al. Nurse case management improves blood pressure, emotional distress and diabetes complication screening,. Diabetes Research & Clinical Practice 2006;71(1):28‐35. [DOI] [PubMed] [Google Scholar]
Gaede 2001 {published data only}
- Gaede, P, M. Beck, et al. Limited impact of lifestyle education in patients with Type 2 diabetes mellitus and microalbuminuria: results from a randomized intervention study. Diabetic Medicine 2001;18(2):104‐8. [DOI] [PubMed] [Google Scholar]
Gallegos 2006 {published data only}
- Gallegos, E C, F. Ovalle‐Berumen, et al. Metabolic control of adults with type 2 diabetes mellitus through education and counseling. Journal of Nursing Scholarship 2006;38(4):344‐51. [DOI] [PubMed] [Google Scholar]
Gary 2003 {published data only}
- Gary, T L, L. R. Bone, et al. Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetes‐related complications in urban African Americans. Preventive Medicine 2003;37(1):23‐32. [DOI] [PubMed] [Google Scholar]
Gentile 2004 {published data only}
- Gentile, L, E. Borgo, et al. ROMEO: Rethink Organization to improve education and outcomes. A randomised controlled multicentre trial of group care for the management of type 2 diabetes. [Italian],. Giornale Italiano di Diabetologia e Metabolismo. 2004;24(1):9‐16. [Google Scholar]
Ghosh 2007 {published data only}
- Ghosh, H A, A. Shaar, et al. Diabetes control in 3 villages in Palestine: A community‐based quality improvement intervention,. Journal of Ambulatory Care Management. 2007;30(1):74‐78. [DOI] [PubMed] [Google Scholar]
Gilliland 2002 {published data only}
- Gilliland, S S, S. P. Azen, et al. Strong in body and spirit: Lifestyle intervention for Native American adults with diabetes in New Mexico,. Diabetes Care 2002;25(1):78‐83. [DOI] [PubMed] [Google Scholar]
Glasgow {published data only}
- Glasgow Re, T. Nutrition education and social learning interventions for type II diabetes.. Diabetes care 1989;12(2):150‐2. [DOI] [PubMed] [Google Scholar]
Hae 2005 {published data only}
- Hae, M C, S. Mitrovich, et al. Proactive case management of high‐risk patients with type 2 diabetes mellitus by a clinical pharmacist: A randomized controlled trial. American Journal of Managed Care 2005;11(4):253‐260. [PubMed] [Google Scholar]
Hajdinjak 2003 {published data only}
- Hajdinjak, D, M. Cokolic. Improvement of control of type 2 diabetes after patient education. Diabetes & Metabolism 2003;29:(Hors serie 2). [Google Scholar]
Hanefeld 1991 {published data only}
- Hanefeld, M, S. Fischer, et al. Diabetes Intervention Study. Multi‐intervention trial in newly diagnosed NIDDM. 1991 Diabetes Care;14(4):308‐17. [DOI] [PubMed] [Google Scholar]
Holtrop 2002 {published data only}
- Holtrop, J S, J. Hickner, et al. "Sticking to it ‐‐ diabetes mellitus": a pilot study of an innovative behavior change program for women with type 2 diabetes. American Journal of Health Education 2002;33(3):161‐6. [Google Scholar]
Jayasuriya 2000 {published data only}
- Jayasuriya, R, R. Griffiths, et al. Outcome assessment of a community based model of general practitioner care diabetes patients,. Practical Diabetes International 2000;17(6):179‐182. [Google Scholar]
Jones 2003 {published data only}
- Jones, H, L. Edwards, et al. Changes in diabetes self‐care behaviors make a difference in glycemic control ‐ The diabetes stages of change (DiSC) study. Diabetes care 2003;26(3):732‐737. [DOI] [PubMed] [Google Scholar]
Jungmann 1997 {published data only}
- Jungmann, E, G. Jungmann, et al. Patient education of non‐insulin‐dependent diabetic patients. Effect of an ambulatory educational program on metabolism and risk factors. Fortschritte der Medizin 1997;115:20‐1. [PubMed] [Google Scholar]
Kirk 2004 {published data only}
Ko, S. H., K. 2007 {published data only}
