Abstract
BACKGROUND/OBJECTIVES:
The treatment of type 2 diabetes in older adults requires special considerations including avoidance of hypoglycemia, yet variation in diabetes treatment with aging is not well understood. In this study, we compared nationally representative diabetes treatment patterns and trends between older adults (≥65 y) and younger adults (30–64 y).
DESIGN:
Repeated cross-sectional physician surveys from 2006 to 2015.
SETTING:
The National Ambulatory Medical Care Survey, an annual probability sample of visits to office-based US physicians.
PARTICIPANTS:
Adults with type 2 diabetes using one or more diabetes medications.
MEASUREMENTS:
Proportions of visits in which patients treated with each diabetes medication class were compared between older and younger adults in 2-year intervals.
RESULTS:
From 2006 to 2015, the average number of yearly visits for older and younger adults was 25.4 million and 24.2 million, respectively. In 2014–2015, visits for older compared with younger adults involved less use of metformin (56.0% vs 70.0%; p < .001) and glucagon-like peptide 1 receptor agonists (2.9% vs 6.2%; p = .004), and more use of long-acting insulin (30.2% vs 22.4%; p = .017); other classes were used similarly. During the study period, long-acting insulin use increased markedly in older adults, particularly between 2010 and 2015 where it rose from 12.5% to 30.2% of visits (P-trend <.001). In younger adult visits, long-acting insulin use increased modestly (17.2% to 22.4%) and at a slower rate compared with older adult visits (p < .001).
CONCLUSION:
The ambulatory treatment of type 2 diabetes differs between older and younger adults, with the treatment of older adults characterized by low use of newer diabetes medications and a greater and rapidly increasing use of long-acting insulin. These findings call for further research clarifying the comparative effectiveness and safety of newer diabetes medications and long-acting insulin to optimize diabetes care for older patients.
Keywords: age groups, aged, diabetes mellitus, type 2/drug therapy, diabetes mellitus, type 2/epidemiology, drug utilization
One in four US adults aged 65 years or older has diabetes, and older adults are the fastest growing segment of the diabetes population.1–3 Selecting the optimal treatment regimen for older adults with type 2 diabetes requires special considerations.4– 6 Older adults with diabetes often have multiple comorbid conditions that may present medication contraindications or interactions that limit the use of certain pharmacologic classes.4–8 Functional and cognitive limitations become more common with aging which could limit the use of complex regimens.4–6,9 Further, preventing hypoglycemia is critical for older patients, and guidelines recommend avoiding medications with the highest hypoglycemia risk, particularly long-acting sulfonylureas and sliding-scale insulin.4–6,10–12
In recent years, three newer classes of diabetes medications have become available: glucagon-like peptide 1 (GLP-1) receptor agonists, dipeptidyl peptidase 4 (DPP-4) inhibitors, and sodium/glucose cotransporter 2 (SGLT-2) inhibitors.13 These agents have a lower risk of hypoglycemia compared with sulfonylureas or insulin.14 However, evidence is lacking for their comparative effectiveness and safety in older patients who are frequently excluded from diabetes drug trials.14,15 Practice guidelines for older adults provide little direction for clinicians choosing between older medications with greater hypoglycemia risk and newer medications with less established evidence.4–6
Diabetes prescribing patterns provide insight into how the challenges of treating type 2 diabetes in older adults translate into clinical practice. US insurance claims data from 2006 to 2014 showed sparse uptake of newer diabetes medications in older adults, with sulfonylureas and insulin remaining the most common therapies after metformin.16,17 These findings suggest that sulfonylureas and insulin remain the mainstay of second-line therapy for older adults despite their higher hypoglycemia risk. To confirm these trends and determine whether they are unique to older adults, nationally representative data are needed that compare diabetes treatment between older adults and other age groups.
To fill these gaps, we compared national type 2 diabetes treatment patterns and trends among older adults (aged ≥65 y) and younger adults (aged 30–64 y) using the National Ambulatory Medical Care Survey (NAMCS), a nationally representative sample of ambulatory care in the United States. Insights from this study will help identify areas where diabetes treatment in older adults remains sub-optimal and inform future research agendas that are most likely to improve the care of older patients.
METHODS
Data source
We used the 2006–2015 publicly available data from NAMCS, a national sample of visits to office-based physicians primarily engaged in direct patient care conducted by the US Centers for Disease Control and Prevention, National Center for Health Statistics.18–20 NAMCS performs a stratified multistage sample of physician visits during 1-week reporting periods.18,19 Physicians are excluded if they are federally employed, a specialist in anesthesiology, pathology, or radiology, or 85 years or older.18,19 Data are collected by physicians and trained census field representatives who coordinate with physicians to standardize data collection. NAMCS methods are publicly available18,19 and described in detail in the supplement.
Study population
This study included visits in which a patient was identified as having type 2 diabetes and was treated with any diabetes medication, referred to here as treated diabetes visits. Type 2 diabetes was indicated on the NAMCS survey via a direct question asking whether the patient had type 2 diabetes (vs type 1 diabetes or unspecified diabetes). NAMCS respondents also reported up to three diagnoses associated with the visit that were coded according to the International Classification of Diseases, 9th Revision, Clinical Modification21; visit diagnoses are less sensitive for ascertaining diabetes status than the direct survey question.19,22 Before 2014, the direct survey question asked only whether the patient had diabetes with no question about subtype. Therefore, for years 2006 to 2013, we included visits for patients indicated by the direct survey question as having diabetes and having no visit diagnosis of type 1 diabetes, gestational diabetes, or other diabetes.31 Visits were excluded if the patient was younger than 30 years to increase the specificity for type 2 diabetes.
