Abstract
Background
Maintaining high water intake reduces kidney stone recurrence, but is difficult to do. Strategies to reduce stone recurrence among adolescents are lacking.
Methods
We conducted an ecological momentary assessment study to identify factors associated with water intake among 25 adolescents with nephrolithiasis. Over 7-days, participants used smart bottles to self-monitor water intake and received questionnaires randomly four times daily that were completed in real-time on mobile devices. The questionnaires ascertained awareness of water intake volume, awareness of water intake goals, perceived need to drink, access to water, alternative beverage consumption, and attitudes towards bathrooms. Linear mixed-effects models were fit to estimate the association between momentary responses and daily water intake.
Results
Over 175 person-days, 595 (85%) assessments were completed. Median daily water intake was 1304mL (IQR 848–1832); 20% of participants met their intake goal for ≥4 days. Unawareness of water intake volume was associated with drinking 690mL less water a day (p=0.04). A strong self-perceived need to drink more was associated with drinking 1954 mL less water each day compared to no need to drink more (p<0.01). Unawareness of intake goals was weakly associated with drinking 1129 mL less water each day(p=0.1). Access to water, alternative beverage consumption, and bathroom aversion were not associated with water intake.
Conclusions
Unawareness of water volume consumed and low responsiveness to the perceived need to drink more were associated with low water intake. Interventions that help adolescents recognize when and identify how to increase water intake may be effective in reducing stone recurrence.
Keywords: nephrolithiasis, behaviors, water intake, ecological momentary assessment, adolescents
Introduction
Kidney stone (nephrolithiasis), which results in annual healthcare costs exceeding $10 billion, is associated with increased risks of chronic kidney disease and fracture.1 Since the 1990s, the prevalence of nephrolithiasis in the United States has increased by 70%.2 The greatest increases have been observed among adolescents, among whom the incidence doubled between 1997 and 2012.3 For patients who develop nephrolithiasis in childhood, approximately 50% will have a symptomatic recurrence within three years.4 However, little is known about secondary prevention strategies to reduce stone recurrence among adolescents.
High fluid intake is associated with a decreased risk of incident and recurrent nephrolithiasis.5–7 Although guidelines do not recommend a specific fluid type to reduce recurrence, many beverages are unsuitable for adolescents (e.g. alcoholic beverages). Additionally, sugary drinks, the consumption of which is high amongst adolescents, increase urine calcium and have been associated with an increased risk of incident nephrolithiasis.8 Water, therefore, is considered the ideal fluid to prevent stone recurrence in childhood. However, drinking enough water to decrease recurrence is difficult. Among adults with nephrolithiasis, the average increase in 24-hour urine volume after recommendations to maintain high fluid intake is only 300mL.9 Among children, 75% of 9–18 year olds have insufficient daily water intake.10
No studies have examined water drinking behaviors among adolescents with kidney stones. Identifying potential barriers and facilitators of water intake will inform strategies to decrease stone recurrence throughout the lifetime. We hypothesized that unawareness of water goals and aversion to bathrooms would be associated with lower water intake.
Methods
Study Design and Population
We conducted an ecological momentary assessment (EMA) study to identify factors associated with daily water intake among adolescents with nephrolithiasis. EMA is a study design in which real-time data is collected in real-world environments at multiple points during the day. The study period was 7 consecutive days, a typical study period in EMA research11 that ensured coverage of weekdays and weekends.
Twenty-six patients aged 12–18 years with at least one prior kidney stone of any composition except stones caused by infection (e.g. struvite) were enrolled at visits to the Kidney Stone Center at The Children’s Hospital of Philadelphia between June 2016 and April 2017. To capture heterogeneity in time, temperature, and place, ≤7 participants completed the study during a 3-month season. We excluded patients who did not speak English, could not operate mobile devices, or who had conditions causing increased fluid loss (e.g. chronic diarrhea) or changes in dietary intake (e.g. gastric bypass).
