Abstract
Background:
There are few effective treatments for bipolar depression, a common and debilitating illness.
Aims:
We aimed to examine the feasibility and preliminary efficacy of a four-week, telephonedelivered positive psychology (PP) intervention for patients with bipolar depression.
Methods:
Twenty-five patients hospitalized for bipolar depression were randomized to receive a PP (n=14) or control condition (CC; n=11) intervention. Following discharge, participants completed weekly exercises and phone calls with a study trainer. PP intervention feasibility was assessed by the number of exercises completed, and acceptability was examined on 5-point Likert-type scales of ease and utility. Between-group differences on psychological constructs at 4 and 8 weeks post-enrollment were assessed using mixed effects regression models.
Results:
Participants in the PP group completed an average of three out of four PP exercises and found PP exercises to be subjectively helpful, though neither easy nor difficult. Compared to CC, the PP intervention led to trends towards greater improvements in positive affect and optimism at follow-up, with large effect sizes (modified Cohen’s d=0.95–1.24). PP had variable, non-significant effects on negative psychological constructs.
Conclusions:
Larger, randomized trials are needed to further evaluate the efficacy of this intervention in this high-risk population.
Trial Registration:
ClinicalTrials.gov identifier: NCT01820286
Keywords: bipolar disorder, positive psychology, depression, anxiety, optimism
Introduction
Bipolar disorder affects 2.8% of adults worldwide (Kessler et al., 2011) and 3.9% of adults in the United States (Kessler et al., 2005) and has been linked to poor functioning, high healthcare- and productivity-related costs, and increased rates of premature death and suicide (Miller, Dell’Osso, & Ketter, 2014). Depressive episodes (“bipolar depression”) are particularly problematic for patients with bipolar disorder. In this population, depressive symptoms are experienced significantly more frequently than manic symptoms (Calabrese, Hirschfeld, Frye, & Reed, 2004; Miller et al., 2014) and are independently associated with functional impairment in multiple life domains (Simon, Bauer, Ludman, Operskalski, & Unutzer, 2007). During periods of bipolar depression, patients are at a markedly (~18-fold) increased risk of attempted suicide compared to other phases of illness (Valtonen et al., 2008).
Despite these risks, there are relatively few effective treatments for bipolar depression. Atypical antipsychotic medications and mood stabilizers are first-line interventions, but these treatments are commonly associated with side effects, require substantial time to become efficacious, and may not lead to a full remission of depressive symptoms (Fountoulakis et al., 2016; Frye, Gitlin, & Altshuler, 2004). Psychotherapy is an appealing alternative or adjunctive treatment to pharmacotherapy for bipolar depression. Psychotherapies like cognitive behavioral therapy have been associated with improved mental health outcomes—including improved functioning, greater life satisfaction, and reduced rates of relapse—in this population (Deckersbach et al., 2016; Hofmann, Asnaani, Vonk, Sawyer, & Fang, 2012; Picardi & Gaetano, 2014; Swartz & Swanson, 2014; Thase, 2007). However, these therapies are intensive (Thase, 2007), may not be available or appeal to all patients, and require specialized provider training (Dorflinger, Fortin, & Foran-Tuller, 2016). Simple, cost-effective treatment interventions that improve mental health outcomes in patients with bipolar depression are needed.
Positive psychology (PP) interventions—which focus on the amplification of positive feelings—are a promising adjunctive treatment for bipolar depression (Seligman, Rashid, & Parks, 2006). PP focuses on the performance of systematic exercises to promote positive psychological constructs, such as optimism, gratitude, and positive affect (Seligman et al., 2006; Seligman, Steen, Park, & Peterson, 2005). These exercises are easy to complete and may include writing a letter of gratitude to others, performing acts of kindness, or recalling a past success (Sonja Lyubomirsky & Layous, 2013; Seligman et al., 2005). PP interventions can be delivered individually or in groups, in-person or by phone, and require minimal provider training, making them an appealing treatment choice for patients engaged in other treatment programs or unable to attend in-person sessions regularly.
PP interventions may be particularly promising for patients with bipolar depression. Patients with bipolar disorder frequently experience depressive symptoms (Calabrese et al., 2004; Miller et al., 2014), and both depression and pessimism are linked to an increased risk for suicide attempts (Galfalvy et al., 2006; Oquendo et al., 2004). Two recent meta-analyses suggest that PP interventions improve well-being and reduce depression (Bolier et al., 2013; Sin & Lyubomirsky, 2009), and small studies of PP interventions in outpatients with unipolar depression have been promising (Fava, Rafanelli, Cazzaro, Conti, & Grandi, 1998; Seligman et al., 2006), though a recent study in patients with severe depression and suicidal ideation found PP to be inferior to a cognition-focused control condition (CC) (Celano et al., 2016). However, no studies have been performed to assess the efficacy of PP interventions in patients with bipolar depression.
Accordingly, we conducted a randomized, controlled pilot trial to examine the feasibility and preliminary efficacy of a four-week, telephone-delivered PP intervention for patients recently hospitalized for bipolar depression. We hypothesized that the PP intervention would be feasible, acceptable to patients, and associated with greater improvements in positive and negative psychological constructs, compared to a CC focusing on the recollection of neutral events.
Methods
This study was a single-blind, two-site randomized trial of a four-week, telephone-based PP intervention for patients with an acute depressive episode in the context of bipolar disorder. All participants were admitted between April 2013 and April 2016 to inpatient psychiatric units at an urban general hospital or psychiatric hospital. Institutional Review Board approval at both sites was obtained, and the trial was registered on clinicaltrials.gov (ClinicalTrials.gov Identifier: NCT01820286). All participants provided informed consent prior to participation in the trial.