Survey variables
We classified older adults as 65 years or older and younger adults as 30 to 64 years of age. NAMCS ascertained the medications ordered, supplied (given to the patient at the visit), administered, or continued at the surveyed visits. This represents a patient’s active medication list, that is, the medications that the physician intends the patient to be taking at the end of the visit. The maximum number of medications that could be reported changed during the study period from 8 (2006–2011) to 10 (2012–2013) to 30 (2014–2015). Priority was given to new or continued medications and the medications used for the visit diagnoses.
Medications were identified by their generic components using Lexicon Plus (Cerner Multum, Inc).19,23 We grouped medications by pharmacologic class: metformin, sulfonylureas, thiazolidinediones, GLP-1 receptor agonists, DPP-4 inhibitors, SGLT-2 inhibitors, and insulin; data were insufficient to analyze other diabetes medication classes. Combination products contributed to each medication class in the combination. We also examined subcategories of interest: long-acting sulfonylureas (glyburide or chlorpropamide), long-acting insulin (insulin glargine or insulin detemir), and rapid-acting insulin (insulin aspart or insulin glulisine).
Statistical analysis
The main dependent variable was the proportion of treated diabetes visits in which the patient used a specified class of diabetes medication, reported as percentages. Data were grouped in 2-year intervals to provide adequate sample size to estimate subgroups. We also reported the total number of treated diabetes visits in which the patient used a specified diabetes medication class, presented as the yearly average.
All analyses were weighted to yield nationally representative estimates using Taylor-linearized variance estimation, and they met reliability standards recommended by the National Center for Health Statistics unless otherwise noted (see supplement for details).18,19,24 The confidence intervals (CIs) for survey-weighted proportions were calculated using a logit transform so that the end points fell between zero and one.25,26 Cross-sectional comparisons of categorical variables by age category were performed using survey-weighted Pearson χ2 tests with the Rao and Scott second-order correction.26,27 Temporal trends were modeled using survey-weighted logistic regression as done in Kantor et al.28 We used Stata v.14 (StataCorp LP, College Station, TX) for all analyses. Two-sided p ≤ .05 was considered statistically significant.
Subgroup and sensitivity analyses
To further characterize patterns of diabetes treatment across the age spectrum, we subdivided age into four categories that were approximate quartiles: age 30 to 54 years, 55 to 64 years, 65 to 74 years, and 75 years or older.
We conducted two sensitivity analyses to examine whether longitudinal changes in the NAMCS survey affected our findings. (1) We repeated our analysis of treatment patterns and trends after reclassifying visits in 2014–2015 using the less specific definition of type 2 diabetes that was available in previous study years. (2) We repeated our analysis of medication trends and number of medications used per visit, limiting the analysis to the first eight recorded medications to make this consistent across the study period.
RESULTS
Visit characteristics
The average number of yearly treated diabetes visits during the study period was 25.4 million (95% CI = 22.9–28.0) for older adults and 24.2 million (95% CI = 21.5–26.9) for younger adults. Longitudinal trends in treated diabetes visits can be found in Supplementary Table S1. The mean patient age was 74.7 years (standard deviation [SD] = 5.8 y) in older adult visits and 54.2 years (SD = 5.9 y) in younger adult visits; other visit characteristics can be found in Supplementary Table S2.
Diabetes treatment in older and younger adults, 2014–2015
Table 1 shows the cross-sectional comparison of diabetes treatment by age in the most recent survey period, 2014–2015. Compared with younger adult visits, older adult visits had greater use of long-acting insulin (30.2% vs 22.4% of visits; p = .017) and lower use of metformin (56.0% vs 70.0%; p < .001) and GLP-1 receptor agonists (2.9% vs 6.2%; p = .004). The estimate for GLP-1 receptor agonist use in older adult visits did not meet reliability criteria by a small margin; we repeated the analysis using an additional year of data (2013–2015) that met reliability criteria and found similar results (2.7% vs 5.9%; p < .001). Use of sulfonylureas, thiazolidinediones, and DPP-4 inhibitors was similar by age. SGLT-2 inhibitors were used in 7.2% of younger adult visits; data were insufficient to estimate this for older adult visits. The use of any insulin or any sulfonylurea was greater in older compared with younger adult visits (65.3% vs 54.8%; p = .016). Among visits in which sulfonylureas were used, there was less use of long-acting sulfonylureas (predominantly glyburide) in older compared with younger adults (19.9% vs 34.1%; p = .017).
Table 1.