As part of clinical care, patients had been provided a personalized daily water intake goal per National Academy of Medicine recommendations for adequate daily water intake (e.g. 2,640mL for a 16-year-old boy).12 These recommendations, which consider water from food and other beverages, were used as the daily goal because higher than adequate fluid intake is needed to maintain urine volume sufficient to decrease recurrence risk and specific 24-urine volumes guidelines do not exist for pediatric patients.13 We did not include a wash-in period in order to best capture the natural variation in water intake that occurs after these recommendations. This study was approved by the local institutional review board.
Ecological Momentary Assessments
We developed a 2-minute EMA questionnaire (LifeData)14 that assessed: 1) awareness of water intake volume, 2) awareness of water intake goals, 3) perceived need to drink, 4) access to water, 5) alternative beverage consumption, and 6) attitudes towards bathrooms (Appendix). We tested the face validity, comprehensiveness, and interpretability of the questionnaire among 10 adolescents with nephrolithiasis, and revised it based on their feedback.
During the 7-day study period, prompts to complete the EMA questionnaire were sent to participants’ mobile devices at random times four times daily. Participants completed the assessments on their mobile devices and had 45 minutes to complete the assessment after receiving the prompt in order to allow participants to respond on a break if they received the prompt during class.14 Participants completed baseline and end-of-study questionnaires. We requested permission for study participation during school. Participants received $100 if they completed ≥85% of the EMAs.
Outcomes
The primary outcomes were daily water intake volume (mL) and the proportion of the personalized daily water intake goal met (%), which normalizes water intake across age and sex. The secondary outcome was meeting the daily intake goal ≥4 days. Participants were provided a smart bottle (HidrateSpark) to measure water intake. HidrateSpark allows accurately measures fluid intake through real-time data transfer to mobile devices.15 Participants were instructed to drink all water from the bottle during the study period. Participants recorded the volume and timing of water not consumed from HidrateSpark using the mobile device app. Participants were allowed to drink other beverages, but the volume of alternative beverages was not measured.
Statistical Analysis
We used linear mixed-effects models to estimate the association between EMA domains and daily water intake. We fit separate models for each domain, using water volume consumed since the previous prompt as the outcome. Each model included a random intercept for each patient and adjusted for age, sex, prior kidney stone surgery, prior kidney stone passage, weekday indicator, and time of prompt (morning, noon, afternoon, evening). For models assessing awareness, interaction terms for prior stone surgery and stone passage were included to evaluate whether these events modified the association between awareness of intake volume, awareness of intake goals, and actual water intake.
Because the outcome of clinical interest was daily water intake, we used the results of the mixed-effects models to evaluate differences in daily water intake between the levels of agreement for each EMA domain (Appendix). Model coefficients were used to estimate water intake volume since the last prompt and summed within days to obtain daily volume estimates for each patient. We assumed participants responded to every questionnaire and were followed for the entire week. Under these conditions, we estimated daily water intake assuming the whole cohort was exposed and then assuming the whole cohort was not exposed (i.e. responded the same way to each EMA question). In this way, we compared average daily water intake, proportion of the daily water goal met, and the proportion of individuals meeting their daily water intake goals ≥4 days by exposure groups. We thus obtained a distribution of daily water volumes for each person assuming they always responded affirmatively to each response option. We performed a sensitivity analysis excluding manually-added water volume. P-value <0.05 was the threshold for statistical significance. Analyses were performed in R v3.3.3.
Results
Patient Characteristics
Twenty-five of 26 participants enrolled had analyzable data and were followed for 175 person-days. One participant’s device did not reliably sync with HidrateSpark and was thus excluded. The response rate to the EMA prompts was 85% (595/700).
