Abstract
Objective:
To examine trends in 12-month post-fracture residual disability, nursing home placement, and mortality among patients with a hip fracture between 1990 and 2011.
Design:
Secondary analysis of 12-month outcomes from three cohort studies and control arms of two randomized controlled trials.
Setting:
Original studies were conducted as part of the Baltimore Hip Studies (BHS).
Participants:
Community-dwelling patients ≥65 years of age hospitalized for surgical repair of a non-pathological hip fracture (n=988).
Main Outcomes:
12-month residual disability, mortality, and nursing home residency were examined in case-mix adjusted models by sex and study. Residual disability was calculated by subtracting pre-fracture scores of Lower Extremity Physical Activities of Daily Living from scores at 12-months post fracture. We also examined the proportion of individuals with a 12-month score higher than their pre-fracture score (residual disability >0).
Results:
Only small improvements were seen in residual disability between 1990 and 2011. No significant differences were seen for men between BHS2 (enrollment 1990–1991; mean residual disability=3.1 activities, 95% CI: 2.16, 4.10) and BHS7 (enrollment 2006–2011; mean=3.1 activities, 95% CI: 2.41, 3.82). In women, residual disability significantly improved from BHS2 (mean=3.5 activities, 95% CI: 2.95, 3.99) to BHS3 (enrollment 1992–1995; mean=2.7 activities, 95% CI: 2.01, 3.30) with no significant improvements in later studies. After adjustment, a substantial proportion (91% of men and 79% of women) had a negative outcome (residual disability, died, or nursing home residence at 12 months) in the most recently completed study (BHS7).
Conclusions:
Over two decades, patients undergoing usual care post-hip fracture still had substantial residual disability. Additional clinical and research efforts are needed to determine how to improve hip fracture treatment, rehabilitation, and subsequent outcomes.
Keywords: Hip Fractures, Rehabilitation, Disability Evaluation, Outcome Assessment
INTRODUCTION
Hip fractures are a burdensome geriatric health problem. In 2010, over 250,000 older adults (≥65 years of age) were hospitalized for a hip fracture.1 Additionally, due to aging of the population, the number of hip fractures is expected to increase almost 12% in the United States between 2010 and 2030.2 Hip fracture patients have significant increases in disability, mortality, and nursing home admission over the 12-months post fracture, compared to age-matched controls.3 Patients also have an increased risk of subsequent hospitalizations.4 For those 65 and over, in 2005, the cost for hip fractures accounting for inpatient, outpatient, and long-term care was over 11 billion dollars.5
The recovery process after a hip fracture can take many months.6 Many patients do not reach their pre-fracture levels of mobility and independence.7 With respect to activities of daily living, 30%−75% of patients fail to return to their pre-fracture levels.8–10 Outcomes may also differ by sex.11
Mortality, nursing home residency, and disability after fracture has been frequently studied12–18. While secular trends in mortality12–16 and nursing home residency12,14 at 12-months after fracture have been examined, no study, to our knowledge, has investigated secular trends in disability among hip fracture survivors. Given the increasing burden and costly nature of hip fractures, it is important to understand whether outcomes among patients have improved over time given the potential for increases in disability attributable to hip fracture in the population. Due to changes in surgical management14, policy19, and extensive research on rehabilitation approaches20 over the last few decades, this study examined trends in residual disability, mortality, and nursing home placement among hip fracture patients between 1990 and 2011 using data from five longitudinal studies conducted in a metropolitan area.
METHODS
Study Sample
The Baltimore Hip Studies (BHS) began in 1983 to study outcomes in older adults with hip fractures. The BHS assessed recovery among hip fracture patients within five cohort studies (BHS19, BHS26, BHS321, BHS622, BHS723) and two randomized controlled trials (BHS424 and BHS525). These studies were approved by the Institutional Review Boards of the University and the individual study hospitals where recruitment took place. Informed consent was obtained from participants and/or their proxies.
Two of the BHS cohort studies (BHS1 and BHS6) were excluded from this secondary analysis because the primary outcome, Lower Extremity Physical Activities of Daily Living (LPADL) was not collected. All subjects from BHS2 (n=486), BHS3 (n=150), and BHS7 (n=233) were included. To focus on the natural history of hip fracture recovery for those receiving usual care, only those in the usual care arms of the randomized controlled trials (BHS4 [n=76] and BHS5 [n=44]) were included in the secondary analysis (i.e., intervention group was excluded).
Details of the design, enrollment period, entry criteria, sample composition, follow-up, and objectives of the five studies included in this secondary anlysis are displayed in Table 1. All studies enrolled individuals who were community-dwelling and admitted to the hospital for surgical repair of a non-pathologic hip fracture. Only two studies included men (BHS2 and BHS7).
Table 1.
