Abstract
Bosworth ankle fracture-dislocation is rare, known to be an irreducible type of ankle injury, with a high incidence of complication. We present two cases of even rarer variants of Bosworth ankle fracture-dislocation. The first case is a type of supination external rotation adduction, and the second case is a type of supination external rotation adduction. These types have not been described before. In both of the cases we failed to achieve close reduction, and therefore proceeded with emergency surgeries, with open reduction and internal fixation. Both of the cases were performed with a postero-lateral approach to reduce the dislocations, and fix the fractures successfully. Unfortunately in one of the cases, acute compartment syndrome developed post-surgically. However, both cases showed good functional outcomes.
Keywords: Fracture dislocation, Supination, Rotation, Ankle injuries, Complications
Introduction
Bosworth ankle fracture-dislocation is a rare injury. Most of these cases show supination and external rotation patterns according to the Lauge-Hansen classification, in other words, Danis-Weber C or Maisonneuve pattern.1 Bosworth injury with medial malleolus fracture caused by an adduction force is not well described previously. We report two cases of this variant of Bosworth fracture-dislocation with medial malleolus fracture as an adduction pattern; the first case is a type involving supination external rotation adduction, and the second case pronation external rotation adduction.
Case report
Case 1
A 19-year-old male, twisted his ankle when he fell off a motorbike. He could not remember his foot position when the accident happened. He went to a local hospital where a radiograph was performed and then he was transferred to our emergency department by ambulance. A severe deformity, with the foot fixed in an external rotation position, was noticed. The skin tenting at the lateral edge of the fractured distal tibia was easily palpated. The pulses of the dorsalis pedis artery and the arteria tibialis caudalis could not be detected.
The radiographs showed a trimalleolar fracture with posterior dislocation of the talus. The tibiofibular relationship showed no obvious diastasis in an anteroposterior radiograph view, but the fibula showed posterior translation with a lateral radiograph.
The fracture of the distal fibula had a Danis-Weber B oblique pattern, which matched the Lauge-Hansen supination and external rotation type. However, the fracture of medial malleolus showed an oblique fracture line starting from the superomedial corner of the mortise dome and ending 4 cm above the syndesmosis level, matching a Lauge-Hansen supination adduction type (Fig. 1). An urgent attempt at closed reduction resulted in failure, and then CT was performed. The distal fibula had rotated, sticking out from the tibiofibular notch and trapped behind the posterior aspect of the tibia (Fig. 2).
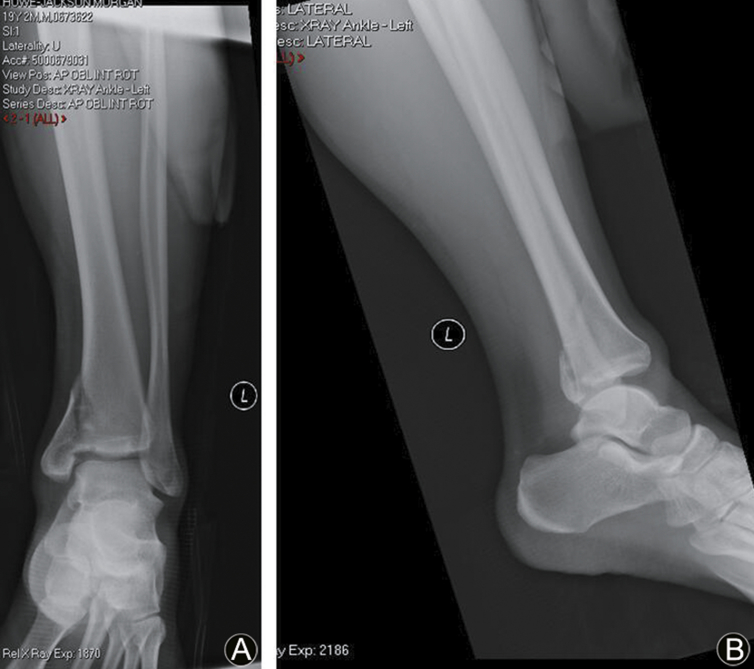
Fig. 1.
(A) Anteroposterior radiograph demonstrating no obvious syndesmosis diastasis. The lateral malleolus fracture was a Lauge-Hansen supination external rotation type, but the medial malleolus fracture was a supination adduction type. (B) Lateral radiograph demonstrating a posterior translation of the fibula.
