Abstract
Objective
To investigate the validity of the 8th edition of the American Joint Committee on Cancer (AJCC) TNM staging system for gastric cancer.
Methods
The clinicopathologic data of 7371 patients who were diagnosed with gastric cancer and had 16 or more involved lymph nodes (LNs) were retrieved from the Surveillance, Epidemiology, and End Results (SEER) database and retrospectively reviewed.
Results
Stage migration occurred primarily during stage III between the 7th and 8th edition TNM staging systems. Stages IIIB and IIIC in the 7th edition staging system were divided in the 8th edition and had obvious differences in survival rates (both P < 0.001). The 8th edition TNM stages IIIC and IV showed similar survival rates (P = 0.101). The prognosis of patients with T4aN3bM0 was not different from that of patients with TxNxM1 (P = 0.433), while the prognosis of patients with T4bN3bM0 was significantly poorer than that of patients with TxNxM1 (P = 0.008). A revised TNM system with both T4aN3bM0 and T4bN3bM0 incorporated into stage IV was proposed. Multivariable regression analysis showed that the revised TNM system, but not the 7th and 8th editions, was an independent factor for disease-specific survival (DSS) in the third step of the analysis. Further analyses revealed that the revised TNM system had superior discriminatory ability to the 8th edition staging system, which was also an improvement over the 7th edition staging system.
Conclusion
The 8th edition of the AJCC TNM staging system is superior to the 7th edition for predicting the DSS rates of gastric cancer patients. However, for better prognostic stratification, it might be more suitable for T4aN3bM0/T4bN3bM0 to be incorporated into stage IV in the 8th edition TNM staging system.
1. Introduction
Although its incidence is declining, gastric cancer remains one of the most common malignant tumors throughout the world and the second leading cause of cancer-related death worldwide [1, 2]. Accurate categorization of the tumor stage, including the invasive depth, lymph node (LN) metastasis and optimization of T and N categories, is crucial for prognostic assessment and decision-making of the stage-specific therapeutic strategy [3]. The American Joint Committee on Cancer (AJCC) TNM staging system for gastric cancer is the most important independent prognostic factor, and this system has been revised several times over the past three decades [4–7]. The 7th edition of the AJCC staging system was published in 2010. Although many studies have demonstrated that the 7th edition TNM staging system is better for prognostic prediction and has better reproducibility than the previous TNM staging systems, several limitations still exist [8, 9]. One such limitation is that although the N3 category was divided into N3a (7-15 involved regional LNs) and N3b (≥16 involved regional LNs), these divisions were not incorporated throughout the TNM staging system, which could reduce the efficiency of its prognostic prediction. Another limitation is that the prognosis of patients with disease classified into parts of stage IIIc according to the 7th edition TNM system, including T4aN3bM0, T4bN3aM0, and T4bN3bM0, was similar to that of patients with stage IV, which reduced the prognostic stratification capacity between stage IIIC and stage IV. The 8th edition of the AJCC TNM staging system was introduced in 2017 and reflected several changes from the 7th edition, particularly regarding the combination of stage III [10–13]. Several studies [14–18] have reported that, compared with the 7th edition, the 8th edition provides better or comparable discrimination of overall survival differences among each TNM stage. However, little is known regarding the prognostic prediction ability of the 8th edition staging system for disease-specific survival (DSS) in gastric cancer, especially for patients with 16 or more examined LNs.
In light of this evidence, we performed a retrospective study with 7371 gastric cancer patients selected from the Surveillance, Epidemiology, and End Results (SEER) Program database to evaluate the efficacy and validity of the 8th edition of the AJCC TNM staging system for prognostic assessment and to provide guidelines for revising future editions of the AJCC staging system for gastric cancer staging.
2. Materials and Methods
2.1. Patients
A retrospective review of all gastric cancer patients from the SEER database between 1973 and 2013 was performed. A total of 99,253 patients from 18 SEER registries were initially screened. Cases were selected based on the primary site code (C16.0-C16.9, stomach) and associated histology codes (8021-8022, 8140, 8142-8145, 8210-8211, 8255, 8260-8263, 8323, 8480-8481, 8490, 8560, 8570, and 8574) [19, 20]. Patients with secondary tumors and negative histology were excluded. Patients were also excluded if they had not undergone lymphadenectomy (n = 24,834) or had fewer than 16 examined LNs (n = 62,065) or if incomplete information regarding T stage (n = 4918), N stage (n = 5), and M stage (n = 60) was available. Finally, a total of 7371 patients were enrolled in the study (Supplementary Figure 1).
2.2. Study Design
Patients' clinicopathological characteristics, such as age at diagnosis, gender, race, tumor site, tumor size, grade, T stage, N stage, and M stage, were collected. The pathological T stage, N stage, M stage, and final TNM stage were restaged to reflect the 7th and 8th editions of the AJCC staging system [10, 21]. Univariate survival analysis was used to assess the relationships between clinicopathological factors and DSS. To investigate the validity of the revised TNM system, a 3-step multivariate analysis was performed. In the 1st step, all the factors that were significant in the univariate analysis as well as the 7th edition TNM staging system were included; the 8th edition and the revised staging system were excluded. In the 2nd step, the 8th edition TNM staging system was also included but not the revised staging system. Finally, in the 3rd step, all three TNM systems were included.
