Abstract
Objective:
Discharge to skilled nursing facilities (SNF) is common in patients with heart failure (HF). It is unknown whether the transition from SNF to home is risky for these patients. Our objective was to study outcomes for the 30 days after discharge from SNF to home among Medicare patients hospitalized with HF who had subsequent SNF stays of 30 days or less.
Design:
Retrospective cohort study.
Setting and Participants:
All Medicare fee-for-service beneficiaries 65 and older admitted 2012 to 2015 with a HF diagnosis discharged to SNF then subsequently discharged home.
Measures:
Patients were followed for 30 days following SNF discharge. We categorized patients by SNF length of stay: 1-6 days, 7-13 days, 14-30 days. For each group, we modeled time to a composite outcome of unplanned readmission or death after SNF discharge. Our model examined 0-2 days and 3-30 days post-SNF discharge.
Results
Our study included 67,585 HF hospitalizations discharged to SNF and subsequently discharged home. Overall, 16,333 (24.2%) SNF discharges to home were readmitted within 30 days of SNF discharge. The hazard rate of the composite outcome for each group was significantly increased on days 0-2 after SNF discharge compared to days 3-30, as reflected in their hazard rate ratios: for patients with SNF length of stay 1-6 days, 4.60 (4.23-5.00), SNF length of stay 7-13 days, 2.61 (2.45-2.78), SNF length of stay 14-30 days, 1.70 (1.62-1.78).
Conclusions/Implications
The hazard rate of readmission after SNF discharge following HF hospitalization is highest during the first 2 days home. This risk attenuated with longer SNF length of stay. Interventions to improve post-discharge outcomes have primarily focused on hospital discharge. This evidence suggests that interventions to reduce readmissions may be more effective if they also incorporate the SNF-to-home transition.
Keywords: readmission, post-acute care, skilled nursing facility, heart failure, hospitalization
Brief summary:
Discharge from hospital to skilled nursing facility (SNF) is common in heart failure patients. The 30-day readmission risk during the transition from SNF to home is almost 25%. Readmission risk decreases as SNF length of stay increases.
Introduction
Discharge from hospital to skilled nursing facility (SNF) is common in patients with heart failure (HF), occurring in 1 in 5 Medicare beneficiaries.1 SNFs are often used as a transition from hospital to home to regain strength, function, and independence, particularly for medically complex patients. Discharge home from SNF is often the ultimate goal, as the vast majority of these patients were residing at home prior to hospitalization.1 However, these are vulnerable patients,1, 2 and SNF stays add another layer of complexity to the final transition back to the community. While the level of care at a SNF is less intense than in an inpatient facility, they are still medical settings with daily nursing care and physician oversight. During this SNF stay, new medications may be started, medication adjustments may occur, and lab tests may be obtained, which may be still pending at time of SNF discharge.
While several studies have examined the transition from hospital to home among patients with HF,3–7 much less is known about transitions from SNF to home, including associated risks of readmission and mortality. As Medicare pays for SNF at full cost only for the first 20 days8 after hospital discharge, many patients may be discharged on day 21, a time period within the 30-day readmission window of interest to health care systems trying to avoid readmission penalties. Furthermore, in October 2018, the Centers for Medicare and Medicaid (CMS) implemented the Skilled Nursing Facility Value-Based Purchasing Program, which offers Medicare incentive payments to SNFs paid under the SNF Prospective Payment System related to performance on specified measures of readmissions.9 Thus, understanding the risk trajectories associated with the transition from SNF to home is important on multiple fronts.
Accordingly, our objective was to study outcomes for the 30 days after discharge from SNF to home among Medicare patients hospitalized with HF who had subsequent SNF stays of 30 days or less. We hypothesized that this transition is associated with a risk of hospital readmission.
Methods
Study sample
This was a retrospective cohort study of all Medicare fee-for-service (FFS) beneficiaries 65 and older admitted from July 2012 to June 2015 with a principal discharge diagnosis of HF as defined by CMS for hospital quality measurement.10, 11 Medicare Standard Analytic Files identified admissions to acute care hospitals and skilled nursing facilities, and provided readmission data for up to one year after discharge from each index hospitalization. These were merged with Medicare Denominator Files containing information on patient-level characteristics including date of birth, sex, and race.12 American Hospital Association 2012 survey data were linked to provide information on hospital-level characteristics, such as size of index hospital. To focus on the transition to home that occurs after a temporary SNF stay, we excluded patients remaining in SNF more than 30 days after hospital discharge (n=13,139). We also excluded admissions with less than one day in SNF (n=17) and hospital admissions initially admitted from SNF (n=84), as the former often represents patients without a true SNF stay and the latter long-term SNF patients.
