Abstract
Millions of US veterans have returned from military service with posttraumatic stress disorder (PTSD), for which a substantial number receive Department of Veterans Affairs (VA) disability benefits. Although PTSD is treatable, comorbid serious mental illness could complicate these veterans’ recovery. Using VA administrative data, we examined the burden of persistent serious mental illness in a nationally representative cohort of 1,067 men and 1,513 women who applied for VA PTSD disability benefits between 1994 and 1998 and served during or after the Vietnam conflict. Self-reported outcomes were restricted to the 713 men and 1,015 women who returned surveys at each of 3 collection points. More than 10% of men and 20% of women had persistent serious mental illness; of these, more than 80% also had persistent PTSD. On repeated measures modeling, those with persistent serious mental illness consistently reported more severe PTSD symptoms and poorer functioning in comparison to other participants (ps < .001); their employment rate did not exceed 21.0%. Interactions between persistent serious mental illness and PTSD were significant only for employment (p = .002). Persistent serious mental illness in this population was almost 2 to 19 times higher than in the general US population. Implications are discussed.
Along with traumatic brain injury, posttraumatic stress disorder (PTSD) has become the “signature” war injury of the United States’ recent military actions around the world (Brundage et al., 2015; Taniellian and Jaycox, 2008). However, long before the current period, millions of military veterans returned from prior wars, conflicts, and even peacetime service with PTSD symptoms. Consequently, nearly 650,000 US veterans currently receive Department of Veterans Affairs (VA) disability benefits for PTSD; of these, approximately 40% are Vietnam era veterans; 30% are Gulf War I era veterans; and 24% are veterans of more recent conflicts (Dept. Veterans Affairs, Veterans Benefits Administration, 2014).
In U S. general populations, approximately one half to four-fifths of PTSD cases remit after 6 years, even without treatment (Breslau et al., 1998; Kessler et al., 1995). Unfortunately, few additional remissions are observed after 6 years have passed (Breslau, et al. 1998; Kessler, et al., 1995). Historically, applicants for VA PTSD disability benefits have waited at least 10 years after their military separation to file claims (Murdoch et al., 2003c). This suggests that VA disability applicants may have experienced longer, more intractable disease courses than Veterans with PTSD who never applied for such benefits. In the Social Security Disability Insurance and Supplemental Security Income (SSDI/SSI) programs, for example, disability applicants with mental disorders tend to be substantially more symptomatic than individuals with similar mental disorders who never apply. SSDI/SSI applicants with mental disorders are also more likely than non-applicants to have thought disorders, such as schizophrenia (Estroff et al., 1997; Kouzis and Eaton, 2000).
The idea that serious mental illness, defined here as schizophrenia, schizoaffective disorder, and bipolar spectrum disorders, might be complicating the recovery course of Veterans applying for PTSD disability benefits has not, to our knowledge, been explored. However, individuals with serious mental illnesses are at increased risk for developing PTSD (Buckley et al., 2009; Mauritz et al., 2013; Otto et al., 2004; Sareen et al., 2005). For example, delusional symptoms have been found to be more common in those with PTSD (Alsawy et al., 2015; Scott et al., 2007), and, in at least one small cohort of individuals with a first episode of psychosis, 69% had antecedent PTSD (Strakowski, et al., 1995). In 2009, nearly one fifth of men and one quarter of women with PTSD in the VA system received atypical antipsychotics (Bernardy et al., 2012). Whereas these medications might have been prescribed as adjunctive treatments for PTSD symptoms, it is also possible they were being used to treat coexisting psychoses. Serious mental illness coexisting with PTSD hampers the management of both conditions (Frueh et al., 2009; Mauritz, et al., 2013; Otto, et al., 2004; Salyers, et al., 2004). Proposals designed to reduce veterans’ enrollment into or tenure on the VA disability rolls (e.g., “Treatment First” requirements, Satel, 2011) might work well for PTSD sufferers without co-existing serious mental illness but prove unrealistic or even harmful for those with serious mental illness. Understanding the burden of serious mental illness within the population of veterans seeking or receiving PTSD disability benefits therefore is necessary for creating compassionate, informed policies that account for these veterans’ potential complexities. This is particularly important given that the pool of individuals affected by these policies is large.
As part of a 15-year cohort study, we recently completed 64 qualitative interviews with former applicants for PTSD disability benefits. Almost a quarter of these interviewees described manic symptoms, paranoia, or hearing voices or offered other clues suggesting they had coexisting serious mental illness. This unexpected finding caused us to revisit diagnostic codes that had been collected for the entire cohort between 1994 and 2006. In the present paper, we describe the proportion of cohort members with persistent serious mental illness based on those codes. Because symptom reduction, improved functioning, and gainful employment would, we hypothesized, be critical to successfully transitioning any veteran off the disability rolls (Hennessey & Muller, 1994; Hogg-Johnson & Cole, 2003; Muller, 1992), we examined PTSD symptom severity; work, role, and social functioning; and gainful employment over time according to participants’ serious mental illness status. Lastly, we explored the interaction of serious mental illness and PTSD on these outcomes.
