Abstract
Previous measures of childhood adversity have enabled the identification of powerful links with later-life wellbeing. The challenge for the next generation of childhood adversity assessment is to better characterize those links through comprehensive, fine-grained measurement strategies. The expanded, retrospective measure of childhood adversity presented here leveraged analytic and theoretical advances to examine multiple domains of childhood adversity at both the micro-level of siblings and the macro-level of families. Despite the fact that childhood adversity most often occurs in the context of families, there is a dearth of studies that have validated childhood adversity measures on multiple members of the same families. Multilevel psychometric analyses of this childhood adversity measure administered to 1,194 siblings in 500 families indicated that the additional categories of childhood adversity were widely endorsed, and increased understanding of the sources and sequalae of childhood adversity when partitioned into within- and between-family levels. For example, Multilevel Confirmatory Factor Analyses (MCFAs) indicated that financial stress: bills/food, unsafe neighborhood, and parental unemployment were often experienced similarly by siblings in the same families and stemmed primarily from family-wide (between-family) sources. On the other hand, being bullied and school stressors were often experienced differently by siblings and derived primarily from individual (within-family) processes. Multilevel Structural Equation Modeling (MSEM) further illuminated differential criterion validity correlations between these categories of childhood adversity with midlife psychological, social, and physical health. Expanded, multi-domain and multilevel measures of childhood adversity appear to hold promise for identifying layered causes and consequences of adverse childhood experiences.
Keywords: childhood adversity measurement, validation, multilevel factor analysis
The discovery of powerful links between childhood adversity and physical and psychosocial health in adulthood (e.g. Felitti et al., 1998; Springer, Sheridan, Kuo, & Carnes, 2007; Taylor, Lerner, Sage, Lehman, & Seeman, 2004) has inspired a surge of interest in childhood adversity measurement in recent years (Cronholm et al., 2015; Finkelhor, Shattuck, Turner, & Hamby, 2013; Mersky, Janczewski, & Topitzes, 2017). Although the growing number of childhood adversity tools have resulted in better measurement, there remains a need for a comprehensive, standard measure of childhood adversity (Finkelhor, Shattuck, Turner, & Hamby, 2015; McLaughlin, 2016). In addition, although much of what shapes adversity in childhood is related to family-level processes, no existing studies have validated a childhood adversity measure on multiple siblings within families. This paper describes a process of creating and testing an expanded retrospective measure of childhood adversity that builds on three established measures of adversity, adds items absent from these measures that have recently been indicated as important elements of childhood adversity, and examines the validity of a multi-domain structure of adversity as it occurs both among siblings nested within families and across families.
Three measures have been foundational to shaping studies of the long-term effects of childhood adversity and abuse. The Adverse Childhood Experiences (ACE) scale was developed for a study of 13,494 adults who were found to display a strong, graded relationship between reported abuse and household dysfunction during childhood and a variety of adult health disorders (Felitti et al., 1998). The abuse items in the ACE scale were taken from Straus et al.’s (1998) Parent-Child Conflict Tactics Scale (CTS-PC), an adaptation of their widely-used Conflict Tactics Scale. Around the same time, based on allostatic load theory (McEwen, 1998), the Risky Family Environment measure (Repetti et al., 2002; Taylor et al., 2004) was adapted from the ACEs scale to examine how warmth and conflict in the childhood family environment are associated with mental and physical health across the lifespan.
Childhood adversity measures have traditionally been conceptualized as containing multiple events that contribute to an overall childhood adversity score (Ford et al., 2014; McLaughlin & Sheridan, 2016). However, this approach can obscure differential sources and effects of particular adverse experiences (Green et al., 2010; Savla et al., 2013), as well as how certain types of events may co-occur (Scott, Burke, Weems, Hellman, & Carrión, 2013). For example, although the 11 ACE items have been found to be intercorrelated (Ford et al., 2014; Mersky et al., 2017), factor analyses using one overall factor structure implicitly assume all of these diverse events stem from the same underlying cause, an unlikely representation of real-world experience. Additionally, although previous findings have been mixed as to whether specific types of childhood adversity are tied to specific adult outcomes (e.g. Green et al., 2010; Iniguez & Stankowski, 2016; McLaughlin & Sheridan, 2016), differentiating meaningful subscales of adversity could assist in identifying unique pathways between adversities and later life outcomes. Lastly, traditional childhood adversity measures have not separated parent-specific dysfunction during childhood (e.g., parental substance abuse) from that of other household members. Given that family systems theories and empirical studies support the powerful role of parents in shaping the well-being of children (Chen, Miller, Kobor, & Cole, 2011; Morris, Robinson, Hays-Grudo, Classen, Hartwig, & Treat, 2017), this study investigated whether differentiating parent-related events could add validity to the interpretation of childhood adversity test scores.
Recent research has also highlighted the importance of new categories of adverse events absent from traditional measures, events which could improve the validity of test score interpretations. The original ACEs measures encompassed psychological, physical, and sexual abuse, as well as household substance abuse, mental illness, criminal behavior, and domestic violence toward mother (Felitti et al., 1998). Later versions incorporated parental divorce (Ford et al., 2014), as well as emotional and physical neglect (Scott et al., 2013). Recent studies have supported the utility of additional items not included in the ACEs measure (e.g. Finkelhor, Shattuck, Turner, & Hamby, 2013; Wade, Shea, Rubin, & Wood, 2014), especially socioeconomic (SES) stressors and bullying from peers, which have been found to be associated with later life functioning (Copeland et al., 2014; Culpin, Stapinski, Miles, Araya, & Joinson, 2015). Socioeconomic disadvantage during childhood is commonly studied as a marker for chronic environmental stress, one of the strongest risk factors for mental and physical illness (Conger, Ge, Elder, Lorenz, & Simons, 1994; Evans & Kim, 2013). Being bullied during childhood is also increasingly understood to be detrimental to adult health and social functioning (Wolke, Copeland, Angold, & Costello, 2013).
Other new adverse childhood experiences in this measure include exposure to violence outside the home and school stressors (Cronholm et al., 2015; Wade et al., 2014), family physical illness (Finkelhor, Shattuck, Turner, & Hamby, 2013), caregiver separation (McLanahan, Tach, & Schneider, 2013; Mersky et al., 2017), stressful transitions such as multiple house moves and blending step-families (Tiet et al., 1998), and death of a close family member (Berg, Rostila, Saarela, & Hjern, 2014; Fletcher, Mailick, Song, & Wolfe, 2013). Two other seemingly important childhood events – parental death and divorce – have had mixed results with later life outcomes in recent literature, and needed further examination (Finkelhor et al., 2015; Green et al., 2010; Hetherington, 2005; Mersky et al., 2017; Wallerstein, 1991). Lastly, recent domestic violence research indicates that children’s exposure to spousal abuse against fathers as well as mothers has a negative impact on later functioning (Douglas & Hines, 2016), and so both were included.
Multilevel Psychometric Analyses
Although childhood adversities often occur in the family context, few studies have measured childhood adversity in multiple siblings within the same families (for exceptions, see Hines, Kantor, & Holt, 2006 and Laporte, Paris, Guttman, Russell, & Correa, 2012). Furthermore, to our knowledge, no existing psychometric studies have used multilevel modeling to validate a childhood adversity measure administered to siblings. Indeed, although the field has come to a general consensus that multilevel analyses are necessary for hypothesis testing with clustered data to avoid biased statistical inference (Geiser, 2013), much less research has utilized multilevel psychometric analyses to validate measures given to non-independent respondents (Dedrick & Greenbaum, 2011; Geldhof, Preacher, & Zyphur, 2014). However, multilevel psychometric analyses are also necessary when measures are administered to nested samples, as separate validities of test score interpretations may exist at each level (Geldhof et al., 2014). Furthermore, developing a valid measure of childhood adversity at both the micro-level of siblings and the macro-level of families would pave the way for studies clarifying the mechanisms underlying associations between childhood adversity and later life outcomes at different levels. Childhood adversity may vary within-families due to differences in siblings’ genes, perceptions, personality, and experiences, and between-families as a result of family-wide characteristics that are associated with childhood adversities, such as family structure, resources, and geographical location (Dedrick & Greenbaum, 2011; Dick, Johnson, Viken, & Rose, 2000; Geiser, 2013). Multilevel studies examining childhood adversity and adult well-being in siblings raised in the same families have the potential to control for variation at either level, distinguishing the source of associations with later life outcomes (Dick et al., 2000).
Conceptualizing Childhood Adversity
After identifying a list of items and factors of childhood adversity based on past literature, it was also important to establish a correctly-specified model in terms of the direction of influence between measured items and latent constructs (Edwards & Bagozzi, 2000). This direction of influence has important implications for understanding causes and consequences (Bollen, 1984; Bollen & Diamantopoulos, 2015). Well-known internal consistency psychometric analyses such as factor analyses assume items in each factor are “reflective,” meaning they all arise from the same underlying construct and should covary. Measures of broad constructs such as childhood adversity may also include “formative” items which do not necessarily stem from any common underlying source, but do contribute to the construct being measured (Bollen, 1984; Edwards & Bagozzi, 2000).