Outcomes
Readmission Timing:
In order to examine readmission patterns among homogenous sets of patients to inform our final model, 30 cohorts were created for patients with SNF stays of 1 to 30 days, respectively. We then plotted the percentage of readmissions that occurred on each day (0-30) after discharge from SNF for each of these cohorts.
Readmission Risk:
Our primary event of interest was time from SNF discharge to home to a composite outcome of unplanned readmission or death within 30 days after discharge from SNF to home. Planned readmissions as defined by Horwitz et al.10 were censored. Secondary outcome was time to unplanned readmission as its own outcome. In this second model, planned readmission and death were considered competing risks.
Statistical Analysis
Study population characteristics were summarized with descriptive analyses. Next, for each of the 30 cohorts defined by the number of SNF days, we used violin plots to illustrate the probability density of 30-day readmissions that occurred on each day (0-30) after discharge from SNF to home for a descriptive analysis of the timing of readmission.
Readmission patterns qualitatively appeared to be different for patients with a SNF length of stay of 1-6 days, 7-13 days, and 14-30 days, respectively. We then visually examined readmission risk in each of the three groups by plotting the log probability of being free of readmission over time. We observed two qualitatively different hazards for two separate time intervals (0-2 days and 3-30 days). As a result, we utilized piecewise exponential Bayesian models to partition the time scale in order to estimate baseline hazard of readmission for these time periods separately.13–16 Thus in our main analysis of the composite outcome of readmission risk and death after discharge from SNF to home, multivariable piecewise exponential Bayesian models were estimated separately for those three groups. These models controlled for age, sex, race, Elixhauser comorbidity score, length of SNF stay, Medicaid dual-eligibility, bed size of index hospital, urban versus rural hospital, and teaching versus non-teaching hospital. Elixhauser comorbidity score was calculated using ICD codes associated with the index hospitalization. Medicaid dual-eligibility was calculated using patient-level data from the Medicare Denominator Files. Length of SNF stay was calculated using Medicare data from the associated SNF stay. We reported the hazard rate and credible interval of the composite outcome and readmission for each time interval. Analyses were conducted using SAS 9.4 (SAS Institute, Cary, NC). The need to obtain informed consent was waived by our institutions, both of which provided approval for the overall study.
Results
Figure 1 illustrates a flow chart of our cohort selection. Our study included 67,585 HF hospitalizations that were discharged to SNF and subsequently discharged home (median age, 84 years [IQR; 78-89]; female, 61.0%); 13,257 (19.6%) were discharged from SNF with home care, 54,328 (80.4%) without. Median length of SNF admission was 17 days (IQR; 11-22) (Table 1). In total, 16,333 (24.2%) SNF discharges to home were readmitted within 30 days of SNF discharge; median time to readmission for those readmitted up to 30 days was 10 days (IQR; 3-18). Overall median time to readmission was 48 days (IQR; 14-121).