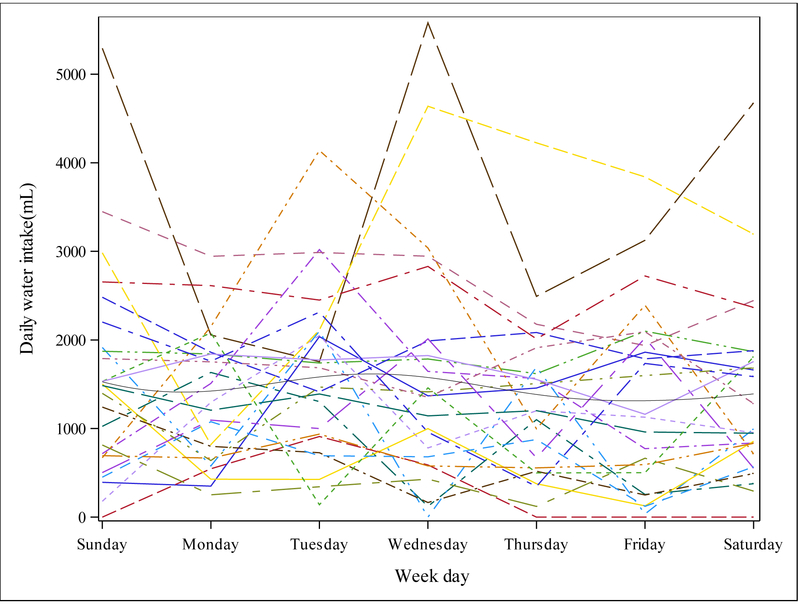
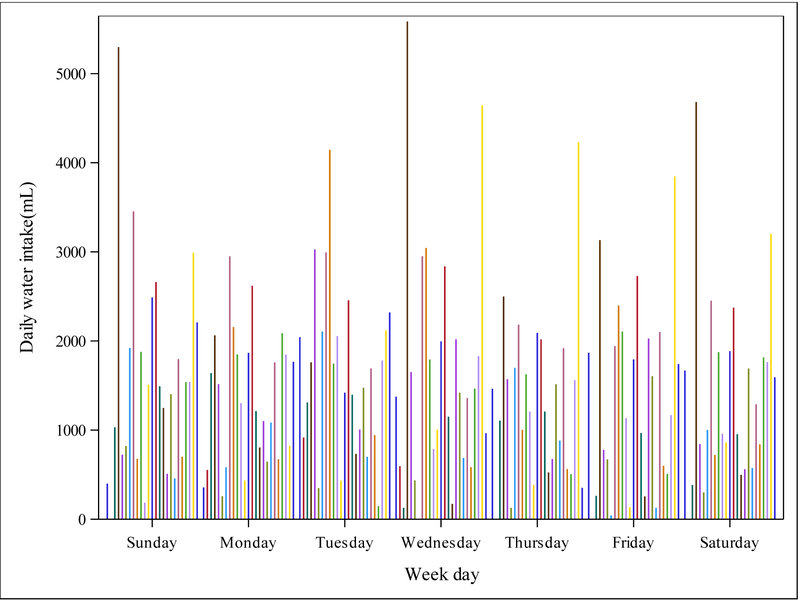
Median daily water intake was 1304mL (IQR 848–1832) and the median proportion of the daily water goal met was 66% (IQR 32–98%). Five participants (20%) met their water goal ≥4 days. The median daily water intake of participants who did and did not meet their water goal ≥4 days was 2698mL and 1175mL, respectively (Table 1). Most water consumption occurred in the early afternoon and evening, with similar daily intake across the study period (Figure 1; Appendix). There was no evidence that EMA prompts increased water intake, with sips equally distributed before and after the prompt (Appendix).