For both theoretical and data analytic reasons, we specified a model with three between-family reflective factors (Chaotic Families, Stressful Environments, Poor Family-Environment Fit), six within-family reflective factors (Family Conflict, Impaired Caregiving, Parental Dysfunction, Financial Insecurity, Poor Child-Environment Fit, Household Dysfunction), and six formative items. Theoretically, we had anticipated greater variation among siblings within a family than at the between-family level, given the understanding that individuals are likely to have more nuanced experiences than overall families. Data analytically, fewer between-level factors than within-level factors is a common finding in MCFA studies (e.g. Dedrick & Greenbaum, 2011; Miller, Chen, & Parker, 2011; Wright, Beltz, Gates, Molenaar, & Simms, 2015), since most items have less variance at the between-level than at the within-level, as well as a smaller sample size (a smaller number of families than the total number of siblings). The six formative childhood adversity items were conceptualized as Independent Unfortunate Events that would occur more randomly and not necessarily co-vary with other items or factors (see Table 1).
Table 1.
Origin, Prevalence, and ICCs for Childhood Adversity Items, In Order of Prevalence
| Adversity Item | Origin | N | (%) | ICC |
|---|---|---|---|---|
| Witnessed or experienced family conflict | RF | 903 | 75.95 | 0.50 |
| Minor assault: spanked, slapped, pinched | ACE, CTS-PC, RF | 846 | 71.15 | 0.32 |
| Emotional abuse | ACE, CTS-PC, RF | 686 | 57.70 | 0.39 |
| Teased or bullied by peers | New | 505 | 42.47 | 0.18 |
| Financial stress: bills, food | New | 500 | 42.05 | 0.66 |
| Parent substance abuse | ACE, RF | 377 | 31.71 | 0.86 |
| Domestic violence between adults | ACE, RF | 320 | 26.91 | 0.70 |
| Parent mental illness | ACE | 308 | 25.90 | 0.66 |
| Family serious physical illnessa | New | 306 | 25.74 | 0.51 |
| Stressful family transitionsa | New | 274 | 23.04 | 0.59 |
| Divorce | ACE | 258 | 21.70 | 0.95 |
| School stressors | New | 250 | 21.03 | 0.13 |
| Neglect (physical or emotional) | ACE, CTS-PC, RF | 242 | 20.35 | 0.41 |
| Severe assault: hit with fist, kicked | ACE, CTS-PC | 231 | 19.43 | 0.46 |
| Sexual maltreatment: molestation | ACE, CTS-PC | 224 | 18.84 | 0.22 |
| Chaotic, disorganized household | RF | 200 | 16.82 | 0.48 |
| Primary caregiver unemployed or fired | New | 192 | 16.15 | 0.59 |
| Separation from primary caregivera | New | 150 | 12.62 | 0.46 |
| Household mental illness (not parent) | ACE | 149 | 12.53 | 0.49 |
| Experienced violence outside homea | New | 143 | 12.03 | 0.23 |
| Death of close family membera | New | 117 | 9.84 | 0.41 |
| Household substance abuse (not parent) | ACE, RF | 112 | 9.42 | 0.53 |
| Very severe assault: beat up, choked | ACE, CTS-PC | 101 | 8.49 | 0.41 |
| Death of parent or primary caregivera | New | 100 | 8.41 | 0.92 |
| Household legal trouble (not parent) | ACE | 74 | 6.22 | 0.57 |
| Unsafe or violent neighborhood | New | 72 | 6.06 | 0.41 |
| Severe sexual maltreatment: rape | ACE, CTS-PC | 62 | 5.21 | 0.22 |
| Parent legal trouble or prison | ACE | 26 | 2.19 | 0.70 |
Note. ACE = Adverse Childhood Experiences Questionnaire; CTS-PC = Conflict Tactics Scale Parent Child Version; RF = Risky Family Environment Measure. ICC = intraclass correlation coefficient. New = new item.
= indicates formative item (all others are reflective).
N = 1,194
Reflective Factor Structure
Chaotic Families.
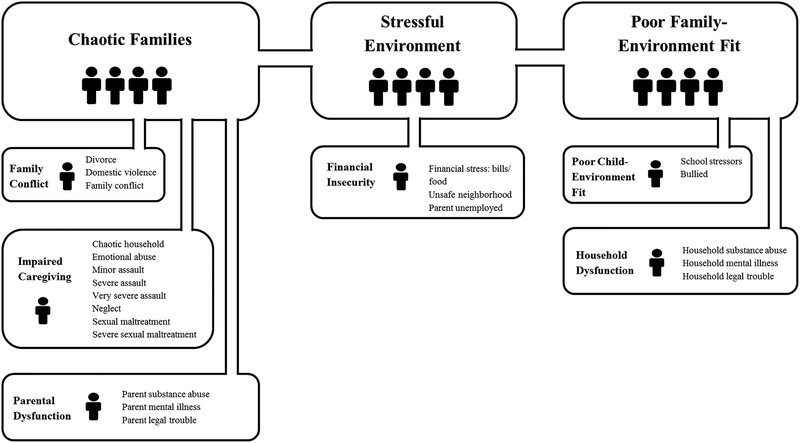
Consistent with existing research (Green et al., 2010), chaotic family conditions were theorized as underlying a collection of marital and family conflict events, problematic household management styles, child maltreatment, and parental dysfunction as reported by the siblings in that family (see Figure 1). Conflictual, chaotic, and abusive characteristics of families have been found to co-occur, and to be linked with psychological and physical health disorders across siblings (Downey & Coyne, 1990; Repetti et al., 2002; Zeitlin, 1994). The item reflective of chaotic families at the between-family level were theorized to have greater specificity at the within-family level, which captures differences amongst the sibling’s exposure to, response to, and perceptions of (1) Family Conflict, (2) Impaired Caregiving, and (3) Parental Dysfunction, as described below:
Figure 1.
Illustration of between-family and within-family factors of childhood adversity. Financial stress: bills/food was removed from the within-family level in the final model, but was retained on the between-family level.
Family Conflict.
Research has shown that children who observe or are directly involved in family conflict such as divorce, domestic violence, and overall family conflict are more likely to have social, emotional, and behavioral challenges than those exposed to less family conflict (Davies et al., 2016; Kashani, Daniel, Dandoy, & Holcomb, 1992). However, individual children within the same families can be more or less impacted by family conflict depending on individual characteristics, such as their emotion regulation abilities (Schulz, Waldinger, Hauser, & Allen, 2005).
Impaired Caregiving.
Child maltreatment such as abuse and neglect is one of the most consistent predictors of negative later life outcomes (Vincent J. Felitti et al., 1998; Finkelhor, Shattuck, Turner, & Hamby, 2013b; Green et al., 2010). Maltreatment can be directed toward all children in a family, or toward some children in a family but not others (Gilbert et al., 2009). In addition, a chaotic household which lacks predictability or routine created by caregivers often leads to a chronic sense of insecurity and anxiety in children, with resulting behavior problems (Bronfenbrenner & Ceci, 1994; Morris, Silk, Steinberg, Myers, & Robinson, 2007).
Parental Dysfunction.
Parental substance abuse, parental mental illness, and parental legal problems have been found to be associated with children’s later life mental health outcomes (Downey & Coyne, 1990; Green et al., 2010; Lee, Fang, & Luo, 2013; Zeitlin, 1994). Parental problems were theorized to uniquely impact children due to the primacy of parents to the well-being of their offspring (Barlow, 2014; Luby et al., 2012).1
Stressful Environment, Financial Insecurity.
Socioeconomic stressors are the most commonly cited domains missing from traditional childhood adversity measures (e.g. Finkelhor et al., 2013, 2015; Wade et al., 2014). Financial insecurity has been theorized to arise from both environmental characteristics affecting the overall family as well as individual children’s experiences with financial stress (Finkelhor et al., 2013; Taylor et al., 2004). As shown in Figure 1, the between-level Stressful Environment factor and within-level Financial Insecurity factor were theorized to reflect the same three items: (1) financial stress bills/food, (2) unsafe neighborhood, and (3) parent unemployed or fired.
Poor Family-Environment Fit.
Difficulty adapting to normative community standards for behavior has been shown to be a risk factor for deleterious outcomes (Braucht, 1979; Kupersmidt, Griesler, DeRosier, Patterson, & Davis, 1995). Poor Family-Environment Fit is based on the idea that human development depends on constant interactions between families and the contexts within which they are embedded (Bronfenbrenner, 1994). The family-level variables of school stressors, being bullied, and household members’ substance use, mental illness, and legal problems are conceptualized as arising from Poor Family-Environment Fit (Figure 1). At the same time, siblings from the same family may vary widely in their experiences and reactions to fit with the environments in which their families are embedded. At the within-family level items were hypothesized to reflect the influence of two separate constructs, (1) Poor Child-Environment Fit, and (2) Household Dysfunction, as described below.
Poor Child-Environment Fit.
(Lerner, Lerner, & Zabski, 1985) argue that a child’s success in school and with peers is due to the goodness of fit between the child’s individual characteristics, such as temperament, and the demands of school and their peers. They also found that adaptation in the context of school was related to adaptation in the context of peers (Lerner et al., 1985). Research has also found sibling-specific factors that influence bullying experiences, such as gender (Paquette & Underwood, 1999).
Household Dysfunction.
