Abstract
Background
Faculty vitality is the main ingredient to enhance professional education and competence. Enriching the faculty vitality in key domains of teaching, assessing, research, professionalism, and administration is perceived to improve educational environment significantly and enhances the academic performance of learners. Faculty development program (FDP) has been considered as a stand-alone educational pedagogy in fostering knowledge and professional skills of faculty. However, few studies have provided objective reports about the impact of such programs in a healthcare system.
Methods
This research was conducted by selecting data sources of PubMed-Medline, Wiley online library, Cochrane library, Taylor & Francis Online, CINAHL, Springer link, Proquest, ISI Web of knowledge, ScienceDirect, EJS, EBSCO, Blackwell, Emerald and ABI Inform. This search followed a step-wise approach defined by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). A total of 37 studies that explored the impact of FDPs on medical and allied health faculty’s professional development were selected.
Results
This meta-analysis reported a mean effect size of 0.73 that reflects a significant and positive impact of FDPs in enhancing faculty’s knowledge and professional competence (z-statistics of 4.46 significant at p-value < 0.05) using the random effects model and forest plot.
Conclusion
This article reiterates the incorporation of FDPs in all healthcare institutions for improving the academic performance of faculty with resultant enrichment of learners’ knowledge and skills.
Keywords: Faculty, Medical and allied health faculty, Faculty development program, Healthcare institutions, Personal development
1. Introduction
Faculty development refers to a range of activities that are perceived to help academicians in improving their professional skills that are vital for carrying out their teaching, research or administrative activities in medical education (Kwan et al., 2009). In medical education conventions, faculty development has been considered to play a decisive role in sustaining academic vitality (Amin et al., 2009). Traditionally, the stereo-typed medical teachers were presumed to possess teaching capabilities based on knowledge of content and due to their own experience of how they were taught (Cate et al., 2014, Lim and Choy, 2014). Over the last 30 years, medical education has gradually evolved due to several reasons such as the emerging variations in healthcare standards and changing goal settings and desired outcomes, the effect of new technologies, and approaches in educational theory (Guraya et al., 2016c, Khoshhal and Guraya, 2016). This change has resulted in an improved landscape of medical education where current teachers are performing very different from the teachers by whom they were taught.
The professional development and academic stature of an institution's faculty members are connected to its educational vivacity (Guraya et al., 2016b). This can be materialized by a dynamic and energetic FDP that has been shown to lead to enhancement of faculty's skills in all the five desired domains, i.e., teaching, assessment, curriculum support, organizational leadership and mentoring (Guraya et al., 2016b). Faculty development endorses the educational improvements and strategies that are dignitary and are executed in a professional manner. Professional organizations and experts have recommended FDPs for greater awareness and attainment of knowledge in teaching and learning (Ghazvini et al., 2014, Jones et al., 2015). Steinert et al. (2009) have proposed key features of effective FD; usage of experiential learning; timely and effective feedback; peer and colleague relationships; well-organized interventions in models for principles of teaching and learning; and diverse educational strategies.
Over the past three decades, we have witnessed a staggering rise in the body of published literature about FDPs in medical, nursing and health sciences disciplines (McLean et al., 2008, Wilkerson and Irby, 1998). However, the impact and effectiveness of these programs on clinical and academic activities of participants have not been studied well (Irby and Hekelman, 1997, Reid et al., 1997). Furthermore, regardless of sustained availability and attentiveness in teaching development opportunities for faculty of STEM (Science, Technology, Engineering, and Mathematics), there is insignificant factual verification to establish the relevant effect of professional development programs on teaching practice (Garet et al., 2001, Henderson et al., 2011, Henderson et al., 2012). This systematic review and meta-analysis attempts to provide a quantitative analysis of the impact and effectiveness of FDPs in enhancing the professional competency and skills of medical and allied health science faculty.
2. Material and methods
This systematic review and meta-analysis was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) format suggested by Moher et al. (2009) in August 2016 to explore the impact of FDPs on professional development using MeSH terms: “faculty development,” “professional development,” “professional,” “competencies,” “career advancement,” “personal development,” and “medical education”. The databases searched included PubMed-Medline, Wiley online library, Cochrane library, Taylor & Francis Online, CINAHL, Springer link, Proquest, ISI Web of knowledge, ScienceDirect, EJS, EBSCO, Blackwell, Emerald, and ABI Inform. Full-text English original research studies, published during 2003–2016, were included in this search while editorials, personal opinions, commentaries, and review articles were excluded. The studies that investigated the following domains were included in this meta-analysis: the studies that explored the impact of FDPs on professional development and these studies must have reported their results empirically.
During initial search, 525 articles were retrieved as shown in Fig. 1. As many as 412 studies were excluded as these articles described general information about FDPs and did not probe the impact of professional development. Later, during the review of titles and abstracts, 63 studies were excluded as irrelevant. Only 50 studies were found relevant as they empirically explored the impact of FDPs on health care system. During full-text analysis of these 50 relevant studies, 13 were furtherer excluded due to inappropriate data for meta-analysis. Finally, a total of 37 relevant studies were finalized for this meta-analysis. A summary of 37 selected articles is shown in Appendix A which includes intervention type, setting and sample, research design, and key findings of each study. Faculty development fellowship is most commonly used intervention type among selected studies. Most of the studies are done in the USA setting on health professionals and academicians. Survey is most commonly employed research method among selected studies to evaluate the effectiveness of FDPs.
Fig. 1.
Flow diagram illustrating the selection of studies to explore the effectiveness of faculty development programs.