Fig. 2.
Axial CT image showing distal fibula dislocated out of the tibiofibular notch and trapped behind the posterior aspect of the tibia.
Emergency surgical management with open reduction and internal fixation was performed immediately after CT scan, under general anesthesia. A postero-lateral approach was applied. The distal fibula was put back in the tibiofibula notch using a bone elevator to reduce ankle dislocation. The reduction was confirmed by an intra-operative radiograph. Three screws were used to fix the posterior malleolus fracture. A lateral malleolus plate, a medial malleolus buttress plate, and a syndesmosis screw were used (Fig. 3).
Fig. 3.
(A) Postoperative radiograph showing reduction and fixation of the lateral malleolus fracture, syndesmosis diastasis and medial malleolus fracture. A buttress plate was applied to support the medial malleoli. (B) Reduction and fixation of the posterior malleolus fracture and posterior translation of the fibula.
Unfortunately, compartment syndrome developed the day after surgery. We performed a fasciotomy immediately with secondary wound closure two days afterwards. Post-operative short-leg cast immobilization was applied for two weeks, changed to an airboot for touch-weight-bearing and then regular physiotherapy started. The syndesmosis screw was removed after eight weeks post-surgery. Follow-up after two years showed full functional recovery of the ankle. The patient had no subjective complaints.
Case 2
A 19-year-old male sprained his left ankle when playing Rugby. He was running and jumped to his left side, landing awkwardly on his left foot. When he was brought to hospital, physical examination showed a severe external rotation deformity. The skin was tenting at the lateral edge of the fractured distal tibia. There was no tenderness at the proximal fibula. The pulse of the dorsalis pedis artery could be detected but that of the arteria tibialis caudalis pulses could not.
Radiographs showed an oblique medial malleolus fracture, but no fibular fracture. The distal tibiofibular relationship showed increased overlap in an anteroposterior view, and the distal fibula moved posteriorly in a lateral view. Immediate trial of close reduction was not successful under sedation. The fracture of the medial malleolus showed an oblique fracture line starting from the superomedial corner of the mortise dome, ending at 4 cm above the syndesmosis level, indicating that an adduction force was imposed on the medial malleolus (Fig. 4). A CT scan showed the distal fibula had rotated out of the tibia fibula notch, and was entrapped at the postero-lateral position of tibial tuberosity (Fig. 5).
Fig. 4.
(A) AP radiograph showing a distal tibiofibular joint excessive overlap and a vertical shear fracture of the medial malleolus; (B) Lateral radiograph demonstrating a posterior translation of the fibula.
Fig. 5.
Axial CT image showing distal fibula dislocated out of the tibiofibular notch and trapped behind the posterior aspect of the tibia.
The patient was immediately taken open reduction and internal fixation. The postero-lateral approach was applied, and the distal fibula was put back in the tibiofibular notch, and the ankle dislocation was reduced. A buttress plate was applied in order to fix the posterior malleolus, another buttress plate was used to fix the medial malleolus, and a syndesmosis screw was applied to fix the syndesmosis diastasis (Fig. 6).
Fig. 6.
(A) Postoperative radiographs showing reduction and fixation of the syndesmosis excessive overlap and medial malleolus fracture. A buttress plate was applied to support the medial malleolus. (B) Reduction and fixation of the posterior malleolus fracture and posterior translation of the fibula.
Post-operative short-leg cast immobilization was applied for two weeks, changed to an airboot for touch-weight-bearing and then regular physiotherapy started. The syndesmosis screw was removed after eight weeks post-surgery. At follow-up after 18 months, the patient showed full functional recovery with a pain-free, normal range of motion in his ankle joint.
Discussion
It has been reported that Bosworth fracture dislocation can be divided into three types. The first is the distal fibula dislocation, associated with epiphysis fracture of distal tibia. This type of lesion occurs in children and adolescents. The second is the distal fibula dislocation without fibula fracture, similar to the Maisonneuve lesion, in young adults. The third is the fibula dislocation with fibula fracture, including Danis-Weber B and C fibular fractures. This type happens in older adults.1, 2, 3, 4
The general mechanism of Bosworth fracture dislocation is due to the force of an extreme external rotation, in which the talus external rotates in the ankle mortise and pushes the lateral malleolus out of the fibular notch externally and posteriorly and is trapped in behind the posterior tibia tubercle. Meanwhile, the dislocated distal fibula exerts an external rotation force pushing the fractured posterior malleolus and making the medial malleolus rotate externally.
