Abstract
Low-intensity extracorporeal shockwave therapy (Li-ESWT) has been reported as a useful and noninvasive treatment for erectile dysfunction (ED). Systematic review and meta-analysis are utilized to evaluate the efficacy of Li-ESWT by comparing the changes in the International Index of Erectile Function erectile function domain (IIEF-EF) and the Erection Hardness Score (EHS) versus sham therapy in men with ED. A systematic search of the MEDLINE, EMBASE, ClinicalTrials.gov, CBM, CNKI, WANGFANG, and VIP was conducted to obtain randomized controlled trials (RCTs) published in peer-reviewed journals or presented in abstract forms of Li-ESWT for ED treatment from January 2010 to June 2018. If RCTs are published in peer-reviewed literature and IIEF-EF scores and EHS are used to assess erectile function outcomes, they are eligible for inclusion. A meta-analysis was used to summarize the estimates. The meta-analysis included seven RCTs involving 522 participants. The data revealed that men treated with Li-ESWT showed significant improvement in pooled mean IIEF-EF scores from baseline to follow-up compared with sham therapy (MD: 1.99 points; 95% CI [1.35, 2.63]; p < .00001). Changes in the IIEF-EF score increased significantly in the treatment group (MD: 3.62; 95% CI [2.99, 4.25]; p < .00001). The EHS increased significantly in the treatment group in four studies (OR: 16.02; 95% CI [7.93, 32.37]; p < .00001). Patients with moderate and/or severe ED reported better results in mean IIEF scores (MD: 3.95; 95% CI [2.44, 5.46]; p < .00001). In meta-analysis of seven RCTs with men who received Li-ESWT for ED, there was evidence that the IIEF-EF and EHS experienced improvements following Li-ESWT.
Keywords: Erectile dysfunction, low-intensity extracorporeal shock waves, meta-analysis, IIEF-EF, EHS
Erectile dysfunction (ED) is a common disease around the world, which is defined as the inability of men to acquire or maintain an erection in order to achieve satisfactory sexual performance, with the course of disease lasting for more than 3 months (Wessells, Joyce, Wise, & Wilt, 2007). The incidence of ED is increasing by the increase of age and comorbid conditions. A study reported that the incidence of ED in the population was around 20% (Hatzimouratidis et al., 2010). Phosphodiesterase type 5 inhibitor (PDE5is) is currently widely used and the most effective treatment for patients with ED. Some patients are not responding to the drug for various reasons (Smith et al., 2013), and often offered other treatments, such as intracorporal injection, penile prosthesis implantation, and so forth (Hatzimouratidis et al., 2010). These methods are used as second-line or even third-line options, while the frequency of long-term use is still affected by side effects and complications (Mulhall et al., 1999). They are powerless for potential pathophysiology of ED (Feldman, Goldstein, Hatzichristou, Krane, & McKinlay, 1994).
In 2010, Vardi, Appel, Jacob, Massarwi, and Gruenwald (2010) first reported the use of low-intensity extracorporeal shockwave therapy (Li-ESWT) in the treatment of ED; before that, the method had been proved to improve vascular function in other experiments, and, the method was tolerable and effective, indicating the physiological effects on cavernous hemodynamics. After 8 years of long-term clinical observation, Li-ESWT has gradually become a therapeutic option by physicians in ED treatment.
Lu et al. (2017) and (Clavijo, Kohn, Kohn, & Ramnsamy, 2017) completed their meta-analyses about the effect of Li-ESWT in treating ED in 2016 and published their articles the following year. Since then, some new and high-quality randomized controlled trails (RCTs) about Li-ESWT on ED treatment had been published in the past 2 years. More and more countries have gradually carried out this treatment in clinic, which leads to a large amount of new clinical evidence that needs to be reassessed to explore whether Li-ESWT can improve the International Index of Erectile Function erectile function domain (IIEF-EF) and the Erection Hardness Score (EHS) in patients with ED. A systematic review and meta-analysis have been performed about the topic of Li-ESWT in treating ED in which the IIEF-EF and EHS were assessed and compared with sham therapy, seven RCTs were included to the meta-analysis.
Methods
Search Strategy
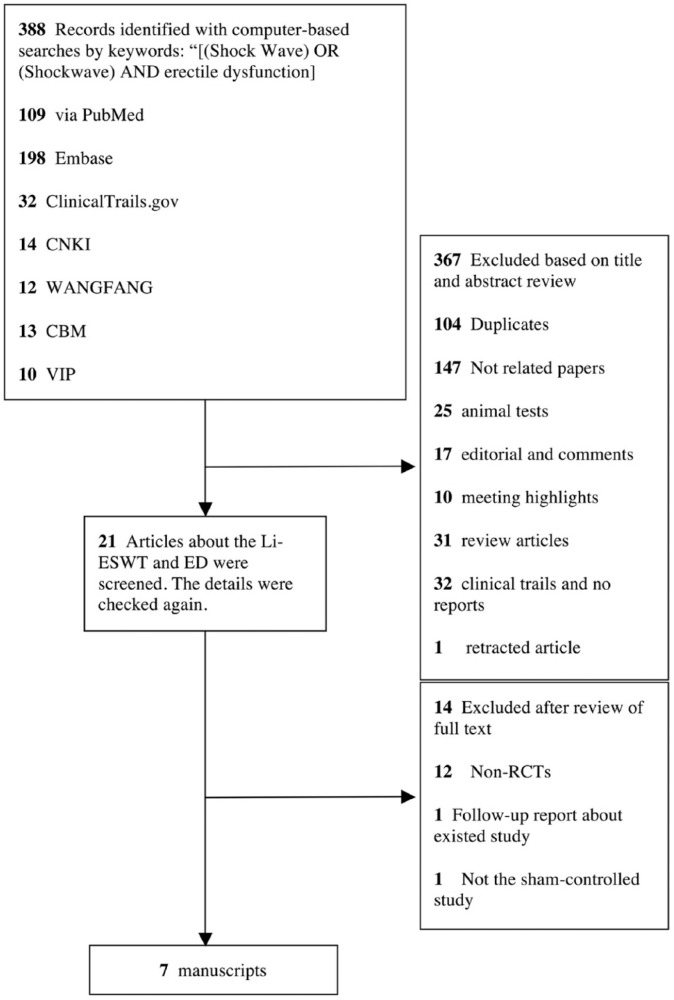
The electronic databases of MEDLINE, EMBASE, Clinicaltrails.org., China National Knowledge Infrastructure Database (CNKI), Wan fang Database, China Biology Medicine Database (CBM), VIP Science Technology Periodical Database, and Cochrane library were retrieved; related articles were collected and selected from January 2010 to June 2018. The search terms used through the internet were: “[(Shock Wave) OR (Shockwave) AND erectile dysfunction].” This systematic retrospective and meta-analysis is carried out in strict accordance with the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Moher, Liberati, Tetzlaff, & Altman, 2009). Since the purpose of meta-analysis is to summarize previous studies, ethical approval and informed consent are not necessary. A flow diagram for study selection is presented in Figure 1.
