Key Points
Question
How do the type and duration of surgical antimicrobial prophylaxis affect postoperative outcomes?
Findings
In this national cohort study including 79 058 patients undergoing surgical procedures in the VA health care system, increasing duration of surgical prophylaxis was not associated with additional reductions in surgical site infection but was associated with increases in acute kidney injury and Clostridium difficile infections. The type of regimen was also an important driver of postoperative adverse events; limiting the use of vancomycin may improve clinical outcomes.
Meaning
The risk of adverse events increases with each additional day of antimicrobial exposure.
This national cohort study assesses the association of type and duration of prophylaxis with surgical site infection, acute kidney injury, and Clostridium difficile infection.
Abstract
Importance
The benefits of antimicrobial prophylaxis are limited to the first 24 hours postoperatively. Little is known about the harms associated with continuing antimicrobial prophylaxis after skin closure.
Objective
To characterize the association of type and duration of prophylaxis with surgical site infection (SSI), acute kidney injury (AKI), and Clostridium difficile infection.
Design, Setting, and Participants
In this multicenter, national retrospective cohort study, all patients within the national Veterans Affairs health care system who underwent cardiac, orthopedic total joint replacement, colorectal, and vascular procedures and who received planned manual review by a trained nurse reviewer for type and duration of surgical prophylaxis and for SSI from October 1, 2008, to September 30, 2013, were included. Data were analyzed using multivariable logistic regression, with adjustments for covariates determined a priori to be associated with the outcomes of interest. Data were analyzed from December 2016 to December 2018.
Exposures
Duration of postoperative antimicrobial prophylaxis (<24 hours, 24-<48 hours, 48-<72 hours, and ≥72 hours).
Main Outcomes and Measures
Surgical site infection, AKI, and C difficile infection.
Results
Of the 79 058 included patients, 76 109 (96.3%) were men, and the mean (SD) age was 64.8 (9.4) years. Among 79 058 surgical procedures in the cohort, all had SSI and C difficile outcome data available; 71 344 (90.2%) had AKI outcome data. After stratification by type of surgery and adjustment for age, sex, race, diabetes, smoking, American Society of Anesthesiologists score greater than 2, methicillin-resistant Staphylococcus aureus colonization, mupirocin, type of prophylaxis, and facility factors, SSI was not associated with duration of prophylaxis. Adjusted odds of AKI increased with each additional day of prophylaxis (cardiac procedure: 24-<48 hours: adjusted odds ratio [aOR], 1.03; 95% CI, 0.95-1.12; 48-<72 hours: aOR, 1.22; 95% CI, 1.08-1.39; ≥72 hours: aOR, 1.82; 95% CI, 1.54-2.16; noncardiac procedure: 24-<48 hours: aOR, 1.31; 95% CI, 1.21-1.42; 48-<72 hours: aOR, 1.72; 95% CI, 1.47-2.01; ≥72 hours: aOR, 1.79; 95% CI, 1.27-2.53). The risk of postoperative C difficile infection demonstrated a similar duration-dependent association (24-<48 hours: aOR 1.08; 95% CI, 0.89-1.31; 48-<72 hours: aOR, 2.43; 95% CI, 1.80-3.27; ≥72 hours: aOR, 3.65; 95% CI, 2.40-5.53). The unadjusted numbers needed to harm for AKI after 24 to less than 48 hours, 48 to less than 72 hours, and 72 hours or more of postoperative prophylaxis were 9, 6, and 4, respectively; and 2000, 90, and 50 for C difficile infection, respectively. Vancomycin receipt was also a significant risk factor for AKI (cardiac procedure: aOR, 1.17; 95% CI, 1.10-1.25; noncardiac procedure: aOR, 1.21; 95% CI, 1.13-1.30).
Conclusions and Relevance
Increasing duration of antimicrobial prophylaxis was associated with higher odds of AKI and C difficile infection in a duration-dependent fashion; extended duration did not lead to additional SSI reduction. These findings highlight the notion that every day matters and suggest that stewardship efforts to limit duration of prophylaxis have the potential to reduce adverse events without increasing SSI.
Introduction
National guidelines recommend that surgical antimicrobial prophylaxis be initiated within 1 hour prior to incision and discontinued within 24 hours postoperatively for most procedures and within 48 hours for cardiac surgery.1,2 These guidelines were based on strong clinical trial data demonstrating that administration of antimicrobials after skin closure does not lead to additional risk reduction; 2017 updates from the American College of Surgeons and the Surgical Infection Society3 state that antimicrobials should be discontinued after skin closure following most procedures but that the optimal duration for surgical prophylaxis remains unknown for others, including cardiac procedures and procedures with foreign body placement.4 Limited data are available regarding the risks of prolonged prophylaxis regimens, but prior studies demonstrate that antimicrobials are a leading cause of adverse drug reactions and emergency department visits.5 Additionally, little is known about the association of the duration of exposure with tangible and quantifiable adverse effects on patient outcomes.
The clear benefit of surgical antimicrobial prophylaxis is a reduction in surgical site infections (SSIs); preincisional administration of antimicrobials was a major driver in reducing postoperative infectious outcomes.1 Known risks of antimicrobials include acute kidney injury (AKI), particularly for regimens containing multiple prophylactic agents or known nephrotoxic agents, such as vancomycin and aminoglycosides.6,7,8 Another important risk following antimicrobial exposure is Clostridium difficile infection. Studies suggest that among patients undergoing cardiac surgery, duration of surgical prophylaxis may be a major contributor to postoperative C difficile infection.9,10,11 Data from other types of procedures, where duration of prophylaxis may be shorter, are limited, as are data regarding the impact of specific prophylaxis regimens.