Participants
Participants were adults admitted to an inpatient psychiatric unit with an admission diagnosis of bipolar depression. Bipolar depression diagnosis was confirmed using the Mini International Neuropsychiatric Interview (MINI) (Sheehan et al., 1998), inpatient chart review, and discussion with the patient’s psychiatrist. Participants were excluded if they exhibited psychotic symptoms (assessed using the MINI and chart review), cognitive impairment (assessed using a six-item cognitive screen) (Callahan, Unverzagt, Hui, Perkins, & Hendrie, 2002), or had a primary admission diagnosis of a substance use disorder.
Study Procedures
Participants were identified through review of inpatient censuses and approached during their admission. One to two days prior to discharge, interested and eligible participants provided informed consent and were enrolled in the study. After completing baseline outcome measures, participants were randomized (using a random number generator) to either the PP or CC group. In both treatment conditions, participants were provided with a corresponding treatment manual and assigned the first exercise prior to discharge. Over the subsequent four weeks, a study trainer (CMC or CAM) spoke with participants weekly via telephone to review the exercise and to assign an additional exercise, with participants completing a total of four exercises. A blinded assessor administered self-report measures by telephone at four and eight weeks post-enrollment.
Study trainers had clinical degrees (MD or LICSW) and experience delivering the PP and CC interventions to patients. Prior to delivering this intervention, they reviewed both treatment manuals and practiced delivering the interventions together to minimize variability in delivery. Trainers were available to deliver either intervention to participants.
Study Interventions
Positive psychology:
The PP intervention was developed based on prior published interventions (S. Lyubomirsky, King, & Diener, 2005; Seligman et al., 2005; Sheldon & Lyubomirsky, 2006), our work in patients with psychiatric and medical illness (Celano et al., 2016; Huffman, Albanese, et al., 2016; Huffman et al., 2014; Huffman et al., 2011; Huffman, Millstein, et al., 2016), and our pre-pilot work in patients with bipolar depression. Each week, participants completed an exercise and then reviewed it with their study trainer. During the weekly phone calls, trainers focused on increasing participants’ vocabularies for positive emotions, reinforcing the positive emotions experienced while performing the exercise, and promoting integration of the exercises into daily life. The PP intervention consisted of the following four exercises:
Week 1 – Gratitude letter (Seligman et al., 2005): Participants wrote a letter thanking someone for an act for which they were grateful.
Week 2 – Using personal strengths (Seligman et al., 2005): Participants used a strength in a new way.
Week 3 – Performing acts of kindness (S. Lyubomirsky et al., 2005): Participants performed three acts of kindness in one day.
Week 4 – Imagining a best possible self (Sheldon & Lyubomirsky, 2006): Participants wrote about their best possible life in the future.
Control condition (CC):
The CC was designed to mirror the PP intervention in the number of phone contacts with a clinician and the number and type of mental assignments completed between phone sessions. Participants in the CC group were asked to recall and write down three neutral events that occurred each day over the previous week. Similar to those receiving PP, participants in the CC intervention engaged in weekly phone calls to review the prior week’s exercise and to assign the next week’s exercise. To maintain interest, participants were asked to write about neutral events in their lives related to a different topic each week:
Week 1 – Daily events: Participants recalled events that occurred in their day-to-day life.
Week 2 – Health-related events: Participants recalled events related to their mental or physical health.
Week 3 – Social events: Participants recalled events that involved interaction with others.
Week 4 – Morning and evening events: Participants recalled events that occurred at different times during the day.
This condition has been used in studies of PP interventions in healthy, medically ill, and psychiatrically ill populations (Celano et al., 2016; Huffman et al., 2011; Sheldon & Lyubomirsky, 2006). While it was designed to have little impact on psychiatric symptoms and has minimal effects on positive and negative affect in healthy and medically ill individuals (Huffman et al., 2011; Sheldon & Lyubomirsky, 2006), a recent study of patients hospitalized for depression and suicidal ideation found this CC to be superior to an active psychological intervention (Celano et al., 2016), raising the possibility that it may have benefits for patients with acute psychiatric illnesses.
Outcomes
Sociodemographic information, psychiatric history, and post-discharge treatments were obtained from the patient’s medical record.
Feasibility (primary study outcome):
Feasibility was measured by recording the number of PP exercises completed by participants randomized to that condition, as well as the proportion of participants who provided follow-up data. We hypothesized that most participants would complete at least three of four PP exercises, and 80% of participants would provide follow-up assessment data. Acceptability was examined using participants’ ratings of how easy (ease) and helpful (utility) each PP exercise was to complete, which were obtained from participants following the completion of each exercise. Ease and utility scores were separately rated on a 5-point Likert scale (ease: 1 = very difficult and 5 = very easy; utility: 1 = not helpful and 5 = very helpful).
Immediate impact on hopelessness and optimism:
The impact of each PP and CC exercise on hopelessness and optimism was examined by asking participants to rate their hopelessness and optimism on 5-point Likert scales before and after each exercise (hopelessness: 1 = not hopeless and 5 = very hopeless; optimism: 1 = not optimistic and 5 = very optimistic). Pre-post changes in these constructs were considered to represent the immediate impact of the PP or CC exercises on these constructs. We hypothesized that PP exercises would lead to significant pre-post improvements in optimism and hopelessness and that these improvements would be greater than those of the CC group.
Positive psychological constructs:
Optimism:
Life Orientation Test-Revised (LOT-R; range 0–24; Cronbach’s α=0.86) (Scheier, Carver, & Bridges, 1994): This 6-item self-report scale is well-validated (Herzberg, Glaesmer, & Hoyer, 2006) and has been used as a measure of optimism in patients with psychiatric illness (Celano et al., 2016).