Meta-analysis was done using Forest plot that graphically presents the consistency and reliability of results of selected studies in a meaningful way. The Forest plot has been designed by following the steps recommended by Neyeloff et al. (2012). In this plot, the effect size of each study is computed as an outcome, and the pooled effect summary is also calculated to observe the heterogeneity across studies. Q test is the tool used for checking the heterogeneity in selected studies and its null hypothesis is that “all studies are identical.” The I squared (I2) statistic is an excellent method to ensure the quantity of heterogeneity in percentage terms, and it is a much better way to check the consistency of selected studies (Higgins et al., 2003). After carefully analyzing the heterogeneity, next step is to apply appropriate effect summary model fixed effects or random effects model. If heterogeneity is low, then it is better to apply fixed effects model while random effects model is most commonly used when heterogeneity is greater. The Tau squared (Tau2) estimates the between-study variance in random effects model. The level of significance in this study is 5% (P < .05). The study with pre-post design and interventional studies from the selected sample are analyzed through Review Manager 5.3 software (RevMan) developed by Cochrane Library (RevMan).
3. Empirical results
Table 1 shows the results of effect size measure and the random effects model for the selected 37 studies. The overall estimated average effect size is 0.73 with associated z-value 4.46, which is significant at 5% level of significance. This reflects a significant and positive impact of FDPs on professional development of faculty. However, there is significant heterogeneity among studies as the Q test value of 838.56 is statistically significant at 5% level of significance and this finding rejects the null hypothesis (all studies are equal). Further, I2 of 95.71%, indicates greater heterogeneity across the studies. Due to greater heterogeneity, the random effects model was more appropriate for adjusting the variation across studies. The results of random effects model show insignificant Qv of 24.5; the I2v heterogeneity level was adjusted to −46.41%. Finally, the random effects V value at 0.08 adjusted heterogeneity among the studies. The effect summary of the random effects model came out to be 0.072, which is used to portray the heterogeneity in studies through a forest plot graphically.
Table 1.
Breakdown of the empirical results of selected studies in this meta-analysis.
| Sr. | Study | Responses | Sample | ES | SE | CI lower | CI upper |
|---|---|---|---|---|---|---|---|
| 1 | Chang and Pribbenow (2016) | 260 | 272 | 0.96 | 0.06 | 0.84 | 1.07 |
| 2 | Behar-Horenstein et al. (2016) | 115 | 204 | 0.91 | 0.12 | 0.67 | 1.14 |
| 3 | Fleming et al. (2015) | 104 | 114 | 0.91 | 0.09 | 0.74 | 1.09 |
| 4 | Davis et al. (2015) | 51 | 53 | 0.96 | 0.13 | 0.70 | 1.23 |
| 5 | Jones et al. (2015) | 12 | 13 | 0.92 | 0.27 | 0.40 | 1.45 |
| 6 | Rahal et al. (2015) | 117 | 296 | 0.40 | 0.04 | 0.32 | 0.47 |
| 7 | Branch et al. (2014) | 52 | 58 | 0.90 | 0.12 | 0.65 | 1.14 |
| 8 | Lim and Choy (2014) | 39 | 95 | 0.41 | 0.07 | 0.28 | 0.54 |
| 9 | Chou et al. (2014) | 47 | 51 | 0.92 | 0.13 | 0.66 | 1.19 |
| 10 | Frantz et al. (2015) | 61 | 64 | 0.95 | 0.12 | 0.71 | 1.19 |
| 11 | Cate et al. (2014) | 16 | 29 | 0.55 | 0.14 | 0.28 | 0.82 |
| 12 | Ghazvini et al. (2014) | 15 | 76 | 0.20 | 0.05 | 0.10 | 0.30 |
| 13 | Singh et al. (2013) | 65 | 70 | 0.93 | 0.12 | 0.70 | 1.15 |
| 14 | Thompson et al. (2011) | 55 | 127 | 0.43 | 0.06 | 0.32 | 0.55 |
| 15 | Scarbecz et al. (2011) | 208 | 554 | 0.38 | 0.03 | 0.32 | 0.43 |
| 16 | Sarikaya et al. (2010) | 118 | 145 | 0.81 | 0.07 | 0.67 | 0.96 |
| 17 | Cilliers and Herman (2010) | 128 | 248 | 0.52 | 0.05 | 0.43 | 0.61 |
| 18 | Burdick et al. (2010) | 47 | 54 | 0.87 | 0.13 | 0.62 | 1.12 |
| 19 | Mukhtar (2010) | 45 | 65 | 0.69 | 0.10 | 0.49 | 0.89 |
| 20 | Haden et al. (2010) | 496 | 565 | 0.88 | 0.04 | 0.80 | 0.96 |
| 21 | Lown et al. (2009) | 40 | 43 | 0.93 | 0.15 | 0.64 | 1.22 |
| 22 | Steinert et al. (2009) | 16 | 48 | 0.33 | 0.08 | 0.17 | 0.50 |
| 23 | Kwan et al. (2009) | 25 | 37 | 0.68 | 0.14 | 0.41 | 0.94 |
| 24 | Boerboom et al. (2009) | 196 | 251 | 0.78 | 0.06 | 0.67 | 0.89 |
| 25 | Amin et al. (2009) | 223 | 272 | 0.82 | 0.05 | 0.71 | 0.93 |
| 26 | Beck et al. (2008) | 50 | 53 | 0.94 | 0.13 | 0.68 | 1.20 |
| 27 | Farley et al. (2008) | 240 | 954 | 0.25 | 0.02 | 0.22 | 0.28 |
| 28 | Gjerde et al. (2008) | 80 | 100 | 0.80 | 0.09 | 0.62 | 0.98 |
| 29 | Al-Musawi (2008) | 66 | 160 | 0.41 | 0.05 | 0.31 | 0.51 |
| 30 | Sullivan et al. (2006) | 149 | 156 | 0.96 | 0.08 | 0.80 | 1.11 |
| 31 | Thorndyke et al. (2006) | 38 | 56 | 0.68 | 0.11 | 0.46 | 0.89 |
| 32 | Searle et al. (2006) | 42 | 81 | 0.56 | 0.05 | 0.46 | 0.67 |
| 33 | Knight et al. (2005) | 200 | 242 | 0.83 | 0.06 | 0.71 | 0.94 |
| 34 | Sullivan et al. (2005) | 149 | 152 | 0.98 | 0.08 | 0.82 | 1.14 |
| 35 | Cole et al. (2004) | 210 | 228 | 0.92 | 0.06 | 0.80 | 1.05 |
| 36 | Osborn and DeWitt (2004) | 30 | 32 | 0.94 | 0.17 | 0.60 | 1.27 |
| 37 | Morzinski and Simpson (2003) | 30 | 35 | 0.86 | 0.16 | 0.55 | 1.16 |
Note: Mean ES = 0.73; z statistics = 4.46*; Q test = 838.56*; I2 = 95.71%; V = 0.08; Qv test = 24.59; Iv2 = −46.41%; and Effect summary (as) = 0.72 with confidence interval of 62.72–81.63%. * represents significance level of 5%.