Thus, we sought to characterize the association of the duration of postoperative surgical prophylaxis with the incidence of important postoperative outcomes, including SSI, AKI, and C difficile infection. A secondary aim was to determine how the choice of antimicrobial regimen affects this association.
Methods
The study cohort included all Veteran patients undergoing major cardiac, orthopedic total joint replacement, colorectal, and vascular procedures between October 1, 2008, and September 30, 2013, who received manual review by a trained clinician as part of the VA External Peer Review Program, which collects information about preoperative quality metrics, including type, timing, and duration of surgical prophylaxis regimens.12 For each unique procedure, VA External Peer Review Program data were matched to the VA Surgical Quality Improvement Project (VASQIP) database for relevant postoperative outcomes (ie, SSI).12 Based on a validated sampling algorithm, VASQIP manually reviews approximately 80% of all major surgical cases, applying recent National Healthcare Safety Network definitions, with the exception of a 30-day end point for all types of SSI, regardless of surgical procedure.13 Data from these manually validated quality reviews were combined with additional data (eg, laboratory data, pharmacy data) available in the VA Corporate Data Warehouse for each patient to create the final data set used in the analyses. Approvals from the VA Boston Institutional Review Board, the Surgical Quality Data Group, and the External Peer Review Program were obtained prior to data collection. Because of the retrospective nature of the study, a waiver of informed consent was obtained.
Outcomes
The outcome variables of interest were 30-day SSI, 7-day incidence of AKI, and 90-day incidence of C difficile infection. The SSI outcome was determined by planned medical record review by a trained clinician applying National Healthcare Safety Network definitions, modified by applying a 30-day window period for all surgical types. Surgical site infection in noncardiac procedures was defined as the presence of a VASQIP-assessed superficial, deep, or organ/space infection. For cardiac procedures, SSIs were defined as VASQIP-assessed mediastinitis or endocarditis for the entire study period and superficial SSI in the years that it was collected. Acute kidney injury was defined according to the Acute Kidney Injury Network definitions (ie, a postoperative increase in serum creatinine level of 0.3 mg/dL [to convert to micromoles per liter, multiply by 88.4] or more or a 1.5-fold or greater increase relative to the most recent preoperative result) or a determination of AKI as documented by the VASQIP reviewer.14 The C difficile infection outcome was defined as the presence of positive laboratory test results (ie, on enzyme-linked assay, polymerase chain reaction analysis, or stool culture) for C difficile within 90 days after the date of surgery. Patients with negative C difficile laboratory results and no test identified were classified as negative. Surgical site infection and C difficile outcomes were available for all 79 058 patients. The AKI outcome was only calculated for the 71 344 patients (90.2%) with both preoperative and postoperative creatinine measurements.
Covariates
The exposure variables of interest were duration and type of surgical prophylaxis, which were determined by prospectively planned manual review by a trained nurse clinician. The duration in hours was calculated between the first and last dose of the antimicrobial prophylaxis. The antimicrobial prophylaxis variable was classified into β-lactam, vancomycin, intravenous aminoglycoside, and any other systemic antimicrobial (either alone or in combination). Antimicrobial exposure was then classified into mutually exclusive categories, including both single-drug (eg, vancomycin alone) and combination (eg, vancomycin plus a β-lactam) regimens. To account for potential increased nephrotoxicity of combinations including multiple nephrotoxic agents,15 an additional category including patients who received both vancomycin and an intravenous aminoglycoside was created. The β-lactam category (predominantly, cefazolin) administered for less than 24 hours was used as the reference group for all surgery types.
Additional covariates determined a priori to be of interest included demographic variables and medical comorbidities (ie, age, sex, race, smoking status within 1 year preoperatively, history of diabetes, and American Society of Anesthesiologists score >2), medication exposures (ie, receipt of nonsteroidal anti-inflammatories and proton pump inhibitors), methicillin-resistant Staphylococcus aureus (MRSA) colonization status, and mupirocin administration. Surgical variables included anesthesia type and duration (general vs other, for noncardiac procedures), cardiopulmonary bypass time in hours (for cardiac procedures), and intraoperative blood loss requiring transfusion (categorical, with the none category as the reference group).16,17 To control for facility-level factors that may have affected both exposure and outcomes, a variable with facility median duration of prophylaxis was broken into quartiles and included in all logistic regression models; to account for guideline differences, median facility duration of prophylaxis was calculated separately for cardiac and noncardiac procedures.
Statistical Analysis
Logistic regression was used to estimate the odds of the 3 postoperative adverse outcomes (SSI, AKI, and C difficile infection) as a function of patient characteristics, surgical features, perioperative antibiotic prophylaxis, and facility factors. Given inherent differences in antimicrobial choice and duration by surgery type, SSI outcome models are presented as a stratified analysis. Because of differences in type of anesthesia and available exposures (ie, cardiopulmonary bypass time vs duration of general anesthesia), AKI models were stratified by cardiac and noncardiac procedures. A preplanned stratified analysis among patients with and without MRSA colonization was completed to further evaluate the association of receipt of vancomycin with AKI outcome. One model was developed to evaluate the association of type and duration of prophylaxis with C difficile infection. A sensitivity analysis excluding patients who were being treated preoperatively for an unrelated infection (eg, urinary tract infection or pneumonia) was also performed.