2.3. Statistical Analysis
All enumeration and measurement data were analyzed using SPSS 17.0 for Windows. The univariate survival analysis was performed using the Kaplan-Meiermethod, and the significance of the differences between the groups was analyzed using the log-rank test. Stepwise multivariate survival analysis was performed using a Cox proportional hazards regression model to measure the independent contribution of each variable to survival. The concordance index (C-index), area under the curve (AUC) of the receiver operating characteristic (ROC) curve, and the Akaike information criterion (AIC) were used to measure the discriminatory ability of the models. For all analyses, only P < 0.05 was considered statistically significant.
3. Results
3.1. Patients and Demographics
For the present analysis, we enrolled 7371 gastric cancer patients from the SEER database who had 16 or more examined LNs and complete TNM staging and follow-up information. The majority of the patients were white (63.0%), 61.4% of the cohort was male, and the median age was 64 years. The total number of dissected LNs was 197,760, with an average of 26.8 ± 11.5 (mean ± standard deviation (SD)) dissected nodes per case. The mean number of metastatic nodes was 7.4 ± 9.5 overall. The median DSS for the entire cohort was 19 months (range, 0-119 months). The clinicopathological characteristics of all patients are listed in Supplementary Table 1.
3.2. Stage Migration
Table 1 reports changes in stage distribution between the 7th and 8th TNM classification systems for the overall gastric cancer group. Stages I, II, and IV showed almost no change. Only 3.4% of the cases classified by the 7th edition as stage IIIA shifted to be classified by the 8th edition as stage IIIB, whereas 44.2% of the stage IIIC cases shifted to stage IIIB according to the 8th edition TNM system. Cases that were classified as stage IIIB using the 7th edition system shifted either to the more advanced stage IIIC (23.8%) or to stage IIIA (24.1%) with the 8th edition TNM system. As shown, there were significant differences in survival for the 7th edition stage IIIB and IIIC (both P < 0.001) patients but not for the stage IIB (P = 0.221) and IIIA patients (P = 0.458) stratified according to the 8th edition TNM system. However, when stratified according to the 7th edition TNM system, significant differences in survival could not be observed for the 8th edition stage IIIA (P = 0.091) patients, but the 8th edition stage IIIB (P = 0.029) and IIIC (P = 0.006) patients showed significant differences.
Table 1.
Comparison of the 5-year survival rates based on the 7th edition of the TNM system and the 8th edition of the TNM system.
| 7th edition | 8th edition (5-YSR) | P value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| IA | IB | IIA | IIB | IIIA | IIIB | IIIC | IV | ||
| IA | 937 | N/A | |||||||
| IB | 517 | N/A | |||||||
| IIA | 915 | N/A | |||||||
| IIB | 808 (53.8%) | 8 (37.5%) | 0.221 | ||||||
| IIIA | 770 (43.0%) | 27 (50.8%) | 0.458 | ||||||
| IIIB | 328 (39.5%) | 709 (30.3%) | 324 (11.9%) | <0.001 | |||||
| IIIC | 536 (21.4%) | 676 (9.2%) | <0.001 | ||||||
| IV | 816 | N/A | |||||||
| P value | N/A | N/A | N/A | N/A | 0.091 | 0.029 | 0.006 | N/A | |
To investigate whether the number of examined LNs affected the stage migration from the 7th edition system to the 8th edition, patients were divided into two groups according to the total number of examined LNs [12]: 5320 patients with 16-29 examined LNs and 2051 patients with ≥30 examined LNs. As shown in Supplementary Table 2 and Supplementary Figure 2, for patients with 16-29 examined LNs, patients with disease classified by the 7th edition as stage IIIB and IIIC disease (both P < 0.001) had significant differences in survival when stratified according to the 8th edition system, which was consistent with the results obtained from the overall cohort. Interestingly, for patients with ≥30 examined LNs, there were significant differences in survival for those classified by the 7th edition with stages IIB, IIIB, and IIIC disease (all P < 0.001) but not for those classified by the 8th edition system with stage IIIA disease (P = 0.826). However, when stratified according to the 7th edition system, significant differences in survival could not be observed for all the subgroup of the 8th edition stage III patients (all P > 0.05) (Supplementary Table 3 and Supplementary Figure 2). These results suggested that the 8th edition system could provide better accuracy than the 7th edition for stage III stratification, especially for patients with ≥30 examined LNs.