Table 1:
Characteristics of Participants Who Did and Did Not Achieve Daily Water Intake Goals for ≥4 days
| Characteristic | Overall N=25 |
Met Goal N=5 |
Did Not Meet Goal N=20 |
|---|---|---|---|
| Daily water intake, median (IQR) | 1304 (848, 1832) | 2698 (1928, 3116) | 1175 (694, 1498) |
| Age, median (IQR) | 16 (15, 17) | 16 (16, 17) | 16 (15, 17) |
| Sex, No. (%) | |||
| Female | 15 (60) | 4 (80) | 11 (55) |
| Male | 10 (40) | 1 (20) | 9 (45) |
| Race, No. (%) | |||
| Black | 3 (12) | - | 3 (15) |
| White | 22 (88) | 5 (100) | 17 (85) |
| Ethnicity, No. (%) | |||
| Missing | 4 (16) | - | 4 (20) |
| Non-Hispanic | 21 (84) | 5 (100) | 16 (80) |
| BMI, median (IQR) | 22 (19, 26) | 27 (18, 27) | 22 (20, 24) |
| Family encourage water intake, No. (%) | |||
| Always | 10 (40) | 2 (40) | 8 (40) |
| Neutral | 1 (4) | - | 1 (5) |
| Never | 1 (4) | - | 1 (5) |
| Often | 8 (32) | 2 (40) | 6 (30) |
| Sometimes | 5 (20) | 1 (20) | 4 (20) |
| Prior kidney stone passage, No. (%) | |||
| No | 6 (24) | 1 (20) | 5 (25) |
| Yes | 19 (76) | 4 (80) | 15 (75) |
| Prior kidney stone surgery, No. (%) | |||
| No | 17 (68) | 1 (20) | 16 (80) |
| Yes | 8 (32) | 4 (80) | 4 (20) |
| Sports participation, No. (%)* | |||
| No | 11 (44) | 3 (60) | 8 (40) |
| Yes | 14 (56) | 2 (40) | 12 (60) |
| Believes drinking water prevents kidney stones, No. (%) | |||
| Disagree/strongly disagree | 1 (4) | - | 1 (5) |
| Neutral | 4 (16) | 2 (40) | 2 (10) |
| Strongly agree/agree | 20 (80) | 3 (60) | 17 (85) |
Sports participation was not classified into organized sports, any sports participation, or whether they were actively participating at the time of the EMA study.
Figure 1. Mean daily water intake for each day of the 7-day study period, by participant.
Each light grey line represents an individual participant. The dark grey line is the mean daily water intake for the 25 participants. Mean daily water intake for the entire cohort was similar across the study period with no observable differences between weekday and weekend days.
Patient factors and water intake
Participants who had prior stone surgery drank an estimated 941mL more per day than those who never had surgery (95% CI: 162–1721). Kidney stone passage was not associated with higher daily water intake (difference 404mL; 95% CI: −437–1318).
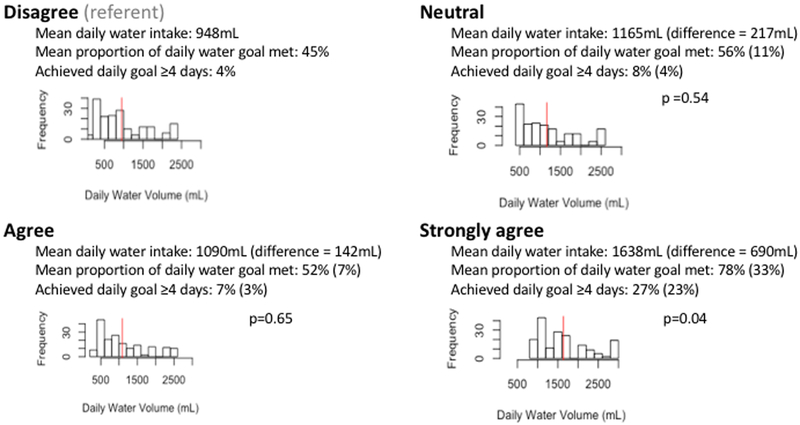
Participants who reported unawareness of water intake volume drank an estimated 690mL less water each day than who were strongly aware (p=0.04; Figure 2). Prior kidney stone surgery or passage did not modify the association between awareness of water intake and water intake (p=0.1 for surgery interaction, p=0.61 for passage interaction).
Figure 2. Association between awareness of amount of water consumed and daily water intake.
Linear mixed-effects models were used to determine the association between momentary awareness of water intake volume on a Likert scale and daily water intake. Models included a random intercept for each patient and adjusted for age, sex, weekday indicator, time of prompt (morning, noon, afternoon, evening), and prior kidney stone passage or surgery. We assumed every participant always responded affirmatively to each level of agreement with the statement: “I know how many glasses of water I have drunk today (or how many bottles of HidrateSpark I have drunk today.” to estimate daily water intake, proportion of daily water goal met, and proportion of participants who met the daily water goal ≥4 days. The histograms represent the frequency of estimated daily water intake volume for each level of agreement. The reported differences and p-values reflect comparisons of estimated daily water intake for each level of agreement with “disagree”.