- Ko, S H, K. H. Song, et al. Long‐term effects of a structured intensive diabetes education programme (SIDEP) in patients with Type 2 diabetes mellitus ‐ A 4‐year follow‐up study,. Diabetic Medicine 2007;24(1):55‐62. [DOI] [PubMed] [Google Scholar]
Korhonen 1987 {published data only}
- Korhonen, T, M. Uusitupa, et al. Efficacy of dietary instructions in newly diagnosed non‐insulin‐dependent diabetic patients. Comparison of two different patient education regimens. Acta Medica Scandinavica 1987;222(4):323‐31. [DOI] [PubMed] [Google Scholar]
Kronsbein 1988 {published data only}
- Kronsbein, P, V. Jorgens, et al. Evaluation of a structured treatment and teaching programme on non‐insulin‐dependent diabetes. Lancet 1988;2:1407‐11. [DOI] [PubMed] [Google Scholar]
Kulzer 2007 {published data only}
- Kulzer, B, N. Hermanns, et al. Effects of self‐management training in Type 2 diabetes: a randomized, prospective trial. Diabetic Medicine 2007;24(4):415‐423. [DOI] [PubMed] [Google Scholar]
Laitinen 1993 {published data only}
- Laitinen Jh, A. Impact of intensified dietary therapy on energy and nutrient intakes and fatty acid composition of serum lipids in patients with recently diagnosed non‐insulin‐dependent diabetes mellitus.. Journal of the American Dietetic Association 1993;93(3):276‐83. [DOI] [PubMed] [Google Scholar]
Li 2003 {published data only}
- Li, X. Experiences of carrying out health education in type 2 diabetes patients [Chinese]. Chinese Nursing Research 2003;17(2B):195‐7. [Google Scholar]
Li, X., Y. Cao, 2003 {published data only}
- Li, X, Y. Cao, et al. Effects of education on blood sugar and complications of 2 type diabetes,. Zhongguo Linchuang Kangfu 2003;7(3):509. [Google Scholar]
Litzelman 1993 {published data only}
- Litzelman Dk, S. Reduction of lower extremity clinical abnormalities in patients with non‐insulin‐dependent diabetes mellitus. A randomized, controlled trial. Annals of internal medicine 1993;119(1):36‐41, 1993. [DOI] [PubMed] [Google Scholar]
Lorig 2003 {published data only}
- Lorig, K R, P. L. Ritter, et al. Hispanic chronic disease self‐management: a randomized community‐based outcome trial. Nursing Research 2003;52(6):361‐9. [DOI] [PubMed] [Google Scholar]
Lou 2006 {published data only}
- Lou, V W. Q, Y. Q. Zhang. Evaluating the effectiveness of a Participatory Empowerment Group for Chinese type 2 diabetes patients. Research on Social Work Practice 2006;16(5):491‐499. [Google Scholar]
Lozano 1999 {published data only}
- Lozano, M L, M. J. Armale, et al. [The education of type‐2 diabetics: why not in groups?].[see comment][erratum appears in Aten Primaria 1999 Jul‐Aug;24(3):178]. Atencion Primaria 1999;24(3):485‐92. [PubMed] [Google Scholar]
Maislos 2004 {published data only}
- Maislos, M, D. Weisman. Multidisciplinary approach to patients with poorly controlled type 2 diabetes mellitus: A prospective, randomized study,. Acta Diabetologica 2004;41(2):44‐48. [DOI] [PubMed] [Google Scholar]
Martinus 2006 {published data only}
- Martinus, R, R. Corban, et al. Effect of psychological intervention on exercise adherence in type 2 diabetic subjects. Annals of the New York Academy of Sciences 2006;1084:350‐60. [DOI] [PubMed] [Google Scholar]
Mayer‐Davis 2004 {published data only}
- Mayer‐Davis, E J, A. M. D'Antonio, et al. Pounds off with empowerment (POWER): A clinical trial of weight management strategies for black and white adults with diabetes who live in medically underserved rural communities,. American Journal of Public Health 2004;94(10):1736‐1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mazzuca 1986 {published data only}
- Mazzuca, S A, N. H. Moorman, et al. The Diabetes Education Study: A controlled trial of the effects of diabetes patient education,. Diabetes Care 1986;9(1):1‐10. [DOI] [PubMed] [Google Scholar]
Mshelia 2007 {published data only}