Given our findings that vancomycin-containing regimens have benefits but also harms in cardiac surgery, a post hoc subanalysis among patients undergoing cardiac surgery receiving vancomycin, a β-lactam, or both in combination was completed measuring benefits (SSI reduction) and harms (AKI, classified as any or broken into Acute Kidney Injury Network stages).14 Binomial regression models adjusted for age, diabetes, and American Society of Anesthesiologists score were estimated. Numbers needed to treat and numbers needed to harm were calculated based on the relative risk estimated from the multivariate models.
Results
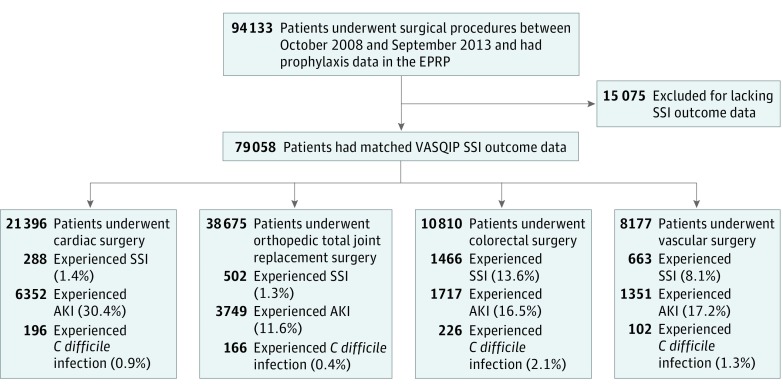
In total, 79 058 eligible patients undergoing surgical procedures (21 396 cardiac procedures [27.1%], 38 675 orthopedic procedures [48.9%], 10 810 colorectal procedures [13.7%], and 8177 vascular procedures [9.4%]) with outcomes and manually extracted prophylaxis regimen data were included (Figure 1). Most patients were male (76 109 [96.3%]), and the mean (SD) age of the cohort was 64.8 (9.4) years. A total of 21 550 patients (27.3%) had diabetes, and 23 006 (29.1%) were active smokers. We included 109 unique facilities across the United States. Most patients received β-lactam-based regimens (54 780 [69.3%]) or vancomycin-based regimens (19 417 [24.6%]) for surgical prophylaxis; the median (interquartile range) duration of surgical prophylaxis across all facilities was 18.5 (14.5-18.5) hours after skin closure (eFigure 1 in the Supplement). Baseline characteristics of the cohort are presented in Table 1.
Figure 1. Cohort Creation Diagram With Distribution of Outcomes Stratified by Surgical Type.
AKI indicates acute kidney injury; C difficile, Clostridium difficile; EPRP, VA External Peer Review Program; SSI, surgical site infection; VASQIP, VA Surgical Quality Improvement Project.
Table 1. Baseline Characteristics of Cohort.
| Characteristic | No. (%)a | |||
|---|---|---|---|---|
| Whole Cohort | SSI | AKIb | C difficile | |
| Total, No. | 79 058 | 2919 | 13 169 | 690 |
| Surgery type | ||||
| Cardiac | 21 396 (27.1) | 288 (1.4) | 6352 (30.4) | 196 (0.9) |
| Orthopedic | 38 675 (48.9) | 502 (1.3) | 3749 (11.6) | 166 (0.4) |
| Colorectal | 10 810 (13.7) | 1466 (13.6) | 1717 (16.5) | 226 (2.1) |
| Vascular | 8177 (10.3) | 663 (8.1) | 1351 (17.2) | 102 (1.3) |
| Age, mean (SD), y | 64.8 (9.4) | 64.5 (9.6) | 66.9 (9.4) | 69.2 (10.2) |
| Race | ||||
| White | 61 766 (78.1) | 2301 (3.7) | 9811 (14.9) | 568 (0.9) |
| Black | 10 954 (13.9) | 393 (3.6) | 2231 (22.3) | 78 (0.7) |
| Other/unknown | 6375 (8.1) | 225 (3.5) | 1127 (19.8) | 44 (0.7) |
| Male | 76 109 (96.3) | 2830 (3.7) | 12 927 (18.8) | 673 (0.9) |
| Diabetes | 21 550 (27.3) | 955 (4.4) | 5184 (25.9) | 192 (0.9) |
| Smoking | 23 006 (29.1) | 1155 (5.0) | 3370 (16.1) | 204 (0.9) |
| Prophylaxis duration, h | ||||
| <24 | 57 844 (73.2) | 2334 (4.0) | 7530 (14.7) | 464 (0.8) |
| 24-<48 | 17 602 (22.3) | 450 (2.6) | 4422 (26.4) | 149 (0.9) |
| 48-<72 | 2724 (3.5) | 110 (4.0) | 852 (32.1) | 52 (1.9) |
| ≥72 | 886 (1.1) | 25 (2.8) | 364 (41.9) | 25 (2.8) |
| Antimicrobial prophylaxisc | ||||
| Vancomycin + aminoglycoside | 932 (1.2) | 21 (2.4) | 212 (23.2) | 13 (1.4) |
| Aminoglycoside | 1490 (1.9) | 36 (2.4) | 136 (13.5) | 9 (0.6) |
| Vancomycin | 19 417 (24.6) | 378 (2.0) | 4559 (25.5) | 162 (0.8) |
| β-Lactam | 54 780 (69.3) | 2335 (4.3) | 7957 (16.1) | 473 (0.9) |
| Other | 2439 (3.1) | 149 (6.1) | 305 (14.7) | 33 (1.4) |
Abbreviations: AKI, acute kidney injury; C difficile, Clostridium difficile infection; SSI, surgical site infection.