Children’s experiences with non-parental household members’ substance abuse, mental illness, and legal problems made up the within-family Household Dysfunction factor. Research has shown that children’s exposure to siblings’, grandparent’s, and aunts’ and uncles’ substance abuse, mental illness, and legal problems has harmful sequelae, depending on the amount of exposure and the individual child’s relationship with that person (Brent et al., 1994; Gjelsvik, Dumont, & Nunn, 2013).
Formative Childhood Adversity Items
Formative items may or may not be correlated with each other or with the factors, but do contribute to the construct being measured (Bollen, 1984). As indicated in Table 1, the six formative “Independent Unfortunate Events” in childhood included in this measure were family physical illness, parental death, another close family death, exposure to violence outside the home, stressful family transitions, and caregiver separation. In addition to the random events of death, illness, and societal violence, stressful family transitions and caregiver separation were theorized to be formative given the diverse causes of family transitions and separations. For example, stressful transitions such as multiple house moves could be due to parents’ employment, family structural changes, or socioeconomic stressors. Similarly, caregiver separation can occur for a variety of reasons, such as military deployment or parental incarceration. All six of these events were conceptualized as experiences during childhood that would contribute to childhood adversity.
Present Study
The overall hypotheses in this study were: (1) substantial proportions of respondents would endorse the items added to the traditional measures of childhood adversity, (2) siblings’ reports of adversity would be interrelated due to belonging to the same families; (3) the theorized multilevel, multi-domain factor structure would fit the real-world data better than one overall factor on both levels, suggesting nuanced family- and sibling-level sources of childhood adversities; and (4) differentiated factors and formative items would add criterion validity of the childhood adversity test score interpretations at the family- and sibling-levels, beyond those of the traditional overall measures, ACEs (including the CTS-PC), and Risky Family Environment measures.
Method
Second Generation (G2) Study
This childhood adversity measure was developed as part of a Second Generation Study of Development, an ongoing study of the middle-aged sons and daughters of participants in an 80-year longitudinal study. The original first generation (G1) cohort consisted of 268 college sophomores and 456 inner city adolescents, all of whom entered the study between 1938 and 1942. A primary goal of the Second Generation (G2) study is to investigate associations between childhood adversity and midlife health. The G2 study began by conducting telephone interviews to assess multiple domains, including the midlife children’s current health, social functioning, and psychological wellbeing. Those who completed the interview were mailed a follow-up battery of questionnaires, which contained the childhood adversity measure. Later, participants who could not be reached by telephone were mailed a combined questionnaire which contained both the telephone interview questions and the questionnaires, including the childhood adversity measure. These combined questionnaires targeted participants with fathers from the inner-city cohort, with more socioeconomic disadvantage and less consistent phone numbers. The study was completed in compliance with the first and last authors’ Institutional Review Board.
Sample
Out of the eligible 1,941 adult (G2) children from 591 families (G1) in the Study of Development (238 College, 353 Inner City), 1,054 G2 siblings participated in the telephone interview, and 946 returned the follow-up questionnaire. Two hundred forty-eight additional participants completed the combined questionnaire, making the total sample size 1,302 individuals (67%) in 517 families (87%). Since the childhood adversity measure was included in the questionnaires, 1,194 individuals in 500 families (222 College, 278 Inner City) completed the childhood adversity questionnaire.
The number of siblings per family ranged from 1 to 8, with an average of 2.52. The sample was 49.0% male and 50.7% female, with a mean age of 59-years old (SD = 6.64). Reflecting the demographics of their G1 parents in this northeast city of the United States in the 1940s (97% white), the G2 sample was 97.5% white, with a median household income of $100,000. Participants reported substantial socioeconomic diversity in their families-of-origin as 56% were from the inner-city sample: 4% of the overall sample reported growing up poor, 30% working class, 29% middle class, 30% upper middle class, and 7% upper class.
Childhood adversity measure
As shown in Table 1, the 28 items in our retrospective measure of childhood adversity encompassed the Adverse Childhood Experiences scale (ACE; Felitti et al., 1998), including the physical, emotional, sexual abuse and neglect items from the Conflict Tactics-Parent Child Scale (CTS-PC; Straus et al., 1998), and the Risky Family Environment measure (Repetti et al., 2002; Taylor et al., 2004). Eleven additional items culled from recent studies of childhood adversity were also included. The financial stress question combined two questions of family economic pressure (Conger et al., 1994), (1) difficulty paying bills, and (2) difficulty affording food. Following existing childhood adversity measures, respondents indicated yes or no to each adverse event that occurred before they were 19-years-old. If a participant failed to respond to an item, it was treated as no exposure to that event. As part of the content validation, the items were pilot tested with ten volunteers, and revised for clarity before being administered to participants.
Validity measures
The validity measures for the majority of respondents were collected during the interview to reduce shared-method variance with the paper-and-pencil childhood adversity questionnaire (Cunningham, Preacher, & Banaji, 2001). Similar to previous research (Taylor et al., 2004), convergent construct validity was assessed with the question “Overall, how stressful was your life during childhood? Would you say not at all, a little, somewhat, very, or extremely stressful?” Responses were converted to 0–4, with higher scores indicating greater stress (M = 1.41, SD =1.11). A question about whether participants had children of their own (0 = no, 1 = yes) was used to test discriminant construct validity, as it was not expected that childhood adversity would be correlated in either direction with having one’s own children.
To establish criterion validity of the test score interpretations, multilevel correlations were examined between childhood adversity and three major domains of adult functioning: psychological, social, and physical health. To assess psychological health, participants were asked, “During the last 12 months, have you had any emotional, nervous, or psychiatric problems?” (0 = no, 1 = yes). Positive correlations indicated that greater childhood adversity was associated with psychological problems in the past year. For social functioning, participants answered four family support questions, including, “How much do members of your family really care about you?,” with responses ranging from 1 = not at all to 4 = a lot (M = 3.52, SD = .66) (Walen & Lachman, 2000). Multilevel reliability for the social support items was high in the current sample, within-family ω = 0.89 and between-family ω = 0.95 (reliability procedure detailed by Geldhof et al., 2014). To assess physical health, respondents were asked whether their current health was excellent, very good, good, fair, or poor, converted to 0 = poor to 4 = excellent (M = 2.81, SD =1.03). This was the same self-report measure of health used in the original ACEs study (Felitti et al., 1998).
Data analysis strategy
Data analyses proceeded in three main steps. First, descriptive analyses were conducted to examine how often the childhood adversity items were endorsed, focusing on the additional items not included in the traditional measures. We also compared the prevalence rates of childhood adversity in our sample to existing samples in the literature. A critical piece of the descriptive analyses was to examine the intraclass correlation coefficients (ICCs), both to establish the need for multilevel modeling (Pornprasertmanit, Lee, & Preacher, 2014) and to examine the degree of overlap in siblings’ reports of adversity. Past research on parental maltreatment of siblings has found intraclass correlations in the moderate-to-high range (>.50) for identical twins, low-to-moderate for fraternal twins and full siblings (<.50), and low or nonsignificant for adoptive siblings (Hines et al., 2006). Intraclass correlations greater than .05 generally indicate that the interrelatedness of clustered data needs to be accounted for to avoid statistical bias (Julian, 2001). To calculate ICCs, we utilized a saturated covariance model fit to all 28 binary items, using an unweighted least squares (ULSMV) estimator in Mplus v. 8 (L. K. Muthén & Muthén, 1998).2
Second, the proposed multilevel factorial structure of the reflective childhood adversity items was tested. An overall multilevel confirmatory factor analysis (MCFA) with one-factor at both levels was first conducted as a baseline against which to compare our hypothesized multi-factorial structure. Next, we split the sample of families into two random halves to allow for a preliminary multi-domain MCFA on the first half, followed by modest modifications and re-testing of the final model on the second half (Bentler, 1980). This model fitting process allowed for a replication test and also took into consideration the dangers of overfitting models based on modifications that capitalize on chance if too many models are tested. Third, we examined the construct and criterion validity of the adversity factors using multilevel structural equation modeling (MSEM) correlations. Following the widely-used tradition of Campbell and Fiske (1959) and Westen and Rosenthal (2003), a matrix of MSEM correlations was used to assess whether the adverse events in childhood were associated positively, negatively, or practically not at all with other variables in expected ways based on prior theory and research.
Multilevel confirmatory factor analyses
MCFAs were used rather than exploratory factor analyses (EFAs), as MCFAs are typically used for constructs with a substantial body of existing evidence on which to form hypotheses about which observed items will load on which latent factors (Bryne, 2012). Furthermore, EFAs, which are less-theory informed and standardized, can be vulnerable to producing idiosyncratic (non-replicable) results due to sampling issues (e.g., unusual variances or associations) or subjective decisions (e.g. number of factors, rotation criteria, and interpretation of loading patterns) that may be particular to that study or EFA.
MCFAs disaggregate variance into within- and between-levels (Dedrick & Greenbaum, 2011). To assess the strength of associations in the factor structures, standardized factor loadings, credibility intervals, and inter-factor correlations were estimated at each level (Pornprasertmanit et al., 2014). Items with standardized factor loadings less than .45 were considered weak, and below .32 were removed except in the one case noted (Comrey & Lee, 1992). Factors that correlated above .80 were combined given their substantial overlap. Although some of the items in this study proved to have high ICCs (that is, most of the variance was due to belonging to the same families), they were retained on the within-family level MCFA as the sibling level variance was enough to warrant investigation. The formative Independent Unfortunate Events were not included in the MCFAs given that they were not expected to conform to any factor structure (Bollen, 1984).
