Abstract
Background
Childhood obesity is highly prevalent and carries substantial health consequences. Childhood obesity interventions have had mixed results, which may be partially explained by the absence of theory that incorporates broader family context and methods that address implementation challenges in low-resource settings. Communities for Healthy Living (CHL) is an obesity prevention program for Head Start preschools designed with careful focus on theory and implementation. This protocol paper outlines the design, content, implementation, and evaluation of CHL.
Methods/design
CHL integrates a parenting program co-led by Head Start staff and parents, enhanced nutrition support, and a media campaign. CHL content and implementation is informed by the Family Ecological Model, Psychological Empowerment Theory, and Organizational Empowerment Theory. The intervention is directed by community-based participatory research and implementation science principles, such as co-leadership with parents and staff, and implementation in a real world context. CHL is evaluated in a three-year pragmatic cluster-randomized trial with a stepped wedge design. The primary outcome is change in child Body Mass Index z-score. Secondary outcomes include children’s weight-related behaviors (i.e., diet, physical activity, screen use, and sleep), parenting practices targeted at these behaviors (e.g., food parenting), and parent empowerment. The evaluation capitalizes on routine health data collected by Head Start (e.g., child height and weight, diet) coupled with parent surveys completed by subsamples of families.
Discussion
CHL is an innovative childhood obesity prevention program grounded in theory and implementation science principles. If successful, CHL is positioned for sustained implementation and nationwide Head Start scale-up.
Trial Registration
Keywords: Childhood Obesity, Theory, Implementation, Pragmatic Trial, Trial Protocol, Community-Based Participatory Research
1. INTRODUCTION
Childhood obesity is a major public health concern with significant health consequences including type 2 diabetes, poor psychosocial health, and adult obesity [1]. In the United States, where 13.9% of 2 – 5 year old children have obesity [2], children from low-income and racial/ethnic minority families are disproportionately affected [2,3]. This pattern highlights the need to address childhood obesity in these communities as a matter of social justice.
Early childhood obesity interventions are promising because young children’s weight-related health behaviors are pivotal in preventing obesity [4] and establishing healthy patterns for later life [5,6]. While family-based approaches are considered the ‘gold standard’ for early childhood obesity intervention [7], they have not consistently achieved sustainable effects [8], which may be explained by theory failure and/or implementation failure [9]. For example, few childhood obesity prevention programs are founded in family theory, resulting in interventions that do not address broader life circumstances such as housing instability, family illness, and unemployment [10]. Neglecting these acute needs may preclude families from engaging in child health behaviors targeted in interventions, resulting in theory failure. On the implementation side, recruiting and retaining families is challenging; interventions often require substantial time commitments outside of family routines. Furthermore, intervention development and implementation often rely heavily on research staff. The resultant lack of community engagement exacerbates challenges to recruitment, retention, and sustainability, leading to implementation failure.
Informed by the Family Ecological Model [11] and empowerment theories [12–16], Communities for Healthy Living (CHL) is an innovative childhood obesity prevention program integrated into Head Start, a service already accessed by low-income families. Community-based participatory research (CBPR) is used to plan the content and implementation of CHL. CBPR emphasizes equal community-researcher partnership in all research phases [17], laying the groundwork for successful implementation by building trust [18,19]. To accelerate translation of this research into practice, CHL is aligned with Head Start performance standards and implemented as a pragmatic trial [20–22], including detailed outcome and process evaluations utilizing measures of interest to critical stakeholders such as Head Start teachers, family engagement staff, and administrators [20,22].
CHL builds upon a 2009–2011 pilot study in five Head Start centers in Troy, NY, which demonstrated a 4% decrease in childhood obesity prevalence, and improvements in child diet and physical activity [23–25]. Moreover, parent participation was linked with increased empowerment, which in turn predicted improved health-related parenting practices (e.g., frequency of offering fruits and vegetables) [25].
The current trial evaluates CHL effectiveness in 16 Greater Boston area Head Start programs using a stepped wedge design over three years. Objectives are to examine CHL effects on: 1) children’s BMI z-score; 2) children’s weight-related behaviors (fruit and vegetable intake, sugary beverage consumption, physical activity, sleep, and screen behaviors [3–6]); and 3) anticipated parent- (weight-related parenting practices, empowerment) and organizational- (organizational empowerment) level mechanisms of change. In this paper, we describe how theory, implementation science principles, and CBPR methods informed CHL content and implementation strategies, and outline the evaluation design, measures, and analytic plan for the trial.
2. METHODS
a. Study Setting and Population
Head Start is a federally funded, evidence-based school readiness program that provides early education for children from low-income families in the United States [26,27]. In addition to early childhood education, Head Start targets children’s physical and emotional health through nutrition, health screenings, and parent involvement services [27]. As such, Head Start is an ideal partner for reaching and engaging diverse families with children at high risk for obesity. CHL is implemented in Head Start programs in Boston (N=12 programs) and Cambridge/Somerville (N=4 programs), which are overseen by Action for Boston Community Development (ABCD) and the Community Action Agency of Somerville (CAAS), respectively. While ABCD and CAAS operate a small number of Head Start classrooms in nine other locations, these classrooms are administratively distinct from the others and it was therefore not deemed feasible to implement CHL there. All other ABCD and CAAS programs were included in the CHL trial. Table 1 summarizes program characteristics for each Head Start agency and demographic characteristics of the families they serve.
Table 1.
Baseline demographics of the families served by ABCD and CAAS Head Start programs in CHL trial.
| ABCD | CAAS | All programs (ABCD+CAAS) | |
|---|---|---|---|
| Number of children served | 1,414 | 241 | 1,655 |
| Number of programs | 12 | 4 | 16 |
| Number of teachers | 317 | 36 | 353 |
| Number of program staff (non-teachers) | 269 | 19 | 288 |
| N (%) | N (%) | N (%) | |
| Child race | |||
| American Indian/Alaska | 2 (0.1) | 0 (0) | 2 (0.1) |
| Black/African American | 577 (40.8) | 52 (21.7) | 629 (38.0) |
| Asian | 120 (8.5) | 54 (22.5) | 174 (10.5) |
| Multi-race | 83 (5.9) | 14 (5.8) | 97 (5.9) |
| White | 59 (4.1) | 36 (15.0) | 95 (5.7) |
| Other | 573 (40.5) | 84 (23.8) | 657 (39.7) |
| Child ethnicity | |||
| Hispanic | 617 (43.6) | 79 (43.7) | 696 (43.6) |
| Non-Hispanic | 797 (56.4) | 102 (56.4) | 899 (56.4) |
| Child sex | |||
| Female | 699 (49.4) | 135 (56.0) | 834 (50.4) |
| Male | 715 (50.6) | 106 (44.0) | 821 (49.6) |
| Child overweight/obese* | |||
| BMI % ≥85th - <95th | 214 (16.3) | 30 (14.0) | 244 (16.0) |
| BMI % ≥95th | 249 (19.0) | 48 (22.4) | 297 (19.4) |
| Parent highest level of education | |||
| <High school | 353 (25.2) | 40 (20.8) | 393 (24.7) |
| High School or GED | 552 (39.4) | 97 (50.5) | 649 (40.8) |
| Some college | 301 (21.5) | 21 (10.9) | 322 (20.2) |
| ≥ Associate’s degree completed | 194 (13.9) | 34 (17.7) | 228 (14.3) |
| Married | 353 (27.8) | 90 (57.0) | 443 (31.0) |
| Parent primary language | |||
| English | 497 (35.4) | 32 (16.3) | 529 (33.0) |
| Other | 908 (64.6) | 164 (83.7) | 1072 (67.0) |
ABCD – Action for Boston Community Development, the Boston Head Start agency
CAAS – Community Action Agency of Somerville, the Cambridge and Somerville Head Start agency
ABCD Head Start serves over 1,400 preschool-aged children and their families each year across Boston, Massachusetts. Twelve ABCD Head Start programs operating across 19 centers are participating in the study. Each program has its own director and has a nutrition and health services manager who is responsible for overseeing the implementation of child and parent health programming. In the 2016–2017 school year, 41% of the children were Black/African American, 4% were Caucasian/White, 9% were Asian, 6% were multiracial, and 44% were Hispanic/Latino. Approximately 16% of children had overweight and 19% had obesity.