Figure 1:
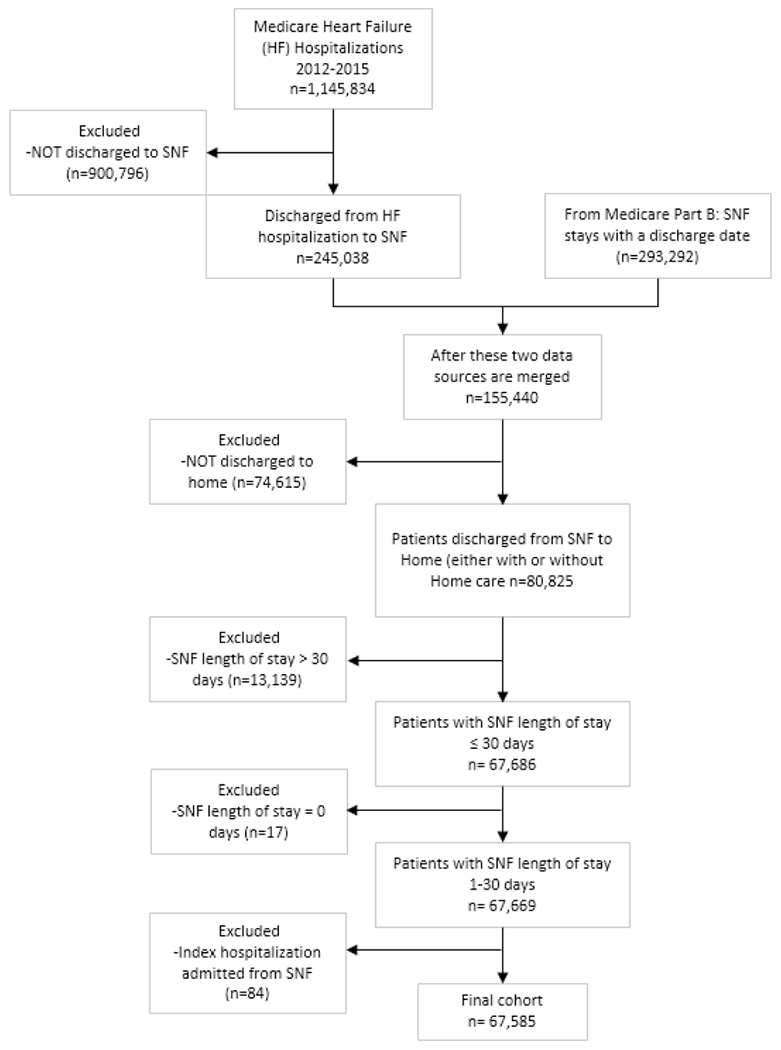
Flow chart for cohort selection
Table 1:
Characteristics of Those Discharged Home from SNF Following HF Hospitalization
| Characteristic | n=67,585 |
|---|---|
| Age, Median (IQR) | 84 (78-89) |
| Male | 26386 (39.0%) |
| Race | Race |
| White | 60084 (88.9%) |
| Black | 5467 (8.1%) |
| Other | 2034 (3.0%) |
| Length of stay in hospital, Median (IQR) | 7.0 (5.0-9.0) |
| Length of stay in SNF, Median (IQR) | 17.0 (11.0 - 22.0) |
| Elixhauser comorbidity score, Median (IQR) | 22.0 (12.0 - 32.0) |
| Dual eligible | 9351 (13.8%) |
| Hospital beds | Hospital beds |
| 1-99 | 7450 (11.0%) |
| 100-199 | 14696 (21.7%) |
| 200-299 | 13680 (20.2%) |
| 300-399 | 10725 (15.9%) |
| 400-499 | 5826 (8.6%) |
| 500+ | 14617 (21.6%) |
| Hospital Location | |
| Urban | 65280 (96.6%) |
| Rural | 1714 (2.5%) |
| Teaching hospital | 43338 (64.1%) |
SNF: Skilled Nursing Facility
HF: Heart Failure
IQR: Interquartile Range
As noted in the methods, we qualitatively observed that readmission patterns appeared to be different for patients with a LOS of 1-6 days, 7-13 days, and 14-30 days, respectively (Figure 2). Next, our plot of the log probability of being free of readmission over time demonstrated two separate linear relationships in the 30 days after SNF to home discharge: at 0-2 days and 3-30 days (Figure 3). This represents two different readmission hazards for each of these time periods. Consequently, we created separate piecewise exponential Bayesian models for patients with a length of stay of 1-6 days, 7-13 days, and 14-30 days, respectively and examined the baseline hazard of readmission for each of these groups at 0-2 days after SNF to home discharge and at 3-30 days after SNF to home discharge.