Description of design, enrollment, eligibility, study sample, follow-up, and objectives of Baltimore Hip Studies (BHS) included in overall analysis.
| Study | Design | Enrollment Period | Entry Criteria | Sample Composition | Follow-Up from Time of Fracture | Objective |
|---|---|---|---|---|---|---|
| BHS26 | Prospective Cohort | 1990–1991 | Community-dwelling, ≥65 years of age | 152 Men 522 Women | 2, 6, 12, 18, 24 months | To identify factors that impact hip fracture survival and recovery |
| BHS321 | Prospective Cohort | 1992–1995 | White, community-dwelling | 205 Women | 2, 6, 12 months | To examine changes in muscle and bone after hip fracture |
| BHS424 | Randomized Controlled Trial | 1998–2004 | Community-dwelling, ≥65 years of age, cognitively intact, able to walk independently prior to fracture, no contraindications to exercise, cleared by orthopedic surgeon | 180 Women | 2, 6, 12 months | To determine the impact of exercise on bone metabolism post-fracture |
| BHS525 | Randomized Controlled Trial | 2000–2004 | Community-dwelling, ≥65 years of age, cognitively intact, able to walk independently prior to fracture, no contraindications to exercise | 208 Women | 2, 6, 12 months | To determine the effectiveness of exercise and motivation and exercise behavior and recovery after hip fracture |
| BHS723 | Prospective Cohort | 2006–2011 | Community-dwelling, ≥65 years of age, cognitively intact, ambulatory in six months prior to fracture | 168 Men 171 Women | 2, 6, 12 months | To compare hip fracture recovery between men and women |
Outcome Measures
The LPADL is a measure of lower extremity disability specifically adapted for hip fracture patients from the Functional Status Index.26 The same questionnaire was used for all studies. Subjects were asked if they performed and received help performing twelve activities (walk 10 feet, walk 1 block, climb 5 stairs, get into car, get in/out of bed, rise from an armless chair, put on pants, put on socks/shoes, get into/out of bath/shower, wash all parts of body, get on/off toilet, reach for item on ground). Responses for each activity were: no help, used equipment, used human assistance, used equipment and human assistance, did not perform due to health reasons, and did not perform due to non-health reasons.6 The LPADL score for each individual was the count of the number of activities in which a person was disabled, defined as needing equipment and/or human assistance or not performing a given task for a health reason. LPADL scores range from 0 to 12 with higher scores indicating more disability.
At baseline (<22 days post-hip fracture), individuals were asked to self-report the level of assistance needed in the week prior to fracture. At the 12-month post-fracture interview, survivors were asked, regardless of whether they resided in the community or not, to self-report on the level of assistance used over the past week. BHS2, BHS3, and BHS7 allowed patient and proxy responses for the LPADL question; patient data was preferentially used for analyses.
Within each study, residual disability was calculated by comparing pre-fracture LPADL scores to LPADL scores 12-months post-fracture. Residual disability was assessed both in terms of mean intra-individual change in LPADL score and whether an individual had a worse 12-month post-fracture LPADL score (higher score) than the pre-fracture score (proportion). Twelve-month mortality (proportion) and the proportion of subjects residing in a nursing home at 12-months post-fracture were calculated. Nursing home placement was determined by where the individual was residing at the 12-month post-fracture interview. Two composite outcomes were assessed. The first was the proportion who had a higher 12-month post-fracture LPADL score than pre-fracture or had died by 12 months (composite outcome one). Composite outcome two was the proportion who met the criteria for composite outcome one or who resided in a nursing home at 12-months post-fracture.
Covariates
Variables examined included age, race, marital status, education, Mini-Mental State Examination (MMSE)27 score, body mass index (BMI), type of fracture (intertrochanteric or any other type), type of surgery (internal fixation or arthroplasty), length of stay, initial hospitalization discharge location, comorbidities, and pre-fracture LPADL score. In one study (BHS7), the Modified Mini-Mental State (3MS) examination28 was used instead of the MMSE; for consistency, 3MS scores were converted to MMSE score equivalents.28
The comorbidities assessed differed across studies, so those analyzed were restricted to the 15 common comorbidities captured across the studies (heart problems, arthritis, cancer, cirrhosis/substance abuse, respiratory disease, dementia/Alzheimer’s, diabetes, epilepsy/seizures, ulcers, hypertension, osteoporosis/Paget’s disease, Parkinson disease, peripheral vascular disease, and stroke). Comorbidity level was the count of the number of conditions (out of 15) an individual endorsed.
Statistical Methods
Analysis was conducted in SAS v9.4 (Cary, NC). Descriptive analysis was conducted stratified by BHS study. As men and women may have differing outcomes after fracture, studies were further stratified by sex.29,30 ANOVA and Chi-squared tests were used to examine differences across BHS studies by sex.
Crude proportions were calculated for residual disability, mortality, and nursing home placement at 12 months for those with non-missing respective outcome data. Chi-squared tests were used to compare outcomes across studies by sex. Ordinary least squares regression was used to fit a linear regression model comparing mean residual disability (LPADL at 12-months post-fracture – LPADL pre-fracture) across the cohorts, including a sex interaction term. To account for case-mix and entry criteria differences across studies that may affect the outcomes, the comparisons were subsequently case-mix adjusted for age, count of comorbidities, body mass index, fracture type, and MMSE score. To facilitate interpretability, all continuous covariates were standardized. An analogous, case-mix adjusted logistic regression model was used for the comparison of the proportion of subjects with composite outcome one and two. All odds ratios and 95% confidence interval estimates were converted to proportions [p̂=odds ratio/(1-odds ratio)].
To evaluate which particular activities contributed most to residual disability, pooled mean intra-individual differences between LPADL scores 12-months post-fracture and pre-fracture for each LPADL item were calculated by sex.
RESULTS
Table 2 displays the distributions of socio-demographic and clinical characteristics stratified by study and sex. Across cohorts, significant differences (p<0.05) were seen for women in age, race, marital status, education, comorbidity count, MMSE, BMI, length of stay, discharge location, and baseline LPADL. Significant differences (p<0.05) in men between BHS2 and BHS7 were present for the same characteristics, except race and marital status.