3.3. Survival Analysis for the 7th and 8th Edition TNM Systems
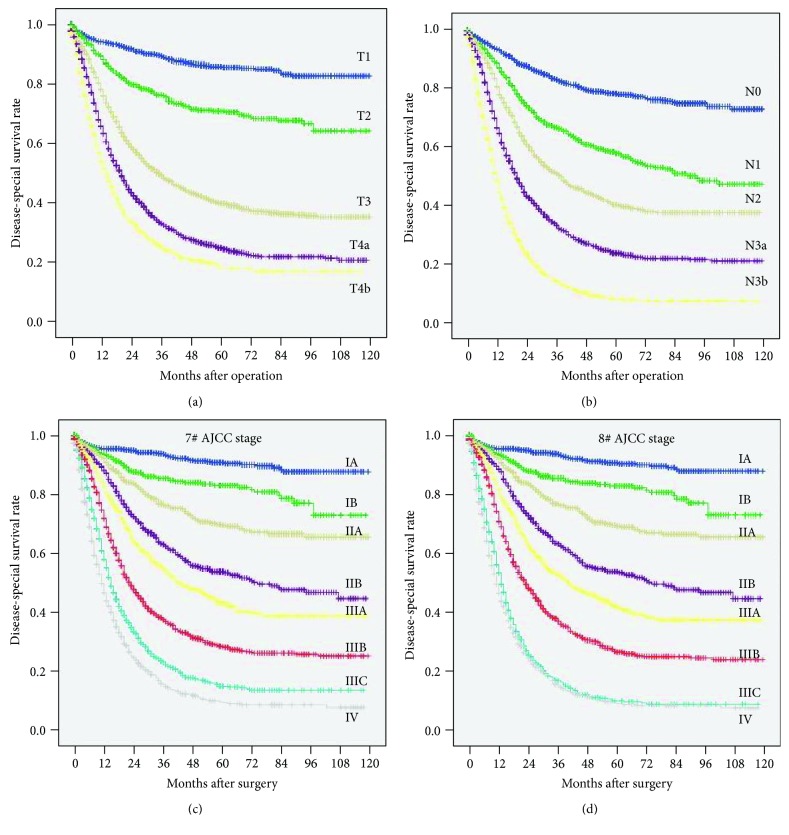
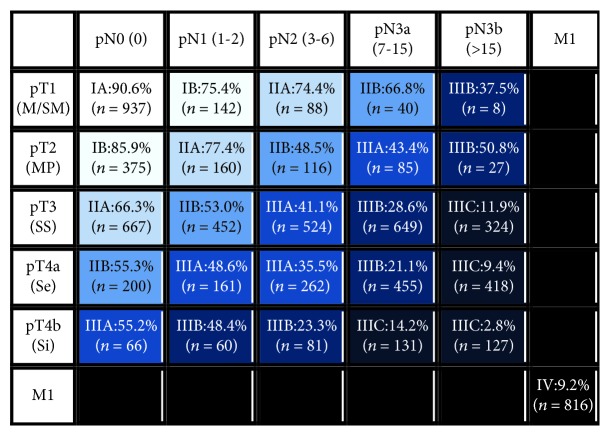
Comparisons of survival curves among patients with different T and N categories according to the 7th and 8th edition TNM systems are presented in Figures 1(a) and 1(b). Significant differences in prognosis were observed, including those between patients with the N3a and N3b categories (P < 0.001). Additionally, significantly different survival rates were observed among most of the groups classified by the two different editions of the TNM system (all P < 0.001), except between patients with stages IIIC and IV disease as classified by the 8th edition (Figures 1(c) and 1(d)). The 5-year survival rates according to the T and N categories are shown in Figure 2. For the patients with disease in each T category, survival was significantly different among patients with disease in different N categories (all P < 0.001). Similarly, for the patients with disease in each N category, survival was significantly different among patients with disease in different T categories (all P < 0.001). Moreover, significant differences in prognosis between the N3a and N3b categories were observed for patients with disease in the T3 (P < 0.001), T4a (P < 0.001), and T4b (P < 0.001) categories but not for those with disease in the T1 (P = 0.332) and T2 (P = 0.610) categories.
Figure 1.
Comparison of survival curves. (a) According to the 8th edition T category. (b) According to the 8th edition N category. (c) According to the 7th edition AJCC TNM stage. (d) According to the 8th edition AJCC TNM stage.
Figure 2.
Five-year survival rates according to the 8th edition T and N categories.
