Abstract
Objective
A substantial amount of individuals with substance use disorders (SUD) also meet criteria for posttraumatic stress disorder (PTSD). Prolonged exposure (PE) is an effective, evidenced-based treatment for PTSD, but there is limited data on its use among individuals with current alcohol or drug use disorders. This study evaluated the efficacy of an integrated treatment that incorporates PE (Concurrent Treatment of PTSD and Substance Use Disorders Using Prolonged Exposure or COPE) among veterans.
Method
Military veterans (N = 81, 90.1% male) with current SUD and PTSD were randomized to 12 sessions of COPE or Relapse Prevention (RP). Primary outcomes included the Clinician-Administered PTSD Scale (CAPS), PTSD Checklist-Military version (PCL-M), and the Timeline Follow-back (TLFB).
Results
On average, participants attended 8 out of 12 sessions and there were no group differences in retention. Intent-to-treat analyses revealed that COPE, in comparison to RP, resulted in significantly greater reductions in CAPS (d = 1.4, p <. 001) and PCL-M scores (d = 1.3, p = .01), as well as higher rates of PTSD diagnostic remission (OR = 5.3, p < .01). Both groups evidenced significant and comparable reductions in SUD severity during treatment. At 6-months follow-up, participants in COPE evidenced significantly fewer drinks per drinking day than participants in RP (p = .05).
Conclusions
This study is the first to report on the use of an integrated, exposure-based treatment for co-occurring SUD and PTSD in a veteran sample. The findings demonstrate that integrated, exposure-based treatments are feasible and effective for military veterans with SUD and PTSD. Implications for clinical practice are discussed.
Keywords: substance use disorder, PTSD, posttraumatic stress disorder, addiction, prolonged exposure, veterans
1. Introduction
Substance use disorders (SUD) and posttraumatic stress disorder (PTSD) are two of the most prevalent psychiatric disorders in the United States. In the general population, lifetime estimates are approximately 29.1% for alcohol use disorder, the most common SUD (Grant et al., 2015), and 8.3% for PTSD (Kilpatrick et al., 2013). Among military personnel and veterans, rates of SUD and PTSD are 2–4 times higher than in the general population (Hoge, 2015; Petrakis, Rosenheck, & Desai, 2011; Stein et al., 2017; Teeters et al., 2017).
Research demonstrates high rates of comorbidity between SUD and PTSD. Epidemiologic data indicate that individuals with, as compared to without, an SUD are 6.5 times more likely to have comorbid PTSD (Mills, Teesson, Ross, & Peters, 2006). Comorbid SUD/PTSD is associated with substantial psychiatric comorbidity (e.g., depression), medical problems, vocational impairment, increased violence, and poor treatment outcomes (Barrett, Teeson, & Mills, 2014; Simpson, Lehavot & Petrakis, 2017; Stein et al., 2017).
Integrated treatments, in which both disorders are addressed concurrently, may help optimize outcomes. Concurrent Treatment of PTSD and Substance Use Disorders Using Prolonged Exposure (COPE) is an integrated treatment that utilizes Prolonged Exposure (PE; Foa, Hembree, & Rothbaum, 2007) in combination with cognitive behavioral therapy for SUD. Previous studies of COPE among civilians demonstrate efficacy in reducing SUD and PTSD severity (Brady et al., 2001; Mills et al., 2012; Persson et al., 2017; Ruglass et al., 2017). Despite extensive research demonstrating the ability of PE to significantly reduce PTSD severity (Powers, Halpern, Ferenschak, Gillihan, & Foa, 2010), some clinicians are reluctant to engage in exposure-based trauma work with SUD patients (Norman & Hamblen, 2017). Accumulating evidence demonstrates, however, that PE is safe and associated with significant reductions in SUD severity, even among individuals with complex trauma histories (Foa et al., 2013, 2017; Mills et al., 2012; Norman et al., 2016; Peck et al., 2018; Persson et al., 2017; Ruglass et al., 2017). Further support is provided by recent meta-analyses and critical reviews of the literature demonstrating that exposure-based, integrated treatment results in significant improvements in SUD and PTSD (Roberts, Roberts, Jones, & Bisson, 2015; Simpson et al., 2017).
Given the sustained military operations in Afghanistan and Iraq, and the disproportionately high rates of SUD and PTSD among veterans, the current study addresses a clinically important need by evaluating, for the first time, the efficacy of COPE among military veterans. An active treatment control group was used to control for time and therapeutic attention. We hypothesized that the integrated treatment would reduce self-report and clinician-rated PTSD symptoms, as well as SUD severity (i.e., percent days using and abstinence rates) significantly more than the control group at the end of treatment (session 12).