Figure 2:
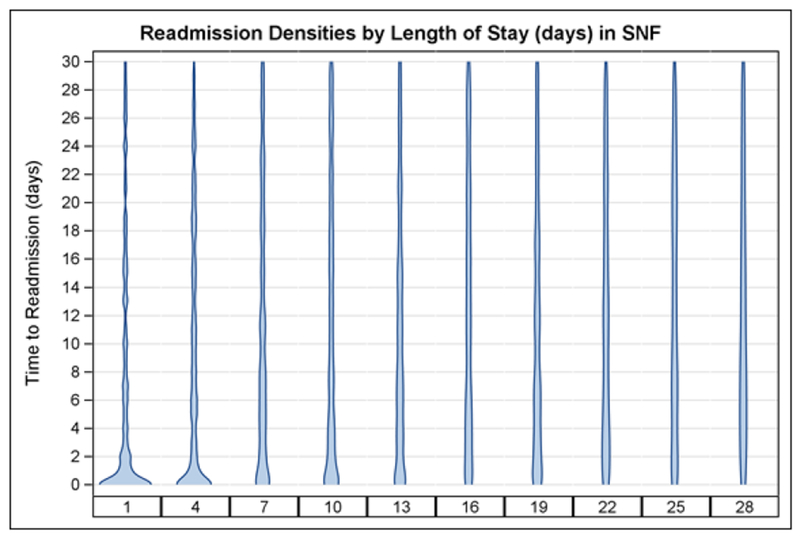
Violin plots of Readmission Densities by Length of Stay in SNF.
We graphed out 30-day readmissions for patients based on SNF length of stay. On the horizontal axis are representative cohorts. The vertical axis represents the day after SNF discharge when readmission occurred. The density shows the relative number of 30-day readmissions that occurred on each day. This provides us a descriptive analysis of the timing of readmission. We qualitatively observed that proportion of readmissions appeared to be higher on days 0-3 after SNF discharge to home versus days 4-30 after SNF discharge to home We also qualitatively observed that readmission patterns appeared to be different for patients with a LOS of 1-6 days, 7-13 days, and 14-30 days, respectively. Depicted above are representative cohorts.
Figure 3:
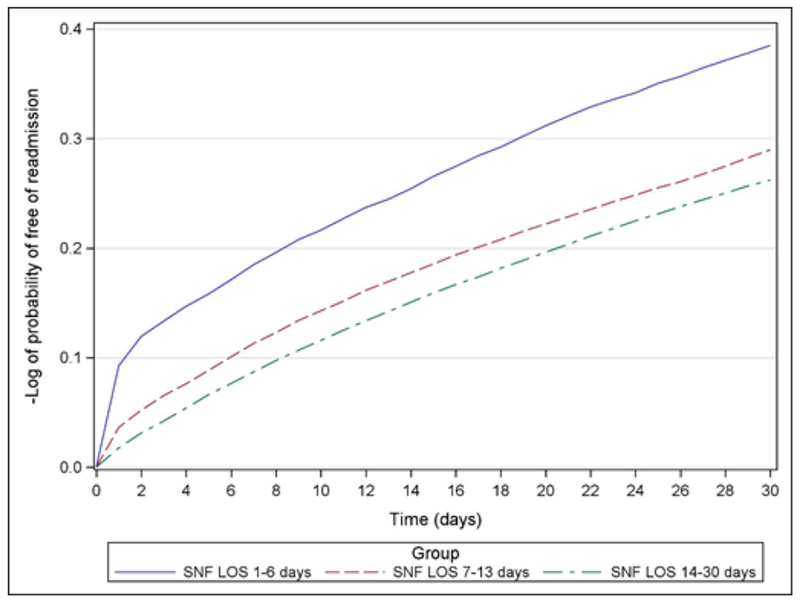
Risk of first hospital readmission for 30 days after discharge from SNF to home following hospitalization for heart failure.
We found the hazard rate of the composite outcome for each group was about 2-4 times higher on days 0-2 after discharge from SNF than on days 3-30 after discharge from SNF, regardless of SNF length of stay (Table 2). However, the ratio of the hazard rate of the first 0-2 days after discharge from SNF to the hazard rate during days 3-30 decreased as the length of stay in SNF increased (Table 3).
