VR in pharmacy has huge potential: drug design and discovery, pharmacist education, patient counseling/behavior modification, and more. Today’s technology is more affordable, flexible, and portable, and eminently suitable for therapeutic purposes. But despite VR’s compelling features, challenges remain, such as validating clinical efficacy, cost/accessibility issues, technical capabilities, and consumer acceptance.
Abstract
Virtual reality (VR) has been widely studied and applied in numerous medical applications.1 In pharmacy, VR can potentially be applied as follows: adjunctively or as a replacement for pharmacotherapy; in drug design and discovery; in pharmacist education; and in patient counseling and behavior modification.1–6 Research applying VR in pharmacy is currently limited; however, interest in these applications is increasing. The majority of studies conducted during the past decade have found VR to be safe and effective, and to promote a high degree of user satisfaction.4 VR technology has become increasingly affordable, flexible, and portable, enabling its use for therapeutic purposes in both inpatient and outpatient environments.4 But despite the compelling features of VR, a number of challenges exist, such as validation of clinical efficacy, cost/accessibility and usability issues, technical capabilities, and acceptance.1–5 This article discusses the potential for the use of VR in pharmacy for clinical, research, and educational applications.
What is Virtual Reality?
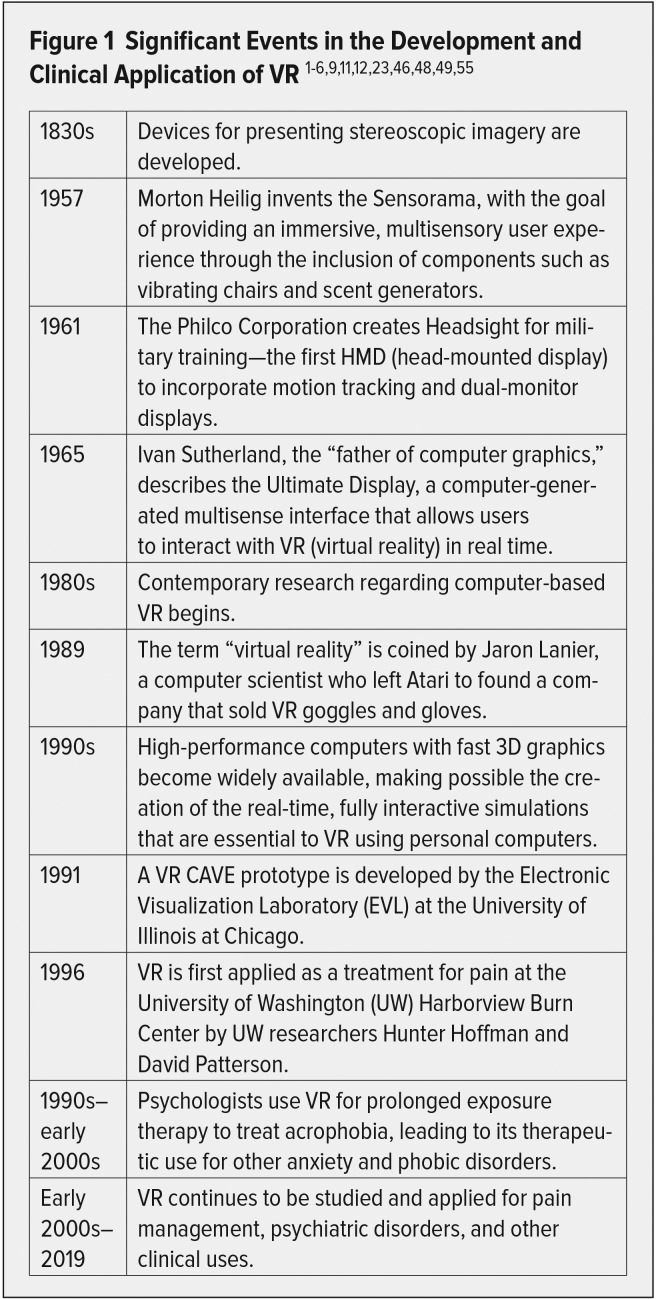
During the past century, developments in film and television, computers, the Internet, and multimedia have enhanced the power of images.7 VR was developed based on contributions from these media (see Figure 1); however, it is quite different from those technologies because it provides a sense of “presence”—the feeling of actually being within a virtual experience.8 This is achieved through the real-time, fully interactive interface of an individual with a three-dimensional (3D) computer-generated environment that stimulates multiple senses, including sight, hearing, and touch.4,9 The ability to render 3D imagery in real time was made possible by the development of more powerful computers and graphics processors.2
Figure 1.
Significant Events in the Development and Clinical Application of VR 1–6,9,11,12,23,46,48,49,55
An interactive VR system typically includes a desktop or laptop computer, a game console, or a smartphone, which is capable of real-time animation.2,4–6,8,9 The system also includes a position tracker that tracks user movement and a head-mounted display (HMD) with head-tracking systems or wall projectors for visual output.2,4,5,8,9 Display devices are particularly significant as audio-visual simulation is a key component to creating VR. The HMD fully engages the user’s field of vision, allowing him or her to perceive a 3D-stereoscopic effect through LCD displays and lenses that project different images with slightly different points of view for each eye, mimicking an observer’s viewpoint in the physical world.3,10 Motion-tracking sensors sense the user’s position in the simulated environment and supply this data to the visualization system, which updates the scene in real time.3,8,9,11 Output devices such as data gloves, joysticks, or wands provide the user with the ability to interact with virtual objects.3 Headphones are included to supply sound effects or music.3 All of these components enable the multisensory sensation of actually moving through a simulated world created by the VR system: this virtual experience can be nearly anything imaginable––from role playing with virtual patients in a pharmacy setting to physically exploring the interaction between a drug and a receptor to introducing a patient to a healthier or sicklier “virtual future self,” based upon projections of their current positive or negative habits.3
VR systems range in complexity and are available in many different arrangements.5,10 They can be as simple as a cardboard viewer and a smartphone (i.e., Google Cardboard) or as complex as whole-room arrangements known as cave automatic virtual environments (i.e., CAVEs).5,10,12 Room-scale VR navigation allows users a much greater range of motion to physically approach virtual items, whereas systems that involve a seated position use controllers to navigate the environment.5 HMD-based systems like the Oculus Rift or HTC Vive fall in the midrange of the complexity scale.10 These HMDs are relatively easy to use and program, with good display quality and affordable prices.10 The prominence of HMDs among the gaming community has been useful for health care researchers, as software programming tools that utilize HMD capabilities have become easier to use and more streamlined, even for people who don’t have a background in computer graphics programming.10
Augmented and Immersive VR
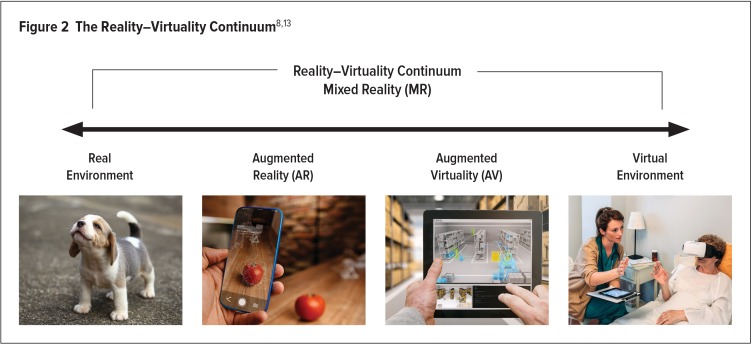
All VR systems fall within the “mixed reality” spectrum (also known as the reality–virtuality continuum), where actual physical reality and VR are positioned on opposite ends (see Figure 2). Augmented reality (AR) often involves a computer, game console, smartphone, or tablet, and an interactive HMD that allow the merging of digital content and the real environment surrounding the user.2,8 AR embellishes the real-world experience by blending “real-world elements” and “virtual elements” that may involve sight, hearing, touch, and smell.8 AR technology allows the user to perceive digitally generated elements and objects within the real-world experience.2,9 On the reality–virtuality continuum, AR falls within the range between actual reality and VR.8,13 In contrast, immersive VR completely replaces the patient’s actual environment with a virtual one.8 Full immersion is achieved with an HMD that blocks the user’s view of the real world and headphones that are designed to exclude sound from the actual environment.1,2 This provides users with a completely lifelike experience of a computer-generated world instead.1,2
Figure 2.