Total and percentage use of diabetes medications in treated diabetes visits by age, 2014–2015
| Treatment | Age 30–64 y |
Age ≥ 65 y |
P-valuea | Most common medicationb |
||
|---|---|---|---|---|---|---|
| Visits, 100 000 (95% Cl) |
Visits, % (95% Cl) |
Visits, 100 000 (95% Cl) |
Visits, % (95% Cl) |
|||
| Metformin | 141.0 (117.5–164.6) | 70.0 (64.1–75.4) | 130.4 (107.5–153.3) | 56.0 (50.1–61.7) | <.001 | Metformin |
| Any sulfonylurea | 58.2 (43.5–73.1) | 28.9 (23.6–34.9) | 75.8 (62.0–89.7) | 32.6 (27.7–37.9) | .39 | Glipizide |
| Long-acting sulfonylureasc | 19.9 (9.8–29.9) | 9.9 (6.3–15.1) | 15.1 (10.5–19.6) | 6.5 (4.9–8.5) | .13 | Glyburide |
| Thiazolidinediones | 9.3 (5.1–13.5) | 4.6 (3.0–7.1) | 9.3 (5.3–13.3) | 4.0 (2.6–6.1) | .59 | Pioglitazone |
| DPP-4 inhibitors | 33.0 (22.7–43.3) | 16.3 (12.8–20.7) | 39.7 (28.5–51.0) | 17.1 (13.9–20.7) | .82 | Sitagliptin |
| GLP-1 receptor agonists | 12.5 (6.9–18.1) | 6.2 (4.1–9.1) | 6.8 (2.5–11.0)d | 2.9 (1.6–5.4)d | .004 | Liraglutide |
| SGLT-2 inhibitors | 14.6 (5.9–23.3) | 7.2 (4.3–12.0) | e | e | Canagliflozin | |
| Any insulin | 66.4 (48.7–84.1) | 33.0 (26.9–39.6) | 90.7 (68.1–113.3) | 39.0 (34.2–43.9) | .11 | Insulin glargine |
| Long-acting insulin | 45.1 (30.9–59.2) | 22.4 (17.3–28.5) | 70.3 (48.8–91.9) | 30.2 (25.0–35.9) | .017 | Insulin glargine |
| Rapid-acting insulin | 21.7 (11.2–32.2) | 10.8 (7.1–16.0) | 21.3 (14.5–28.1) | 9.1 (7.1–11.7) | .51 | Insulin aspart |
Data are average number of treated diabetes visits per year in 100 000s or percentage of treated diabetes visits in the designated age category. Combination products contributed to each medication class in the combination.
Comparing age categories by survey-weighted Pearson χ2 test.
The generic name of the most common medication in each class is shown. These are the same for both age categories.
Predominantly glyburide, <1% chlorpropamide.
Estimated based on 90 unweighted visits with relative standard error of 32%.
Too few visits for accurate estimation.
Abbreviations: CI, confidence interval; DPP, dipeptidyl peptidase; GLP glucagon-like peptide; SGLT, sodium/glucose cotransporter.
Diabetes medication trends in older and younger adults
Figures 1 and 2 show trends from 2006 to 2015 in the use of noninsulin diabetes medications and insulin, respectively, presented quantitatively in Table 2. Trends in diabetes medication use in both older and younger adult visits were characterized by increasing use of metformin, DPP-4 inhibitors, and insulin, and decreasing use of sulfonylureas and thiazolidinediones. In older adult visits, long-acting sulfonylurea use decreased substantially during the study period from 18.5% to 6.5% (P-trend <.001), whereas the decrease was modest in younger adult visits (13.6% to 9.9%; P-trend = .059).
Figure 1.
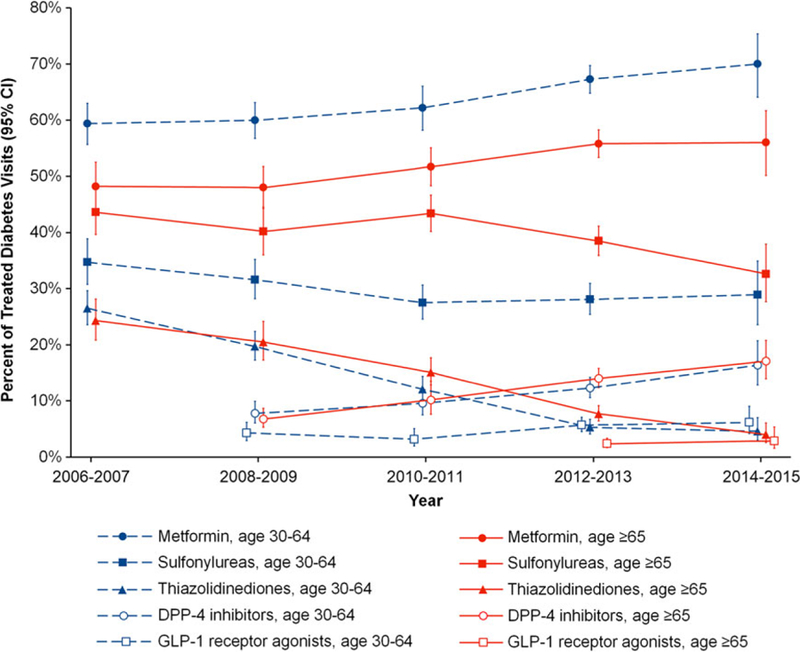
Trends in noninsulin diabetes medications used in treated diabetes visits by age, 2006–2015.
Estimates are jittered to show confidence intervals (CIs). Time periods with too few visits for accurate estimation are excluded.
Figure 2.