Table 2.
Baltimore Hip Study (BHS) Patient Characteristics Stratified by Study and Sex
| BHS2 | BHS3 | BHS4 | BHS5 | BHS7 | ANOVA or Chi-Square P-Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Women | Women | Women | Men | Women | Men | Women | |
| n=121 | n=365 | n=150 | n=76 | n=44 | n=119 | n=114 | |||
| Characteristic | |||||||||
| Age (yrs)*, m (sd) | 79.1 (7.5) | 81.5 (7.3) | 76.7 (11.6) | 81.8 (6.3) | 79.2 (6.5) | 81.1 (7.7) | 81.9 (7.8) | 0.05 | <0.01 |
| Race, n (%) | 0.35 | 0.01 | |||||||
| White | 110 (90.9) | 341 (93.4) | 150 (100.0) | 75 (98.7) | 43 (97.7) | 112 (94.1) | 107 (93.9) | ||
| Non-white | 11 (9.1) | 24 (6.6) | 0 (0) | 1 (1.3) | 1 (2.3) | 7 (5.9) | 7 (6.1) | ||
| Marital Status, n (%) | 0.37 | 0.03 | |||||||
| Married | 67 (55.4) | 75 (20.5) | 33 (22.0) | 26 (34.2) | 14 (31.8) | 59 (49.6) | 34 (29.8) | ||
| Not Currently Married | 54 (44.6) | 290 (79.5) | 116 (77.3) | 50 (65.8) | 30 (68.2) | 60 (50.4) | 80 (70.2) | ||
| Unknown | 0 (0) | 0 (0) | 1 (0.7) | 0 (0) | 0 (0) | 0 (0) | 0 (0.0) | ||
| Education, n (%) | <0.01 | <0.01 | |||||||
| < High School | 45 (37.2) | 140 (38.4) | 42 (28.0) | 20 (26.3) | 14 (31.8) | 32 (26.9) | 18 (15.8) | ||
| ≥High School | 63 (52.1) | 178 (48.8) | 106 (70.7) | 54 (71.1) | 30 (68.2) | 86 (72.3) | 96 (84.2) | ||
| Unknown | 13 (10.7) | 47 (12.9) | 2 (1.3) | 2 (2.6) | 0 (0.0) | 1 (0.8) | 0 (0.0) | ||
| Comorbidity Count, m (sd) | 2.5 (1.5) | 2.1 (1.4) | 2.3 (1.6) | 2.4 (1.5) | 3.0 (1.5) | 3.1 (1.6) | 2.6 (1.5) | 0.01 | <0.01 |
| MMSE (score range 0 to 36, high=good), m (sd) | 21.3 (6.3) | 22.4 (5.4) | 23.1 (4.4) | 27.0 (2.4) | 26.9 (2.7) | 23.0 (4.5) | 24.4 (4.2) | 0.03 | <0.01 |
| BMI (kg/m2), m (sd) | 23.2 (4.1) | 22.2 (4.3) | 22.6 (4.7) | 24.4 (4.6) | 23.5 (4.3) | 25.8 (4.4) | 25.2 (6.2) | <0.01 | <0.01 |
| Type of Fracture, n (%) | 0.09 | 0.09 | |||||||
| Intertrochan teric | 66 (54.5) | 200 (54.8) | 71 (47.3) | 34 (44.7) | 22 (50.0) | 52 (43.7) | 47 (41.2) | ||
| Other | 55 (45.5) | 165 (45.2) | 79 (52.7) | 42 (55.3) | 22 (50.0) | 66 (55.5) | 67 (58.8) | ||
| Missing | 1 (0.8) | ||||||||
| Type of Surgery, n (%) | 0.19 | 0.06 | |||||||
| Internal Fixation | 79 (65.3) | 239 (65.5) | 87 (58.0) | 43 (56.6) | 24 (54.5) | 67 (56.3) | 60 (52.6) | ||
| Other | 41 (33.9) | 121 (33.2) | 59 (39.3) | 33 (43.4) | 20 (45.5) | 52 (43.7) | 54 (47.4) | ||
| Unknown | 1 (0.8) | 5 (1.4) | 4 (2.7) | 0 (0) | 0 (0) | 0 (0.0) | 0 (0.0) | ||
| Length of Stay (days), m (sd) | 16.6 (10.3) | 13.9 (7.5) | 8.6 (4.7) | 4.1 (1.2) | 4.6 (1.5) | 5.5 (2.5) | 5.2 (3.1) | <0.01 | <0.01 |
| Discharge Location, n (%) | <0.01 | <0.01 | |||||||
| Home | 46 (38.0) | 98 (26.8) | 29 (19.3) | 2 (2.6) | 1 (2.3) | 5 (4.2) | 5 (4.4) | ||
| Facility | 69 (57.0) | 253 (69.3) | 120 (80.0) | 74 (97.4) | 42 (95.5) | 114 (95.8) | 109 (95.6) | ||
| Unknown | 6 (5.0) | 14 (3.8) | 1 (0.7) | 0 (0) | 1 (2.3) | 0 (0) | 0 (0.0) | ||
| Baseline LPADL, m (sd) | 4.0 (3.8) | 3.4 (3.6) | 4.8 (3.4) | 2.1 (2.3) | 1.5 (2.5) | 2.4 (2.4) | 2.7 (2.4) | <0.01 | <0.01 |
m, mean; sd, standard deviation
Deidentified datasets were used for BHS4 and BHS5 analysis whereby all women 90 or older had their age assigned to 90. In our study sample, this impacted ten subjects in BHS4 and two subjects in BHS5.
