Abstract
Cardiogenic shock from biventricular failure that requires acute mechanical circulatory support carries high 30 day mortality. Acute mechanical circulatory support can serve as bridge to orthotopic heart transplant (OHT) in selected patients. We report a patient with biventricular failure secondary to rapidly progressive cardiac sarcoidosis refractory to medical management who was bridged to OHT with Impella 5.0 and Impella RP—temporary left and right ventricular assist devices, respectively. This is the first successful bridge to transplantation using these devices in biventricular heart failure and cardiogenic shock. We discuss considerations for using this strategy over veno‐arterial extracorporeal membrane oxygenation or surgically implanted assist devices in patients with cardiogenic shock and biventricular failure as a bridge to OHT.
Keywords: Biventricular acute heart failure, Cardiogenic shock, Bridge to heart transplant, Percutaneous mechanical circulatory support, Minimally invasive mechanical circulatory support, Biventricular mechanical circulatory support, Cardiac sarcoidosis
Introduction
From 2009 to 2016, the percentage of patients bridged with mechanical devices prior to orthotopic heart transplant (OHT) was 42.9%, compared with 39.8% on inotropes.1 Treating patients with cardiogenic shock secondary to biventricular heart failure is challenging because of limited options for mechanical circulatory support that can serve as a bridge to cardiac transplantation. While the 1 year survival for durable left ventricular (LV) assist devices approaches 90%, survival for biventricular mechanical support devices is significantly lower.2 The treatment of choice remains OHT, but a significant number do not survive to transplantation. We present a case of a patient with favourable characteristics for OHT who was bridged to transplantation with Impella 5.0 and Impella RP (Abiomed, Inc, Danvers, MA), temporary minimally invasive LV and right ventricular (RV) acute mechanical support devices, respectively. This is the first known case of successful bridge to OHT using these two devices simultaneously in a patient with biventricular heart failure and cardiogenic shock. The use of biventricular Impella devices in cardiogenic shock as a bridge to recovery and LV assist device has been previously reported.3, 4, 5, 6, 7
Case report
A 67‐year‐old female presented with chest discomfort and was diagnosed with complete heart block. Transthoracic echocardiogram (TTE) showed mildly reduced LV ejection function (LVEF) of 45%. Angiogram showed no obstructive coronary disease. She underwent dual‐chamber pacemaker implantation and was discharged. Three weeks later, she presented with new heart failure symptoms. Repeat TTE showed worsened LVEF of 15% with multiple segmental wall motion abnormalities. She also developed ventricular tachycardia requiring amiodarone and lidocaine infusions. Sarcoidosis and giant cell myocarditis were considered as possible diagnoses. Cardiac magnetic resonance imaging performed 26 days after pacemaker implantation revealed marked thinning of septal myocardium, mild thinning of mid and basal inferior myocardium, and associated delayed myocardial enhancement (Figure 1 ).
Figure 1.
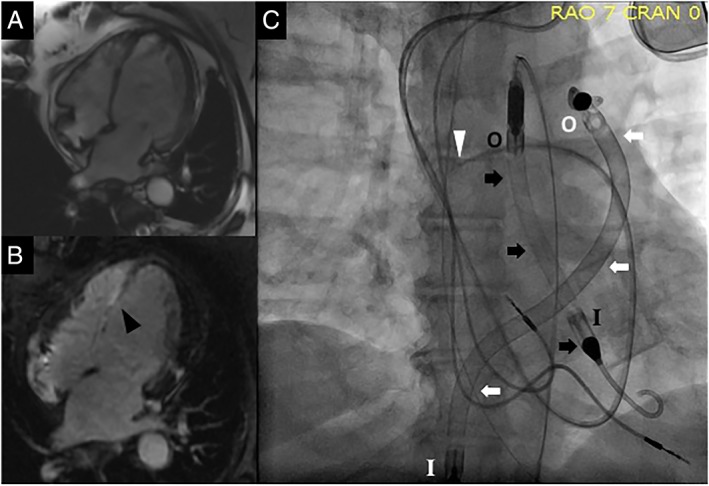
(A) Four‐chamber view on cardiac magnetic resonance imaging showing thinning of entire inter‐ventricular septum; (B) delayed contrast‐enhanced four‐chamber view on cardiac magnetic resonance imaging showing fibrosis/scarring of the inter‐ventricular septum (black arrow head); (C) fluoroscopic image showing pulmonary artery catheter (white arrow head), Impella 5.0 (black arrows), and Impella RP (white arrows). The Impella 5.0 has its inlet in the left ventricle (black ‘I’) and outlet in the ascending aorta (black ‘O’), while the Impella RP has its inlet in the inferior vena cava–right atrial junction (white ‘I’) and outlet in the pulmonary artery (white ‘O’).
