To the Editor:
Therapy advances have led to dramatic improvements in outcomes such that acute promyelocytic leukemia (APL) now represents one of the most curable forms of leukemia. Despite this, early death persists, with rates from 6% in clinical trials to 29% in population-based analyses.[1] We examined trends in early mortality and associated complications, sociodemographic and clinical factors among APL patients, stratified by age.
Patients >15 years of age diagnosed with a first primary APL and treated at a hospital in California from 1999–2014 were identified using linked data between California Cancer Registry (CCR) and California Office of Statewide Health Planning and Development Patient Discharge Database (PDD). The CCR contains sociodemographic and clinical information on all patients diagnosed with cancer in California. The PDD contains information about all hospitalizations including principal medical diagnoses and procedures. Our final cohort included 963 APL patients. The primary outcome was death within 7- and 30-days of APL diagnosis. Secondary outcomes were complications occurring during any hospitalization within 30 days of APL diagnosis. Chi-square tests were used to assess differences in complications and mortality by age-group. The Cochran-Armitage Trend Test evaluated changes of early mortality rates over time. Multivariate logistic regression analysis was used to determine the associations between sociodemographic and clinical factors, including complications, with 30-day mortality. Interactions by age were examined for each complication.
Most of the 963 APL patients were non-Hispanic white (48.0%) or Hispanic (31.6%), married (57.8%), lived in less affluent neighborhoods (59.7%), had private insurance (57.4%), and had ≥1 comorbidity (83.4%). Only 13.2% of the patients were treated at a National Cancer Institute (NCI)-designated cancer center. At 7 days from diagnosis, 16.7% (n=161) died; 27.2% (n=262) died within 30 days of diagnosis. Seven-day mortality decreased over time (19.8%, 1999–2002; 13.7%, 2011–2014; p for trend =0.02) with significantly higher rates of intracranial bleeding (79.5% vs. 36.1%) and respiratory failure (59.0% vs 36.1%) in those aged 15–39 who died compared to patients aged ≥60. Thirty-day mortality also improved (33.3%, 1999–2002; 22.74%, 2011–2014; p for trend < 0.01), with significantly higher rates of stroke (5.8% vs 1.8%), renal (24.2% vs 14.4%) and respiratory failure (22.7% vs 15.3%) in those aged ≥60 compared to younger patients. [Figure 1] In multivariable models, age ≥60 years (OR 6.25, CI 3.42–11.43), having ≥3 comorbidities (OR 3.08, CI 1.51–6.29), treatment at non-NCI cancer centers (OR 2.08, CI 1.03–4.19), intracranial bleeding (OR 12.13, CI 7.36–19.98), renal failure (OR 2.19, CI 1.35, 3.55) and respiratory failure (OR 8.49, CI 5.23–13.78) were associated with 30-day mortality. Race/ethnicity, marital status, neighborhood socioeconomic status, and health insurance were not significantly associated with 30-day mortality. In those aged 15–39, respiratory failure was associated with higher 30-day mortality compared to older patients.
Figure 1:
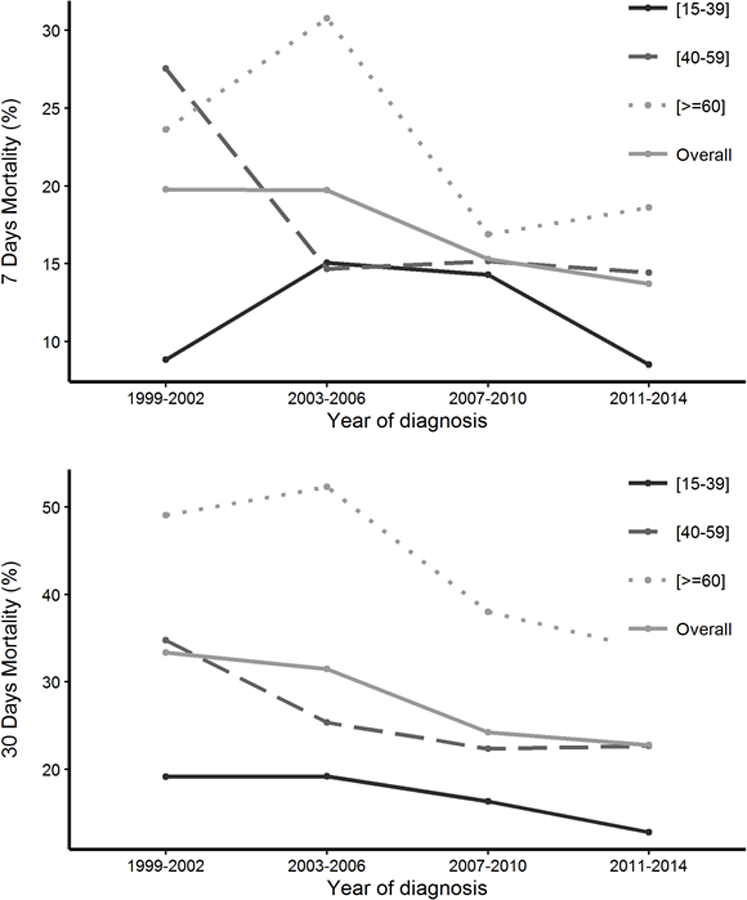
7-day and 30-day mortality in hospitalized acute promyelocytic leukemia patients by age at diagnosis (years), in California, 1999–2014
In a large, social and demographically diverse cohort of hospitalized APL patients, we found high early mortality rates, with nearly one-third of APL patients dying within 30 days of diagnosis, 61% of these died within the first seven days. Those aged ≥60 had the highest early death rates but also had the largest decrease in early mortality over time. While age, comorbidities and complications of intracranial bleeding, renal and respiratory failure continue to be major determinants of early death, we did not find significant disparities in early mortality by sociodemographic factors. Location of care played a role with improved outcomes seen in those treated at NCI-designated cancer centers. This study confirms that early mortality continues to be a primary reason for treatment failure in APL patients, and is significantly higher in population-based studies than patients enrolled in clinical trials.[2] Older age was a negative prognostic factor, though this group also experienced an improvement in early mortality over time. This may be due to newer strategies that depend on treatments that have more favorable toxicity profiles like arsenic trioxide.