Table 3 displays the proportion experiencing the single and composite outcome measures across the five BHS studies prior to case-mix adjustment (crude). For men, there were no significant differences (p<0.05) between BHS2 and BHS7 for any of the outcomes. For women, significant differences (p<0.05) were found across studies for residual disability, nursing home placement, and both composite outcomes. There was no significant difference across studies for mortality. For BHS2, 15.9% of women died by 12-months post-fracture while, for BHS7, 11.4% died. Among survivors, 88.1% had residual disability and 24.9% were residing in nursing homes, compared to 11.4% and and 7.9% for BHS7.
Table 3.
Baltimore Hip Study (BHS) patient single and composite unadjusted outcomes stratified by study and sex
| Hip Study | Sex | Baseline n | Residual Disability Mean | Residual Disability* % | Dead at 12 Months % | Nursing Home Residency at 12 months % | Residual Disability* or Dead (Composite Outcome 1) % | Residual Disability* or Dead or Nursing Home Residency at 12 months (Composite Outcome 2) % |
|---|---|---|---|---|---|---|---|---|
| BHS2 | W | 365 | 3.8 | 88.1 | 15.9 | 24.9 | 90.2 | 92.3 |
| BHS2 | M | 121 | 3.5 | 85.5 | 38.0 | 16.0 | 91.3 | 91.7 |
| BHS3 | W | 150 | 2.7 | 74.4 | 15.3 | 11.0 | 78.4 | 79.3 |
| BHS4 | W | 76 | 2.2 | 72.2 | 5.3 | 1.4 | 73.7 | 73.7 |
| BHS5 | W | 44 | 3.0 | 78.1 | 6.8 | 0.0 | 79.6 | 79.6 |
| BHS7 | W | 113 | 2.4 | 75.0 | 11.4 | 7.9 | 77.9 | 79.8 |
| BHS7 | M | 119 | 3.2 | 86.8 | 29.4 | 10.7 | 90.7 | 90.8 |
M, men; W, women
Residual disability is defined here as having a value of greater than zero when baseline Lower Extremity Physical Activities of Daily Living (LPADL) score is subtracted from the 12 month LPADL score
Figure 1 shows the mean level of residual disability at 12-months for each study plotted by study, stratified by sex, and adjusted for case-mix (age, comorbidities, MMSE, BMI, and surgery type). In BHS2, women had residual disability in an average of 3.5 activities (95% CI: 2.95, 3.99). Compared to BHS2, there was significantly less residual disability present in BHS3 (mean=2.7 activities, 95% CI: 2.01, 3.30), BHS4 (mean=2.3, 95% CI: 1.54, 3.10), and BHS7 (mean=2.7, 95% CI: 1.64, 2.90). There was no significant difference between the amount of residual disability in BHS2 and BHS5 (mean=3.0, 95% CI: 1.95, 4.01) nor were BHS3, BHS4, BHS5, and BHS7 significantly different from one another. For men, there was no significant difference between BHS2 (mean=3.1, 95% CI: 2.16, 4.10) and BHS7 (mean=3.1, 95% CI: 2.41, 2.82).
Figure 1. Adjusted* 12-month residual disability with 95% confidence intervals stratified by study and sex.
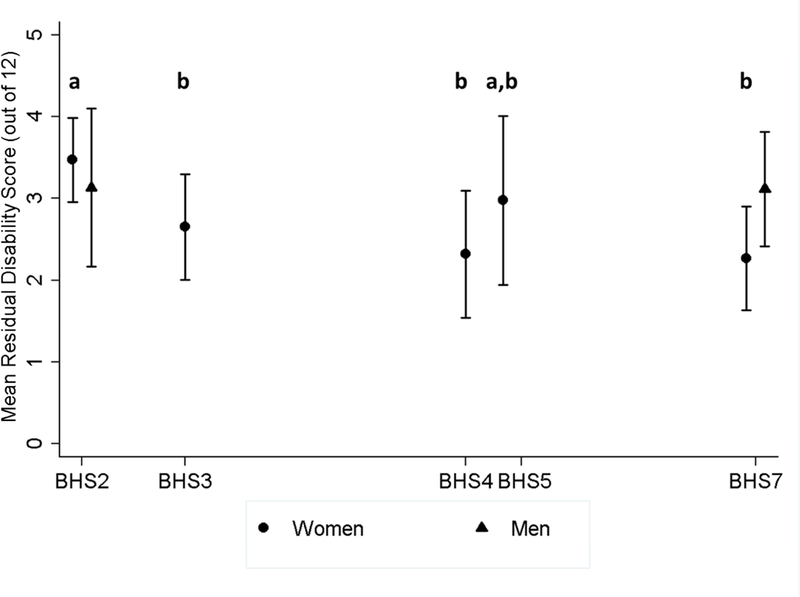
a,bBlack letters indicate study pairwise comparisons for women. Different letters indicate significant differences (p<0.05). For example, for women, BHS2 was significantly different from BHS3, BHS4, and BHS7 but not BHS5. Pairwise comparisons are not shown for men as there was not a significant difference between BHS2 and BHS7.