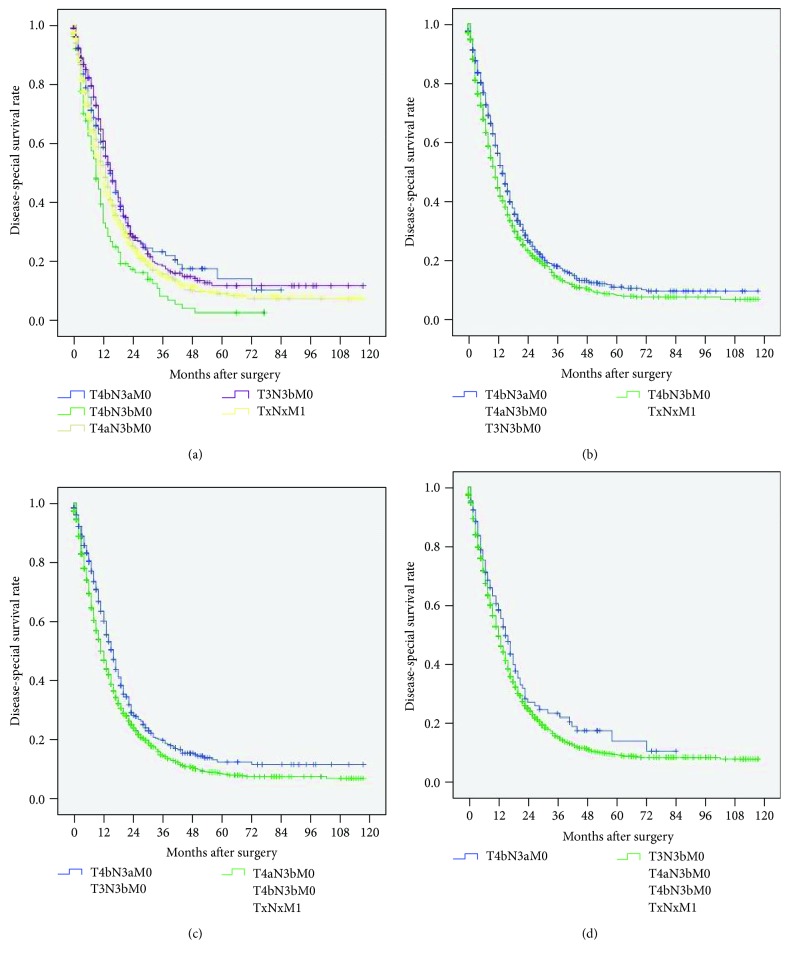
3.4. Revised TNM System
In the 8th edition TNM system, patients with stages IIIC and IV disease showed similar survival rates (P = 0.101, Figure 1(d)). Further analyses showed that the prognosis of patients with T4bN3aM0/T3N3bM0 disease was significantly better than that of patients with TxNxM1 disease (P = 0.044 and P = 0.002, Figure 3(a)), and the prognosis of patients with T4bN3bM0 disease was significantly worse than that of patients with TxNxM1 disease (P = 0.008, Figure 3(a)). Additionally, the prognosis of patients with T4aN3bM0 stage disease was not significantly different from that of patients with TxNxM1 stage disease (P = 0.433, Figure 3(a)). We hypothesized that T4bN3bM0, T4aN3bM0, and T3N3bM0 were incorporated step by step into stage IV so that the prognosis of patients with T4bN3bM0/TxNxM1 stage disease was significantly different from that of patients with T4aN3bM0/T4bN3aM0/T3N3bM0 stage disease (hazard ratio (HR): 1.047, 95% confidence interval (CI): 1.020-1.076, P = 0.001, Figure 3(b)); the prognosis of patients with T4bN3bM0/T4aN3bM0/TxNxM1 stage disease was significantly different from that of patients with T4bN3aM0/T3N3bM0 stage disease (HR: 1.062, 95% CI: 1.029-1.097, P < 0.001, Figure 3(c)), and the prognosis of patients with T4bN3bM0/T4aN3bM0/T3N3bM0/TxNxM1 stage disease was significantly different from that of patients with T4bN3aM0 stage disease (HR: 1.048, 95% CI: 0.993-1.106, P = 0.089, Figure 3(d)). Based on these results, we proposed a revised TNM system in which both T4aN3bM0 and T4bN3bM0 were incorporated into stage IV.
Figure 3.
Comparison of survival curves based on the 8th edition staging system. (a) Among T4bN3aM0/T4bN3bM0/T4aN3bM0/T3N3bM0/TxNxM1. (b) Between T4bN3aM0/T4aN3bM0/T3N3bM0 and T4bN3bM0/TxNxM1 (HR: 1.047, 95% CI: 1.020-1.076, P = 0.001). (c) Between T4bN3aM0/T3N3bM0 and T4aN3bM0/T4bN3bM0/TxNxM1 (HR: 1.062, 95% CI: 1.029-1.097, P < 0.001). (d) Between T4bN3aM0 and T4aN3bM0/T4bN3bM0/T3N3bM0/TxNxM1 (HR: 1.048, 95% CI: 0.993-1.106, P = 0.089).
3.5. Univariate Analysis and 3-Step Multivariate Analysis
In the univariate analysis, age, race, tumor site, tumor size, grade, the 7th edition TNM system, the 8th edition TNM system, and the revised TNM system were significantly correlated with survival (all P < 0.05). In the 1st step of multivariate analysis, age, race, tumor size, grade, and the 7th edition TNM system were confirmed to be independent prognostic factors (all P < 0.05). When the 8th edition TNM system was included in the 2nd step of multivariate analysis, it was also confirmed to be an independent prognostic factor (P < 0.05). However, when all three TNM systems were analyzed in the 3rd step, only the revised TNM system but not the 7th or 8th TNM staging systems was an independent prognostic factor (P < 0.05) (Table 2).