Methods
Participants
Between January 1994 and December 1998 100,750 male veterans and 3,866 female veterans applied for, but did not necessarily receive, VA PTSD disability benefits. From this frame we randomly selected 2,466 men and 2,452 women (total N = 4,918) to participate in a Time 1 (1998-2000) survey that examined race, gender, and regional disparities in PTSD disability awards.(Murdoch et al., 2003a,b; Murdoch et al., 2005) Almost 68% of veterans responded (n = 3,337; 1,654 men and 1,683 women). These respondents comprised the cohort for the present study. At Time 2 (2004-2006) all 2,925 surviving and trackable Time 1 respondents were invited to participate in a second survey that examined long-term outcomes associated with receiving PTSD disability benefits (Murdoch et al., 2011). There were 87.2% of Veterans who responded (n = 2,551; 1,203 men and 1,348 women). The Time 3 survey (2011-2012) was intended to explore factors associated with recovery or non-recovery from PTSD. To improve the study’s relevancy to most PTSD disability recipients and to avoid conflating the effects of advanced aging on mental health recovery, we limited the Time 3 survey to cohort members who served during or after the Vietnam conflict. As of January 1, 2011, 2,580 cohort members (1,067 men and 1,513 women) were still living and had served during or after the Vietnam conflict. These individuals contributed to the present study’s primary outcome and to the secondary outcome of PTSD comorbidity.
Remaining secondary outcomes were limited to Time 3 survey respondents. Veterans eligible to receive the Time 3 survey had served during or after the Vietnam conflict, responded to the Time 2 survey, were still living, had a valid address, and were not incarcerated. Thus, from the Time 2 respondents we excluded 469 cohort members—mostly men—and 24 veterans who requested no further contact after Time 2. Of the 871 men eligible for the Time 3 survey, 713 (81.9%) responded and of the 1,229 women who were eligible, 1,015 (82.6%) responded.
Differences between Time 1 respondents and non-respondents were negligible (Murdoch, et al., 2003a). Compared to their Time 2 non-respondent counterparts, Time 2 male respondents who served during or after the Vietnam conflict were more likely to have had some college experience (44.0% vs. 52.3%, p> = .003) and to have worked for pay at Time 1 (21.1% vs. 26.6%, p = .044); Time 2 female respondents were more likely to be receiving VA disability benefits (76.6% vs. 82.9%, p< 001). Among Time 3 eligible men, respondents were approximately 30% less likely than non-respondents to have ever been diagnosed with schizophrenia (p = .045). Among Time 3 eligible women, there were no meaningful differences between respondents and non-respondents on any parameter.
Procedure
The study is a mixed-methods, ambispective cohort study (ambispective = retrospective and prospective elements). VA diagnostic codes were collected on the cohort between 1994 and 2006. The Minneapolis VA Health Care System’s Internal Review Board for Human Studies reviewed and approved the study’s protocol. We mailed surveys to veterans’ homes with a money incentive ranging from $5 (Time 1) to $10 (Time 2 and 3). Cover letters described the surveys’ risks and benefits and emphasized that participation was voluntary. Veterans signified consent by returning a completed survey.
Measures
Persistent serious mental illness.
We used the VA National Patient Care Database to determine whether cohort members had been diagnosed with an anxiety disorder, bipolar disorder, depressive disorder, PTSD, or schizophrenia between 1994 and 2006. Schizo-affective disorder was included with schizophrenia. Bipolar disorder and schizophrenia/schizo-affective diagnoses are strikingly stable over time (Bromet et al., 2011; Fusar-Poli et al., 2016; Marneros, Deister, & Rohde, 1991; Mason et al., 1996). Once reconfirmed by chart 6-24 months later, neither diagnosis is likely to ever be lost subsequently (Harvey et al., 2012; Kessing, 2005). In those few cases in which a bipolar or schizophrenia/schizo-affective disorder diagnosis is dropped, it is typically because the individual has acquired the other diagnosis. Thus, the stability of either a bipolar or schizophrenia diagnosis over 10 years is estimated to be 93% (Bromet et al., 2011).
In the present study, our goal was to be particularly conservative in classifying individuals as having persistent serious mental illness. Thus, even though data suggest 2 diagnoses should be adequate, we categorized veterans as having “persistent serious mental illness” only if they were diagnosed with bipolar disorder or schizophrenia/schizo-affective disorder at least once in 3 separate calendar years.
Secondary outcomes.
A high burden of persistent serious mental illness in this patient population could reflect high comorbidity with PTSD or it could reflect substitution effects. For example, veterans with persistent serious mental illness but no PTSD might preferentially apply for PTSD disability benefits for a reason other than their primary diagnosis if they perceived PTSD benefits as being easier to obtain. We therefore examined the percentage of cohort members with persistent serious mental illness only, with both persistent serious mental illness and persistent PTSD, with persistent PTSD only, and neither. Veterans were classified as having persistent PTSD if they had a VA chart diagnosis of PTSD at least once in 3 separate calendar years.