Figure 1.
Flow diagram for study selection.
Inclusion Criteria and Trial Selection
The studies included must be RCTs about Li-ESWT on the treatment of ED, and the IIEF-EF, EHS, or other indexes were necessary for the assessment of the disease. There were no restrictions on language of publication, minimum number of patients in the study, use of PDE5is during the treatment period, and the severity of the disease. Only the largest or recently studies were included when similar patients and same methods used. The exclusion criteria of trails were: articles unrelated to the analysis, lack of essential information on patients or intervention measures of the treatment, nonoriginal research, reviews, comments, cohort studies, animal models, and case reports.
Data Extraction
Related data in the included articles were extracted independently by three investigators (Liang Dong, Yali Yang, Shanshan Yong) according to the PRISMA statement, and all discrepancies were resolved through adjudication and discussion by other reviewers. The words in abstracts such as “randomized” or “quasi-randomized” were used in all studies, regardless of whether they were blind or not. For each study, the following information were extracted: first author’s name, year of publication, publication type, practice setting, duration of follow-up, population, model of Li-ESWT machine, evaluation tools for ED (IIEF-EF, EHS, the others), sample size, mean or median participant age, and participant inclusion and exclusion criteria.
Quality Assessment
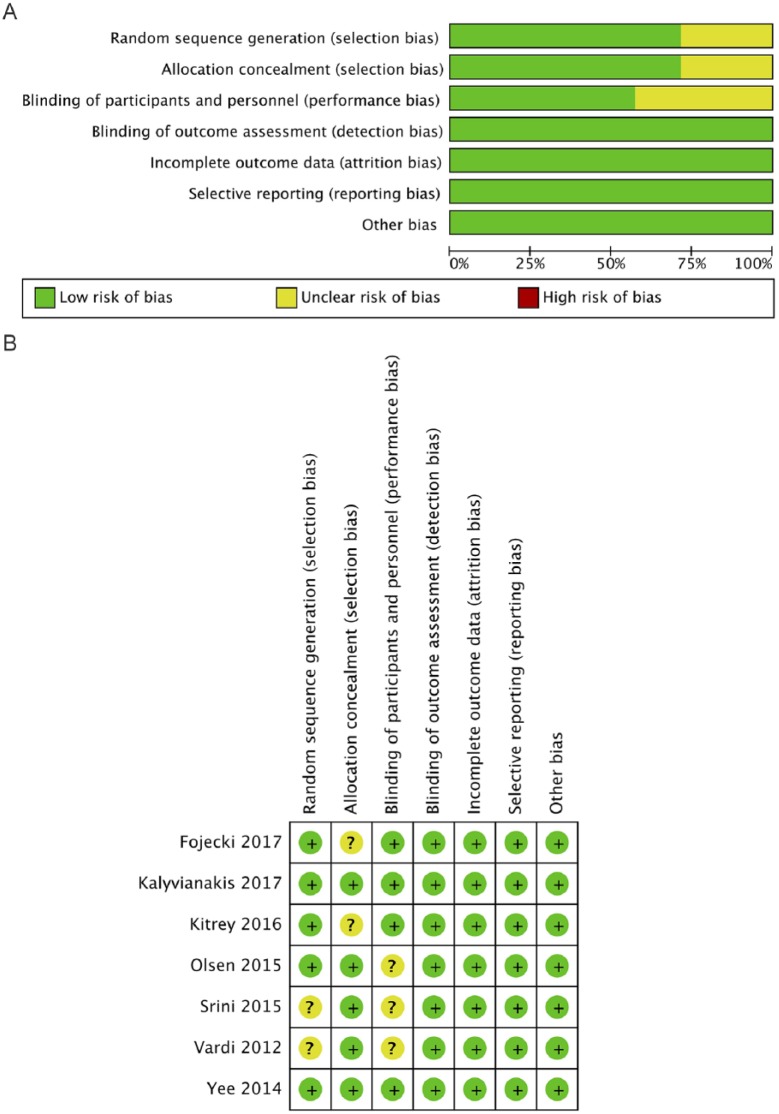
The quality of the RCTs was evaluated by the Cochrane Risk of Bias Assessment tool. The items of randomization, method to generate the sequence of randomization, randomization concealment, blinding, results data integrity, selective outcome reports, and other potential bias sources were assessed (Higgins & Green, 2011). Graph and summary about risk of bias were produced with RevMan 5.3. (Review Manager, 2014). All the domains were independently assessed by three trained investigators (Liang Dong, Yali Yang, Shanshan Yong). All the disputes were resolved by a fourth professional reviewer through discussion and adjudication.
Data Synthesis and Analysis
The average IIEF-EF and EHS scores measured before and after treatment with Li-ESWT or sham therapy in each study were calculated. Statistics analyses were estimated with RevMan 5.3 and Stata/SE 14.1. Statistical tests were two-sided and used p value less than .05 as a significance threshold. The Egger test and Funnel plot were used for investigating publication bias to small study effects (Egger, Smith, Schneider, & Minder, 1997; Sterne & Egger, 2001). Sensitivity analysis was conducted by continuously excluding the impact of individual studies on overall aggregated estimates (Viechtbauer, 2010). The heterogeneity between studies was assessed by standard X2 test and I2 statistics (Higgins, Thompson, Deeks, & Altman, 2003). If heterogeneity existed (p < .05), data were analyzed using a random effects model or a fixed-effects model (Borenstein, Hedges, Higgins, & Rothstein, 2010).