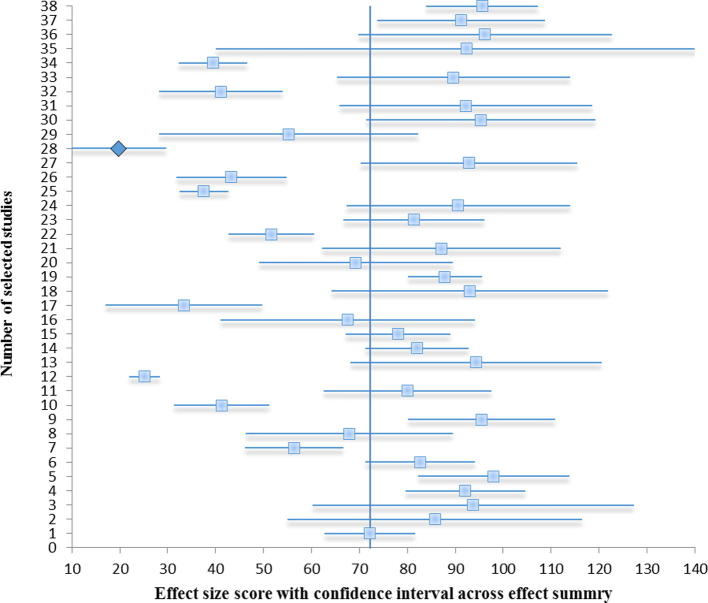
The Forest plot depicts a series of estimates and their confidence intervals at 95% level. Each study's effect size (outcome) is shown by a square per box and their confidence intervals represented by horizontal lines. At first glance, this plot reveals that the selected studies have wider confidence intervals and with inconsistent response rates that indicates gross heterogeneity.
Fig. 2 graphically presents studies in descending order from 2016 to 2003 and the effect summary at 72.17% of the random effects model with a confidence interval of 62.72–81.63%. We found great heterogeneity across all studies with few studies lies on the extreme left side. The forest plot shows that selected studies are not consistent and not reliable due to significant heterogeneity.
Fig. 2.
Effect size score with confidence interval using Forest plot. Note: Selected studies have been taken on the vertical axis. The horizontal axis has effect summary (random effects) which is relative point 72.17% in central line around individual study effect size (each study's effect size is shown by a square box and their confidence intervals represented by horizontal lines).
The results of Forest plots of pre-post design and intervention studies are shown in Fig. 3, Fig. 4. The ten pre-post design studies, with overall z statistics value at 4.21 showed p-value < 0.0001 significant at 1% level of significance that shows significantly enhanced the impact of FDPs on the professional development of faculty as shown in Fig. 3. The Q (Chi2 = 327.83) test is significant at 5% level of significance (p-value < 0.05) that rejects aforesaid null hypothesis (“all studies are identical”) and concludes that studies are not identical. By considerable heterogeneity, random effects model is the most appropriate model for this study. The effect summary represented by a diamond has a standardized mean difference (SMD) of 2.24 with confidence interval (1.20–3.28) and indicates positive impact of FDPs on professional development after intervention as it exceeds from the rule of thumb value of 0.8 suggested by Cohen (1988).
Fig. 3.
Forest plot of pre-post design studies.
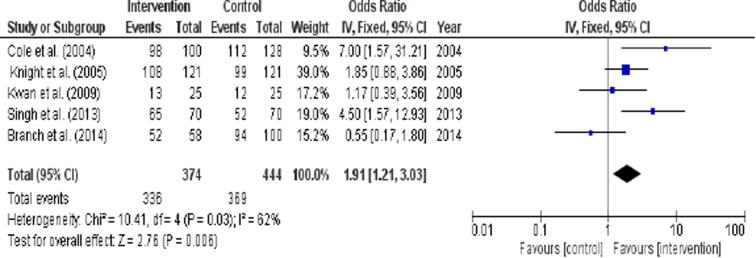
Fig. 4.
Forest plot of intervention studies.
Fig. 4 shows the results of 5 intervention studies, the overall Z test with value at 2.76 is significant at 1% level of significance (p < .006). This finding again endorses the significant positive impact of FDPs after intervention by fixed-effects model. The Q (Chi2 = 10.41) test is significant at 5% level of significance (p = .03), finding that reject the aforesaid null hypothesis (“all studies are identical”) and concludes that studies are not identical. The I2 value of 62% indicates low heterogeneity across studies, which shows that the fixed effects model is the most appropriate model for this study. The effect summary, represented by a diamond, with an odds ratio of 1.91 and confidence interval of 1.21–3.03 shows the positive impact of FDPs on professional development after intervention as it exceeds from the rule of thumb value 0.8 suggested by Cohen (1988).
