This cross-sectional study analyzes the rates of fentanyl positivity in urine drug test results that were positive for cocaine or methamphetamine.
Key Points
Question
Among urine drug test results positive for cocaine or methamphetamine, how has the prevalence of positive results for nonprescribed fentanyl changed through time?
Findings
In this cross-sectional study of 1 million urine drug test results from January 2013 through September 2018, positivity rates for nonprescribed fentanyl in the cocaine-positive group increased significantly. Positivity rates for nonprescribed fentanyl in the methamphetamine-positive group also increased significantly, from 0.9% to 7.9%, a 798% increase.
Meaning
The concomitant use of fentanyl with a stimulant poses a significant risk to public health because of heightened risk of overdose.
Abstract
Importance
Drug overdose deaths continue to increase, despite the leveling off of prescription opioid use and policy changes limiting opioid prescribing. Illicit fentanyl is the leading cause of drug overdose death, and it is important to characterize the emerging combination of other illicit drugs with fentanyl, which increases the risk of overdose.
Objective
To determine whether rates of the combination of nonprescribed fentanyl with cocaine or methamphetamine have changed in urine drug test (UDT) results through time.
Design, Setting, and Participants
This cross-sectional study of UDT results from January 1, 2013, through September 30, 2018, included patient specimens submitted for UDTs by health care professionals as part of routine care. Patients were selected from health care practices across the United States, including substance use disorder treatment centers, pain management practices, primary care practices, behavioral health practices, obstetrics and gynecology practices, and multispecialty groups. The UDT analysis used liquid chromatography–tandem mass spectrometry to detect benzoylecgonine (cocaine metabolite), methamphetamine, fentanyl, and norfentanyl. Specimens from individuals reported to have been prescribed fentanyl were excluded. A convenience sample approach was used to randomly select 1 million unique patient UDT specimens from Millennium Health’s UDT database for further analysis. Each specimen had associated cocaine, methamphetamine, and fentanyl UDT results.
Exposures
Medically necessary UDT to detect benzoylecgonine (cocaine metabolite), methamphetamine, fentanyl, and norfentanyl, ordered by a health care professional as part of routine patient care.
Main Outcomes and Measures
Rates of nonprescribed fentanyl positivity among cocaine- or methamphetamine-positive UDT results, quantified through time.
Results
In a sampling of 1 million unique patients’ UDT specimens analyzed for cocaine and fentanyl (median [interquartile range] age, 44 [19-69] years; 55.0% women), positivity rates for nonprescribed fentanyl among the cocaine-positive results increased significantly, from 0.9% (n = 84) (95% CI, 0.7%-1.1%) in 2013 to 17.6% (n = 427) (95% CI, 16.1%-19.1%) in 2018, a 1850% increase (τ = 0.78; z = 9.45; P < .001). In the same sampling of 1 million specimens, positivity rates for nonprescribed fentanyl among the methamphetamine-positive results also increased significantly, from 0.9% (n = 29) (95% CI, 0.6%-1.2%) in 2013 to 7.9% (n = 344) (95% CI, 7.1%-8.7%) in 2018, a 798% increase (τ = 0.72; z = 8.75; P < .001).
Conclusions and Relevance
An increasing number of UDT results positive for cocaine or methamphetamine were also positive for nonprescribed fentanyl. This provides additional insight into recently reported increases in cocaine- and methamphetamine-related overdoses. Stimulant users who may be opioid naive are at a heightened risk of overdose when exposed to fentanyl. Clinicians need to be aware that patients presenting for treatment of suspected drug overdose or substance use disorder may have been exposed, knowingly or unknowingly, to multiple substances, including the combination of stimulants and opioids.
Introduction
Drug overdose deaths continue to increase, despite the leveling off of prescription opioid use and policy changes limiting opioid prescribing. A research letter by Jones et al1 in 2018 highlighted the major role of synthetic opioids (primarily illicit fentanyl) in increasing drug overdose deaths from 2010 to 2016, most of which also involved another drug or alcohol. Data as recent as 20172 suggest a continued expansion of the fentanyl overdose epidemic, along with emerging concerns about the combination of fentanyl with stimulants, such as cocaine and methamphetamine.
