Abstract
Ectopic scrotum (ES) is a particularly rare congenital malformation of the scrotum and commonly associated with other congenital malformations. A 2-year-old boy was presented with ectopic scrotum, low lesion imperforate anus, spina bifida and pubic diastasis since birth. There are various surgical methods available to be discussed in the management of ES. We performed correction of the ectopic scrotum and concomitant bilateral orchidopexy in one stage of surgery. This procedure is relatively simpler to perform and gives out favorable cosmetic result.
Keywords: Ectopic scrotum, One stage rotation flap, Scrotoplasty, Orchidopexy
Introduction
Ectopic scrotum (ES) is a particularly rare congenital malformation of the scrotum and commonly associated with other congenital malformations. The ectopic scrotal location is variable, and the testicles may be present or absent in the abnormal scrotum. ES can occur in various locations, starting from the perineum and inguinal canal to the medial thigh, majority of which are usually found in the inguinal, suprainguinal, infrainguinal, or perineal area. A defect in the gubernaculum formation during the conception period is hypothesized to be strongly associated with the development of ES.1
Case presentation
A 2-year-old boy was presented with ectopic scrotum, anal atresia, spina bifida and pubic diastasis since birth. The child underwent posterior sagittal anorectoplasty in June 2016, followed by spina bifida closure in February 2017. Upon clinical examination, right hemiscrotum was normal in size and location with normal testicle located in the high scrotal position. The left hemiscrotum was present in the left inguinal region, with the left testicle located below the superficial inguinal ring. Scrotal raphe and the phallus developed normally. The sizes of both testicles were approximately 30 × 20 mm. Pelvic X-ray revealed pubic diatheses which were decided in a conference with pediatric orthopedics to be left alone due to the risk of surgery outweighing the benefits. We performed correction of the ectopic scrotum and bilateral orchidopexy in one stage of surgery.
An inguinal incision was first performed on the left side to mobilize the funiculus until the left testis was able to be moved down to the anatomical position of the scrotum. This was followed by correction of the ectopic scrotum that was initiated with a Y incision that extends from the right hemiscrotum until it reached the ectopic scrotal sac (Fig. 1). An inguinal rotational scrotal skin flap was used to relocate the scrotal sac (Fig. 2). The median raphe and two hemiscrotum sacs were constructed inferiorly to the penis, where the scrotal sac should have formed. Bilateral orchidopexy was performed afterwards, started with positioning the left testis in the left hemiscrotum sac with the fixation of tunica vaginalis using Vicryl® 4.0 with anchoring suture in the 6 0′clock direction. The fixation of the right testis to the right hemiscrotal sac was also performed afterwards followed by adequate skin closure.
Fig. 1.
A. Clinical Features; B. Marked Flap Incisions; C. Pelvic X-ray showing Pubic Diastasis.
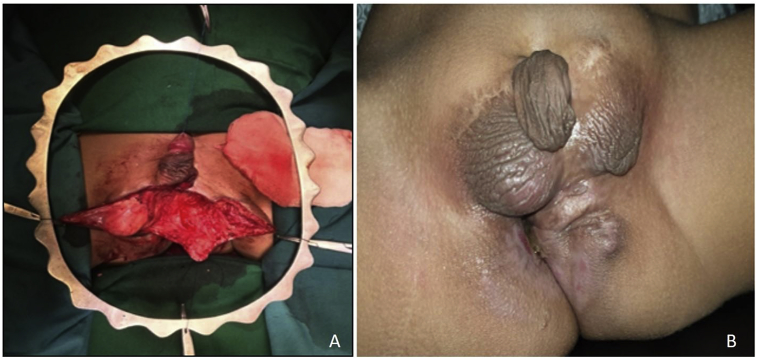
Fig. 2.