The Whole Cohort column contains column percentages; other columns contain row percentages.
Acute kidney injury results available for 71 344 patients (90.2%).
Patients entered into highest risk category for AKI; thus antibiotic categories presented may be the only prophylactic agents administered, or other antibiotics may have been administered in conjunction with the listed highest-risk antibiotic. Given the well-characterized combined toxicity of vancomycin plus aminoglycosides, this specific combination was evaluated separately.
After adjusting for SSI risk factors determined a priori, antimicrobial courses lasting more than 24 hours did not lead to reductions in SSI among any of the surgical types evaluated (Table 2). Among cardiac procedures, there was a reduction in SSI among patients who received vancomycin (either alone or in combination with another agent) vs a β-lactam alone (adjusted odds ratio [aOR], 0.73; 95% CI, 0.57-0.93); similar risk reductions were not identified for other surgical subspecialties.
Table 2. Association of Type and Duration of Antimicrobial Prophylaxis With Surgical Site Infection.
| Variable | aOR (95% CI) |
|---|---|
| Cardiac Surgerya | |
| Antimicrobial type | |
| β-Lactam | 1 [Reference] |
| Vancomycin + aminoglycoside | 1.29 (0.52-3.20) |
| Aminoglycoside | 2.35 (0.72-7.62) |
| Vancomycin | 0.73 (0.57-0.93) |
| Other | 2.83 (0.68-11.83) |
| Antimicrobial duration, h | |
| <24 | 1 [Reference] |
| 24-<48 | 0.96 (0.71-1.29) |
| 48-<72 | 0.73 (0.42-1.30) |
| ≥72 | 0.99 (0.49-2.00) |
| Orthopedic Surgeryb,c | |
| Antimicrobial type | |
| β-Lactam | 1 [Reference] |
| Vancomycin + aminoglycoside | 1.26 (0.57-2.80) |
| Aminoglycoside | 0.74 (0.40-1.35) |
| Vancomycin | 1.00 (0.80-1.26) |
| Other | 1.23 (0.80-1.89) |
| Antimicrobial duration, h | |
| <24 | 1 [Reference] |
| 24-<48 | 1.11 (0.82-1.51) |
| 48-<72 | 2.04 (1.00-4.16) |
| ≥72 | 1.63 (0.22-12.07) |
| Colorectal Surgeryb,d | |
| Antimicrobial type | |
| β-Lactam | 1 [Reference] |
| Vancomycin + aminoglycoside | 2.53 (0.97-6.61) |
| Aminoglycoside | 1.12 (0.68-1.86) |
| Vancomycin | 1.17 (0.85-1.60) |
| Other | 1.21 (0.97-1.52) |
| Antimicrobial duration, h | |
| <24 | 1 [Reference] |
| 24-<48 | 0.87 (0.73-1.04) |
| 48-<72 | 0.81 (0.60-1.09) |
| ≥72 | 0.96 (0.52-1.79) |
| Vascular Surgeryb,e | |
| Antimicrobial type | |
| β-Lactam | 1 [Reference] |
| Vancomycin + aminoglycoside | 0.49 (0.19-2.07) |
| Aminoglycoside | 0.50 (0.18-1.40) |
| Vancomycin | 0.89 (0.72-1.11) |
| Other | 0.97 (0.63-1.49) |
| Antimicrobial duration, h | |
| <24 | 1 [Reference] |
| 24-<48 | 0.95 (0.81-1.21) |
| 48-<72 | 1.27 (0.87-1.86) |
| ≥72 | 0.48 (0.15-1.56) |
Abbreviation: aOR, adjusted odds ratio.
Model adjusted for age, sex, race, diabetes, smoking status, American Society of Anesthesiologists score greater than 2, methicillin-resistant Staphylococcus aureus colonization status, mupirocin receipt, and facility median duration of surgical prophylaxis for cardiac procedures only. Model C statistic, 0.64.
Model adjusted for age, sex, race, diabetes, smoking status, American Society of Anesthesiologists score greater than 2, methicillin-resistant Staphylococcus aureus colonization status, mupirocin receipt, and facility median duration of surgical prophylaxis for noncardiac procedures only.
Model C statistic, 0.60.
Model C statistic, 0.58.
Model C statistic, 0.61.