CAAS Head Start is a smaller agency serving nearly 250 children and their families across Cambridge and Somerville, Massachusetts. Four CAAS Head Start programs are participating in the current study; unlike ABCD, all programs operate under a single director and health services manager. In the 2016–2017 school year, 22% of the children were Black/African American, 15% were Caucasian/White, 23% were Asian, 6% were multiracial, and 44% were Hispanic/Latino. Approximately 14% of children had overweight and 22% had obesity.
b. Trial design and randomization procedure
Group-based random assignment to the CHL intervention versus control (i.e., usual practice) is implemented at the level of the Head Start program (N=16). We elected to randomize at the program versus the center level to reduce the risk of contamination. Multi-center programs share staff across centers, and most centers in the same program are in close proximity. In some instances, health or nutrition staff work across multiple programs; that is, there are 10 health/nutrition staff for 16 programs. Given the central role of these staff in intervention implementation and to prevent such staff from simultaneously being in control and intervention conditions, programs that were serviced by the same health/nutrition staff were randomly assigned as a unit to an intervention condition. Thus the random assignment procedure, which was implemented by the data manager with oversight from the study statistician, placed a greater emphasis on minimizing contamination than ensuring equality of groups at baseline. The within group design utilized (summarized next) minimized the potential impact of this decision on the internal validity of the results.
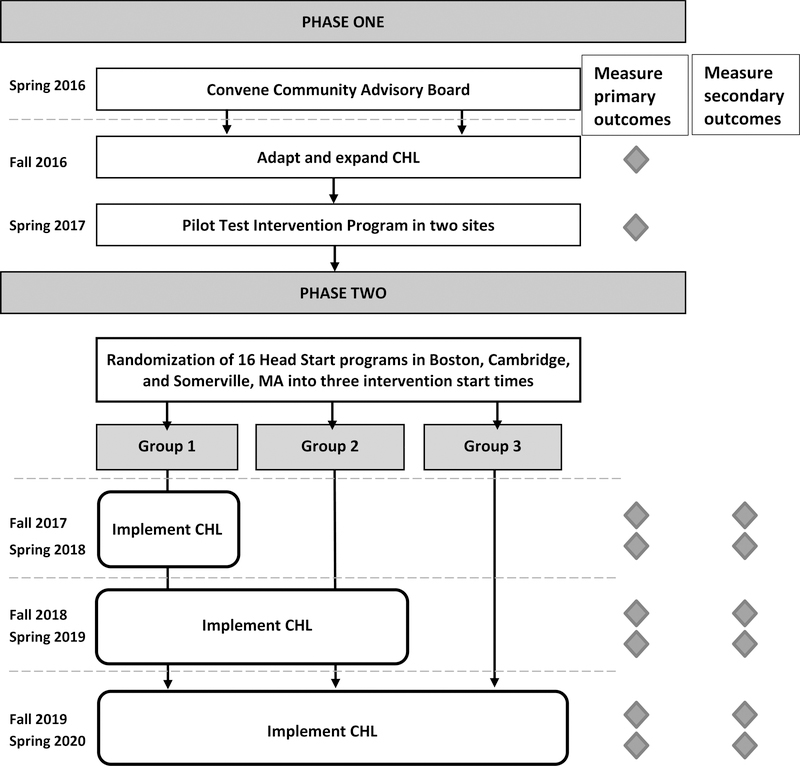
In a standard two-arm cluster-randomized trial, half of the 16 participating Head Start programs would not receive the intervention they helped design. To avoid this, we used a stepped wedge design [28,29] in which all Head Start programs receive the intervention, but with the timing of intervention initiation randomly assigned. Since CHL is implemented over three academic years (i.e., September through to June), Head Start programs were assigned to one of three start times; five programs were assigned to start in fall 2017, five programs to start in fall 2018, and six programs to start in fall 2019. The one-year step length was chosen because CHL intervention elements are offered on a yearly basis. Two Head Start sites participated in a pilot test of the parent class in spring 2017; the Head Start programs containing these sites were non-randomly assigned to begin the intervention in the first year of the trial because the health staff at these programs had already implemented part of the intervention. Parent exposure to intervention content at these sites prior to the start of the trial was minimal because only ~15 parents participated in the pilot test and many of those parents did not return the following academic year because their children aged out of Head Start. Programs overseen by other staff were randomly assigned to intervention start times across the three years. The study design and timeline are illustrated in Figure 1. As a pragmatic study, the stepped wedge balances the goal of causal inference and the constraints of a policy or service delivery setting [28]. This was particularly important given the vulnerable populations with which this study is working and the expectation that CHL will do more good than harm based on the results of the pilot trial [23]. Furthermore, this design is consistent with the principles of CBPR, which include integration of knowledge and action for the benefit of all partners [30].
Figure 1.
Timeline and stepped wedge design for the Communities for Healthy Living (CHL) trial.
c. Theoretical Frameworks and Participatory Methods
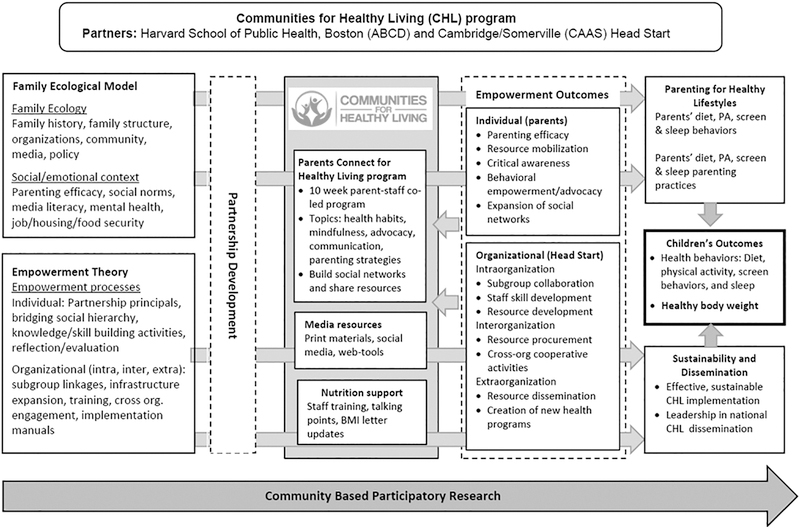
CHL’s theory of change, which integrates family and empowerment theories, is illustrated in Figure 2. Intervention content is informed by the Family Ecological Model, which emphasizes that broader environmental factors shape the proximal social and emotional context of families, and therefore must be addressed to facilitate sustainable behavior changes that promote healthy child weight. As such, CHL’s intervention content spans contextual factors such as neighborhoods and social networks in order to more effectively target the five Healthy Habits at the core of the intervention that promote healthy child weight (i.e., increased fruit and vegetable consumption, decreased sugary beverage consumption, increased physical activity, increased sleep, and reduced screen time [3–6]).
Figure 2.
Communities for Healthy Living (CHL) Theory of Change.
CHL was designed to affect parent and organizational outcomes through the processes of individual [15,16] and organizational empowerment [12–14] (see Table 2), which are, in turn, expected to lead to positive child health outcomes. Empowerment processes began with engaging Head Start staff and parents as equal partners in the development of intervention components, using CBPR best processes [31,32]. To build the ethos of CBPR into the structure of CHL, financial resources were shared between academic researchers and Head Start partners through subcontracts. Additionally, CHL Coordinators were hired to work within each Head Start agency to ensure adequate organizational capacity to develop CHL and compile evaluation data.
Table 2.