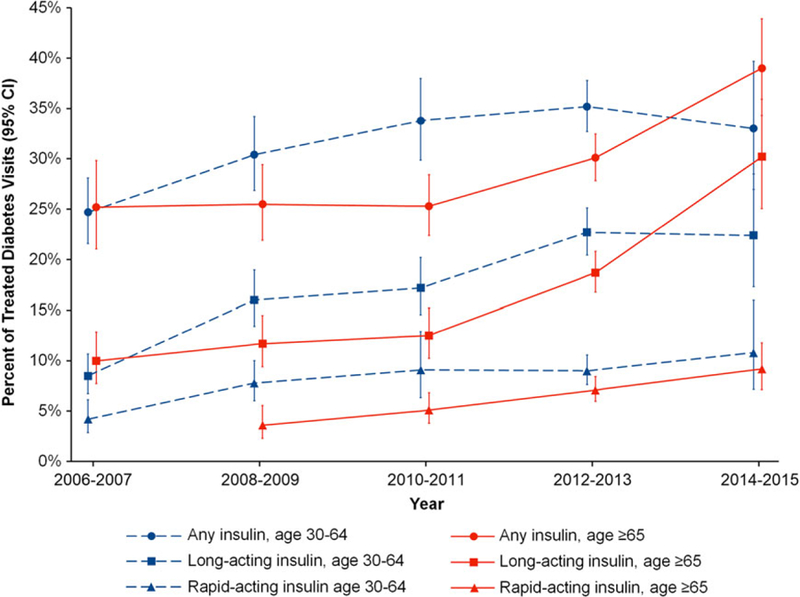
Trends in insulin used in treated diabetes visits by age, 2006–2015.
Estimates are jittered to show confidence intervals (CIs). Time periods with too few visits for accurate estimation are excluded.
[Color figure can be viewed at wileyonlinelibrary.com]
Table 2.
Trends in diabetes medications used in treated diabetes visits by age, 2006–2015
| Treatment | Age 30–64 y |
Age ≥ 65 y |
P-interactionc | ||
|---|---|---|---|---|---|
| Yearly change in % using drug class (95% Cl)a |
P-trendb | Yearly change in % using drug class (95% Cl)a |
P-trendb | ||
| 2006–2015 | |||||
| Metformin | 1.43 (0.79 to 2.08) | <.001 | 1.20 (0.49 to 1.92) | .001 | .45 |
| Any sulfonylurea | −0.76 (−1.50 to −0.02) | .045 | −1.17 (−1.88 to −0.46) | .001 | .62 |
| Long-acting sulfonylureas | −0.53 (−1.06 to −0.00) | .059 | −1.39 (−1.79 to −0.99) | <.001 | .038 |
| Thiazolidinediones | −3.10 (−3.51 to −2.68) | <.001 | −2.75 (−3.21 to −2.29) | <.001 | .12 |
| DPP-4 inhibitors | 1.38 (0.73–2.02) | <.001 | 1.73 (1.14–2.32) | <.001 | .53 |
| GLP-1 receptor agonists | 0.39 (−0.04 to 0.83) | .073 | 0.25 (−0.74 to 1.24) | .61 | .78 |
| Any insulin | 1.07 (0.33–1.82) | .005 | 1.61 (0.93–2.30) | <.001 | .18 |
| Long-acting insulin | 1.70 (1.07–2.34) | <.001 | 2.40 (1.77–3.04) | <.001 | .031 |
| Rapid-acting insulin | 0.70 (0.20–1.19) | .003 | 0.93 (0.49–1.38) | <.001 | .061 |
| Insulin 2010–2015 | |||||
| Any insulin | −0.16 (−1.97 to 1.66) | .87 | 3.33 (2.00–4.68) | <.001 | <.001 |
| Long-acting insulin | 1.37 (−0.21–2.94) | .081 | 4.33 (2.98–5.69) | <.001 | <.001 |
| Rapid-acting insulin | 0.38 (−0.83–1.60) | .56 | 0.88 (0.35–1.42) | .003 | .24 |
Insulin products are additionally presented between 2010 and 2015 to examine qualitatively different trends during this time frame. Excluded from analysis are periods with insufficient data (DPP-4 inhibitors before 2008; GLP-1 receptor agonists before 2008 in age 30–64 years, before 2012 in age ≥ 65 years; rapid-acting insulin before 2008 in age ≥ 65 years).
Predicted using survey-weighted logistic regression for the outcome of use of the designated medication, with the 2-year period as a linear predictor.
The P-value of the β-coefficient for 2-year period in the logistic regression described above.
Comparing trends in younger and older adults as the P-value of the β-coefficient for the interaction term in survey-weighted logistic regression for the outcome of use of the designated medication, with predictors of 2-year period, age category, and their interaction.
Abbreviations: CI, confidence interval; DPP, dipeptidyl peptidase; GLP glucagon-like peptide; SGLT, sodium/glucose cotransporter.
There was a marked increase in the use of insulin in older adult visits, particularly from 2010–2011 onward. During this period, any insulin use rose from 25.3% to 39.0% of older adult visits (P-trend <.001), and long-acting insulin use rose from 12.5% to 30.2% (P-trend <.001). In younger adult visits, use of any insulin was stable (33.8% to 33.0%; P-trend = 0.87); long-acting insulin increased modestly (17.2% to 22.4%, P-trend = 0.081). The use of any insulin and long-acting insulin increased significantly faster in older adult visits than in younger adult visits during this time period (p < .001 for each interaction between age category and medication trend).
