Abstract
Background.
High levels of positive mental health protects individuals from mental illness. This study investigates longitudinal change in positive mental health as a predictor of mental illness recovery in a cohort group.
Methods.
Using data from the 1995 and 2005 Midlife in the United States cross-sectional surveys (n=1,723), logistic regression was used to estimate the odds ratio that individuals diagnosed with a mental illness in 1995 would have recovered in 2005 based on whether their level of positive mental health changed over the 10-year period.
Results.
Individuals who maintained or gained the highest levels of positive mental health were more than 27.6 and 7.4 times, respectively, more likely to recover when compared to those who maintained the lowest level of positive mental health. Those who maintained or gained moderate levels of positive mental health had more moderate likelihood of recovery, and those whose positive mental health declined to the lowest levels had no significantly different likelihood of recovery compared to participants whose positive mental health remained low.
Limitations.
This study was limited by the age of the data, and the inability to control for some predictors of recovery.
Conclusions.
This study suggests that positive mental health may be an important resource for individuals to recover from mental illness and stay mentally healthy. Results point to the need to include positive mental health assessment and interventions into mental health care systems.
Keywords: positive mental health, recovery, complete state model of mental health, mental health care reform
Introduction
There has been little progress in reducing the burden of mental illness around the world, prompting calls for improved access to quality mental health care and assessment of mental disorders and for “programs to prevent mental disorders and promote mental health” (U. S. Burden of Disease Collaborators, 2018; Vigo et al., 2016). The distinction between mental disorder and mental health is a fundamental underlying element of this call for improvement, but this important distinction is often misunderstood.
Mental illness and mental health are traditionally conceptualised as opposite ends of the same continuum, and modem mental health care systems are primarily designed to reduce mental illness to concurrently improve mental health. It has been argued that health care systems designed this way risk providing ‘reactive’ health care and creating avoidance, fear, and stigma of the pathology (see Herron and Trent (2000) for a review). However, evidence indicates that positive mental health and mental illness are distinct, yet interrelated, constructs that reflect separate continua (Keyes, 2005; Suldo and Shaffer, 2008) (Figure 1).
Figure 1:
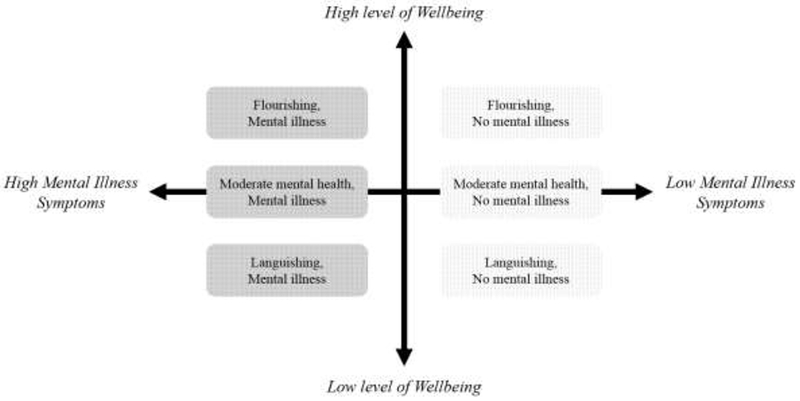
The Complete State Model of Mental Health. The 6 sub-groups constructed by Keyes et al. (2010) are depicted, the light-coloured squares indicate the groups analysed in the Keyes et al. (2010) article, and dark-coloured squares indicate groups analysed in the current study.
Growing evidence suggests that high levels of positive mental health protect individuals from mental illness, and that low levels of positive mental health are a risk factor for mental illness. Keyes et al. (2010) conducted a longitudinal study of mentally healthy participants (without a diagnosis of mental illness) of the 1995 and 2005 waves of the Midlife in the United States (MIDUS) National Study of Health and Well-being. Participants were divided into 6 groups, based on their level of positive mental health and mental illness status in 1995 (Figure 1). The study showed that participants who gained or maintained high levels of positive mental health over the 10-year period had a decreased risk of developing a mental illness (defined as depression, anxiety, and panic disorder), and that participants whose positive mental health declined or remained low had significantly increased odds of developing mental illness. Similar results were observed by Wood and Joseph (2010), who found that people with low levels of positive mental health were several times more likely to be depressed 10 years later. Grant et al. (2013) and Lamers et al. (2015) supported this bidirectional relationship between positive mental health and psychopathology, finding that low levels of positive mental health predicted risk of higher depressive symptoms within one year. This research indicates that mental health protection and promotion should become a mental health care priority to reduce the burden of mental illness, and that building and maintaining high levels of positive mental health is fundamental to this cause (Keyes, 2013).