Table 2.
Univariate analysis and 3-step multivariate analysis of prognostic factors for gastric cancer patients.
| Univariate analysis | Multivariate analysis 1st | Multivariate analysis 2nd | Multivariate analysis 3rd | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | P value | HR | 95% CI | P value | HR | 95% CI | P value | HR | 95% CI | P value | |
| Age | 1.234 | 1.151-1.322 | <0.001 | 1.472 | 1.372-1.579 | <0.001 | 1.473 | 1.374-1.580 | <0.001 | 1.453 | 1.355-1.559 | <0.001 |
| Gender | 1.038 | 0.967-1.115 | 0.297 | |||||||||
| Race | 0.866 | 0.831-0.903 | <0.001 | 0.880 | 0.844-0.918 | <0.001 | 0.880 | 0.844-0.918 | <0.001 | 0.876 | 0.840-0.913 | <0.001 |
| Tumor site | 1.018 | 0.999-1.037 | 0.059 | |||||||||
| Tumor size | 1.373 | 1.310-1.440 | <0.001 | 1.139 | 1.080-1.200 | <0.001 | 1.135 | 1.077-1.197 | <0.001 | 1.120 | 1.062-1.182 | <0.001 |
| Grade | 1.220 | 1.167-1.275 | <0.001 | 1.113 | 1.056-1.174 | <0.001 | 1.110 | 1.052-1.170 | <0.001 | 1.099 | 1.042-1.159 | 0.001 |
| TNM stage (AJCC 7th) | 1.511 | 1.482-1.541 | <0.001 | 1.504 | 1.475-1.534 | <0.001 | 1.081 | 1.002-1.166 | 0.044 | |||
| TNM stage (AJCC 8th) | 1.530 | 1.500-1.560 | <0.001 | 1.413 | 1.310-1.524 | <0.001 | ||||||
| Revised TNM system | 1.501 | 1.482-1.511 | <0.001 | 1.333 | 1.249-1.410 | <0.001 | ||||||
3.6. The Revised TNM System Has Better Prognostic Stratification Than the Other Two Systems
The performances of all three TNM stage systems were assessed using the C-index, AUC, and AIC (Table 3 and Supplementary Figure 3). The 8th edition TNM system had a higher C-index (7th edition vs. 8th edition: 0.725 vs. 0.734), a higher AUC (0.770 vs. 0.773), and a smaller AIC value (56,463.140 vs. 56,396.524) than the 7th edition TNM system. A similar result was observed for stage III of the 8th edition compared with stage III of the 7th edition. However, the revised system had a higher C-index (8th edition vs. revised system: 0.734 vs. 0.741), a higher AUC (0.773 vs. 0.774), and a smaller AIC value (56,396.524 vs. 56,355.250) than the 8th edition TNM system. Taken together, these results revealed that the revised TNM system had superior discriminatory ability to the 8th edition system, which was also an improvement over the 7th edition system.
Table 3.
Comparison of the performance of various editions of the TNM staging system.
| Model | Concordance index | ROC curve | AIC | ||
|---|---|---|---|---|---|
| C-index | 95% CI | AUC | 95% CI | ||
| TNM stage (AJCC 7th) | 0.725 | 0.717-0.740 | 0.770 | 0.759-0.781 | 56,463.140 |
| TNM stage (AJCC 8th) | 0.734 | 0.720-0.741 | 0.773 | 0.762-0.783 | 56,396.524 |
| Stage III (AJCC 7th) | 0.594 | 0.581-0.607 | 0.607 | 0.587-0.626 | 31,552.480 |
| Stage III (AJCC 8th) | 0.608 | 0.599-0.624 | 0.621 | 0.602-0.640 | 31,515.240 |
| Revised TNM system | 0.741 | 0.730-0.748 | 0.774 | 0.763-0.784 | 56,355.250 |
ROC curve: receiver operating characteristic curve; AUC: area under curve; 95% CI: 95% confidence interval; AIC: Akaike information criterion.
4. Discussion
The TNM classification of cancer is the most important independent prognostic factor and is considered to play a fundamental role in treatment. For gastric cancer, several editions of the TNM system have been published in the past 30 years. Major changes in these editions have mainly focused on both the T staging system and the N staging system [7, 21]. The 7th edition of the AJCC TNM classification system released in 2010 has proven to be an excellent classification system and has been extensively used for gastric cancer staging worldwide. However, several problems, including N3a and N3b subcategories that do not require individual determinants in the final TNM stage, have been associated with its use [8, 22]. Consequently, the 8th edition of the AJCC TNM classification system for gastric cancer was published in 2017 and included major revisions in the N classifications and stage III. However, the validity of these revisions remains unknown.