Diabetes monotherapy and combination therapy in older and younger adults
The most common monotherapies in both older and younger adult visits were metformin, insulin, and sulfonylureas (Table 3). In older compared with younger adult visits, metformin monotherapy was used less often (43.4% vs 59.6%, p = .010); sulfonylurea monotherapy was used more often (15.7% vs 4.4%, p < .001). Combination therapies were overall similar in older and younger adult visits. Notably, the combination of sulfonylurea and insulin was the third most common combination among older adult visits, accounting for 8.4% of combination therapy visits.
Table 3.
Most common diabetes medications used alone and in combination by age, 2014–2015
| Age 30–64 y |
Age ≥ 65 y |
P-valuea | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Treatment | Visits, 100 000 (95% Cl) |
Visits, % (95% Cl) | Treatment | Visits, 100 000 (95% Cl) |
Visits, % (95% Cl) | |||||
| Monotherapy visitsb | ||||||||||
| Monotherapies | ||||||||||
| 1: most common | Metformin | 64.1 (49.6–78.5) | 59.6(51.4–67.3) | Metformin | 58.8 (45.1–72.6) | 43.4 (35.3–51.8) | .010 | |||
| 2 | Insulin | 27.6 (19.6–35.7) | 25.7(18.8–34.1) | Insulin | 46.2 (31.7–60.6) | 34.0 (28.4–40.1) | .083 | |||
| 3 | Sulfonylurea | 4.8 (2.7–6.8) | 4.4 (2.8–7.0) | Sulfonylurea | 21.2 (14.2–28.2) | 15.7 (11.6–20.7) | <.001 | |||
| Total | 107.5 (81.4–113.6) | 100.0 | 135.7 (107.2–164.1) | 100.0 | ||||||
| Combination therapy visits | ||||||||||
| Combinations: mutually exclusive | ||||||||||
| 1: most common | Metformin + sulfonylurea | 22.7 (15.2–30.2) | 24.2(17.9–31.8) | Metformin + sulfonylurea | 23.0 (17.2–28.8) | 23.7 (18.7–29.4) | .90 | |||
| 2 | Metformin + insulin | 10.1 (6.3–13.9) | 10.8 (7.5–15.2) | Metformin + insulin | 15.9 (7.6–24.2) | 16.3 (10.2–25.2) | .19 | |||
| 3 | Metformin + DPP-4 | 8.3 (4.0–12.6) | 8.8(5.4–14.0) | Sulfonylurea + insulin | 8.2 (3.6–12.7) | 8.4 (4.9–14.0) | .36 | |||
| Combinations: not mutually exclusive | ||||||||||
| 1: most common | Metformin + any | 77.0 (61.1–92.9) | 82.0(73.1–88.3) | Metformin + any | 71.6 (56.9–86.3) | 73.7 (66.5–79.8) | .16 | |||
| 2 | Sulfonylurea + any | 53.5 (39.2–67.8) | 57.0 (47.9–65.6) | Sulfonylurea + any | 54.6 (43.6–65.6) | 56.2 (47.1 −64.9) | .90 | |||
| 3 | Insulin + any | 38.7 (25.9–51.6) | 41.3 (33.3–49.7) | Insulin + any | 44.5 (32.3–56.7) | 45.8 (38.6–53.2) | .30 | |||
| 4 | DPP-4 + any | 29.5 (20.0–39.1) | 31.4(24.1–39.7) | DPP-4 + any | 32.1 (23.6–40.6) | 33.0 (27.1 −39.6) | .74 | |||
| 5 | GLP-1 + any | 10.0 (5.6–14.4) | 10.6 (7.0–15.7) | TZD + any | 8.4 (4.4–12.4) | 8.6 (5.6–13.0) | .057 | |||
| Total | 93.9 (74.4–113.4) | 100.0 | 97.2 (79.2–115.1) | 100.0 | ||||||
Data are average number of treated diabetes visits per year in 100 000’s, or percentage of single- or multiclass visits in the respective age category.
Comparing age categories by survey-weighted Pearson χ2 test. Where the listed treatment differs by age category, the P-value refers to the treatment listed for age 30–64 years.
Monotherapy defined as visits in which a single drug class is used.
Abbreviations: CI, confidence interval; DPP, dipeptidyl peptidase; GLP glucagon-like peptide; SGLT, sodium/glucose cotransporter; TZD, thiazolidinedione.a
In 2014–2015, the number of diabetes medications used per visit was similar in older and younger adults (Supplementary Table S3), with 30.6% of older adult visits using two medication classes and 11.2% using three or more classes; 29.9% of younger adult visits used two classes, and 16.7% used three or more classes. Over time, there was an increase in the proportion of younger adult visits using three or more classes (P-trend = 0.036) and in the proportion of older adult visits using two or more classes (P-trend = 0.032).
Diabetes treatment in four age subgroups
Examining diabetes treatment in 2014–2015 among four age subgroups revealed several notable findings (Supplementary Table S4). Metformin use decreased across categories of increasing age (P-trend <.001) and was much lower among individuals 75 years or older compared with other age categories (49.2% vs 66.5%; p < .001). Temporal trends in diabetes treatment showed similar increases in the use of long-acting, rapid-acting, and any insulin for individuals aged 65 to 74 years and 75 years or older (Supplementary Figure S1).