4. Discussion
FDP is a contemplative educational platform that is inclusive of intended self-analysis, identification of a person's requirements, the work requirements, the recognition of spaces, and the decision about actions. It is best delivered in a structured format as workplace-based education that should be pitched to match learning styles of faculty for enhancing its effectiveness (Guraya et al., 2014a, Guraya, 2015). For a successful and satisfying career in academic medicine, continued professional development is the centrepiece (Farley et al., 2008). Morzinski and Simpson (2003) observed the results of a 2-year comprehensive FDP that was applied within their institution. The program's focal point was productivity and detainment of participants in academics, and all evaluation levels showed remarkable positive results. Sullivan et al. (2005) assessed the efficacy of their FDP in Palliative Care Education and Practice (PCEP), an extensive faculty enhancement program at Harvard Medical School. The authors suggested that combining clinical content with learning about educational processes was an efficient and effective avenue to improve clinical faculty’s ability to model and teach clinical care. Sullivan et al. (2006) examined the effect of FDP in Palliative Care Education and Practice (PCEP). The findings showed large-scale consistent variations across a range of domains in physician and nurse attitudes.
Gjerde et al. (2008) reported FDP to be helpful in improving professional skills and self-confidence of teachers. They observed the satisfaction of graduates with the program (Kirkpatrick). The program got scholarly and academic results. Through the program, the participants learned skills, and after the program, their confidence level enhanced. Interestingly, Kwan et al. (2009) examined the efficacy of an FDP that was offered to clinical faculty in promoting inter-professional education proficiencies. They reported no remarkable distinctions among the control and intervention groups and proposed that faculty development may truly be a vital but inadequate mediation in stimulating inter-professional education accomplishments. In contrast, our meta-analysis showed a striking and significant impact of FDPs in enriching faculty’s knowledge and skills.
Boerboom et al. (2009) investigated the effect of FDP on veterinary medical teachers and gathered the participants’ perceptions about their capability in seven distinct roles. The result showed that there was a positive impact on the perceived ability of veterinary medical teachers. Behar-Horenstein et al. (2010) demonstrated the achievement of consistent learning during professional development actions. Participants incorporated strategies that were taught during seminars and these strategies were by teaching critical thinking skills. Burdick et al. (2010) evaluated the impact of FDP in FAIMER Institute, an international health professions education fellowship that consolidates education content, leadership, and management topics through mixed methods in resource-rich countries. The outcomes showed that participation of health professions faculty from developing countries enhanced their knowledge and skills in educational leadership, management, and methodology, and the participants were able to apply the gained knowledge at their native institutions.
Lim and Choy (2014) investigated the effect of a structured foundational staff development programs on new academics in their role as classroom teachers in a problem-based learning (PBL) environment. The results revealed that the program had caused additions in knowledge relevant to basic rules or plans of self-directed learning, also a variation in academics’ orientation towards teaching and learning to a more developmental perspective that can be detected. Further, participants noticed that they were capable of using their learning for promoting key student behaviors in PBL, such as collaborative learning. Unfortunately, there is not a single unified educational and training framework for FDPs across the world. However, principles of academic integrity (Guraya et al., 2016c), emerging strands of teaching and assessing (Guraya et al., 2010), research and medical ethics (Guraya et al., 2016a), scholarly writing (Guraya, 2014, Guraya et al., 2014b), leadership (Khoshhal and Guraya, 2016), and updating the content knowledge are invariably included in the package of FDPs in all institutions.
In a study by Branch et al. (2014), authors have claimed that FDPs retain experiential learning and critical reflection and improves humanistic teaching and role modeling. Jones et al. (2015) explained the effect of FDPs on faculty's confidence and capability to aid inter-professional learning. The authors have demonstrated that this educational strategy efficiently trained faculty to facilitate inter-professional education and created a positive effect on their learning to take an active part in future activities. Zheng et al. (2017) shared the scheme, enactment and initial results of two FDPs to improve dental faculty's didactic skills, the Teaching and Learning Seminar Series and the Course Director Orientation. The participants purported that the programs encouraged them to enhance didactic practice and they increased their knowledge of didactic innovation. Some faculty members proposed that execution of new instructional plans and tools was helpful in generating an active and communicative learning environment that was liked by their students. Fleming et al. (2015) investigated the draft, execution, and capability of a faculty development program in a category of early-career junior faculty. This group training program for junior faculty was effectual in enhancing the self-reported knowledge, skills, and attitudes that are vital to advance early career promotion and group networking, particularly for females. Davis et al. (2015) observed a positive effect of facilitator development course and participation in the teaching activity on perceived knowledge, skills and behaviors toward inter-professional teamwork. Frantz et al. (2015) focused on the judgment of the perceptions of participants about the effect of SAFRI fellowship on their personal and professional development. They used Kirkpatrick's evaluation framework. Although this paper has mainly underpinned positive and significant effect of faculty development program in fostering the faculty’s professional competence, the incorporation and establishment of such programs demand resources, staff, space, budget, and commitment by a dedicated team of organizers. There should be clearly defined goals, purposes, and models that can conveniently guide and influence program development in congruence with the institution’s vision and mission.
4.1. Study limitations
This systematic review and meta-analysis included empirical studies that analyzed the impact of FDPs in all medical and allied heal disciplines. A more precise and dedicated analysis could have been the review and quantitative analysis of studies on only one of the disciplines in health care. This might be a future effort that can explicitly explore the impact of FDP in a single field of health care system.
5. Conclusions
This systematic review and meta-analysis emphatically endorses the effectiveness and positive impact of FDPs in healthcare institutions. FDPs have been shown to foster the teaching, assessing, research, leadership, and administrative skills of medical and allied health faculty. However, there is not a unified and standard faculty educational framework, but the programs can be structured and tailored to match the desired goals and educational needs. Such programs demand resources, budget, administrative efforts and support, space, and commitment. Although institutions practice such programs, however, a well-structured theoretical framework that can be incorporated across institutions is not available. The results of this meta-analysis urge the educators in developing an educational framework that can precisely address the faculty needs and expertise. The key features of faculty development that equip educators with tools to teach and consolidate their core knowledge should be embedded within institutional support programs. Per se, a single model of FDP cannot be applied across all disciplines due to varying dynamics of each subject. However owing to the added value of this program, a useful approach can be employed by floating a needs analysis survey. Such exercise will identify the needs and desired strands of FDP that will be then conveniently tailored to meet the defined goals.