Bayesian estimation in Mplus v. 8 was used to implement the models (Muthén & Muthén, 2010). Initially, we tried Weighted Least Squares (WLS) estimation, which permits comparison of models using traditional fit indices such as χ2, CFI, and RMSEA. However, binary data present significant computational challenges due to restrictions in variability, resulting in difficulty with convergence of WLS estimated models. Muthén and Asparahov (2012) identify Bayesian estimation as an alternative and analogous approach to WLS (maximum likelihood) estimation for categorical outcomes. Bayesian estimation led to convergence of our models, with fairly consistent findings and few problems, suggesting that the failure to converge using WLS was due to computational challenges rather than a problem with the specification of the models themselves. Using Bayesian estimation, the Posterior predictive p-value (PPP) was used to test model fit of the MCFAs (Muthén & Asparouhov, 2009).3 A 95% CI was produced for the difference between observed and replicated chi-square values generated by posterior predictive checking; a smaller (more negative) CI and p (PPP) > .05 provided evidence of model fit (Muthén & Asparouhov, 2009; Muthén & Muthén, 2010). Twenty thousand iterations were used, and Mplus discarded the first half of the iterations in each chain (of which there were two) as “burn-in.”
Multilevel validity analyses using structural equation modeling
Multilevel validity correlations using structural equation modeling were estimated for the final six within-family and three between-family childhood adversity factors in the MCFA, the overall items, equivalent ACEs and Risky Family Environment scales, and the six formative Independent Unfortunate Events. The Bayes estimator automatically provided robust asymmetric credible intervals, even for standardized results and for nonnormally distributed parameters. The within-family model parameters captured micro-level differences in siblings’ childhood adversity controlling for variation across their families, whereas the between-family level represented the macro-level family’s collective experience of adversity (aggregating across siblings) compared to other family units (Byrne, 2012). Multilevel structural equation modeling (MSEM) treats the domains of childhood adversity as level-specific latent variables disattenuated from measurement error, and thus relationships among these variables were not biased (Rush & Hofer, 2014). Under classic methods of establishing validity, if the factor interpretations are consistent with what we expect on the basis of theory and the loading pattern at each level, then the factors should (a) correlate with some variables, reflecting convergent validity; and (b) fail to correlate with other variables, reflecting discriminant validity.
Results
Descriptive Analyses
As shown in Table 1, many of the participants reported having experienced childhood adversities not present in traditional instruments. The most frequently endorsed new item was having been teased or bullied, followed by financial stress: bills/food. Eight out of the eleven additional items were endorsed by at least 10% of the sample. In addition, the number of adverse events reported in this sample was comparable to past studies of adversity. Participants endorsed a mean of 6.45 events (s.d. = 4.28); a recent study with an expanded set of 17 ACEs reported a mean of 5.3 events (s.d. = 3.7) (Mersky et al., 2017). Using only the 10 equivalent ACEs items, our sample had a mean of 2.6 and a s.d. of 2.0; the above study found an average endorsement of 3.3 events and a s.d. of 2.5 (Mersky et al., 2017). For the Risky Family Environment items, our sample had a mean score of 1.47 (s.d. = .56), compared to a study of 3,248 respondents who had a mean of 1.66 (s.d. = .58) (Taylor, Lehman, Kiefe, & Seeman, 2006).
The items’ intraclass correlations (ICCs) ranged from .13-.95, with almost half of the ICCs being >.50, and three-quarters being >.40. These ICCs indicated overlap between siblings requiring multilevel analytic approaches even at the lower end (Julian, 2001). However, the degree of nonindependence depended on the nature of the adversity. Items with the highest ICCs included divorce, death of a parent, and parental substance abuse and legal problems. The lowest ICCs were found for school stressors, teased or bullied by peers, and both types of sexual maltreatment.
Multilevel Confirmatory Factor Analyses
Overall Adversity Model.
We began by fitting an overall, one-factor within-family and between-family (1W1B) MCFA model to all 22 reflective items, similar to the traditional approach. Several items had low factor loadings. On the within-family level, these items were divorce, household mental illness, school stressors, teased or bullied and financial stress: bills/food (see Appendix A). Financial stress: bills/food and teased or bullied loaded poorly on the between-family level, as did minor assault, severe sexual maltreatment, and household legal problems. Model fit was acceptable, p = .09, 95% CI [−31.94, 163.49].4
Preliminary Multi-Factor Model.
In the initially hypothesized six-factor within-family and four-factor between-family model (6W4B), most item loadings supported this factor structure (Appendix B). Model fit was good, p = .26, 95% CI [−61.81, 128.85]. The only problematic item on the within-family level was financial stress: bills/food, so it was aggregated to the between-family Stressful Environment factor. On the between-family level, minor assault, severe sexual maltreatment, and teased or bullied had low standardized loadings. Minor assault and teased or bullied were removed by centering them at the family mean, while severe sexual maltreatment was retained on the between-family level given its borderline loading. The Chaotic Families and Parental Dysfunction factors were highly correlated at the between-family level and so were combined (Appendix C), resulting in the final 6W3B factor structure tested on the second random half of the sample.
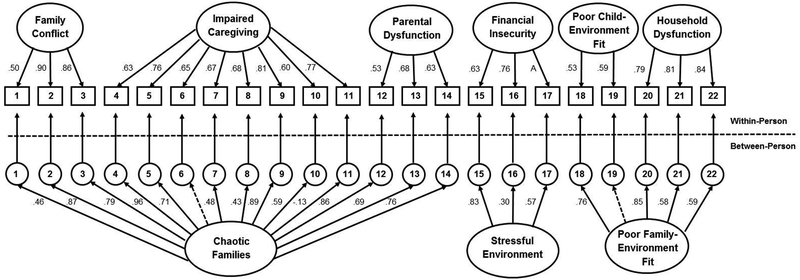
Final Multi-Factor model.
Analysis of the final 6W3B model (Figure 2) indicated strong support for this factor structure at both levels (for credibility intervals, see Appendix D). Model fit was strong, p = .30, 95% CI [−65.62, 119.99]. All of the items loaded well on the within-family level. Severe sexual maltreatment was now the only item on the between-family level that was low enough to be removed before the validity analyses. Although unsafe neighborhood and very severe assault had loadings on the lower end, they were retained given that they represented central theoretical aspects of their respective constructs. The final inter-factor correlations (Tables 2 and 3) demonstrated that factors on both levels exhibited some overlap but with enough differentiation to be maintained as separate domains.
Figure 2.
Standardized factor loadings for final Multilevel Confirmatory Factor Analysis (MCFA) model. Broken lines indicate parameters removed. See Table 4 for inter-factor correlations. A = aggregated to level 2; 1 = divorce: 2 = domestic violence; 3 = family conflict; 4 = chaotic household; 5 = emotional abuse; 6 = minor assault; 7 = severe assault; 8 = very severe assault; 9 = neglect; 10 = sexual maltreatment; 11 = severe sexual maltreatment; 12 = parent substance abuse; 13 = parent mental illness; 14 = parent legal trouble; 15 = caregiver unemployment; 16 = unsafe neighborhood; 17 = financial stress; 18 = school stressors; 19 = teased or bullied; 20 = household substance abuse; 21 = household mental illness; 22 = household legal problems.
Table 2.
Final Multilevel Confirmatory Factor Analysis Within-Family Factor Inter-correlations
| Factor | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. Family conflict | |||||
| 2. Impaired caregiving | 0.74 | ||||
| 3. Parental dysfunction | 0.61 | 0.77 | |||
| 4. Financial insecurity | 0.29 | 0.43 | 0.54 | ||
| 5. Poor child-environment fit | 0.55 | 0.65 | 0.52 | 0.62 | |
| 6. Household dysfunction | 0.44 | 0.47 | 0.66 | 0.27 | 0.16 |
Table 3.
Final Multilevel Confirmatory Factor Analysis Between-Family Factor Inter-correlations
| Factor | 1 | 2 |
|---|---|---|
| 1. Chaotic families | ||
| 2. Stressful environment | 0.54 | |
| 3. Poor family-environment fit | 0.54 | 0.49 |
Validity Analyses Using Multilevel SEM
As shown in Table 4, all six within-family and three between-family reflective factors demonstrated construct validity, both convergent and discriminant. The overall scale and equivalent Adverse Childhood Experiences (including the CTS-PC items), and the Risky Family Environment questions also demonstrated evidence for convergent and discriminant construct validity at both levels, as well as criterion validity. A surprising pattern of criterion validity emerged from the six within-family childhood adversity factors. Differences in siblings reports of Impaired Caregiving and Poor Child-Environment Fit were consistently linked with differences in adult psychological problems, family social support, and physical health in the expected directions. However, sibling’s reports of Family Conflict were not associated with any of the adult validity outcomes. In addition, Financial Insecurity was significantly correlated with sibling’s reports of family social support and physical health in adulthood, but not with psychological problems. Conversely, Parental Dysfunction and Household Dysfunction were both correlated in the expected directions with adult psychological problems, but not with family social support nor current physical health.
Table 4.