PTSD symptoms; work, role, and social functioning; and gainful employment were assessed by survey at all three time points. The Penn Inventory for PTSD (Penn Inventory, Hammarberg, 1992) assessed veterans’ PTSD symptom severity in the 2 weeks prior to each survey. Among veterans, scores ≥ 35 have .90 to .98 sensitivity and .94 to 1.00 specificity for PTSD diagnosis (Hammarberg, 1992). Cronbach’s α = .94 in this sample. The overall summary score of the self- reported Social Adjustment Scale (SAS-SR, Weissman et al., 1981) assessed veterans’ work, role, and social functioning in the 2 weeks before each survey. The SAS-SR measures functioning in 7 domains: major “work” role (i.e., paid employment, homemaker, student); social and community activities; marriage, extended family, family unit, and parental relationships; and economic self-sufficiency. Higher scores indicate poorer adjustment across all domains. Normal, community-dwelling adults have average SAS-SR scores of 1.6, whereas scores for individuals with psychiatric illness usually exceed 2.0 (Weissman et al., 2001). Cronbach’s α = .84 in this sample. We considered veterans’ scores to be impaired if their Penn Inventory exceeded 34 or their SAS-SR exceeded 2.0. For Time 3 respondents under age 65, a single SAS-SR item, “Did you work any hours for pay in the last 2 weeks?,” measured gainful employment.
Data Analysis
We used Pearson’s χ2 and ANOVA to test unadjusted differences in outcomes within each gender. To investigate whether any associations between persistent serious mental illness and secondary outcomes varied by time, we used marginal (population-averaged) repeated measures modeling (SAS PROC MIXED or SAS PROC GLIMMIX) with a Toeplitz working correlation. This produced the smallest Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC) for continuous outcomes and the χ2/df closest to 1 for gainful employment (Stroup, 2016). The repeated measures models also tested for interactions between persistent serious mental illness and persistent PTSD. Model predictors included gender, to account for our stratified sampling strategy; persistent serious mental illness and persistent PTSD case status; time as a categorical variable; and the interactions between these variables. We had complete ascertainment for all predictors. A conventional two-tailed p ≤ .050 denoted statistical significance. Computations used SPSS 19.0 or SAS 9.2.
Results
Descriptive Statistics
Table 1 describes the cohort’s and Time 3 respondents’ sociodemographic characteristics by gender. As can be seen, there were minimal differences between respondents and the overall cohort. Men were on average 11 years older than the women. Almost 90% of men served during the Vietnam conflict compared to slightly less than one quarter of the women.
Table 1.
Descriptive Statistics.
| Characteristic | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| Cohort | Time 3 | Cohort | Time 3 | |||||
| Respondents | Respondents | |||||||
| N = 1,067 | n = 713 | N = 1,513 | n = 1,015 | |||||
| M | SD | M | SD | M | SD | M | SD | |
| Age | 63.15 | 5.87 | 63.09 | 5.75 | 52.48 | 9.07 | 52.91 | 8.84 |
| n | % | n | % | n | % | n | % | |
| Race/ethnicity | ||||||||
| White | 750 | 70.3 | 506 | 70.9 | 1095 | 72.4 | 749 | 73.8 |
| Black or African American | 187 | 17.5 | 125 | 17.5 | 286 | 18.9 | 185 | 18.2 |
| Hispanic or Latino | 76 | 7.1 | 47 | 6.6 | 71 | 4.7 | 46 | 4.5 |
| Other | 54 | 5.1 | 35 | 4.9 | 61 | 4.0 | 35 | 3.4 |
| Served during the Vietnam conflict | 933 | 87.4 | 644 | 90.3 | 343 | 22.7 | 248 | 24.4 |
| At least some college experiencea | 590 | 55.3 | 424 | 59.4 | 1274 | 84.2 | 857 | 84.4 |
| Marrieda | 608 | 57.0 | 409 | 57.4 | 551 | 36.4 | 365 | 36.0 |
As of the Time 1 (1998-2000) survey. Time 3 respondents are the subset of the cohort who returned Time 3 surveys.
Persistent Serious Mental Illness and Other Mental Disorders
More than a tenth of the cohort’s men and a fifth of the cohort’s women met our criteria for persistent serious mental illness (Table 2). Almost three fourths of the men and two thirds of women had persistent PTSD. Except for PTSD, women in the cohort were significantly more likely than men to have received any of the abstracted diagnoses.
Table 2.
Burden of Persistent Serious Mental Illness and Other Mental Health Disorders by Gender-- Based on VA Chart Diagnoses between 1994 and 2006
| Diagnosis | Cohort Men | Cohort Women | ||
|---|---|---|---|---|
| N = 1,067 | N = 1,513 | |||
| n | % | n | % | |
| Persistent serious mental illness | 108 | 10.1 | 327 | 21.6*** |
| Persistent PTSD | 816 | 76.5 | 988 | 65.3*** |
| Serious mental illness, diagnosed ever | ||||
| Bipolar disorder | 212 | 19.9 | 495 | 32.7*** |
| Schizophrenia or Schizo-affective disorder | 127 | 11.9 | 269 | 17.8*** |
| Other mental health disorders, diagnosed ever | ||||
| Anxiety disorder | 426 | 39.9 | 778 | 51.4*** |
| Depressive disorder | 761 | 71.3 | 1201 | 79.4*** |
| PTSD | 931 | 87.3 | 1230 | 81.3*** |
PTSD = Posttraumatic stress disorder.
p < .001
Comorbidity with PTSD
Among men in the cohort, 8.4% had persistent PTSD and serious mental illness, 1.7% had persistent serious mental illness only, 68.0% had persistent PTSD only, and 21.8% had neither. Thus, of the 108 men with persistent serious mental illness, 83.3% also had persistent PTSD. Among women in the cohort, 18.3% had persistent PTSD and serious mental illness, 3.3% had persistent serious mental illness only, 47.0% had persistent PTSD only, and 31.4% had neither. Of the 327 women with persistent serious mental illness, 84.7% also had persistent PTSD.