More than 70 000 individuals in the United States died from drug overdoses in 2017.2 Fentanyl-related and fentanyl analog–related deaths continue to be the leading contributors; however, a sharp increase has also been noted for cocaine.2 According to the Centers for Disease Control and Prevention,2 the number of overdose deaths involving cocaine is now similar to the number of deaths involving heroin and prescription-type opioids, such as hydrocodone and oxycodone. Deaths associated with methamphetamine have also increased, along with increasing reports of methamphetamine confiscations by law enforcement.2,3 The number of cocaine-related overdose deaths in 2017 was roughly 2-fold the previously observed peak in 2006, while methamphetamine-related deaths have increased nearly 5-fold since 2010.2 Of note, deaths involving more than 1 type of drug are included in rates for each drug category.4 There are numerous sources linking fentanyl contamination to these stimulant overdoses.5,6 For example, a US Drug Enforcement Administration bulletin issued in February 20186 warned of an illicit drug confiscation purported to be only cocaine but also containing fentanyl. A 2019 commentary7 on the opioid epidemic states that people who use illicit drugs can no longer be certain of drug makeup because of possible adulteration with other substances, such as fentanyl, other opioids, and even stimulants. Using data from January 1, 2013, to September 30, 2018, our analysis builds on previous research to describe trends in the combination of fentanyl with cocaine and methamphetamine.
Methods
We conducted a cross-sectional study of urine drug test (UDT) results from January 1, 2013, to September 30, 2018, of patient specimens submitted for testing by health care professionals as part of routine care. Specimens were collected from health care practices across the United States. The analysis used a convenience sample of tests ordered for definitive drug testing by liquid chromatography–tandem mass spectrometry for cocaine, methamphetamine, and fentanyl. Each test was individually ordered by the health care professional based on medical necessity. The liquid chromatography–tandem mass spectrometry testing method is a laboratory-developed test with performance characteristics determined by Millennium Health, San Diego, California, which is certified by the Clinical Laboratory Improvement Amendments and accredited by the College of American Pathologists for high-complexity testing. Analyte concentrations at or greater than fentanyl, 2 ng/mL; norfentanyl (fentanyl metabolite), 8 ng/mL; benzoylecgonine (cocaine metabolite), 50 ng/mL; or methamphetamine, 100 ng/mL, were considered positive. Order forms completed by the health care professionals included an option to report the patient’s prescribed medications. Specimens from patients reported to have been prescribed fentanyl were removed from randomization and further analysis. One million unique patient specimens randomly selected from the entire period of the study were included for further analysis. The study protocol was approved by the Aspire Independent Review Board and includes a waiver of consent for the use of deidentified data. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Fentanyl positivity rates and Clopper-Pearson 95% binomial CIs were calculated among the methamphetamine-positive and cocaine-negative results and among the cocaine-positive and methamphetamine-negative results. Urine drug test results that were positive for both methamphetamine and cocaine were excluded; thus, there was no overlap between groups. Loess smoothing curves were estimated to illustrate the trend in positivity rates through time. A formal trend analysis was performed using a nonparametric Mann-Kendall test on fentanyl positivity rates calculated at 1-month intervals. This test evaluates the possibility of a monotonic upward or downward trend in a variable through time. This is similar to testing for a nonzero slope in ordinary least squares regression but without the assumptions of normality or linearity. P values were 2-tailed, and the significance level was set at .05. R version 3.5.0 (R Foundation for Statistical Computing) was used for data analysis.
Results
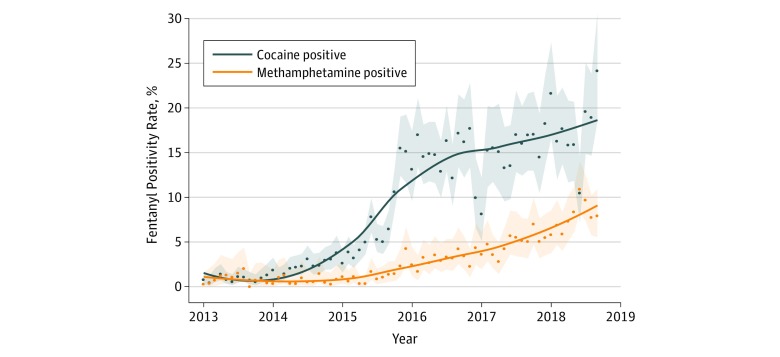
One million UDT results from individual patients, collected during nearly 6 years, were analyzed for combinations of cocaine and fentanyl or methamphetamine and fentanyl (Table 1). The median (interquartile range) age of the population was 44 (19-69) years, and 550 361 patients (55.0%) were women. Patients represented multiple health care specialties, including 199 850 patients (20.0%) treated at substance use disorder treatment centers, 335 368 patients (33.5%) treated by pain management practices, 237 415 patients (23.7%) treated by primary care practices, 106 564 patients (10.7%) treated by behavioral health practices, 57 071 patients (5.7%) treated by obstetrics and gynecology practices, and 63 732 patients (6.4%) treated by multispecialty groups or other practices. Total positivity rates were 4.0% for cocaine, 3.1% for methamphetamine, and 1.4% for fentanyl. Positivity rates for nonprescribed fentanyl in the cocaine-positive and methamphetamine-negative results group increased from 0.9% (n = 84) (95% CI, 0.7%-1.1%) in 2013 to 17.6% (n = 427) (95% CI, 16.1%-19.1%) in 2018, a 1850% increase (τ = 0.78; z = 9.45; P < .001). Positivity rates for nonprescribed fentanyl in the methamphetamine-positive and cocaine-negative results group also increased, from 0.9% (n = 29) (95% CI, 0.6%-1.2%) in 2013 to 7.9% (n = 344) (95% CI, 7.1%-8.7%) in 2018, a 798% increase (τ = 0.72; z = 8.75; P < .001) (Figure). Trend tests demonstrate significant increases in nonprescribed fentanyl positivity in UDT results for both cocaine- and methamphetamine-positive specimens during the period.