Positive affect:
Positive and Negative Affect Schedule (PANAS; range 10–50; α=0.87) (Watson & Clark, 1984): The 10-item positive affect subscale of the PANAS is valid (Watson, Clark, & Tellegen, 1988) and has been used to measure positive affect in samples of depressed individuals (Berman et al., 2012; Celano et al., 2016).
Gratitude:
Gratitude Questionnaire-6 (GQ-6; range 6–42; α=0.57) (McCullough, Emmons, & Tsang, 2002): The GQ-6 is a 6-item measure of gratitude that has been used in a variety of clinical populations, including those with significant depression (Huffman, Beale, et al., 2016; Ivtzan & Papantoniou, 2014; McCullough et al., 2002).
Suicide risk factors:
Hopelessness:
Beck Hopelessness Scale (BHS; range 0–20; α=0.94): The 20-item BHS was used to measure hopelessness (Beck, Weissman, Lester, & Trexler, 1974). This valid scale has been used in multiple depression studies, and elevated scores are associated with an increased risk of suicide (Beck, Brown, Berchick, Stewart, & Steer, 1990; Beck, Brown, & Steer, 1989).
Suicidal ideation:
Concise Health Risk Tracking scale (CHRT; range 0–48; α=0.91): The CHRT (Trivedi et al., 2011), a well-validated 12-item questionnaire, was used as a measure of suicidality.
Depression:
Quick Inventory of Depressive Symptomatology, Self-Report (QIDS-SR; range 0–27; α=0.78): Depressive symptoms were measured using the QIDS-SR (Rush et al., 2003), a widely used and validated self-report measure (Trivedi, 2009).
Data Analysis
Sociodemographic information, psychiatric history, and post-discharge treatments:
Baseline sociodemographic information was summarized using means (standard deviation [SD]) or proportions. Between-group differences on sociodemographic information and psychiatric variables, as well as baseline scores on outcome measures, were assessed using t-tests for continuous variables and chi-square analyses for categorical ones.
Feasibility and acceptability:
We performed descriptive statistics to examine the proportion of PP exercises completed and the mean ease and utility scores for PP exercises. Between-group differences in ease and utility scores were assessed using mixed effects regression models, which allowed us to control for intra-individual variability (since each participant could have completed up to 4 PP or CC exercises).
Immediate impact on hopelessness and optimism:
We performed paired t-tests to determine whether hopelessness and optimism scores differed before and after each PP exercise. We also examined whether the immediate impact of the PP and CC interventions differed using mixed effects regression models, accounting for intra-individual variability. Effect sizes (modified Cohen’s d) were calculated by dividing the group coefficient by the SD of the residual in the regression model.
Impact on positive and negative psychological constructs at 4 and 8 weeks:
To examine the impact of the PP and CC interventions on psychological constructs, paired t-tests were performed. To examine the impact of the PP intervention on psychological states compared to CC, we created mixed effects regression models to compare between-group differences in change in psychological states at four and eight weeks. Given the small sample size of this pilot trial, we did not expect to find statistically significant between-group differences on psychological outcomes. Instead, effect sizes (modified Cohen’s d) were calculated by dividing the Group x Time interaction coefficient by the standard deviation (SD) of the residual in the regression model, to determine the sample size needed to identify significant differences on these outcomes in future studies.
All analyses were performed using Stata 14 (StataCorp., College Station, TX). Twotailed alpha was set at .05 for all analyses.
Results
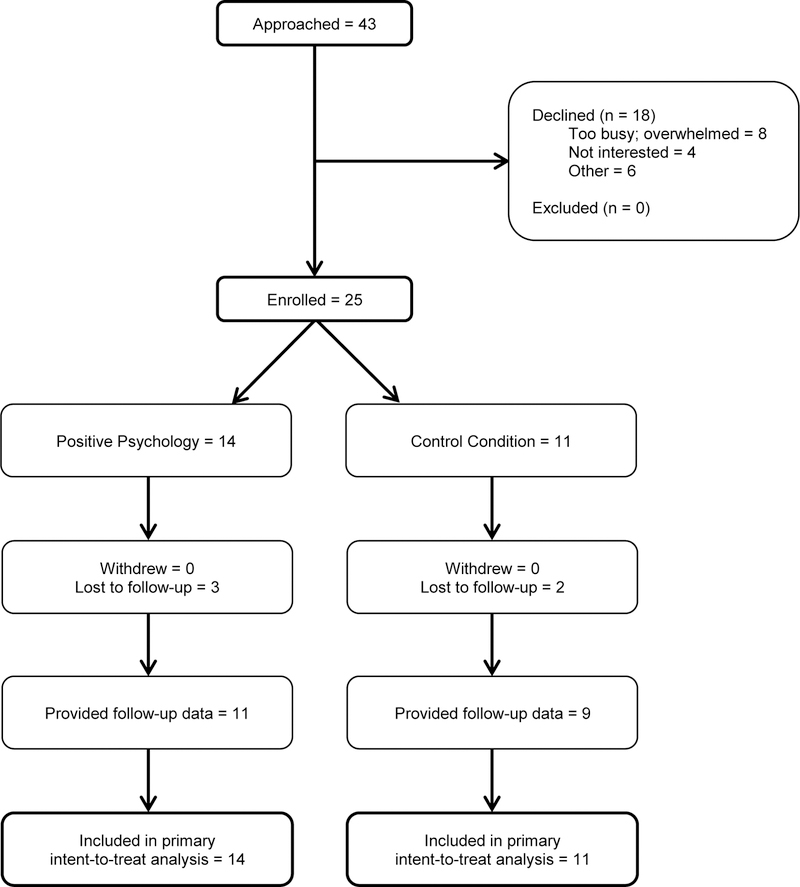
Approximately 200 patients were considered for recruitment, and 43 were approached. The most common reasons for not approaching patients included the presence of manic or psychotic symptoms, active/severe substance use, and lack of a clear diagnosis of bipolar depression. Of those 43 patients approached about the study, 25 enrolled, with 14 randomized to the PP intervention and 11 randomized to CC (see Figure 1). Baseline sociodemographic and psychiatric characteristics of participants are included in Table 1. Participants had a mean age of 45.4 years, and 88% were Caucasian. Nineteen (79%) had been hospitalized in the past, 17 (68%) had a comorbid substance use disorder, and 13 (54%) had a history of a prior suicide attempt. Baseline psychological characteristics were similar between groups, though participants in CC had more suicidal ideation than participants in PP.