*Adjusted for age, comorbidity, MMSE, BMI, and fracture type
The case-mix adjusted proportion of subjects with 12-month residual disability or death (composite outcome one) by study year and sex is displayed in Figure 2. Similar to residual disability, women saw significant improvements from BHS2 (p̂=0.87, 95% CI: 0.83, 0.89) to BHS3 (p̂=0.76, 95% CI: 0.71, 0.81), to BHS4 (p̂=0.69, 95% CI: 0.62, 0.75), and to BHS7 (p̂=0.76, 95% CI: 0.71, 0.80) but not to BHS5 (p̂=0.80, 95% CI: 0.72, 0.86). There were no significant differences between BHS3, BHS4, BHS5, and BHS7. Men saw no significant improvements between BHS2 (p̂=0.86, 95% CI: 0.80, 0.90) and BHS7 (p̂=0.90, 95% CI: 0.87, 0.93).
Figure 2. Adjusted* proportion of hip fracture patients with 12-month residual disability or death with 95% confidence intervals stratified by study and sex.

a,bBlack letters indicate study pairwise comparisons for women. Different letters indicate significant differences (p<0.05). For example, for women, BHS2 was significantly different from BHS3, BHS4, and BHS7 but not BHS5. Pairwise comparisons are not shown for men as there was not a significant difference between BHS2 and BHS7.
*Adjusted for age, comorbidity, MMSE, BMI, and fracture type
Sex- and study-stratified case-mix adjusted proportions of subjects with residual disability or death or nursing home residency at 12 months (composite outcome two) is displayed in Figure 3. Again, males saw no significant improvements between BHS2 (p̂=0.88, 95% CI: 0.85, 0.90) and BHS7 (p̂=0.91, 95% CI: 0.87, 0.93). Females saw significant improvement from BHS2 (p̂=0.88, 95% CI: 0.85, 0.90) to BHS3 (p̂=0.78, 95% CI: 0.73, 0.82) and to BHS4 (p̂=0.71, 95% CI: 0.65, 0.77). There were no significant pairwise differences between any other studies, including BHS5 (p̂=0.82, 95% CI: 0.74, 0.87) and BHS7 (p̂=0.79, 95% CI: 0.74, 0.83).
Figure 3. Adjusted* proportion of hip fracture patients with 12-month residual disability or death or nursing home residency with 95% confidence intervals stratified by study and sex.

a,bBlack letters indicate study pairwise comparisons for women. Different letters indicate significant differences (p<0.05). For example, for women, BHS2 was significantly different from BHS3 and BHS4 but not BHS5 and BHS7. Pairwise comparisons are not shown for men as there was not a significant difference between BHS2 and BHS7.
*Adjusted for age, comorbidity, MMSE, BMI, and fracture type
Among those with LPADL measures at baseline and 12 months, men had most pronounced incerases in disability in getting on and off the toilet (52.0%), walking 1 block (35.1%) and getting in and out of the bath (34.5%). Females had the largest increases in disability in getting on and off the toilet (45.1%), getting in and out of the bath (36.7%), and climbing 5 stairs (36.1%).
DISCUSSION
This secondary analysis of five hip fracture studies found that over the course of two decades (1990 to 2011), patients still have substantial residual disability 12 months after fracture, with only slight improvements in outcomes from BHS2 (1990–1991 enrollment) to BHS7 (2006–2011 enrollment). In the most recent study (BHS7), after case-mix adjustment, women and men, 12 months after fracture, had additional disability in 2.5 and 3.1 additional activities, respectively, compared to pre-fracture. In BHS7, after adjustment, 79% of women and 91% of men had a negative outcome (greater disability, died, or nursing home residence at 12-months post-fracture). Women had slight reductions in these negative outcomes between 1990 and 2001, but men did not.
The crude, 12-month mortality for the analyzed studies ranged from 5.3%−15.9% for women and 29.4–38.0% for men. Mortality after fracture is associated with older age, male sex, and more comorbidities.7,15,31 The lowest 12-month, unadjusted mortality rate was seen for BHS4, which was a randomized controlled trial and enrolled a healthier patient population. Although mortality at 12 months was lower for both sexes in BHS7, compared to BHS2, there were no significant differences in mortality across studies. Although not statistically significant, findings from this study are consistent with other reports of declining mortality in the general population and hip fracture patients.12,13,15,32
During the analysis period, residential options for older adults drastically increased, with substantial growth between 1993 and 2007 in the number of assisted living facilities per the number of older adults.33 Between BHS2 and BHS7, men saw a non-significant 5.3% decline in 12-month nursing home placement while women saw a significant 17.0% decline. One study found that 12-month nursing home residency remained stable among Medicare beneficiaries with hip fractures between 2000 and 2008.12 Although this is consistent with our findings in men, it is contrary to our findings in women.
Over the time period studied, older men undergoing usual care post-fracture had no significant improvements in 12-month outcomes after fracture. Women experienced significant improvements in outcomes from BHS2 (enrollment 1990–1991) to BHS3 (enrollment 1992–1995) with no subsequent improvements in later studies. The BHS had varying recruitment strategies, study designs, and study samples. To account for these differences, careful case-mix adjustments were made in the analyses; residual disability remained across all studies even after adjustment for these case-mix differences. This adjustment allowed us to isolate the impact of other factors such as surgical treatment, in-hospital care, rehabilitation, and policies versus shifts in patient characteristics, on outcomes.