Table 2:
Risk of Composite Outcome [readmission or death] after Discharge from SNF Following HF Hospitalization
| SNF Length of Stay | Hazard Rate of Composite Outcome on days 0-2 after SNF to home discharge (95% credible interval) | Hazard Rate of Composite Outcome on days 3-30 after SNF to home discharge (95% credible interval) | Ratio of Hazard Rates (95% credible interval) |
|---|---|---|---|
| 1-6 days (n=6033) | 0.051 (0.036 - 0.072) | 0.011 (0.008 - 0.016) | 4.60 (4.23 – 5.00) |
| 7-13 days(n=16773) | 0.027 (0.020 - 0.035) | 0.010 (0.008 - 0.013) | 2.61 (2.45 - 2.78) |
| 14-30 days (n=44779) | 0.013 (0.011 - 0.016) | 0.008 (0.007 - 0.009) | 1.70 (1.62 - 1.78) |
SNF: Skilled Nursing Facility
HF: Heart Failure
Table 3:
Risk of Readmission after Discharge from SNF Following HF Hospitalization
| SNF Length of Stay | Hazard Rate of Readmission on days 0-2 after SNF to home discharge (95% credible interval) | Hazard Rate of Readmission on days 3-30 after SNF to home discharge (95% credible interval) | Ratio of Hazard Rates (95% credible interval) |
|---|---|---|---|
| 1-6 days (n=6033) | 0.048 (0.033 - 0.069) | 0.010 (0.007 - 0.015) | 4.74 (4.31 - 5.20) |
| 7-13 days (n=16773) | 0.026 (0.019 - 0.034) | 0.010 (0.007 - 0.013) | 2.55 (2.37 - 2.73) |
| 14-30 days (n=44779) | 0.013 (0.011 - 0.016) | 0.008 (0.007 - 0.010) | 1.66 (1.58 - 1.75) |
SNF: Skilled Nursing Facility
HF: Heart Failure
We observed similar hazard rates when modeling readmission risk alone (Table 2).
Discussion
In our analysis of Medicare claims data among all patients discharged to SNF after HF hospitalization, we found that almost a quarter were readmitted to the hospital within 30 days of SNF discharge. Risk for readmission was 2-4 times higher immediately after SNF to home discharge compared to later time periods and this early readmission risk dropped by half for patients with SNF stays of 1-2 weeks compared to those with shorter stays. However, even those patients had a twofold increase in the relative risk of readmission immediately following discharge from SNF to home. While this heightened risk of readmission immediately after discharge from SNF may be related to patient-level factors, the persistence of increased risk across multiple cohorts of patients suggests that the disruption in care continuity when a patient is transferred from SNF to home may be playing an important role.
Existing research has primarily focused on the care transition from hospital discharge to home3–7 while evidence about the care transition from post-acute care to home is lacking. Though organizations have recently started publishing expert opinion based guidelines17 for the SNF to home transition, there is no evidence that formal discharge practices occur routinely. HF patients discharged from hospital to SNF are more medically and functionally complicated than the overall Medicare HF population,18, 19 the latter who have a readmission rate of 21.7%.20 Therefore, patients discharged from SNF may benefit from discharge planning since during a SNF stay medications may be started or adjusted, diets may be monitored and lab tests may be obtained, which may need post-SNF discharge follow up.
Prior work on the transition from hospital to home provides useful lessons for institutional post-acute care, such as SNFs.3–7 For example, studies on discharge practices have demonstrated the effectiveness of discharge instructions21 and early outpatient physician follow up after hospital discharge.22 Moreover, guidelines such as the Transitions of Care Consensus Conference (TOCCC)23 have established standards on transitions between the inpatient and outpatient settings, while major organizations such as the Joint Commission mandate that specific elements be included in all U.S. hospital discharge summaries,24 and have established medication reconciliation as a National Patient Safety Goal.25 Similarly, organizations like the Society of Hospital Medicine have produced toolkits like Project BOOST (Better Outcomes by Optimizing Safe Transitions),26 designed to improve discharge processes at hospitals.
Some of these programs have been modified and applied to the SNF-to-home transition to improve care coordination and minimize care disruption. Pre-post studies have examined implementation of comprehensive care transition checklists27 and a transitional care clinic28 during the SNF-to-home transition; while another study has piloted a team-based transitional care intervention for SNF patients.29 Another secondary data analysis study using the Older Adults Transition Study database also demonstrated reduced hazard of readmission with those patients who have a home health visit within a week of SNF discharge.30 However, given the complex interplay of drivers that affect readmission and death for older HF patients during transitions, further evidence is needed to inform such practices as HF patients are at a particularly high risk for readmission.
Indeed, as hospital length of stay declines and uses of SNF rises,31 the importance of identifying best practices for HF management in SNFs will become increasingly evident32 particularly since HF is a chronic problem that requires ongoing disease management. It is necessary to target these high risk patients throughout their care continuum to optimize medical therapy, reinforce self-management skills, and ensure adequate services are in place to regularly assess volume and symptoms to facilitate outpatient provider management. Our finding that readmission risk is highest during the early discharge period, particularly in those with short SNF stays, could help guide when these interventions may be most efficacious.