Perry et al.2 reported the Bosworth injury mechanism through cadaver experiment, and showed that there are five steps when Bosworth fracture dislocation occurs. The first step is rupture of the anteromedial part of the capsule. The second step is rupture of the interosseous membrane at a point of 4–6cm above the ankle mortise level. The third step is fracture of the fibular, pushed by the lateral rotation of the talus and pulled by the intact lateral collateral ligament of the ankle. In the meantime, the distal fibula moves out of the tibiofibular notch and becomes entrapped behind the tibia. The fourth step is that the talus, continuing to rotate, causes a distal fibula fracture according to the Lauge-Hansen supination external rotation pattern. Finally, the fifth step is fracture of the medial malleolus or rupture of the deltoid ligament rupture. Bartonicek et al.5 reported that 88% of Bosworth fracture dislocations had a Weber type B fracture pattern. However, there are plenty of different forces working in combination to produce different types of Bosworth fracture dislocation, with or without distal fibular fractures.
We think that Bosworth lesions of supination external rotation happen according to the same mechanism as Lauge-Hansen supination external rotation ankle fractures. In the Lauge-Hansen classification, the talus rotates externally in the ankle mortise in a supinated foot position. The injuries are divided into four grades. Grade I is the anterior-inferior tibiofibular ligament (AITFL) tear. Grade II is a typical Danis-Weber B lateral malleolus fracture with the distal fibula rotating postero-laterally to the tibia tuberosity. In Grade III, the distal fibula pushes the posterior malleolus producing a posterior malleolus fracture. The fracture segments rotate externally to the posterior of the medial malleolus. In Grade IV, the external rotation force is imposed on the deltoid ligament producing a deltoid ligament rupture or a transverse medial malleolus fracture at the ankle dome level.
We also think that Bosworth lesions of pronation external rotation have a similar mechanism to Lauge-Hansen pronation external rotation ankle fractures. In Lauge-Hansen pronation external rotation fractures, Danis-Weber C fractures can be located in the middle 1/3 of the fibula or the proximal fibula. In Grade I, the deltoid ligament ruptures or the medial malleolus breaks in the transverse fracture at the ankle mortise dome level. Grade II is the anterior inferior tibiofibular ligament rupture. Grade III is the fibula rotating postero-laterally, with or without fibular fractures, depending on the patient's age and bone quality. Grade IV involves the external rotation force of the distal fibula producing posterior malleolus fracture or distal inferior posterior tibio-fibular ligament rupture. The distal fibula is trapped behind the posterior tibia tubercle.
Interestingly, the two cases we report here do not fit in all the types above. Both of the cases showed adduction mechanism which provided a shearing force leading to an oblique fracture of the medial malleolus. Case 1 was similar to Lauge-Hansen supination-external rotation type IV, except that it had an oblique fracture of the medial malleolus. This only can be explained as supination, external rotation, and adduction. Case 2 appeared to be like a Maisonneuve lesion, however, the last stage of this injury should be an adduction force. Therefore, we think our two Bosworth dislocation-fractures involve complicated forces of pronation, external rotation, and adduction.
In terms of the management of Bosworth dislocation-fractures, all trauma and orthopedic surgeons should be aware the irreducible nature of this injury. Some literature suggests that close reduction can be achieved if you pay attention to the mechanism of the injury. Bartonicek et al.5 reported that the reduction could be achieved by pulling, and gradual internally rotating the foot. On the other hand, far more clinical reports give warning of the difficulty of close reduction. In Bosworth fracture-dislocation injuries, the distal fibula rotates and is entrapped behind the posterior tibia tuberosity. The intact interosseous membrane acts as a pulling force, which makes the dislocation quite rigid, leading to close reduction difficulty.4, 6, 7, 8 In both of our cases, close reduction failed even when we tried under sedation. When we see a severe deformity of the ankle fracture-dislocation, we need to do a CT scan, looking for Bosworth type irreducibility, and this prompts surgical management.