Acknowledgments
Conflict of interest
The authors have no conflicts of interest.
Acknowledgements
This research is supported by the National Natural Science Foundation of China under the project of (NSFC-71372016, 71672009) and Specialized Research Fund for Doctoral Program of Higher Education of China (SRFD-20131101110053).
Footnotes
Peer review under responsibility of King Saud University.
Appendix A. Summary of selected studies.
| Sr. | Study | Intervention type | Setting and sample | Study Design | Key findings |
|---|---|---|---|---|---|
| 1 | Chang and Pribbenow (2016) | Fellowship | USA, 260 Health professionals from 26 disciplines from 2010 to 2014 | Mixed methods | Fellowship accomplished its anticipated objective of faculty professional development. |
| 2 | Behar-Horenstein et al. (2016) | Faculty development | USA, 115 Florida’s dental hygiene and dental assisting faculty | Survey | Faculty should offer educational experiences to boost the teaching and leadership abilities of their related dental faculty. |
| 3 | Fleming et al. (2015) | Short course in small groups | USA, 104 junior faculty members from different disciplines of health | Survey | Findings suggest that program has significantly changed the faculty’s perceived professional development. |
| 4 | Davis et al. (2015) | Inter-professional training | USA, 51 facilitators in inter-professional education from all disciplines | Experimental design | Findings show a positive impact on perceived knowledge, skills and attitudes toward inter-professional education. |
| 5 | Jones et al. (2015) | Inter-professional training | USA, 12 faculty members from the Colleges of Pharmacy and Health Sciences | Mixed methods | The program has successfully organized faculty to facilitate IPE as well as positively influenced their wish to contribute to future activities. |
| 6 | Rahal et al. (2015) | Workshops | Lebanon, 117 faculty members of academic and clinical departments | Survey | Faculty was interested in FDP, but they face challenges to achieve personal and professional goals. |
| 7 | Branch et al. (2014) | Fellowship | USA, 52 faculty members from 8 academic medical centers while 94 faculty members as control group | Experimental design | Longitudinal, intensive faculty development that employs experiential learning and critical reflection likely enhances humanistic teaching and role modeling. |
| 8 | Lim and Choy (2014) | Workshops | Singapore, 39 new faculty members | Mixed methods | The program has resulted in increased knowledge of principles and policies of self-directed learning. |
| 9 | Chou et al. (2014) | Facilitator Training Program | USA, 47 alumni | Mixed methods | The program is an effective learning that enhances faculty skills in principles of relationship-centred care. |
| 10 | Frantz et al. (2015) | Fellowship | Sub-Saharan Africa, 61 alumni members | Retrospective | Fellowship has a positive impact on the personal and professional development of faculty members. |
| 11 | Cate et al. (2014) | International Medical Educators Exchange (IMEX) | Netherlands, Canada, Sweden and the UK, 16 faculty members from IMEX alumni | Survey | IMEX has recognized as being an important faculty development opportunity for medical educators. |
| 12 | Ghazvini et al. (2014) | Workshops | Iran, 15 faculty members | Survey (pre-post) | The findings indicate that the program had a positive impact on participants’ abilities and they were highly satisfied. |
| 13 | Singh et al. (2013) | Fellowship | India and South Africa, 65 fellowship group and 52 non-fellowship | Quasi-experimental | Fellowship has an incremental impact on faculty members’ knowledge and skills gained. |
| 14 | Thompson et al. (2011) | Fellowship | USA, 55 medical teachers from different schools | Survey | Fellowship has a positive impact on participants’ teaching abilities, curriculum design, and research work. |
| 15 | Scarbecz et al. (2011) | Fellowship | USA, 208 faculty members | Survey | Fellowship has a positive impact on faculty members’ personal and professional growth. |
| 16 | Sarikaya et al. (2010) | Faculty training program | Turkey, 118 faculty members | Survey (pre-post) | There is a significant change in the behaviour of faculty members, and program has improved their skills. |
| 17 | Cilliers and Herman (2010) | Education development | South Africa, 128 faculty members | Mixed methods | Program has significant positive influence on personal and professional faculty members. |
| 18 | Burdick et al. (2010) | Fellowship | 19 countries in South America, Africa, and South Asia, 47 health professionals | Mixed methods | Participants perceived enhancement in their abilities and knowledge in management, education leadership, and experience in implementing FDPs at their home institutions. |
| 19 | Mukhtar (2010) | Workshops | Pakistan, 45 dental and medical professionals | Survey | Professionals require developmental training to improve their skills, but there is a lack of quality trainers. |
| 20 | Haden et al. (2010) | Fellowship | USA, 496 professionals from 49 members institutions | Survey | Professionals are extremely interested in personal and professional growth and career advancement. |
| 21 | Lown et al. (2009) | Fellowship | USA, 40 alumni members of fellowship in medical education | Qualitative | The most common theme is the improvement of knowledge about medical education and teaching skills. |
| 22 | Steinert et al. (2009) | Workshops | Canada, Focus group of 16 clinical teachers | Qualitative | Personal and career development are the main priorities of clinical teachers. |