Although researchers began to study the health care applications of VR a number of years ago, over the past decade the technology has rapidly expanded from the entertainment industry to include uses in medicine, as well as to the currently limited but growing applications in pharmacy.3 VR systems used in health care applications are similar to those used in gaming or entertainment, but they may require specialized hardware or software.3 Sensors may be included in a system used in clinical research to allow investigators to monitor and record a patient’s level of interactivity in a reliable, safe, and replicable manner.4 VR simulators for psychotherapeutic applications may focus on emotional response and feedback, whereas those for education may focus on the generation of instructive feedback.3 HMDs are also gaining importance in medicine and pharmacy because of their use for education, visualization of data, telemedicine, telemonitoring, and other applications.6
HOW VIRTUAL REALITY WORKS
VR aims to create a virtual world parallel to reality that is both immersive and interactive.9 “Immersion” is the extent to which a user feels present in the computer-generated environment, rather than the actual physical environment.5 Users experiencing immersion within the VR-generated environment have a sense of self-location (including a feeling of being surrounded by the virtual space), and can move to explore or interact with their virtual surroundings.5 This enables them to feel a sense of actual presence in the virtual environment, and a connection between their actions and what happens within it.5
The two most important technological and experiential factors that contribute to a sense of presence are vividness and interactivity.5 Users become fully immersed in VR when disbelief is suspended and they believe that the VR experience is the real world.5,9 Technology facilitates users’ ability to have an immersive multisensory experience, within which they can naturally interact and explore.1,9 The inclusion of stereoscopic imagery is widely thought to be the most important factor that enhances immersion in the VR experience.5 Precise control of auditory, tactile, and olfactory cues by the VR system also increases the sense of presence users experience within the virtual environment.5,9 Other technological factors, such as a wide field of view or greater display resolution, are also significant.5
The immersive quality of VR “hijacks” the user’s auditory, visual, and proprioception senses, acting as a distraction that limits the ability to process stimuli from the real world.1,5 Humans have finite attentional resources, so a distraction that occupies some portion of those resources is believed to leave less cognitive ability available for processing actual physical and sensory stimuli.2,4 The entertaining and immersive effects of VR are, therefore, useful for reducing or distracting attention away from the actual internal or external environment.4 Therapeutic distraction interventions other than VR (including deep-breathing exercises, watching a video, or listening to music) have also been studied in health care.2 In a clinical context, an enhanced sense of immersion and presence is the key factor that differentiates VR from these other distractive or cognitive approaches.5 When the user is deeply engaged in such an immersive experience, it is difficult and sometimes impossible to perceive stimuli outside of the focus of attention.1
VIRTUAL REALITY APPLICATIONS IN PHARMACY
Adjunctive or Replacement Treatment for Pharmacotherapy in Pain Management
Research has demonstrated that VR is effective for the treatment of pain associated with a variety of physical and psychological illnesses.14,15 It has been found to be effective for acute or chronic pain caused by injuries, cancer, diabetic neuropathy, migraine headaches, and pruritus, as well as many other conditions.1,8,9,14 VR has also been found to be effective in treating pain associated with medical or surgical procedures, such as wound-dressing changes, intravenous-line placement, or dental work.1,8,9,14 A controlled trial comparing VR with other distraction techniques found that in children undergoing burn treatment, VR was more effective in reducing subjective pain severity than interacting with a child care worker or listening to music.16
VR is also useful in supplementing traditional pharmacotherapies and increasing analgesic efficacy.1,3,4,14 In a review of seven studies, five demonstrated that VR is an effective nonpharmacologic adjunct to standard opioid analgesic treatments.17–23 In those studies, VR was found to reduce pain, distress, and anxiety in adult and pediatric patients who were undergoing unpleasant medical procedures.17–21 Another randomized trial compared analgesia administered with and without a VR game.24 This trial demonstrated that VR combined with analgesics was significantly more effective in reducing pain in children undergoing burn treatment than were analgesics alone.24 Research has also been conducted to determine whether the benefits of VR last beyond the immediate treatment period.1 A large, randomized, controlled trial studying VR’s efficacy as an adjunct to opioid and non–opioid pain medication for the treatment of pain in medical and surgical patients was recently conducted.1 This study, which followed patients during and after their hospital stay, monitored outcomes with respect to pain levels, medication requests, and quality of life.1,25 The results of the study have not yet been published.1,25
Exactly how VR works to reduce pain perception is not known.1,5 Most proposals attribute its benefits to simple distraction,1 and the ability to perceive pain is thought to depend on a patient’s capacity to direct cognitive attention toward a painful stimulus.4,5,9,14 As humans have a finite attention capacity, a task that involves distraction such as immersing the patient in a VR environment is believed to leave less cognitive capacity available for processing pain.2–5,14 VR attenuates pain perception by indirectly or directly altering neurological signaling pathways involving attention, concentration, memory, emotion, sight, hearing, and touch.5 VR’s entertaining and immersive effects redirect the patient’s attention away from the pain, reducing anxiety, discomfort, or unpleasantness.4,14 By taking over sight, hearing, and proprioception, VR acts as a distraction to limit the patient’s capacity to process painful stimuli.1,3 Studies have shown that immersive VR technology is more likely to relieve pain than non-immersive VR.3,5
VR has also been very effective for relaxation.3 Virtual environments can be relaxing and stress-reducing, making them widely applicable for treating stress-related physical disorders that cause pain.14 These disorders, including fibromyalgia, neuropathic pain, and postherpetic neuralgia, are very common in primary care practices.14 VR that is based on a cognitive-behavioral therapy (CBT) model can train patients to shift attention away from stressful thoughts that induce pain.14 A system has been developed in which patients take a virtual meditative walk to learn mindfulness-based stress reduction, and preliminary results in patients with chronic pain suggest that it reduces subjective pain compared to non-VR mindfulness conditioning.26 Examples of other VR experiences that could be prescribed to reduce stress might include swimming with dolphins or a virtual vacation on a tropical beach.1
A study in patients with fibromyalgia also found that VR led to significant improvements regarding functional disability compared with standard treatments.27 Self-reported patient observations of reduced anxiety, time spent thinking about pain, and pain severity during VR treatment have been corroborated by neuro-imaging studies.3,4 These studies detected reduced activity in five brain regions related to sensory and emotional pain processing (thalamus, insula, anterior cingulate cortex, and primary and secondary somatosensory cortices) during VR interventions.4,5,9,28
Overall, both physiological and psychological measures suggest that VR is a helpful clinical tool in the treatment of pain.4 Perhaps the most important implication regarding its efficacy is its potential to reduce the use of opioid analgesics. The rates of addiction and misuse of opioid analgesics are staggering.29,30 According to the National Institute on Drug Abuse (NIDA), approximately 19,354 people in the U.S. died from prescription opioid-analgesic overdose in 2016.30 Furthermore, although opioid analgesics have proven to be quite effective in providing pain relief, they don’t control pain in every patient because of the development of treatmenttolerance.14 Some opioids also have a significant side-effect profile, causing nausea or increased length of hospitalization.4