CHL intervention components and corresponding theory, implementation science principles, and Head Start performance standards.
| Intervention component | Theoretical constructs | Example implementation science principles | Relevant Head Start performance standards | |
|---|---|---|---|---|
| Individual-Level |
Parents Connect for Healthy Living (PConnect) A 10-week parent empowerment class co-led by a Head Start staff member and a Head Start parent. Class sessions are supplemented with parent Facebook groups, which also serve to help parents stay connected after the program. |
Family Ecological Model1: • sessions 1 – 5: child-level • sessions 6 – 7: family-level topics • sessions 8 – 9: broader context (neighborhoods, social networks, advocacy) • culture is integrated into all sessions Psychological Empowerment Theory2: • activities build knowledge, selfefficacy, and interpersonal skills • participation expands parents’ social networks and introduces community resources that promote family health Organizational Empowerment Theory3: • implementation by Head Start staff and parents builds organizational capacity for family engagement |
Formative research and community buy-in: • key stakeholders (e.g., parents, Head Start staff) developed PConnect with researchers through the CBPR process, building community buy-in and ensuring culturally appropriate content Adaptation of delivery to cultural context: • Trained parent facilitator is encouraged to make culturally- relevant connections to class content • PConnect offered in different languages across sites Intervention implementation • PConnect is co-facilitated by a Head Start staff member and Head Start parent |
• Family support services for health, nutrition, and mental health (1302.46) • Family engagement (1302.50) • Parent activities to promote child learning and development (1302.51) • Family partnership services (1302.52) |
| Organizational-Level |
Enhanced Nutrition Support Child health screening reports, which include child BMI, were revised with CAB input to effectively communicate the meaning of BMI and highlight next steps parents can take. Standardized protocols and resources were developed to enhance nutrition counseling offered by Head Start. Staff also receive ongoing training. |
Family Ecological Model1: • Increases parent knowledge about child health • Improved organizational capacity to communicate with parents about health Psychological Empowerment Theory2: • Connect parents to community resources to support family health. Organizational Empowerment Theory3: • Staff have opportunities for training and continued professional growth |
Alignment to organizational priorities: • Enhanced nutrition support builds on current required Head Start practices: biannual child health screenings and family nutrition counseling Ongoing training and support: • Non-health and nutrition staff (e.g., teachers) receive training and resources to discuss child health with parents |
• Child Health Status and Care (1302.42) • Family support services for health, nutrition, and mental health (1302.46) • Family partnership services (1302.52) |
|
Media Campaign Parents receive brochures promoting key weight- related child health behaviors. Health behavior messaging is reinforced with posters displayed in Head Start Centers. Parents can find information and resources online through Facebook and the Neighborhood Resource Map. |
Family Ecological Model1: • Increases parent knowledge about child health • Connects parents to community resources through CHL website Psychological Empowerment Theory2: • The media campaign equips parents with key knowledge to promote child health and connects them to a broad network of community resources, such as farmers markets that accept federal nutrition assistance benefits and family activities that can serve as alternatives to screen time Organizational Empowerment Theory3: • Builds organizational capacity to communicate with parents about child health • Staff build skills in working collaboratively within and across Head Start organizations to develop materials through the CBPR process |
Working within existing systems of care: • CHL uses existing strategies of communicating with families to disseminate educational materials and connect families to community resources |
• Family support services for health, nutrition, and mental health (1302.46) |
Family ecological model - Family ecology (e.g., community factors, media and policy factors) shapes the family social and emotional context (e.g., social disparities and chronic stress), which, in turn, shapes the parenting practices that are critical for child health (e.g., food parenting, physical activity parenting) [11].
Psychological empowerment theory - Empowerment at the individual level, or the processes by which people gain control over their lives, can be described in four domains: emotional component (e.g., perceived competence), cognitive component (e.g., skill development), relational component (e.g., network mobilization), and behavioral component (e.g., community involvement) [15].
Organizational empowerment theory - Empowerment at the organizational level, or an organization’s ability to achieve its goals and empower its members, can be de scribed in three domains: intraorganizational (e.g., leadership, social support), interorganizational (e.g., participating in alliance-building activities with other organizations), and extraorganizational empowerment (e.g., implementing community actions) [12–14].
CBPR - community-based participatory research, CAB - community advisory board, BMI - body mass index
With intentional integration of family ecological factors and empowerment processes in the development, design, and implementation of the trial, CHL is expected to lead to improvements in parents’ individual empowerment (e.g. parenting efficacy, advocacy skills, and expansion of social networks), and Head Start organizational empowerment (e.g. Head Start staff skill development and cross-organization cooperation) (Figure 2). In turn, we hypothesize that empowerment will lead to positive parenting practices that support all five Healthy Habits, thereby impacting child weight.
d. CHL Intervention Components
During the 2009–2011 pilot study, the original version of CHL encompassed: 1) a group-based 6- week parenting program (total of 12 hours), 2) nutrition resources such as revised health letters sharing the results of Head Start child health screenings (i.e., hearing, vision, and BMI), and 3) media resources to increase parent awareness of childhood obesity and its health implications. As summarized in Figure 1, in the current trial, each Head Start agency convened a community advisory board (CAB) consisting of Head Start parents and staff. In the early stages of the trial, the CABs were responsible for adapting and improving the original intervention components, including ensuring their cultural relevance for the diverse parents in the greater Boston area. Key modifications to CHL resulting from this process include the expansion of the parenting program to 10 weeks (total 20 hours) and the addition of nutrition support resources for Head Start staff, including protocols for family outreach. Media resources in the original pilot study were limited to posters; for the current trial, this was expanded to also include brochures, social media, and other online resources. The revised parenting program and the evaluation surveys developed specifically for the study were pilot tested in spring 2017 prior to initiation of the randomized trial in fall 2017. The final intervention components are described below and summarized in Table 2 along with their corresponding theoretical constructs, implementation science principles, and Head Start performance standards.
Parent Program
Parents Connect for Healthy Living (PConnect) is a 10-week health and empowerment class co-led by a Head Start parent and a Head Start staff member (Table 2). Parents are eligible to participate if they are a primary caregiver or family member of a child currently enrolled in an intervention Head Start program. Each intervention Head Start program implements PConnect once per school year in English or Spanish. Staff leaders determine the day and time to hold their PConnect program and the method of recruiting parent participants most feasible at their center (e.g. informational flyers, sign-ups at parent meetings, etc.).
Every PConnect program runs for two hours once per week. Sessions are designed to address the key topics highlighted as important by the CAB. These topics align with the levels of the Family Ecological Model; sessions 1–5 focus on the child (e.g. child health behaviors), culminating in parents developing a goal for their family based on one of the five Healthy Habits. Sessions 6 and 7 focus on the parent (e.g. stress management, healthy family relationships), and the final sessions address the broader environment (e.g., social networks, neighborhoods, and advocacy). The ten-week length of PConnect provides sufficient time to address the topics deemed important by the CAB while being a feasible time commitment for parents and facilitators. It is worth noting that sessions place a consistent focus on child and family mental and physical health; neither weight nor weight loss are a focus to avoid propagating weight stigma [33]. The topics covered in each session are further detailed in Table 3.
Table 3.
Content for each session of the Parents Connect for Healthy Living (PConnect) program.