Results
Study Characteristics
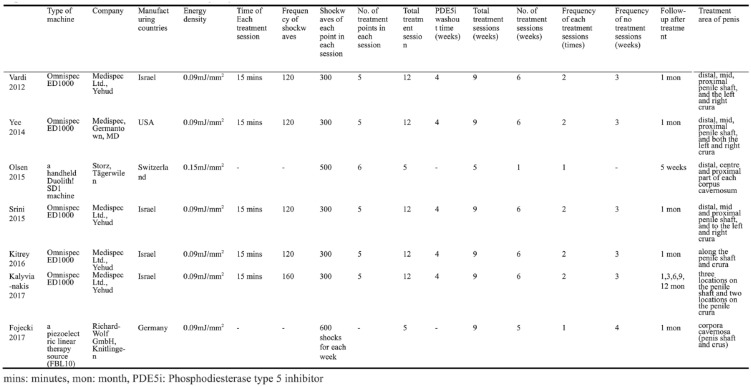
The meta-analysis included seven RCTs involving 522 participants (see Table 1). Five clinical studies used Omnispec ED1000 (Medispec Ltd., Yehud, Israel), and the remaining two used a piezoelectric linear therapy source (FBL10, Richard-Wolf GmbH, Knitlingen, Germany), and Li-ESWT equipment and a handheld Duolith® SD1 machine (Storz, Tägerwilen, Switzerland), respectively. Figure 2 represents how the main machines used in the majority of the studies work. All the seven studies were RCTs, while the control group received sham therapy with shock wave probes, which looked and sounded similar to active therapy probes. All the studies indicated that the patients included had vasculogenic ED or called organic ED. The study by Kitrey et al. (2016) included patients with moderate and severe ED who also took PDE5is during the Li-ESWT process. Three studies by (Kalyvianakis et al., 2017; Olsen, Persiani, Boie, Hanna, & Lund, 2015; Srini, Reddy, Shultz, & Denes, 2015) included patients with mild to moderate, moderate, and severe ED. The remaining three studies did not specify the severity of the disease. Five studies were conducted in Europe and two in Asia. Five studies treated the patients twice a week for 3 weeks, then without treatment for 3 weeks, followed by 3 weeks of the same treatments, a total of 18,000 treatments shocks (energy flux density = 0.09 mJ/mm2, frequency = 5 Hz). One study executed the treatment once a week for 5 weeks, followed by no treatment for 5 weeks, with 3,000 shocks (energy flux density = 0.15 mJ/mm2, frequency = 5 Hz) each time, leading to 15,000 treatments shocks in total. The last study was designed such that each participant received a round of five weekly treatment sessions with a 4-week interval, with 600 shockwaves (energy flux density = 0.09 mJ/mm2, frequency = 5 Hz) for each session; therefore, a total of 3,000 shockwaves were delivered in 9 weeks. IIEF-EF scores were taken as the main results in all the seven experimental studies, but only six studies of the IIEF-EF indicators could be calculated and then for meta-analysis. Five studies reported the results of EHS, and the data can be used for meta-analysis. All the seven studies were published in journals. RevMan 5.3, developed by Cochrane Collaboration, was used to assess the quality of the study and the risk of bias. In most studies, the risk of bias was low (see Figure 3).
Table 1.
Characteristics of the Included Study of Li-ESWT for ED Patients.
| Study | Year | Country | Follow-up | Weeks of treatment | No. of shocks per treatment | Total shocks | Sample | IIEF-EF score before treatment | Change in IIEF-EF score | EHS | Type of ED | Type of machine | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| treatment | control | treatment | control | treatment | control | treatment | control | |||||||||
| Vardi, Appel, Kilchevsky, and Gruenwald (2012) | 2012 | Israel | 1mo | 9 | 1500 | 18000 | 40 | 20 | 12.6 ± 0.75 | 11.5 ± 0.86 | 6.7 | 3.0 | 31 | 7 | vasculogenic ED | Omnispec ED1000 |
| Yee et al. (2014) | 2014 | China | 4wks | 9 | 1500 | 18000 | 30 | 28 | 10.2 ± 3.8 | 10.2 ± 3.8 | 5.3 ± 5.5 | 3.8 ± 3.6 | - | - | vasculogenic ED | Omnispec ED1000 |
| Olsen et al. (2015) | 2015 | Denmark | 5wks | 5 | 3000 | 15000 | 51 | 54 | - | - | - | - | 29 | 5 | vasculogenic ED | Storz |
| Srini et al. (2015) | 2015 | India | 12mos | 9 | 1500 | 18000 | 60 | 17 | 9.5 | 9.2 | 12.5 | 1.4 | 47 | 0 | vasculogenic ED | Omnispec ED1000 |
| Kitrey et al. (2016) | 2016 | Israel | 4wks | 9 | 1500 | 18000 | 37 | 18 | 7(IQR) | 8(IQR) | 5 | 0 | 20 | 0 | vasculogenic ED | Omnispec ED1000 |
| Kalyvianakis and Hatzichristou (2017) | 2017 | Greece | 12mos | 9 | 1500 | 18000 | 30 | 16 | 13.8 ± 3.6 | 14.6 ± 3.4 | 18.46 ± 3.6(1m) | 16.43 ± 3.5(1m) | - | - | vasculogenic ED | Omnispec ED1000 |
| Fojecki et al. (2017) | 2017 | Denmark | 4wks | 9 | 600 | 3000 | 58 | 63 | 10.9 | 11.5 | 2.2 | 2.5 | - | - | vasculogenic ED | FBL10 |
Note. Li-ESWT = low-intensity extracorporeal shockwave therapy; IIEF-EF = International Index of Erectile Function erectile function domain; ED = erectile dysfunction; EHS = Erection Hardness score; IQR = interquartile range; mo = month; wk = week.
Figure 2.
How main machines used in the majority of the studies work to exert their effects.
Figure 3.
Seven randomized controlled trials included in our meta-analysis. Quality of studies was assessed with the Cochrane Collaboration’s tool (A: Risk of bias graph; B: Risk of bias summary).
