ABSTRACT
Background
Critically ill obstetric patients represent a small proportion of intensive care unit (ICU) admissions. Physiological changes of pregnancy along with pregnancy specific diseases may lead to rapid deterioration of the health status of the parturient warranting ICU care. The present study aims to study the clinical profile and outcomes of the obstetric patients requiring ICU care.
Study design and settings
Prospective observational study in the multidisciplinary ICU of a tertiary care teaching hospital conducted for a period of 2 years.
Materials and methods
Demographic details, indication for ICU admission, severity of illness scores, interventions, complications and outcomes of the consecutive obstetric patients transferred to ICU were studied.
Results
Ninety-one patients were admitted (26 per 1000 deliveries) to the ICU. Majority of them were postpartum (84.6%) and unbooked or referred (63.8%). Hypertensive disorders (24.2%) and obstetric hemorrhage (23.1%) were the major cause for admission to ICU. Forty three patients (47.3%) underwent cesarean delivery. Mechanical ventilation (54.9%), blood transfusion (46%), vasopressor therapy (22%) and dialysis (9.9%) were the various interventions provided in the ICU. Patients with sepsis had high mortality accounting for one third of ICU mortality. The ICU mortality rate was 9.9%.
Conclusion
The present study showed a clinical profile and outcomes similar to the current scenario of critically ill obstetric patients nationwide. Further studies with a larger sample size may provide a better insight in this population.
How to cite this article
Sailaja B, Renuka MK, et al. Critically Ill Obstetric Admissions to an Intensive Care Unit: A Prospective Analysis from a Tertiary Care University Hospital in South India. Indian J of Crit Care Med 2019;23(2):78-82.
Keywords: Maternal outcome, Mechanical ventilation, Obstetric critical care, Postpartum, PRES
BACKGROUND
Maternal mortality refers to death due to complications of pregnancy and child birth. It reflects the quality of women's health care of a nation. The global maternal mortality rate (MMR) has declined by 44% over the last 25 years (1990-2015). The magnitude of reduction, however, shows a large discrepancy both within and between countries. The global MMR in 2015 was 216 deaths per 100000 live births. Almost 99% of these deaths occurred in developing countries 1. India recorded a MMR of 130 deaths per 100000 live births during this period2.
Young, healthy pregnant woman either exhibit a rapid worsening of their preexisting comorbidity because of present pregnant status or develop major complications without prior warning signs even leading to maternal death. The majority of such deaths can be prevented if these complications are managed with timely and effective obstetric critical care. There is a wide gap in the admission and mortality rate of obstetric patients admitted to the critical care units between developed and developing countries despite their similar clinical profile. The present study aims to analyse the incidence, clinical profile and outcomes of obstetric patients requiring admission to the multidisciplinary intensive care unit (ICU) of a tertiary care teaching hospital in South India.
PROCEDURE
With the approval of institutional ethics committee, a prospective observational study was conducted for a 2-year period. All consecutive obstetric admissions (pregnant or within 6 weeks postpartum) to the multidisciplinary ICU during this period were enrolled into the study.
Patients data regarding age, gravida, parity, booking status, gestational age, preexisting diseases, medical conditions attributed by pregnancy, cause for ICU admission, parturient status on ICU admission, complications in ICU and interventions done were recorded. The severity of illness was assessed by admission day APACHE II (Acute Physiology And Chronic Health Evaluation II) and worst SOFA (Sequential Organ Failure Assessment) scores. The primary outcome was maternal mortality and ICU length of stay (LOS), and ventilator days were the secondary outcomes studied.
All statistical analyses were performed using Statistical Package for Social Science (SPSS, version 17) for Microsoft Windows. Descriptive statistics were presented as numbers and percentages. The data were expressed as mean and standard deviation. Independent sample student T test/Mann-Whitney test and Chi square test were applied for continuous variables and qualitative data respectively. Multiple Logistic Regression method was used wherever necessary and a p value <0.05 was considered statistically significant.
RESULTS
A total of 91 obstetric patients were admitted to the ICU during the study period (Table 1). This accounted for 1.8% of the total admissions to the multidisciplinary ICU. The incidence of obstetric admissions to ICU was 2.6% (26 per 1000 deliveries) as there were 3,694 deliveries in the hospital during the study period. The ICU maternal death rate was 9.9 % (n = 9). The calculated MMR was 217 deaths per 100000 deliveries.
Table 1.