| Objectives | Activities | |
|---|---|---|
| All Sessions | Parents share a meal together and: 1. Deepen the sense of community already forming. 2. Practice healthy mealtime habits that can be replicated at home. |
Open with Meal and Group Discussion: Share a meal together; share experiences related to PConnect from the past week; reflect on goal. Close with Reflection and Wrap Up: Reflect on what we did today, review additional resources, and talk about what is coming up next week. |
| 1: Welcome and Health Connections | 1. Explain how PConnect will help my family become healthier. 2. Contribute to the PConnect Community Ground Rules that will allow families in the PConnect community to achieve their goals. 3. Describe what health means to me. |
1. Welcome to PConnect: Meet others and get an overview of PConnect. 2. Setting Community Ground Rules: Contribute to setting ground rules. 3.What is Health?: Define what health means to each of us and explore how session topics are interconnected. |
| 2: Nutrition and Physical Activity | 1. Use the healthy eating, avoid sugary drinks, and physical activity brochures to teach others about these topics. 2. Name at least three strategies I plan to use to help my children and family with nutrition and physical activity. |
1. Why are Nutrition and Physical Activity Important for Children? Learn about nutrition and physical activity. 2. Parent Experts: Share and discuss parenting strategies to make sure Head Start kids are eating healthy, avoiding sugary drinks, and being active. 3. Healthy Habit Station: Get a hands-on experience to promote healthy nutrition and physical activity at home. |
| 3: Sleep and Screen Time | 1. Use the sleep and screen time brochures to teach others about these topics. 2. Name at least three strategies I plan to use to improve my child’s sleep and reduce their screen time. |
1. Why are Sleep and Screen Time Important for Children? Learn about sleep and screen time. 2. Parent Experts: Share and discuss parenting strategies to make sure Head Start kids are sleeping well and limiting screen time. 3. Creating a sleep and screen time plan: Create a plan to improve my child’s sleep and screen time habits. |
| 4: Goal Setting and Supporting Resources | 1. Use the CHL Neighborhood Resources Map and www.HelpSteps.com to identify local resources. 2. Add new resources to the CHL Neighborhood Resources Map. 3. Describe a Healthy Habit goal I have set for my child. |
1. Choosing a Healthy Habit Focus: Pick one of the five Healthy Habits to focus on. 2. Neighborhood Resource Map: Learn how to identify community resources for the Healthy Habits using the CHL Neighborhood Resources Map. 3. HelpSteps.com: Learn how to identify resources using HelpSteps.com. 4. Healthy Habit Goal Setting: Create a SMART goal for one of the Healthy Habits to accomplish by the end of PConnect. |
| 5: Child Personality | 1. Describe the eight parts of child temperament/personality. 2. Identify and use parenting strategies specific to my child’s personality. 3. Use positive guidance as a general parenting strategy for all child personalities. |
1. Child Personality: Learn about the eight personality traits and connect them to my own child. 2. Parenting toward the Big Goal: Identify parenting strategies to help achieve my PConnect Big Goal that are specific to my child’s personality. 3. Positive Guidance: Learn about and plan to use positive guidance strategies |
| 6: Mindfulness | 1. Explain the importance of self-care in my own life. 2. Identify the signs and symptoms of stress and explain the effects of stress on health and family. 3. Identify ways to incorporate stress management techniques, including mindfulness, into daily life. |
1. The Giving Tree: Read the Giving Tree and discuss the importance of self-care as a parent. 2. Acknowledging our Stress: Discuss the health effects of stress. 3. Stress Management and Mindfulness: Share stress management strategies and learn about mindfulness. 4. Practicing Mindfulness: Practice mindfulness exercises. |
| 7: Healthy Family Relationships | 1. Identify healthy and unhealthy characteristics of family relationships. 2. Identify my own parenting style. 3. Use communication strategies to resolve conflict with my child’s other caregivers. 4. Incorporate healthy communication practices into daily life. |
1. My Family RelationSHIP: Share ideas about what makes a relationship healthy. 2. Parenting Styles:Identify personal parenting style and conflicts that arise between caregivers. 3. Healthy Communication Skills: Identify healthy communication skills for conflict resolution and daily life. |
| 8: Neighborhoods and Social Networks | 1. Describe the positive and negative effects of my neighborhood on my family’s health. 2. Know how to make healthy changes in my neighborhood by getting involved. 3. Define “social network” and identify my own. 4. Explain how social networks can be used to improve the health of children, parents, and families. |
1. Welcome to the Neighborhood: Identify positive and negative effects that neighborhoods have on health. 2. Introduction to Community Involvement: Learn about government and other ways to get involved in the community. 3. Social Networks for Health: Identify my own social network and learn how it can be used to make my community healthier. |
| 9: Parental Advocacy | 1. Define advocacy and explain its importance for my child’s health and the health of my family. 2. Name the steps required to advocate for something I care about. 3. Use the advocacy steps and effective communication strategies to advocate for my child. |
1. What is Advocacy: Learn the definition of advocacy and see an example of parents using the five advocacy steps to work on an issue in their neighborhood. 2. Advocacy at School: Discuss an example of a parent using the five advocacy steps to help her child in Head Start. 3. Advocacy at the Doctor’s Office: Create a plan to advocate for my child at the doctor’s office. |
| 10: Graduation | 1. Describe my family’s progress towards health goals set at the beginning of PConnect. 2. Describe new health goals for families to pursue. 3. Have a plan promote healthy families in my community. 4. Express gratitude for one another and the people who have supported me throughout PConnect. |
1. How Far We’ve Come: Reflect on the progress made with my goal and create a new goal. 2. Committing to Leadership: Make a plan to promote healthy families in our community. 3. Graduation Ceremony: Receive a certificate and give thanks to those who supported me during PConnect. |
To support parent engagement between sessions, PConnect participants are provided an activity to complete outside of the session that requires application of new knowledge and skills; often, these activities include involvement of their children and other family members. Additionally, all participants are invited to a closed Facebook group, where facilitators post content related to that week’s session and encourage parent input. The Facebook group is also a platform for parents to strengthen relationships with one another and maintain relationships after their PConnect program ends.
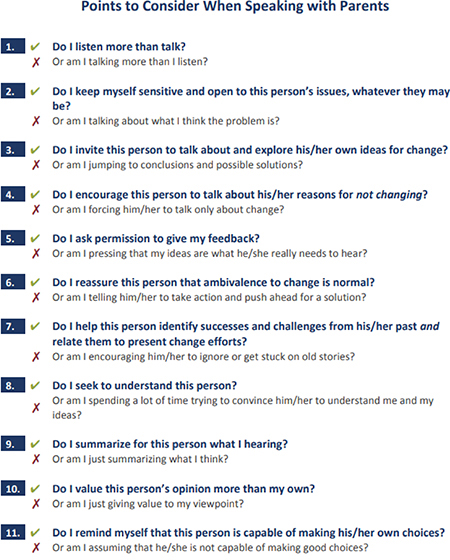
An innovative feature of PConnect is its co-facilitation by a Head Start parent and staff member. Inclusion of parents as facilitators supports the CHL goal of parent empowerment and helps to ensure that PConnect delivery at each Head Start center matches the cultural context of that center. Parent facilitators are recruited through a variety of approaches: CAB members, informational flyers, and direct recommendations from Program Directors and other Head Start staff. Facilitators complete a three-day training on the use of all PConnect materials, collaborating with their co-facilitator, group facilitation skills, and managing the Facebook group. In addition, facilitators participate in weekly coaching sessions with the CHL Coordinators during the PConnect program to help them reflect on each session and prepare for the coming week. Parent facilitators are given a stipend to compensate them for their time and effort.
Enhanced Nutrition Support
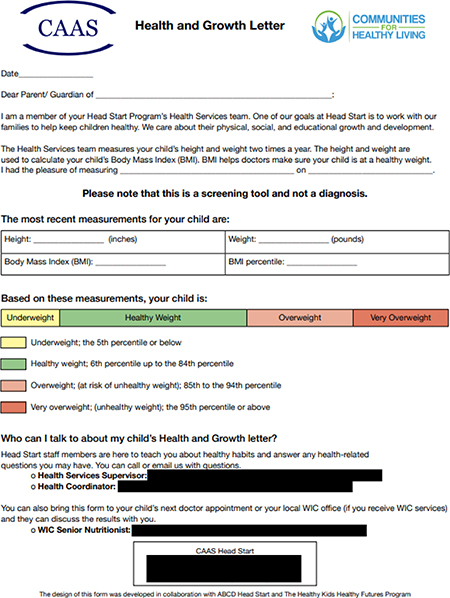
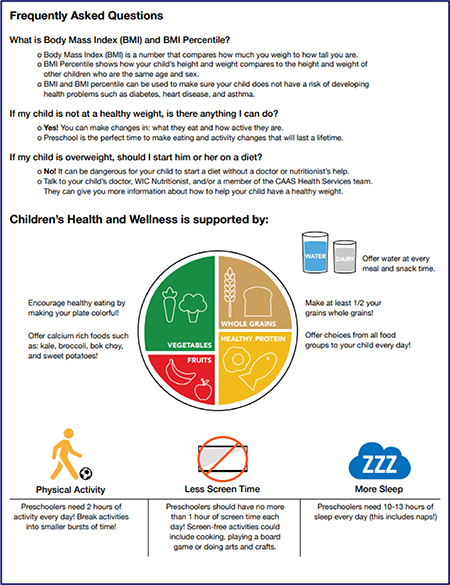
Enhanced nutrition support is an organizational component designed to reach all Head Start families in intervention programs (Table 2). Head Start already distributes a Health and Growth Letter, which communicates results from child health screenings to families, including information about their child’s BMI. Our formative work revealed that this letter is often ignored or poorly understood. Parents often underestimate the weight of children with overweight and obesity [34], which is concerning because accurate perception of childhood overweight is associated with readiness to make health behavior changes like improving the family’s diet [35]. To address this challenge, the CAB developed a Primer Letter to precede the Health and Growth Letter, giving families in intervention programs advanced notice about the Health and Growth Letter and helping them understand the content. Additionally, families at intervention sites receive a revised Health and Growth Letter designed to optimize parent understanding and highlight next steps to support child health. A sample copy of the letter can be found in Appendix A. Next steps included in the letter, such as ways to increase physical activity, are highlighted as ways to promote child health, not ways to promote child weight loss. Not all parents may be interested in changing their child’s weight status due to personal beliefs and/or cultural values regarding child weight [34]. As such, while the letter does aim to increase parents’ weight perception accuracy, which may have a stronger effect for the parents of children with overweight or obesity, CHL encourages healthy lifestyles for all children because all parents are interested in promoting their children’s health.