Table 1. Characteristics of Urine Specimens Tested for Cocaine, Methamphetamine, and Nonprescribed Fentanyl, January 1, 2013, to September 30, 2018 .
| Characteristic | Specimens Tested, No. (%) |
|---|---|
| Total specimens, No. | 1 000 000 |
| Total patients, No. | 1 000 000 |
| Age, median (IQR), y | 44 (19-69) |
| Men | 447 777 (44.8) |
| Women | 550 361 (55.0) |
| Positive result | |
| Cocaine | 39 576 (4.0) |
| Methamphetamine | 30 578 (3.1) |
| Fentanyl | 13 770 (1.4) |
| Specialty of the referring health care practice | |
| Substance use disorder treatment center | 199 850 (20.0) |
| Pain management | 335 368 (33.5) |
| Primary care physician | 237 415 (23.7) |
| Behavioral health | 106 564 (10.7) |
| Obstetrics and gynecology | 57 071 (5.7) |
| Multispecialty or other | 63 732 (6.4) |
Abbreviation: IQR, interquartile range.
Figure. Nonprescribed Fentanyl Positivity Among Urine Drug Test Results Positive for Cocaine or Methamphetamine.
Dots represent monthly fentanyl positivity values; shaded areas, binomial 95% CIs.
Urine drug test results from patient specimens collected from substance use disorder treatment centers had the highest rate of nonprescribed fentanyl positivity in cocaine (28.8%; 95% CI, 26.1%-31.7%) and second highest rate in methamphetamine (10.4%; 95% CI, 9.1%-11.8%) in a subanalysis of the 2018 data (Table 2). For nonprescribed fentanyl positivity in the cocaine-positive group, UDT results from primary care, behavioral health, pain management, obstetrics and gynecology, and multispecialty practices or other specialties had rates ranging from 5.9% (95% CI, 0.2%-28.7%) in obstetrics and gynecology to 10.2% (95% CI, 7.7%-13.2%) in behavioral health. For nonprescribed fentanyl positivity in the methamphetamine-positive group, UDT results from primary care practices, behavioral health practices, pain management practices, obstetrics and gynecology practices, and multispecialty groups or other specialties had rates ranging from 0% (95% CI, 0%-16.1%) in obstetrics and gynecology to 11.0% (95% CI, 6.9%-16.5%) in multispecialty practices or other specialties.
Table 2. Nonprescribed Fentanyl Positivity Rates in Cocaine- or Methamphetamine-Positive Urine Drug Test Results by Practice Specialty, January 1, 2018, to September 30, 2018.
| Practice Specialty | Cocaine-Positive Results, % (95% CI) | Methamphetamine-Positive Results, % (95% CI) |
|---|---|---|
| Pain management | 6.0 (3.6-9.2) | 4.7 (2.6-8.1) |
| Primary care | 9.5 (7.0-12.6) | 6.8 (5.1-8.9) |
| Substance use disorder treatment | 28.8 (26.1-31.7) | 10.4 (9.1-11.8) |
| Behavioral health | 10.2 (7.7-13.2) | 4.7 (3.5-6.1) |
| Obstetrics and gynecology | 5.9 (0.2-28.7) | 0 (0-16.1) |
| Multispecialty or other | 8.6 (3.2-17.7) | 11.0 (6.9-16.5) |
| Total | 17.6 (16.1-19.1) | 7.9 (7.1-8.7) |
Discussion
An increasing number of UDT results are positive for nonprescribed fentanyl and either cocaine or methamphetamine. This provides additional insight into recently reported increases in cocaine- and methamphetamine-related overdoses.2 The data revealed positive results for fentanyl and either cocaine or methamphetamine across all treatment specialties.