PTSD Symptoms and Functioning
Table 3 shows the observed, unadjusted mean Penn Inventory and SAS-SR scores for respondents with and without persistent serious mental illness at each time point. Because they were so similar to the estimated means generated by repeated measures modeling (details available from the authors upon request), only observed results are reported.
Table 3.
Observed, Unadjusted Penn Inventory for PTSD and Social Adjustment-Self-Report Scores over Time by Persistent Serious Mental Illness Status and Gender (Time 3 Respondents Only)
| Scores | Time 1 | Time 2 | Time 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| With SMI | Without SMI | With SMI | Without SMI | With SMI | Without SMI | |||||||
| Men | n = 60 | n = 653 | n = 60 | n = 653 | n = 60 | n = 653 | ||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | |
| Penn Inventory | 55.06 | 14.85*** | 47.35 | 15.28 | 48.15 | 15.00** | 42.59 | 14.52 | 44.65 | 14.06 | 41.20 | 14.55 |
| SAS-SR | 3.21 | 0.73*** | 2.81 | 0.71 | 2.96 | 0.75* | 2.71 | 0.73 | 2.84 | 0.71** | 2.60 | 0.66 |
| Women | n = 222 | n = 793 | n = 222 | n = 793 | n = 222 | n = 793 | ||||||
| Penn Inventory | 48.32 | 13.33*** | 40.91 | 14.91 | 43.43 | 14.42*** | 37.56 | 14.87 | 41.43 | 14.14*** | 37.61 | 14.34 |
| SAS-SR | 2.99 | 0.71*** | 2.65 | 0.72 | 2.89 | 0.73*** | 2.60 | 0.71 | 2.81 | 0.69*** | 2.60 | 0.68 |
Time 1 = 1998 – 2000; Time 2 = 2004 – 2006; Time 3 = 2001 – 2012. SMI = with persistent serious mental illness. Penn Inventory = Penn Inventory for PTSD. SAS-SR = Social Adjustment Score-Self-Report.
p ≤ .001,
p ≤ .01,
p ≤ .05
Repeated measures modeling showed that, after controlling for gender and time, respondents with persistent serious mental illness had consistently poorer mean Penn Inventory scores, F (1, 1724) = 34.64, p < .001, and SAS-SR scores, F (1, 1724) = 41.39, p < .001, in comparison to those without persistent serious mental illness. For either outcome, there were no statistically significant interactions between persistent serious mental illness and time or between persistent serious mental illness and persistent PTSD (ps > .368)
Figure 1 shows that at Time 1, more than 90% of men and 80% of women with persistent serious mental illness had impaired Penn Inventory scores, as compared to 79% of men and 67% of women without persistent serious mental illness (Panel A). Panel B shows that almost 90% of men and women with persistent serious mental illness had impaired SAS-SR scores, as compared to 80% of men and 86% of women without persistent serious mental illness. Over time all groups improved slightly on both measures, but, as shown in the Figure 1, differences by persistent serious mental illness status were maintained.
Figure 1.
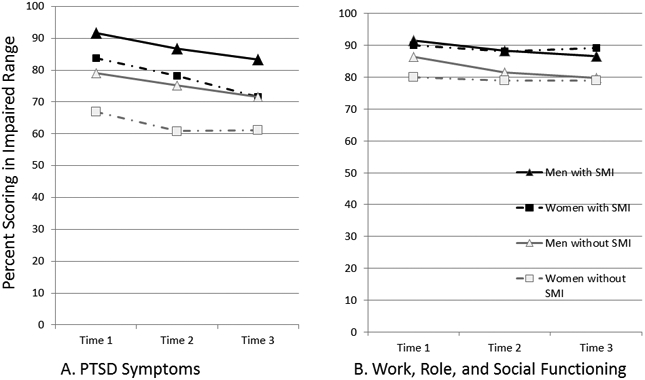
Percentage of respondents scoring in the impaired range on the Penn Inventory for PTSD (Panel A) and on the Social Adjustment Scale-Self-Report (Panel B). SMI = Persistent Serious Mental Illness.
Time 1 = 1998-2000; time 2 = 2004-2006; Time 3 = 2011-2012
Employment
Except for women respondents without persistent serious mental illness, few Time 3 respondents under age 65 reported working for pay at any survey point (Figure 2). Employment rates for men with persistent serious mental illness were particularly low and never exceeded 10%. On repeated measures modeling, there were no statistically significant interactions between time, persistent serious mental illness, and employment (p = .113). However, as shown in Table 4, there was a statistically significant interaction between persistent serious mental illness, persistent PTSD, and employment, F (1, 1429) = 5.27, p = .022. Consistent with the unadjusted results, persistent serious mental illness was associated with very low averaged employment rates regardless of persistent PTSD status.
Figure 2.