With respect to surgical care, internal fixation is becoming less common and nonoperative treatment is on the decline.14 Surgical procedure did not significantly differ across studies, suggesting that shifts in surgical type did not substantially impact patient outcomes. The lack of improvement in patient disability over time is consistent with recent reviews concluding that although the current state of rehabilitation for hip fracture patients is beneficial, usual rehabilitation practices are still not fully returning patients to their pre-fracture level of function.10,34 Rehabilitation, in general, aims to improve mobility and independence in patients and can include strength training, mobility training (potentially with assistive devices), and pain management.34 However, “usual care” for hip fracture patients at all phases of rehabilitation (acute, post-acute setting, community) is not standardized and often based on provider experience and local protocols.34 Rehabilitation intervention studies also provide insufficient detail on the care that control groups received, making the assessment of outcomes across studies difficult.20 Despite many years of extensive research on hip fracture outcomes, the most effective interventions to improve mobilization, physical function, and psychosocial function after hip fracture remain elusive.35,36 Australia37 and the United Kingdom38 have published recommendations for rehabilitation in hip fracture patients, although no such guidelines have been published in the United States.39 The majority of research on hip fracture outcomes, treatment, and rehabilitation focuses on women11. The improvements seen in women between BHS2 and BHS3 could be the result of women disproportionately benefitting from this sex-specific research. Lastly, the overall findings of this study may reflect the lack of consideration of psychosocial factors, such as depression40 and resilience41 that influence recovery following hip fracture.
Study Limitations
The lack of improvement in residual disability for men and small improvements in women over the 20 years represented by these studies could also be explained by selection bias, specifically survivorship. For example, if mortality improved over time, sicker patients that would have previously died after a hip fracture are now surviving and inflating residual disability. However, no significant improvement in survival was seen in this study and the composite outcome results accounting for mortality suggest a similar pattern to the residual disability outcome alone.
The trends in residual disability, mortality, and nursing home placement in this study may not be generalizable to the larger hip fracture population given that these studies were conducted in community-dwelling, older adults meeting restricted entry criteria from a limited geographic area. Still, differences observed across the BHS cohorts match changes in some outcomes observed nationally. Differences across studies were present for MMSE scores, education, length of stay, and discharge location. Nationally, MMSE scores and education levels have improved over time.42 Changes in Medicare reimbursement policy, such as the Balanced Budged Act19, have shifted rehabilitative care from the hospital to skilled nursing facilities (SNFs) and other settings, which is also reflected in the present analysis where lengths of hospital stay decreased and use of subacute care in SNFs increased over 20 years.
There are some additional limitations of this study. We were unable to examine changes in other patient outcome measures over time as we were restricted to those measures captured across the studies. We may have missed additional improvements in the LPADL beyond 12 months as only one study included a two-year follow-up (BHS2).6 However, BHS2 found that maximal recovery in lower extremity ADLs was reached at 11.2 months.6 Despite adjustment for case-mix, residual confounding may remain given that models were only adjusted for baseline differences in studies and for baseline characteristics collected across all studies. Although residual confounding cannot be ruled out, key factors known to be associated with recovery outcomes, such as age, comorbid disease, and cognitive status, were adjusted for in models of 12-month residual disability and composite outcomes.7 Outcomes may also differ by where rehabilitation takes place.34,43–45. The use of proxies in the cohort studies may also be problematic. Proxies systematically rate greater disability than patients self-report in hip fracture patients.46 Lastly, limited data were available in BHS cohorts on outcomes among men.
CONCLUSIONS
As Medicare data does not have functional outcomes, the BHS provides a unique opportunity to compare over 20 years of data on patients from a similar source population. In summary, we have not yet resolved the problem of residual disability following hip fracture. From 1991 to 2011, men receiving usual care for hip fracture have seen no improvements in outcomes and women have seen initial, early improvements with no subsequent improvements. The vast majority of hip fracture patients face new disabilities, despite rehabilitative care. Further, contemporary studies are needed to understand how treatment and rehabilitation can be improved or better implemented across the continuum of post-hip fracture care to minimize long-term disability among this patient population.47 Future studies will need to operationalize usual care into multidisciplinary, multimodal interventions that can be tested in carefully controlled efficacy studies and in pragmatic clinical trials.
Acknowledgements:
This research was supported by grants from the National Institute on Aging [R37 AG009901, R01 AG06322, R01 HD0073, R01 AG018668, R01 AG17082, R01 AG029315, P30 AG028747, and T32 AG000262]. The funding sponsors had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
We also acknowledge the cooperation of the hospitals, DXA facilities, patients, and families participating in this project.
ABBREVIATIONS:
- 3MS
Modified Mini-Mental State
- BHS
Baltimore Hip Studies
- BMI
Body Mass Index
- LPADL
Lower Extremity Physical Activities of Daily Living
- MMSE
Mini-Mental State Examination
- SNFs
Skilled Nursing Facilities
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Prior Presentation:
This material has not been previously presented.
Conflicts of Interest:
DSA, EB, GVO, JRH, JG, ALG-B, MCH, and BR have no conflicts of interest to disclose. JMG reports personal fees from Pluristem Pharma, Boeringer-Ingleheim, and Viking Therapeutics. DLO reports consulting agreements with Viking Therapeutics, Inc. and Kinexum. JSM reports personal fees from Pluristem, Novartis, Viking, Ammonett, Sanofi, and Scholar Rock.