Our formative work also revealed that parents frequently ask questions about the Health and Growth Letter to non-health staff at Head Start. However, these staff members do not receive any training on fielding questions related to child BMI or other health topics, so the CHL team developed staff talking points to guide these conversations. Staff in intervention programs are trained on best practices for using the talking points during regular staff training.
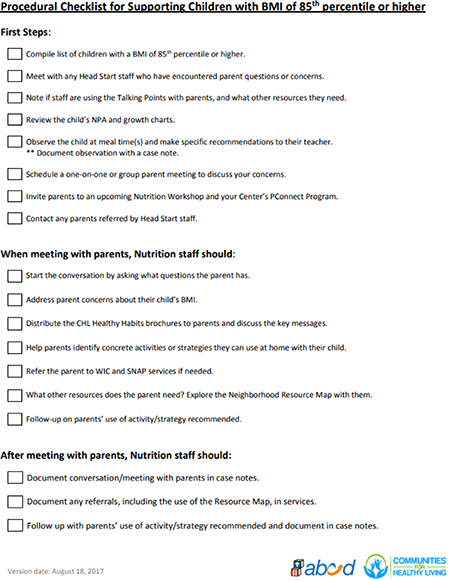
Head Start performance standards require follow-up with the families of children at or above the 85th percentile for BMI (overweight or obese) (Table 2), but it was cumbersome for staff to reference the existing protocols for these meetings. In close collaboration with Head Start health and nutrition staff, the CHL team updated the protocol for nutrition counseling meetings with these families. The team also made procedural checklists to provide staff with an easy-to-follow outline of key domains and messages to cover. A sample procedural checklist can be found in Appendix B.
Media Campaign
The CHL media campaign is another organization-wide strategy to ensure that key intervention messaging reaches all families in Head Start intervention programs (Table 2). Educational brochures were created to present key information related to each of the five Healthy Habits and highlight practical strategies to encourage behavior change at home. Brochures are distributed on a monthly basis to all parents at intervention programs using established channels of communication with parents at that program (e.g., placing brochures into children’s backpacks). Distribution is also incorporated into existing Head Start programming when feasible. For example, upon entering the intervention arm of the trial, brochures are distributed at ongoing monthly health and nutrition workshops offered by some Head Start programs. Posters and targeted flyers are displayed at all intervention sites in areas frequented by parents (e.g. event bulletin boards, classroom doors, entryways) to further reinforce the health messaging of the brochures and promote CHL branding.
The brochures, posters, and flyers can teach families about health recommendations, but they may be limited on their own because many families lack the resources necessary to implement health behavior changes at home. To connect families with supportive resources, the research team created an online Neighborhood Resource Map that highlights affordable resources related to the each of the five Healthy Habits across the greater Boston area. For example, nutrition resources on the map include food retailers such as grocery stores and farmers markets where federal nutrition assistance benefits can be redeemed (i.e., the Supplemental Nutrition Assistance Program and the Special Supplemental Nutrition Assistance Program for Women, Infants and Children) and food pantries. All Healthy Habits brochures prominently feature a link to the Neighborhood Resource Map, which parents can access on a computer, phone, or tablet using a password. To restrict access to parents in intervention Head Start programs, the map is password-protected. A final unique feature to this element of the media campaign is that the map is a “living” resource; staff and parents can share their knowledge of health-promoting resources in their neighborhoods by adding them to the map.
Alignment with Head Start performance standards
All CHL components are designed to align with Head Start performance standards (Table 2), which were updated nationally in November 2016 prior to the start of the trial, to ensure that CHL matches Head Start organizational priorities. For example, PConnect helps participating programs meet their family engagement performance standard (1302.50). By implementing CHL, Head Start centers can meet key performance standards, improving CHL’s potential for scale-up.
e. Data collection and measures
A summary of the study measures, example questions, and measure sources is provided in Table 4. Child outcomes include child BMI (primary outcome) and child health behaviors including diet, physical activity, sleep, and screen use (secondary outcomes). Data for all child outcomes are extracted from an existing Head Start database utilized by both agencies (ABCD and CAAS Head Start) for all children currently enrolled at a participating Head Start program. Child outcome data will be extracted for the year preceding the trial (i.e., 2016–2017) and all three years of the trial (2017–2020). Parent outcomes, which include child health behavior parenting practices (e.g., food parenting, physical activity parenting) and parent empowerment, are measured by the research team for a subsample of families using a survey administered in fall and spring for all three intervention years (Figure 1). Any parent, guardian, or primary caregiver of a child currently enrolled at a participating Head Start program is eligible for the parent survey.
Table 4.
Primary and secondary outcomes measures and their sources.
| Construct | Example item | Measure or item source | Data source |
|---|---|---|---|
| Primary outcome | |||
| Child weight status Body Mass Index z-score, overweight status |
Measured height and weight | Direct height and weight measurement by trained Head Start staff | Head Start database |
| Secondary outcomes | |||
| Child diet Fruit, vegetables, 100% juice, sugary beverages, water, snacks, fast food |
In the past month, on average, how often did your child eat vegetables (do not include French fries, fried potatoes or potato chips) | Harvard Service Food Frequency Questionnaire [36], School Physical Activity & Nutrition Survey [37] | Head Start database Nutrition and Physical Activity survey (NPA) |
| Child physical activity Structured and unstructured min/day |
On a typical day, how much time does your child spend in organized physical activities (ex. Swimming, soccer, gymnastics) | Adapted from Burdette, 2004 [38] (validated parent report of preschool child physical activity) | Head Start database NPA |
| Child screen use TV, computer or game console, smartphone or tablet, screens in sleep environment |
On a typical day, how much time does your child spend using a smartphone or tablet? | School Physical Activity & Nutrition Survey [37] | Head Start database NPA |
| Child sleep Regular bedtime, sleep |
What times does your child usually fall asleep at night/wake up in the morning)? | Brief Infant Sleep Questionnaire and extended version [39] | Head Start database NPA |
| duration (evening) | |||
| Food parenting | I offer sweets (candy, ice cream, cake, pastries) to my child as a reward for good behavior. | Comprehensive feeding practices questionnaire [40] | Parent Outcomes survey (POS) |
| Physical activity parenting | I take my child outside to play when the weather is nice. | Activity Support Scale [41] | POS |
| Screen parenting | I limit my child’s screen time. | Generic | POS |
| Parent Diet | During the past 4 weeks, on average, how often did you eat vegetables including raw, cooked, canned or frozen vegetables? | National Health and Nutrition Examination Survey Dietary Screener Questionnaire [42] | POS |
| Parent Physical Activity | How much time do you spend walking or bicycling for travel on a typical day? | National Health and Nutrition Examination Survey Physical activity and fitness questionnaire [43] | POS |
| Parent Sleep | About how many hours of sleep do you usually get on a typical day? | Generic | POS |
| Parent Empowerment | I know how to find programs, services, or other resources that my child needs in my community. | Developed by CHL team based on Spreitzer’s Empowerment Scale [44] | POS |
Primary outcome
The primary outcome is change in child age- and sex-specific Body Mass Index z-score (BMIz) calculated with the Centers for Disease Control and Prevention 2000 growth charts [45]. Head Start programs nationally are mandated to measure children’s height and weight each year of enrollment. In this trial, per standard practice, child height and weight are measured each year by Head Start health services staff within 45–90 days of enrollment (typically September-October) and in spring (April-June), and entered into the Head Start administrative database. To support the validity of these measurements, the research team leads a training session each fall on recommended practices for child height and weight measurement [46] for the health services staff. During this training, staff are given manuals the CHL team created to improve data quality. Prior to spring BMI measurements, the CHL team checks in with staff and addresses any questions or concerns regarding measurement. Any new staff members are trained personally by a CHL Coordinator as soon after their hire date as possible. Furthermore, prior to the first baseline BMI measurement in Fall 2016, all measurement equipment was replaced to standardize the exact model used across all sites.
Secondary outcomes
Child secondary outcomes (i.e., diet, physical activity, screen time, and sleep) are measured using a parent report survey, referred to as the Nutrition and Physical Activity Assessment (NPA). The NPA is integrated into the annual Head Start enrollment process to maximize the proportion of families completing the survey; an additional administration each spring (April – June) is supported by research funds distributed to Head Start through subcontracts as part of the CHL trial. The survey is available in English, Spanish, Chinese, Haitian Creole, Portuguese, Somali, and Arabic. To support standardized data collection across all programs, the research team conducts multiple trainings per year with Head Start staff on the administration of the NPA. Head Start health and nutrition staff enter NPA responses into the child’s record in the Head Start database, along with information on date of completion, survey language, and respondent (i.e., mother, father, grandmother, etc.).