Effect of Li-ESWT on Mean IIEF-EF Score
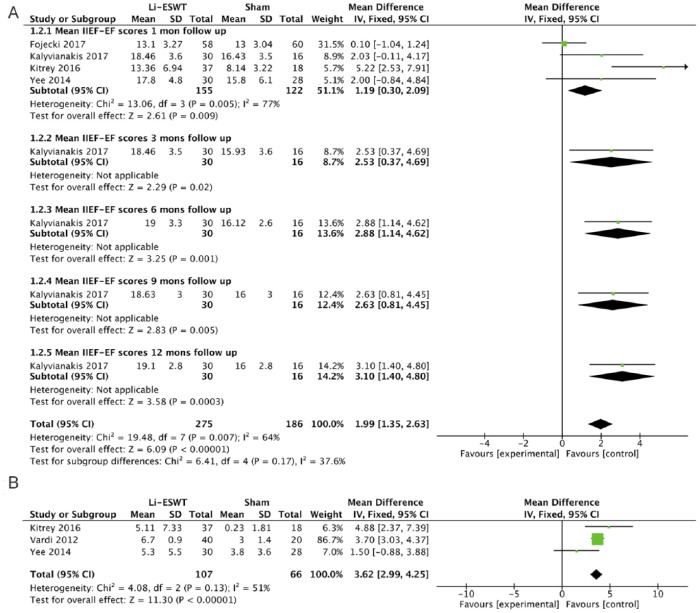
The studies by (Fojecki, Tiessen, & Osther, 2017), Kalyvianakis and Hatzichristou (2017), and Yee, Chan, Hou, and Ng (2014) concluded that the IIEF did not increase significantly in the treatment group compared with the control group in the 1-month follow-up, while Kitrey et al. (2016) reported that the IIEF increased significantly in the Li-ESWT group compared with the control group. The meta-analysis of the data revealed that IIEF scores in Li-ESWT group were significant improved compared with the sham therapy in the 1-month follow-up (MD: 1.19 points; 95% CI [0.30, 2.09]; I2 = 77%, p = .009). In addition, subgroup analysis was performed. According to the follow-up records of 3, 6, 9, and 12 months, Kalyvianakis and Hatzichristou (2017) indicated that IIEF scores had increased significantly in the Li-ESWT group. The overall meta-analysis of the data revealed that men treated with Li-ESWT showed significant improvement in pooled mean IIEF-EF scores from baseline to follow-up compared with sham therapy (MD: 1.99 points; 95% CI [1.35, 2.63]; I2 = 64%, p < .00001; see Figure 4A). Subsequently, sensitivity analyses were presented. The result demonstrated that two studies—Fojecki et al. (2017) and Kitrey et al. (2016)—were identified to affect the overall prevalence estimate by an absolute difference of 0.5 point (Table 2A).
Figure 4.
Clinical outcomes of meta-analysis on the IIEF-EF score (A: Mean IIEF-EF score; B: Change of IIEF-EF score.).
Table 2.
Sensitivity Analysis
A. Sensitivity Analysis of the Mean IIEF-EF Scores Data.
| Study | Mean Difference | Lower CI | Upper CI | p | I 2 |
|---|---|---|---|---|---|
| Omitting Fojecki et al. (2017) | 2.94 | 1.50 | 4.39 | <.0001 | 48 |
| Omitting Kalyvianaki and Hatzichristou (2017) | 1.02 | 0.03 | 2.00 | .04 | 84 |
| Omitting Kitrey et al. (2016) | 0.69 | −0.26 | 1.64 | .15 | 40 |
| Omitting Yee et al. (2014) | 1.10 | 0.16 | 2.05 | .02 | 84 |
Note. CI = confidence interval.
B. Sensitivity Analysis of Change in IIEF-EF Scores Data.
| Study | Mean Difference | Lower CI | Upper CI | p | I 2 |
|---|---|---|---|---|---|
| Omitting Kitrey et al. (2016) | 3.54 | 2.89 | 4.18 | <.00001 | 67 |
| Omitting Vardi et al. (2012) | 3.1 | 1.38 | 4.83 | .0004 | 73 |
| Omitting Yee et al. (2014) | 3.78 | 3.13 | 4.43 | <.00001 | 0 |
Note. CI = confidence interval.
C. Sensitivity Analysis of the Severity of ED Data.
| Study | Mean Difference | Lower CI | Upper CI | p | I 2 |
|---|---|---|---|---|---|
| Omitting Yee et al. (2014) | 3.27 | 1.60 | 4.95 | .07 | 70 |
| Omitting Kalyvianakis and Hatzichristou (2017) | 5.84 | 3.71 | 7.97 | <.00001 | 0 |
| Omitting Kitrey et al. (2016) | 3.36 | 1.53 | 5.19 | .0003 | 81 |
Note. CI = confidence interval.
Effect of Li-ESWT on Change in IIEF-EF Score
Changes in IIEF-EF scores were provided in three studies (Kitrey et al., 2016; Vardi et al., 2012; Yee et al., 2014), and these date were extracted and analyzed, and the results suggested that the change in the IIEF-EF score increased significantly in the treatment group compared with the control group (MD: 3.62 points; 95% CI [2.99, 4.25]; I2 = 51%, p < .00001; see Figure 4B). Subsequently, the sensitivity analyses were presented. The result demonstrated that Yee et al. (2014) was identified as affecting the overall prevalence estimate by an absolute difference of 0.5 point (Table 2B).
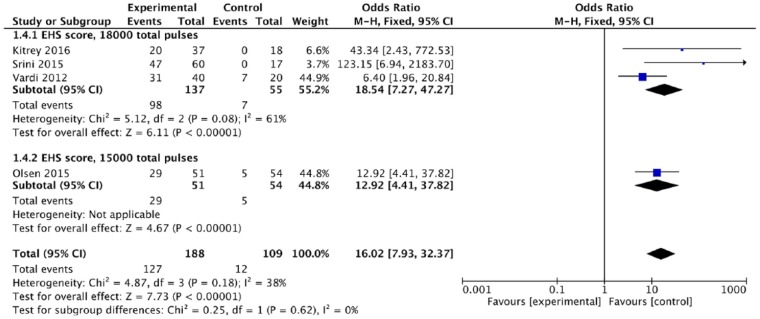
Effect of Li-ESWT on EHS Score
The EHS data could be extracted from four RCTs. The scores increased significantly at 1 month after Li-ESWT in all four studies (OR: 16.02; 95% CI [7.93, 32.37]; I2 = 38%, p < .00001). The total number of shockwaves in the study by Olsen et al. (2015) was 15,000 while in the other three studies, it was 18,000 (Kitrey et al., 2016; Srini et al., 2015; Vardi et al., 2012). These results indicated that Li-ESWT improved the EHS of the penis in ED patients, irrespective of the number of shockwaves (Figure 5).
Figure 5.
Clinical outcomes of meta-analysis on the EHS score.