| 23 | Kwan et al. (2009) | Fellowship | Canada, 25 professionals from various disciplines (13 in experimental group while 12 as control group) | Pre-post randomized control group | After the program, there is a significant expansion of knowledge and professional development. |
| 24 | Boerboom et al. (2009) | Fellowship | Netherlands, veterinary medical teachers. | Survey | Fellowship has a positive impact on the perceived competence of respondents. |
| 25 | Amin et al. (2009) | Faculty development | Singapore, 223 faculty members from different institutions | Survey | Respondents’ main priority is personal growth as they stated advanced knowledge regarding their teaching. |
| 26 | Beck et al. (2008) | Fellowship | USA, 50 faculty members from 29 states and Puerto Rico | Survey (pre-post) | Participants viewed fellowship productive after training as it enhances their skills and confidence. |
| 27 | Farley et al. (2008) | Faculty development | USA, 240 junior clinicians in emergency medicine | Survey | Junior faculty requires a faculty development for their career needs, especially for personal and professional growth. |
| 28 | Gjerde et al. (2008) | Fellowship | USA, 80 graduates of fellowship | Survey | The program has positive impacts on the abilities and the confidence of participants. |
| 29 | Al-Musawi (2008) | Workshops | Oman, 66 faculty members of Sultan Qaboos University | Survey | Professional development workshops are very productive, and faculty needs more innovate methods and on merit selection. |
| 30 | Sullivan et al. (2006) | Fellowship | North America and Europe, 149 Physician and nurse educators | Survey (pre-post) | The educational model has a measurable impact on practices and professional development of physician and nurse educators. |
| 31 | Thorndyke et al. (2006) | Fellowship | USA, 38 junior faculty members | Survey | The program increased the participants’ perception of their capabilities and resulted in their career development. |
| 32 | Searle et al. (2006) | Fellowships | North America, 40 faculty members in various medical schools | Survey | It seems that effective programs necessarily meet the needs and do not go beyond the resources of their institutes. |
| 33 | Knight et al. (2005) | Fellowship | USA states and Canada, 200 alumni of Johns Hopkins Faculty Development Program and 99 control group | Experimental | Participation in FDP was linked with unrelenting teaching activities, expected teaching actions, and high self-assessments associated with providing feedback and learner-centeredness. |
| 34 | Sullivan et al. (2005) | Fellowship | USA, 149 Physicians and faculty members of medical schools | Surveys | The program provides an educational model that motivates variations in practice, involves practitioners, and suggests opportunities for professional reactivation. |
| 35 | Cole et al. (2004) | Fellowship | USA, 98 faculty members participants and 112 non-participants as control | Experimental | Participants’ professional and teaching skills significantly improved as compared to non-participants. |
| 36 | Osborn and DeWitt (2004) | Fellowship | USA, 32 executive leadership track scholars | Survey (pre-post) | Findings show that program has resulted in advocates for medical education and also the effective leaders. |
| 37 | Morzinski and Simpson (2003) | Fellowship | USA, 30 family medicine faculty members | Survey (pre-post) | Findings show substantial positive changes in participants’ presentations, capabilities, leadership, and publications. |
References
- Al-Musawi A. Faculty perceptions of the professional development workshops conducted at Sultan Qaboos University. J. Uni. Teach. Learn. Prac. 2008;5:92–104. [Google Scholar]
- Amin Z., Eng K.H., Seng C.Y., Hoon T.C., Sun G.P., Samarasekera D.D., Huak C.Y., Rhoon K.D. A multi-institutional survey on faculty development needs, priorities and preferences in medical education in an Asian medical school. Med. Educ. Online. 2009;14:16. doi: 10.3885/meo.2009.Res00317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck E., Wingard D.L., Zuniga M.L., Heifetz R., Gilbreath S. Addressing the health needs of the underserved: a national faculty development program. Acad. Med. 2008;83:1094–1102. doi: 10.1097/ACM.0b013e3181890484. [DOI] [PubMed] [Google Scholar]
- Behar-Horenstein L.S., Childs G.S., Graff R.A. Observation and assessment of faculty development learning outcomes. J. Dent. Educ. 2010;74:1245–1254. [PubMed] [Google Scholar]
- Behar-Horenstein L.S., Garvan C.W., Catalanotto F.A., Su Y., Feng X. Assessing faculty development needs among Florida's allied dental faculty. J. Dent. Hyg. 2016;90:52–59. [PubMed] [Google Scholar]
- Boerboom T., Dolmans D., Muijtjens A., Jaarsma A., Beukelen P.V., Scherpbier A. Does a faculty development programme improve teachers’ perceived competence in different teacher roles? Med. Teach. 2009;31:1030–1031. doi: 10.3109/01421590903183779. [DOI] [PubMed] [Google Scholar]
- Branch W.T., Jr., Chou C.L., Farber N.J., Hatem D., Keenan C., Makoul G., Quinn M., Salazar W., Sillman J., Stuber M., Wilkerson L., Mathew G., Fost M. Faculty development to enhance humanistic teaching and role modeling: a collaborative study at eight institutions. J. Gen. Intern. Med. 2014;29:1250–1255. doi: 10.1007/s11606-014-2927-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdick W.P., Diserens D., Friedman S.R., Morahan P.S., Kalishman S., Eklund M.A., Mennin S., Norcini J.J. Measuring the effects of an international health professions faculty development fellowship: the FAIMER Institute. Med. Teach. 2010;32:414–421. doi: 10.3109/01421590903394587. [DOI] [PubMed] [Google Scholar]
- Cate O.T., Mann K., McCrorie P., Ponzer S., Snell L., Steinert Y. Faculty development through international exchange: the IMEX initiative. Med. Teach. 2014;36:591–595. doi: 10.3109/0142159X.2014.899685. [DOI] [PubMed] [Google Scholar]