[3] Hemorrhagic complications, specifically intracranial bleeding, continue to impact all APL patients. In those that died within 7 days of diagnosis, 54% had intracranial bleeding events. Intracranial bleeding was also strongly associated with 30-day mortality in multivariate analysis. Our findings underscore the complex coagulopathy associated with APL and the impact of the acquired bleeding diathesis on early death. Strict monitoring and aggressive blood product support should be performed in all APL patients. Prompt identification and management of intracranial bleeding may also improve outcomes. Respiratory failure occurred in 20% of all APL patients within 30 days of diagnosis. In those that died within seven days, almost half had respiratory complications. We speculate that the high rates of respiratory failure may represent the development of differentiation syndrome, a potential life threatening adverse reaction. The ECOG-ACRIN EA9131 trial will assess whether a simplified patient care strategy with strict transfusion protocols and prophylactic steroids will lead to improvement in early mortality.[4]
Sociodemographic factors did not affect early mortality in our study, contrary to prior studies.[5] However, the location where a patient received care impacted early death, with better outcomes in those treated at NCI-designated centers. This may be due to better expertise and experience due to higher volumes of cases and access to clinical trial availability. [6] Future research should evaluate how differences in access to care and health care delivery at NCI-designated cancer centers lead to improved outcomes.
There are several limitations to this study. We did not have detailed information on laboratory measurements to risk stratify patients, types of chemotherapy used or timing of ATRA administration. Despite these limitations, our study includes a diverse patient population with findings that may be more generalizable of treatment and healthcare delivery. We observed that almost one-third of APL patients died within 30 days of diagnosis, the majority within the first seven days. Older age, comorbidities, treatment at non-NCI cancer centers and complications of intracranial bleeding, renal and respiratory failure were associated with higher early mortality. Because early mortality, not drug resistance, continues to be a major cause of treatment failure in APL patients, more robust initiatives to address these complications, including more aggressive supportive measures and universal prophylaxis of differentiation syndrome, may lead to better outcomes.
Acknowledgements
The collection of cancer incidence data used in this study was supported by the California Department of Public Health pursuant to California Health and Safety Code Section 103885; Centers for Disease Control and Prevention’s (CDC) National Program of Cancer Registries, under cooperative agreement 5NU58DP003862–04/DP003862; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the author(s) and do not necessarily reflect the opinions of the State of California, Department of Public Health, the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors.
BAJ is supported by the National Cancer Institute of the National Institutes of Health under Award Number K12CA138464. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
TW is supported by UL1 TR001860, NCATS, NIH
Footnotes
The authors declare no potential conflicts of interest.
REFERENCES:
- 1.Lehmann S, et al. , Continuing high early death rate in acute promyelocytic leukemia: a population-based report from the Swedish Adult Acute Leukemia Registry. Leukemia, 2011. 25(7): p. 1128–34. [DOI] [PubMed] [Google Scholar]
- 2.Park JH, et al. , Early death rate in acute promyelocytic leukemia remains high despite all-trans retinoic acid. Blood, 2011. 118(5): p. 1248–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang Y, et al. , Long-term efficacy and safety of arsenic trioxide for first-line treatment of elderly patients with newly diagnosed acute promyelocytic leukemia. Cancer, 2013. 119(1): p. 115–25. [DOI] [PubMed] [Google Scholar]
- 4.EA9131, E.A. https://clinicaltrials.gov/ct2/show/NCT03253848
- 5.Abrahao R, et al. , Disparities in early death and survival in children, adolescents, and young adults with acute promyelocytic leukemia in California. Cancer, 2015. 121(22): p. 3990–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ho G, et al. , Decreased early mortality associated with the treatment of acute myeloid leukemia at National Cancer Institute-designated cancer centers in California. Cancer, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]