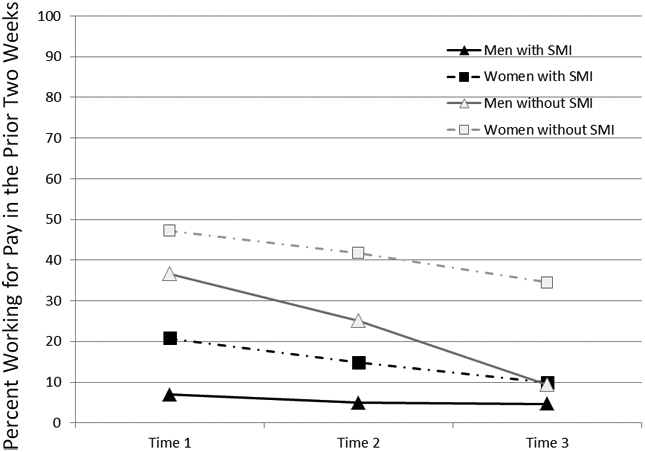
Percentage of respondents under age 65 at Time 3 who said they worked for pay in the prior two weeks. SMI = Persistent Serious Mental Illness. Time 1 = 1998-2000; Time 2 = 2004-2006; Time 3 = 2011-2012
Table 4.
Time 3 Respondents under Age 65 who had Worked for Pay in the Prior Two Weeks, Averaged over Time (1998-2012), by Persistent Serious Mental Illness and PTSD Status
| Status | N | Estimated Averaged Percentage (%) | 95% CI |
|---|---|---|---|
| SMI with PTSD | 224 | 9.5 | [7.1, 12.5] |
| SMI without PTSD | 30 | 10.4 | [4.9, 24.8] |
| No SMI with PTSD+ | 786 | 22.3 | [19.9, 24.8] |
| No SMIwithout PTSD− | 394 | 47.1 | [42.9, 51.3] |
Results of a marginal (population-averaged) repeated measures model controlling for gender-stratified sampling and within-subject correlation over time. CI= Confidence Intervals. SMI = persistent serious mental illness. PTSD = persistent PTSD.
Discussion
Almost one tenth of the men and one fifth of the women in this cohort of former PTSD disability applicants had a persistent serious mental illness. Depression and anxiety have frequently been described in clinical samples of veterans with PTSD (Bernardy, et al., 2012; Kehle et al., 2011), but this is the first study to our knowledge to show such striking rates of schizophrenia and bipolar disorder. In the general US population, the lifetime prevalence of schizophrenia is approximately 1.1% (Bourdon et al., 1992), and the lifetime prevalence of bipolar disorders, including subthreshold disorders is about 4.4% (Merikangas et al., 2011). In the VA health care system overall, approximately 3.6% of Veterans have schizophrenia and 3.0%, bipolar disorder (Zivin et al., 2011).
In the present cohort, women were almost two times more likely than the men to have been diagnosed with persistent schizophrenia/schizo-affective disorder or bipolar disorder. In general populations, prevalence rates of bipolar spectrum disorders and schizophrenia are roughly equal between men and women (Bourdon, et al., 1992; McGrath et al., 2008), whereas men are slightly more likely to be diagnosed with schizophrenia in the VA system (Blow et al., 2004). However, in the subset of veterans who apply for PTSD disability benefits, clinicians may have a greater propensity to diagnose serious mental illnesses in women than in men (Dept. of Veterans Affairs, Office of the Inspector General, 2010). Persistent serious mental illness also might be more strongly associated with PTSD diagnosis in women veterans; for example, women veterans with persistent serious mental illness might be more susceptible to experiencing trauma or to developing PTSD after trauma exposure in comparison to men (Neria et al., 2002), or trauma might be a stronger risk factor for later serious mental disorders in women compared to men. There also might be a greater propensity for women with comorbid PTSD and serious mental illness to apply for VA disability benefits as compared to men.
The high prevalence of persistent serious mental illness in this population did not seem be explained by substitution effects. Very few veterans in this cohort had persistent serious mental illness without comorbid persistent PTSD. Serious mental illness may be a correlate—if not an actual risk factor—for applying for VA PTSD disability benefits. Having a thought disorders predicts applying for SSDI/SSI benefits (Estroff, et al., 1997; Kouzis and Eaton, 2000), and it makes sense that thought disorders also might predict application for VA disability benefits. As highly impaired as this cohort proved to be overall, impairments were higher yet among those with persistent serious mental illness.
Given our respondents’ high rates of impairment, it is not surprising that they also reported very low employment. Veterans with persistent serious mental illness, with or without accompanying persistent PTSD, were those least likely to report ever working for pay, followed by those with persistent PTSD only. In the U.S. population generally, employment typically exceeds 70% among those under age 65 years (U.S. Bureau of Labor Statistics, 2015) but ranges between 17% and 25% for those with disabilities (U.S. Bureau of Labor Statistics, 2014). For veterans being treated for bipolar disorder or schizophrenia, employment rates typically range from 10% to 20% (Zivin et al., 2011). During the times studied here, at most only a fifth of women and less than a tenth of men with persistent serious mental illness ever worked for pay.