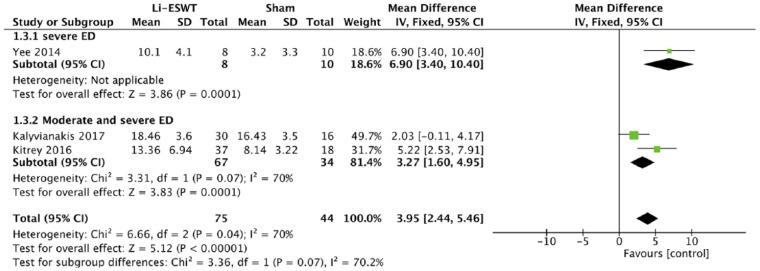
Effect of Li-ESWT on Severity of ED
Only three studies included patients with moderate to severe ED. Other studies did not classify the disease by severity. In the study of Yee et al. (2014), IIEF-EF scores were reported in severe ED patients after treatment, while scores of both severe and moderate ED patients had been reported by Kitrey et al. (2016) and Kalyvianakis and Hatzichristou (2017). IIEF-EF scores increased significantly in the treatment group compared with the control group (MD: 3.95 points; 95% CI [2.44, 5.46]; I2 = 70%, p < .00001; Figure 6). Subsequently, the sensitivity analyses were presented. The result demonstrated that Kalyvianakis and Hatzichristou’s (2017) study was identified as affecting the overall prevalence estimate by an absolute difference of 0.5 point (Table 2C).
Figure 6.
Clinical outcomes of meta-analysis on the severity of ED.
Assessment of Publication Bias
Although less than 10 studies were included in this meta-analysis, funnel plots were drawn and Egger’s and Begg’s tests were conducted for the assessment of publication bias. The asymmetry is minimal by naked eye examination of funnel plots in the mean IIEF-EF score and EHS, which indicates that the pooled estimates were unlikely to produce significant bias secondary to small study effects. The Egger’s test and Begg’s test supported this finding (mean IIEF-EF score: z = 1.02, p = .076; EHS: z = 1.36, p = .149). All the included studies in this meta-analysis were of a small scale, and reported an improvement during treatment, that is, few publication biases existed.
Discussion
Li-ESWT, a new therapeutic method for ED, has been increasingly adopted by both doctors and patients in the past 10 years. This systematic review and meta-analysis of seven RCTs involving 522 men demonstrated a statistical improvement in the IIEF-EF score and EHS using Li-ESWT. In the past 5 years, clinical studies and articles on this item have increased dramatically, especially in 2015. And the result of this review indicates that Li-ESWT might clinically improve erectile function in men with ED.
In this review, some studies reported that the therapeutic effect of Li-ESWT group was slightly better than that in the control group, indicating that some patients in the control group had a certain placebo effect (Fojecki et al., 2017; Yee et al., 2014).
Measurement tools that are validated and widely accepted such as the IIEF and EHS are used in this meta-analysis. It is realized that the IIEF-EF score assessment is a completely subjective indicator. The IIEF-EF score is a generally acknowledged and most important index for evaluating erectile function, which is a validated six-question questionnaire that assesses erection frequency, erection firmness, penetration ability, maintenance frequency, maintenance ability, and erection confidence on a scale of 0 to 5 (Clavijo et al., 2017; Rosen et al., 1997).
The treatment of vasculogenic ED with Li-ESWT is based on the indication of penis cavernous artery flow by color Doppler ultrasonography and is reliant on the timely response of injected vasoactive agents (Vardi et al., 2012). At present, there are no objective physiological parameters for evaluating the effectiveness of shockwave therapy (SWT) on ED in the world. Because of the differences of race, religion, and culture, there is no uniform standard for objective physiological parameters, which is not applicable to all groups of people. In view of the fact that the IIEF can intuitively reflect the erectile condition of the patient and accurately assess the sexual life of spouses, this become a widely accepted method of assessing erectile function worldwide. The same principle applies to the EHS, which is a scoring system that divides erectile hardness into four different degrees.
In this meta-analysis, the range of improvement in the IIEF-EF score in the Li-ESWT group changes from 2.1 to 7.4. It is undeniable that some studies report that the improvement is neither statistically significant nor necessarily of significant clinical value. It is well known that the minimal clinically significant difference (MCID) of the IIEF can better evaluate the real clinical efficacy of Li-ESWT. One study has reported that the change of 4 points in the IIEF-EF score is the MCID in clinic, which suggests that there may be clinical differences and potential changes in management for patients (Rosen, Allen, Ni, & Araujo, 2011). The use of MCID in the IIEF-EF was recommended as an accurate and meaningful tool for evaluating Li-ESWT treatment in the future.
Previous studies have revealed that Li-ESWT could significantly improve blood supply, but the underlying mechanism still been unclear. All the patients in this meta-analysis included researches were diagnosed as vasculogenic ED. In vitro and animal studies have identified that SWT could promote the formation of neovascularization in tissues. With the increase of angiogenesis biomarkers, the tissues can be redistributed (Holfeld et al., 2016; Wang et al., 2003; Yan, Zeng, Chai, Luo, & Li, 2008). One study has shown that this effect was mainly related to cell proliferation, tissue regeneration, and angiogenesis (Li et al., 2016). Animal models with diabetic ED were also treated by Li-ESWT in some studies; the phenomenon of regeneration occurs in endothelial cells and smooth muscle, and erectile function was shown to improve (Liu et al., 2013; Qiu et al., 2013). Whether it is related to neuronal nitric oxide synthase (nNOS) or not is controversial (Assaly-Kaddoum et al., 2016; Qiu et al., 2013). In 2013, Siegfried et al. reported that Li-ESWT could stimulate the regeneration of damaged nerve fibers. Its potential mechanism was neovascularization by regenerated nerves, which is associated with VEGF and transforming growth factor B (Mense & Hoheisel, 2013). Li et al. reported that the erectile function as well as the penile blood vessels and nerve tissue demonstrated improved by Li-ESWT in rats with pelvic nerve and blood vessel injury (Li et al., 2016). It is speculated that microvascular regeneration and improvement of penile hemodynamics are the basic mechanism of therapeutic efficacy of SWT (Pan, Raees, & Kovac, 2016).