References
- 1.National Hospital Discharge Survey (NHDS). Number of discharges form short-stay hospitals, by first-listed diagnosis and age: United States, 2010 https://www.cdc.gov/nchs/data/nhds/3firstlisted/2010first3_numberage.pdf. Accessed August 31, 2017.
- 2.Stevens JA, Rudd RA. The impact of decreasing U.S. hip fracture rates on future hip fracture estimates. Osteoporos Int 2013;24(10):2725–2728. doi: 10.1007/s00198-013-2375-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leibson CL, Tosteson AN, Gabriel SE, Random JE, Melton LJ. Mortality, disability, and nursing home use for persons with and without hip fracture: A population-based study. J Am Geriatr Soc 2002;50(10):1644–1650. doi: 10.1046/j.1532-5415.2002.50455.x. [DOI] [PubMed] [Google Scholar]
- 4.Wolinsky FD, Fitzgerald JF. The effect of hip fracture on mortality, hospitalization, and functional status: A prospective study. Am J Public Health 1997;87(3):398–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the united states, 2005–2025. J Bone Miner Res 2007;22(3):465–475. [DOI] [PubMed] [Google Scholar]
- 6.Magaziner J, Hawkes W, Hebel R, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci 2000;55A(9):M498–507. [DOI] [PubMed] [Google Scholar]
- 7.Zuckerman JD. Hip fracture. N Engl J Med 1996;334(23):1519–1525. doi: 10.1056/NEJM199606063342307. [DOI] [PubMed] [Google Scholar]
- 8.Jette AM, Harris BA, Cleary PD, Campion EW. Functional recovery after hip fracture. Arch Phys Med Rehabil 1987;68(10):735–740. [PubMed] [Google Scholar]
- 9.Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Predictors of functional recovery one year following hospital discharge for hip fracture: A prospective study. J Gerontol 1990;45(3):M101–M107. [DOI] [PubMed] [Google Scholar]
- 10.Dyer SM, Crotty M, Fairhall N, et al. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr 2016;16:158–158. doi: 10.1186/s12877-016-0332-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Orwig DL, Chan J, Magaziner J. Hip fracture and its consequences: Differences between men and women. Orthop Clin North Am 2006;37(4):611–622. [DOI] [PubMed] [Google Scholar]
- 12.Becker DJ, Arora T, Kilgore ML, et al. Trends in the utilization and outcomes of medicare patients hospitalized for hip fracture, 2000–2008. J Aging Health 2014;26(3):360–379. [DOI] [PubMed] [Google Scholar]
- 13.Mundi S, Pindiprolu B, Simunovic N, Bhandari M. Similar mortality rates in hip fracture patients over the past 31 years. Acta Orthop 2014;85(1):54–59. doi: 10.3109/17453674.2013.878831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cram P, Yan L, Bohm E, et al. Trends in operative and nonoperative hip fracture management 1990–2014: A longitudinal analysis of manitoba administrative data. J Am Geriatr Soc 2017;65(1):27–34. doi: 10.1111/jgs.14538. [DOI] [PubMed] [Google Scholar]
- 15.Pedersen AB, Ehrenstein V, Szépligeti S, et al. 35-year trends in first-time hospitalization for hip fracture, one year mortality, and the prognostic impact of comorbidity: A danish nationwide cohort study, 1980–2014. J Am Geriatr Soc 2017;65(1):22–24. doi: 10.1097/EDE.0000000000000729; 10.1111/jgs.14686. [DOI] [PubMed] [Google Scholar]
- 16.Bentler SE, Liu L, Obrizan M, et al. The aftermath of hip fracture: Discharge placement, functional status change, and mortality. Am J Epidemiol 2009;170(10):1290–1299. doi: 10.1093/aje/kwp266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neuman MD, Silber JH, Magaziner JS, Passarella MA, Mehta S, Werner RM. Survival and functional outcomes after hip fracture among nursing home residents. JAMA Intern Med 2014;174(8):1273–1280. doi: 10.1001/jamainternmed.2014.2362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Papadimitriou N, Tsilidis KK, Orfanos P, et al. Burden of hip fracture using disability-adjusted life-years: A pooled analysis of prospective cohorts in the CHANCES consortium. Lancet Public Health 2017(5):e239–e246. doi: 10.1016/S2468-2667(17)30046-4. [DOI] [PubMed] [Google Scholar]
- 19.Gage B. Impact of the BBA on post-acute utilization. Health Care Financ Rev 1999;20(4):103–126. [PMC free article] [PubMed] [Google Scholar]
- 20.Chudyk AM, Jutai JW, Petrella RJ, Speechley M. Review article (meta-analysis): Systematic review of hip fracture rehabilitation practices in the elderly. Arch Phys Med Rehabil 2009;90:246–262. doi: 10.1016/j.apmr.2008.06.036. [DOI] [PubMed] [Google Scholar]
- 21.Wehren LE, Hawkes WG, Hebel JR, et al. Predictors of bone loss after hip fracture. Osteoporosis Int 2004;15(2):125–131. [DOI] [PubMed] [Google Scholar]