A number of limitations of the present study should be considered. Although this cohort is representative of the veterans who applied for PTSD disability benefits between 1994 and 1998, the results may not generalize to veterans who applied after this time and in particular may not apply to veterans from more recent military operations. Individuals self-selecting into an all-volunteer armed forces may have more or fewer risk factors for persistent serious mental illness than veterans who were conscripted, for example. Given that earlier treatment appears to result in better outcomes for people with schizophrenia (Melle et al., 2004), it would be especially important to learn whether more recent and younger applicants for PTSD disability benefits also carry high burdens of serious mental illness. A recent review of 500,000 military separations between 2005 and 2006 showed that 4.9% to 11.8% of these veterans had affective psychoses (Dept. of Veterans Affairs Office of the Inspector General, 2010)—a prevalence higher than that of the general population, but not as high as our cohort’s. Unfortunately, the authors of that study did not cross-tabulate the prevalence of affective psychosis among those with and without PTSD.
Our results also cannot be generalized to all veterans with PTSD or to non-veterans with PTSD. We may have underestimated this cohort’s prevalence of persistent serious mental illness because we did not have medical record information before 1994 or after 2006 and because we did not have access to data from other medical systems. Requiring at least one serious mental disorder diagnosis in 3 separate calendar years may have been overly stringent (Harvey et al., 2012). We also limited our definition of severe mental illness to schizophrenia/schizoaffective disorder and bipolar disorder, but other diagnoses, such as major depression, can be deeply impairing. All of these choices likely reduced the apparent differences between those with and without persistent serious mental illness. Men with schizophrenia were less likely to participate in the Time 3 survey than other men and their under representation could have biased results in unpredictable ways. Finally, the present study is exploratory and not explanatory. We do not know why outcomes were poorer for those with persistent serious mental illness, for example, only that they were. This important question and its corollary—namely, how do we improve these Veterans’ well-being—will require further investigation.
In conclusion, to our knowledge this is the largest, longest-running cohort study of former disability applicants that has been conducted. Findings showed that persistent serious mental illness was strikingly high, frequently comorbid with PTSD, and associated with more severe long-term impairments and lower employment. If serious mental illness is indeed a correlate of seeking VA disability benefits, as we speculate, then other subgroups of disability applicants in the VA system, such as those with musculoskeletal pain, might also bear higher than expected burdens of serious mental illness. Our data suggest that this population’s overall needs for rehabilitation may be more complex than has been previously appreciated. Women’s burden of persistent serious mental illnesses exceeded men’s for unclear reasons and should be explored further. Nearly one third of the entire VA budget is allocated for direct payments to disabled Veterans, yet we know surprisingly little about these veterans’ characteristics, challenges, or long-term trajectory. To fashion compassionate, realistic policies for these individuals we must reverse this trend.
Acknowledgments
This study was supported by grant (#IIR-09-359) from VA Health Services Research and Development (HSR&D) service. Drs. Murdoch, Spoont, Harwood, and Kehle-Forbes are core-investigators; Dr. Sayer, Deputy Director, Ms. Bangerter, data manager; and Ms. Clothier, statistician for the Center for Chronic Disease Outcomes Research at the Minneapolis VA Medical Center, which is a VA HSR&D Service Center of Innovation (#CIN-13-406). Dr. Kehle-Forbes was supported by a VA HSR&D Career Development Award (#09-020). Dr. Spoont is investigator for the National Centers for PTSD, US Department of Veterans Affairs.
References
- Alsawy S, Wood L, Taylor P, & Morrison A (2015). Psychotic experiences and PTSD: Exploring associations in a population survey. Psychological Medicine, 45, 2849–59. doi: 10.1017/S003329171500080X [DOI] [PubMed] [Google Scholar]
- Bernardy N, Lund B, Alexander B, Jenkyn A, Schnurr P, & Friedman M (2012). Gender differences in prescribing among Veterans diagnosed with posttraumatic stress disorder. Journal of General Internal Medicine, 28, S542–S8. doi: 10.1007/s11606-012-2260-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blow FC, Zeber JE, McCarthy JF, Valenstein M, Gillon L, & Bingham CR (2004). Ethnicity and diagnostic patterns in veterans with psychoses. Social Psychiatry and Psychiatric Epidemiology, 39, 841–51. [DOI] [PubMed] [Google Scholar]