Policy such as the Readmissions Reduction Program aim to reduce avoidable 30 day readmissions for HF patients.33 While previous work has examined readmission patterns after hospital discharge,34, 35 the health care continuum often includes post-acute care, such as SNFs. Most hospital-to-SNF patients lived at home prior to hospital admission and return home after a temporary SNF stay.1 Consequently, many patients discharged to SNF incur a second transition, from SNF to home, within 30 days of hospital discharge. We found the risk of readmission after SNF discharge declines as SNF length of stay increases, which may be because patients have had more time to recover from their acute illness. However this finding is subject to survivor bias as we only include those who have survived to SNF discharge. Our study also builds on previous work on readmission patterns by studying how additional transitions experienced by patients after hospital discharge may affect their readmission risk. Processes used to allay readmissions may be made more effective if they take these additional risks into account.
Strengths and Limitations
This analysis differs from prior work in that it focuses on readmission and mortality after SNF discharge, not during SNF stay.1, 36, 37 The few studies that have examined outcomes from SNF to home did not use national data.38, 39 In addition, while previous work has examined state level data on SNF readmissions after any hospitalization and those with end-stage renal disease in North and South Carolina, it has not examined transitions specific to HF patients, who are particularly vulnerable to readmission40 and may benefit from HF specific discharge care. Furthermore, the national data in this study examines most older HF patients in the United States, who are an important target of Medicare policy.
Our study is limited by its observational design, which precludes making causal inferences, though our aim was to illustrate risk trajectories over time. In addition, as this study examines an administrative database, there may be misclassification regarding accuracy of admission and discharge dates; however, there is no systematic reason why any particular dates would be erroneous and these fields in CMS data in general are reliable.12 Furthermore, Medicare SNF claims data cannot account for disease severity or patient function (such as frailty or cognitive impairment), which may differ between patients with different SNF LOS. We also did not adjust for quality of discharge care at the SNF in this study, as this study was intended to describe readmission risk for the SNF cohort in general. We plan to address SNF-level factors and post-discharge factors in our future work.
Conclusion/Relevance
Post-acute care skilled nursing facilities are common destinations from the acute care setting. We found discharge from SNF to home is associated with a risk of hospital readmission. Length of stay at SNF also has an effect on risk of readmission immediately after discharge from SNF; patients with a longer length of stay in SNF were less likely to be readmitted in the first 2 days after discharge from SNF. Transitions across the health care continuum must be enhanced in order to improve longitudinal care. Further work should examine if formal discharge practices currently used in hospitals could be applied to the transition from SNF to home.
Acknowledgments:
This data has been presented at the SGIM 2018 Annual Meeting, April 11, 2018, Denver, Colorado; at Translational Science 2018, April 20, 2018, Washington, D.C.; and the 7th Conference of the American Society of Health Economists, June 11, 2018, Atlanta, Georgia.
Funding/Support: This work was supported by research grants R01HS022882 (Dr. Horwitz, Dr. Li, Dr. Bao, Dr. Herrin, Dr. Ross) from the Agency for Healthcare Research and Quality; the NYU CTSA grant KL2TR001446 (Dr. Weerahandi) from the National Center for Advancing Translational Sciences, National Institutes of Health.
In the past 36 months, Dr. Ross has received support through Yale University from the Food and Drug Administration as part of the Centers for Excellence in Regulatory Science and Innovation (CERSI) program, from Medtronic, Inc. and the Food and Drug Administration (FDA) to develop methods for postmarket surveillance of medical devices, from Johnson and Johnson to develop methods of clinical trial data sharing, from the Centers of Medicare and Medicaid Services (CMS) to develop and maintain performance measures that are used for public reporting, from the Blue Cross Blue Shield Association to better understand medical technology evaluation, from the Agency for Healthcare Research and Quality (AHRQ), and from the Laura and John Arnold Foundation to support the Collaboration on Research Integrity and Transparency (CRIT) at Yale. At the time this research was conducted, Dr. Horwitz, Dr. Dharmarajan, Dr. Li, Dr. Bao, Dr. Herrin, and Dr. Ross worked under contract with CMS to develop and maintain performance measures. Dr. Dharmarajan was also a consultant and scientific advisory board member of Clover Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Disclosures:
Author Statement: To the best of our knowledge, no conflict of interest, financial or other, exists.