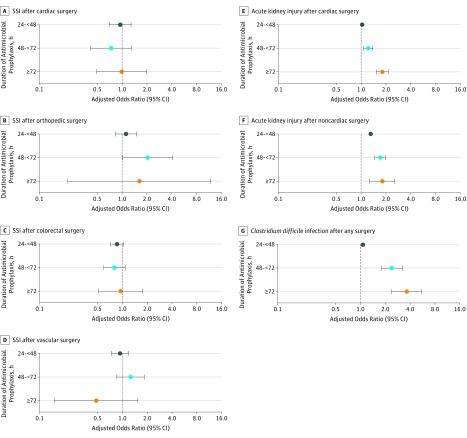
Duration of prophylaxis was independently associated with increasing odds of postoperative AKI and C difficile infection; risk increased with each additional day of antimicrobial exposure (Table 3). Among cardiac procedures, after adjusting for age, race, sex, diabetes, American Society of Anesthesiologists score, smoking, cardiopulmonary bypass time, intraoperative blood loss, receipt of nonsteroidal anti-inflammatories and proton pump inhibitors, and facility factors, odds of AKI nonsignificantly increased by 3.2% after 24 to less than 48 hours of antimicrobial prophylaxis (aOR, 1.03; 95% CI, 0.95-1.12) and significantly increased by 22.3% after 48 to less than 72 hours (aOR, 1.22; 95% CI, 1.08-1.39) and by 82.0% after 72 hours or more (aOR, 1.82; 95% CI, 1.54-2.16); a similar significant daily risk increase was seen among noncardiac procedures (24-<48 hours: 31.0%; aOR, 1.31; 95% CI, 1.21-1.42; 48-<72 hours: 71.5%; aOR, 1.72; 95% CI, 147-2.01; ≥72 hours: 79.2%; aOR, 1.79; 95% CI, 1.27-2.53). Odds of C difficile infection (all procedures) nonsignificantly increased by 7.8% after 24 to less than 48 hours of antimicrobial prophylaxis (aOR, 1.08; 95% CI, 0.89-1.31) and significantly increased by 142.6% after 48 to less than 72 hours (aOR, 2.43; 95% CI, 1.80-3.27) and by 265.1% after 72 hours or more (aOR, 3.65; 95% CI, 2.40-5.55). A summary of the association of duration of prophylaxis with postoperative adverse events is presented in Figure 2. A sensitivity analysis in which patients with preoperative infections (368 [0.5%]) were excluded did not substantially change effect estimates; however, the AKI risk in cardiac surgery after 24 to less than 48 hours of antimicrobial prophylaxis became significant (aOR, 1.12; 95% CI, 1.04-1.19).
Table 3. Association of Type and Duration of Antimicrobial Exposure With Postoperative Acute Kidney Injury (AKI) and Clostridium difficile Infection.
| Variable | aOR (95% CI) |
|---|---|
| AKI (Cardiac Surgery)a | |
| Antimicrobial type | |
| β-Lactam | 1 [Reference] |
| Vancomycin + aminoglycoside | 1.24 (0.95-1.61) |
| Aminoglycoside | 0.60 (0.37-0.99) |
| Vancomycin | 1.17 (1.10-1.25) |
| Other | 1.07 (0.58-2.00) |
| Antimicrobial duration, h | |
| <24 | 1 [Reference] |
| 24-<48 | 1.03 (0.95-1.12) |
| 48-<72 | 1.22 (1.08-1.39) |
| ≥72 | 1.82 (1.54-2.16) |
| AKI (Noncardiac Surgery)b | |
| Antimicrobial type | |
| β-Lactam | 1 [Reference] |
| Vancomycin + aminoglycoside | 1.77 (1.42-2.20) |
| Aminoglycoside | 1.12 (0.90-1.38) |
| Vancomycin | 1.21 (1.13-1.30) |
| Other | 1.13 (0.98-1.29) |
| Antimicrobial duration, h | |
| <24 | 1 [Reference] |
| 24-<48 | 1.31 (1.21-1.42) |
| 48-<72 | 1.72 (1.47-2.01) |
| ≥72 | 1.79 (1.27-2.53) |
| C difficile Infectionc | |
| Antimicrobial type | |
| β-Lactam | 1 [Reference] |
| Vancomycin + aminoglycoside | 1.42 (0.81-2.48) |
| Aminoglycoside | 0.72 (0.37-1.41) |
| Vancomycin | 0.87 (0.72-1.05) |
| Other | 1.53 (1.07-2.19) |
| Antimicrobial duration, h | |
| <24 | 1 [Reference] |
| 24-<48 | 1.08 (0.89-1.31) |
| 48-<72 | 2.43 (1.80-3.27) |
| ≥72 | 3.65 (2.40-5.55) |
Abbreviation: aOR, adjusted odds ratio.
Model adjusted for age, sex, race, smoking status, diabetes, American Society of Anesthesiologists score less than 2, cardiopulmonary bypass pump time (quartiles), intraoperative blood transfusion (categorical; reference, none), receipt of perioperative nonsteroidal anti-inflammatory drugs and proton pump inhibitors, and facility median duration of surgical prophylaxis for cardiac procedures. Model C statistic, 0.64.
Model adjusted for age, sex, race, smoking status, diabetes, anesthesia type (categorical) and duration (categorical, quartiles), receipt of intraoperative blood transfusions (categorical; reference, none), receipt of nonsteroidal anti-inflammatory drugs and proton pump inhibitors, and facility median duration of surgical prophylaxis for noncardiac procedures only. Model C statistic, 0.66.
Model adjusted for age, sex, race, diabetes, smoking status, receipt of perioperative proton pump inhibitors, and facility median duration of surgical prophylaxis. Model C statistic, 0.65.
Figure 2. Adjusted Odds of Surgical Site Infection (SSI), Acute Kidney Injury, and Clostridium difficile Infection by Duration of Antimicrobial Prophylaxis.
Type of prophylaxis was associated with both AKI and C difficile infection risk (Table 3). Use of vancomycin for surgical prophylaxis (alone or in combination) was independently associated with increased odds of AKI following both cardiac procedures (17.1%; aOR, 1.17; 95% CI, 1.10-1.25) and noncardiac procedures (21.0%; aOR, 1.21; 95% CI, 1.13-1.30). The addition of aminoglycosides to vancomycin was significantly associated with increased AKI risk among patients undergoing noncardiac procedures (76.6%; aOR, 1.77; 95% CI, 1.42-2.20) but was not associated with increased AKI risk among patients undergoing cardiac procedures (23.5%; aOR, 1.24; 95% CI, 0.95-1.61). Aminoglycosides alone or in combination with an antimicrobial prophylaxis other than vancomycin were not associated with increases in AKI risk among cardiac or noncardiac procedures (Table 3). Clostridium difficile infections were increased in patients who received regimens containing other types of antimicrobials (aOR, 1.53; 95% CI, 1.07- 2.19), most of which included clindamycin (1950 of 2439 [80.0%]) and/or fluoroquinolones (650 of 2439 [26.7%]).