- Bourdon K, Rae D, Locke B, Narrow W, & Regier D (1992). Estimating the prevalence of mental disorders in U.S. adults from the Epidemiologic Catchment Area Survey. Public Health Reports, 107, 663–8. [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Kessler R, Chilcoat H, Schultz L, Davis G, & Andreski P (1998). Trauma and posttraumatic stress disorder in the community: The 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry, 55, 626–32. [DOI] [PubMed] [Google Scholar]
- Bromet E, Kotov R, Fochtmann L, Carlson G, Tanenberg-Karant M, Ruggero C, & Chang S (2011). Diagnostic stability revisited: Shifts during the decade following first-admission for psychosis. American Journal of Psychiatry, 168, 1186–1194. doi: 10.1176/appi.ajp.2011.11010048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brundage J, Taubman S, Hunt D, & Clark L (2015). Wither the "signature wounds of the war" after the war: Estimates of incidence rates and proportions of TBI and PTSD diagnoses attributable to background risk, enhanced ascertainment, and active war zone service, active component, US Armed Forces, 2003-2014. Medical Surveillance Monthly Report, 22, 2–11. [PubMed] [Google Scholar]
- Buckley P, Miller B, Lehrer D, & Castle D (2009). Psychiatric comorbidities and schizophrenia. Schizophrenia Bulletin, 35, 383–402. doi: 10.1093/schbul/sbn135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dept. Veterans Affairs Office of Inspector General. (2010). Review of Combat Stress in Women Veterans Receiving VA Health Care and Disability Benefits. Washington, D.C.: Dept. Veterans Affairs Office of Inspector General; 81 pp. [Google Scholar]
- Dept. Veterans Affairs Veterans Benefits Administration (2014). Annual Benefits Report Fiscal Year 2013. Washington D.C.: Department of Veterans Affairs. [Google Scholar]
- Estroff S, Zimmer C, Lachiotte W Jr., Benoit J, & Patrick D (1997). "No other way to go." Pathways to disability income application among persons with severe, persistent mental illness In: Bonnie R, Monahan J, editors. Mental Disorder, Work Disability and the Law. Chicago: University of Chicago Press; p. 55–104. [Google Scholar]
- Frueh B, Grubaugh A, Cusack K, & Elhai J (2009). Disseminating evidence-based practices for adults with PTSD and severe mental illness in public-sector mental health agencies. Behavavior Modification, 33, 66–81. doi: 10.1177/0145445508322619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusar-Poli P, Cappucciati M, Rutigliano G, Heslin M, Stahl D, Brittenden Z, Caverzasi E, McGuire P, & Carpenter W (2016). Diagnostic stability of ICD/DSM first episode psychosis diagnoses: Meta-analysis. Schizophrenia Bulletin. doi: doi: 10.1093/schbul/sbw020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammarberg M (1992). Penn Inventory for Posttraumatic Stress Disorder: Psychometric properties. Psychological Assessessments, 4, 67–76. 10.1037/1040-3590.4.1.67 [DOI] [Google Scholar]
- Harvey P, Heaton R, Carpenter WJ, Green M, Gold J, & Schoenbaum M (2012). Diagnosis of schizophrenia: Consistency across information sources and stability of the condition. Schizophrenia Research, 140, 9–14. doi: 10.1016/j.schres.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennessey J, Muller S (1994). Work efforts of disabled-worker beneficiaries: Preliminary findings from the New Beneficiary Followup Survey. Social Security Bulletin, 57, 42–51. [PubMed] [Google Scholar]
- Hogg-Johnson S, Cole D (2003). Early prognostic factors for duration on temporary total benefits in the first year among workers with compensated occupational soft tissue injuries. Occupational and Enviromental Medicine, 60, 244–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kehle S, Reddy M, Ferrier-Auerbach A, Erbes C, Arbisi P, & Polusny M (2011). Psychiatric diagnoses, comorbidity, and functioning in National Guard troops deployed to Iraq. Journal of Psychiatric Research, 45, 126–32. doi: 10.1016/j.jpsychires.2010.05.013 [DOI] [PubMed] [Google Scholar]
- Kessing L (2005). Diagnostic stability in bipolar disorder in clinical practise as according to ICD-10. Journal of Affecive Disorders, 85, 293–299. doi: doi: 10.1016/j.jad.2004.11.001 [DOI] [PubMed] [Google Scholar]
- Kessler R, Sonnega A, Bromet E, Hughes M, & Nelson C (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–60. [DOI] [PubMed] [Google Scholar]
- Kouzis A, Eaton W Psychopathology and the initiation of disability payments. (2000). Psychiatric Services, 51, 908–13. [DOI] [PubMed] [Google Scholar]
- Marneros A, Deister A, & Rohde A (1991). Stability of diagnoses in affective, schizoaffective and schizophrenic disorders. Cross-sectional versus longitudinal diagnosis. European Archives of Psychiatry and Clinical Neuroscience, 24, 187–192. [DOI] [PubMed] [Google Scholar]
- Mason P, Harrison G, Glazebrook C, Medley I, & Croudace T (1996). The course of schizophrenia over 13 years. A report from the International Study on Schizophrenia (ISoS) coordinated by the World Health Organization. British Journal of Psychiatry, 169, 580–586. doi: 10.1192/bjp.169.5.580 [DOI] [PubMed] [Google Scholar]
- Mauritz M, Goossens P, Draijer N, & van Achterberg T (2013). Prevalence of interpersonal trauma exposure and trauma-related disorders in severe mental illness. European Journal of Psychotraumatology, 4, 19985-http://dx.doi.otg/10.3402/ejpt.v4i0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath J, Saha S, Chant D, & Welham J (2008). Schizophrenia: A concise overview of incidence, prevalence, and mortality. Epidemiology Review, 30, 61–76. doi: 10.1093/epirev/mxn001 [DOI] [PubMed] [Google Scholar]