Parent secondary outcomes are measured using a second parent survey, the Parent Outcomes Survey (POS). As indicated in Table 4, all survey items are drawn from validated surveys (e.g., School Physical Activity and Nutrition Survey) or from large national studies (e.g., National Health and Nutrition Examination Survey). This survey was pilot tested in a quality improvement phase during spring 2017 with a sample of 27 parents. Changes were made to the wording of items to better match the literacy level of the parents who participated in pilot testing. Based on cognitive interviews done with these parents, questions that were confusing, repetitive, or lengthy were removed from the POS.
The POS is administered in fall each year in English, Spanish, or Chinese to a subsample of parents and primary caregivers of children enrolled in participating Head Start sites. While all families are invited to complete the POS, only ~30% of families from each center are needed to complete it to achieve the target sample size; recruitment efforts stop after reaching the target at each center. In the baseline and first year of the trial, trained research assistants (most of whom are bilingual in English-Spanish or English-Chinese) recruited participants at events that draw large numbers of parents (e.g., drop-off/pick-up times, recurring and regularly scheduled parent programs, workshops, meetings). Starting with the second year of the trial, POS questionnaires are delivered to all parents through their childr en’s classrooms; parents self-administer the POS. Additionally, all parents/caregivers who participate in the PConnect program are invited to complete the POS if they have not already done so. Parents who complete the survey in fall are contacted in spring (April-June) and invited to complete the survey a second time. Parents complete the spring survey using an online survey link they receive through email, by phone with a trained research assistant, or with a hard copy of the questionnaire that they receive and return to their child’s classroom teacher or family advocate. The method of survey administration is documented.
f. Process Evaluation
In addition to evaluating child and parent outcomes, we will conduct a comprehensive process evaluation to document intervention implementation. Full details are described in a forthcoming publication. Briefly, using the Pérez et al. evaluation framework for adaptive interventions [47], CHL’s process evaluation captures implementation of all intervention elements in three domains: adherence to intervention protocols, adaptation of intervention protocols, and moderators of intervention implementation and effectiveness. Intervention implementation is monitored using multiple data sources including administrative records (e.g., sign in sheets), brief surveys, and semi-structured interviews with parents and staff. Organizational outcomes including organizational capacity (i.e., job satisfaction, role overload, professional development, effects on other Head Start functions) are also integrated into the process evaluation.
The adaptive intervention framework was deemed appropriate because adaptations are expected in order to make CHL fit the demographically and culturally diverse communities in the greater Boston area. Core, non-adaptable aspects of CHL are differentiated from adaptable elements during staff and parent trainings. For example, the PConnect manual highlights aspects of sessions that can be adapted and even provides examples of potential adaptations, which are reviewed during the PConnect facilitator training. Adaptations made are carefully tracked.
g. Informed consent and data integration
Data for child outcomes (i.e., BMI, weight-related behaviors) and family demographics are collected using passive consent procedures. Each year, Head Start families receive information specifying the health measures that Head Start collects for all children (e.g., height, weight, diet, hearing and vision screening) and are informed that de-identified health information for their child could be used for quality improvement or research purposes. Parents have the opportunity to opt out at this point. De-identified child health data and family demographics are extracted biannually from all participating programs, and are transferred to the research team through a data sharing agreement. The extracted variables include child height and weight measurements, child sex, child age in months at BMI measurement, family demographic information (e.g. marital status, education, race/ethnicity), child health behavior from the NPA, administration data (e.g. survey language), and child and family Head Start ID number. Of note, the Head Start ID numbers are agency-specific and cannot be used to identify an individual or linked with personal information outside of each agency’s Head Start database.
Data for parent outcomes are collected using an active consent protocol. At the time of recruitment to complete the POS in fall each year, trained research assistants explain potential risks and benefits of completing the survey, the procedures in place to protect their privacy, that their responses will be linked to their child’s health and demographic data using their Head Start ID number, and that they will be contacted the following spring to complete the survey again. Parents receive a $10 gift card for each survey they complete. Research assistants respond to any questions or concerns raised by parents. Parents indicate whether they agree to participate via a check box on the survey. Data are housed on a secure server at the Harvard T.H. Chan School of Public Health.
3. ANALYTIC STRATEGY
a. Sample Size and Power
Statistical power was evaluated using the approach developed by Hussey and Hughes for mixed effects models analysis of data arising from a cluster-randomized trial [29]. Based on preliminary analyses of all children aged 3 to 5 years enrolled at the participating Head Start centers from 2015–2016 and data from the pilot study [23], we anticipate (in the absence of the intervention) a mean BMIz of 0.65 and a standard deviation of 0.15. For the proposed design, we anticipate having at least 90% power to detect a reduction in mean BMIz from 0.65 to 0.60 under the proposed intervention, assuming an average of 50 children per program, a within-site standard deviation of 0.20, and a coefficient of variation of 0.20. Each of the latter three components were chosen so that the evaluation would be conservative. Specifically, while an average of only 50 children was assumed, the actual average across 16 programs in 2015–2016 was 100.
Furthermore, the coefficient of variation was set at the lower bound of the range recommended by Hussey and Hughes [29]. Finally, we note that even under the more conservative setting of a standard deviation of the BMIz score of 0.25, statistical power is expected to be above 85%. Because primary outcome data are collected from all children, the only attrition will be due to children leaving the program, which was factored into the average program size of 100 observed in 2015–2016.
b. Statistical Methods
We will test the following hypotheses:
H1: Compared with pre-intervention, children enrolled in intervention Head Start programs will show significant declines in BMIz (H1a) and improvements in diet, physical activity, screen time, and sleep (H1b);
H2: Compared with pre-intervention, parents of children enrolled in intervention Head Start programs will exhibit significant improvements in food, physical activity, screen, and sleep parenting;
H3: Intervention-related improvements in parenting practices will be explained by changes in empowerment-related mediators.
Prior to hypothesis testing, we will conduct detailed exploratory descriptive analyses to examine the distributions of key baseline demographic variables. Additionally, we will characterize any missingness in these variables, including patterns across key demographic variables. While our primary analysis will examine the effect of CHL on change in child BMIz (H1a), we will use the same analytic strategy for all child and parent outcomes; the description provided here is, therefore, for a generic outcome. Let Δkit denote the change in the outcome between fall and spring of the tth year for ith child in the kth Head Start program. Furthermore, let Xkt be a binary indicator of whether the kth Head Start program has initiated the intervention in the tth year. To evaluate the impact of the intervention on the outcome, we will build a series of regression models for the mean of Akit as a function of Xkt. To account for the repeated measurements within children over time and the clustering of children within Head Start programs, we will use generalized linear mixed models using appropriate child- and center-specific random effects [48]. In addition to the intervention indicator, baseline (i.e. pre-intervention) indicators of the outcome will be included as well sex and age of the child/parent and family socioeconomic status. Based on these models, the regression parameter for Xkt, βx will be tested for clinical and statistical significance. We will perform mediation analyses to examine the impact of empowerment measures following the approach of Baron and Kenny [49].
Despite integration of data collection into Head Start enrollment and other standard organizational procedures designed to capture all enrolled families, some missing data is likely. Since analyses using generalized linear mixed models are likelihood-based, estimation and inference is valid when the data are missing-at-random (i.e., when the processes/decisions that govern whether complete data are available solely depend on variables that are either unrelated to the study question or are measured) [50]. In the event of a potential violation of the missing-at-random assumption (i.e., the data are missing-not-at-random or, equivalently, the missingness is non-ignorable), we will use the selection model framework as a basis for conducting sensitivity analyses [51].
4. ETHICS
The CHL trial protocol has been approved by the Institutional Review Board at the Harvard T.H. Chan School of Public Health. This study was designed and is being conducted in accordance with the principles of the Declaration of Helsinki, 5th revision.
The trial is registered at ClinicalTrials.gov (NCT03334669). All participants will receive written information about the study and provide consent. Signed consent is not required for every measure and the participants are informed about their right to opt out at any time. No more than minimal risk is associated with participating in the CHL trial (i.e., negligible emotional discomfort while completing the Parent Outcome surveys and attending PConnect sessions). However, risk will be mitigated by training and re-training of the facilitators.