Positive mental health is also proposed as an important resource for recovery from mental illness and therapies have been designed specifically to improve the positive mental health of individuals with diagnosed mental illness (Slade et al., 2017). However, there has been little to no research on whether positive mental health is associated with recovery (Seow et al., 2016). Investigating whether positive mental health is a resource for recovery can provide evidence necessary to develop better models of mental health care (Keyes, 2014).
In the current study, we extend the Keyes et al. (2010) study using the same large dataset, focusing instead on participants diagnosed with a mental illness at baseline (those who are situated to the left of the vertical axis in Figure 1), rather than those that were mentally healthy (those who can be found in the right half of Figure 1). We hypothesise that gains in positive mental health from 1995 to 2005 are associated with greater odds of ‘recovering’ from that mental illness in 2005, and that losses in positive mental health will be associated with lesser odds of recovery 10 years later. We acknowledge the important discourse between clinical and personal recovery, and use recovery here to indicate an individual that was assessed with depression, anxiety, or panic disorder in 1995 and not in 2005.
Methods
This study replicates the methodology used in the original Keyes et al. (2010) study. A representative sample of U.S. adults above the age of 18 who participated in the MIDUS study provided data on their mental illness and positive mental health in 1995 and 2005 (n=l,723). Although the third MIDUS wave is available, the sample size was unsuitable for this analysis due to small sample size resulting from participant drop out over the 20 year follow up. The 12-month prevalence of mental illnesses measured in the MIDUS dataset (major depressive episode, generalized anxiety, and panic disorder) for both time-points was determined using the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Text Revised (DSM-IV-TR) criteria through the Composite International Diagnostic Interview-Short Form (CIDI-SF) scale. The degree of positive mental health (flourishing, languishing, or moderate mental health) was based on their scores on emotional, psychological and social well-being scales (Keyes et al., 2010). To be defined as flourishing, individuals exhibited high levels (scores in the upper tertile) on 1 of the 2 measures of emotional well-being and at least 6 or more of the 11 scales of psychological and social wellbeing. To be defined as languishing, individuals exhibited low levels (scores in the lower tertile) on 1 of the 2 measures of emotional well-being and 6 or more of the 11 scales of psychological and social well-being. Individuals that did not fit the criteria for flourishing or languishing were categorised with moderate mental health.
Logistic regression was performed using SPSS v.25 (SPSS Inc, Chicago, IL) to generate prevalence Odds Ratios (OR) of mental illness in 2005 as a function of change in mental health levels between 1995 and 2005, along with baseline mental illness (1995) and covariates (age, gender, race/ethnicity, education, employment status, marital status, physical illness). For prevalence- and incidence-based analyses, we created a categorical variable that measured change in positive mental health between 1995 and 2005. These categories included: individuals who (1) stayed flourishing, (2) improved to flourishing, (3) declined to moderate, (4) stayed moderate, (5) improved to moderate, (6) declined to moderate, (7) stayed languishing. The latter category was used as the reference group.
Results
Table 1 reports the outcomes of the binary logistic regression analysis. Participants who were flourishing at both time points, and participants who improved from languishing or moderate mental health to flourishing, demonstrated significantly higher odds of recovering from their mental illness, OR = 27.617 and OR = 7.444 respectively. While marginally nonsignificant, those who declined from flourishing to moderate positive mental health kept a higher odds of recovery (OR=2.931; p=.067) as those who stayed languishing. Those who maintained moderate positive mental health or improved to moderate demonstrated significantly higher odds (OR = 1.839, p=.011 and 1.771, p=.048 respectively). Participants who declined to languishing over the 10 years were no more likely to have recovered from their mental illness than those who stayed languishing.