- Melle I, Larsen T, Haahr U, Friis S, Johannessen J, Opjordsmoen S, et al. (2004). Reducing the duration of untreated first-episode psychosis: Effects on clinical presentation. Archives of General Psychiatry, 61, 143–50. [DOI] [PubMed] [Google Scholar]
- Merikangas K, Jin R, He J, Kessler R, Lee S, Sampson N, et al. (2011). Prevalence and correlates of bipolar spectrum disorder in the World Mental Health Survey initiative. Archives of General Psychiatry, 68, 241–51. doi: 10.1001/archgenpsychiatry.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller L (1992). Disability beneficiaries who work and their experience under program work incentives. Social Security Bulletin, 55, 2–19. [PubMed] [Google Scholar]
- Murdoch M, Hodges J, Cowper D, Fortier L, & van Ryn M (2003a). Racial disparities in VA service connection for posttraumatic stress disorder disability. Medical Care, 41, 536–49. [DOI] [PubMed] [Google Scholar]
- Murdoch M, Hodges J, Cowper D, & Sayer N (2005). Regional variation and other correlates of Department of Veterans Affairs (VA) disability awards for posttraumatic stress disorder. Medical Care, 43, 112–21. [DOI] [PubMed] [Google Scholar]
- Murdoch M, Hodges J, Hunt C, Cowper D, Kressin N, & O'Brien N (2003b). Gender differences in service connection for PTSD. Medical Care, 41, 950–61. [DOI] [PubMed] [Google Scholar]
- Murdoch M, Nelson D, & Fortier L (2003c). Time, gender, and regional trends in the application for service-related post-traumatic stress disorder disability benefits, 1980-1998. Military Medicine, 168, 662–70. [PubMed] [Google Scholar]
- Murdoch M, Sayer N, Spoont M, Rosenheck R, Noorbaloochi S, Griffin J, et al. (2011). Long-term outcomes of disability benefits in US Veterans with posttraumatic stress disorder. Archives of General Psychiatry, 68, 1072–80. doi: 10.1001/archgenpsychiatry.2011.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neria Y, Bromet E, Siever S, Lavelle J, & Fochtmann L (2002). Trauma exposure and posttraumatic stress disorder in psychosis: Findings from a first-admission cohort. Journal of Consulting and Clinical Psychology, 70, 246–51. doi: 10.1111/j.1399-5618.2008.00589.x [DOI] [PubMed] [Google Scholar]
- Otto M, Perlman C, Wernicke R, Reese H, Bauer M, & Pollack M (2004). Posttraumatic stress disorder in patients with bipolar disorder: A review of prevalence, correlates, and treatment strategies. Bipolar Disorders, 6, 470–9. [DOI] [PubMed] [Google Scholar]
- Salyers M, Evans L, Bond G, & Meyer P (2004). Barriers to assessment and treatment of posttraumatic stress disorder and other trauma-related problems in people with severe mental illness: Clinician perspectives. Community Mental Health Journal, 40, 17–31. [DOI] [PubMed] [Google Scholar]
- Sareen J, Cox B, Goodwin R, & Asmundson G (2005). Co-occurrence of posttraumatic stress disorder with positive psychotic symptoms in a nationally representative sample. Journal of Traumatic Stress, 18, 313–22. [DOI] [PubMed] [Google Scholar]
- Satel S (2011). Witness testimony Hearing Transcript on Mental Health: Bridging the Gap between Care and compensation for Veterans. Washington DC: US Government Printing Office. [Google Scholar]
- Scott JD, Chant D, Andrews G, Martin GJ, & McGrath J (2007). Association between trauma exposure and delusional experiences in a large community-based sample. British Journal of Psychiatry, 190, 339–43. [DOI] [PubMed] [Google Scholar]
- Strakowski S, Keck PJ, McElroy S, Lonczak H, & West S (1995). Chronology of comorbid and principal syndromes in first-episode psychosis. Comprehensive Psychiatry, 36, 106–12. [DOI] [PubMed] [Google Scholar]
- Stroup W (2016). Generalized linear mixed models: Modern concepts, methods and applications. New York City, New York: CRC Press; 555 pp. [Google Scholar]
- Taniellian T, Jaycox L (2008). Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. Santa Monica, CA: RAND Corp; 499 pp. [Google Scholar]
- U.S. Bureau of Labor Statistics. (2014). Table 1. Employment status of the civilian noninstitutional population by disability status and selected characteristics, 2013 annual averages Economic News Release. United States Department of Labor. http://www.bls.gov/news.release/disabl.t01.htm. Accessed May 7, 2015. [Google Scholar]
- U.S. Bureau of Labor Statistics. (2015). Activity Rate: Aged 15-64: All Persons for the United States. retrieved from FRED, Federal Reserve Bank of St. Louis. https://research.stlouisfed.org/fred2/series/LRAC64TTUSQ156S. Accessed Aug. 11, 2015. [Google Scholar]
- Weissman M, Olfson M, Gameroff M, Fedler A, & Fuentes M (2001). A comparison of three scales for assessing social functioning in primary care. American Journal of Psychiatry, 158, 460–6. [DOI] [PubMed] [Google Scholar]
- Weissman M, Sholomskas D, & John K (1981). The assessment of social adjustment: An update. Archives of General Psychiatry, 38, 1250–8. [DOI] [PubMed] [Google Scholar]
- Zivin K, Bohnert A, Mezuk B, Ilgen M, Welsh D, Ratliff S, et al. (2011). Employment status of patients in the VA health system: Implications for mental health services. Psychiatric Services, 62, 35–8. doi: 10.1176/appi.ps.62.1.35. [DOI] [PubMed] [Google Scholar]