She was treated empirically with methylprednisolone 1000 mg daily for 3 days. Because of cardiogenic shock and recurrent ventricular tachycardia, an intra‐arterial balloon pump (IABP) was inserted prior to transfer for consideration of advanced heart failure therapies at our institution. Endomyocardial biopsy to identify the diagnosis was considered, but this was deferred because of the patient's clinical instability. Repeat TTE showed depressed LVEF of 24%, RV systolic tissue Doppler velocity (S′) of 11.1 cm/s, and tricuspid annular plane systolic excursion of 2.0 cm. Because of a persistently low cardiac index (1.5 L/min/m2) while supported by an IABP, escalation of mechanical support was needed. Initial strategy was to surgically place an Impella 5.0 via the axillary position, but small artery size precluded this; therefore, a femoral approach was performed via surgical cut‐down. However, post‐operatively, the patient continued to decompensate, with increasing lactate and decreasing mean arterial pressures. TTE revealed newly dilated RV with septal shift towards the LV, and invasive haemodynamics revealed newly decreased pulmonary artery pulsatility index (0.9), both consistent with acute RV failure. Impella RP, which was inserted percutaneously via the R femoral vein, was chosen due to relatively short expected time to donor heart availability because of the patient's small body surface area (1.9 m2), blood type (A), and low panel‐reactive antibody score (0%). The Impella 5.0 and Impella RP were set to deliver estimated 4.0–4.5 L/min and 4.0 L/min flow, respectively. Cardiac index improved to 2.4 L/min/m2 after biventricular mechanical support. Post‐operatively, she suffered severe vasoplegia, which resolved with intravenous methylene blue. She continued to receive intravenous diuresis and was extubated after 5 days of biventricular mechanical support, but she remained bedbound because of femoral biventricular Impella cannulation. She ultimately waited 20 days before undergoing OHT with surgical decannulation of the primary devices from the femoral artery and vein. There were no complications from the Impella devices; prior to transplantation, the patient did not require any blood transfusion, and the Impella devices did not require replacement. The patient was discharged from the hospital 3 weeks after transplantation and went home after inpatient rehabilitation. She is thriving over 12 months post‐transplant with normal functional capacity. Histology of the explanted heart revealed biventricular cardiac sarcoidosis.
Discussion
For patients with biventricular heart failure and cardiogenic shock refractory to pharmacologic therapy, bridging options while waiting for OHT are limited. Surgical approaches include Total Artificial Heart (SynCardia Systems, Inc, Tucson, AZ) and centrally cannulated, extracorporeal pumps such as CentriMag (Thoratec, Pleasanton, CA). Durable ventricular assist devices implanted into the LV and RV as a bridge to transplantation have also been previously reported.8 Advantages include high flows, durability, and possibility of ambulation. Disadvantages include need for sternotomy, bleeding risk, mediastinal adhesions, and prolonged intubation. Minimally invasive options include veno‐arterial extracorporeal membrane oxygenation (VA‐ECMO), biventricular TandemHeart (CardiacAssist, Inc, Pittsburgh, PA), and biventricular Impella devices. Advantages include potentially less peri‐procedural morbidity, less need for volume resuscitation, less bleeding, and fewer transfusions than with surgically implanted circulatory support. VA‐ECMO has the least durability predominantly because of the need for LV unloading, requiring concurrent IABP or LV Impella. Ambulation is not possible with approaches that involve femoral cannulation, which is required for Impella RP—a significant limitation for patients expected to wait for OHT for an extended period. In patients with Impella 5.0 support who then demonstrate acute RV failure, escalation with Impella RP may be a reasonable initial approach. If biventricular support with Impella devices is inadequate or complications arise, emergent transition to surgically implanted devices may be required. At our centre, if we anticipate OHT within 1 week, VA‐ECMO or biventricular Impella devices are considered. For appropriate patients who will likely wait up to 1 month, we consider biventricular Impella devices for temporary support. If we expect longer waiting times, biventricular CentriMags and Total Artificial Heart are main options. Capability to transition emergently to other forms of biventricular mechanical support is needed if Impella devices provide inadequate support or complications, such as major bleeding, pump thrombosis, and pump failure, arise. In summary, we report the first‐in‐the‐world biventricular Impella support for a patient with severe biventricular failure who was successfully bridged to OHT.