VR may offer a safe and effective treatment for pain, without the many side effects or the risk of addiction associated with opioids.31 NIDA is examining the intersection of pain treatment with the abuse of and addiction to opioid medications, with the goal of developing alternative pain-management solutions (such as VR) that have less potential for addiction.14 The National Institutes of Health has also identified VR as a viable option for reducing pain and has made its development a priority, providing tens of millions of dollars in funding for research projects studying VR and pain over the past decade.29
Adjunctive or Replacement Treatment for Pharmacotherapy in Anxiety and Other Disorders
During the past few decades, the clinical application of VR has also been studied in psychotherapeutic uses for anxiety and phobia disorders.1,5 VR exposure therapy has been applied in the treatment of post-traumatic stress disorder (PTSD), generalized anxiety disorder, social anxiety disorder, panic disorder, obsessive-compulsive disorder, agoraphobia, arachnophobia, and claustrophobia.1,3,6 Traditional treatment for these disorders typically requires patients to confront the situations they fear––a form of CBT known as exposure therapy.3 If the belief remains unchallenged, avoiding a dreaded situation can reinforce anxiety and phobias.8 In exposure therapy, patients are exposed gradually to the situations they fear that provoke anxiety.3 When the catastrophic events the patient expects don’t materialize, sensory, affective, and cognitive processes are altered, anxiety attenuates with each exposure, and beliefs about the feared consequences subside.3–5,8,9 With each successive exposure to the anxiety or phobia-provoking scenario, anxiety is further reduced.8 VR exposure therapy has been used in combination with pharmacotherapy for the treatment of anxiety and phobic disorders.14,32 Pharmaceuticals primarily affect physiological systems, whereas VR treats cognitive systems.14,32 Similar to other forms of CBT, VR exposure therapy provides a treatment approach that may alleviate anxiety in ways that are not addressed by drug treatment.14
Studies have demonstrated that VR exposure therapy can achieve similar efficacy compared with traditional exposure interventions.9 VR has been broadly shown to have a significant impact on a patient’s life, resulting in long-lasting effects that reduce anxiety.9 In a review of the medical literature, four meta-analyses and seven systematic reviews on the use of VR in the treatment of emotion-, anxiety-, and stress-related disorders were identified.8 The results of these studies support the therapeutic use of VR in panic disorder, PTSD, phobias, and stress management.8 Research also indicate that patients accept and are satisfied with VR-based therapy, sometimes more so than conventional approaches.9 In a study of exposure therapy in 150 patients with specific phobias, 3% refused VR exposure whereas 27% declined real-life exposure.33 In a study of patients with PTSD resulting from motor vehicle accidents, participants reported that they were highly satisfied with VR exposure.34 A study of 352 U.S. soldiers who had enlisted after 9/11 also suggested that the high degree of acceptance of technology-based treatments (rather than in-person counseling) such as VR may reduce barriers to seeking mental health care.35
In addition to other benefits, VR is a versatile tool with which one can build as many scenarios as needed that can be replicated, monitored, and modified much more easily than real-life environments.1,5,8,9 War, storms, injury, social situations, and other anxiety- or phobia-inducing stimuli can be very challenging or expensive to recreate solely for the purpose of exposure therapy.3,9 VR offers a convenient and inexpensive option for constructing complex or impractical exposure scenarios.3,9 For example, for veterans with PTSD, VR has been used to simulate traumatic scenarios, complete with the sound of artillery blasts, the vibration of rolling military vehicles, and the smell of burning oil.1,5 VR also permits the adjustment of elements that are present in a virtual simulation to make them more or less threatening, such as the physical characteristics of a space, the presence of protective elements, or the duration of a situation.8,9
Recent studies have also shown that exposure to multiple VR contexts reduces recurrent fear to a greater extent than exposure to a single scenario.36 In addition, VR allows the construction of “virtual adventures” at different difficulty levels in which subjects are immersed in an environment that allows them to experience themselves as competent and effective.8 While immersed in a virtual adventure, patients discover that they can overcome the conflicts or situations they fear through effort and confrontation.8 An even more fantastic feature of VR is that unrealistic worlds can be simulated, if necessary.8 For example, patients can experience a world that enables them to travel back in time, allowing them to relive a sequence of events in which they can intervene to change the outcome, which can lead to transformative effects.8
VR has also been employed in the treatment of addiction, eating disorders, and autism.6,8 Two systematic reviews revealed that VR stimuli (e.g., drugs, alcoholic drinks, or cigarettes) and environments (e.g., a party or bar) are effective at inducing cravings for alcohol, cigarettes, or cocaine in dependent subjects.37,38 Using VR in patients with addictions allows them to develop coping skills in response to a cue that induces cravings, through repeated exposure and practice in a controlled setting.39 As reported by three systematic literature reviews, VR was also found to be effective in changing a patient’s response to cue exposure involving food stimuli in the treatment of obesity and eating disorders.40–43 In these disorders, VR is used to reinforce nutritional education and provide visual feedback and simulations that improve self-perception and body image.5 Furthermore, VR has been used in the treatment of autistic spectrum disorder because of its ability to provide a controlled setting in which patients can develop new skills.8 Two systematic reviews support the use of VR to help patients with autism learn communication and imitation skills, to assist them in coping with social situations.44,45
Pharmacological Modeling for Drug Discovery
VR offers a number of advantages compared to other computer-based approaches used in drug design and discovery, including a far superior 3D-view of molecular structures and targets.46 Over the last few decades, the number of drugs approved by the FDA has not kept pace with rising drug-development costs, so a rapid and efficient approach to drug development is critical.46 There are also numerous drug targets that have not yet been exploited.46 In 2017, there were a total of 1,578 FDA-approved drugs that act against 893 pathogen-derived and human targets.46 This is a small portion of the more than 4,479 potential drug targets listed in Ensembl (ensembl.org) that can be investigated for the potential development of novel, more effective drugs.46,47
Immersive VR has tremendous prospects for its use in molecular modeling for the identification and design of novel candidates for drug development.10,46 In drug design and discovery, visualization tools serve an important role with respect to the investigation of interactions between ligands that are potential drugs and macromolecules.10,46 Accurate visualization of the way ligands bind to large, complex structures like proteins is critical.10,46 VR allows researchers to observe the dynamics of protein-structure configurations while they focus on ligand-binding sites and other areas of interest.10 In the context of antimicrobial resistance, viewing protein structures and understanding how mutations lead to changes in their binding regions is essential.10 This ability is crucial for predicting the modifications that are necessary to create more effective next-generation drugs.10