5. DISSEMINATION
Results of the CHL study will be disseminated via scientific publications and conferences according to pre-determined publication policy. There will be presentations to public health working groups and Head Start internal sources as well as a public CHL website (https://www.hsph.harvard.edu/chl/).
6. TRIAL STATUS
The randomized trial started in October 2017 and is ongoing. The trial is currently in the phase of participant enrollment, facilitator training, and second year data collection. Data collection will continue until June 2020.
7. DISCUSSION
This trial utilizes a novel protocol that incorporates a CBPR approach to childhood obesity prevention in order to address both theory and implementation failure. A major strength of CHL is its grounding in the Family Ecological Model and Empowerment Theory. While health knowledge is necessary to change health behaviors, it is seldom sufficient - particularly for low-income families who face substantial challenges to wellbeing such as food insecurity and housing insecurity. At the parent level, CHL aims to ensure that families not only have essential knowledge about child health, but also the skills and resources needed to overcome common barriers families face across multiple facets of their lives beyond nutrition and physical activity. At the organizational level, CHL aims to improve Head Start resources and enhance staff capacity to provide effective health and nutrition support to families.
Another major strength of CHL is its employment of implementation science principles to maximize effectiveness, sustainability, and potential for scale-up and dissemination. For example, CHL was designed to align with Head Start performance standards and be implemented by Head Start parents and staff, facilitating integration into services already used by families with children at high risk for obesity. Additionally, intervention components have been fully detailed in manuals and toolkits to facilitate the sustainability of CHL and enhance its potential for national dissemination. For instance, all aspects of PConnect are laid out in facilitator and parent manuals, allowing new parent and staff facilitators to effectively run the program, whether they join during the trial or they join during scale-up efforts after the trial. Last, by utilizing and improving on existing data collection processes within Head Start, CHL evaluation presents less participant burden compared to working in other settings and reduces selection bias inherent in active recruitment methods.
The stepped-wedge design of the CHL trial presents both opportunities and challenges. This trial design, compared to a classic cluster-randomized trial, aligns with the CBPR principle of mutual benefit for all partners because it allows all Head Start programs to receive the intervention during the trial. Additionally, it presents an opportunity to study both implementation and outcomes across a broader range of communities than would be observed in a classic design, which can provide insights that optimize sustainability and scale-up efforts. However, in a stepped wedge design, there are fewer clusters that experience the intervention for the full duration of the trial, potentially reducing power to observe effects of the intervention that require a longer period of time to occur. In the case of CHL, the randomization procedure resulted in six programs, including one of the largest programs, being randomly assigned to the third group, which will only receive the intervention for one year, starting the last year of the trial. Another potential drawback is the risk of contamination and attrition of participants from a cluster that is randomized to receive the intervention at one of the later steps. We have minimized the threat of contamination by maintaining ongoing communication with Head Start partners and by designing the randomization to minimize the degree to which staff need to serve an intervention and non-intervention center simultaneously. The threat of differential dropout from clusters randomized to a later intervention period is small, as registering with a different Head Start program generally requires moving to a new catchment area.
Despite the mixed results of previous childhood obesity prevention interventions, we are optimistic that the careful attention to both theory and implementation in CHL can produce positive results in child weight and weight-related behaviors, as well as parenting practices and empowerment. If successful, CHL is in a strong position for sustained implementation in the greater Boston area and scale-up to Head Start programs nationwide.
Acknowledgements
The authors would like to acknowledge the Head Start staff and parents involved in this intervention, especially those who served on the Community Advisory Board and worked as partners alongside the research team in developing this intervention.
In addition to the authors listed, the CHL study team includes Christopher Hosman, Matthew Kardonsky, Sonia Carter, Timothy Chambers, Alen Agaranov, Erica Gabriel-Tukianien, Benjamin Hong, Michelle Woodford, Breanne Wilhite, Max Blumenthal, Xinting Yu, and Yu-Tien Hsu.
Funding Sources: This work was supported by the National Institutes of Health (grant number R01DK108200). Jacob Beckerman was supported by the National Institutes of Health (grant number T32DK0077). Roger Figueroa was supported by the National Institutes of Health (grant number T32DK007703). No funding agency was involved in the study design, writing of the report, or decision to submit the article for publication.
Abbreviations
- CHL
Communities for Healthy Living
- CBPR
Community-Based Participatory Research
- ABCD
Action for Boston Community Development
- CAAS
Community Action Agency of Somerville
- CAB
Community Advisory Board
- PConnect
Parents Connect for Healthy Living
- BMIz
Body Mass Index z-score
- NPA
Nutrition and Physical Activity Assessment
- POS
Parent Outcomes Survey
Appendix A. Sample Health and Growth Letter
Appendix B. Sample Procedural Checklist for Nutrition Counseling
Footnotes
Competing interests: No authors have any competing interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Daniels SR. The consequences of childhood overweight and obesity. Futur Child 2006;16:47–67. [DOI] [PubMed] [Google Scholar]
- [2].Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity Among Adults and Youth: United States, 2015–2016. NCHS Data Brief 2017:1–8. [PubMed] [Google Scholar]
- [3].Glickman D, Parker L, Sim LJ, Del H, Cook V, Ann E, et al. Accelerating Progress in Obesity Prevention. 2012. doi: 10.17226/13275. [DOI] [PubMed] [Google Scholar]
- [4].Monasta L, Batty GD, Cattaneo A, Lutje V, Ronfani L, Van Lenthe FJ, et al. Early-life determinants of overweight and obesity: a review of systematic reviews. Obes Rev 2010;11:695–708. doi: 10.1111/j.1467-789X.2010.00735.x. [DOI] [PubMed] [Google Scholar]
- [5].Birch LL, Davison KK. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr Clin North Am 2001;48:893–907. [DOI] [PubMed] [Google Scholar]
- [6].Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act 2008;5:15. doi: 10.1186/1479-5868-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Lindsay AC, Sussner KM, Kim J, Gortmaker S. The role of parents in preventing childhood obesity. Futur Child 2006;16:169–86. [DOI] [PubMed] [Google Scholar]
- [8].Yavuz HM, van Ijzendoorn MH, Mesman J, van der Veek S. Interventions aimed at reducing obesity in early childhood: a meta-analysis of programs that involve parents. J Child Psychol Psychiatry 2015;56:677–92. doi: 10.1111/jcpp.12330. [DOI] [PubMed] [Google Scholar]
- [9].Weiss C Theory-based evaluation: past, present, and future. New Dir Eval 1997:41–55. doi: 10.1002/ev.1086. [DOI] [Google Scholar]
- [10].Skelton JA, Buehler C, Irby MB, Grzywacz JG. Where are family theories in family-based obesity treatment?: conceptualizing the study of families in pediatric weight management. Int J Obes (Lond) 2012;36:891–900. doi: 10.1038/ijo.2012.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Davison KK, Jurkowski JM, Lawson HA. Reframing family-centred obesity prevention using the Family Ecological Model. Public Health Nutr 2013;16:1861–9. doi: 10.1017/S1368980012004533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Griffith DM, Allen JO, DeLoney EH, Robinson K, Lewis EY, Campbell B, et al. Community-Based Organizational Capacity Building as a Strategy to Reduce Racial Health Disparities. J Prim Prev 2010;31:31–9. doi: 10.1007/s10935-010-0202-z. [DOI] [PubMed] [Google Scholar]