- Mshelia, D S, O. M. Akinosun, et al. Effect of increased patient‐physician contact time and health education in achieving diabetes mellitus management objectives in a resource‐poor environment. Singapore Medical Journal 2007;48(1):74‐9. [PubMed] [Google Scholar]
Neder 2003 {published data only}
- Neder, S, P. Nadash, et al. Individualized education can improve foot care for patients with diabetes. Home Healthcare Nurse 2003;21(12):837‐40. [DOI] [PubMed] [Google Scholar]
Odegard 2005 {published data only}
- Odegard, P S, A. Goo, et al. Caring for poorly controlled diabetes mellitus: a randomized pharmacist intervention. Annals of Pharmacotherapy 2005;39(3):433‐40. [DOI] [PubMed] [Google Scholar]
Pedersen 2003 {published data only}
- Pedersen, O, P. Gaede. Intensified multifactorial intervention and cardiovascular outcome in type 2 diabetes: The Steno‐2 study,. Metabolism: Clinical & Experimental. 2003;52(8 Suppl 1):19‐23. [DOI] [PubMed] [Google Scholar]
Pennings‐Van 1992 {published data only}
- Pennings‐Van der Eerden, L, T. Ripken, et al. Evaluation of the impact of a patient education programme for NIDDM patients on knowledge, self‐care behaviour, metabolic control and lipid profiles. Gedrag & Gezondheid: Tijdschrift voor Psychologie en Gezondheid 1992;19(5):246‐260. [Google Scholar]
Philis‐Tsimikas 2004 {published data only}
- Philis‐Tsimikas, A, C. Walker, et al. Improvement in diabetes care of underinsured patients enrolled in Project Dulce: A community‐based, culturally appropriate, nurse case management and peer education diabetes care model. Diabetes Care 2004;27(1):110‐115. [DOI] [PubMed] [Google Scholar]
Pibernik‐Okanovi2004 {published data only}
- Pibernik‐Okanovic, M, M. Prasek, et al. Effects of an empowerment‐based psychosocial intervention on quality of life and metabolic control in type 2 diabetic patients. Patient Education and Counseling 2004;52(2):193‐9. [DOI] [PubMed] [Google Scholar]
Trento 2001 {published data only}
- Trento M, Passera P, et al. Group visits improve metabolic control in type 2 diabetes: a 2‐year follow‐up. Diabetes Care 2001;24(6):995‐1000. [DOI] [PubMed] [Google Scholar]
Wilson 1987 {published data only}
- Wilson, W, C. Pratt, et al. The impact of diabetes education and peer support upon weight and glycemic control of elderly persons with noninsulin dependent diabetes mellitus (NIDDM). American Journal of Public Health 1987;77(5):634‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wolf 2004 {published data only}
- Wolf, A M, M. R. Conaway, et al. Translating lifestyle intervention to practice in obese patients with type 2 diabetes: Improving Control with Activity and Nutrition (ICAN) study.[see comment]. Diabetes Care 2004;27(7):1570‐6. [DOI] [PubMed] [Google Scholar]
Woollard 2003 {published data only}
- Woollard, J, V. Burke, et al. Effects of general practice‐based nurse‐counselling on ambulatory blood pressure and antihypertensive drug prescription in patients at increased risk of cardiovascular disease. Journal of Human Hypertension 2003;17(10):689‐95. [DOI] [PubMed] [Google Scholar]
Additional references
AADE 2003
- AADE. Standards for Outcomes Measurement of Diabetes Self‐Management Education. Position Statement.. Diabetes Educator 2003;29(5):804‐16. [DOI] [PubMed] [Google Scholar]
ADA 1999
- The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the diagnosis and classification of diabetes mellitus. Diabetes Care 1999;22 Suppl 1:S5‐19. [DOI] [PubMed] [Google Scholar]
ADA 2003
- American Diabetes Association. Economic costs of diabetes in the US in 2002.. Diabetes Care 2003;26:917‐932. [DOI] [PubMed] [Google Scholar]
Corabian 2001
- Corabian P, Harstall C. Patient Diabetes Education in the Management of Adult Type 2 Diabetes. Health Technology Assessment ‐ Alberta Heritage Foundation for Medical Research. Alberta: Alberta Heritage Foundation for Medical Research, 2001; Vol. HTA 23 Series A, issue Feb:1‐90.