Two factors may be contributing to this phenomenon. Fentanyl may be deliberately or unintentionally (as a contaminant) added to the illicit supply of cocaine or methamphetamine by drug trafficking organizations. Deliberate addition may seek to expose stimulant users to the opioid, potentially creating dependence and desire for reuse.5 Additionally, substance users may seek out these drugs for the “speedball” effects that result from combining a depressant (eg, fentanyl) with a stimulant (eg, cocaine or methamphetamine). The combination increases the risk of overdose, particularly from respiratory depression once the stimulant effects decline.8 Overdose risk is also heightened in stimulant users who may be opioid naive prior to fentanyl exposure; they may be at increased risk of adverse effects because of an absence of opioid tolerance.9
The lack of awareness regarding the potentially deadly combination of fentanyl with cocaine or methamphetamine poses a significant risk to public health because of the heightened risk of overdose.5,7 Additionally, clinicians need to be aware that patients presenting for treatment for suspected drug overdose or substance use disorder may have been exposed, knowingly or unknowingly, to multiple substances, including the combination of stimulants and opioids. This population may also benefit from access to the opioid overdose antidote naloxone. Prevention efforts previously targeted toward opioid users may require expansion to also reach stimulant users who may be at risk for fentanyl exposure.9
Limitations
Our study has some limitations. Data are limited to patient specimens submitted for testing by health care professionals as part of routine care, wherein the test requisition included (but was not limited to) definitive drug testing by liquid chromatography–tandem mass spectrometry for cocaine, methamphetamine, and fentanyl. Individuals included in the analysis may have had an incomplete or inaccurate medication list for prescribed fentanyl reported by the ordering health care professional.
Conclusions
Cocaine- and methamphetamine-related drug overdose deaths are increasing sharply. Data from UDT results suggest this increase may be related to the simultaneous presence of fentanyl, either added directly to the drug supply or used concomitantly. The combination of nonprescribed fentanyl with cocaine or methamphetamine places an individual at increased risk of overdose. Clinicians treating these individuals, and the individuals themselves, should be aware of this risk. Additionally, efforts should be made to educate the public about this risk and about overdose prevention.
References
- 1.Jones CM, Einstein EB, Compton WM. Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010-2016. JAMA. 2018;319(17):-. doi: 10.1001/jama.2018.2844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Institute on Drug Abuse Overdose death rates. https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates. Accessed January 23, 2019.
- 3.US Drug Enforcement Administration, Diversion Control Division National Forensic Laboratory Information System: NFLIS-Drug 2017 Annual Report. Springfield, VA: US Drug Enforcement Administration; 2018. [Google Scholar]
- 4.Drug and opioid-involved overdose deaths: United States, 2013–2017. MMWR Morb Mort Wkly Rep. 2019;67(5152):1419-1427. doi: 10.15585/mmwr.mm675152e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Drug Enforcement Administration Cocaine laced with fentanyl leads to multiple deaths, overdoses [press release]. https://www.dea.gov/press-releases/2018/09/14/cocaine-laced-fentanyl-leads-multiple-deaths-overdoses. Accessed March 13, 2019
- 6.US Drug Enforcement Administration Cocaine/fentanyl combination in Pennsylvania. https://www.dea.gov/sites/default/files/2018-07/BUL-061-18%20Cocaine%20Fentanyl%20Combination%20in%20Pennsylvania%20--%20UNCLASSIFIED.PDF. Accessed March 13, 2019.
- 7.Trecki J. A perspective regarding the current state of the opioid epidemic. JAMA Netw Open. 2019;2(1):e187104. doi: 10.1001/jamanetworkopen.2018.7104 [DOI] [PubMed] [Google Scholar]
- 8.US Drug Enforcement Administration 2017 National Drug Threat Assessment summary. https://www.dea.gov/documents/2017/10/01/2017-national-drug-threat-assessment. Accessed March 13, 2019.
- 9.Nolan ML, Shamasunder S, Colon-Berezin C, Kunins HV, Paone D. Increased presence of fentanyl in cocaine-involved fatal overdoses: implications for prevention. J Urban Health. 2019;96(1):49-54. doi: 10.1007/s11524-018-00343-z [DOI] [PMC free article] [PubMed] [Google Scholar]