Demographic data of the obstetric patients admitted to the ICU during the study period
| Total (n = 91) | Survivors (n = 82) | Non survivors (n = 9) | P value | |
|---|---|---|---|---|
| Age(years), mean± SD | 29.52 ± 5.9 | 29.78 ± 5.9 | 27.33 ± 6.1 | 0.25 |
| Parity [n, (%)] | 0.71 | |||
| < 2 | 63(69.2) | 56(88.9) | 7(11.1) | |
| ≥ 2 | 28(30.8) | 26(92.9) | 2(7.1) | |
| Trimester [n, (%)] | 0.27 | |||
| I Trimester | 5 (5.5) | 5(100) | 0(0) | |
| II Trimester | 19(20.9) | 15(78.9) | 4(21) | |
| III Trimester | 46(50.5) | 42(91.3) | 4(8.7) | |
| Postpartum | 21(23.1) | 20(95.2) | 1(4.8) | |
| Prenatal care [n, (%)] | 0.132 | |||
| Booked | 33(36.3) | 32(97) | 1(3) | |
| Unbooked | 20(22) | 16(80) | 4(20) | |
| Referred | 38(41.8) | 34(89.5) | 4(10.5) | |
| Parturient status [n, (%)] | 0.004 | |||
| Antepartum | 14(15.4) | 9(64.3) | 5(35.7) | |
| Postpartum | 77(84.6) | 73(94.8) | 4(5.2) | |
| Hospital LOS(Days), mean± SD | 10.11 ± 5.7 | 10.06 ± 5.3 | 10.56 ± 9.0 | 0.59 |
| ICU LOS(Days), mean± SD | 3.04 ± 4 | 2.6 ± 3 | 7.0 ± 8 | 0.44 |
| APACHE II, mean± SD | 11.1 ± 7.6 | 10.17 ± 7.1 | 19.56 ± 7.9 | 0.002 |
| Worst SOFA, mean± SD | 6.2 ± 5.2 | 4.9 ± 3.7 | 17.6 ±3.5 | 0.000 |
| Ventilator days, mean± SD | 2.72±4.6 | 1.88 ± 3.41 | 6.51 ± 7.39 | 0.03 |
| Vasopressor therapy [n, (%)] | 20(21.9) | 11(55) | 9(45) | 0.000 |
| Days on vasopressors, mean± SD | 3.30 ± 2.79 | 2 ± 1.18 | 4.89 ± 3.4 | 0.035 |
SD: Standard Deviation; LOS: length of stay; ICU: Intensive Care Unit; APACHE: Acute Physiology and Chronic Health Physiology; SOFA: Sequential Organ Failure Assessment;
The mean age (years) of the study group was 29.52 ±5.9 with no significant difference among survivors (29.76 ±5.9) and non survivors (27.33 ±6.1). Thirty eight patients (41.8%) were referred from other hospitals and 20 (22%) patients did not undergo regular antenatal checkups. Fifty two (57.14%) patients had associated medical conditions, 63 (69.2%) patients were primipara and 77 patients (84.6%) were postpartum on transfer to the ICU. The mean APACHE II scores were significantly higher in non survivors compared to survivors [19.56±7.9 vs 10.17±7.1 (P =0.02)]. The worst SOFA was significantly higher in non survivors [(17.67±3.5 vs 4.97±3.7 (p = 0.00)] and maximum SOFA score observed was 22.
The booking status, presence of coexisting medical disorders and parity did not affect the maternal outcome. But patients admitted in antepartum state had a significantly higher mortality (p value 0.04) than postpartum patients.
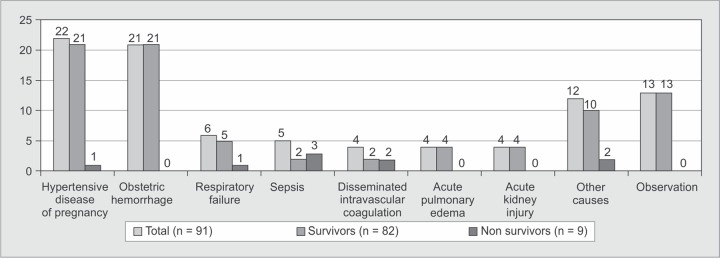
The obstetric causes accounted for majority of ICU admissions (Graph 1) with hypertensive disorders [n = 22, (24.2%)] and obstetric hemorrhage [n = 21, (23.1%)] being the most common. Respiratory failure [n = 6, (6.6%)] was the commonest non obstetric cause for ICU transfer. Emergency cesarean section was done in 31 patients (34.1%) (Table 2). Mechanical ventilator support was provided to 50 patients (54.9%) for a mean duration of 2.72 days. Transfusions were needed in 42 patients (46.1%) and dialysis in nine patients (10.1%). Renal failure [n = 20 (22%)] and Posterior Reversible Encephalopathy Syndrome (PRES) [n = 12 (13%)] were the common complications observed in our patients (Graph 2).