During the process of data extraction, it was found that one study by Kitrey et al. (2016) reported data neither on mean IIEF-EF score nor on the change in the IIEF-EF nor on the change in the number of patients before and after treatment. Instead, it provided data such as interquartile range (IQR), median of the sample, and size of the sample. For consistency and comparability of statistical data, the method provided by researchers was used to estimate the sample mean and standard deviation (SD; Hozo, Djulbegovic, & Hozo, 2005; Luo, Wan, Liu, & Tong, 2018; Wan, Wang, Liu, & Tong, 2014). Fortunately, web page versions through web links (http://www.comp.hkbu.edu.hk/~xwan/median2mean.html) have been provided, and the results could be obtained by inserting the data directly. The purpose of doing so was to make better use of the data provided by the study and it could reflect the effect of Li-ESWT more objectively.
Three similar articles about this topic have been published up to now (Clavijo et al., 2017; Lu et al., 2017; Man & Li, 2018). Patients with ED, chronic pelvic pain syndrome (CPPS), and Peyronie’s disease (PD), or even ED after radical prostatectomy (RP) were included in the meta-analyses published by Lu et al. (2017) and Man and Li (2018). This would lead to the existence of a heterogeneous population. In addition, the two meta-analyses included both RCTs and cohort studies. With the inclusion of cohort studies, the authors presented their results at a level of 2A evidence. A mistake of the included data in the meta-analysis was found. Lu et al. (2017) and Man and Li (2018) had regarded the baseline data of the study by Vardi et al. as the outcome after Li-ESWT treatment, and it would lead to some deviation in the meta-analyses as well. The meta-analysis by Clavijo et al. (2017) was the first to publish on a homogenous population of men only with ED, and it included only RCTs which could be regarded as level 1A evidence. But only the change in IIEF-EF scores was analyzed in this article; no analysis of other types of data or further subgroup was undertaken. Two abstracts were included in the study by Clavijo et al. (2017), and the full texts have been published by now, but some data were slightly different from the previous abstracts. Although there were some minor problems, their pioneering work was of great value. Since this article is not the first to report a systematic review and meta-analysis about Li-ESWT for ED, this study differs in the following aspects. The patients included were diagnosed with ED without any comorbidity, the type of studies were RCTs with sham therapy, all studies had been published in full text, and the data were loyal to original research, including the mean IIEF-EF score, the change in the IIEF-EF score, and the EHS. There are also some limitations in this meta-analysis, such as the small samples of most researches; the largest sample size is 122 male patients (Fojecki et al., 2017). Though all the studies in this review were RCTs, there were some shortcomings. The basic factors for evaluating the quality of the study include randomized details, double-blind implementation, treatment details, and long-term follow-up data. As shown in the risk of bias summary, it was found that some RCTs did not accurately describe the details of randomization or blinding, and the potential bias involved was not clear, which may cause errors in the interpretation of the meta-analysis. In the review, five studies clearly reported that no PDE5i used during the therapeutic period (Olsen et al., 2015), or there was a period of washout time stage before entering the experiment (Kalyvianakis, & Hatzichristou, 2017; Srini et al., 2015; Vardi et al., 2012; Yee et al., 2014). Only Kitrey et al. (2016) reported PDE5i usage in the last 2 weeks of the treatment cycle during the SWT phase. No information about the usage of PDE5i was presented in the last study (Fojecki et al., 2017). In this study, there were increased heterogeneities in mean the IIEF-EF score statistics (I2 = 77%), which can be attributed to two studies (Fojecki et al., 2017; Kitrey et al., 2016) according to the presented sensitivity analysis, affected the overall prevalence estimate to change by more than 0.5 point. The possible reasons for the heterogeneity might be the different therapeutic regimen and patient selection. The former one could explain the heterogeneity of the study by Fojecki et al. (2017) in which a total of 3,000 treatment shocks were conducted for 9 weeks; the presence of heterogeneity can be explained by the different treatment regimen. The other studies used 15,000 shocks or 18,000 shocks in total. With the least number of shocks, Fojecki et al. (2017) reported a worsened effect in the treatment. Patient selection may be the reason for the better average therapeutic effect in Kitrey et al.’s study. The patients included had vasculogenic ED with moderate and severe levels of severity; these two categories may be more responsive to the Li-ESWT treatment. Omitting the above two studies by Kitrey et al. (2016) and Fojecki et al. (2017) separately and together, the heterogeneity decreased (I2 = 40%, I2 = 48%, I2 = 0%, respectively). In addition, there were increased heterogeneities in the change in the IIEF-EF score statistics (I2 = 51%) and severity of ED (I2 = 70%), which can be attributed to Yee et al. (2014) and Kalyvianakis and Hatzichristou (2017), respectively. As seen from Figure 2, the machine, total shocks, shock intensity, treatment frequency, and treatment area in the original studies of the two groups of meta-analysis were the same. The difference is that Yee et al. (2014) and Kalyvianakis and Hatzichristou (2017) showed no significant increase in the IIEF score (95% CI [–0.88, –3.88]) and (95% CI [–0.11, –4.17], respectively). This may be the main cause of heterogeneities; no other reasons were found.
In this article, Li-ESWT with different shocks, intensities, and lengths of treatment for ED were not yet analyzed, because there was no enough consistent data in the original literature for meta-analysis. Lu et al. (2017) had found that in men with ED or Peyronie’s disease, more shock waves reported a significant increase in the IIEF compared with the studies delivering fewer shock waves and it did not reach statistical significance between different shock wave intensities. Surprisingly, treatment course of <6 weeks reported a significant increase in the IIEF than a 9-week treatment. In summary, lower energy density, increased number of pulses, and shorter treatment courses of <6 weeks resulted in better therapeutic efficacy (Lu et al., 2017). In the upcoming studies, some recommendations that should be put forth: Studies should be randomized; sample should ensure only men with ED; there should be division into different groups according to the shockwaves characteristics; the follow-up duration should be longer than 3 months.
Factors related to ED, such as age, hypertension, diabetes, hyperlipidemia, and psychological disorders, were not elaborated in the original study, and no further information was provided on the relationship between clinical outcomes of Li-ESWT and these comorbidities. With the stratification of age and comorbidities, more RCTs are needed in the future to analyze the impact of these factors on the efficacy of Li-ESWT for ED patients.
This study has important limitations as follows: Most included studies had small samples—the largest had only 122 men in the meta-analysis; the follow-up in five studies seems very short (only 1 month); no objective parameters were provided in the original studies; there was no unified protocol of Li-ESWT on ED in the included studies. Maximizing the improvement of erectile function may be critical to patients with ED, and the combination of Li-ESWT and PDE5is may be the best choice (Lu et al., 2017). To independently determine the efficacy of Li-ESWT, studies should prohibit any other treatment that might affect erectile function to avoid confusion. Therefore, more RCTs with good research designs are needed in the future.
