Abstract
Introduction
Liver disease forms a global health burden and is a cause of significant morbidity and mortality. Good patient education has proven to be a key tool in disease management, providing significant benefit in knowledge and behavioral modifications. To develop effective educational tools, a good understanding of patient educational needs and preferred learning methods is necessary. Few studies have evaluated the educational needs of patients with liver disease. This study aims to assess the educational needs of patients at a large tertiary liver center.
Method
This study was a questionnaire-based cross-sectional study evaluating patient demographics,perceived and unperceived educational needs (hepatitis B and hepatitis Cknowledge) at a tertiary liver centre
Results
A total of 300 patients completed the questionnaire. Most patients stated they were “extremely” or “quite” interested in learning more about their liver condition (84.9%, n=242), in either “moderate” or “a lot of” detail (94.6%, n=202). There was no association between gender, age, level of education, annual income and interest of patients in learning more about their liver condition. There was a significant association between number of clinic visits and interest to learn more (p=0.022), but there was no association between the duration of their follow-up at the clinic and their interest to learn more (p=0.243).
Conclusions
Overall, patients showed great interest in learning more about their liver condition, potentially indicating a need for more educational programs. Most patients prefer reading (via internet or pamphlets/brochures) or one-to-one discussions, giving us a good sense of potentially successful educational strategies that will fit the needs of most patients.
Keywords: Cirrhosis, Liver disease, Patient education, Patient knowledge
INTRODUCTION
Liver disease with all its etiologies forms a global health burden and is a cause of significant morbidity and mortality. Despite recent advancements in treatment options, the global impact of liver disease on morbidity and mortality remains quite significant (1, 2), with an estimated 30% increased mortality in the past eight years (3). In Canada, the major etiologies of liver disease are alcoholic liver disease, chronic viral infections (hepatitis B and C) and fatty liver (4). Many of these conditions lead to long-term consequences such as cirrhosis and hepatocellular carcinoma (HCC). Adherence to medications, diet, follow-up appointments and appropriate self-care are all key factors in improving quality of life and preventing long-term complications in these patients (5).
Good patient education has proven to be a key tool in disease management, providing significant benefit in knowledge and behavioral modifications (5). It has been shown that the wide variation in patient knowledge may affect patients’ willingness to accept and adhere to medical interventions (6). Studies show that patient knowledge across many types of liver disease is quite low, albeit difficult to accurately estimate (7). A systematic review found that simple educational interventions for patients with viral hepatitis significantly increased patients’ knowledge about their disease (5). More complex educational interventions may also lead to positive behavioral changes. Although many studies have assessed patient knowledge, there is a lack of focus on patient perceptions and whether their actual knowledge correlates well with their self-perceived knowledge. Several studies have addressed the perceived educational needs of patients with liver disease (7–12) with variable results.
In order to develop effective education tools, it is essential that healthcare educators are aware of the perceived and unperceived needs of their patients, as well as their preferred learning methods. Although there are currently many educational tools available for patients with liver disease worldwide, comprehensive patient education modules that are tailored to the specific needs of these patients are yet to be developed in Canada. The high degree of heterogeneity of liver disease and the wide variety of potential comorbid conditions suggest that patients warrant specialized educational programs using a variety of educational strategies. This is supported by one of Canada’s hepatitis C (HCV) strategies which aim to reduce the health and social impact of hepatitis B (HBV) and HCV on the liver health of Canadians through the development, delivery and evaluation of peer-driven and focused educational initiatives. This would ensure that initiatives are culturally appropriate and target various learning styles, languages and literacy levels (13).
This cross-sectional study assesses the learning needs of liver disease patients in the form of a paper-based questionnaire. It was conducted at a large tertiary liver centre in Canada. This study is unique in that it is the first to include patients with various types of liver disease, as most studies to date have assessed patients with HBV or HCV. It is also one of the few studies that assesses both the perceived and unperceived needs of patients with viral hepatitis. The data collected will provide information to develop relevant education modules for patients with all types of liver disease, which will in turn aim to improve their understanding of the disease and allow them to become active participants in their own care.