Validity Correlations from Multilevel Structural Equation Models with Construct and Criterion Indicators – Reflective Factors
| Construct Validity | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Convergent | Discriminant | Criterion Validity | ||||||||
| Factor (level) | Child Stress (W) | Child Stress (B) | Have Child (W) | Have Child (B) | Psych Prob (W) | Psych Prob (B) | Family Support (W) | Family Support (B) | Health (W) | Health (B) |
| Family conflict (W) | 0.35* | - | 0.06 | - | 0.03 | - | 0.00 | - | 0.00 | - |
| Impaired caregiving (W) | 0.46* | - | 0.01 | - | 0.30* | - | −0.20* | - | −0.16* | - |
| Parental dysfunction (W) | 0.55* | - | 0.06 | - | 0.46* | - | −0.04 | - | −0.13 | - |
| Financial insecurity (W) | 0.24* | - | −0.02 | - | 0.10 | - | −0.20* | - | −0.18* | - |
| Child-environment fit (W) | 0.41* | - | −0.01 | - | 0.25* | - | −0.20* | - | −0.19* | - |
| Household dysfunction (W) | 0.18* | - | 0.08 | - | 0.24* | - | 0.02 | - | −0.05 | - |
| Chaotic Families (B) | - | 0.88* | - | 0.06 | - | 0.59* | - | −0.38* | - | −0.26* |
| Stressful environment (B) | - | 0.43* | - | −0.36 | - | 0.44* | - | −0.44* | - | −0.83* |
| Family-environment fit (B) | - | 0.67* | - | −0.07 | - | 0.53* | - | −0.53* | - | −0.45* |
| Childhood adversity (W) | 0.50* | - | 0.02 | - | 0.18* | - | −0.17* | - | −0.12* | - |
| Childhood adversity (B) | - | 0.89* | - | 0.06 | - | 0.65* | - | −0.38* | - | −0.19* |
| ACEs (W) | 0.51* | - | 0.00 | - | 0.42* | - | −0.18* | - | −0.13* | - |
| ACEs (B) | - | 0.94* | - | 0.28 | - | 0.59* | - | −0.28* | - | −0.26* |
| Risky Family (W) | 0.55* | - | 0.02 | - | 0.34* | - | −0.27* | - | −0.13* | - |
| Risky Family (B) | - | 0.89* | - | 0.08 | - | 0.58* | - | −0.26* | - | −0.32* |
Note. W = Within-family (sibling) level; B = Between-family level; Childhood adversity = overall 22 reflective items; ACEs= equivalent ACEs items; Risky Families = equivalent Risky Family items. Estimates are standardized.
Significant = credible intervals exclude zero.
All three between-family factors were associated with the adult outcomes with correlations ranging from −.38 (i.e., medium) to −.83 (i.e. large). Notably, between-family Stressful Environment had a significantly stronger link with between-family levels of adult physical health than did either Chaotic Families (covariance difference = −0.37, one-tailed p = .00, 95% Crl [−.57, −.15]) or Poor Family-Environment Fit (covariance difference = −0.41, one-tailed p = .00, 95% Crl [−.61, −.30]).5
The six formative Independent Unfortunate Events generally demonstrated construct validity, but with more mixed criterion validity correlations than the reflective scales (see Table 5). The items with the strongest validity were between-family physical illness and within-level caregiver separation. Between-family death of a close family member and within-family violence outside the home had links only with midlife physical health, whereas within-family stressful transitions was associated with midlife psychological problems and family social support. Between-family caregiver separation was significantly correlated with adult social support. Parental death, within-family physical illness and death of a close family member, and between-family violence outside the home and stressful transitions lacked criterion validity.
Table 5.
Validity Correlations from Multilevel Structural Equation Models with Construct and Criterion Indicators – Formative Items
| Construct Validity | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Convergent | Discriminant | Criterion Validity | ||||||||
| Adversity Item (level) | Child Stress (W) | Child Stress (B) | Have Child (W) | Have Child (B) | Psych Prob (W) | Psych Prob (B) | Family Support (W) | Family Support (B) | Health (W) | Health (B) |
| Family physical illness (W) | 0.28* | - | 0.04 | - | 0.01 | - | −0.07 | - | 0.09 | - |
| Family physical illness (B) | - | 0.37* | - | −0.34 | - | 0.31* | - | −0.27* | - | −0.32* |
| Parental death (W) | 0.52 | - | 0.01 | - | 0.16 | - | −0.19 | - | 0.10 | - |
| Parental death (B) | - | 0.31* | - | 0.35 | - | 0.24 | - | −0.03 | - | −0.12 |
| Death of close family (W) | 0.03 | - | 0.37 | - | 0.07 | - | 0.01 | - | 0.12 | - |
| Death of close family (B) | - | 0.33* | - | −0.36 | - | 0.23 | - | −0.23 | - | −0.47* |
| Caregiver separation (W) | 0.29* | - | 0.09 | - | 0.45* | - | −0.29* | - | −0.31* | - |
| Caregiver separation (B) | - | 0.79* | - | 0.02 | - | 0.22 | - | −0.36* | - | −0.27 |
| Violence outside home (W) | 0.24* | - | 0.08 | - | 0.12 | - | −0.17 | - | −0.26* | - |
| Violence outside home (B) | - | 0.23 | - | 0.16 | - | 0.40 | - | −0.14 | - | −0.31 |
| Stressful transitions (W) | 0.36* | - | 0.36 | - | 0.31* | - | −0.30* | - | 0.00 | - |
| Stressful transitions (B) | - | 0.55* | - | −0.02 | - | 0.05 | - | −0.21 | - | −0.20 |
Note. W = Within-family level; B = Between-family level. Estimates are standardized.
Significant = credible intervals exclude zero.
A final set of regression analyses was implemented (see Table 6) to address two questions: (1) at each level, how much total variance do the adversity factors combine to explain in key adult outcomes; and (2) is there evidence for unique contributions of the factors individually in predicting these adult outcomes. When examined together, the childhood adversity factors predicted between 22 and 83% of the variance in adult psychological, social support, and physical health. However, the partial regression coefficients which capture the predictive link of each adversity factor net of all of the others (or holding the others constant), found that none of the childhood adversity factors were significantly predictive of the adult outcomes at the within-family level. At the between-family level, Chaotic Families and Poor family-environment fit were significantly predictive of retrospectively recalled childhood stress from the telephone interview, as was Poor family-environment fit with adult family social support, and Stressful environment and Chaotic families with adult physical health, although the latter in the unexpected direction.
Table 6.
Unique Association Regressions from Multilevel Structural Equation Models with Construct and Criterion Indicators – Reflective Factors
| Construct | Criterion Validity | |||||||
|---|---|---|---|---|---|---|---|---|
| Factor (level) | Child Stress (W) | Child Stress (B) | Psych Prob (W) | Psych Prob (B) | Family Support (W) | Family Support (B) | Health (W) | Health (B) |
| Family conflict (W) | −0.56 | - | −0.68 | - | 0.04 | - | 0.73 | - |
| Impaired caregiving (W) | 0.41 | - | 1.77 | - | −1.03 | - | −0.33 | - |
| Parental dysfunction (W) | 0.75 | - | −0.61 | - | 1.22 | - | 0.02 | - |
| Financial insecurity (W) | −1.60 | - | 0.85 | - | −0.12 | - | 0.01 | - |
| Poor child-environment fit (W) | 1.79 | - | 0.25 | - | −0.33 | - | −0.54 | - |
| Household dysfunction (W) | 0.21 | - | −1.01 | - | −0.55 | - | −0.36 | - |
| Chaotic Families (B) | - | 0.75* | - | 0.36 | - | −0.02 | - | 0.38* |
| Stressful environment (B) | - | −0.15 | - | 0.09 | - | −0.21 | - | −0.98* |
| Poor family-environment fit (B) | - | 0.37* | - | 0.22 | - | −0.44* | - | −0.15 |
| R2 | .72 | .88 | .52 | .43 | .33 | .36 | .22 | .83 |
Note. W = Within-family level; B = Between-family level. Estimates are standardized.
Significant = credible intervals exclude zero.
Discussion
Given the growing interest in comprehensive childhood adversity measures, combined with the fact that childhood adversities often occur in the context of families, the goal of this study was to examine the multilevel psychometric properties of an expanded childhood adversity measure administered to siblings within the same families. Our multilevel, multi-domain measure of childhood adversity included additional items widely endorsed by participants but absent from traditional measures. Results demonstrated validity of the test score interpretations and revealed nuance in sources of variance and outcomes, suggesting that this approach could yield a deeper understanding of the causes and consequences of childhood adversity.
What can be learned from multilevel childhood adversity measures administered to siblings in the same families?