Figure 1.
CONSORT diagram of recruitment
Table 1:
Baseline characteristics of PP and CC groups*
| Characteristic | PP (n=14) | CC (n=11) | Test statistic | p-value |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Age; mean (SD) | 42.6 (12.8) | 48.9 (13.2) | t = 1.20 | .24 |
| Female gender | 9 (64) | 8 (73) | Χ2 = 0.20 | .65 |
| Caucasian race | 12 (86) | 10 (91) | Χ2 = 0.83 | .66 |
| Lives alone | 5 (36) | 1 (9) | Χ2 = 2.39 | .12 |
| Employed or student | 5 (36) | 3 (27) | Χ2 = 0.20 | .65 |
| Psychiatric characteristics | ||||
| Prior hospitalization** | 10 (71) | 9 (90) | Χ2 = 1.22 | .27 |
| Prior suicide attempt** | 7 (50) | 6 (60) | Χ2 = 0.24 | .63 |
| History of substance use disorder | 9 (64) | 8 (73) | Χ2 = 0.20 | .65 |
| Treatments at discharge | ||||
| Mood stabilizer | 7 (50) | 8 (73) | Χ2 = 1.33 | .25 |
| Lithium | 7 (50) | 4 (36) | Χ2 = 0.46 | .50 |
| Antipsychotic | 8 (57) | 8 (73) | Χ2 = 0.65 | .42 |
| Antidepressant | 8 (57) | 6 (55) | Χ2 = 0.02 | .90 |
| Anxiolytic | 5 (36) | 3 (27) | Χ2 = 0.20 | .65 |
| Referral for ECT | 2 (14) | 3 (27) | Χ2 = 0.65 | .42 |
| Referral for partial hospital program | 4 (29) | 3 (27) | Χ2 = 0.01 | .94 |
| Baseline psychological characteristics; mean (SD) | ||||
| Optimism (LOT-R; range 0–24) | 7.0 (5.8) | 8.8 (6.9) | t = 0.72 | .48 |
| Gratitude (GQ-6; range 6–42) | 27.9 (5.6) | 27.0 (6.6) | t = −0.38 | .71 |
| Positive affect (PANAS; range 10–50) | 18.5 (6.3) | 16.7 (7.5) | t = −0.64 | .53 |
| Hopelessness (BHS; range 0–20) | 12.3 (6.9) | 12.4 (6.4) | t = 0.03 | .98 |
| Suicidal ideation (CHRT; range 0–48) | 13.9 (8.6) | 23.2 (14.0) | t = 2.03 | .05 |
| Depression (QIDS-SR; range 0–27) | 15.8 (5.7) | 18.8 (5.1) | t = 1.38 | .18 |
All variables are presented as n (%) unless specified.
n=10 in CC
BHS = Beck Hopelessness Scale; CC = control condition; CHRT = Concise Health Risk Tracking; GQ-6 = Gratitude Questionnaire-6; LOT-R = Life Orientation Test – Revised; PANAS = Positive and Negative Affect Schedule; PP = positive psychology; QIDS-SR = 16-item Quick Inventory of Depressive Symptomatology – Self-Report
Feasibility and acceptability:
Overall, the PP intervention was feasible and acceptable. Participants in the PP group completed an average of 3.0 (SD 1.7) out of 4 (75%) PP exercises, and 10 of the 14 participants (71%) in the PP group completed three or more exercises. Follow-up data were obtained from 22/25 (88%) of participants. Participants found the PP intervention to be subjectively helpful (mean utility score = 3.1±1.3), and ease ratings suggested that exercises were neither easy nor difficult to complete (mean ease score = 2.8±1.2). These scores were similar to those in the CC intervention (mean ease score = 2.8±1.3; mean utility score = 3.4±1.2) when compared in the mixed effects model (ease: β=0.53, 95% CI [−0.69, 0.80], p=.89; utility: β=−0.25, 95% CI [−1.01, 0.52], p=.52).
Immediate impact on hopelessness and optimism:
Individual PP exercises led to significant reductions in hopelessness and increases in optimism. On average, each PP exercise led to a 0.9 point reduction in hopelessness (2.9±1.3 [pre] vs. 2.0±1.1 [post], t=−4.71, p<.001) and a 0.7 point increase in optimism (2.2±0.8 [pre] vs. 3.0±1.1 [post], t=5.10, p<.001). In our mixed effects model, accounting for intra-individual variability, PP exercises led to marginally significant reductions in hopelessness (β=−0.73, 95% CI [−1.55, 0.08], p=.08, d=−0.72) and numerically greater but not significant increases in optimism (β=0.34, 95% CI [−0.33, 1.01], p=.32, d=0.34), compared to CC. These effects were small to moderate in size.