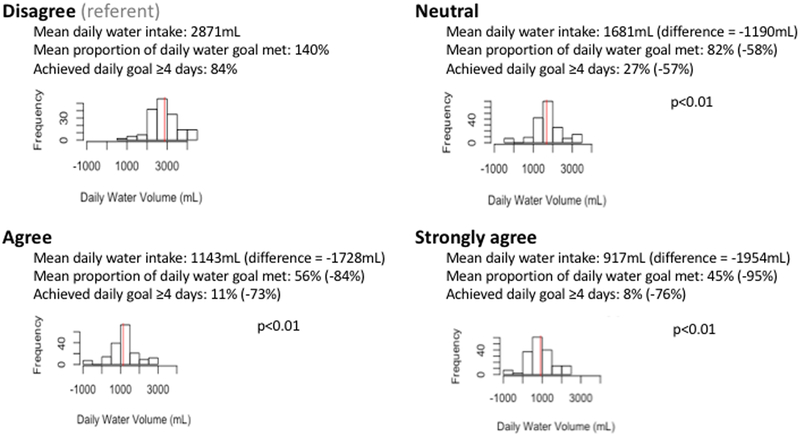
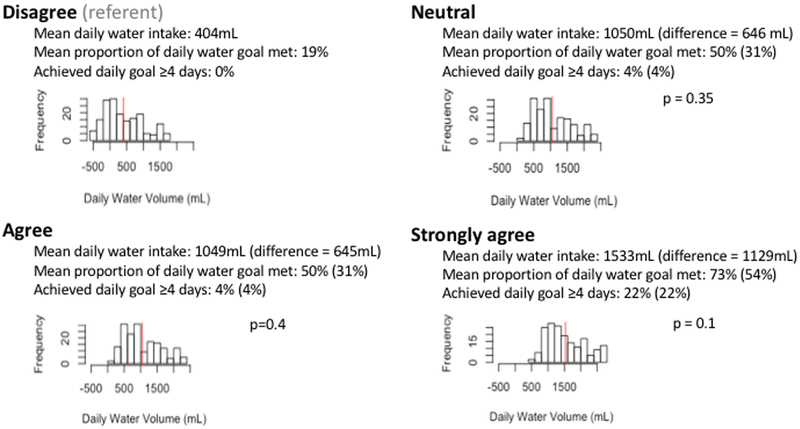
Participants who reported strong self-perceived need to drink more consumed an estimated 1954mL less water each day than those who reported no need to drink more (p<0.01; Figure 3). Unawareness of intake goals was weakly associated with lower water intake (p=0.1; Figure 4). We could not examine interactions between awareness of intake goals and prior surgery or stone passage because all participants who had surgery or passed a stone reported knowing how much they were supposed to drink. Access to water, alternative beverage consumption, and aversion to nearby bathrooms were not associated with water intake (Appendix). The results did not change after excluding water not consumed from HidrateSpark.
Figure 3. Association between perceived need to drink more and daily water intake.
Linear mixed-effects models were used to determine the association between momentary perceived need to drink more on a Likert scale and daily water intake. Models included a random intercept for each patient and adjusted for age, sex, weekday indicator, time of prompt (morning, noon, afternoon, evening), and prior kidney stone passage or surgery. We assumed every participant always responded affirmatively to each level of agreement with the statement: “I need to drink more water than I have today.” to estimate daily water intake, proportion of daily water goal met, and proportion of participants who met the daily water goal ≥4 days. The histograms represent the frequency of estimated daily water intake volume for each level of agreement. The reported differences and p-values reflect comparisons of estimated daily water intake for each level of agreement with “disagree”.
Figure 4. Association between awareness of water intake goals and daily water intake volume.
Linear mixed-effects models were used to determine the association between momentary awareness of daily water intake goals on a Likert scale and daily water intake. Models included a random intercept for each patient and adjusted for age, sex, weekday indicator, time of prompt (morning, noon, afternoon, evening), and prior kidney stone passage or surgery. We assumed every participant always responded affirmatively to each level of agreement with the statement: “I know how much water I am supposed to drink today.” to estimate daily water intake, proportion of daily water goal met, and proportion of participants who met the daily water goal ≥4 days. The histograms represent the frequency of estimated daily water intake volume for each level of agreement. The reported differences and p-values reflect comparisons of estimated daily water intake for each level of agreement with “disagree”
In the 8 assessments during which respondents reported being thirsty but unwilling to drink the water nearby, the reason most commonly reported was water not being cold (n=5; 63%). The remainder reported the water or water source was dirty/gross (n=3; 38%). An alternative beverage was consumed in 27% of assessment periods.