VR offers several advantages over traditional visualization tools such as 2D projections or 3D physical models, which can obscure important molecular features.10 For example, it can provide researchers with a more accurate perception of a protein’s catalytic pocket than 2D projections can provide.10 Such information can translate into modifications that can be incorporated into the design of more effective drugs.10 Through VR systems, researchers can also participate in the simulation process, rather than merely being observers of automatic simulations.10,46 VR drug modeling allows real-time haptic interaction with the molecule, as well as the ability to customize representations of macromolecules (e.g., DNA, RNA, protein, sugar molecules, or whole viruses).10,46 The immersive nature of VR can conceivably provide solutions to issues encountered during visualization, as it allows the scientist to experience and interact with molecular models by “stepping inside” them.10,46
Researchers can explore and select ligands for investigation based on biochemical parameters such as distance, binding energy, and bonding information.46 They can then drag and rotate the ligand within the binding site to make instantaneous modifications.46 In this way, scientists can observe and interact with the ligand-target complex to identify more efficiently conformational changes and the ligands that are suitable candidates for drug development.10,46 The information gathered can then be translated to the design and synthesis of new drug candidates in the laboratory.46 This approach is much more informative and less tedious and time-consuming than the traditional use of algorithms for this purpose.46
Moreover, VR is reportedly more accurate and efficient at identifying drug-like ligands compared to traditional approaches such as fragment or diversity-oriented methods.46 With the rapid advancement and increasing affordability of computer hardware and software packages, VR is becoming more accessible to researchers; thus, its application in drug development will likely become more widespread and accelerate the development of new drugs.10,46 VR can also serve as an educational tool for the general public to enhance their understanding of biochemical research and drug discovery.10
Pharmacist Education and Training
The use of VR in pharmacist education and training offers a new method for novel instructive experiences, reinforcing lessons, and learning assessment.6,11,48–50 VR is currently more commonly used in nursing and medical education, although several features favor its use for pharmacist training.48,50 Using VR in pharmacy education affords opportunities for engaged and active learning, as well as an entertaining instructional experience.48,50 VR may also be helpful to pharmacy students who prefer visual learning opportunities rather than reading textbooks.31 It can also create difficult-to-simulate scenarios, or be used to standardize situations during testing.49 The use of VR to simulate pharmacy environments could help students practice techniques such as compounding medications, or the procedures required for working in a community or hospital pharmacy setting.50 VR’s ability to simulate a real-life experience through role playing allows users to improve clinical and communication skills by learning from their mistakes when providing care to virtual patients.6,48–51 Through VR, this can be done without the health or financial consequences brought about by mistakes that can occur in a real-life environment.6,48,50,51
VR can also be used to teach pharmacology. When learning pharmacology, pharmacy students are required to understand how drugs and receptors interact,31 but as drugs and receptors are three-dimensional, this information can be difficult to illustrate and explain during classroom sessions.31 Therefore, students may be better able to learn drug-receptor interactions by viewing a 3D model rather than the 2D graphics that are often presented during lectures.31,50 Anatomy and physiology could also be taught through 3D schematics that incorporate demonstrations of how drugs affect specific organ systems to achieve clinical outcomes.50 At present, although researchers have access to VR software and hardware that could be used for medical education, the technology is not yet widely applied in undergraduate programs.31 Instead, 2D representations are still commonly used during pharmacy lectures, as they can be easily viewed by a large group of students.31
VR also allows pharmacy students to access and interact with different VR scenarios remotely, facilitating distance learning or training.49,50 Students can participate in continuing education courses or attend lectures or medical conferences irrespective of geographical location.48,50 This is particularly important in rural areas where pharmacists have limited access to training opportunities.48 Umeå University in northern Sweden has been using VR for instruction since the inception of its clinical pharmacy course in 2011.48 All pharmacy courses at the university are offered as distance-education courses in a web-based online format, and most of the teaching takes place online.48 Students can access training opportunities in a 3D VR world, where simulated ward rounds and patient meetings occur.48 Eighty-three percent of the 42 students who completed an online evaluation stated that they felt they could adopt the role of a clinical pharmacist while using this technology.48 The environment was described as feeling authentic by 60% of the students, although some participants noted that it “could never be the same” as interacting with real patients.48 The students described their experiences as “fun,” “new and exciting,” “exceeding expectations,” and helpful for easing into the role of a clinical pharmacist.48 However, some students commented that the technical aspects of VR took too much time, distracting them from work for other courses.48
Despite the positive results from this and other studies, more research is needed to assess the effectiveness of VR instruction and barriers to its implementation.49 Beyond pharmacy education, VR can also be used in pharmacy practice to simulate work processes, consumer or staff behavior, or some other study of the work environment to improve procedures and outcomes.7 Further, VR scenarios incorporating facts and values can be used in the context of decision making regarding pharmaceutical care.7
Patient Counseling and Behavior Modification
In recent years, the practice of pharmacy has evolved from simply dispensing drugs to a more service-based model, where pharmacists counsel patients on how to prevent and manage disease.51 Trends in health care are moving toward a stronger emphasis on preventive medicine and healthier behaviors, and pharmacist expertise can help to achieve these goals.51 The implementation of VR for patient counseling and care can assist pharmacists in serving this function.51
Pharmacist–patient meetings have been shown to be important for patient compliance.48 The availability of VR systems in pharmacies can promote medication-therapy management and help patients develop a medication-related action plan, advancing safe and efficacious medication use.11,51 VR applications for medication management are available for use by geriatric patients and in inpatient aftercare.6 The educational use of VR apps that provide visual and auditory instructions regarding standard medication safety and efficacy could be implemented when a patient receives a new prescription.11 For more complex medication regimens, the VR system could demonstrate techniques or administration procedures, such as how to self-administer an injectable medication.11 Patients could then use the system to perform these behaviors virtually, allowing them to practice without harming themselves or wasting medication.11 Through feedback, VR can also be used to confirm that patients correctly understand and can perform the technique they were taught.11 While the immediate recitation of what was just experienced in a VR session does not necessarily equate to long-term retention and application of what was learned, it does allow for patient practice and the opportunity for the pharmacist to identify misunderstandings.11
As VR technologies grow and evolve, they can play an even greater role in the promotion of health and disease prevention to combat one of the major challenges of chronic disease management and/or prevention—the lack of reinforcement that patients experience when implementing healthy behavior changes.51 VR centers in pharmacies could use computer algorithms to predict how positive and negative changes made in patients’ behavior today may affect their body and health in a number of years or decades.51 Predicted conditions could be generated from extensive data programmed into these machines based on existing knowledge of how nutrition, activity, medication use, current laboratory measures, ethnicity, and family history predict disease and health in the future.51 VR could be used to demonstrate the deleterious effects that cigarette smoking, weight gain, or alcohol abuse has on a patient’s body at designated time intervals in the future.51