Sensitivity analyses
The results of sensitivity analyses can be found in Supplementary Tables S5 through S8. Reclassifying visits in 2014–2015 using the less specific definition of type 2 diabetes from previous study years resulted in an additional 12.0 million yearly visits and 12.5 million yearly visits for older and younger adults, respectively. Of these additional visits, 9.5% were classified as type 1 diabetes; 90.5% were classified as unspecified diabetes in the primary analysis. Compared with results of the primary analysis, sulfonylurea use in 2014–2015 was now significantly greater in older than younger adult visits; there were no other substantial differences in treatment patterns and trends. Using only the first eight recorded medications found that temporal trends in the number of diabetes medications used per visit were attenuated compared with the primary analysis.
DISCUSSION
This study compared the ambulatory treatment of type 2 diabetes among older and younger adults in the United States using nationally representative data from 2006 through 2015. During the most recent survey years, there was greater use of long-acting insulin in older adult visits compared with younger adult visits, and lower use of metformin and GLP-1 receptor agonists. There was a marked increase in the use of insulin in older adult visits over time, particularly long-acting insulin, whereas insulin use in younger adult visits was relatively stable. Therefore, the treatment of type 2 diabetes is evolving differently in older and younger adults, driven in part by a rapid increase in long-acting insulin use among older adults.
We found key treatment differences between older and younger adults in 2014–2015. There was lower use of metformin in older adult visits, particularly for those individuals aged 75 years or older, likely due in part to a higher prevalence of chronic kidney disease among older adults, which is the major contraindication to metformin use.8,29,30 In 2016, the US Food and Drug Administration adopted less restrictive guidelines on the use of metformin in chronic kidney disease.31 Future studies should examine the impact of this change. We also found that DPP-4 inhibitor use was similar by age, whereas GLP-1 receptor agonists were used less commonly in older adult visits. It is possible that GLP-1 receptor agonists are less desirable for older patients due to their side-effect profile or injectable mode of administration.8,32
Longitudinal trends in older adult visits were characterized by decreasing use of sulfonylureas and thiazolidinediones and increasing use of metformin, insulin, and newer diabetes medications, consistent with previous studies using claims data.16,17 Notably, long-acting insulin use in older adult visits more than doubled between 2010–2011 and 2014–2015, resulting in insulin now being the second most common treatment after metformin. This could reflect the increasing complexity of diabetes treatment among older adults, although we observed only a small increase in the number of diabetes medications used per visit during the study period.
We hypothesize that several other factors are driving this trend. First, use of sulfonylureas and thiazolidinediones is decreasing, in accordance with practice guidelines to avoid these classes in older patients.4,5,12 Second, use of newer classes of diabetes medications has been sparse in older adults, with GLP-1 receptor agonists used particularly infrequently. Third, whereas use of DPP-4 inhibitors has increased substantially in older adults, they have lower glycemic efficacy than other classes and thus may not substitute for insulin.14 Notably, evidence is lacking that long-acting insulin is safer or more effective than newer medication classes in older adults.4–6 Therefore, the rapidly increasing use of long-acting insulin in older adults calls for further research to clarify its effectiveness and safety compared with newer classes of diabetes medications to determine whether, and under which circumstances, long-acting insulin should be preferred for older patients.
These findings also have implications for the prevention of hypoglycemia that is almost entirely due to sulfonylureas or insulin.4,5,10 Sulfonylureas or insulin were used in nearly two-thirds of older adult visits, a significantly higher proportion than younger adult visits. The progressive nature of type 2 diabetes may contribute to greater insulin use over time8,33; data on diabetes duration are not available in NAMCS. Use of long-acting sulfonylureas, predominantly glyburide, has been decreasing in older adult visits, which may be related to the inclusion of glyburide in the American Geriatrics Society Beers Criteria in 2012.12,34 However, glyburide still accounts for approximately 20% of sulfonylureas used in older adult visits. Therefore, the treatment of type 2 diabetes in older adults remains suboptimal with respect to minimizing the use of agents with higher hypoglycemia risk.
Our findings also have implications for understanding the rising cost of diabetes care in the United States.35 Currently, insulin accounts for approximately half of diabetes medication expenditures, and rising costs have been attributed to use of expensive long-acting insulin products.35,36 We identified that increasing use of long-acting insulin is predominantly attributed to older adults. Therefore, understanding the reasons for this trend will be critical to achieving high-value care for patients with type 2 diabetes in the United States.
This study has several limitations. NAMCS data represent ambulatory visits and not individual patients who may be over- or underrepresented depending on their use of ambulatory care. In particular, patients with multiple chronic conditions have greater healthcare utilization and may be overrepresented compared with the general population.37 A dedicated survey question identifying patients with type 2 diabetes was available in NAMCS starting in 2014; before this we relied on diagnosis codes to exclude other diabetes subtypes. Our data suggest this method likely failed to exclude a small number of individuals with type 1 diabetes and some individuals with other subtypes. However, our findings of diabetes treatment patterns in 2014–2015 and temporal trends were similar regardless of diabetes definition. NAMCS increased the number of medications that could be listed during the survey period, and we cannot exclude that our findings of increasing number of medications used per visit were a result of this change.