- Chang A.L., Pribbenow C.M. The ASM-NSF biology scholars program: an evidence-based model for faculty development. J. Microbiol. Biol. Educ. 2016;17:197. doi: 10.1128/jmbe.v17i2.1094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou, C.L., Hirschmann, K., Fortin, A.H.t., Lichstein, P.R., 2014. The impact of a faculty learning community on professional and personal development: the facilitator training program of the American Academy on Communication in Healthcare. Acad. Med. 89, 1051–1056. [DOI] [PubMed]
- Cilliers F.J., Herman N. Impact of an educational development programme on teaching practice of academics at a research-intensive university. Int. J. Acad. Dev. 2010;15:253–267. [Google Scholar]
- Cohen J. second ed. L. Erlbaum Associates, New Jersey; Hillsdale, N.J.: 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- Cole K.A., Barker L.R., Kolodner K., Williamson P., Wright S.M., Kern D.E. Faculty development in teaching skills: an intensive longitudinal model. Acad. Med. 2004;79:469–480. doi: 10.1097/00001888-200405000-00019. [DOI] [PubMed] [Google Scholar]
- Davis B.P., Clevenger C.K., Posnock S., Robertson B.D., Ander D.S. Teaching the teachers: faculty development in inter-professional education. Appl. Nurs. Res. 2015;28:31–35. doi: 10.1016/j.apnr.2014.03.003. [DOI] [PubMed] [Google Scholar]
- Farley H., Casaletto J., Ankel F., Young K.D., Hockberger R. An assessment of the faculty development needs of junior clinical faculty in emergency medicine. Acad. Emerg. Med. 2008;15:664–668. doi: 10.1111/j.1553-2712.2008.00152.x. [DOI] [PubMed] [Google Scholar]
- Fleming G.M., Simmons J.H., Xu M., Gesell S.B., Brown R.F., Cutrer W.B., Gigante J., Cooper W.O. A facilitated peer mentoring program for junior faculty to promote professional development and peer networking. Acad. Med. 2015;90:819–826. doi: 10.1097/ACM.0000000000000705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frantz J.M., Bezuidenhout J., Burch V.C., Mthembu S., Rowe M., Tan C., Van Wyk J., Van Heerden B. The impact of a faculty development programme for health professions educators in sub-Saharan Africa: an archival study. BMC. Med. Edu. 2015;15:1–8. doi: 10.1186/s12909-015-0320-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garet M.S., Porter A.C., Desimone L., Birman B.F., Yoon K.S. What makes professional development effective? Results from a national sample of teachers. Am. Educ. Res. J. 2001;38:915–945. [Google Scholar]
- Ghazvini K., Mohammadi A., Jalili M. The Impact of the Faculty Development Workshop on Educational Research Abilities of Faculties in Mashhad University of Medical Sciences. Future. Med. Educ. J. 2014;4:24–27. [Google Scholar]
- Gjerde C.L., Hla K.M., Kokotailo P.K., Anderson B. Long-term outcomes of a primary care faculty development program at the University of Wisconsin. Fam. Med. 2008;40:579–584. [PubMed] [Google Scholar]
- Guraya S., Alzobydi A., Salman S. Objective structured clinical examination: Examiners’ bias and recommendations to improve its reliability. J. Med. Med. Sci. 2010;1:269–272. [Google Scholar]
- Guraya S.S., Guraya S.Y., Habib F.A., Khoshhal K.I. Learning styles of medical students at Taibah University: trends and implications. J. Res. Med. Sci. 2014;19:1155–1162. doi: 10.4103/1735-1995.150455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guraya S.Y. Accuracy of references in scholarly journals: an analysis of 450 references in ten biomedical journals. Eur. Sci. Ed. 2014;40:88–90. [Google Scholar]
- Guraya S.Y. Workplace-based assessment; applications and educational impact. Malays. J. Med. Sci. 2015;22:5–10. [PMC free article] [PubMed] [Google Scholar]
- Guraya S.Y., Guraya S.S., Almaramhy H.H. The legacy of teaching medical professionalism for promoting professional practice: a systematic review. Biomed. Pharmacol. J. 2016;9:809–817. [Google Scholar]
- Guraya S.Y., Guraya S.S., Mahabbat N.A., Fallatah K.Y., Al-Ahmadi B.A., ALalawi H.H. The Desired concept maps and goal setting for assessing professionalism in medicine. J. Clin. Diagn. Res. 2016;10:JE01–JE05. doi: 10.7860/JCDR/2016/19917.7832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guraya S.Y., London N.J.M., Guraya S.S. Ethics in medical research. J. Micro. Ultra. 2014;2:121–126. [Google Scholar]
- Guraya S.Y., Norman R.I., Roff S. Exploring the climates of undergraduate professionalism in a Saudi and a UK medical school. Med. Teach. 2016;38:630–632. doi: 10.3109/0142159X.2016.1150987. [DOI] [PubMed] [Google Scholar]
- Haden N.K., Chaddock M., Hoffsis G.F., Lloyd J.W., Reed W.M., Ranney R.R., Weinstein G.J. Preparing faculty for the future: AAVMC members' perceptions of professional development needs. J. Vet. Med. Educ. 2010;37:220–232. doi: 10.3138/jvme.37.3.220. [DOI] [PubMed] [Google Scholar]
- Henderson C., Beach A., Finkelstein N. Facilitating change in undergraduate STEM instructional practices: an analytic review of the literature. J. Res. Sci. Teach. 2011;48:952–984. [Google Scholar]
- Henderson C., Dancy M., Niewiadomska-Bugaj M. Use of research-based instructional strategies in introductory physics: where do faculty leave the innovation-decision process? Phys. Rev. Phys. Educ. Res. 2012;8:01–15. [Google Scholar]
- Higgins J., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irby D., Hekelman F. Future directions for research on faculty development. Fam. Med. 1997;29:287–289. [PubMed] [Google Scholar]
- Jones M., Schuer K.M., Ballard J.A., Taylor S.A., Zephyr D., Jones M.D. Outcomes of an immersive pilot faculty development program for interprofessional facilitation: a mixed methods study. J. Interprof. Care. 2015;1:83–89. [Google Scholar]