METHODOLOGY
Study subjects
Surveys were distributed randomly to patients presenting for outpatient appointments at the Toronto Liver Centre from March to December 2015. A pilot survey was distributed initially, and questions were altered prior to study commencement based on feedback from patients. Implied consent was obtained with an explanatory document and the entirely voluntary nature of participation. Patients presenting to the clinic had a variety of liver disease, including HBV, HCV, compensated and decompensated cirrhosis, and autoimmune liver disease. No transplant patients are followed at this clinic. Patients are referred to this clinic by any local or regional physician. Patients who could not fill out the survey on their own could seek the help of a family member or a clinic volunteer. Patients who participated once were asked not to fill out the survey during another visit. Patients who did not wish to participate were not counted, but may have been asked to fill out the survey on a subsequent clinic visit. The study protocol was approved by the University Health Network Research Ethics Board in Toronto, Ontario.
Measures
The survey contained 54 questions covering several domains. Survey questions were designed to cover the goals of this study:
• Demographic information: This section of the survey contained 10 questions covering patient gender, year of birth, formal education status, annual income, English language fluency, preferred language (reading and speaking), type of liver condition(s), duration of follow-up at the liver clinic and approximate number of visits to the clinic to date.
• Perceived educational needs: This section contained 18 questions using a Likert scale, as well as both open- and close-ended questions. It aimed to assess current perceived knowledge level, preferred learning styles, learning topics, educational materials and interest in support groups.
• Unperceived educational needs: HBV and HCV knowledge was assessed using 26 questions covering several knowledge domains: diagnosis, symptoms, complications, treatment, self-care, modes of transmission and prevention. These questions were designed by the authors based on prior patient assessment questionnaires. Patients with HBV or HCV were asked to answer these. Questions were not subdivided into those pertaining to HBV or HCV.
RESULTS
Standard descriptive statistical methods were used. Data collection included 300 completed surveys.
Patient demographics
The socio-demographic characteristics of the study group are shown in Table 1. Our sample consisted of 50.5% males (n=150) and 49.5% females (n=147), with the remaining not specifying a gender. Mean age was 50.4 years (SD=14.4). Baseline data indicated that about half of patients (47.62%, n=140) had completed a formal college or university degree, while 2.38% of patients (n=7) had no formal education.
Table 1.
Patient demographics
| n, % | Response rate | |
|---|---|---|
| Gender | 99% | |
| Male n, % | 150, 50.51 | |
| Female n, % | 147, 49.49 | |
| Age, years | 78% | |
| Mean ± SD | 50.41 ± 14.37 | |
| Formal Education n, % | 98% | |
| College/Uni (Postgrad) | 140, 47.62 | |
| Some College/Uni | 55, 18.71 | |
| High School | 48, 16.33 | |
| Some high school | 27, 9.18 | |
| Elementary | 12, 4.08 | |
| None | 7, 2.38 | |
| Other | 5, 1.7 | |
| Annual Income n, % | 78% | |
| <30,000$ | 95, 35.19 | |
| 30–60,000$ | 53, 19.63 | |
| 60–100,000$ | 41, 15.19 | |
| >100,000$ | 44, 16.3 | |
| Liver Condition(s) n, % | 94% | |
| HBV | 50, 17.67 | |
| HCV | 114, 40.28 | |
| Both HBV & HCV | 2, 0.71 | |
| Other | 83, 29.33 | |
| Did not know | 34, 12.01 | |
| Duration of follow-up | 90% | |
| <6 months | 47, 17.47 | |
| 6–12 months | 43, 15.99 | |
| 1–3 years | 66, 24.54 | |
| 3–5 years | 40, 14.87 | |
| >5 years | 73, 27.14 | |
| Number of appointments | 99% | |
| First visit | 48, 16.22 | |
| <5 visits | 98, 33.11 | |
| >5 visits | 150, 50.68 |
Regarding self-reported liver disease, the majority of patients had HBV or HCV or both. There were 84 patients (29.7%) who had other types of liver disease. Twelve per cent of patients (n=34) did not know what type of liver disease they had. The remaining patients (5.7%, n=17) did not specify their type of liver disease.