References
- 1.Allen LA, Hernandez AF, Peterson ED, et al. Discharge to a Skilled Nursing Facility and Subsequent Clinical Outcomes Among Older Patients Hospitalized for Heart FailureClinical Perspective, Circ Heart Fail 2011. ;4:293–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mor V, Intrator O, Feng Z, Grabowski DC. The Revolving Door of Rehospitalization From Skilled Nursing Facilities, Health Aff (Millwood) 2010;29:57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forster AJ, Murff HJ, Peterson JF, et al. The incidence and severity of adverse events affecting patients after discharge from the hospital, Ann Intern Med 2003;138:161–167. [DOI] [PubMed] [Google Scholar]
- 4.Roy CL, Poon EG, Karson AS, et al. Patient safety concerns arising from test results that return after hospital discharge, Ann Intern Med 2005;143:121–128. [DOI] [PubMed] [Google Scholar]
- 5.Horwitz L, Jenq G, Brewster U, et al. - Comprehensive quality of discharge summaries at an academic medical center. J Hosp Med. 2013. August;8(8):436–43. doi: 10.1002/jhm.2021. Epub 2013 Mar 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ziaeian B, Araujo K, Van N PH, Horwitz L Medication reconciliation accuracy and patient understanding of intended medication changes on hospital discharge. J Gen Intern Med .2012. November;27(11):1513–20. doi: 10.1007/s11606-012-2168-4. Epub 2012 Jul 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horwitz LI, Moriarty JP, Chen C, et al. Quality of discharge practices and patient understanding at an academic medical center, JAMA Intern Med 2013;173:1715–1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Medicare & Medicaid Services. Medicare Coverage of Skilled Nursing Facility Care, 2015;p.23.
- 9.Centers for Medicare & Medicaid. The Skilled Nursing Facility Value-Based Purchasing Program (SNFVBP), 2017.
- 10.Horwitz LI, Grady JN, Cohen D, et al. Development and validation of an algorithm to identify planned readmissions from claims data, Journal of hospital medicine 2015;10:670–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keenan PS, Normand ST, Lin Z, et al. An Administrative Claims Measure Suitable for Profiling Hospital Performance on the Basis of 30-Day All-Cause Readmission Rates Among Patients With Heart FailureCLINICAL PERSPECTIVE, Circ Cardiovasc Qual Outcomes 2008;1:29–37. [DOI] [PubMed] [Google Scholar]
- 12.Virnig B, Parsons H. Strengths and Limitations of CMS Administrative Data in Research, Research Data Assitance Center: ResDAC 2018. [Google Scholar]
- 13.Kubo J, Cullen MR, Cantley L, et al. Piecewise exponential models to assess the influence of job-specific experience on the hazard of acute injury for hourly factory workers, BMC Med Res Methodol 2013;13:89-2288-13-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clark DE, Ryan LM, Lucas FL. A Multi-state Piecewise Exponential Model of Hospital Outcomes after Injury, Journal of Applied Statistics 2007;34:1225–1239. [Google Scholar]
- 15.Rodriguez G Generalized Linear Models: The Piece-Wise Exponential Model. [http://data.princeton.edu/wws509/notes/c7s4.html] Last Updated, Year: 2017 Accessed, Year: 2018 2017;2018. [Google Scholar]
- 16.SAS Institute Inc. Example 64.14 Bayesian Analysis of Piecewise Exponential Model In: SAS Institute Inc. ed. SAS/STAT(R) 9.2 User’s Guide, Second Edition Cary, NC: SAS Institute Inc., 2008. [Google Scholar]
- 17.Lindquist LA, Miller RK, Saltsman WS, et al. SGIM-AMDA-AGS Consensus Best Practice Recommendations for Transitioning Patients’ Healthcare from Skilled Nursing Facilities to the Community, Journal of General Internal Medicine 2017;32:199–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Orr NM, Forman DE, De Matteis G, Gambassi G. Heart Failure Among Older Adults in Skilled Nursing Facilities: More of a Dilemma Than Many Now Realize, Current geriatrics reports 2015;4:318–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Burke RE, Lawrence E, Ladebue A, et al. How Hospital Clinicians Select Patients for Skilled Nursing Facilities, J Am Geriatr Soc 2017;65:2466–2472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Centers for Medicare and Medicaid Services. Hospital Compare. 2017. Available at: [https://www.medicare.gov/hospitalcompare/Data/Data-Updated.html#] Accessed September 12, 2018.