- Khoshhal K.I., Guraya S.Y. Leaders produce leaders and managers produce followers. A systematic review of the desired competencies and standard settings for physicians’ leadership. Saudi. Med. J. 2016;37:1061–1067. doi: 10.15537/smj.2016.10.15620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight A.M., Cole K.A., Kern D.E., Barker L.R., Kolodner K., Wright S.M. Long-term follow-up of a longitudinal faculty development program in teaching skills. J. Gen. Intern. Med. 2005;20:721–725. doi: 10.1111/j.1525-1497.2005.0145.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwan D., Barker K., Richardson D., Wagner S., Austin Z. Effectiveness of a faculty development program in fostering interprofessional education competencies. J. Res. Interprof. Pract. Educ. 2009;1:24–41. [Google Scholar]
- Lim L.A., Choy L.F.J. Preparing staff for problem-based learning: outcomes of a comprehensive faculty development program. Int. J. Res. Stud. Educ. 2014;3:53–68. [Google Scholar]
- Lown B.A., Newman L.R., Hatem C.J. The personal and professional impact of a fellowship in medical education. Acad. Med. 2009;84:1089–1097. doi: 10.1097/ACM.0b013e3181ad1635. [DOI] [PubMed] [Google Scholar]
- McLean M., Cilliers F., Van Wyk J.M. Faculty development: yesterday, today and tomorrow. Med. Teach. 2008;30:555–584. doi: 10.1080/01421590802109834. [DOI] [PubMed] [Google Scholar]
- Moher, D., Liberati, A., Tetzlaff, J., Altman, D.G., The PRISMA Group, 2009. Research methods and reporting. preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS. Med. 6, e1000097. [PMC free article] [PubMed]
- Morzinski J.A., Simpson D.E. Outcomes of a comprehensive faculty development program for local, full-time faculty. Fam. Med. 2003;35:434–439. [PubMed] [Google Scholar]
- Mukhtar F. Faculty development in medical institutions: where do we stand in Pakistan? J. Ayub. Med. Coll. Abbot. 2010;22:210–213. [PubMed] [Google Scholar]
- Neyeloff J.L., Fuchs S.C., Moreira L.B. Meta-analyses and Forest plots using a microsoft excel spreadsheet: step-by-step guide focusing on descriptive data analysis. BMC. Res. Notes. 2012;5:1–6. doi: 10.1186/1756-0500-5-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn L.M., DeWitt T. The HRSA-APA Faculty Development Scholars Program: executive leadership track. Ambul. Pediatr. 2004;4:98–102. doi: 10.1367/1539-4409(2004)004<0098:thfdsp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Rahal B., Mansour N., Zaatari G. Towards developing a sustainable faculty development program: an initiative of an American Medical School in Lebanon. J. Med. Liban. 2015;63:213–217. doi: 10.12816/0017970. [DOI] [PubMed] [Google Scholar]
- Reid A., Stritter F.T., Arndt J.E. Assessment of faculty development program outcomes. FM. 1997;29:242–247. [PubMed] [Google Scholar]
- RevMan. Review Manager (RevMan) is the software used for preparing and maintaining Cochrane Reviews. http://tech.cochrane.org/revman (accessed 10 September 2016).
- Sarikaya O., Kalaca S., Yeğen B.Ç., Cali S. The impact of a faculty development program: evaluation based on the self-assessment of medical educators from preclinical and clinical disciplines. Adv. Physiol. Educ. 2010;34:35–40. doi: 10.1152/advan.00024.2010. [DOI] [PubMed] [Google Scholar]
- Scarbecz M., Russell C.K., Shreve R.G., Robinson M.M., Scheid C.R. Faculty development to improve teaching at a health sciences center: a needs assessment. J. Dent. Educ. 2011;75:145–159. [PubMed] [Google Scholar]
- Searle N.S., Hatem C.J., Perkowski L., Wilkerson L. Why invest in an educational fellowship program? Acad. Med. 2006;81:936–940. doi: 10.1097/01.ACM.0000242476.57510.ce. [DOI] [PubMed] [Google Scholar]
- Singh T., de Grave W., Ganjiwale J., Supe A., Burdick W.P., van der Vleuten C. Impact of a fellowship program for faculty development on the self-efficacy beliefs of health professions teachers: a longitudinal study. Med. Teach. 2013;35:359–364. doi: 10.3109/0142159X.2013.769672. [DOI] [PubMed] [Google Scholar]
- Steinert Y., McLeod P.J., Boillat M., Meterissian S., Elizov M., Macdonald M.E. Faculty development: a ‘field of dreams’? Med. Edu. 2009;43:42–49. doi: 10.1111/j.1365-2923.2008.03246.x. [DOI] [PubMed] [Google Scholar]
- Sullivan A.M., Lakoma M.D., Billings J.A., Peters A.S., Block S.D. Teaching and learning end-of-life care: evaluation of a faculty development program in palliative care. Acad. Med. 2005;80:657–668. doi: 10.1097/00001888-200507000-00008. [DOI] [PubMed] [Google Scholar]
- Sullivan A.M., Lakoma M.D., Billings J.A., Peters A.S., Block S.D. Creating enduring change: demonstrating the long-term impact of a faculty development program in palliative care. J. Gen. Intern. Med. 2006;21:907–914. doi: 10.1111/j.1525-1497.2006.00486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson B.M., Searle N.S., Gruppen L.D., Hatem C.J., Nelson E.A. A national survey of medical education fellowships. Med. Educ. Online. 2011;16:5642. doi: 10.3402/meo.v16i0.5642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorndyke L.E., Gusic M.E., George J.H., Quillen D.A., Milner R.J. Empowering junior faculty: Penn State's faculty development and mentoring program. Acad. Med. 2006;81:668–673. doi: 10.1097/01.ACM.0000232424.88922.df. [DOI] [PubMed] [Google Scholar]
- Wilkerson L., Irby D.M. Strategies for improving teaching practices: a comprehensive approach to faculty development. Acad. Med. 1998;73:387–396. doi: 10.1097/00001888-199804000-00011. [DOI] [PubMed] [Google Scholar]
- Zheng M., Bender D., Nadershahi N. Faculty professional development in emergent pedagogies for instructional innovation in dental education. Eur. J. Dent. Educ. 2017;21:67–78. doi: 10.1111/eje.12180. [DOI] [PubMed] [Google Scholar]