Family and individual contributions have not typically been examined concurrently. Most existing studies of childhood adversity only include one family member, preventing the disaggregation of family-level and individual-level variability in adverse events in childhood (Geldhof et al., 2014). This confounding of variance limits the ability to pinpoint the specific source of different childhood adversities that lead to deleterious outcomes. This study is the first to our knowledge to demonstrate that some adversities in childhood occur more commonly among siblings from the same families and may stem from family-wide influences (e.g., divorce, parental death, financial stress: bills/food, parent substance use, parent legal problems, domestic violence), while others are experienced differently by siblings and result more from individual processes (school stressors, teased or bullied, both types of sexual maltreatment, experienced violence outside the home, minor assault [corporal punishment], and emotional abuse). The adversity items in this study with higher ICCs support the understanding of these events as family-wide occurrences, with important research and clinical implications. Clinically, treatment providers would be wise to assess all of the siblings in a family when one child has been found to have experienced these adverse events. For research, it highlights the importance of using multilevel analyses for these childhood adversities, to capture variance at each level of analysis, especially for multilevel hypotheses (Geldhof et al., 2014). On the other hand, the seven items with ICCs below .40 indicate that the majority of the variance in these items stem from differences among siblings. Differences in sibling reports could stem from a wide range of causes, including varying exposure, perceptions, peers and individual characteristics such as emotion regulation, personality, and gender. Addressing adversities that are often experienced in largely unique ways by siblings may call for an individualized approach to treatment and research. The promise of multilevel investigations could be extended further to studies of siblings nested within families nested within larger communities, to examine the role of societal-level influences on childhood adversity (Molnar, Buka, Brennan, Holton, & Earls, 2003).
Differentiating levels and factors, which illuminated variations in the sources of childhood adversity found in the MCFA, in combination with the specific criterion validity correlations, could have important implications for intervention and prevention. For example, within-family school stressors and being bullied (Poor Child-Environment Fit) had more criterion validity links with adult psychological, social, and physical health than did divorce, domestic violence, and overall family conflict (Family Conflict). Combining this with the finding that being bullied primarily reflected within-level individual experiences could direct health professionals toward targeting individual children’s adaptation to their environment in order to prevent peer victimization and ultimately midlife dysfunction and disease.
How do the additional childhood adversity items benefit future research?
Four of the ten most frequently endorsed categories in this study were newly-added items that would have been missed by traditional measures of childhood adversity (teased or bullied, financial stress: bills/food, family physical illness, and stressful family transitions). The two most widely endorsed additional items, being bullied and financial stress, also contributed to new factors of childhood adversity, which increased construct validity in the multilevel factor analysis. The final model of six factors at the within-family level, including the new domain of poor-child environment fit (with being teased or bullied), and three factors at the between-family level, including stressful environment (with financial stress: bills/food), resulted in a stronger model fit than one overall factor, suggesting that expanded and differentiated subscales of adversity more closely described the real-world experience of this sample. The most frequently endorsed formative items, illness and transitions, also demonstrated validity of childhood adversity test score interpretations. The family’s recollection of physical illness exhibited strong construct and criterion validity links with midlife biospsychosocial health. Sibling’s recollection of stressful transitions also demonstrated construct and criterion validity with midlife psychosocial functioning.
An important overall function of childhood adversity measures is to facilitate studies of later life outcomes. Our new reflective items of childhood adversity demonstrated criterion validity correlations with midlife adult functioning variables and added to our understanding of these pathways. For example, the finding that between-family Stressful Environment was more highly correlated with physical health than were Chaotic Families or Poor Family-Environment Fit suggested that family-wide socioeconomic stress in childhood was particularly tied to siblings’ later physical health. Additionally, the new caregiver separation formative item was significantly correlated on the within-family level with siblings’ midlife psychological, social, and physical health.
The expanded differentiated domains also suggest the potential for identifying specific links between childhood adversity and particular areas of adult functioning. For example, differences in siblings’ memories of their family’s substance use, mental illness, and legal problems (within-family Household Dysfunction) were correlated with differences in their current psychological problems, but not with their current family social support or physical health. These nuances are obscured when all of the items were combined into one scale. For the formative items, within-family violence outside the home had links with adult physical health, whereas stressful transitions were associated with psychological problems and social support. Continuing to explore multidomain, multilevel models could increase our understanding of which specific types of childhood adversity are tied to which specific adult outcomes (e.g. Green et al., 2010; Iniguez & Stankowski, 2016; McLaughlin & Sheridan, 2016), informing future targeted efforts at prevention and treatment.
What were the limitations of this study and where do we go from here?
Participants in this study reported whether or not they were exposed to a particular adverse event following the approach used in several widely-used measures of childhood adversity. However, dichotomous items create data computational challenges for testing scale construction, such as preventing maximum likelihood estimation in the MCFA and the assessment of multilevel internal consistency reliability of the reflective items. However, combining the reflective items into continuous latent factors facilitated the MSEM validity analyses, as the factors became “more continuous” with larger numbers of items. This may also help explain why the between-family factor score interpretations had overall stronger validity correlations than the within-family factors which had fewer items in more categories, followed by the weakest validity correlations for the single formative items.
The specific criterion validity correlations found in this study between childhood adversity domains and adult outcomes should be replicated in future studies, and alternative outcomes could be tested. For example, although (contrary to our hypothesis) our analyses did not find additional criterion validity correlations with adult outcomes by separating the dysfunction of parents from that of other household members, perhaps differences would be found with other adult outcomes. This could also be the case for parental death and stressful transitions. On the other hand, if weakly-supported factors and items continue to lack validity, they could be removed or combined in future versions of the measure. In addition, different factor structures could be found in different samples, but given that this sample reported typical levels of childhood adversity, there is reason to believe that this factor structure is valid and could be generalizable to future samples. We hope that this study can serve as an example for future researchers of how to use multilevel methods to conduct psychometric analyses of both reflective and formative items in nested samples, as well as how to handle problematic items.
The regression analyses in this study suggested that childhood adversities as a group have strong predictive power in explaining key indices of adult functioning, and pointed to the need for further study of more differentiated childhood adversity predictors. The lack of significant unique associations at the within-family level was consistent with past findings that the effect of childhood adversities may be nonspecific, with the cumulative predictive power being greater than that of specific items or factors (Green et al., 2010; Mersky et al., 2017). Given that other studies suggest specificity of connections (e.g., McLauglin & Sheridan, 2016), additional research is needed. The findings from this study’s MCFA and validity correlations could provide a useful roadmap for future outcome research investigating such specificity.
Retrospective reports of childhood adversity are subject to bias inherent in any recall process (Colman et al., 2016). There is a chance of bias in the direction of over-reporting; participants with current psychological problems, low social support from family, or recent health decline could have endorsed more adverse events in childhood (Colman et al., 2016), which could have affected our validity analyses. However, comparison studies have shown that participants are more likely to underreport than overreport adverse childhood events (e.g., (Ferraro, Schafer, & Wilkinson, 2016; Hardt & Rutter, 2004).
Finally, findings from this predominantly white, relatively high-SES sample of adults may not generalize to more diverse populations. Participants in this study did grow up in socioeconomic diverse homes, approximately half having fathers raised in poor, inner-city areas. The frequency of adverse childhood events reported in this study was comparable to other samples, which is consistent with past research that adverse childhood events are prevalent across sociodemographic groups (Taylor et al., 2004; Wade, Becker, Bevans, Ford, & Forrest, 2016). It will be important for future investigations to replicate these findings with more diverse groups.
This study presents the first multilevel psychometric analysis of an expanded childhood adversity measure, administered to siblings within families, with distinct factor structures at the within-family and between-family levels. The resulting empirically-supported domains of adversity hold promise as important tools for future fine-grained examinations of causes and consequences of childhood adversity. In practice, future investigators could distinguish the reflective items as within-family latent factors, as between-family, or as both. This approach, as well as using the supported formative items, has the potential to enhance future investigations into specific mechanisms involved in the prevention of micro and macro influences on emotional, physical, and social dysfunction in individuals and families.
Supplementary Material
Public Significance Statement.
Although adverse childhood events most often occur in the context of family life, there is a dearth of studies examining the multilevel structure of childhood adversity among siblings nested within families. Validating a new multi-domain measure of childhood adversity using multilevel psychometric analyses, this study advances traditional assessments in two ways: (1) the measure includes previously-omitted adverse events relevant to later life outcomes, and (2) multilevel modeling of nested data allows for disaggregation of individual- and family-level sources and sequelae of childhood adversity, which holds promise for revealing fine-grained links with adult functioning that can be targeted for prevention and intervention.
Acknowledgments
Support for this project was provided by the National Institute of Mental Health (5T32MH16259) to the first author, and the National Institute of Aging (R01AG045230) to the last author.
Footnotes
Although Parental Dysfunction was originally tested as a separate between-family factor, Parental Dysfunction and Chaotic Families were highly intercorrelated (.85) on the between-family level in the preliminary model (see Appendix C) and therefore were combined in the final model. This combination supports previous findings that parental substance use, mental illness, and legal problems stem from similar overall family characteristics as family conflict, chaos, and abuse (Green et al., 2010).
For continuous variables, ICC = v/(v+e), where v is the level-2 variance and e is the level-1 variance of a variable. However, in logit and probit models there is no separately estimated level-1 residual variance; instead, it is a constant regardless of what predictors are included. The constant is (π2)/3 for logistic models with binary items, and it is 1 for probit models.
The Deviance Information Criterion (DIC) index, which balances fit with model complexity, has not yet been extended to models with categorical indicators.
These confidence intervals are for a likelihood-ratio statistic (Muthén & Asparouhov, 2009), while the p values are a Bayesian numeric measure of model fit.
The p-value reported in Bayes output uses the posterior distribution, which is analogous to the sampling distribution in frequentist statistics. Because we know which side of the posterior distribution the null value is on, a one-tailed p-value is used.