Patients could experience their predicted reality using HMDs with head tracking, motion tracking, surround-sound audio, olfactory stimulus, and an advanced bodysuit with sensors that provide feedback—emphasizing strength with improved health and exercise, or accentuating fatigue in sickly individuals who are sedentary.51 Having patients actually experience or “live” in this predicted body could be an effective means of demonstrating the importance of healthy behaviors and incentivizing them to modify their lifestyles.4,51 Indeed, research has shown future health status to be an important motivator for patients to change.51 If patients with diabetes suddenly see themselves hooked up to a dialysis machine or missing a foot, they may become more motivated to control their blood glucose and blood pressure.51 Generating a future virtual body that is better (or less) able to function in the world as a result of current deleterious or future improved habits is the focus for VR use in patient behavior modification.51
Long recognized as the most accessible providers in the health care system, pharmacists are in an excellent position to encourage behavior modification in patients.51 Pharmacists could act as coaches, helping patients to prioritize their behavior changes and work toward finding feasible goals and achievements that can be maintained over time.51 Pharmacists could work with patients to identify behavioral changes that could be programmed into the VR system to demonstrate how their new habits might change their future appearance and health.51 Through the availability of VR technologies to reinforce pharmacist recommendations, patients could be instantly gratified by actually seeing, feeling, and even smelling what the future may hold for them if they were to implement the healthy strategies recommended by the pharmacist.4,51
VR technology can be extremely effective in motivating patients to implement and sustain positive lifestyle changes.51 For behavior modification, patients have used VR to facilitate weight loss and increase physical activity, helping to combat eating disorders, diabetes, and obesity.4,51 VR has also been used to help patients improve body-image perceptions and self-sufficiency, promote healthier eating habits, and help patients practice healthy decision making through inhabiting realistic avatars in stress-inducing virtual situations, such as food shopping.4
CHALLENGES
Validation of Clinical Efficacy
Although it generally yields positive results, the use of VR in clinical research presents multiple challenges.5 A list of these challenges and other barriers to the use of VR is included in Table 1. Still in its early stages, research involving VR technology faces practical and theoretical obstacles that prevent the thorough validation of clinical efficacy.5 Studies to date demonstrate efficacy for various clinical applications of VR, but there is a need for better designed studies to show both clinical effectiveness and cost effectiveness.4,5,8 Among the deficiencies that have been identified are poor study design, small sample sizes, lack of control groups, varying technical standards for techniques and tools, and lack of consideration of economic feasibility.1,5,9 Also, published study results often fail to mention adverse reactions, such as motion sickness, dry eyes, or headache.2
Table 1.
Validation of Clinical Efficacy
|
VR: virtual reality; HMD: head-mounted display; EHR: electronic health record
Researchers have recommended that future clinical studies of VR should utilize larger samples, assess patient adherence, follow better standardized clinical protocols, and investigate long-term effects.1,4,8 Post-treatment assessments should ideally occur over a follow-up period of at least 12 months, to assess treatment effects over time.9 These issues need to be addressed to improve the rigor of VR clinical research and the significance of its findings.5 To this end, an international working group of VR experts recently met to standardize and create best practices for VR clinical research; an article summarizing the committee’s recommendations was published in January 2019.52
VR applications and hardware introduce another variable that can differ greatly between clinical studies.5 Some studies involve 2D images that are projected onto video screens; 360° 2D presentations in HMDs; or room-sized virtual environments created by CAVE projection systems.5 Other studies involve a 3D virtual environment viewed with motion-tracked stereoscopic HMDs.5 The audio used in clinical studies also varies: some studies use non-spatial audio and others use positional stereo sound that changes as users moves their head or body.5 In other cases, the VR equipment that was used in a clinical study is not well defined.5 VR hardware and software also change quickly as a result of rapid advancements in the field.5 Clinical studies only one year apart may differ with regard to hardware or software capabilities, which may affect the consistency and reproducibility of results.5
If VR is to be used for clinical applications, then a “virtual pharmacy” also needs to be developed so that the correct VR experiences can be prescribed for and accessed by patients.1 According to the medical literature, VR software influences treatment outcomes, and virtual environments for medical therapies should vary according to the patient’s specific symptoms.3 For example, for psychotherapeutic applications, software that allows the therapist to control panoramic photos, videos, and interaction methods according to therapeutic progress may be helpful.3 The best features for VR treatments to relieve pain symptoms also need to be further investigated.14 VR simulations that allow the “cyber dosage” for pain relief to be dialed up or down as appropriate, either by the health care provider or the patient, may be helpful.14 A system to evaluate and quantify the effects of the clinical application of VR therapy alone or combined with other therapeutic methods is also needed.3,14
Cost/Accessibility
Early VR studies used costly platforms that were unlikely to be adopted for widespread use; however, the affordability and accessibility of VR has since improved.4 Nevertheless, in some circumstances, the cost of VR equipment may remain a barrier to its use,49 and development of VR software applications is also expensive.5 This presents a significant disadvantage for disseminating VR in clinical settings, especially large-scale trials or settings involving multiple users.5,9 Although the cost of HMDs has dropped, quality VR environments still require expensive, high-end computer systems with advanced graphics processing.5 As of October 2018, the cost of a portable system to run a quality VR clinical experience was estimated at $2,500 per unit, plus maintenance.5,51 A room-sized, fully immersive system, such as a CAVE, can be much more expensive, with low-end systems priced in the tens of thousands of dollars and high-end systems in the hundreds of thousands of dollars.31,53,54 An expenditure this size may be beyond the budget of some research or academic institutions.31 Attrition also causes the value of VR equipment to decline rapidly when newer technology makes older equipment obsolete.5 Often, a system is expected to retain only minimal value three years after its purchase.5
Lower-cost VR systems have become available as prices have decreased over time.1,9 Smartphone-based systems are now available starting at $600, and VR HMDs that tether to a computer have been available for around $400 since 2016.11 However, there is a caveat with this increased affordability, as there is evidence that the efficacy of VR therapy is at least partially dependent on the quality of the equipment used.3,4 For example, one review identified two clinical studies in which the use of low-cost HMD visors and off-the-shelf VR software to treat burn patients did not achieve significant differences in self-reported pain measures or anxiety.4,23,55 Further investigation is needed to determine the association between higher-end hardware or software and clinical efficacy.4 Still, the decline of prices to what could be considered a reasonable expense may allow VR systems to become routinely available in health care settings, such as pharmacies and doctors’ offices.11 Decreasing prices could also allow VR to be used for patient self-care, both in the hospital and at home.3,4 Despite the expenses associated with VR, it is still generally considered to be an effective and efficient tool within the areas it has been studied, compared to many traditional medical approaches.3