Conflict of interest
E.S. receives speaking honoraria from Abiomed, Inc (Danvers, MA).
All other authors report no conflict of interest.
Varian, K. , Xu, W. D. , Lin, W. , Unai, S. , Tong, M. Z. , Soltesz, E. , Krishnaswamy, A. , Kapadia, S. , Feitell, S. , Hanna, M. , Joyce, E. , Schoenhagen, P. , Starling, R. C. , Taylor, D. O. , and Perez, A. L. (2019) Minimally invasive biventricular mechanical circulatory support with Impella pumps as a bridge to heart transplantation: a first‐in‐the‐world case report. ESC Heart Failure, 6: 552–554. 10.1002/ehf2.12412.
References
- 1. Lund LH, Khush KK, Cherikh WS, Goldfarb S, Kucheryavaya AY, Levvey BJ, Meiser B, Rossano JW, Chambers DC, Yusen RD, Stehlik J. International Society for Heart and Lung Transplantation. The Registry of the International Society for Heart and Lung Transplantation: thirty‐fourth adult heart transplantation report—2017; focus theme: allograft ischemic time. J Heart Lung Transplant 2017; 36: 1037–1046. [DOI] [PubMed] [Google Scholar]
- 2. Kirklin JK, Pagani FD, Kormos RL, Stevenson LW, Blume ED, Myers SL, Miller MA, Baldwin JT, Young JB, Naftel DC. Eighth annual INTERMACS report: special focus on framing the impact of adverse events. J Heart Lung Transplant 2017; 36: 1080–1086. [DOI] [PubMed] [Google Scholar]
- 3. Kamioka N, Patel A, Burke MA, Greenbaum A, Babaliaros V. Biventricular Impella placement via complete venous access. Catheter Cardiovasc Interv 2017. doi: 10.1002/ccd.27103 [DOI] [PubMed] [Google Scholar]
- 4. Kuchibhotla S, Esposito ML, Breton C, Pedicini R, Mullin A, O'Kelly R, Anderson M, Morris DL, Batsides G, Ramzy D, Grise M, Pham DT, Kapur NK. Acute biventricular mechanical circulatory support for cardiogenic shock. J Am Heart Assoc 2017; 6: e006670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chiu CY, Hättasch R, Praeger D, Knebel F, Stangl K, Ramirez ID, Dreger H. Percutaneous biventricular Impella support in therapy‐refractory cardiogenic shock. Heart Lung 2018; 47: 250–252. [DOI] [PubMed] [Google Scholar]
- 6. Pappalardo F, Scandroglio AM, Latib A. Full percutaneous biventricular support with two Impella pumps: the Bi‐Pella approach. ESC Heart Fail 2018; 5: 368–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lasa JJ, Castellanos DA, Denfield SW, Dreyer WJ, Tume SC, Justino H, Qureshi AM. First report of biventricular percutaneous Impella ventricular assist device use in pediatric patients. ASAIO J 2018; 64: e134–e137. [DOI] [PubMed] [Google Scholar]
- 8. Garg V, Tan W, Ardehali R, Shah J, Huynh T, Aksoy O. Giant cell myocarditis masquerading as orbital myositis with a rapid, fulminant course necessitating mechanical support and heart transplantation. ESC Heart Fail 2017; 4: 371–375. [DOI] [PMC free article] [PubMed] [Google Scholar]