Post-study evaluation (Appendix)
Most participants (82%) agreed or strongly agreed that the smart bottle was easy to use and helped them drink water and 79% had the bottle with them at the time of the EMA prompt. The interventions that participants reported would have increased their water intake were: preventing another kidney stone (86%), financial incentive (45%), and reaching their personal water goal (41%). Only 14% reported that scolding would improve adherence.
Discussion
In this study, the median proportion of the daily water intake goal met was 66% and the median daily water intake of 1304mL was less than the daily goal for even the youngest participants. Despite provision of water intake goals, education about the importance of water, and providing a smart bottle, only 20% of participants met their daily goal for most of the study period, suggesting that knowledge and self-monitoring of water intake alone are insufficient to change behavior. We found that momentary unawareness of the amount of water consumed was associated with lower total daily water intake and lower achievement of water intake goals. In addition, adolescents reporting a strong need to drink more consumed less water. This result suggests that there is a disconnect between understanding the benefits of water intake and responding appropriately. Contrary to our hypotheses, we found no evidence that aversion to bathrooms and alternative beverage consumption (surprising low in this population) were associated with water intake. These findings have relevance to developing strategies to maintain high water intake to decrease kidney stone recurrence.
The shift of the onset of nephrolithiasis to childhood presents substantial challenges and opportunities to decrease the lifetime burden of kidney stone disease. Adolescents will likely experience more recurrent stone events than those who develop nephrolithiasis as adults. However, adolescents also may be more receptive to changing behaviors, such as increasing water intake, that decrease stone recurrence.16 Insufficient water intake is a common risk factor for nephrolithiasis, with most adult patients neither meeting urine output goals nor substantially increasing fluid intake despite education of its benefits.9 Barriers to maintaining high fluid among adults with nephrolithiasis include not understanding the benefits of fluid intake, not remembering to drink, and desire not to void frequently.17 Our results indicate that unawareness of water volume consumed and low responsiveness to the perceived need to drink more are barriers for maintaining high water intake among adolescents with nephrolithiasis.
These unique barriers may be due to differences in cognitive control, decision making processes,18 and daily activities. These differences may also be due to features of our study design that allowed us to more accurately ascertain factors in daily lives associated with water intake. First, we used EMA to assess patients’ awareness and attitudes, which change over the course of the day. The focus on momentary assessment—collecting data about what is going on at the moment or over the recent past—provides advantages over interviews or surveys, by overcoming recall bias and allowing for the understanding of how time, context, and place influences behaviors. Second, we used a smart bottle to measure water intake. This method, which was highly endorsed by participants, accurately measured the volume and timing of water intake, and eliminated recall and misclassification bias.
These results can be used to design interventions that increase self-awareness of water intake and improve responses to the perceived (correct) need to drink more water. Financial incentives to meet daily fluid intake goals could potentially increase awareness of water consumed.19 Financial incentives leverage present bias (tendency to focus on the present and heavily discount the future) through regular, ongoing positive reinforcement, thereby shifting focus from a possible future event (stone recurrence) to an immediately achievable goal.20 Financial incentives have improved glucose monitoring adherence among adolescents21 and smoking cessation and weight loss among adults.22, 23 Social incentives (e.g. competition to achieve intake goals) operate similarly. However, such incentives alone may be insufficient to maintain high fluid intake over the lifetime since behaviors may reverse after incentives are withdrawn.24 Problem-solving skills training may be an important adjuvant to education and financial incentives, and has been shown to increase fluid intake for younger children with constipation,25 weight loss among women,26 and medication adherence among adolescents with inflammatory bowel disease.27 Problem-solving that helps patients identify when and how to increase water intake (e.g. identification of individual barriers to water intake and development of feasible solutions to overcome them) may be particularly effective in helping adolescents respond appropriately to the self-perceived need to drink more. The efficacy of financial incentives and problem solving in maintaining high fluid intake to decrease stone recurrence are being tested in the ongoing Prevention of Urinary Stones with Hydration (PUSH) trial conducted by NIDDK-supported Urinary Stone Disease Research Network.28 Pending these results, the results from this study support counseling patients that they should be aware how much they actually drink each day and should respond to the need to drink more.