Although it is difficult to predict whether health insurance will pay for VR medical applications, some companies may do so, seeing the model is consistent with many existing health care plans.51 For example, plans that focus on preventive medicine and a healthy lifestyle may reimburse for VR equipment or treatment sessions.51 Important health care issues, such as the high prevalence of diabetes and the rapid rise of obesity (both of which can be prevented through education and behavior modification using VR sessions), have become a national focus.51 The Patient Protection and Affordable Care Act has also strongly oriented the health care system toward preventive care and the avoidance of hospital readmission.51
Usability
In the past, VR systems were difficult to set up and would frequently malfunction, creating a barrier to their use.9 Although the usability of VR technology has improved, the possibility of glitches and malfunctions still exists, creating a potential disadvantage for clinicians and patients.5,9 Technical difficulties and the need for in-depth training to achieve technical proficiency remain the primary obstacles to VR use.5,48 VR equipment should be considered as a tool that requires users to be properly trained to resolve possible malfunctions so that clinical care is not interrupted.5,9,48 Vendors that sell systems for VR therapy often offer Internet-based training as well as onsite instruction.9 This training generally includes information regarding the rationale for incorporating VR into patient care; troubleshooting glitches; and contacting the vendor.9 It is expected that the more widespread the medical application of VR becomes, the more proficient users will become.48
Another impediment interfering with usability is the adverse physical effects that can occur with VR, such as dizziness, nausea, headache, and eyestrain, i.e., “cybersickness.”5,50 HMDs can also be heavy and cumbersome, which may be a problem for patients with limited head or neck mobility resulting from injury or a medical condition.5 Furthermore, most current VR applications are not usable for patients with visual or cognitive disabilities, because of difficulties interacting with the VR interface.5 High-end HMDs are tethered to a computer, which can be a tripping hazard or distraction, especially for elderly patients.5 Elderly patients may also have difficulty using VR software because of a lack of computer or video-game literacy.5 Prolonged exposure to an HMD screen, which is just a few centimeters away from the user’s eyes, leads to eyestrain and headaches.5 An educational lecture can last hours, and some users cannot comfortably use VR equipment for more than 10 minutes.56 This issue may improve as the technology advances; however, the length of time a patient engages with VR during a health care application may need to be constrained.50,56
It is important to discuss these limitations with patients in advance, especially those participating in long-term clinical studies.5 In addition, most VR research has taken place in clinical settings, so there is much that needs to be determined regarding in-home applications of VR.5 There are common considerations regarding the in-home use of any technology, such as the learning curve, logistics, and technical support.5 However, some additional challenges are associated with VR, such as the need for dedicated space and the potential for interference, especially by pets or children.5 Room-scale VR systems require at least 5 ft2 of dedicated space in a patient’s living environment, which may interfere with the usability of the space for other purposes.5 VR-system cables may also create tripping hazards, and infrared sensors can interfere with other electronic devices, such as TV remote controls.5 The motion-tracking calibration of VR equipment is also very sensitive and can be easily disturbed by moving the equipment.5 Despite these disadvantages, users in home, clinical, or educational settings often remain enthusiastic to participate in VR studies or treatment.1,5,9,48
Technical Capabilities
The technical capabilities of VR systems are currently limited, as the systems are not responsive to input delivered by the user’s voice.11 This capability is necessary for implementing teach-back exercises during educational use.11 Another ideal feature for systems is the incorporation of data from other devices, such as wearable technologies that track weight, exercise, diet, blood glucose levels, and other factors.11 Ideally, a VR system could analyze these data comprehensively and make associations with the patient’s state of health, as well as positive and negative projections regarding whether certain behaviors and habits (e.g., smoking, caloric intake, medication adherence) are maintained or changed.11 With the increasing use of electronic health records and patient portals, these tools may eventually be used as an access point through which VR systems can collect patient data.11 Ultimately, technological advancements in medicine may make it possible to collect data through biosensors used for monitoring during medical procedures.2
There is also a need to improve the virtual participants and environments depicted in VR systems.48 At present, avatars in VR applications are not especially realistic, which may adversely affect the ability of clinicians and patients to fully immerse themselves in a patient-care scenario.49 Facial expressions, physical gestures, and visual cues may not seem authentic; these limitations in nonverbal communication may reduce VR’s effectiveness in role-playing scenarios and as a replacement for face-to-face meetings.48,49 The efficacy of pain relief achieved with VR has also been shown to be correlated with the technological capabilities of the equipment or system.4,8,23,55 The more advanced the equipment, the greater the sense of presence in the virtual world, a factor that has been identified as necessary for alleviating pain.3 With time and investment in further technological development, the equipment is likely to become more sophisticated, with the inclusion of speech recognition and more realistic avatars with authentic physical gestures and facial expressions.49
Acceptance
In spite of increasing awareness regarding VR in the medical and pharmacy community, whether and how to apply this technology in everyday clinical practice remains unclear.1 The extent to which patients will accept VR also remains to be seen.1 During many clinical studies, most subjects found VR to be a pleasant and positive experience, which at a minimum provides a distraction from the anxiety and distress associated with illness.1,5 Most subjects state that they would opt to use VR again, should the opportunity arise.1 It is also true that younger patients, generally speaking, tend to be more willing and able to use VR than older patients.1 Some patients also find the equipment to be confusing, uncomfortable to use, or difficult to operate1, and some occasionally describe VR experiences as having an unclear benefit.1 With regard to using VR in education, students and teachers may prefer traditional instructional approaches, creating a barrier to implementation.48 Having to design lessons that utilize VR could place a burden on teachers to create learning exercises that fulfill specific teaching goals.48 For these reasons, support may be required to encourage teachers to move away from traditional instructional methods and explore VR as a new approach to teaching and learning.48
CONCLUSION
Although it is still novel, the application of VR in pharmacy has significant potential.4 With further research, more data will become available regarding its efficacy in this arena, as well as other advantages and disadvantages.1 As the technology improves, costs and other obstacles will be reduced, likely increasing VR’s influence as a viable and helpful instrument in clinical, research, educational, and patient-counseling practices in pharmacy.4
Footnotes
Disclosure: The author reports no commercial or financial interest in regard to this article.