In the present study, significant differences in survival were observed among patients with disease in different T categories according to the 8th edition staging system. Moreover, for patients with disease in each N category, there were significant differences in prognosis among those with disease in different T categories. These results indicate that the T staging system in the 8th edition has excellent prognostic stratification. Although the same subcategories of the N staging system are used in the 7th and 8th editions, the N3a and N3b categories are individual determinants of the final TNM stage in the 8th edition but not in the 7th edition. In the present study, for the 8th edition N staging system, significant differences in survival were observed between patients with disease in the N3a and N3b categories and among those with disease in different N categories. Additionally, for patients with disease in each T category, there were significant differences in prognosis among those with disease in different N categories, including the N3a and N3b categories. Our data are consistent with those of previous studies, which indicated that the prognosis of patients with more than 15 metastatic LNs is significantly worse than that of patients with 7-15 metastatic LNs [9, 23, 24]. These results suggest that it is reasonable to subclassify the N3 category into N3a and N3b subcategories and, more importantly, to include different determinants in the final TNM system.
In addition, stage migration mainly occurred in stage III between the 7th and 8th TNM systems. There were significant differences in survival among patients with disease classified by the 7th edition as stages IIIB and IIIC disease when they were stratified using the 8th edition TNM system. This result was similar to previous data showing that the overall survival rates were significantly different in patients with stages IIIB and IIIC disease as stratified by the 8th system whose disease was classified by the 7th edition system as stage IIIB disease [11]. However, no significant differences in prognosis were observed among patients with disease classified by the 8th edition as stage IIIA disease when they were stratified using the 7th edition TNM system. Moreover, the prognostic stratification for stage III disease according to the 8th edition system was superior to that of the 7th edition in terms of the HR (data not shown). These results further indicate that the 8th edition system can provide more reasonable classification with more power than the 7th edition system to subclassify patients with more homogenous prognoses.
However, drawbacks persist in the 8th edition of the TNM system. As the present study shows, there were no significant differences between the 8th edition stages IIIC and IV in terms of DSS rates. Moreover, similar prognoses were observed between patients with T4bN3aM0/T4bN3bM0/T4aN3bM0 and TxNxM1 disease when the prognoses of patients with disease in stage IIIC and stage IV subcategories were analyzed. Through the step-by-step incorporation of T4bN3bM0, T4aN3bM0, and T4bN3aM0 into stage IV, we further confirmed that the best prognostic stratification of stages IIIC and IV occurred when T4bN3bM0 and T4aN3bM0 were incorporated into stage IV. According to these results, we propose a revision of the 8th edition TNM staging system in which both T4bN3bM0 and T4aN3bM0 are incorporated into stage IV because of their similar prognoses.
To investigate the validity of the revised TNM system, a 3-step multivariate analysis was performed. In the 2nd step of the analysis, both the 7th and the 8th edition systems were confirmed to be independent predictors of patient survival. Additionally, compared with the 7th TNM system and its stage III, both the 8th TNM system and its stage III had better or at least comparable discriminatory ability, which was consistent with the findings of previous studies [12, 13]. These results indicate that the 8th TNM system is superior to the 7th system for predicting the 5-year DSS rates of gastric cancer patients due to the optimum prognostic stratification of stage III disease. However, when the revised system was also included in the 3rd step of the analysis, it became an independent predictor of survival, whereas both the 7th and 8th edition staging systems were no longer independent predictors. Most importantly, the proposed system had a higher C-index, a higher AUC, and a smaller AIC value than the 7th and 8th edition systems, which suggested that the revised system had superior discriminatory ability to the 7th and 8th edition systems. Although there were no extreme differences between the revised system and the 8th edition system, the revised system indeed had superior prognostic stratification for stage IIIC and stage IV disease. Therefore, our results demonstrated that the revised system is superior to the 7th and 8th edition systems for prognostic assessment.
The main limitation of the current study is its retrospective analysis setting. The impact of various treatment-related outcomes could not be evaluated fully in this study. Despite this limitation, our data provide important insight into the application of the 8th edition system and the revised TNM classification system for gastric cancer patients. Our study could be the basis for a subsequent prospective clinical study.
In conclusion, the present study demonstrates that the 8th TNM system is superior to the 7th system for predicting the 5-year DSS rates of gastric cancer patients due to the optimal prognostic stratification of stage III disease. However, for better prognostic stratification, we propose a revised TNM system in which T4aN3bM0 and T4bN3bM0 are incorporated into stage IV. Since the revised system was superior to the 8th edition system in terms of its discriminatory ability, we recommended that this system be considered for clinical application. Further studies should be carried out to confirm our results.
Acknowledgments
The authors thank Prof. Yao Lin for providing valuable advice. This work was funded by the Scientific and Technological Innovation Joint Capital Projects of Fujian Province (no. 2016Y9031), the MiaoPu Fund for Scientific Research, Fujian Medical University (no. 2014MP022), the Youth Research Project of Fujian Provincial Health and Family Planning Commission (2011532#), and the Startup Fund for Scientific Research, Fujian Medical University (no. 2016QH024).
Contributor Information
Chao-Hui Zheng, Email: wwkzch@163.com.
Chang-Ming Huang, Email: hcmlr2002@163.com.
Data Availability
The data used to support the findings of this study are available from the corresponding author upon request.