Stratified Analysis by MRSA Status
After stratifying by MRSA status, the association of vancomycin exposure with postoperative AKI persisted among MRSA-negative patients (cardiac surgery: aOR, 1.17; 95% CI, 1.10-1.25; noncardiac surgery: aOR, 1.20; 95% CI, 1.17-1.30). The magnitude of the association was similar in MRSA-positive patients but was not statistically significant (cardiac surgery: aOR, 1.12; 95% CI, 0.80-1.56; noncardiac surgery: aOR, 1.25; 95% CI, 0.93-1.68).
Subanalysis by Combination Regimens
Among 20 876 patients undergoing cardiac procedures, 7205 (34.5%) received vancomycin plus a β-lactam, 10 611 (50.8%) received a β-lactam alone, and 3060 (14.7%) received vancomycin alone. There were 2469 episodes of AKI (34.3%) and 71 episodes of SSI (1.0%) in patients receiving combination regimens compared with 3870 episodes of AKI (28.3%) and 215 episodes of SSI (1.6%) in patients receiving either single-drug regimen. After adjustment, receipt of combination regimens was associated with statistically significant increases in all stages of Acute Kidney Injury Network–defined AKI (eTable in the Supplement); AKI risk increased with each additional day of exposure and with receipt of combination vs single-drug regimens (eFigure 2 in the Supplement). The absolute increase in AKI of 6.0% is weighed against an absolute risk reduction in SSI of 0.6%; the number needed to harm for 1 episode of AKI was 18.7 and for stage 3 AKI, typically requiring intervention such as hemodialysis, was 116; the number needed to prevent 1 SSI was 167.
Discussion
In this large, multicenter national cohort of veterans undergoing major surgical procedures, longer durations of surgical prophylaxis did not result in additional reductions in SSI but were associated with increasing harms; risk of AKI and C difficile infection consistently increased with each additional day of antimicrobial exposure (Figure 2), and risk of both types of adverse events was independent of presence of preoperative infection. Receipt of vancomycin as a prophylactic agent also appeared to be an important driver of antimicrobial-associated AKI. Critically, there appeared to be a dose-dependent association of duration with postoperative adverse outcomes. The unadjusted number needed to harm for AKI was 9 after 24 to less than 48 hours of postoperative prophylaxis, 6 after 48 to less than 72 hours, and 4 after 72 hours or more. A similar duration-dependent association in number needed to harm was found for C difficile infection (24-<48 hours, 2000; 48-<72 hours, 90; ≥72 hours, 50). Taken together, these findings suggest that strategies that limit duration of exposure to preincision and intraoperative doses only—including after cardiac surgery and implantation procedures—have the potential to maximize benefits (ie, reduction in SSIs) while minimizing harms (ie, AKIs and C difficile infections).
Current surgical prophylaxis guidelines recommend that antimicrobials be stopped within 24 hours after incision for most procedures.2 Although multisociety guidelines permit durations lasting up to 48 hours following cardiac surgical procedures,2 this recommendation is not based on any evidence demonstrating a benefit to additional doses following skin closure.4 In our study, conducted in the national VA health care system, most patients received high-quality, guideline-driven care (eFigure 1 in the Supplement). In line with prior studies, our results demonstrate no additional SSI reduction associated with extended prophylaxis beyond the initial 24-hour postoperative period. However, increasing duration of surgical prophylaxis is associated with increases in postoperative adverse events in a duration-dependent manner. Thus, these data suggest that the routine practice of continuing antimicrobial prophylaxis after skin closure should be discontinued, given that results are consistent with a lack of benefit and demonstrate preventable harm with longer regimens.
Annually, 5 antibiotic prescriptions are written for every 6 people in the United States, primarily in the outpatient setting.18 The US Centers for Disease Control and Prevention estimates that more than 30% of these prescriptions are unnecessary.5 Furthermore, antimicrobials are among the most common causes of emergency department visits for drug-related adverse events among both children and adults.19 Thus, improving antimicrobial prescribing is a major goal of the Choosing Wisely campaign,20 which aims to reduce unnecessary tests, treatments, and procedures. Our findings highlight the importance of limiting antimicrobial use in all settings.
Total antibiotic exposure is a well-characterized risk factor for antimicrobial-associated adverse events, including AKI, rash, antimicrobial resistance, and C difficile infection; however, limited data are available regarding the association of duration with tangible clinical outcomes. In many cases, clinicians prescribe expanded and prolonged antimicrobials, given the general perception among patients and health care professionals that antimicrobials may be helpful and are unlikely to cause harm.21,22 Our data can be used to inform patients and clinicians about the daily risk of increased antimicrobial exposure; these data may also be useful to antimicrobial stewardship programs by providing a more precise quantification of the increased risk of adverse events—with clear and immediate adverse effects on direct patient care—with each additional day of exposure.