Contributor Information
Melinda I. Morrill, Massachusetts General Hospital, Harvard Medical School
Marc S. Schulz, Bryn Mawr College
Michael D. Nevarez, Massachusetts General Hospital, Harvard Medical School
Kristopher J. Preacher, Vanderbilt University
Robert J. Waldinger, Massachusetts General Hospital, Harvard Medical School
References
- Barlow J (2014). Group-based parent training programmes for improving parental psychosocial health. Cochrane Database of Systematic Reviews, (5). Retrieved from http://ezp-prod1.hul.harvard.edu/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=chh&AN=CD002020&site=ehost-live&scope=site [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM (1980). Multivariate Analysis with Latent Variables: Causal Modeling. Annual Review of Psychology, 31(1), 419–456. 10.1146/annurev.ps.31.020180.002223 [DOI] [Google Scholar]
- Berg L, Rostila M, Saarela J, & Hjern A (2014). Parental Death During Childhood and Subsequent School Performance. Pediatrics, 133(4), 682–689. 10.1542/peds.2013-2771 [DOI] [PubMed] [Google Scholar]
- Bollen KA (1984). Multiple indicators: Internal consistency or no necessary relationship? Quality and Quantity, 18(4), 377–385. 10.1007/BF00227593 [DOI] [Google Scholar]
- Bollen KA, & Diamantopoulos A (2015). In Defense of Causal–Formative Indicators: A Minority Report. Psychological Methods. 10.1037/met0000056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braucht GN (1979). Interactional analysis of suicidal behavior. Journal of Consulting and Clinical Psychology, 47(4), 653–669. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, Liotus L, Schweers J, Balach L, & Roth C (1994). Familial risk factors for adolescent suicide: a case-control study. Acta Psychiatrica Scandinavica, 89(1), 52–58. 10.1111/j.1600-0447.1994.tb01485.x [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U (1994). Ecological Models of Human Development In International Encyclopedia of Education (2nd ed., Vol. 3, pp. 37–43). Oxford: Elsevier. [Google Scholar]
- Bronfenbrenner Urie, & Ceci SJ (1994). Nature-nuture reconceptualized in developmental perspective: A bioecological model. Psychological Review, 101(4), 568–586. 10.1037/0033-295X.101.4.568 [DOI] [PubMed] [Google Scholar]
- Byrne BM (2012). Structural equation modeling with Mplus: Basic concepts, applications, and programming. New York, NY, US: Routledge/Taylor & Francis Group. [Google Scholar]
- Chen E, Miller GE, Kobor MS, & Cole SW (2011). Maternal warmth buffers the effects of low early-life socioeconomic status on pro-inflammatory signaling in adulthood. Molecular Psychiatry, 16(7), 729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colman I, Kingsbury M, Garad Y, Zeng Y, Naicker K, Patten S, … Thompson AH (2016). Consistency in adult reporting of adverse childhood experiences. Psychological Medicine, 46(03), 543–549. 10.1017/S0033291715002032 [DOI] [PubMed] [Google Scholar]
- Comrey AL, & Lee HB (1992). A first course in factor analysis, 2nd ed Hillsdale, NJ, US: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Conger RD, Ge X, Elder GH, Lorenz FO, & Simons RL (1994). Economic Stress, Coercive Family Process, and Developmental Problems of Adolescents. Child Development, 65(2), 541–561. 10.2307/1131401 [DOI] [PubMed] [Google Scholar]
- Copeland WE, Wolke D, Lereya ST, Shanahan L, Worthman C, & Costello EJ (2014). Childhood bullying involvement predicts low-grade systemic inflammation into adulthood. Proceedings of the National Academy of Sciences, 111(21), 7570–7575. 10.1073/pnas.1323641111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronholm PF, Forke CM, Wade R, Bair-Merritt MH, Davis M, Harkins-Schwarz M, … Fein JA (2015). Adverse Childhood Experiences. American Journal of Preventive Medicine, 49(3), 354–361. 10.1016/j.amepre.2015.02.001 [DOI] [PubMed] [Google Scholar]
- Culpin I, Stapinski L, Miles ÖB, Araya R, & Joinson C (2015). Exposure to socioeconomic adversity in early life and risk of depression at 18 years: The mediating role of locus of control. Journal of Affective Disorders, 183, 269–278. 10.1016/j.jad.2015.05.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham WA, Preacher KJ, & Banaji MR (2001). Implicit attitude measures: consistency, stability, and convergent validity. Psychological Science, 12(2), 163–170. 10.1111/1467-9280.00328 [DOI] [PubMed] [Google Scholar]
- Davies PT, Hentges RF, Coe JL, Martin MJ, Sturge-Apple ML, & Cummings EM (2016). The multiple faces of interparental conflict: Implications for cascades of children’s insecurity and externalizing problems. Journal of Abnormal Psychology, 125(5), 664–678. 10.1037/abn0000170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dedrick RF, & Greenbaum PE (2011). Multilevel Confirmatory Factor Analysis of a Scale Measuring Interagency Collaboration of Children’s Mental Health Agencies. Journal of Emotional and Behavioral Disorders, 19(1), 27–40. 10.1177/1063426610365879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick DM, Johnson JK, Viken RJ, & Rose RJ (2000). Testing between-family associations in within-family comparisons. Psychological Science, 11(5), 409–413. [DOI] [PubMed] [Google Scholar]
- Douglas EM, & Hines DA (2016). Children’s Exposure to Partner Violence in Homes Where Men Seek Help for Partner Violence Victimization. Journal of Family Violence, 31(4), 515–525. 10.1007/s10896-015-9783-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downey G, & Coyne JC (1990). Children of depressed parents: An integrative review. Psychological Bulletin, 108(1), 50–76. 10.1037/0033-2909.108.1.50 [DOI] [PubMed] [Google Scholar]
- Edwards JR, & Bagozzi RP (2000). On the nature and direction of relationships between constructs and measures. Psychological Methods, 5(2), 155. [DOI] [PubMed] [Google Scholar]
- Evans GW, & Kim P (2013). Childhood Poverty, Chronic Stress, Self-Regulation, and Coping. Child Development Perspectives, 7(1), 43–48. 10.1111/cdep.12013 [DOI] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- Ferraro KF, Schafer MH, & Wilkinson LR (2016). Childhood Disadvantage and Health Problems in Middle and Later Life: Early Imprints on Physical Health? American Sociological Review, 81(1), 107–133. 10.1177/0003122415619617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelhor D, Shattuck A, Turner H, & Hamby S (2013). Improving the Adverse Childhood Experiences Study Scale. JAMA Pediatrics, 167(1), 70 10.1001/jamapediatrics.2013.420 [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Shattuck A, Turner H, & Hamby S (2015). A revised inventory of Adverse Childhood Experiences. Child Abuse & Neglect, 48, 13–21. 10.1016/j.chiabu.2015.07.011 [DOI] [PubMed] [Google Scholar]
- Fletcher J, Mailick M, Song J, & Wolfe B (2013). A Sibling Death in the Family: Common and Consequential. Demography, 50(3), 803–826. 10.1007/s13524-012-0162-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford DC, Merrick MT, Parks SE, Breiding MJ, Gilbert LK, Edwards VJ, … Thompson WW (2014). Examination of the factorial structure of adverse childhood experiences and recommendations for three subscale scores. Psychology of Violence, 4(4), 432–444. 10.1037/a0037723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geiser C (2013). Data analysis with Mplus. New York, NY, US: Guilford Press. [Google Scholar]
- Geldhof GJ, Preacher KJ, & Zyphur MJ (2014). Reliability estimation in a multilevel confirmatory factor analysis framework. Psychological Methods, 19(1), 72–91. 10.1037/a0032138 [DOI] [PubMed] [Google Scholar]
- Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, & Janson S (2009). Burden and consequences of child maltreatment in high-income countries. The Lancet, 373(9657), 68–81. [DOI] [PubMed] [Google Scholar]
- Gjelsvik A, Dumont DM, & Nunn A (2013). Incarceration of a Household Member and Hispanic Health Disparities: Childhood Exposure and Adult Chronic Disease Risk Behaviors. Preventing Chronic Disease, 10 10.5888/pcd10.120281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, & Kessler RC (2010). Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Archives of General Psychiatry, 67(2), 113–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardt J, & Rutter M (2004). Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. Journal of Child Psychology and Psychiatry, 45(2), 260–273. [DOI] [PubMed] [Google Scholar]
- Hetherington EM (2005). Divorce and the Adjustment of Children. Pediatrics in Review, 26(5), 163–169. 10.1542/pir.26-5-163 [DOI] [PubMed] [Google Scholar]
- Hines DA, Kantor GK, & Holt MK (2006). Similarities in siblings’ experiences of neglectful parenting behaviors. Child Abuse & Neglect, 30(6), 619–637. 10.1016/j.chiabu.2005.11.008 [DOI] [PubMed] [Google Scholar]
- Idler EL, & Angel RJ (1990). Self-rated health and mortality in the NHANES-I Epidemiologic Follow-up Study. American Journal of Public Health, 80(4), 446–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler EL, Russell LB, & Davis D (2000). Survival, functional limitations, and self-rated health in the NHANES I epidemiologic follow-up study, 1992. American Journal of Epidemiology, 152(9), 874–883. [DOI] [PubMed] [Google Scholar]