Ethical Approval
The study was approved by the Ethics Committee of Fujian Union Hospital.
Consent
Written consent was obtained from all patients whose information was stored in the hospital database and used for our research.
Conflicts of Interest
The authors have no conflicts of interest associated with the publication of this manuscript to declare.
Authors' Contributions
Chang-Ming Huang, Long-Long Cao, Jun Lu, and Jian-Xian Lin conceived the study, analyzed the data, and drafted the manuscript. Chao-Hui Zheng helped critically revise the manuscript for important intellectual content. Ping Li, Jian-Wei Xie, Jia-Bin Wang, Qi-Yue Chen, Mi Lin, and Ru-Hong Tu helped collect the data and design the study.
Supplementary Materials
Supplementary Figure 1: flow diagram of patient inclusion and exclusion. Supplementary Figure 2: comparison of survival curves according to the total examined lymph nodes (ELN). (A) The 7th edition AJCC stage for patients with 16-29 ELN. (B) The 8th edition AJCC stage for patients with 16-29 ELN. (C) The 7th edition AJCC stage for patients with ≥30 ELN. (D) The 8th edition AJCC stage for patients with ≥30 ELN. Supplementary Figure 3: predictive values of 7th and 8th edition AJCC stage and the revised system by receiver operating characteristic (ROC) curve. The area under curve (AUC) of the 7th and 8th edition AJCC stage and the revised system is 0.770 (95% IC: 0.759-0.781), 0.773 (0.762-0.783), and 0.774 (0.763-0.784), respectively. Supplementary Table 1: demographics and clinical characteristics of study patients. Supplementary Table 2: comparison of 5-year survival rate based on the 7th edition system according to the 8th edition system for patients with 16-29 examined lymph nodes. Supplementary Table 3: comparison of 5-year survival rate based on the 7th edition system according to the 8th edition system for patients with ≥30 examined lymph nodes.
References
- 1.Jemal A., Bray F., Center M. M., Ferlay J., Ward E., Forman D. Global cancer statistics. CA: a Cancer Journal for Clinicians. 2011;61(2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Plummer M., Franceschi S., Vignat J., Forman D., de Martel C. Global burden of gastric cancer attributable to Helicobacter pylori. International Journal of Cancer. 2015;136(2):487–490. doi: 10.1002/ijc.28999. [DOI] [PubMed] [Google Scholar]
- 3.Dicken B. J., Bigam D. L., Cass C., Mackey J. R., Joy A. A., Hamilton S. M. Gastric adenocarcinoma: review and considerations for future directions. Annals of Surgery. 2005;241(1):27–39. doi: 10.1097/01.sla.0000149300.28588.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hermanek P., Sobin L. H. TNM Classification of Malignant Tumors (UICC) 4th. Berlin: Springer; 1987. [DOI] [PubMed] [Google Scholar]
- 5.Sobin L. H., Wittekind C. H. TNM Classification of Malignant Tumors (UICC) 5th. New York: Wiley; 1997. [Google Scholar]
- 6.Sobin L. H., Gospodarowicz M. K., Wittekind C. International Union Against Cancer (UICC) TNM Classification of Malignant Tumors. 7th. New York: Wiley-Liss; 2010. [Google Scholar]
- 7.Greene F. L., Page D. L., Fleming I. D., et al. American Joint Committee on Cancer (AJCC) Cancer Staging Manual. 6th ed. New York: Springer; 2002. [DOI] [Google Scholar]
- 8.Sun Z., Wang Z. N., Zhu Z., et al. Evaluation of the seventh edition of American Joint Committee on Cancer TNM staging system for gastric cancer: results from a Chinese monoinstitutional study. Annals of Surgical Oncology. 2012;19(6):1918–1927. doi: 10.1245/s10434-011-2206-1. [DOI] [PubMed] [Google Scholar]
- 9.Marchet A., Mocellin S., Ambrosi A., et al. The ratio between metastatic and examined lymph nodes (N ratio) is an independent prognostic factor in gastric cancer regardless of the type of lymphadenectomy: results from an Italian multicentric study in 1853 patients. Annals of Surgery. 2007;245(4):543–552. doi: 10.1097/01.sla.0000250423.43436.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Amin M. B., Greene F. L., Edge S., et al. AJCC Cancer Staging Manual. 8th. New York: Springer; 2016. [Google Scholar]
- 11.Kim S. G., Seo H. S., Lee H. H., Song K. Y., Park C. H. Comparison of the differences in survival rates between the 7th and 8th editions of the AJCC TNM staging system for gastric adenocarcinoma: a single-institution study of 5,507 patients in Korea. Journal of Gastric Cancer. 2017;17(3):212–219. doi: 10.5230/jgc.2017.17.e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lu J., Zheng C. H., Cao L. L., et al. The effectiveness of the 8th American Joint Committee on Cancer TNM classification in the prognosis evaluation of gastric cancer patients: a comparative study between the 7th and 8th editions. European Journal of Surgical Oncology. 2017;43(12):2349–2356. doi: 10.1016/j.ejso.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 13.In H., Solsky I., Palis B., Langdon-Embry M., Ajani J., Sano T. Validation of the 8th edition of the AJCC TNM staging system for gastric cancer using the National Cancer Database. Annals of Surgical Oncology. 2017;24(12):3683–3691. doi: 10.1245/s10434-017-6078-x. [DOI] [PubMed] [Google Scholar]