REFERENCES
- 1.Spiegel BM. Virtual medicine: how virtual reality is easing pain, calming nerves, and improving health [published online May 21, 2018] Med J Aust. 2018;209(6):245–24. doi: 10.5694/mja17.00540. [DOI] [PubMed] [Google Scholar]
- 2.Chirico A, Lucidi F, DeLaurentiis M, et al. Virtual reality in health system: beyond entertainment. A mini-review on the efficacy of VR during cancer treatment. J Cell Physiol. 2016;231(2):275–287. doi: 10.1002/jcp.25117. [DOI] [PubMed] [Google Scholar]
- 3.Li L, Yu F, Shi D, et al. Application of virtual reality technology in clinical medicine. Am J Transl Res. 2017;9(9):3867–3880. [PMC free article] [PubMed] [Google Scholar]
- 4.Dascal J, Reid M, Ishak WW, et al. Virtual reality and medical inpatients: a systematic review of randomized, controlled trials. Innov Clin Neurosci. 2017;14(1–2):14–21. [PMC free article] [PubMed] [Google Scholar]
- 5.Garrett B, Taverner T, Gromala D, et al. Virtual reality clinical research: promises and challenges. JMIR Serious Games. 2018;6(4):e10839. doi: 10.2196/10839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grand View Research. Augmented reality (AR) and virtual reality in healthcare market analysis by component (hardware, software, and service), by technology (augmented reality, virtual reality), and segment forecasts, 2018–2025. May, 2017. [Accessed March 19, 2019]. Available at: https://www.grandviewresearch.com/industry-analysis/virtual-reality-vr-in-healthcare-market.
- 7.Mobach MP. The virtual pharmacy, 3D becomes reality? Pharm World Sci. 2005;27(4):271–272. doi: 10.1007/s11096-005-2801-y. [DOI] [PubMed] [Google Scholar]
- 8.Riva G, Baños RM, Botella C, et al. Transforming experience: the potential of augmented reality and virtual reality for enhancing personal and clinical change. Front Psychiatry. 2016;7:164. doi: 10.3389/fpsyt.2016.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maples-Keller JL, Bunnell BE, Kim SJ, Rothbaum BO. The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv Rev Psychiatry. 2017;25(3):103–113. doi: 10.1097/HRP.0000000000000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ratamero EM, Bellini D, Dowson CG, Römer RA. Touching proteins with bare hands: visualizing protein-drug complexes and their dynamics in self-made virtual reality using gaming hardware [published online June 7, 2018] J Comput Aided Mol Des. 2018;32(6):703–709. doi: 10.1007/s10822-018-0123-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fox BI, Felkey BG. Virtual reality and pharmacy: opportunities and challenges. Hosp Pharm. 2017;52(2):160–161. doi: 10.1310/hpj5202-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Electronic Visualization Laboratory (EVL) The CAVETM virtual reality theater. [Accessed March 19, 2019]. Available at: https://www.evl.uic.edu/cave.
- 13.Milgram P, Kishino F. A taxonomy of mixed reality visual displays. IEICE Trans Inf Syst. 1994;12(12):1321–1329. [Google Scholar]
- 14.Wiederhold BK, Soomro A, Riva G, Wiederhold MD. Future directions: advances and implications of virtual environments designed for pain management. Cyberpsychol Behav Soc Netw. 2014;17(6):414–422. doi: 10.1089/cyber.2014.0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.University of Washington Human Photonics Laboratory (HPL) Virtual reality pain reduction. [Accessed March 19, 2019]. Available at: www.vrpain.com.
- 16.van Twillert B, Bremer M, Faber AW. Computer-generated virtual reality to control pain and anxiety in pediatric and adult burn patients during wound dressing changes. J Burn Care Res. 2007;28(5):694–702. doi: 10.1097/BCR.0B013E318148C96F. [DOI] [PubMed] [Google Scholar]
- 17.Schmitt YS, Hoffman HG, Blough DK, et al. A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns [published online August 7, 2010] Burns. 2011;37(1):61–68. doi: 10.1016/j.burns.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoffman HG, Patterson DR, Seibel E, et al. Virtual reality pain control during burn wound debridement in the hydrotank. Clin J Pain. 2008;24(4):299–304. doi: 10.1097/AJP.0b013e318164d2cc. [DOI] [PubMed] [Google Scholar]
- 19.Patterson DR, Jensen MP, Wiechman SA, Sharar SR. Virtual reality hypnosis for pain associated with recovery from physical trauma. Int J Clin Exp Hypn. 2010;58(3):288–300. doi: 10.1080/00207141003760595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li WH, Chung JO, Ho EK. The effectiveness of therapeutic play, using virtual reality computer games, in promoting the psychological well-being of children hospitalised with cancer [published online June 8, 2011] J Clin Nurs. 2011;20:2135–2143. doi: 10.1111/j.1365-2702.2011.03733.x. [DOI] [PubMed] [Google Scholar]
- 21.Carrougher GJ, Hoffman HG, Nakamura D, et al. The effect of virtual reality on pain and range of motion in adults with burn injuries. J Burn Care Res. 2009;30(5):785–791. doi: 10.1097/BCR.0b013e3181b485d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kipping B, Rodger S, Miller K, Kimble RM. Virtual reality for acute pain reduction in adolescents undergoing burn wound care: a prospective randomized controlled trial [published online February 18, 2012] Burns. 2012;38(5):650–657. doi: 10.1016/j.burns.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 23.Morris LD, Louw QA, Crous LC. Feasibility and potential effect of a low-cost virtual reality system on reducing pain and anxiety in adult burn injury patients during physiotherapy in a developing country [published online December 21, 2009] Burns. 2010;36(5):659–664. doi: 10.1016/j.burns.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 24.Das DA, Grimmer KA, Sparnon AL, et al. The efficacy of playing a virtual reality game in modulating pain for children with acute burn injuries: a randomized controlled trial. BMC Pediatr. 2005;5(1):1. doi: 10.1186/1471-2431-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clinicaltrials.gov. Immersive virtual reality intervention for non-opioid pain management: a randomized, controlled trial. NCT02887989. Sep 2, 2016. [Accessed March 20, 2019]. Available at: https://clinicaltrials.gov/ct2/show/NCT02887989.
- 26.Gromala D, Tong X, Choo A, Karamnejad M. The virtual meditative walk: virtual reality therapy for chronic pain management. Proceedings of the 33rd Annual Association for Computing Machinery Conference on Human Factors in Computing Systems; New York. New York: Association for Computing Machinery; 2015. [Accessed March 20, 2019]. pp. 521–524. Available at: https://dl.acm.org/citation.cfm?id=2702123. [Google Scholar]
- 27.Garcia-Palacios A, Herrero R, Vizcaíno Y, et al. Integrating virtual reality with activity management for the treatment of fibromyalgia: acceptability and preliminary efficacy. Clin J Pain. 2015;31(6):564–572. doi: 10.1097/AJP.0000000000000196. [DOI] [PubMed] [Google Scholar]
- 28.Hoffman HG, Richards TL, Coda B, et al. Modulation of thermal pain-related brain activity with virtual reality: evidence from fMRI. Neuroreport. 2004;15(8):1245–1248. doi: 10.1097/01.wnr.0000127826.73576.91. [DOI] [PubMed] [Google Scholar]
- 29.Thomas DA. Virtual reality research continues to progress at the National Institutes of Health. Cyberpsychol Behav Socl Netw. 2014;17(6):334. doi: 10.1089/cyber.2014.1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.National Institute on Drug Abuse. Overdose death rates. Jan, 2019. [Accessed March 20, 2019]. Available at: https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates.