Impact on positive psychological constructs at 4 and 8 weeks:
Paired t-tests suggested that the PP intervention led to significant improvements in positive psychological constructs (see supplementary Table 1 and supplementary Figure 1). The intervention had its greatest impact on positive affect, which increased by 10.6 (SD 7.2) points at four weeks (t=4.37, p=.002) and by 15.5 (SD 8.0) points at eight weeks (t=6.42, p<.001). Gratitude also demonstrated a marginally significant increase at eight—but not four—weeks (4 weeks: 4.7±9.4, t=1.49, p=.17; 8 weeks: 6.5±9.9, t=2.19, p=.05). Finally, though the PP intervention did not lead to a significant improvement in optimism at four weeks (4.7±8.4, t=1.66, p=.14), it led to a significant improvement in optimism at eight weeks (6.3±8.9, t=2.33, p=.04). The CC intervention had much smaller effects on positive constructs. It led to marginally significant increases in positive affect at 8 weeks (change=8.6±11.4, t=2.25, p=.05) but did not impact gratitude or optimism (all p≥.44).
In mixed effects regression analyses, the PP intervention similarly led to greater improvements in positive psychological states than CC (see Figure 2 and Table 2). Specifically, compared to CC, the PP intervention led to marginally (p=.08) greater improvements in optimism at both four and eight weeks (4 weeks: β=5.61, 95% CI [−0.59, 11.81], d=1.24; 8 weeks: β=4.96, 95% CI [−0.54, 10.46], d=1.10), as well as marginally (p=.10) greater improvements in positive affect at four weeks (β=6.81, 95% CI [−1.22, 14.83], d=1.16). The PP intervention also led to numerically greater but non-significant improvements in gratitude at both four and eight weeks and positive affect at eight weeks compared to CC (gratitude at 4 weeks: β=3.91, 95% CI [−3.82, 11.64], d=0.68; gratitude at 8 weeks: β=2.99, 95% CI [−3.95, 9.93], d=0.52; positive affect at 8 weeks: β=5.58, 95% CI [−1.55, 12.71], d=0.95).
Figure 2. Estimated changes in psychological constructs (from baseline to 8 weeks).
BHS = Beck Hopelessness Scale; CHRT = Concise Health Risk Tracking; GQ-6 = Gratitude Questionnaire-6; LOT-R = Life Orientation Test – Revised; PANAS = Positive and Negative Affect Schedule; QIDS = 16-item Quick Inventory of Depressive Symptomatology – Self-Report
Table 2.
Mixed effects regression results indicating the impact of the PP intervention (compared to CC) on psychological outcomes at 4 and 8 weeks.*
| Outcome | 4 weeks | 8 weeks | ||||||
|---|---|---|---|---|---|---|---|---|
| Coefficient | 95% CI | Effect size** | p | Coefficient | 95% CI | Effect size** | p | |
| Positive Affect (PANAS) | 6.81 | −1.22 to 14.83 | 1.16 | .10 | 5.58 | −1.55 to 12.71 | 0.95 | .13 |
| Gratitude (GQ-6) | 3.91 | −3.82 to 11.64 | 0.68 | .32 | 2.99 | −3.95 to 9.93 | 0.52 | .40 |
| Optimism (LOT-R) | 5.61 | −0.59 to 11.81 | 1.24 | .08 | 4.96 | −0.54 to 10.46 | 1.10 | .08 |
| Depression (QIDS-SR) | −0.05 | −6.38 to 6.27 | −0.01 | .99 | −0.31 | −5.95 to 5.32 | −0.07 | .91 |
| Hopelessness (BHS) | −3.67 | −9.81 to 2.47 | −0.81 | .24 | −1.10 | −6.56 to 4.36 | −0.24 | .69 |
| Suicidality (CHRT) | 4.69 | −4.67 to 14.05 | 0.68 | .33 | 2.87 | −5.44 to 11.18 | 0.42 | .50 |
Results of mixed effects regression models. Coefficients are Group x Time interaction values.
Effect size was calculated by dividing the Group x Time interaction coefficient of each variable at each time point by the standard deviation (SD) of the residual in the regression model.
BHS = Beck Hopelessness Scale; CHRT = Concise Health Risk Tracking; GQ-6 = Gratitude Questionnaire-6; LOT-R = Life Orientation Test – Revised; PANAS = Positive and Negative Affect Schedule; QIDS-SR = Quick Inventory of Depressive Symptomatology – Self-Report
Impact on negative psychological constructs at 4 and 8 weeks:
Results from paired t-tests indicated that the PP intervention led to improvements in negative psychological constructs as well (see supplementary Table 1 and supplementary Figure 2). Specifically, the PP intervention led to significant reductions in hopelessness and depression at eight weeks (change in hopelessness: −5.6±7.9, t=−2.37, p=.04; change in depression: −6.4±6.6, t=−3.19, p=.01), as well as marginally significant reductions in hopelessness and suicidal ideation at 4 weeks (change in hopelessness: −5.3±8.6, t=−1.86, p=.10; change in suicidal ideation: 1.9±3.0, t=−1.90, p=.09). Finally, the PP intervention led to smaller, non-significant reductions in depression at four weeks (change in depression: −3.1±5.3, t=−1.74, p=.12) and suicidal ideation at 8 weeks (change in suicidal ideation: −4.5±9.9, t=−1.52, p=.16). In contrast, CC had a smaller impact on negative psychological constructs, leading to a significant reduction in hopelessness at 8 weeks (change=−4.8±6.0, t=−2.41, p=.04) but no other significant changes in hopelessness, depression, or suicidal ideation.