Strengths of the study include high completion of momentary assessments, consistent with prior EMA studies.29 We also had excellent retention, which is likely due to the short, but intensive, evaluation period for EMA studies,30 use of short assessments, and appeal of technology to adolescents. Limitations include the possibility that EMA responses did not accurately reflect participants’ states throughout the period over which water consumption was measured. Second, participants knew their water consumption was being measured and that the purpose of the EMA prompts was to identify factors associated with water intake. However, we did not observe tapering of water intake over the one-week study period, which suggests any Hawthorne effect was minimal. Additionally, participants generally did not drink a lot of water and there was no evidence that prompts acted as a reminder to drink water. Third, we only measured water intake and did not account for fluid volume contributed by alternative beverages or foods. Future studies are needed to identify the optimal fluid intake program for adolescents with nephrolithiasis. We also did not measure urine output, which mediates the effect of high fluid intake on stone recurrence. Finally, larger samples and longer assessment periods are needed to increase generalizability and to explore how prior experiences such at the time since the stone event may modify water intake.
Conclusions
Among adolescents with nephrolithiasis, unawareness of water volume consumed and low responsiveness to the perceived need to drink more were associated with low water intake. Future trials should test whether interventions that help adolescents recognize when and identify how to increase water intake decrease kidney stone recurrence.
Supplementary Material
Funding source:
The study was supported by the National Institute for Diabetes and Digestive Diseases and Kidney Diseases (NIDDK) of the National Institutes of Health (NIH) (K23-DK106428 to GET. GET and SLF were supported by grants K23DK106428 and K24-DK078737, respectively, from the NIDDK. The NIH provided financial support for data management and analysis, but had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The views expressed in this article are those of the authors and do necessarily represent the official view of the NIDDK.
Financial Disclosure:
The authors have no financial relationships relevant to this article to disclose. HidrateSpark bottles were purchased using grant funds and provided to the study participants. There is no financial or consulting relationship between any investigators and HidrateSpark.
Bibliography
- 1.Denburg MR, Jemielita TO, Tasian GE et al. : Assessing the risk of incident hypertension and chronic kidney disease after exposure to shock wave lithotripsy and ureteroscopy. Kidney Int, 89: 185, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scales CD Jr., Smith AC, Hanley JM et al. : Prevalence of kidney stones in the United States. Eur Urol, 62: 160, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tasian GE, Ross ME, Song L et al. : Annual Incidence of Nephrolithiasis among Children and Adults in South Carolina from 1997 to 2012. Clin J Am Soc Nephrol, 11: 488, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tasian GE, Kabarriti AE, Kalmus A et al. : Kidney Stone Recurrence among Children and Adolescents. J Urol, 197: 246, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pearle MS, Goldfarb DS, Assimos DG et al. : AUA GuidelinesMedical Management of Kidney Stones: AUA Guideline In: JURO: Elsevier Ltd, vol. 192, pp. 316–324, 2014 [DOI] [PubMed] [Google Scholar]
- 6.Borghi L, Meschi T, Amato F et al. : Urinary volume, water and recurrences in idiopathic calcium nephrolithiasis: a 5-year randomized prospective study. J Urol, 155: 839, 1996 [PubMed] [Google Scholar]
- 7.Curhan GC, Willett WC, Rimm EB et al. : Prospective study of beverage use and the risk of kidney stones. Am J Epidemiol, 143: 240, 1996 [DOI] [PubMed] [Google Scholar]
- 8.Taylor EN, Curhan GC: Fructose consumption and the risk of kidney stones. Kidney International, 73: 207, 2008 [DOI] [PubMed] [Google Scholar]