- [13].Peterson NA, Zimmerman MA. Beyond the Individual: Toward a Nomological Network of Organizational Empowerment. Am J Community Psychol 2004;34. [DOI] [PubMed] [Google Scholar]
- [14].Griffith DM, Allen JO, Zimmerman MA, Morrel-Samuels S, Reischl TM, Cohen SE, et al. Organizational Empowerment in Community Mobilization to Address Youth Violence. Am J Prev Med 2008;34:S89–99. doi: 10.1016/j.amepre.2007.12.015. [DOI] [PubMed] [Google Scholar]
- [15].Christens BD. Toward Relational Empowerment. Am J Community Psychol 2012:114–28. doi: 10.1007/s10464-011-9483-5. [DOI] [PubMed] [Google Scholar]
- [16].Israel BA, Checkoway B, Schulz A, Zimmerman M. Health education and community empowerment: conceptualizing and measuring perceptions of individual, organizational, and community control. Health Educ Q 1994:149–70. doi: 10.1177/109019819402100203. [DOI] [PubMed] [Google Scholar]
- [17].Holkup PA, Tripp-Reimer T, Salois EM, Weinert C. Community-based participatory research: an approach to intervention research with a Native American community. ANS Adv Nurs Sci n.d.;27:162–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Viswanathan M, Ammerman A, Eng E, Garlehner G, Lohr K, Griffith D, et al. Community-Based Participatory Research: Assessing the Evidence: Summary. Rockville: Agency for Healthcare Research and Quality; 2004. [PMC free article] [PubMed] [Google Scholar]
- [19].Wallerstein N, Duran B. Community-Based Participatory Research Contributions to Intervention Research: The Intersection of Science and Practice to Improve Health Equity. Am J Public Health 2010;100:S40–6. doi: 10.2105/AJPH.2009.184036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Glasgow RE, Magid DJ, Beck A, Ritzwoller D, Estabrooks PA. Practical clinical trials for translating research to practice: design and measurement recommendations. Med Care 2005;43:551–7. [DOI] [PubMed] [Google Scholar]
- [21].Glasgow RE, Davidson KW, Dobkin PL, Ockene J, Spring B. Practical behavioral trials to advance evidence-based behavioral medicine. Ann Behav Med 2006;31:5–13. doi: 10.1207/s15324796abm3101_3. [DOI] [PubMed] [Google Scholar]
- [22].Glasgow RE, Emmons KM. How Can We Increase Translation of Research into Practice? Types of Evidence Needed. Annu Rev Public Health 2007;28:413–33. doi: 10.1146/annurev.publhealth.28.021406.144145. [DOI] [PubMed] [Google Scholar]
- [23].Davison KK, Jurkowski JM, Li K, Kranz S, Lawson HA. A childhood obesity intervention developed by families for families: results from a pilot study. Int J Behav Nutr Phys Act 2013;10. doi: 10.1186/1479-5868-10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].GreenMills LL, Davison KK, Gordon KE, Li K, Jurkowski JM. Evaluation of a Childhood Obesity Awareness Campaign Targeting Head Start Families: Designed by Parents for Parents. J Health Care Poor Underserved 2013;24:25–33. doi: 10.1353/hpu.2013.0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Jurkowski JM, Lawson HA, Green Mills LL, Wilner PG, Davison KK. The Empowerment of Low-Income Parents Engaged in a Childhood Obesity Intervention. Fam Community Heal 2014;37:104–18. doi: 10.1097/FCH.0000000000000024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Deming D Early childhood intervention and life-cycle skill development: Evidence from Head Start. Am Econ J Appl Econ 2009;1:111–34. [Google Scholar]
- [27].Office of Head Start, Office of the Administration for Children and Families. History of Head Start 2018. https://www.acf.hhs.gov/ohs/about/history-of-head-start (accessed September 11, 2018).
- [28].Hemming K, Haines TP, Chilton PJ, Girling AJ, Lilford RJ. The stepped wedge cluster randomised trial: rationale, design, analysis, and reporting. BMJ 2015;350:h391–h391. doi: 10.1136/bmj.h391. [DOI] [PubMed] [Google Scholar]
- [29].Hussey MA, Hughes JP. Design and analysis of stepped wedge cluster randomized trials. Contemp Clin Trials 2007;28:182–91. doi: 10.1016/j.cct.2006.05.007. [DOI] [PubMed] [Google Scholar]
- [30].Israel BA, Schulz AJ, Parker EA, Becker AB. Review of Community-Based Research: Assessing Partnership Approaches to Improve Public Health. Annu Rev Public Heal 1998;19:173–202. [DOI] [PubMed] [Google Scholar]
- [31].Jurkowski JM, Green Mills LL, Lawson HA, Bovenzi MC, Quartimon R, Davison KK. Engaging low-income parents in childhood obesity prevention from start to finish: A case study. J Community Health 2013;38:1–11. doi: 10.1007/s10900-012-9573-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Newman SD, Andrews JO, Magwood GS, Jenkins C, Cox MJ, Williamson DC. Community advisory boards in community-based participatory research: a synthesis of best processes. Prev Chronic Dis 2011;8: A70. [PMC free article] [PubMed] [Google Scholar]
- [33].Alberga AS, Russell-Mayhew S, von Ranson KM, McLaren L. Weight bias: a call to action. J Eat Disord 2016;4:34. doi: 10.1186/s40337-016-0112-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Chaparro MP, Langellier BA, Kim LP, Whaley SE. Predictors of accurate maternal perception of their preschool child’s weight status among Hispanic WIC participants. Obesity (Silver Spring) 2011;19:2026–30. doi: 10.1038/oby.2011.105. [DOI] [PubMed] [Google Scholar]
- [35].Gomes AI, Barros L, Pereira AI. Predictors of parental concerns about child weight in parents of healthy-weight and overweight 2–6 year olds. Appetite 2017;108:491–7. doi: 10.1016/j.appet.2016.11.008. [DOI] [PubMed] [Google Scholar]
- [36].Blum RE, Wei EK, Rockett HR, Langeliers JD, Leppert J, Gardner JD, et al. Validation of a food frequency questionnaire in Native American and Caucasian children 1 to 5 years of age. Matern Child Health J 1999;3:167–72. doi: 10.1023/A:1022350023163. [DOI] [PubMed] [Google Scholar]
- [37].Hoelscher DM, Day RS, Lee ES, Frankowski RF, Kelder SH, Ward JL, et al. Measuring the prevalence of overweight in Texas schoolchildren. Am J Public Health 2004;94:1002–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Burdette HL, Whitaker RC. Neighborhood playgrounds, fast food restaurants, and crime: relationships to overweight in low-income preschool children. Prev Med (Baltim) 2004;38:57–63. [DOI] [PubMed] [Google Scholar]
- [39].Sadeh A A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics 2004;113:e570–7. doi: 10.1542/PEDS.113.6.E570. [DOI] [PubMed] [Google Scholar]
- [40].Musher-Eizenman D, Holub S. Comprehensive Feeding Practices Questionnaire: Validation of a New Measure of Parental Feeding Practices. J Pediatr Psychol 2007;32:960–72. doi: 10.1093/jpepsy/jsm037. [DOI] [PubMed] [Google Scholar]
- [41].Davison KK, Li K, Baskin ML, Cox T, Affuso O. Measuring parental support for children’s physical activity in white and African American parents: The Activity Support Scale for Multiple Groups (ACTS-MG). Prev Med (Baltim) 2011;52:39–43. doi: 10.1016/j.ypmed.2010.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].National Cancer Institute Division of Cancer Control and Population Sciences. National Health and Nutrition Evaluation Survey (NHANES) Dietary Screener Questionnaire 2018. https://epi.grants.cancer.gov/nhanes/dietscreen/questionnaires.html.
- [43].Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) physical activity and physical fitness survey 2015. https://wwwn.cdc.gov/nchs/data/nhanes/2015-2016/questionnaires/PAQ_I.pdf.
- [44].Spreitzer GM. Psychological empowerment in the workplace: Dimensions, measurement, and validation. Acad Manag J 1995;38:1442–65. [Google Scholar]
- [45].Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000. CDC Growth Charts for the United States: methods and development. Vital Health Stat 11 2002:1–190. [PubMed] [Google Scholar]
- [46].Lohman TG, Roche AF. Anthropometric standardization reference manual. Champaign: Human kinetics books; 1988. [Google Scholar]
- [47].Pérez D, Van Der Stuyft P, Del M, Zabala C, Castro M, Lefèvre P. A modified theoretical framework to assess implementation fidelity of adaptive public health interventions. Implement Sci 2016;11. doi: 10.1186/s13012-016-0457-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].McCulloch C, Searle S, Neuhaus J. McCulloch C, Searle S, Neuhaus J. 2nd ed. Hoboken: John Wiley & Sons, Inc; 2008. [Google Scholar]
- [49].Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol 1986;51:1173–82. [DOI] [PubMed] [Google Scholar]
- [50].Little R, Rubin D. Statistical Analysis with Missing Data. 2nd ed. Hoboken: John Wiley & Sons, Inc; 2002. [Google Scholar]
- [51].Ibrahim JG, Molenberghs G. Missing data methods in longitudinal studies: a review. Test 2009; 18:1–43. doi: 10.1007/s11749-009-0138-x. [DOI] [PMC free article] [PubMed] [Google Scholar]