Many studies have examined the nephrotoxic effects of antimicrobial regimens, particularly those containing vancomycin.8,23,24 A limitation of these studies is that they have been conducted in patients in whom acute illness may be driving AKI rather than exposure to any specific antimicrobial agent. Our study design evaluating the use of vancomycin as a prophylactic agent coupled with the sensitivity analysis excluding patients with any preoperative infection limits the potential for this confounding to drive findings and helps to clarify the role of vancomycin in the development of nephrotoxicity. Additionally, we measured the association of nephrotoxicity with combination antimicrobial regimens and found a duration-dependent increase in AKI risk. This suggests that coadministration of multiple antimicrobials may have an additive association with risk of AKI—a risk that increases with each additional day of exposure.
We stratified the analysis by MRSA status and demonstrated an increased risk of AKI among MRSA-negative patients receiving vancomycin, suggesting that the AKI associated with vancomycin is not driven solely by a higher rate of medical comorbidities in the MRSA-positive population. The risk of AKI after vancomycin among MRSA-positive patients was also evaluated and was found to be of a similar magnitude but not statistically significant, possibly owing to limited power. Clearly, in cardiac surgery, there are potential benefits of vancomycin-containing prophylaxis regimens that must be weighed against the harms (28.1% SSI reduction vs 17.7% AKI increase). A rational approach is to target vancomycin use only to those patients at highest risk of MRSA infection and to limit the duration of vancomycin exposure to preoperative and intraoperative doses only, even in patients who may benefit from upfront receipt of combination regimens. Individual patient factors—such as risk of long-term renal impairment and risk of severe disability from SSI—must also be taken into account.
Limitations
Our study is limited by its retrospective, observational nature. However, because SSI and C difficile infection are rare outcomes, these analyses would not be feasible in a randomized clinical trial owing to the large number of patients that would be required to conduct such a trial and the lack of equipoise that exists for randomizing patients to receive antimicrobials with no expectation of benefit and the likelihood of harm. While it is possible that unmeasured factors associated with increasing duration of exposure and adverse outcomes explain some of the risk, the duration-dependent nature of the association strongly suggests that the findings represent a true effect. Patients with MRSA colonization may be at inherently higher risk of AKI and simultaneously more likely to receive vancomycin than other populations. This limitation was controlled for by completing a stratified analysis among patients without MRSA colonization only; effect estimates and the duration dependent-nature of the association did not change, supporting the robustness of the findings. In addition, we focused on specific measurable adverse outcomes, and other adverse effects, such as antimicrobial resistance, hypersensitivity reactions, or red man syndrome, were not captured. These omissions likely resulted in an underestimate of the true harms associated with extending durations of prophylaxis after skin closure, whereas the quantification of the potential benefit is robust and consistent with other studies. Generalizability of our results is limited by the predominantly male population receiving care within a single closed health care system, and future studies should confirm our observations in women and in other health care settings. An additional limitation is that we were not able to fully control for clinician practice effects in the model; however, we were able to adjust for facility effects, thereby minimizing the impact of this limitation.
Conclusions
Longer durations of prophylaxis did not lead to additional SSI reduction but were associated with increases in preventable adverse events, including AKI and C difficile infection in a duration-dependent and regimen-dependent manner. Combination regimens may have an additive association with AKI risk. Choice of surgical prophylaxis affects the incidence of SSI and other adverse events. These data should be used to inform policy surrounding surgical prophylaxis and may have broader implications for antimicrobial stewardship programs aiming to reduce harms associated with unnecessary antimicrobial exposures. Every day—and every dose—matters.
eFigure 1. Mean duration of surgical prophylaxis by VA facility.
eFigure 2. Incidence of acute kidney injury following cardiac surgery, stratified by surgical prophylaxis regimen and duration of prophylaxis.
eTable. Risk of postoperative acute kidney injury and surgical site infection after receipt of single versus combination prophylaxis in patients undergoing cardiac surgery.
References
- 1.Berríos-Torres SI, Umscheid CA, Bratzler DW, et al. ; Healthcare Infection Control Practices Advisory Committee . Centers for Disease Control and Prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg. 2017;152(8):784-791. doi: 10.1001/jamasurg.2017.0904 [DOI] [PubMed] [Google Scholar]
- 2.Bratzler DW, Dellinger EP, Olsen KM, et al. ; American Society of Health-System Pharmacists; Infectious Disease Society of America; Surgical Infection Society; Society for Healthcare Epidemiology of America . Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70(3):195-283. doi: 10.2146/ajhp120568 [DOI] [PubMed] [Google Scholar]