Table 1:
Adjusted Prevalence Odds Ratio (OR) of any Mental Illness in 2005 by Change in Mental Health level between 1995 and 2005: Midlife in the United States Study
| 1995-2005 | |||
|---|---|---|---|
| OR (95% CI) | Sig | n | |
| Stayed flourishing | 27.617 (3.468, 219.902) | .002 | 25 |
| Languishing or moderate to flourishing | 7.444 (2.719, 20.378) | .000 | 42 |
| Flourishing to moderate positive mental health | 2.931 (0.927, 9.271) | .067 | 26 |
| Stayed moderate positive mental health | 1.839 (1.152, 2.935) | .011 | 234 |
| Languishing to moderate positive mental health | 1.771 (1.004, 3.124) | .048 | 106 |
| Flourishing or moderate to languishing | 0.831 (.408, 1.692) | .610 | 58 |
| Stayed languishing (REF) | 1 | - | 144 |
Note: CI = confidence interval, REF = reference category. ORs are adjusted for demographic variables (age, gender, race/ethnicity, education, marital status, and employment in 2005) and whether respondents had any physical health conditions in 1995.
Discussion
This study provides evidence that individuals with diagnosed mental illness who gain or maintain high levels, and those who gain or maintain moderate levels, of positive mental health over a 10-year period have much greater odds of recovering than those with low levels of positive mental health. No difference in odds of recovery was observed among participants who declined from flourishing or moderate positive mental health to languishing. The results indicate that positive mental health may be an important resource for individuals to recover from a mental illness and stay mentally healthy. It also adds to existing evidence highlighting the importance of change in psychopathology and positive mental health over time, as opposed to their respective absolute levels at any given time (Lamers et al., 2015). These results, particularly in combination with Keyes et al. 2010 imply that mental health care systems should focus on promoting and protecting positive mental health, irrespective of a diagnosis of a mental illness. The current study adds to the growing academic literature advocating for the inclusion of positive mental health intervention and assessment into mental health care (de Cates et al., 2015; Provencher and Keyes, 2011; Siddaway et al., 2017; Slade, 2010).
Interventions to improve positive mental health have been designed and tested in a range of modalities, including one-on-one, group-based, and in online format, but predominantly for healthy populations (Bolier et al., 2013). Investigation of evidence-based interventions in mentally ill populations and clinical settings is developing rapidly (Fava et al., 2017; Rashid and Seligman, 2018), and adoption of positive mental health strategies in mental health practice and policy, for instance the inclusion of positive mental health assessment when patients present with mental health problems, should be explored to help reduce the burden of mental illness.
The strength of this study was its longitudinal cohort design. The large sample size enabled sufficient power to detect meaningful temporal associations and most known predictors of mental illness were controlled for. This is not an exhaustive list however, and a limitation of this study is was the lack of information regarding key predictors of recovery, such as illness severity, participant income, social support, or treatment information. Reflecting current diagnostic practice, this study relied on a categorical clinical perspective of recovery, which focuses on the reduction of symptomology to below a clinical threshold. Future research should consider continuous data analysis, which would provide additional insight to a categorical diagnosis. For example, Renshaw et al. (2016) showed that continuous and categorical analysis can produce different results in mental health research and should not be compared directly. A consumer-based movement towards personal recovery is developing, which emphasises hope, identity, meaning, and personal responsibility rather than a sole focus on reducing symptoms (Slade 2010). Future research should investigate whether levels of positive mental health underpin a sense of personal recovery, prior to subsequent clinical recovery as measured in this study. This study was further limited by the age of the data, and replications of these result are recommended in more contemporary data. Finally, it was not possible to understand individual’s pathway to recovery, which likely would have involved cycles of relapse and gain in function.
Conclusions
It has been found that positive mental health is an important resource to minimise the risk of developing an affective disorder. This study provides evidence that positive mental health is also an important resource for recovery from depression, anxiety, and panic disorder. This study contributes to the growing body of evidence advocating for the inclusion of positive mental health interventions and assessment into mental health care system to reduce the burden of mental illness around the world.
Highlights:
Individuals who gain or maintain high levels of positive mental health are much more likely to recover from an affective disorder than those with low positive mental health.
Positive mental health and mental illness are separate constructs, and both should be included in the assessment of patients interacting with mental health care systems.
Improving and maintaining positive mental health may be an important strategic focus for reducing the burden of mental illness.
Mental health care systems should explore offering of services designed to improve positive mental health in addition to reducing mental distress.