- 22.Baumgarten M, Margolis DJ, Orwig DL, et al. Pressure ulcers in elderly patients with hip fracture across the continuum of care. J Am Geriatr Soc 2009;57(5):863–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Orwig D, Hochberg MC, Gruber-Baldini AL, et al. Examining differences in recovery outcomes between male and female hip fracture patients: design and baseline results of a prospective cohort study from the Baltimore Hip Studies. J Frailty Aging 2018;7(3):162–169. doi: 10.14283/jfa.2018.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Orwig DL, Hochberg M, Yu-Yahiro J, et al. Delivery and outcomes of a yearlong home exercise program after hip fracture: A randomized controlled trial. Arch Intern Med 2011;171(4):323–331. doi: 10.1001/archinternmed.2011.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Resnick B, Orwig D, Yu-Yahiro J, et al. Testing the effectiveness of the exercise plus program in older women post-hip fracture. Ann Behav Med 2007;34(1):67–76. doi: 10.1080/08836610701495367. [DOI] [PubMed] [Google Scholar]
- 26.Jette AM. Jette AM. Functional status index: Reliability of a chronic disease evaluation instrument. Arch Phys Med Rehabil 1980;61(9):395–401. [PubMed] [Google Scholar]
- 27.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12(3):189. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 28.Teng EL, Chui HC. The modified mini-mental state (3MS) examination. J Clin Psychiatry 1987;48(8):314–318. [PubMed] [Google Scholar]
- 29.Institute of Medicine (US) Committee on Understanding the Biology of Sex and Gender Differences. Exploring the biological contributions to human health: Does sex matter? J Womens Health Gend Based 2001;10(5):433–439. [DOI] [PubMed] [Google Scholar]
- 30.Sterling RS. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin Orthop Relat Res 2011;469(7):1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miller CW. Survival and ambulation following hip fracture. J Bone Joint Surg Am 1978;60(7):930–934. [PubMed] [Google Scholar]
- 32.Bell FC, Miller ML. Life tables for the united states social security area, 1900–2100 https://www.ssa.gov/oact/NOTES/pdf_studies/study116.pdf. Accessed August 31, 2017.
- 33.Grabowski DC, Stevenson DG, Cornell PY. Assisted living expansion and the market for nursing home care. Health Serv Res 2012;47(6):2296–2315. doi: 10.1111/j.1475-6773.2012.01425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Criss M, Takacs S. Rehabilitation of hip fractures across the continuum of care. Top Geriatr Rehabil 2013;29(4):281–293. [Google Scholar]
- 35.Handoll H, Sherrington C. Mobilisation strategies after hip fracture surgery in adults. Cochrane Database Syst Rev 2007(1). [DOI] [PubMed] [Google Scholar]
- 36.Crotty M, Unroe K, Cameron ID, Miller M, Ramirez G, Couzner L. Rehabilitation interventions for improving physical and psychosocial functioning after hip fracture in older people. Cochrane Database Syst Rev 2010(1). [DOI] [PubMed] [Google Scholar]
- 37.Mak J, Cameron ID, March LM. Evidence-based guidelines for the management of hip fractures in older persons: An update. Med J Aust 2010;192(1):37–41. [DOI] [PubMed] [Google Scholar]
- 38.Ftouh S, Morga A, Swift C. Guidelines: Management of hip fracture in adults: Summary of NICE guidance. BMJ 2011(7812):1413. [DOI] [PubMed] [Google Scholar]
- 39.Carriero FP, Christmas C. In the clinic. hip fracture. Ann Intern Med 2011;155(11):ITC6–1-ITC6–15; quiz ITC6–16. doi: 10.7326/0003-4819-155-11-201112060-01006. [DOI] [PubMed] [Google Scholar]
- 40.Cristancho P, Lenze EJ, Avidan MS, Rawson KS. Trajectories of depressive symptoms after hip fracture. Psychol Med 2016;46(7):1413–1425. doi: 10.1017/S0033291715002974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rebagliati GAA, Sciumé L, Iannello P, et al. Frailty and resilience in an older population. the role of resilience during rehabilitation after orthopedic surgery in geriatric patients with multiple comorbidities. Funct Neurol 2016;31(3):171–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matthews F, Marioni R, Brayne C. Examining the influence of gender, education, social class and birth cohort on MMSE tracking over time: A population-based prospective cohort study. BMC GERIATRICS 2012;12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Munin MC, Seligman K, Dew MA, et al. Effect of rehabilitation site on functional recovery after hip fracture. Arch Phys Med Rehabil 2005;86(3):367–372. [DOI] [PubMed] [Google Scholar]
- 44.Jung HY, Trivedi AN, Grabowski DC, Mor V. Does more therapy in skilled nursing facilities lead to better outcomes in patients with hip fracture? Phys Ther 2016;96(1):81–89. doi: 10.2522/ptj.20150090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mallinson T, Deutsch A, Bateman J, et al. Comparison of discharge functional status after rehabilitation in skilled nursing, home health, and medical rehabilitation settings for patients after hip fracture repair. Arch Phys Med Rehabil 2014;95(2):209–217. [DOI] [PubMed] [Google Scholar]
- 46.Magaziner J, Zimmerman SI, Gruber-Baldini A, Hebel JR, Fox KM. Proxy reporting in five areas of functional status. Am J Epidemiol 1997;146(5):418–428. [DOI] [PubMed] [Google Scholar]
- 47.Ouellet JA, Cooney LM. Hip fracture: Can we do better? J Am Geriatr Soc 2017;65(1):22–24. doi: 10.1111/jgs.14686. [DOI] [PubMed] [Google Scholar]