- 3.Ban KA, Minei JP, Laronga C, et al. Executive summary of the American College of Surgeons/Surgical Infection Society surgical site infection guidelines: 2016 update. Surg Infect (Larchmt). 2017;18(4):379-382. doi: 10.1089/sur.2016.214 [DOI] [PubMed] [Google Scholar]
- 4.McDonald M, Grabsch E, Marshall C, Forbes A. Single- versus multiple-dose antimicrobial prophylaxis for major surgery: a systematic review. Aust N Z J Surg. 1998;68(6):388-396. doi: 10.1111/j.1445-2197.1998.tb04785.x [DOI] [PubMed] [Google Scholar]
- 5.Fleming-Dutra KE, Hersh AL, Shapiro DJ, et al. Prevalence of inappropriate antibiotic prescriptions among US ambulatory care visits, 2010-2011. JAMA. 2016;315(17):1864-1873. doi: 10.1001/jama.2016.4151 [DOI] [PubMed] [Google Scholar]
- 6.Bamgbola O. Review of vancomycin-induced renal toxicity: an update. Ther Adv Endocrinol Metab. 2016;7(3):136-147. doi: 10.1177/2042018816638223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hanrahan TP, Kotapati C, Roberts MJ, et al. Factors associated with vancomycin nephrotoxicity in the critically ill. Anaesth Intensive Care. 2015;43(5):594-599. [DOI] [PubMed] [Google Scholar]
- 8.Burgess LD, Drew RH. Comparison of the incidence of vancomycin-induced nephrotoxicity in hospitalized patients with and without concomitant piperacillin-tazobactam. Pharmacotherapy. 2014;34(7):670-676. doi: 10.1002/phar.1442 [DOI] [PubMed] [Google Scholar]
- 9.Crabtree T, Aitchison D, Meyers BF, et al. Clostridium difficile in cardiac surgery: risk factors and impact on postoperative outcome. Ann Thorac Surg. 2007;83(4):1396-1402. doi: 10.1016/j.athoracsur.2006.10.067 [DOI] [PubMed] [Google Scholar]
- 10.Poeran J, Mazumdar M, Rasul R, et al. Antibiotic prophylaxis and risk of Clostridium difficile infection after coronary artery bypass graft surgery. J Thorac Cardiovasc Surg. 2016;151(2):589-597.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balch A, Wendelboe AM, Vesely SK, Bratzler DW. Antibiotic prophylaxis for surgical site infections as a risk factor for infection with Clostridium difficile. PLoS One. 2017;12(6):e0179117. doi: 10.1371/journal.pone.0179117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Branch-Elliman W, Ripollone JE, O’Brien WJ, et al. Risk of surgical site infection, acute kidney injury, and Clostridium difficile infection following antibiotic prophylaxis with vancomycin plus a beta-lactam versus either drug alone: a national propensity-score-adjusted retrospective cohort study. PLoS Med. 2017;14(7):e1002340. doi: 10.1371/journal.pmed.1002340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Henderson WG, Daley J. Design and statistical methodology of the National Surgical Quality Improvement Program: why is it what it is? Am J Surg. 2009;198(5, suppl):S19-S27. doi: 10.1016/j.amjsurg.2009.07.025 [DOI] [PubMed] [Google Scholar]
- 14.The Acute Kidney Injury Network AKIN studies. http://www.akinet.org/akinstudies.php. Accessed October 1, 2018.
- 15.Goetz MB, Sayers J. Nephrotoxicity of vancomycin and aminoglycoside therapy separately and in combination. J Antimicrob Chemother. 1993;32(2):325-334. doi: 10.1093/jac/32.2.325 [DOI] [PubMed] [Google Scholar]
- 16.Moreira R, Jacinto T, Neves P, Vouga L, Baeta C. Predictors of acute kidney injury in the postoperative period of cardiac surgery associated with cardiopulmonary bypass. Rev Port Cir Cardiotorac Vasc. 2017;24(3-4):154. [PubMed] [Google Scholar]
- 17.Pourafkari L, Arora P, Porhomayon J, Dosluoglu HH, Arora P, Nader ND. Acute kidney injury after non-cardiovascular surgery: risk factors and impact on development of chronic kidney disease and long-term mortality. Curr Med Res Opin. 2018;34(10):1829-1837. doi: 10.1080/03007995.2018.1459527 [DOI] [PubMed] [Google Scholar]
- 18.US Centers for Disease Control and Prevention Outpatient antibiotic prescriptions—United States, 2014. https://www.cdc.gov/antibiotic-use/community/pdfs/annual-reportsummary_2014.pdf. Accessed June 14, 2018.
- 19.Shehab N, Lovegrove MC, Geller AI, Rose KO, Weidle NJ, Budnitz DS. US emergency department visits for outpatient adverse drug events, 2013-2014. JAMA. 2016;316(20):2115-2125. doi: 10.1001/jama.2016.16201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choosing Wisely Avoiding antibiotics overuse. http://www.choosingwisely.org/resources/updates-from-the-field/avoiding-antibiotics-overuse/. Accessed June 14, 2018.
- 21.Broniatowski DA, Klein EY, May L, Martinez EM, Ware C, Reyna VF. Patients’ and clinicians’ perceptions of antibiotic prescribing for upper respiratory infections in the acute care setting. Med Decis Making. 2018;38(5):547-561. doi: 10.1177/0272989X18770664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Livorsi D, Comer A, Matthias MS, Perencevich EN, Bair MJ. Factors influencing antibiotic-prescribing decisions among inpatient physicians: a qualitative investigation. Infect Control Hosp Epidemiol. 2015;36(9):1065-1072. doi: 10.1017/ice.2015.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Courtney PM, Melnic CM, Zimmer Z, Anari J, Lee GC. Addition of vancomycin to cefazolin prophylaxis is associated with acute kidney injury after primary joint arthroplasty. Clin Orthop Relat Res. 2015;473(7):2197-2203. doi: 10.1007/s11999-014-4062-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Filippone EJ, Kraft WK, Farber JL. The nephrotoxicity of vancomycin. Clin Pharmacol Ther. 2017;102(3):459-469. doi: 10.1002/cpt.726 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Mean duration of surgical prophylaxis by VA facility.
eFigure 2. Incidence of acute kidney injury following cardiac surgery, stratified by surgical prophylaxis regimen and duration of prophylaxis.
eTable. Risk of postoperative acute kidney injury and surgical site infection after receipt of single versus combination prophylaxis in patients undergoing cardiac surgery.