- 14.Fang C., Wang W., Deng J. Y., et al. Proposal and validation of a modified staging system to improve the prognosis predictive performance of the 8th AJCC/UICC pTNM staging system for gastric adenocarcinoma: a multicenter study with external validation. Cancer Communications. 2018;38(1):p. 67. doi: 10.1186/s40880-018-0337-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang H., Guo W., Hu Y., et al. Superiority of the 8th edition of the TNM staging system for predicting overall survival in gastric cancer: comparative analysis of the 7th and 8th editions in a monoinstitutional cohort. Molecular and Clinical Oncology. 2018;9(4):423–431. doi: 10.3892/mco.2018.1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu J. Y., Peng C. W., Yang X. J., Huang C. Q., Li Y. The prognosis role of AJCC/UICC 8th edition staging system in gastric cancer, a retrospective analysis. American Journal of Translational Research. 2018;10(1):292–303. [PMC free article] [PubMed] [Google Scholar]
- 17.Fang W. L., Huang K. H., Chen M. H., et al. Comparative study of the 7th and 8th AJCC editions for gastric cancer patients after curative surgery. PLoS One. 2017;12(11, article e0187626) doi: 10.1371/journal.pone.0187626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.He X., Wu W., Lin Z., Ding Y., Si J., Sun L. M. Validation of the American Joint Committee on Cancer (AJCC) 8th edition stage system for gastric cancer patients: a population-based analysis. Gastric Cancer. 2018;21(3):391–400. doi: 10.1007/s10120-017-0770-1. [DOI] [PubMed] [Google Scholar]
- 19.Wang J., Sun Y., Bertagnolli M. M. Comparison of gastric cancer survival between Caucasian and Asian patients treated in the United States: results from the Surveillance Epidemiology and End Results (SEER) database. Annals of Surgical Oncology. 2015;22(9):2965–2971. doi: 10.1245/s10434-015-4388-4. [DOI] [PubMed] [Google Scholar]
- 20.Wang J., Dang P., Raut C. P., et al. Comparison of a lymph node ratio-based staging system with the 7th AJCC system for gastric cancer: analysis of 18,043 patients from the SEER database. Annals of Surgery. 2012;255(3):478–485. doi: 10.1097/SLA.0b013e31824857e2. [DOI] [PubMed] [Google Scholar]
- 21.Edge S. B., Byrd D. R., Compton C. C., Fritz A. G., Greene F. L. American Joint Committee on Cancer (AJCC) Cancer Staging Manual. 7th. Chicago: Springer; 2010. [Google Scholar]
- 22.Marrelli D., Morgagni P., de Manzoni G., et al. Prognostic value of the 7th AJCC/UICC TNM classification of noncardia gastric cancer: analysis of a large series from specialized Western centers. Annals of Surgery. 2012;255(3):486–491. doi: 10.1097/SLA.0b013e3182389b1a. [DOI] [PubMed] [Google Scholar]
- 23.Katai H., Yoshimura K., Maruyama K., Sasako M., Sano T. Evaluation of the New International Union Against Cancer TNM staging for gastric carcinoma. Cancer. 2000;88(8):1796–1800. doi: 10.1002/(SICI)1097-0142(20000415)88:8<1796::AID-CNCR6>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 24.Saito H., Fukumoto Y., Osaki T., et al. Prognostic significance of level and number of lymph node metastases in patients with gastric cancer. Annals of Surgical Oncology. 2007;14(5):1688–1693. doi: 10.1245/s10434-006-9314-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1: flow diagram of patient inclusion and exclusion. Supplementary Figure 2: comparison of survival curves according to the total examined lymph nodes (ELN). (A) The 7th edition AJCC stage for patients with 16-29 ELN. (B) The 8th edition AJCC stage for patients with 16-29 ELN. (C) The 7th edition AJCC stage for patients with ≥30 ELN. (D) The 8th edition AJCC stage for patients with ≥30 ELN. Supplementary Figure 3: predictive values of 7th and 8th edition AJCC stage and the revised system by receiver operating characteristic (ROC) curve. The area under curve (AUC) of the 7th and 8th edition AJCC stage and the revised system is 0.770 (95% IC: 0.759-0.781), 0.773 (0.762-0.783), and 0.774 (0.763-0.784), respectively. Supplementary Table 1: demographics and clinical characteristics of study patients. Supplementary Table 2: comparison of 5-year survival rate based on the 7th edition system according to the 8th edition system for patients with 16-29 examined lymph nodes. Supplementary Table 3: comparison of 5-year survival rate based on the 7th edition system according to the 8th edition system for patients with ≥30 examined lymph nodes.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.