- 31.Richardson A, Bracegirdle L, McLachlan SI, Chapman SR. Use of a three-dimensional virtual environment to teach drug-receptor interactions. Am J Pharm Educ. 2013;77(1):11. doi: 10.5688/ajpe77111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wiederhold MD, Wiederhold BK. Virtual reality and pharmaceuticals: enhanced synergy to improve clinical care. [Accessed March 20, 2019];Cyber-Therapy & Rehabilitation Magazine. 2013 1:10–12. Available at: http://vrphobia.eu/files/cr-611.pdf. [Google Scholar]
- 33.Garcia-Palacios A, Botella C, Hoffman H, Fabregat S. Comparing acceptance and refusal rates of virtual reality exposure therapy vs. in vivo exposure by patients with specific phobias. Cyberpsychol Behav. 2007;10(5):722–724. doi: 10.1089/cpb.2007.9962. [DOI] [PubMed] [Google Scholar]
- 34.Beck JG, Palyo SA, Winer EH, et al. Virtual reality exposure therapy for PTSD symptoms after a road accident: an uncontrolled case series. Behav Ther. 2007;38(1):39–48. doi: 10.1016/j.beth.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 35.Wilson J, Onorati K, Mishkind M, et al. Soldier attitudes about technology-based approaches to mental health care. Cyberpsychol Behavior. 2008;11(6):767–769. doi: 10.1089/cpb.2008.0071. [DOI] [PubMed] [Google Scholar]
- 36.Shiban Y, Pauli P, Mühlberger A. Effect of multiple context exposure on renewal in spider phobia [published online November 11, 2012] Behav Res Ther. 2013;51(2):68–74. doi: 10.1016/j.brat.2012.10.007. [DOI] [PubMed] [Google Scholar]
- 37.Bordnick PS, Carter BL, Traylor AC. What virtual reality research in addictions can tell us about the future of obesity assessment and treatment. J Diabetes Sci Technol. 2011;5(2):265–271. doi: 10.1177/193229681100500210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hone-Blanchet A, Wensing T, Fecteau S. The use of virtual reality in craving assessment and cue-exposure therapy in substance use disorders. Front Hum Neurosci. 2014;8:844. doi: 10.3389/fnhum.2014.00844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Riva G. Virtual reality for health care: the status of research. Cyberpsychol Behav. 2002;5(3):219–225. doi: 10.1089/109493102760147213. [DOI] [PubMed] [Google Scholar]
- 40.Ferrer-García M, Gutiérrez-Maldonado J. The use of virtual reality in the study, assessment, and treatment of body image in eating disorders and nonclinical samples: a review of the literature [published online November 25, 2011] Body Image. 2012;9(1):1–11. doi: 10.1016/j.bodyim.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 41.Ferrer-García M, Gutiérrez-Maldonado J, Riva G. Virtual reality based treatments in eating disorders and obesity: a review [published online June 25, 2013] J Contemp Psychother. 2013;43(4):207–221. doi: 10.1007/s10879-013-9240-1. [DOI] [Google Scholar]
- 42.Koskina A, Campbell IC, Schmidt U. Exposure therapy in eating disorders revisited [published online November 29, 2012] Neurosci Biobehav Rev. 2013;37(2):193–208. doi: 10.1016/j.neubiorev.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 43.Wiederhold BK, Riva G, Gutiérrez-Maldonado J. Virtual reality in the assessment and treatment of weight-related disorders. Cyberpsychol Behav Soc Netw. 2016;19(2):67–73. doi: 10.1089/cyber.2016.0012. [DOI] [PubMed] [Google Scholar]
- 44.Aresti-Bartolome N, Garcia-Zapirain B. Technologies as support tools for persons with autistic spectrum disorder: a systematic review. Int J Environ Res Public Health. 2014;11(8):7767–7802. doi: 10.3390/ijerph110807767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.den Brok WL, Sterkenburg PS. Self-controlled technologies to support skill attainment in persons with an autism spectrum disorder and/or an intellectual disability: a systematic literature review [published online May 22, 2014] Disabil Rehabil Assist Technol. 2014;10(1):1–10. doi: 10.3109/17483107.2014.921248. [DOI] [PubMed] [Google Scholar]
- 46.Liu XH, Wang T, Lin JP, Wu MB. Using virtual reality for drug discovery: a promising new outlet for novel leads. Expert Opin Drug Discov. 2018;13(12):1103–1114. doi: 10.1080/17460441.2018.1546286. [DOI] [PubMed] [Google Scholar]
- 47.Ensembl. Jan, 2019. [Accessed March 20, 2019]. Available at: http://www.ensembl.org/index.html?redirect=no.
- 48.Gustafsson M, Englund C, Gallego G. The description and evaluation of virtual worlds in clinical pharmacy education in Northern Sweden [published online August 21, 2017] Curr Pharm Teach Learn. 2017;9(5):887–892. doi: 10.1016/j.cptl.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 49.Fertleman C, Aubugeau-Williams P, Sher C, et al. A discussion of virtual reality as a new tool for training healthcare professionals. Front Public Health. 2018;6:44. doi: 10.3389/fpubh.2018.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Aungst T. Digital realities could find a place in the pharmacy classroom. Pharmacy Times. Mar 8, 2018. [Accessed March 20, 2019]. Available at: https://www.pharmacytimes.com/contributor/timothy-aungstpharmd/2018/03/digital-realities-could-find-a-place-in-the-pharmacy-classroom-
- 51.Nuffer W, Smith SM, Trinkley K. Integrating virtual reality to expand the public health role of community pharmacists. J Am Pharm Assoc. 2013;53(2):152–158. doi: 10.1331/JAPhA.2013.12200. [DOI] [PubMed] [Google Scholar]
- 52.Birckhead B, Khalil C, Liu X, et al. Recommendations for methodology of virtual reality clinical trials in health care by an international working group: iterative study. JMIR Ment Health. 2019;6(1):e11973. doi: 10.2196/11973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Miller SA, Misch NJ, Dalton AJ. Low-cost, portable, multi-wall virtual reality. Presentation at IPT/EGVE 2005: 9th International Workshop on Immersive Projection Technology, 11th Eurographics Workshop on Virtual Environments; Aalborg, Denmark. 2005; [Accessed March 20, 2019]. Available at: http://ntrs.nasa.gov/archive/nasa/casi.ntrs.nasa.gov/20050240930.pdf. [Google Scholar]
- 54.Gaudiosi J. Dassault Systèmes uses HTC Vive to replace CAVE virtual reality tech. Fortune. Jan 8, 2016. [Accessed March 20, 2019]. Available at: http://fortune.com/2016/01/08/dassault-systemes-htc-vive/
- 55.Kipping B, Rodger S, Miller K, Kimble RM. Virtual reality for acute pain reduction in adolescents undergoing burn wound care: a prospective randomized controlled trial [published online February 18, 2012] Burns. 2012;38(5):650–657. doi: 10.1016/j.burns.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 56.Kuehn BM. Virtual and augmented reality put a twist on medical education. JAMA. 2018;319(8):756–758. doi: 10.1001/jama.2017.20800. [DOI] [PubMed] [Google Scholar]