Graph 1.
Indications for ICU admission of the study population
Table 2.
Obstetric and nonobstetric interventions among the study population
| Intervention | No of patients | Percentage (%) |
|---|---|---|
| Emergency LSCS | 31 | 34 |
| Elective LSCS | 12 | 13 |
| Emergency laparotomy | 13 | 14 |
| Mechanical ventilation | 50 | 55 |
| Blood products transfusions | 42 | 46 |
| Vasopressors | 20 | 22 |
| Renal replacement therapy | 9 | 10 |
| Tracheostomy | 4 | 4 |
LSCS: Lower segment cesarean section
Graph 2.
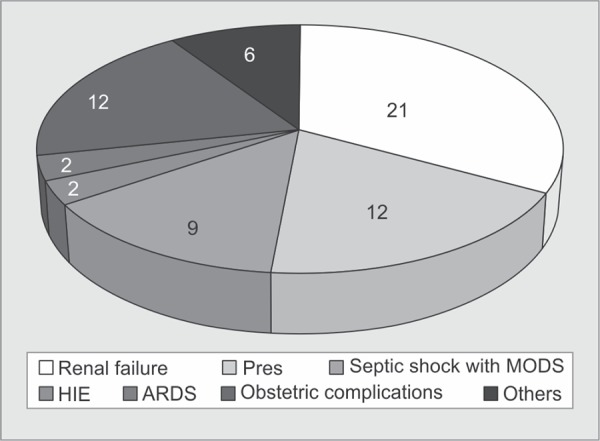
Major Complications in the patients admitted to ICU
DISCUSSION
Obstetric patients are a clinically challenging group to any intensive care unit although they contribute only a small population. This was a prospective observational study conducted over a period of two years to analyse the obstetric admissions, their associated complications and interventions in the multidisciplinary ICU of a tertiary care teaching hospital.
The ICU utilization rate of 1.8% in our study is comparable with studies in the past as detailed in a systematic review by Pollock et al.3 The higher incidence of ICU admissions (2.6%) among obstetric patients in our study was consistent with studies by Harde et al. (2.8%),4 Bhadade et al. (2.8%)5 and Jainet al. (5.4%)6. However, data from previous studies7–10 did not show a similar high incidence. This may be due to differences in the criteria for ICU admission notably patients being transferred to the current facility due to lack of a dedicated obstetric high dependency unit in their hospital, patient referrals from other hospitals due to the severity of their illness and patients who were not booked developing complication subsequently.
Advanced maternal age did not carry an increased risk of maternal mortality in the present study population unlike that observed by Bhadade et al.5 The mean age of the study group with 23% in advanced maternal age (35 yrs and above) was comparable with recent studies4,10–12. Majority of our study population were primiparous (69.2%). Similar observations were made by Gombar et al. (54.3%)7 and Dasgupta et al. (58.3%)8. This is further explained by the higher incidence of PIH in our study population which is common in primipara.
There was a postpartum predominance comparable to other studies7,9,12,13. Postoperative transfer of patients with eclampsia and obstetric haemorrhage irrespective of their haemodynamic status and patients referred from other hospitals following a complication of delivery may explain this. Although the number of antepartum admissions was less and on par with the above studies, we observed a significant mortality among them. The mean hospital and ICU LOS (10.1 and 3.04 days respectively) of the study population were comparable to the recent studies4,6,11,14,15. But wide variations in the duration of ICU stay in both survivors and non survivors had been a confounding factor for this data. This may be the reason for the longer ICU LOS in non survivors (7days versus 2.6 days) not correlating with mortality like in other studies.
Hypertensive disorders followed by obstetric haemorrhage were the common causes for ICU transfer in the present study similar to other national5–7 and international studies12,16. There was an increase in the incidence of sepsis due to obstetric or non-obstetric causes in the recent studies − 11.4%6, 27.15%7, 13.17%8, 12.5%10. Our study observed only 5.5% of admissions to have sepsis. This was similar to other recent Indian studies11,13,15 although Harde et al.4 and Bhadade et al.5 had very low sepsis rate at admission.