Acknowledgements
Role of the Funding Source
This research was supported by a grant from the National Institute on Aging (P01-AG020166) to conduct a longitudinal follow-up of the Midlife in the United States(MIDUS) investigation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
All authors declare that they have no conflicts of interest.
References
- Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E, 2013. Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC public health 13, 119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Cates A, Stranges S, Blake A, Weich S, 2015. Mental well-being: an important outcome for mental health services? The British Journal of Psychiatry 207, 195–197. [DOI] [PubMed] [Google Scholar]
- Fava GA, Cosci F, Guidi J, Tomba E, 2017. Well-being therapy in depression: New insights into the role of psychological well-being in the clinical process. Depression and anxiety 34, 801–808. [DOI] [PubMed] [Google Scholar]
- Grant F, Guille C, Sen S, 2013. Well-being and the risk of depression under stress. PLoS one 8, e67395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herron S, Trent D, 2000. Mental Health: A Secondary Concept to Mental Illness. Journal of Public Mental Health 2, 29–38. [Google Scholar]
- Keyes CL, Dhingra SS, Simoes EJ, 2010. Change in level of positive mental health as a predictor of future risk of mental illness. American Journal of Public Health 100, 2366–2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes CLM, 2005. Mental illness and/or mental health? Investigating axioms of the complete state model of health. Journal of consulting and clinical psychology 73, 539. [DOI] [PubMed] [Google Scholar]
- Keyes CLM, 2013. Promoting and protecting positive mental health: Early and often throughout the lifespan, Mental Well-Being: International Contributions to the Study of Positive Mental Health, pp. 3–28. [Google Scholar]
- Keyes CLM, 2014. Mental health as a complete state: How the salutogenic perspective completes the picture, Bridging occupational, organizational and public health: A transdisciplinary approach. Springer Science + Business Media; US, New York, NY, pp. 179–192. [Google Scholar]
- Lamers SM, Westerhof GJ, Glas CA, Bohlmeijer ET, 2015. The bidirectional relation between positive mental health and psychopathology in a longitudinal representative panel study. The Journal of Positive Psychology 10, 553–560. [Google Scholar]
- Provencher HL, Keyes CL, 2011. Complete mental health recovery: Bridging mental illness with positive mental health. Journal of Public Mental Health 10, 57–69. [Google Scholar]
- Rashid T, Seligman MP, 2018. Positive Psychotherapy: Clinician Manual. Oxford University Press. [Google Scholar]
- Renshaw TL, Eklund KR, Bolognino SJ, Adodo I, 2016. Bidimensional emotional health in college students: A comparison of categorical and continuous analytic approaches. Journal of Psychopathology and Behavioral Assessment 38, 681–694. [Google Scholar]
- Seow LSE, Vaingankar JA, Abdin E, Sambasivam R, Jeyagurunathan A, Pang S, Chong SA, Subramaniam M, 2016. Positive mental health in outpatients with affective disorders: Associations with life satisfaction and general functioning. Journal of Affective Disorders 190, 499–507. [DOI] [PubMed] [Google Scholar]
- Siddaway AP, Wood AM, Taylor PJ, 2017. The Center for Epidemiologic Studies-Depression (CES-D) scale measures a continuum from well-being to depression: Testing two key predictions of positive clinical psychology. Journal of affective disorders 213, 180–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade M, 2010. Mental illness and well-being: the central importance of positive psychology and recovery approaches. BMC health services research 10, 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade M, Oades L, Jarden A, 2017. Wellbeing, recovery and mental health, Wellbeing, recovery and mental health. Cambridge University Press; US, New York, NY, pp. xiii, 341. [Google Scholar]
- Suldo SM, Shaffer EJ, 2008. Looking beyond psychopathology: The dual-factor model of mental health in youth. School Psychology Review 37, 52–68. [Google Scholar]
- Burden US of Disease Collaborators, 2018. The state of US health, 1990-2016: Burden of diseases, injuries, and risk factors among us states. JAMA 319, 1444–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigo D, Thornicroft G, Atun R, 2016. Estimating the true global burden of mental illness. The Lancet Psychiatry 3, 171–178. [DOI] [PubMed] [Google Scholar]
- Wood AM, Joseph S, 2010. The absence of positive psychological (eudemonic) well-being as a risk factor for depression: A ten year cohort study. Journal of affective disorders 122, 213–217. [DOI] [PubMed] [Google Scholar]