Perceived needs
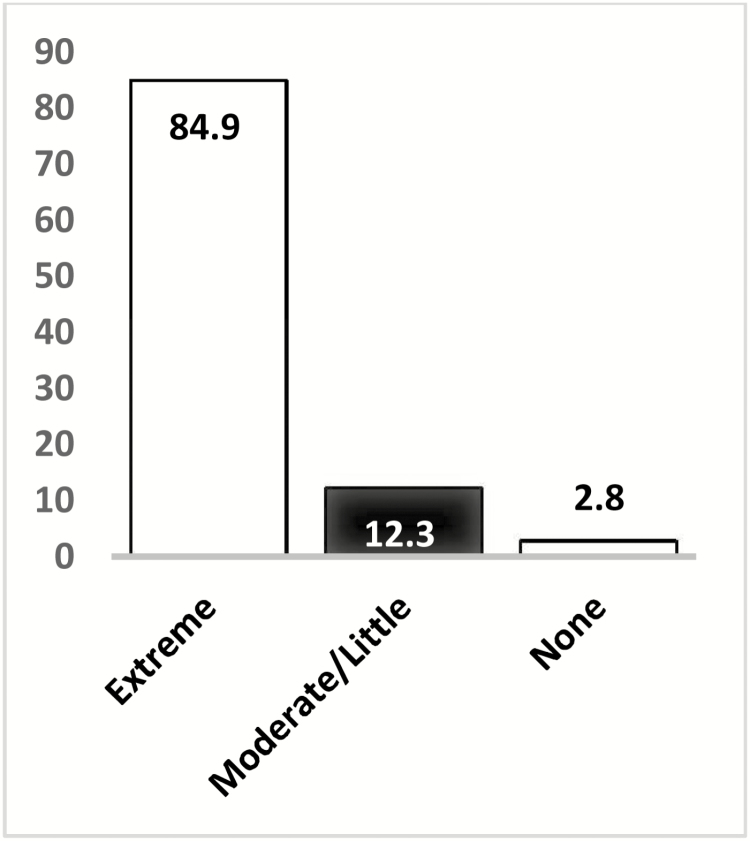
Regarding the interest of patients in learning more about their liver condition, response rate was 95% (n=285). Most patients stated they were “extremely” or “quite” interested (84.9%, n=242). Thirty-five patients (12.3%) had little-moderate interest, with eight patients (2.8%) stating they had no interest at all (Figure 1). Of those, 200 patients responded further and stated they would like to learn “moderate” or “a lot” of details (96%, n=192), with the remainder stating they would only like to learn basics (4%, n=8).
Figure 1.
Interest in learning about liver condition (%, n=285).
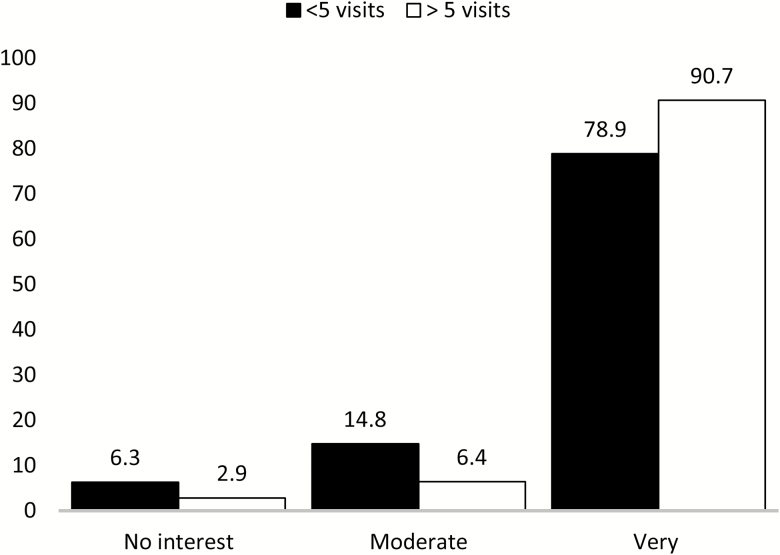
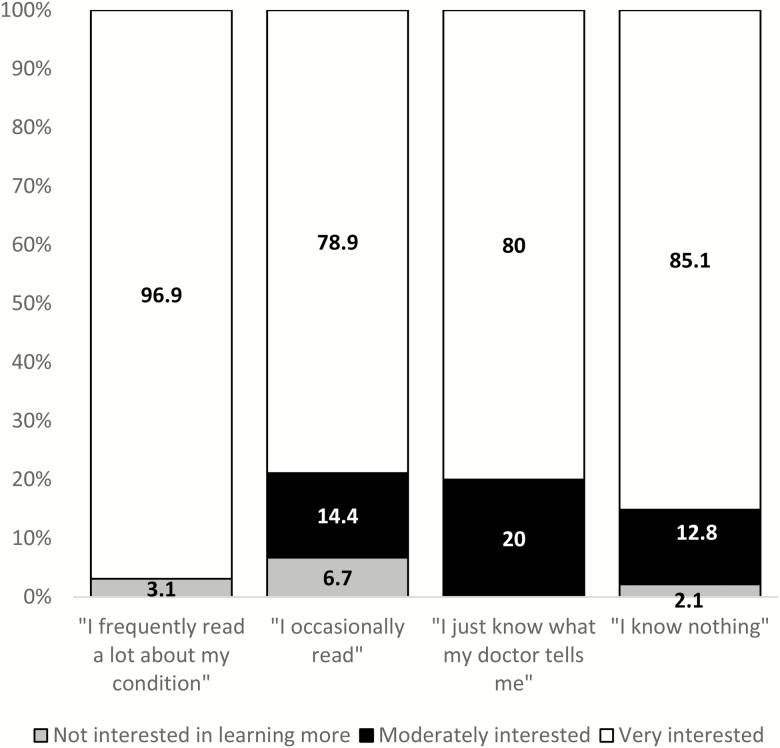
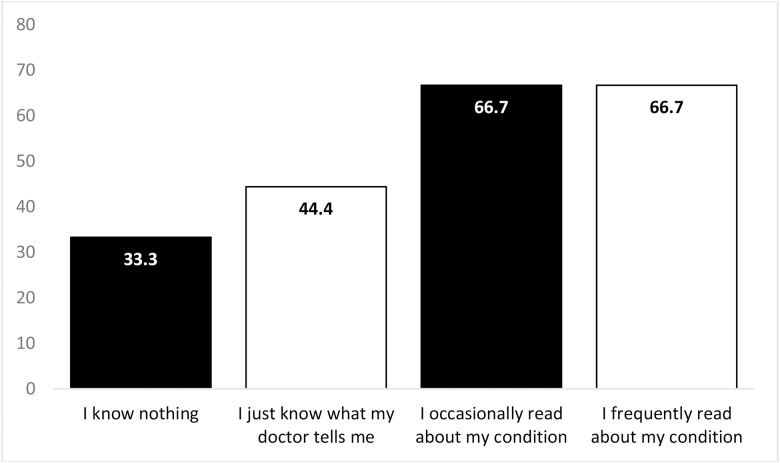
There was no association between gender, age, level of education, annual income and interest of patients in learning more about their liver condition. There was a significant association between number of clinic visits and interest to learn more. Patients who have visited the clinic more times are more interested in further education about their condition than those who have visited less frequently (97.1% versus 93.7%, p=0.022, Figure 2). Interestingly, there was no association between the duration of their follow-up at the clinic and their interest to learn more (p=0.243), which may reflect patients who have been followed long-term for chronic stable conditions. There was also a significant association between patient interest in learning more and current self-perceived knowledge about liver condition. Patients with greater interest in learning more seem to self-perceive their knowledge as being greater than those with less interest (p=0.004, Figure 3).
Figure 2.
Association between number of clinic visits and interest in learning (%, p=0.022).
Figure 3.
Association between patient interest in learning more and current self-perceived knowledge about liver condition (%, p = 0.004).
Preferred learning methods
Almost all patients stated they learned best by reading (n=170, 56.7%) or one-on-one discussions (n=155, 51.7%). The remaining patients stated they learned best with videos (n=82, 27.3%) or group discussions (n=28, 9.3%). A small number of patients preferred other learning methods (n=7, 2.3%), which included learning from their physician, flyers or the internet.