- Iniguez KC, & Stankowski RV (2016). Adverse Childhood Experiences and Health in Adulthood in a Rural Population-Based Sample. Clinical Medicine & Research, 14(3–4), 126–137. 10.3121/cmr.2016.1306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Julian M (2001). The Consequences of Ignoring Multilevel Data Structures in Nonhierarchical Covariance Modeling. Structural Equation Modeling : A Multidisciplinary Journal, 8(3), 325–352. 10.1207/S15328007SEM0803_1 [DOI] [Google Scholar]
- Kashani JH, Daniel AE, Dandoy AC, & Holcomb W (1992). Family violence: Impact on children. Journal of American Academy of Child and Adolescent Psychiatry, 31(2), 181–189. [DOI] [PubMed] [Google Scholar]
- Kupersmidt JB, Griesler PC, DeRosier ME, Patterson CJ, & Davis PW (1995). Childhood Aggression and Peer Relations in the Context of Family and Neighborhood Factors. Child Development, 66(2), 360–375. 10.2307/1131583 [DOI] [PubMed] [Google Scholar]
- Laporte L, Paris J, Guttman H, Russell J, & Correa JA (2012). Using a Sibling Design to Compare Childhood Adversities in Female Patients With BPD and Their Sisters. Child Maltreatment, 17(4), 318–329. 10.1177/1077559512461173 [DOI] [PubMed] [Google Scholar]
- Lee RD, Fang X, & Luo F (2013). The Impact of Parental Incarceration on the Physical and Mental Health of Young Adults. Pediatrics, 131(4), e1188–e1195. 10.1542/peds.2012-0627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerner JV, Lerner RM, & Zabski S (1985). Temperament and elementary school children’s actual and rated academic performance: A test of a ‘goodness-of-fit’ model. Journal of Child Psychology and Psychiatry, 26(1), 125–136. [DOI] [PubMed] [Google Scholar]
- Luby JL, Barch DM, Belden A, Gaffrey MS, Tillman R, Babb C, … Botteron KN (2012). Maternal support in early childhood predicts larger hippocampal volumes at school age. Proceedings of the National Academy of Sciences of the United States of America, 109(8), 2854–2859. 10.1073/pnas.1118003109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS (1998). Protective and damaging effects of stress mediators. New England Journal of Medicine, 338(3), 171–179. [DOI] [PubMed] [Google Scholar]
- McLanahan S, Tach L, & Schneider D (2013). The Causal Effects of Father Absence. Annual Review of Sociology, 39(1), 399–427. 10.1146/annurev-soc-071312-145704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA (2016). Future Directions in Childhood Adversity and Youth Psychopathology. Journal of Clinical Child & Adolescent Psychology, 45(3), 361–382. 10.1080/15374416.2015.1110823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Sheridan MA (2016). Beyond Cumulative Risk A Dimensional Approach to Childhood Adversity. Current Directions in Psychological Science, 25(4), 239–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mersky JP, Janczewski CE, & Topitzes J (2017). Rethinking the Measurement of Adversity: Moving Toward Second-Generation Research on Adverse Childhood Experiences. Child Maltreatment, 22(1), 58–68. 10.1177/1077559516679513 [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, & Parker KJ (2011). Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin, 137(6), 959–997. 10.1037/a0024768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molnar BE, Buka SL, Brennan RT, Holton JK, & Earls F (2003). A Multilevel Study of Neighborhoods and Parent-to-Child Physical Aggression: Results From the Project on Human Development in Chicago Neighborhoods. Child Maltreatment, 8(2), 84–97. 10.1177/1077559502250822 [DOI] [PubMed] [Google Scholar]
- Morris AS, Robinson LR, Hays-Grudo J, Claussen AH, Hartwig SA, & Treat AE (2017). Targeting Parenting in Early Childhood: A Public Health Approach to Improve Outcomes for Children Living in Poverty. Child Development, 88 10.1111/cdev.12743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, & Robinson LR (2007). The Role of the Family Context in the Development of Emotion Regulation. Social Development, 16(2), 361–388. 10.1111/j.1467-9507.2007.00389.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B, & Asparouhov T (2009). Bayesian SEM: A more flexible representation of substantive theory. Retrieved from https://www.statmodel.com/download/BSEMv4.pdf [DOI] [PubMed]
- Muthén B, & Asparouhov T (2012). Muthén B, & Asparouhov T (2012). Bayesian SEM: A more flexible representation of substantive theory. Psychological Methods, 17, 313–335. [DOI] [PubMed] [Google Scholar]
- Muthén B, & Muthén LK (2010, August). Mplus Short Courses Topic 9 Bayesian Analysis Using Mplus. Retrieved from www.statmodel.com
- Muthén LK, & Muthén B (1998–2018). Mplus user’s guide (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Paquette JA, & Underwood MK (1999). Gender Differences in Young Adolescents’ Experiences of Peer Victimization: Social and Physical Aggression. Merrill-Palmer Quarterly, 45(2), 242–266. [Google Scholar]
- Pornprasertmanit S, Lee J, & Preacher KJ (2014). Ignoring Clustering in Confirmatory Factor Analysis: Some Consequences for Model Fit and Standardized Parameter Estimates. Multivariate Behavioral Research, 49(6), 518–543. 10.1080/00273171.2014.933762 [DOI] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, & Seeman TE (2002). Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin, 128(2), 330–366. 10.1037/0033-2909.128.2.330 [DOI] [PubMed] [Google Scholar]
- Rush J, & Hofer S (2014). Differences in within- and between-person factor structure of positive and … [DOI] [PMC free article] [PubMed]
- Savla JT, Roberto KA, Jaramillo-Sierra AL, Gambrel LE, Karimi H, & Butner LM (2013). Childhood abuse affects emotional closeness with family in mid- and later life. Child Abuse & Neglect, 37(6), 388–399. 10.1016/j.chiabu.2012.12.009 [DOI] [PubMed] [Google Scholar]
- Schulz MS, Waldinger RJ, Hauser ST, & Allen JP (2005). Adolescents’ behavior in the presence of interparental hostility: Developmental and emotion regulatory influences. Development and Psychopathology, 17(02). 10.1017/S0954579405050236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott BG, Burke NJ, Weems CF, Hellman JL, & Carrión VG (2013). The Interrelation of Adverse Childhood Experiences within an At-Risk Pediatric Sample. Journal of Child & Adolescent Trauma, 6(3), 217–229. 10.1080/19361521.2013.811459 [DOI] [Google Scholar]
- Springer KW, Sheridan J, Kuo D, & Carnes M (2007). Long-term physical and mental health consequences of childhood physical abuse: Results from a large population-based sample of men and women. Child Abuse & Neglect, 31(5), 517–530. 10.1016/j.chiabu.2007.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, & Runyan D (1998). Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: Development and psychometric data for a national sample of American parents. Child Abuse & Neglect, 22(4), 249–270. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Lehman BJ, Kiefe CI, & Seeman TE (2006). Relationship of Early Life Stress and Psychological Functioning to Adult C-Reactive Protein in the Coronary Artery Risk Development in Young Adults Study. Biological Psychiatry, 60(8), 819–824. 10.1016/j.biopsych.2006.03.016 [DOI] [PubMed] [Google Scholar]
- Taylor SE, Lerner JS, Sage RM, Lehman BJ, & Seeman TE (2004). Early Environment, Emotions, Responses to Stress, and Health. Journal of Personality, 72(6), 1365–1394. 10.1111/j.1467-6494.2004.00300.x [DOI] [PubMed] [Google Scholar]
- Tiet QQ, BIRD HR, DAVIES M, HOVEN C, COHEN P, JENSEN PS, & GOODMAN S (1998). Adverse Life Events and Resilience. Journal of the American Academy of Child & Adolescent Psychiatry, 37(11), 1191–1200. 10.1097/00004583-199811000-00020 [DOI] [PubMed] [Google Scholar]
- Wade R, Becker BD, Bevans KB, Ford DC, & Forrest CB (2016). Development and Evaluation of a Short Adverse Childhood Experiences Measure. American Journal of Preventive Medicine. 10.1016/j.amepre.2016.09.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade RJ, Shea JA, Rubin D, & Wood J (2014). Adverse childhood experiences of low-income urban youth. Pediatrics, 134(1), e13–e20. 10.1542/peds.2013-2475 [DOI] [PubMed] [Google Scholar]
- Walen HR, & Lachman ME (2000). Social support and strain from partner, family, and friends: Costs and benefits for men and women in adulthood. Journal of Social and Personal Relationships, 17(1), 5–30. [Google Scholar]
- Wallerstein JSPD (1991). The Long-Term Effects of Divorce on Children: A Review. Journal of the American Academy of Child, 30(3), 349–360. [DOI] [PubMed] [Google Scholar]
- Wolke D, Copeland WE, Angold A, & Costello EJ (2013). Impact of bullying in childhood on adult health, wealth, crime, and social outcomes. Psychological Science, 24(10), 1958–1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright AGC, Beltz AM, Gates KM, Molenaar PCM, & Simms LJ (2015). Examining the Dynamic Structure of Daily Internalizing and Externalizing Behavior at Multiple Levels of Analysis. Frontiers in Psychology, 6 10.3389/fpsyg.2015.01914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeitlin H (1994). Children with alcohol misusing parents. British Medical Bulletin, 50(1), 139–151. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.