Compared to CC, the impact of PP on negative psychological states was less strong (see Figure 2 and Table 2). PP led to numerically greater but non-significant reductions in hopelessness at four and eight weeks compared to CC (4 weeks: β=−3.67, 95% CI [−9.81, 2.47], d=−0.81; 8 weeks: β=−1.10, 95% CI [−6.56, 4.36], d=−0.24), and there were virtually no differences between groups on depression change scores at either time point (4 weeks: β=−0.05, 95% CI [−6.38, 6.27], d=−0.01; 8 weeks: β=−0.31, 95% CI [−5.95, 5.32], d=−0.07). In contrast, CC led to greater, non-significant reductions in suicidal ideation compared to PP (4 weeks: β=4.69, 95% CI [−4.67, 14.05], d=0.68; 8 weeks: β=2.87, 95% CI [−5.44, 11.18], d=0.42), though these may have been related to the significantly greater levels of suicidal ideation in the CC group at baseline.
Discussion
Our findings suggest that a telephone-delivered, four-week PP intervention may be a potentially useful adjunctive treatment for the management of depression in patients with bipolar disorder. In a group of recently hospitalized patients with bipolar depression, the PP intervention was feasible and subjectively helpful. Individual PP exercises led to significant reductions in hopelessness and increases in optimism. Furthermore, the PP intervention as a whole led to trends towards greater improvements in positive affect and optimism at follow-up compared to CC, which was associated with smaller improvements in psychological constructs. Though these findings were not significant—likely due to the small sample size of the treatment groups—the effect sizes were very large, suggesting that PP may be useful as an adjunct to current psychotherapy and pharmacotherapy treatment options following discharge. This should be tested further in a larger randomized trial.
Our findings are consistent with prior research testing PP interventions, which have found these approaches to be helpful in a broad range of individuals, including those with psychiatric illness. In two recent meta-analyses of mostly healthy and non-depressed individuals, PP interventions led to significant improvements in well-being and reductions in depressive symptoms (Bolier et al., 2013; Sin & Lyubomirsky, 2009). Furthermore, one metaanalysis found that patients with depression derive greater benefit from PP interventions compared to non-depressed individuals (Bolier et al., 2013), and randomized trials in outpatients with unipolar depression have found PP to be effective at improving depression, well-being, and functioning (Fava et al., 1998; Seligman et al., 2006). This study expands these findings to a high-risk group of patients with bipolar depression, for whom there are limited effective interventions.
Of note, the findings in this study run counter to those in a similar study conducted by our team in hospitalized patients with major depression and suicidal ideation (Celano et al., 2016). In that study, the CC (identical to the CC in this study) led to greater improvements in hopelessness, suicidal ideation, optimism, and gratitude at follow-up, compared to PP. However, several factors may explain these differences. First, participants in the prior trial had considerably higher suicidal ideation (CHRT) scores (28.6) than those in the current study (18.0); this degree of suicidal ideation may have made it more difficult for participants in the prior trial to engage in or benefit from PP exercises. Second, while the current intervention lasted for four weeks, the prior trial lasted for six. Longer interventions may be more likely to conflict with work and other responsibilities, and in those cases, more demanding interventions (e.g., PP) may feel overwhelming. Finally, participants in the prior trial were somewhat more likely to be referred to a partial hospitalization program or receive electroconvulsive therapy than those in the current trial, and these care differences may have influenced the intervention’s impact. While further studies are needed to clarify the impact of PP interventions in patients with bipolar depression, the findings that the PP intervention led to moderate to large improvements in psychological constructs compared to a potentially effective control condition is promising.
Our findings that the PP intervention is feasible and acceptable to patients and leads to substantial improvements in positive psychological constructs and reductions in depression suggest that this intervention has the potential to be a strong adjunctive treatment for bipolar depression. The intervention could have several potential benefits in clinical practice. Given that PP is straightforward and requires little provider training, it could be utilized in resourcepoor settings where doctoral level practitioners are not available. Furthermore, since the PP intervention is delivered by telephone and could potentially be adapted online, it can be accessed by patients who are unable to attend in-person visits. Finally, PP targets psychological constructs—such as optimism and positive affect—that are not targeted by current pharmacologic and psychotherapeutic interventions; this may increase its utility as an adjunctive treatment.
The current study has several limitations. First, the small sizes of our samples limited our power to detect significant between-group differences on our psychological outcomes and prevented the examination of the impact of the PP intervention on more tangible outcomes, such as rehospitalizations or suicide attempts. Second, our study’s performance at academic medical centers and our relatively homogeneous study population (68% female and 84% White) may limit the generalizability of our findings. Finally, given our small sample size, we were unable to control for covariates, such as age, gender, and treatment characteristics, in our analyses.
Ultimately, this study suggests that utilizing a telephone-based PP intervention for recently hospitalized patients with bipolar depression is feasible and potentially effective at improving positive psychological outcomes. Larger, well-powered research studies to examine the effects of this intervention on mental health and its cost-effectiveness as an adjunctive treatment may help to elucidate the potential benefits of this intervention for patients with bipolar depression.
Supplementary Material
Acknowledgements:
There are no additional acknowledgements for this submission.
Source of Funding
This research project was supported by a Dupont-Warren fellowship grant from Harvard Medical School. Time for analysis and article preparation was also funded by the National Heart, Lung, and Blood Institute through grants K23HL123607 (to Dr. Celano) and R01HL113272 (to Dr. Huffman). The National Institute of Mental Health funded time and effort through grant K23MH097786 (to Dr. Auerbach). The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health or other funders. Sponsors had no role in the design, analysis, interpretation, or publication of the study. Dr. Celano has received honoraria for talks to Sunovion Pharmaceuticals on topics unrelated to this research.