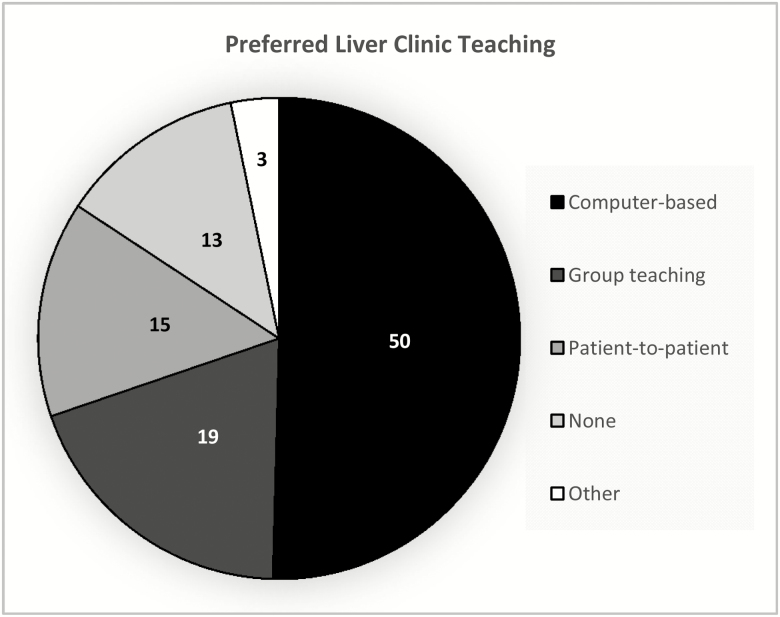
Of the preferred reading materials, most patients preferred the internet (n=189, 63%) or pamphlets/brochures (n=118, 39.3%). The remaining patients preferred books (n=92, 30.7%), preferred not to read (n=17, 5.7%) or preferred other reading material (n=5, 1.7%). When asked about the types of teaching at the liver clinic (Figure 4), more than 80% of patients were interested in computer-based (n=125, 41.7%) or one-to-one teaching (n=132, 44%), with the remainder choosing group teaching (n=48, 16%), patient-to-patient (n=36, 12%), none (n=31, 10.3%) or other (n=8, 2.7%).
Figure 4.
Preferred teaching methods at liver centre (%).
Unperceived needs
A set of 26 questions (true or false and multiple choice questions—MCQs) were used to assess the knowledge of HBV and HCV patients. A total of 166 patients answered these questions. Knowledge domains covered in the questions were diagnosis, prevention, transmission, complications and treatment of HBV and HCV.
Mean correct answers was 52% (±24.4%). We also found a significant association between current self-perceived knowledge about liver condition and test score percentages (Figure 5).
Figure 5.
Mean test scores and self-perceived knowledge about liver condition (%, p< 0.001).
DISCUSSION
It is well-established that good patient education has proven to be a key tool in disease management, providing significant benefit in knowledge and behavioral modifications (1). The wide variation in patient knowledge may affect patients’ willingness to accept and adhere to medical interventions (6). A recent study showed that online resources concerning HBV and HCV which are accessed by patients are beyond the previously determined necessary grade level for patients to properly comprehend (14). Although patient education programs are aimed at providing teaching to help improve patient outcomes, these programs are not always targeted at specific patient interests and personal goals. Overall, there is an increasing need to provide more targeted educational resources to patients.
This study is unique in that it is the first to evaluate the educational needs of patients with various types of liver disease, as most studies to date have only assessed patients with viral hepatitis. This is also one of the few studies to assess both the perceived and unperceived needs of this patient population. The data aims to provide information to develop more specific education modules for patients with all types of liver disease, which will in turn aim to improve their understanding of the disease and allow them to become active participants in their own care.
In this study, patients showed interest in learning more about all aspects of their liver condition in great detail. Preferred methods of learning varied, but most patients preferred reading or one-to-one discussions. Almost half of the patients included in the study had completed postgraduate education, which may be a reflection of their high interest in patient education and may have skewed the results. The only association found between interest in learning more was with the number of clinic visits. Patients with more clinic visits showed more interest in education about their condition. Interestingly, there was no association between the duration of their time as clinic patients and their interest to learn more. This may reflect patients who have been followed long-term for chronic stable conditions, as compared with patients with more acute or severe conditions who have visited the clinic more often in a shorter period of time. There was also a significant association between patient interest in learning more and current self-perceived knowledge about their liver condition. This association was also found between patient knowledge scores and their self-perceived knowledge. This indicates good patient insight on their knowledge (or lack thereof).