The obstetric surgical interventions done were cesarean section in 47.3% and emergency laparotomy in 14.3% patients. Such high rate of cesarean section in patients requiring ICU care was common3,8–10. Mechanical ventilation, transfusion of blood products and initiation and maintenance of vasopressor support were the usual interventions done in our study. Mechanical ventilation was the most common intervention done in the ICU for obstetric patients as described in the systematic review by Pollock et al.3 [Developing countries-41% (range 3.0-100%) and Developed countries-41.5% (range 13.0-76.0%)] and in various recent studies8,10,11. In the present study, 54.9% of patients were mechanically ventilated. Eclampsia (13.2%) and obstetric haemorrhage (17.6%) were the most common indications for mechanical ventilation in our study. Seventy eight percent of these patients were already intubated in operating room or Emergency department. Only 22% of patients required invasive or noninvasive ventilation during the course of ICU stay. Two patients needed prone ventilation in view of acute respiratory distress syndrome (ARDS)17. The mean duration of ventilation was 2.7 days. Non survivors required a significantly longer period of ventilation, (6.5 days versus 1.9 days, p=0.03).
Blood products were transfused in the ICU in 42 patients (46%) while another 13 (14.3%) patients received transfusion even before transfer to ICU. The blood components therapy comprised packed cells in 48.3%, fresh frozen plasma in 38.5%, platelet concentrate in 33% and cryoprecipitate in 22% of patients. The transfusion rates were comparable with Harde et al.4, Sriram Robertson et al.12 and Karnad et al.18 There were no maternal deaths due to obstetric haemorrhage in our study primarily due to adequate and timely resuscitation with blood products. Our observations were consistent with the above studies4,12. Twenty patients (22%) had unstable haemodynamics requiring vasopressor support and they had a significantly high risk for mortality (p = 0.000). We also observed that higher doses and longer duration of vasopressor therapy were associated with adverse maternal outcome leading to death.
The incidence of acute renal failure requiring renal replacement therapy varied among recent studies5,6,8,10,12,18. In the present study 20 patients (22%) developed renal failure. Seventeen patients (18.7%) had developed acute kidney injury (AKI) as per Kidney Disease: Improving Global Outcomes (KDIGO)19 guidelines. Three patients with chronic kidney disease went in for acute deterioration. Though 12 patients (13.2%) required dialysis, three patients could not be dialysed because of severe haemodynamic instability. Six (6.6%) out of the nine patients who underwent dialysis died and three patients were discharged on dialysis.
The maternal mortality rate varied widely between developed and developing countries. It ranged between low or no maternal deaths9,10,12,14,16 in the former to as high as 41.67%13 in the later. The present study population had a mortality rate of 9.9%. Obstetric haemorrhage (27.1%) and hypertensive disorders (14.0%) are the most common causes of maternal mortality globally, followed by sepsis (10.7%)20. Though they together accounted for 57.3% of ICU transfers in our study there was only one maternal death due to these. However, we observed that sepsis due to obstetric or nonobstetric cause led to a significantly high mortality (60%) much higher than that observed by Gombar et al. (48.9%)7. Disseminated intravascular coagulation secondary to intrauterine death (IUD), viral pneumonia ARDS, peripartum cardiomyopathy and tuberculous meningitis were the other causes of death in this study. Among the survivors, nine patients suffered obstetric morbidity needing hysterectomy. Three patients were tracheostomised, one needed mechanical ventilation for more than 10 days following status epilepticus and two patients developed hypoxic ischemic encephalopathy secondary to cardiac arrest outside the ICU. Two patients with AKI became dialysis dependent.
Although the study analyzed various predictors of obstetric illness a multiple logistic regression analysis however found that none of the variables had an association as an independent risk factor for maternal mortality. Furthermore, the results of our study cannot be applied to the entire obstetric population of the nation. Lack of uniformity of health care services across the country and need for referrals to tertiary care hospitals leading to delay in providing treatment may adversely affect the maternal outcome.
CONCLUSION
This study provides an insight into the characteristics of obstetric patients needing intensive care services in South India. However, given the limited sample size and period of study, we conclude that further research may help in achieving a more meaningful data of predictors to reduce maternal mortality and improve health care in this section of patients.