2. Material and Methods
2.1. Participants
Participants were treatment-seeking, U.S. military veterans primarily recruited from newspaper and internet advertisements (e.g., Craigslist). Inclusion criteria included: 1) military veteran, 2) 18–65 years old, 3) met DSM-IV diagnostic criteria for current PTSD and score > 50 on the DSM-IV Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995); and 4) met DSM-IV diagnostic criteria for current SUD and endorsed alcohol or drug use in the past 90 days. Exclusion criteria included: 1) psychiatric conditions that may require a higher level of care, 2) current enrollment in another treatment for SUD or PTSD, and 3) severe cognitive impairment as evidenced by the Mini Mental Status Examination (MMSE; Folstein, Folstein, & McHugh, 1975). Psychotropic medications were required to be stabilized for four weeks prior to enrollment.
2.2. Procedures
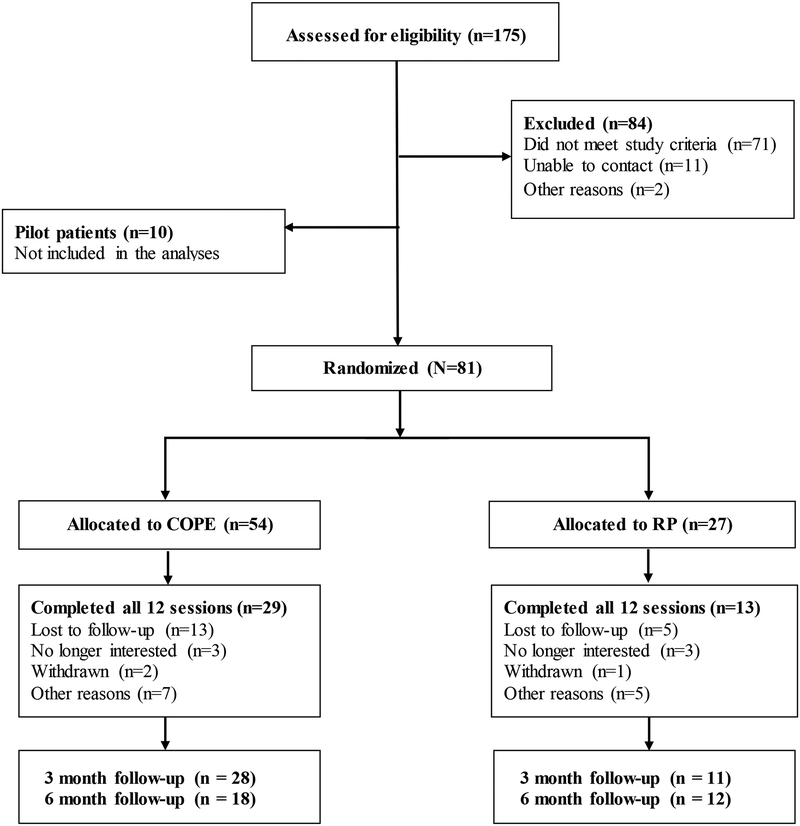
Interested individuals provided written informed consent and completed a baseline assessment. Eligible individuals were randomized (2:1) to receive 12 individual, 90-minute sessions of COPE or Relapse Prevention (RP). Twice as many participants were randomized to COPE as this was a hybrid Stage Ib/Stage II project (Rounsaville, Carroll & Onken, 2001). A biostatistician not directly involved in the study conducted the randomization. Participants were urn randomized (Wei & Lachin, 1988) and stratified to condition by SUD severity (high/low) and psychotropic medication (yes/no). RP participants were offered PTSD treatment referrals at session 12. Evaluators, blind to treatment condition, conducted assessments at baseline, week 6, week 12, and 3- and 6-months follow-up. Participants were compensated for their time and completing assessments ($60 for baseline, ~$50 for weekly assessments, $150 for follow-up visits), All study procedures were approved by the affiliated Institutional Review Board.
Treatment conditions
COPE (Back et al., 2014) employs imaginal and in vivo exposures to treat PTSD (Foa et al., 2007). Sessions 1–2 target psychoeducation about the interrelationship between SUD and PTSD, coping with cravings, substance- and trauma-related triggers, and the rationale for PE. In vivo exposures (sessions 3–12) and imaginal exposures (sessions 4–11) are key components. Abstinence is strongly encouraged, but not required to participate in COPE.
RP (Kadden et al., 1992) teaches skills to help manage cravings and high-risk situations that commonly precipitate substance use. RP was selected as the control condition because it is a manualized, evidence-based treatment often used in VA healthcare settings. The control condition in this study is, however, likely more rigorous than clinical practice in that it is protocol-driven and therapists received weekly supervision. Study therapists were instructed not to focus on PTSD or trauma-related symptoms during RP.
Treatment was provided by six masters- or doctoral-level clinicians who completed a 3-day training which covered content from both interventions. Study therapists attended weekly supervision during the trial. Completion of at least one pilot case of COPE (all 12 sessions) was required before being assigned a randomized case. COPE and RP were administered by the same clinicians to reduce potential therapist-related confounds. Sessions were videotaped and approximately 25% were randomly selected and evaluated using an adaptation of the Yale Adherence and Competence Scale (Carroll et al., 2000) that was modified to address components of the interventions used in this study. Adherence and competency ratings (0 = not at all, 1 = poor, 2 = adequate, 3 = very good, 4 = excellent) were in the “very good” range (M = 3, SD = 0.3), which is similar to prior studies. Holder et al., (2018) found that therapist fidelity rating scores in the “good” range (i.e., 5 on a scale of 1 to 7) were associated with significantly greater reductions in PTSD symptom severity than those scoring below average (< 4 on same scale). Another study found that clinicians delivering cognitive behavioral treatment for PTSD had fidelity ratings in the “good to excellent” range (i.e., 4 on a scale of 1 to 5), which met the certification criteria for achieving competence (Lu et al., 2012).