Several limitations to this study are acknowledged. Although the study included 300 patients with various liver conditions, the questionnaire could be validated with a larger sample size. Also, the generalizability of findings may be influenced by several methodological limitations. Study sample represented outpatients at a tertiary hospital from many different socioeconomic backgrounds with a variety of different liver conditions. The severity of these liver conditions or the impact of their illness on quality of life was not measured. Thus, the need for education in patients with more severe liver disease may have been underestimated. Also, many patients were highly educated, which may have affected the overall results.
Results of this study provide information to help develop relevant educational modules for patients with all types of liver disease. Although the results do indicate that there is a wide variation in patient interest and preferred learning methods, patients were generally quite interested in learning more about their condition. This study also provides a sense of the types of educational programs that would be of greater interest. It is noteworthy that even at a large liver clinic with many available educational programs, patients still felt there was a lack of educational opportunities. As healthcare providers who aim to provide patients with highly effective learning around their liver condition, it is critical that we address these needs. Since every liver clinic will have a unique patient population, the results will likely differ. Future studies should aim at designing a standardized needs assessment questionnaire that may be used at different liver clinics to help identify specific educational needs. It would also be useful to validate the questionnaire in other languages to cater to a larger patient population.
In conclusion, this study suggests that there is a need for more detailed educational resources for patients with all types of liver disease. Educational programs should be tailored to the needs of the target population in order to be more effective.
Author Contributions
SSA contributed to data collection and analysis. Both authors contributed equally to questionnaire development, manuscript writing and editing.
Acknowledgments
The authors thank all members of the Toronto Liver Centre who contributed to survey input and distribution.
Funding: None.
Conflict of interest: None to declare.
References
- 1. Lavanchy D. The global burden of hepatitis C. Liver Int 2009;29(Suppl 1):74–81. [DOI] [PubMed] [Google Scholar]
- 2. Gower E, Estes C, Blach S et al. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol 2014;61(Suppl 1):S45–57. [DOI] [PubMed] [Google Scholar]
- 3. Foundation CL. Liver Disease in Canada. A Crisis in the Making. Vol. 2017, 2013. [Google Scholar]
- 4. Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: Part I. Diagnosis and evaluation. Am Fam Physician 2006;74(5):756–62. [PubMed] [Google Scholar]
- 5. Shah HA, Abu-Amara M. Education provides significant benefits to patients with hepatitis B virus or hepatitis C virus infection: A systematic review. Clin Gastroenterol Hepatol 2013;11:922–33. [DOI] [PubMed] [Google Scholar]
- 6. Saha S, Freeman M, Toure J et al. Racial and Ethnic Disparities in the VA Healthcare System: A Systematic Review. Washington (DC), 2007. [PubMed] [Google Scholar]
- 7. Jennings AR. Assessing educational needs of potential hepatitis C patients at a Veterans Affairs medical center. Educ Health 2011;24(3):532. [PubMed] [Google Scholar]
- 8. Dahl TF, Cowie BC, Biggs BA et al. Health literacy in patients with chronic hepatitis B attending a tertiary hospital in Melbourne: A questionnaire based survey. BMC Infect Dis 2014;14:537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Balfour L, Cooper C, Tasca GA et al. Evaluation of health care needs and patient satisfaction among hepatitis C patients treated at a hospital-based, viral hepatitis clinic. Can J Public Health 2004;95(4):272–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fabris P, Tositti G, Giordani MT et al. Assessing patients’ understanding of hepatitis C virus infection and its impact on their lifestyle. Aliment Pharmacol Ther 2006;23(8):1161–70. [DOI] [PubMed] [Google Scholar]
- 11. North CS, Devereaux R, Pollio DE et al. Patient perspectives on hepatitis C and its treatment. Eur J Gastroenterol Hepatol 2014;26(1):74–81. [DOI] [PubMed] [Google Scholar]
- 12. Bornschlegel K, Crotty KJ, Sahl S et al. Unmet needs among people reported with hepatitis C, New York City. J Public Health Manag Pract 2011;17(4):E9–17. [DOI] [PubMed] [Google Scholar]
- 13. Responding to the Epidemic. Recommendations for a Canadian Hepatitis C Strategy. Vol. 2017, 2005. [Google Scholar]
- 14. Meillier A, Patel S, Al-Osaimi AM. Readability of healthcare literature for hepatitis B and C. Dig Dis Sci 2015;60:3558–62. [DOI] [PubMed] [Google Scholar]