In conclusion, the outpatient treatment of type 2 diabetes differs between older and younger adults, with the treatment of older adults characterized by a low use of newer diabetes medications and a disproportionately high and growing use of long-acting insulin. As a result of these trends, nearly two-thirds of older adults are treated with second-line medications with a high risk of causing hypoglycemia. These findings highlight the need for more research in older adults to clarify the effectiveness and safety of newer diabetes medications that may have a lower risk of hypoglycemia compared to long-acting insulin. These data will be necessary to develop practice guidelines for older adults that address the tension between the use of insulin vs newer diabetes medications, helping clinicians select the optimal treatment for type 2 diabetes across the age spectrum.
Supplementary Material
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article.
Methods Supplement
Supplementary Table S1. Trends in treated diabetes visits and total outpatient visits by age, 2006-2015.
Supplementary Table S2. Characteristics of treated diabetes visits by age, 2014-2015.
Supplementary Table S3. Trends in the number of diabetes medication classes used in treated diabetes visits by ages, 2006-2015.
Supplementary Table S4. Total and percentage use of diabetes medications in treated diabetes visits, 2014-2015, in four age categories.
Supplementary Figure S1. Trends in diabetes medications used in treated diabetes visits, 2006-2015, in four age categories.
Supplementary Table S5. Total and percentage use of diabetes medications in treated diabetes visits by age, 2014-2015; sensitivity analysis using the pre-2014 definition of type 2 diabetes.
Supplementary Table S6. Trends in diabetes medications used in treated diabetes visits by age, 2006-2015; sensitivity analysis using the pre-2014 definition of type 2 diabetes.
Supplementary Table S7. Trends in diabetes medications used in treated diabetes visits by age, 2006-2015; sensitivity analysis limiting to the first eight coded medications.
Supplementary Table S8. Trends in the number of diabetes medication classes used in treated diabetes visits by age, 2006 2015; sensitivity analysis limiting to first eight coded medications.
ACKNOWLEDGMENTS
The authors would like to thank Christine A. Lucas, MSW, MPH, survey statistician for the National Center for Health Statistics, for assistance with reporting NAMCS methodology.
Financial Disclosure: Scott J. Pilla was supported by the National Heart, Lung, and Blood Institute (5T32HL007180–40, PI: Hill-Briggs). Jodi B. Segal was supported by the National Institute on Aging (1K24AG049036). Cynthia M. Boyd was supported by the National Institute on Aging (1K24AG056578–01).
Footnotes
Conflict of Interest: Cynthia M. Boyd is a coauthor for a chapter on multimorbidity for UpToDate. G. Caleb Alexander is chair of the FDA’s Peripheral and Central Nervous System Advisory Committee, has served as a paid advisor to IQVIA, serves on the advisory board of MesaRx Innovations, is a member of OptumRx’s National P&T Committee, and holds equity in Monument Analytics, a healthcare consultancy whose clients include the life sciences industry as well as plaintiffs in opioid litigation. This arrangement was reviewed and approved by Johns Hopkins University in accordance with its conflict of interest policies. The remaining authors have no other relevant relationships to declare.
Sponsor’s Role: The funding source had no role in the design, methods, subject recruitment, data collections, or analysis and preparation of the article.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC). National Diabetes Statistics Report 2017 Atlanta, GA: CDC, US Dept of Health and Human Services; 2017. [Google Scholar]
- 2.Boyle JP, Honeycutt AA, Narayan KM, et al. Projection of diabetes burden through 2050: impact of changing demography and disease prevalence in the U.S. Diabetes Care 2001;24:1936–1940. [DOI] [PubMed] [Google Scholar]
- 3.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr 2010;8:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Diabetes Association. 11. Older adults: standards of medical care in diabetes-2018. Diabetes Care 2018;41:S119–S125. [DOI] [PubMed] [Google Scholar]
- 5.American Geriatrics Society Expert Panel on Care of Older Adults with Diabetes Mellitus, Moreno G, Mangione CM, Kimbro L, Vaisberg E. Guidelines abstracted from the American Geriatrics Society guidelines for improving the care of older adults with diabetes mellitus: 2013 update. J Am Geriatr Soc 2013;61:2020–2026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang ES. Management of diabetes mellitus in older people with comorbidities. BMJ 2016;353:i2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laiteerapong N, Iveniuk J, John PM, Laumann EO, Huang ES. Classification of older adults who have diabetes by comorbid conditions, United States, 2005–2006. Prev Chronic Dis 2012;9:E100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.American Diabetes Association. 8. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2018. Diabetes Care 2018; 41:S73–S85. [DOI] [PubMed] [Google Scholar]
- 9.National Center for Health Statistics. Tables of Summary Health Statistics, National Health Interview Survey, 2016 https://www.cdc.gov/nchs/nhis/SHS/tables.htm. Accessed May 5, 2018.
- 10.Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med 2011;365: 2002–2012. [DOI] [PubMed] [Google Scholar]
- 11.Lipska KJ, Ross JS, Wang Y, et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, 1999 to 2011. JAMA Intern Med 2014;174:1116–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2015;63:2227–2246. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Food & Drug Administration. Drugs@FDA: FDA Approved Drug Products https://www.accessdata.fda.gov/scripts/cder/daf/. Accessed May 5, 2018.