Conclusion
This meta-analysis assessed the effect of Li-ESWT treating ED. The EHS and IIEF-EF score in men received Li-ESWT improved significantly. Setup parameters and treatment protocols are very important for the efficacy of Li-ESWT in the treatment. Further studies are needed to explore the relationship between ED-related factors and the efficacy of Li-ESWT, and to analyze the effect of Li-ESWT combined with PDE5is. From this review, Li-ESWT may have the potential to become the first choice of noninvasive treatment for vasculogenic ED (Pan et al., 2016), but before that, more strict RCTs are warranted prior to widespread acceptance of this treatment.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Natural Science Foundation of China (grant number: 81673808) and Technological Research and Development Project of Chengdu Science and Technology Bureau (grant number: 2015-HM01-00201-SF).
References
- Assaly-Kaddoum R., Giuliano F., Laurin M., Gorny D., Kergoat M., Bernabé J., … Behr-Roussel D. (2016). Low intensity extracorporeal shock wave therapy improves erectile function in a model of type II diabetes independently of NO/cGMP pathway. The Journal of Urology, 196(3), 950–956. doi: 10.1016/j.juro.2016.03.147 [DOI] [PubMed] [Google Scholar]
- Borenstein M., Hedges L. V., Higgins J. P. T., Rothstein H. R. (2010). A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods, 1(2), 97–111. doi: 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- Clavijo R. I., Kohn T. P., Kohn J. R., Ramasamy R. (2017). Effects of low-intensity extracorporeal shockwave therapy on erectile dysfunction: A systematic review and meta-analysis. The Journal of Sexual Medicine, 14(1), 27–35. doi: 10.1016/j.jsxm.2016.11.001 [DOI] [PubMed] [Google Scholar]
- Egger M., Smith G. D., Schneider M., Minder C. (1997). Bias in meta- analysis detected by a simple, graphical test. BMJ(Clinical research ed.), 315(7109), 629–634. Retrieved from https://www.bmj.com/content/315/7109/629.long [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman H. A., Goldstein I., Hatzichristou D. G., Krane R. J., McKinlay J. B. (1994). Impotence and its medical and psychosocial correlates: Results of the Massachusetts Male Aging Study. The Journal of Urology, 151(1), 54–61. doi: 10.1016/S0022-5347(17)34871-1 [DOI] [PubMed] [Google Scholar]
- Fojecki G. L., Tiessen S., Osther P. J. S. (2017). Effect of low-energy linear shockwave therapy on erectile dysfunction-A double-blinded, sham-controlled, randomized clinical trial. The Journal of Sexual Medicine, 14(1), 106–112. doi: 10.1016/j.jsxm.2016.11.307 [DOI] [PubMed] [Google Scholar]
- Hatzimouratidis K., Amar E., Eardley I., Giuliano F., Hatzichristou D., Montorsi F., … Wespes E. (2010). Guidelines on male sexual dysfunction: Eerectile dysfunction and premature ejaculation. European Urology, 57(5), 804–814. doi: 10.1016/j.eururo.2010.02.020 [DOI] [PubMed] [Google Scholar]
- Higgins J. P. T., Green S. (2011). Cochrane handbook for systematic reviews of interventions. (Version 5.1.0 [updated March 2011]). The Cochrane Collaboration. Retrieved from http://handbook.cochrane.org
- Higgins J. P. T., Thompson S. G., Deeks J. J., Altman D. G. (2003). Measuring inconsistency in meta-analyses. BMJ(Clinical research ed.), 327(7414), 557–560. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holfeld J., Zimpfer D., Albrecht-Schgoer K., Stojadinovic A., Paulus P., Dumfarth J., … Grimm M. (2016). Epicardial shock-wave therapy improves ventricular function in a porcine model of ischaemic heart disease. Journal of Tissue Engineering and Regenerative Medicine, 10(12), 1057–1064. doi: 10.1002/term.1890 [DOI] [PubMed] [Google Scholar]
- Hozo S. P., Djulbegovic B., Hozo I. (2005). Estimating the mean and variance from the median, range, and the size of a sample. BMC Medical Research Methodology, 5, 13. doi: 10.1186/1471-2288-5-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalyvianakis D., Hatzichristou D. (2017). Low-Intensity shockwave therapy improves hemodynamic parameters in patients with vasculogenic erectile dysfunction: A triplex ultrasonography-based sham-controlled trial. The Journal of Sexual Medicine, 14(7), 891–897. doi: 10.1016/j.jsxm.2017.05.012 [DOI] [PubMed] [Google Scholar]
- Kitrey N. D., Gruenwald I., Appel B., Shechter A., Massarwa O., Vardi Y. (2016). Penile low intensity shock wave treatment is able to shift PDE5i nonresponders to responders: A double-blind, sham controlled study. The Journal of Urology, 195(5), 1550–1555. doi: 10.1016/j.juro.2015.12.049 [DOI] [PubMed] [Google Scholar]
- Li H., Matheu M. P., Sun F., Wang L., Sanford M. T., Ning H., … Lue T. F. (2016). Low-energy shock wave therapy ameliorates erectile dysfunction in a pelvic neurovascular injuries rat model. The Journal of Sexual Medicine, 13(1), 22–32. doi: 10.1016/j.jsxm.2015.11.008 [DOI] [PubMed] [Google Scholar]
- Liu J., Zhou F., Li G.-Y., Wang L., Li H.-X., Bai G.-Y., … Xin Z.-C. (2013). Evaluation of the effect of different doses of low energy shock wave therapy on the erectile function of streptozotocin (STZ)-induced diabetic rats. International Journal of Molecular Sciences, 14(5), 10661–10673. doi: 10.3390/ijms140510661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Z., Lin G., Reed-Maldonado A., Wang C., Lee Y.-C., Lue T. F. (2017). Low-intensity extracorporeal shock wave treatment improves erectile function: A systematic review and meta-analysis. European Urology, 71(2), 223–233. doi: 10.1016/j.eururo.2016.05.050 [DOI] [PubMed] [Google Scholar]