- 21.Hesselink G, Zegers M, Vernooij-Dassen M, et al. Improving patient discharge and reducing hospital readmissions by using Intervention Mapping, BMC Health Services Research 2014;14:389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hernandez AF, Greiner MA, Fonarow GC, et al. Relationship between early physician follow-up and 30-day readmission among medicare beneficiaries hospitalized for heart failure, JAMA 2010;303:1716–1722. [DOI] [PubMed] [Google Scholar]
- 23.Snow V, Beck D, Budnitz T, et al. Transitions of Care Consensus Policy Statement American College of Physicians-Society of General Internal Medicine-Society of Hospital Medicine-American Geriatrics Society-American College of Emergency Physicians-Society of Academic Emergency Medicine, Journal of General Internal Medicine 2009;24:971–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kind AJH, Smith MA Documentation of Mandated Discharge Summary Components in Transitions from Acute to Subacute Care In: Henriksen K, Battles JB, Keyes MA and Grady ML eds. Advances in Patient Safety: New Directions and Alternative Approaches (Vol. 2: Culture and Redesign) Rockville (MD): 2008. [PubMed] [Google Scholar]
- 25.The Joint CommissionHospital: 2017 National Patient Safety Goals In: Anonymous 2017 National Patient Safety Goals The Joint Commission, 2016. [Google Scholar]
- 26.Society of Hospital Medicine. Project BOOST® Implementation Toolkit, 2014;2017. [Google Scholar]
- 27.Berkowitz RE, Fang Z, Helfand BK, et al. Project ReEngineered Discharge (RED) lowers hospital readmissions of patients discharged from a skilled nursing facility, J Am Med Dir Assoc 2013;14:736–740. [DOI] [PubMed] [Google Scholar]
- 28.Park HK, Branch LG, Bulat T, et al. Influence of a transitional care clinic on subsequent 30-day hospitalizations and emergency department visits in individuals discharged from a skilled nursing facility, J Am Geriatr Soc 2013;61:137–142. [DOI] [PubMed] [Google Scholar]
- 29.Toles M, Colon-Emeric C, Naylor MD, et al. Connect-Home: Transitional Care of Skilled Nursing Facility Patients and their Caregivers, J Am Geriatr Soc 2017;65:2322–2328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carnahan JL, Slaven JE, Callahan CM, et al. Transitions From Skilled Nursing Facility to Home: The Relationship of Early Outpatient Care to Hospital Readmission, Journal of the American Medical Directors Association 2017;18:853–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bueno H, Ross JS, Wang Y, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993-2006, JAMA 2010;303:2141–2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heckman GA, Shamji AK, Ladha R, et al. Heart Failure Management in Nursing Homes: A Scoping Literature Review, Can J Cardiol 2018;34:871–880. [DOI] [PubMed] [Google Scholar]
- 33.McIlvennan CK, Eapen ZJ, Allen LA. Hospital Readmissions Reduction Program, Circulation 2015;131:1796–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia, JAMA 2013;309:355–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dharmarajan K, Hsieh AF, Kulkarni VT, et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study, BMJ 2015;350:h411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burke RE, Whitfield EA, Hittle D, et al. Hospital Readmission From Post-Acute Care Facilities: Risk Factors, Timing, and Outcomes, Journal of the American Medical Directors Association 2016;17:249–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Horney C, Capp R, Boxer R, Burke RE. Factors Associated With Early Readmission Among Patients Discharged to Post-Acute Care Facilities, J Am Geriatr Soc 2017;65:1199–1205. [DOI] [PubMed] [Google Scholar]
- 38.Toles M, Anderson RA, Massing M, et al. Restarting the cycle: incidence and predictors of first acute care use after nursing home discharge, J Am Geriatr Soc 2014;62:79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hall RK, Toles M, Massing M, et al. Utilization of acute care among patients with ESRD discharged home from skilled nursing facilities, Clin J Am Soc Nephrol 2015;10:428–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gheorghiade M, Vaduganathan M, Fonarow GC, Bonow RO. Rehospitalization for Heart Failure: Problems and Perspectives, Journal of the American College of Cardiology 2013;61:391–403. [DOI] [PubMed] [Google Scholar]