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.WHO U. UNFPA, World Bank Group and the United Nations Population Division. Trends in maternal mortality: 1990 to 2015. Estimates by WHO, UNICEF.; [Google Scholar]
- 2.Special report on maternal mortality in India 2014-16, National Institution for Transforming India, Government Of India; https://niti.gov.in/content/maternal-mortality-ratio-mmr-100000-live-births available at: [Google Scholar]
- 3.Pollock W,, Rose L,, et al. Pregnant and postpartum admissions to the intensive care unit: a systematic review. Intensive care medicine. 2010 1;;36((9):):1465-1474.. doi: 10.1007/s00134-010-1951-0. [DOI] [PubMed] [Google Scholar]
- 4.Harde M,, Dave S,, et al. Prospective evaluation of maternal morbidity and mortality in post-cesarean section patients admitted to postanesthesia intensive care unit. Journal of anaesthesiology, clinical pharmacology. 2014;;30((4):):508.. doi: 10.4103/0970-9185.142844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhadade R,, de'Souza R,, et al. Maternal outcomes in critically ill obstetrics patients: A unique challenge. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2012;;16((1):):8.. doi: 10.4103/0972-5229.94416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jain S,, Guleria K,, et al. Predictors and outcome of obstetric admissions to intensive care unit: a comparative study. Indian journal of public health. 2016 1;;60((2):):159.. doi: 10.4103/0019-557X.184575. [DOI] [PubMed] [Google Scholar]
- 7.Gombar S,, Ahuja V,, et al. A retrospective analysis of obstetric patient's outcome in intensive care unit of a tertiary care center. Journal of anaesthesiology, clinical pharmacology. 2014;;30((4):):502.. doi: 10.4103/0970-9185.142843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dasgupta S,, Jha T,, et al. Critically ill obstetric patients in a general critical care unit: a 5 years' retrospective study in a public teaching hospital of Eastern India. Indian journal of critical care medicine: peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2017;;21((5):):294.. doi: 10.4103/ijccm.IJCCM_445_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zwart JJ,, Dupuis JR,, et al. Obstetric intensive care unit admission: a 2-year nationwide population-based cohort study. Intensive care medicine. 2010 Feb 1;;36((2):):256-263.. doi: 10.1007/s00134-009-1707-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vasquez DN,, Neves AV,, et al. Characteristics, outcomes, and predictability of critically ill obstetric patients: a multicenter prospective cohort study. Critical care medicine. 2015 Sep 1;;43((9):):1887-1897.. doi: 10.1097/CCM.0000000000001139. [DOI] [PubMed] [Google Scholar]
- 11.Sodhi K,, Bansal V,, et al. Predictors of mortality in critically ill obstetric patients in a tertiary care intensive care unit: A prospective 18 months study. Journal of Obstetric Anaesthesia and Critical Care. 2018 Jul 1;;8((2):):73.. [Google Scholar]
- 12.Sriram S,, Robertson MS. Critically ill obstetric patients in Australia: a retrospective audit of 8 years' experience in a tertiary intensive care unit. Critical Care and Resuscitation. 2008 Jun;10((2):):120.. [PubMed] [Google Scholar]
- 13.Gupta S,, Naithani U,, et al. Obstetric critical care: A prospective analysis of clinical characteristics, predictability, and fetomaternal outcome in a new dedicated obstetric intensive care unit. Indian journal of anaesthesia. 2011 Mar;55((2):):146.. doi: 10.4103/0019-5049.79895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orsini J,, Butala A,, et al. Clinical profile of obstetric patients admitted to the medical-surgical intensive care unit (MSICU) of an inner-city hospital in New York. Journal of clinical medicine research. 2012 Oct;4((5):):314.. doi: 10.4021/jocmr1079w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tempe A,, Wadhwa L,, et al. Prediction of mortality and morbidity by simplified acute physiology score II in obstetric intensive care unit admissions. Indian Journal of Medical Sciences. 2007 Apr 1;;61((4).) [PubMed] [Google Scholar]
- 16.Harrison DA,, Penny JA,, et al. Case mix, outcome and activity for obstetric admissions to adult, general critical care units: a secondary analysis of the ICNARC Case Mix Programme Database. Critical Care. 2005 Jun;9((3):):S25.. [Google Scholar]
- 17.Force AD,, Ranieri VM,, et al. Acute respiratory distress syndrome. Jama. 2012 Jun;20;307((23):):2526-2533.. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 18.Karnad DR,, Lapsia V,, et al. Prognostic factors in obstetric patients admitted to an Indian intensive care unit. Critical care medicine. 2004 Jun 1;;32((6):):1294-1299.. doi: 10.1097/01.ccm.0000128549.72276.00. [DOI] [PubMed] [Google Scholar]
- 19.Kellum JA,, Lameire N,, et al. Kidney disease: Improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney International Supplements. 2012 Mar 1;;2((1):):1-138.. doi: 10.1038/kisup.2012.1. [DOI] [Google Scholar]
- 20.Say L,, Chou D,, et al. Global causes of maternal death: a WHO systematic analysis. The Lancet Global Health. 2014 Jun 1;;2((6):):e323-333.. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]