- Luo D., Wan X., Liu J., Tong T. (2018). Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Statistical Methods in Medical Research, 27(6), 1785–1805. doi: 10.1177/0962280216669183 [DOI] [PubMed] [Google Scholar]
- Man L., Li G. (2018). Low-intensity extracorporeal shock wave therapy for erectile dysfunction: A systematic review and meta-analysis. Urology, 119, 97–103. doi: 10.1016/j.urology.2017.09.011 [DOI] [PubMed] [Google Scholar]
- Mense S., Hoheisel U. (2013). Shock wave treatment improves nerve regeneration in the rat. Muscle & Nerve, 47(5), 702–710. doi: 10.1002/mus.23631 [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151(4), 264–269. Retrieved from http://annals.org/aim/fullarticle/744664/preferred-reporting-items-systematic-reviews-meta-analyses-prisma-statement [DOI] [PubMed] [Google Scholar]
- Mulhall J. P., Jahoda A. E., Cairney M., Goldstein B., Leitzes R., Woods J., … Goldstein I. (1999). The causes of patient dropout from penile self-injection therapy for impotence. Journal of Urology, 162(4), 1291–1294. doi: 10.1016/S0022-5347(05)68269-9 [DOI] [PubMed] [Google Scholar]
- Olsen A. B., Persiani M., Boie S., Hanna M., Lund L. (2015). Can low-intensity extracorporeal shockwave therapy improve erectile dysfunction? A prospective, randomized, double-blind, placebo-controlled study. Scandinavian Journal of Urology, 49(4), 329–333. doi: 10.3109/21681805.2014.984326 [DOI] [PubMed] [Google Scholar]
- Pan M. M., Raees A., Kovac J. R. (2016). Low-intensity extracorporeal shock wave as a novel treatment for erectile dysfunction. American Journal of Men’s Health, 10(2), 146–148. doi: 10.1177/1557988315574511 [DOI] [PubMed] [Google Scholar]
- Qiu X., Lin G., Xin Z., Ferretti L., Zhang H., Lue T. F., Lin C.-S. (2013). Effects of low-energy shockwave therapy on the erectile function and tissue of a diabetic rat model. The Journal of Sexual Medicine, 10(3), 738–746. doi: 10.1111/jsm.12024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Review Manager (RevMan). 5.3 ed. (2014). Copenhagen: Nordic Cochrane Centre, Cochrane Collaboration. Retrieved from http://handbook.cochrane.org
- Rosen R. C., Allen K. R., Ni X., Araujo A. B. (2011). Minimal clinically important differences in the erectile function domain of the International Index of Erectile Function scale. European Urology, 60(5), 1010–1016. doi: 10.1016/j.eururo.2011.07.053 [DOI] [PubMed] [Google Scholar]
- Rosen R. C., Riley A., Wagner G., Osterloh I. H., Kirkpatrick J., Mishra A. (1997). The International Index of Erectile Dysfunction (IIEF): A multidimensional scale for assessment of erectile dysfunction. Urology, 49(6), 822–830. doi: 10.1016/S0090-4295(97)00238-0 [DOI] [PubMed] [Google Scholar]
- Smith W. B., McCaslin I. R., Gokce A., Mandava S. H., Trost L., Hellstrom W. J. (2013). PDE5 inhibitors: Considerations for preference and long-term adherence. International Journal of Clinical Practice, 67(8), 768–780. doi: 10.1111/ijcp.12074 [DOI] [PubMed] [Google Scholar]
- Srini V. S., Reddy R. K., Shultz T., Denes B. (2015). Low intensity extracorporeal shockwave therapy for erectile dysfunction: A study in an Indian population. The Canadian Journal of Urology, 22(1), 7614–7622. Retrieved from https://www.canjurol.com/abstract.php?ArticleID=&version=1.0&PMID=25694008 [PubMed] [Google Scholar]
- Sterne J. A. C., Egger M. (2001). Funnel plots for detecting bias in meta- analysis: Guidelines on choice of axis. Journal of Clinical Epidemiology, 54(10), 1046–1055. doi: 10.1016/S0895-4356(01)00377-8 [DOI] [PubMed] [Google Scholar]
- Vardi Y., Appel B., Jacob G., Massarwi O., Gruenwald I. (2010). Can low-intensity extracorporeal shockwave therapy improve erectile function? A 6-month follow-up pilot study in patients with organic erectile dysfunction. European Urology, 58(2), 243–248. doi: 10.1016/j.eururo.2010.04.004 [DOI] [PubMed] [Google Scholar]
- Vardi Y., Appel B., Kilchevsky A., Gruenwald I. (2012). Does low intensity extracorporeal shock wave therapy have a physiological effect on erectile function? Short-term results of a randomized, double-blind, sham controlled study. Journal of Urology, 187(5), 1769–1775. doi: 10.1016/j.juro.2011.12.117 [DOI] [PubMed] [Google Scholar]
- Viechtbauer W. (2010). Conducting meta-analyses in R with the meta for package. Journal of Statistical Software, 36, 1–48. doi: 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- Wang C.-J., Wang F.-S., Yang K. D., Weng L.-H., Hsu C.-C., Huang C.-S., Yang L.-C. (2003). Shock wave therapy induces neovascularization at the tendon-bone junction. A study in rabbits. Journal of Orthopaedic Research, 21(6), 984–989. doi: 10.1016/S0736-0266(03)00104-9 [DOI] [PubMed] [Google Scholar]
- Wan X., Wang W., Liu J., Tong T. (2014). Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Medical Research Methodology, 14, 135. doi: 10.1186/1471-2288-14-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wessells H., Joyce G. F., Wise M., Wilt T. J. (2007). Erectile dysfunction. The Journal of Urology 177(5), 1675-1681. doi: 10.1016/j.juro.2007.01.057 [DOI] [PubMed] [Google Scholar]
- Yan X., Zeng B., Chai Y., Luo C., Li X. (2008). Improvement of blood flow, expression of nitric oxide, and vascular endothelial growth factor by low-energy shockwave therapy in random-pattern skin flap model. Annals of Plastic Surgery, 61(6), 646–653. doi: 10.1097/SAP.0b013e318172ba1f [DOI] [PubMed] [Google Scholar]
- Yee C.-H., Chan E. S., Hou S.-S., Ng C.-F. (2014). Extracorporeal shockwave therapy in the treatment of erectile dysfunction: A prospective, randomized, double-blinded, placebo controlled study. International Journal of Urology, 21(10), 1041–1045. doi: 10.1111/iju.12506 [DOI] [PubMed] [Google Scholar]