Davies 2008
- Davies MJ, Heller S, Skinner TC, Campbell MJ, Carey ME, Cradock S, et al. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial.. BMJ 2008;336(7642):491‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deakin 2005
- Deakin T, McShane CE, Cade JE, Williams RDRR. Group based training for self‐management strategies in people with thype 2 diabetes mellitus. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD003417.pub2] [DOI] [PubMed] [Google Scholar]
Deakin 2006
- Deakin TA, Cade JE, Williams R, Greenwood DC. Structured patient education: the diabetes X‐PERT Programme makes a difference. Diabetic Medicine 2006;23(9):944‐54. [DOI] [PubMed] [Google Scholar]
Diabetes Atlas 2005
- International Diabetes Federation. Diabetes Atlas. www.idf.org/e‐atlas. 2005.
Eigenmann 2007
- Eigenmann C, Colagiuri R. Outcomes and Indicators for Diabetes Education ‐ A National Consensus Position.. Diabetes Australia 2007;June:1‐54. [DOI] [PubMed] [Google Scholar]
Ellis 2004
- Ellis SE, Speroff T, Dittus RS, Brown A, Pichert JW, Elasy TA. Diabetes patient education: a meta‐analysis and meta‐regression. Patient Education & Counseling 2004;52(1):97‐105. [DOI] [PubMed] [Google Scholar]
Funnell 2004
- Funnell MM. Patient empowerment. Critical Care Nursing Quarterly 2004;27(2):201‐4. [DOI] [PubMed] [Google Scholar]
Glasgow 1999
- Glasgow R, Fisher E, Anderson B, LeGreca A, Marrero D, Johnson S, Rubin R, Cox D. Behavioural Science in Diabetes: Contributions and Opportunities. Diabetes Care 1999;22(5):832‐43. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analysis. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2005
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5 [updated May 2005]. In: The Cochrane Library, Issue 3, 2005. Chichester, UK: John Wiley & Sons, Ltd.
Holmes 2003
- Holmes J, Gear E, Bottomley J, Gillam S, Murphy M, Williams R. Do people with type 2 diabetes and their carers lose income? (T2ARDIS‐4). Health Policy 2003;64(3):291‐6. [DOI] [PubMed] [Google Scholar]
Jonsson 2002
- Jonsson B. Revealing the cost of Type II diabetes in Europe. Diabetologia 2002;45:S5‐S12. [DOI] [PubMed] [Google Scholar]
King 1998
- King H, Aubert R, Herman W. Global Burden of diabetes, 1995‐2025 prevalence, numerical estimates and projections. Diabetes care 1998;21:1414‐1431. [DOI] [PubMed] [Google Scholar]
Loveman 2003
- Loveman E, Royle P, Waugh N. Specialist nurses in diabetes mellitus. Cochrane Database of Systematic Reviews 2003, Issue 2. [DOI: 10.1002/14651858.CD003286] [DOI] [PMC free article] [PubMed] [Google Scholar]
Loveman 2008
- Loveman E, Frampton GK, Clegg AJ. The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review. The clinical effectiveness of diabetes education models for Type 2 diabetes: a systematic review.. Health Technol Assess Apr 2008;12(9):1‐136. [DOI] [PubMed] [Google Scholar]
Moher 1999
- Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta‐analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta‐analyses. Lancet 1999;354(9193):1896‐900. [DOI] [PubMed] [Google Scholar]
Norris 2001
- Norris SL, Engelgau MM, Narayan KMV. Effectiveness of self‐management training in type 2 diabetes. Diabetes Care 2001;24(3):561‐587. [DOI] [PubMed] [Google Scholar]
Vermeire 2003
- Vermeire E, Wens J, Royen P, Hernshaw H, Lindenmeyer A. Interventions for improving adherence to treatment recomendations in people with type 2 diabetes mellitus. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD003638.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 1980
- WHO Expert Committee on Diabetes Mellitus. Geneva: World Health Organisation, 1980. Second report. Technical Report Series 646. [PubMed]
WHO 1985
- WHO Expert Committee on Diabetes Mellitus. Geneva: World Health Organization, 1985. Technical Report Series 727.. [PubMed]
WHO 1998
- Alberti KM, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its compliactions. Part I: diagnosis and classification of diabetes mellitus. Provisional report of a WHO consultation. Diabetic Medicine 1998;15:539‐53. [DOI] [PubMed] [Google Scholar]
Wild 2004
- Wild S, Roglic G, Green A, Sicree R, King H. Global Prevalence of Diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047‐1053. [DOI] [PubMed] [Google Scholar]