- 14.Maruthur NM, Tseng E, Hutfless S, et al. Diabetes medications as monotherapy or metformin-based combination therapy for type 2 diabetes: a systematic review and meta-analysis. Ann Intern Med 2016;164:740–751. [DOI] [PubMed] [Google Scholar]
- 15.Cruz-Jentoft AJ, Carpena-Ruiz M, Montero-Errasquin B, Sanchez-Castellano C, Sanchez-Garcia E. Exclusion of older adults from ongoing clinical trials about type 2 diabetes mellitus. J Am Geriatr Soc 2013;61: 734–738. [DOI] [PubMed] [Google Scholar]
- 16.Landon BE, Zaslavsky AM, Souza J, Ayanian JZ. Trends in diabetes treatment and monitoring among Medicare beneficiaries. J Gen Intern Med 2018;33:471–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lipska KJ, Yao X, Herrin J, et al. Trends in drug utilization, glycemic control, and rates of severe hypoglycemia, 2006–2013. Diabetes Care 2017;40: 468–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Center for Health Statistics. About the Ambulatory Health Care Surveys https://www.cdc.gov/nchs/ahcd/about_ahcd.htm. Accessed May 5, 2018.
- 19.National Center for Health Statistics. NAMCS micro-data file documentation, 2006 to 2015 ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Datasets/NAMCS/ Accessed May 5, 2018.
- 20.National Center for Health Statistics. NAMCS micro-data set files, 2006 to 2015 ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Datasets/NAMCS/ Accessed May 5, 2018.
- 21.National Center for Health Statistics. ICD-9-CM: International Classification of diseases, 9th Revision, Clinical Modification http://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed May 5, 2018.
- 22.Asao K, McEwen LN, Lee JM, Herman WH. Ascertainment of outpatient visits by patients with diabetes: the National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS). J Diabetes Complications 2015;29:650–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cerner Corporation. Cerner Drug Database https://www.cerner.com/solutions/drug-database. Accessed May 5, 2018.
- 24.McCaig LF, Burt CW. Understanding and interpreting the National Hospital Ambulatory Medical Care Survey: key questions and answers. Ann Emerg Med 2012;60:716–721 e711. [DOI] [PubMed] [Google Scholar]
- 25.Stuart A, Ord JK. Kendall’s Advanced Theory of Statistics: Distribution Theory London, UK: Arnold; 1994. [Google Scholar]
- 26.StataCorp. Stata 14 Base Reference Manual College Station, TX: Stata Press; 2015. [Google Scholar]
- 27.Rao JNK, Scott AJ. The analysis of categorical data from complex sample surveys: chi-squared tests for goodness of fit and Independence in two-way tables. J Am Stat Assoc 1981;76:221–230. [Google Scholar]
- 28.Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999–2012. JAMA 2015;314:1818–1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. Chronic Kidney Disease Surveillance System - Crude Prevalence of CKD Stage 1–4 by Age, 2013–2014 http://www.cdc.gov/ckd. Accessed May 5, 2018.
- 30.Vasisht KP, Chen SC, Peng Y, Bakris GL. Limitations of metformin use in patients with kidney disease: are they warranted? Diabetes Obes Metab 2010;12:1079–1083. [DOI] [PubMed] [Google Scholar]
- 31.Lipska KJ, Flory JH, Hennessy S, Inzucchi SE. Citizen petition to the US Food and Drug Administration to change prescribing guidelines: the metformin experience. Circulation 2016;134:1405–1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ng CJ, Lai PS, Lee YK, Azmi SA, Teo CH. Barriers and facilitators to starting insulin in patients with type 2 diabetes: a systematic review. Int J Clin Pract 2015;69:1050–1070. [DOI] [PubMed] [Google Scholar]
- 33.Pilla SJ, Yeh HC, Juraschek SP, Clark JM, Maruthur NM. Predictors of insulin initiation in patients with type 2 diabetes: an analysis of the look AHEAD randomized trial. J Gen Intern Med 2018;33:839–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc 2012;60:616–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care 2018;41:917–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Turner LW, Nartey D, Stafford RS, Singh S, Alexander GC. Ambulatory treatment of type 2 diabetes in the U.S., 1997–2012. Diabetes Care 2014;37: 985–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lehnert T, Heider D, Leicht H, et al. Review: health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev 2011;68:387–420. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article.
Methods Supplement
Supplementary Table S1. Trends in treated diabetes visits and total outpatient visits by age, 2006-2015.
Supplementary Table S2. Characteristics of treated diabetes visits by age, 2014-2015.
Supplementary Table S3. Trends in the number of diabetes medication classes used in treated diabetes visits by ages, 2006-2015.
Supplementary Table S4. Total and percentage use of diabetes medications in treated diabetes visits, 2014-2015, in four age categories.
Supplementary Figure S1. Trends in diabetes medications used in treated diabetes visits, 2006-2015, in four age categories.
Supplementary Table S5. Total and percentage use of diabetes medications in treated diabetes visits by age, 2014-2015; sensitivity analysis using the pre-2014 definition of type 2 diabetes.
Supplementary Table S6. Trends in diabetes medications used in treated diabetes visits by age, 2006-2015; sensitivity analysis using the pre-2014 definition of type 2 diabetes.
Supplementary Table S7. Trends in diabetes medications used in treated diabetes visits by age, 2006-2015; sensitivity analysis limiting to the first eight coded medications.
Supplementary Table S8. Trends in the number of diabetes medication classes used in treated diabetes visits by age, 2006 2015; sensitivity analysis limiting to first eight coded medications.