Bosworth fracture-dislocations have a high incidence of complications, such as compartment syndrome, avascular necrosis of talus, ankle osteoarthritis, and skin necrosis. Of these, compartment syndrome is the most common complication.5, 9 In our report, we also experienced compartment syndrome (case 1) requiring emergency fasciotomy. Although this had a very good outcome, we need a proactive management plan. Avascular necrosis of the talus is the second most common and severe complication. Delayed reduction may be one of the most important reasons, but severe injury itself may damage vascularization of the talus.4, 9, 10 Some literature warns that special features of Bosworth fracture-dislocation can still be easily missed. This may lead to delayed treatment. We believe delayed treatment will lead to a poor outcome. Lui et al.7 reported three patients with Bosworth fracture-dislocation injury who developed post-traumatic stiffness of the injured ankle. They believe that it may be due to a delay in the reduction of the dislocated ankle joint. In his report, all these cases involved second surgery to release the capsule in order to improve ankle range of motion.
Lastly, we would like to mention our surgical approach. It is reported that a conventional lateral approach is difficult for accessing the fibula in an altered position.1 In order to reduce fibular dislocation and fix the posterior malleolus, we recommend a postero-lateral approach. The postero-lateral approach will also allow us a better means of exposing the posterior malleolus fracture and distal fibula, and make it easier to reduce and fix the fracture-dislocation.
In conclusion, Bosworth fracture-dislocation is not common, and our two cases in this report showed even rarer variants of this injury. Basically we emphasize that for Bosworth fracture-dislocation it is usually not possible to achieve a close reduction, and immediate emergency open reduction and internal fixation is necessary. Awareness of this injury will help reduce the incidence of complications, such as compartment syndrome, skin necrosis, talus necrosis and function loss. Compartment syndrome rate is high even if the injury is treated urgently, and preparation of the fasciotomy will be needed. Lastly, the postero-lateral approach is an effective method of achieving full access to treat difficult Bosworth fracture-dislocations.
Funding
None.
Ethical statement
This study has been approved by the local committee and informed consent has been obtained from all patients or relatives.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Cappuccio M., Leonetti D., Di Matteo B. An uncommon case of irreducible ankle fracture-dislocation: the "Bosworth-like" tibio-fibular fracture. Foot Ankle Surg. 2017;23:e1–e4. doi: 10.1016/j.fas.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 2.Perry C.R., Rice S., Rao A. Posterior fracture-dislocation of the distal part of the fibula. Mechanism and staging of injury. J Bone Joint Surg Am. 1983;65:1149–1157. [PubMed] [Google Scholar]
- 3.Peterson N.D., Shah F., Narayan B. An unusual ankle injury: the Bosworth-Pilon fracture. J Foot Ankle Surg. 2015;54:751–753. doi: 10.1053/j.jfas.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 4.Schepers T., Hagenaars T., Den Hartog D. An irreducible ankle fracture dislocation: the Bosworth injury. J Foot Ankle Surg. 2012;51:501–503. doi: 10.1053/j.jfas.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 5.Bartonicek J., Fric V., Svatos F. Bosworth-type fibular entrapment injuries of the ankle: the Bosworth lesion. A report of 6 cases and literature review. J Orthop Trauma. 2007;21:710–717. doi: 10.1097/BOT.0b013e31815affb7. [DOI] [PubMed] [Google Scholar]
- 6.Ellanti P., Hammad Y., Grieve P.P. Acutely irreducible ankle fracture dislocation: a report of a Bosworth fracture and its management. J Emerg Med. 2013;44:e349–e352. doi: 10.1016/j.jemermed.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 7.Lui T.H., Chan K.B., Kong C.C. Ankle stiffness after Bosworth fracture dislocation of the ankle. Arch Orthop Trauma Surg. 2008;128:49–53. doi: 10.1007/s00402-007-0352-5. [DOI] [PubMed] [Google Scholar]
- 8.Molinari M., Bertoldi L., De March L. Fracture dislocation of the ankle with the fibula trapped behind the tibia. A case report. Acta Orthop Scand. 1990;61:471–472. doi: 10.3109/17453679008993567. [DOI] [PubMed] [Google Scholar]
- 9.Beekman R., Watson J.T. Bosworth fracture-dislocation and resultant compartment syndrome. A case report. J Bone Joint Surg Am. 2003;85:2211–2214. doi: 10.2106/00004623-200311000-00025. [DOI] [PubMed] [Google Scholar]
- 10.Hockenbury R.T., Friermood T.G. Dislocation of the distal tibiofibular joint. J Orthop Trauma. 1992;6:120–124. [PubMed] [Google Scholar]