A. Marked flap before beginning incision; B. Raised Flaps and 6 months post Op Follow Up.
Discussion
Congenital abnormalities of the scrotum are rare medical conditions which usually include 4 distinct groups of anomalies starting from penoscrotal transposition, bifid scrotum, accessory scrotum and finally ectopic scrotum. The beginning of scrotum development starts at 4 weeks of gestation that was initiated by the formation of labio-scrotal swellings. These labio-scrotal swellings are located laterally to the cloacal membrane and posteriorly to the genital tubercle. In the 12 weeks of gestation, they start to move inferomedially and fuse together, thus forming the scrotum. The descent of testes into the scrotum occurs with the insertion of gubernaculum into the labio-scrotal swellings. Any defects in the formation of gubernaculum can impair or even prevent the migration and fusion of labio-scrotal swellings, therefore resulting in ectopic scrotum and concurrent malposition of the testes. The causes of defective gubenarculum formation can be mechanical, genetic, chromosomal or teratogenic. A mechanical pressure effect on the developing fetus usually occurs in pregnancies complicated by oligohydramnios and breech presentation. These conditions together with disproportionate size of the fetus may lead to an abnormally flexed limb posture. This causes the contralateral heel to directly press on the region of developing scrotum. On the other hand, association of lower spine agenesis with pubic diastasis as in this case, may be attributed to more than just a defect that is caused by direct mechanical compressions. Rather, this may because by a single dysmorphogenic event during the late blastogenesis period.2,3
There are various surgical methods available to be discussed in the management of ES. Daniel et al. shared their experience of performing rotation flap scrotoplasty followed by subsequent orchidopexy in the following 6 months after the first surgery.4 On the other hand, Filho et al. used perineal scrotal skin flaps to prepare the scrotal sac.5 A single staged rotation flap scrotoplasty with immediate orchidopexy formed the basis of reconstructive repair in our patient. This procedure is relatively simpler to perform and gives out favorable cosmetic result. Despite the various reparative techniques available in the literature, there is no definite rule as to which surgical approach is more superior to another. Choosing which procedures to perform depends on the competency as well as the preference of the surgeon.
Conclusion
To conclude, ectopic scrotum is speculated to be caused by defective gubernaculum formation and is very well oriented with other congenital malformations such as anorectal malformation, spina bifida or pubic diastasis as presented in this case. We performed a single stage rotational flap scrotoplasty and bilateral orchidopexy with favorable cosmetic results and adequate testicular descent.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Conflicts of interest
The authors declare that they have no competing interests.
Authors’ contributions
I.W, I.A.D, G.R.S and A.R all performed the review of literature, performed patient care, and were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
The authors would like to thank the staff of Urology of Cipto Mangunkusumo Hospital that took part in the care of these patients.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eucr.2019.100886.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Gardikis S., Kambouri K., Tsalkidis A., Angelidou M., Pitiakoudis M., Vaos G. Inguinal ectopic scrotum in a neonate : case report and literature review. Pediatr Int. 2012;54:575–576. doi: 10.1111/j.1442-200X.2012.03656.x. [DOI] [PubMed] [Google Scholar]
- 2.Bawa M., Garge S., Sekhon V., Rao K. Inguinal ectopic scrotum, anorectal malformation with sacral agenesis and limb defects: an unusual presentation. J Korean Pediatr Surg. 2015;21(2):32. [Google Scholar]
- 3.Hoar R.M., Calvano C.J., Reddy P.P., Bauer S.B., Mandell J. Unilateral suprainguinal ectopic scrotum: the role of the gubernaculum in the formation of an ectopic scrotum. Teratology. 1998;57(2):64–69. doi: 10.1002/(SICI)1096-9926(199802)57:2<64::AID-TERA4>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 4.Daniel G., Coleman R. Staged rotation flap scrotoplasty and orchidopexy in a patient with inguinal ectopic scrotum. J Surg Case Rep. 2015;(10):1–3. doi: 10.1093/jscr/rjv137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sobral Filho D.S.R., da Silva H.D., Damazio E. Surgical correction of ectopic penis and scrotum associated with bilateral orchidopexy. Einstein. 2017;15(2):223–225. doi: 10.1590/S1679-45082017RC3927. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.