Footnotes
Conflicts of Interest
The authors report no other conflicts of interest.
References
- Beck AT, Brown G, Berchick RJ, Stewart BL, & Steer RA (1990). Relationship between hopelessness and ultimate suicide: a replication with psychiatric outpatients. American Journal of Psychiatry, 147(2), 190–195. [DOI] [PubMed] [Google Scholar]
- Beck AT, Brown G, & Steer RA (1989). Prediction of eventual suicide in psychiatric inpatients by clinical ratings of hopelessness. Journal of Consulting and Clinical Psychology, 57(2), 309–310. [DOI] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, & Trexler L (1974). The measurement of pessimism: the hopelessness scale. Journal of Consulting and Clinical Psychology, 42(6), 861–865. [DOI] [PubMed] [Google Scholar]
- Berman MG, Kross E, Krpan KM, Askren MK, Burson A, Deldin PJ, … Jonides J (2012). Interacting with nature improves cognition and affect for individuals with depression. J Affect Disord, 140(3), 300–305. doi: 10.1016/j.jad.2012.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, & Bohlmeijer E (2013). Positive psychology interventions: a meta-analysis of randomized controlled studies. BioMed Central Public Health, 13, 119. doi: 10.1186/1471-2458-13-119 1471-2458-13-119 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calabrese JR, Hirschfeld RM, Frye MA, & Reed ML (2004). Impact of depressive symptoms compared with manic symptoms in bipolar disorder: results of a U.S. community-based sample. Journal of Clinical Psychiatry, 65(11), 1499–1504. [DOI] [PubMed] [Google Scholar]
- Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, & Hendrie HC (2002). Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care, 40(9), 771–781. [DOI] [PubMed] [Google Scholar]
- Celano CM, Beale EE, Mastromauro CA, Stewart JG, Millstein RA, Auerbach RP, … Huffman JC (2016). Psychological interventions to reduce suicidality in highrisk patients with major depression: a randomized controlled trial. Psychological Medicine, 1–12. doi: S0033291716002798 [pii] 10.1017/S0033291716002798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deckersbach T, Peters AT, Sylvia LG, Gold AK, da Silva Magalhaes PV, Henry DB, … Miklowitz DJ (2016). A cluster analytic approach to identifying predictors and moderators of psychosocial treatment for bipolar depression: results from STEP-BD. Journal of Affective Disorders, 203, 152–157. doi: 10.1016/j.jad.2016.03.064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorflinger LM, Fortin A. H. t., & Foran-Tuller KA (2016). Training primary care physicians in cognitive behavioral therapy: a review of the literature. Patient Education and Counseling, 99(8), 1285–1292. doi: 10.1016/j.pec.2016.02.014 [DOI] [PubMed] [Google Scholar]
- Fava GA, Rafanelli C, Cazzaro M, Conti S, & Grandi S (1998). Well-being therapy. A novel psychotherapeutic approach for residual symptoms of affective disorders. Psychological Medicine, 28(2), 475–480. [DOI] [PubMed] [Google Scholar]
- Fountoulakis KN, Vieta E, Young A, Yatham L, Grunze H, Blier P, … Kasper S (2016). The International College of Neuropsychopharmacology (CINP) Treatment Guidelines for Bipolar Disorder in Adults (CINP-BD-2017), Part 4: Unmet Needs in the Treatment of Bipolar Disorder and Recommendations for Future Research. The International Journal of Neuropsychopharmacology doi: 10.1093/ijnp/pyw072 [DOI] [PMC free article] [PubMed]
- Frye MA, Gitlin MJ, & Altshuler LL (2004). Unmet needs in bipolar depression. Depression and Anxiety, 19(4), 199–208. doi: 10.1002/da.20013 [DOI] [PubMed] [Google Scholar]
- Galfalvy H, Oquendo MA, Carballo JJ, Sher L, Grunebaum MF, Burke A, & Mann JJ (2006). Clinical predictors of suicidal acts after major depression in bipolar disorder: a prospective study. Bipolar Disorders, 8(5 Pt 2), 586–595. doi: BDI340 [pii] 10.1111/j.1399-5618.2006.00340.x [DOI] [PubMed] [Google Scholar]
- Herzberg PY, Glaesmer H, & Hoyer J (2006). Separating optimism and pessimism: a robust psychometric analysis of the revised Life Orientation Test (LOT-R). Psychological Assessment, 18(4), 433–438. doi: 2006-22005-008 [pii] 10.1037/1040-3590.18.4.433 [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, & Fang A (2012). The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognitive Therapy and Research, 36(5), 427–440. doi: 10.1007/s10608-012-9476-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JC, Albanese AM, Campbell KA, Celano CM, Millstein RA, Mastromauro CA, … Park ER (2016). The Positive Emotions after Acute Coronary Events behavioral health intervention: design, rationale, and preliminary feasibility of a factorial design study. Clinical Trials, 1740774516673365. doi: 10.1177/1740774516673365 [DOI] [PMC free article] [PubMed]
- Huffman JC, Beale EE, Celano CM, Beach SR, Belcher AM, Moore SV, … Januzzi JL (2016). Effects of optimism and gratitude on physical activity, biomarkers, and readmissions after an acute coronary syndrome: the Gratitude Research in Acute Coronary Events study. Circulation: Cardiovascular Quality and Outcomes, 9(1), 55–63. doi: 10.1161/circoutcomes.115.002184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JC, DuBois CM, Healy BC, Boehm JK, Kashdan TB, Celano CM, … Lyubomirsky S (2014). Feasibility and utility of positive psychology exercises for suicidal inpatients. General Hospital Psychiatry, 36(1), 88–94. [DOI] [PubMed] [Google Scholar]