- 9.Parks JH, Goldfischer ER, Coe FL: Changes in urine volume accomplished by physicians treating nephrolithiasis. J Urol, 169: 863, 2003 [DOI] [PubMed] [Google Scholar]
- 10.Kant AK, Graubard BI: Contributors of water intake in US children and adolescents: associations with dietary and meal characteristics--National Health and Nutrition Examination Survey 2005–2006. Am J Clin Nutr, 92: 887, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grenard JL, Stacy AW, Shiffman S et al. : Sweetened drink and snacking cues in adolescents: a study using ecological momentary assessment. Appetite, 67: 61, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate: The National Academies Press, 2005 [Google Scholar]
- 13.Lande MB, Varade W, Erkan E et al. : Role of urinary supersaturation in the evaluation of children with urolithiasis. Pediatr Nephrol, 20: 491, 2005 [DOI] [PubMed] [Google Scholar]
- 14.Runyan JD, Steenbergh TA, Bainbridge C et al. : A smartphone ecological momentary assessment/intervention “app” for collecting real-time data and promoting self-awareness. PLoS One, 8: e71325, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borofsky MS, Dauw CA, York N et al. : Accuracy of daily fluid intake measurements using a “smart” water bottle. Urolithiasis, 2017 [DOI] [PubMed] [Google Scholar]
- 16.Jackson E: Between a Rock and a Hard Place: Getting Families to Change Behaviors to Reduce Pediatric Stone Disease Recurrence. J Urol, 2014 [DOI] [PubMed] [Google Scholar]
- 17.McCauley LR, Dyer AJ, Stern K et al. : Factors influencing fluid intake behavior among kidney stone formers. J Urol, 187: 1282, 2012 [DOI] [PubMed] [Google Scholar]
- 18.Kar BR, Vijay N, Mishra S: Development of cognitive and affective control networks and decision making. Prog Brain Res, 202: 347, 2013 [DOI] [PubMed] [Google Scholar]
- 19.Loewenstein G, Brennan T, Volpp KG: Asymmetric paternalism to improve health behaviors. JAMA, 298: 2415, 2007 [DOI] [PubMed] [Google Scholar]
- 20.Ted OD, Matthew R: The economics of immediate gratification. Journal of Behavioral Decision Making, 13: 233, 2000 [Google Scholar]
- 21.Wong CA, Miller VA, Murphy K et al. : Effect of Financial Incentives on Glucose Monitoring Adherence and Glycemic Control Among Adolescents and Young Adults With Type 1 Diabetes: A Randomized Clinical Trial. JAMA Pediatr, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Volpp KG, John LK, Troxel AB et al. : Financial incentive-based approaches for weight loss: a randomized trial. JAMA, 300: 2631, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Volpp KG, Troxel AB, Pauly MV et al. : A randomized, controlled trial of financial incentives for smoking cessation. N Engl J Med, 360: 699, 2009 [DOI] [PubMed] [Google Scholar]
- 24.Patel MS, Asch DA, Rosin R et al. : Framing Financial Incentives to Increase Physical Activity Among Overweight and Obese Adults: A Randomized, Controlled Trial. Ann Intern Med, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuhl ES, Hoodin F, Rice J et al. : Increasing daily water intake and fluid adherence in children receiving treatment for retentive encopresis. J Pediatr Psychol, 35: 1144, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murawski ME, Milsom VA, Ross KM et al. : Problem solving, treatment adherence, and weight-loss outcome among women participating in lifestyle treatment for obesity. Eat Behav, 10: 146, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greenley RN, Kunz JH, Biank V et al. : Identifying youth nonadherence in clinical settings: data-based recommendations for children and adolescents with inflammatory bowel disease. Inflamm Bowel Dis, 18: 1254, 2012 [DOI] [PubMed] [Google Scholar]
- 28.Prevention of Urinary Stones With Hydration (PUSH). ClinicalTrials.gov: U.S. National Library of Medicine, 2017 [Google Scholar]
- 29.Gwaltney CJ, Bartolomei R, Colby SM et al. : Ecological momentary assessment of adolescent smoking cessation: a feasibility study. Nicotine Tob Res, 10: 1185, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Courvoisier DS, Eid M, Lischetzke T: Compliance to a cell phone-based ecological momentary assessment study: the effect of time and personality characteristics. Psychol Assess, 24: 713, 2012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.