- Huffman JC, Mastromauro CA, Boehm JK, Seabrook R, Fricchione GL, Denninger JW, & Lyubomirsky S (2011). Development of a positive psychology intervention for patients with acute cardiovascular disease. Heart Intl, 6(2), e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman JC, Millstein RA, Mastromauro CA, Moore SV, Celano CM, Bedoya CA, … Januzzi JL (2016). A positive psychology intervention for patients with an acute coronary syndrome: treatment development and proof-of-concept trial. Journal of Happiness Studies, 17(5), 1985–2006. doi: 10.1007/s10902-015-9681-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivtzan I, & Papantoniou A (2014). Yoga meets positive psychology: examining the integration of hedonic (gratitude) and eudaimonic (meaning) wellbeing in relation to the extent of yoga practice. Journal of Bodywork and Movement Therapies, 18(2), 183–189. doi: 10.1016/j.jbmt.2013.11.005 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. doi: 62/6/593 [pii] 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, … Ustun TB (2011). Development of lifetime comorbidity in the World Health Organization world mental health surveys. Arch Gen Psychiatry, 68(1), 90–100. doi: 10.1001/archgenpsychiatry.2010.180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyubomirsky S, King L, & Diener E (2005). The benefits of frequent positive affect: does happiness lead to success? Psychological Bulletin, 131(6), 803–855. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, & Layous K (2013). How do simple positive activities increase well-being? Current Directions in Psychological Science, .22(1), pp. doi: 10.1177/0963721412469809 [DOI] [Google Scholar]
- McCullough ME, Emmons RA, & Tsang JA (2002). The grateful disposition: a conceptual and empirical topography. Journal of Personality and Social Psychology, 82(1), 112–127. doi: 10.1037/0022-3514.82.1.112 [DOI] [PubMed] [Google Scholar]
- Miller S, Dell’Osso B, & Ketter TA (2014). The prevalence and burden of bipolar depression. Journal of Affective Disorders, 169 Suppl 1, S3–11. doi: 10.1016/s0165-0327(14)70003-5 [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Galfalvy H, Russo S, Ellis SP, Grunebaum MF, Burke A, & Mann JJ (2004). Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. American Journal of Psychiatry, 161(8), 1433–1441. doi: 10.1176/appi.ajp.161.8.1433 161/8/1433 [pii] [DOI] [PubMed] [Google Scholar]
- Picardi A, & Gaetano P (2014). Psychotherapy of mood disorders. Clinical Practice and Epidemiology in Mental Health, 10, 140–158. doi: 10.2174/1745017901410010140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, … Keller MB (2003). The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54(5), 573–583. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS, & Bridges MW (1994). Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. Journal of Personality and Social Psychology, 67(6), 1063–1078. doi: 10.1037/0022-3514.67.6.1063 [DOI] [PubMed] [Google Scholar]
- Seligman ME, Rashid T, & Parks AC (2006). Positive psychotherapy. American Psychologist, 61(8), 774–788. [DOI] [PubMed] [Google Scholar]
- Seligman ME, Steen TA, Park N, & Peterson C (2005). Positive psychology progress: empirical validation of interventions. American Psychologist, 60(5), 410–421. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, … Dunbar GC (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59 Suppl 20, 22–33;quiz 34–57. [PubMed] [Google Scholar]
- Sheldon KM, & Lyubomirsky S (2006). How to increase and sustain positive emotion: the effects of expressing gratitude and visualizing best possible selves. J Positive Psychology, 1, 73–82. [Google Scholar]
- Simon GE, Bauer MS, Ludman EJ, Operskalski BH, & Unutzer J (2007). Mood symptoms, functional impairment, and disability in people with bipolar disorder: specific effects of mania and depression. Journal of Clinical Psychiatry, 68(8), 1237–1245. [DOI] [PubMed] [Google Scholar]
- Sin NL, & Lyubomirsky S (2009). Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. Journal of Clinical Psychology, 65(5), 467–487. [DOI] [PubMed] [Google Scholar]
- Swartz HA, & Swanson J (2014). Psychotherapy for bipolar disorder in adults: a review of the evidence. Focus (American Psychiatric Publishing), 12(3), 251–266. doi: 10.1176/appi.focus.12.3.251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thase ME (2007). STEP-BD and bipolar depression: what have we learned? Current Psychiatry Reports, 9(6), 497–503. [DOI] [PubMed] [Google Scholar]
- Trivedi MH (2009). Tools and strategies for ongoing assessment of depression: a measurement-based approach to remission. Journal of Clinical Psychiatry, 70 Suppl 6, 26–31. doi: 10.4088/JCP.8133su1c.04 [DOI] [PubMed] [Google Scholar]
- Trivedi MH, Wisniewski SR, Morris DW, Fava M, Gollan JK, Warden D, … Rush AJ (2011). Concise Health Risk Tracking scale: a brief self-report and clinician rating of suicidal risk. Journal of Clinical Psychiatry, 72(6), 757–764. doi: 10.4088/JCP.11m06837 11m06837 [pii] [DOI] [PubMed] [Google Scholar]
- Valtonen HM, Suominen K, Haukka J, Mantere O, Leppamaki S, Arvilommi P, & Isometsa ET (2008). Differences in incidence of suicide attempts during phases of bipolar I and II disorders. Bipolar Disorders, 10(5), 588–596. doi: 10.1111/j.1399-5618.2007.00553.x BDI553 [pii] [DOI] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1984). Negative affectivity: the disposition to experience aversive emotional states. Psychological Bulletin, 96(3), 465–490. [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.