2.3. Assessments
Demographic information was collected via a self-report measure at baseline. The Life Events Checklist (Gray, Litz & Lombardo, 2004) assessed lifetime exposure to traumatic events. PTSD diagnosis and severity were evaluated using the DSM-IV CAPS, a clinical interview considered a gold standard for PTSD assessment (Blake et al., 1995). The PCL-M (Weathers, Litz, Huska & Keane, 1994), a self-report measure, was administered weekly.
DSM-IV diagnoses for SUD were evaluated using the MINI International Neuropsychiatric Interview (MINI; Sheehan et al., 1998). The Timeline Follow-back (TLFB; Sobell & Sobell, 1992), a calendar-based instrument, was administered weekly as an interview by study staff to measure substance use quantity and frequency. The Addiction Severity Index (ASI; McLellan et al., 1980) assessed alcohol and drug use severity. Breathalyzer tests measured blood alcohol concentration (BAC) before each therapy session (> 0.01 g/dl was considered positive). Urine drug screen (UDS) tests (CLIAwaived Inc.) were administered weekly to assess for the presence of cocaine, marijuana, benzodiazepines, opioids, and amphetamines.
Major depressive episode (MDE) was assessed at baseline using the MINI. The Beck Depression Inventory-II (BDI-II; Beck, Steer & Brown, 1996), a self-report measure, was administered weekly. Several items on the ASI inquire about lifetime suicidal ideation and attempts (McLellan et al., 1980). Finally, the Helping Alliance Questionnaire (HAQ-II; Luborsky et al., 1996), scaled 1–6 with higher scores reflecting a stronger perceived alliance, was administered at sessions 6 and 12.
2.4. Statistical Analyses
Baseline characteristics were compared across treatment groups using independent-samples t-tests, Fisher’s exact tests, and chi-square tests. Intent-to-treat (ITT) data included all randomized participants and all available data from those participants. Completer analyses utilized data from participants who attended all 12 sessions. Abstinence was assessed by the proportion of participants who attained abstinence 1) during the last two weeks of treatment, and 2) for three consecutive weeks at any time during treatment as measured by the TLFB (Carroll et al., 2014). These were compared across groups using chi-square test of independence and binary logistic regression to obtain odds ratios (ORs) and associated 95% confidence intervals (CIs).
Change in PTSD, SUD and depression severity as a function of treatment group was examined via a series of random intercept and slope multilevel models, utilizing robust maximum likelihood (MLR). Two-part modeling was used to examine SUD outcomes due to the presence of zero-inflated data (Olsen & Schafer, 2001). In this approach, one part of the model captures the likelihood of using (dichotomous, 0 = no use, 1 = use) and the other part captures frequency of use (e.g., percent days using).
A series of unconditional models using all data points were fit to determine whether a single linear change model or a piecewise model with separate intercepts and slopes for treatment and follow-up best approximated the data. The best-fitting unconditional models were established, and effect of treatment was examined in conditional models including group (0 = COPE, 1 = RP) and group by session interaction terms. Due to baseline differences, MDE was included as a covariate. We report unstandardized regression coefficients; estimated within-group change from baseline to session 12; estimated between-group differences at baseline, sessions 6 and 12; 95% CIs; and effect sizes as the regression coefficients standardized to the baseline SD of each outcome in the total sample (Feingold, 2009). Minimal missingness (<1%) observed for individual items on the PCL-M and BDI-II were imputed using last observation carried forward. All statistical tests were two-sided with α = 0.05.
3. Results
3.1. Baseline and clinical characteristics
Participants were mostly male with an average age of 40.4 years (see Table 1). The majority served in Operation Enduring Freedom, Operation Iraqi Freedom or Operation New Dawn (OEF/OIF/OND), with an average of 9.8 years of military service. The average number of trauma types experienced was 8.4 (SD = 2.7) and 81.0% reported a military-related index trauma (see Table 2). The average baseline CAPS score was 79.8, indicating severe to extreme PTSD symptomatology (Weathers et al., 2001). Most (90.0%) met criteria for an alcohol use disorder and 55% endorsed a treatment goal of abstinence, as compared to reduced use. At the baseline visit, all but one participant had a negative breathalyzer test and 74.1% had a negative UDS test. Among those with a positive UDS test at baseline, the most common drug detected was marijuana (55.6%) Significantly more participants in COPE met criteria for current MDE, and there were no other group differences in baseline or clinical characteristics.
Table 1.
Baseline Demographic and Clinical Characteristics by Treatment Group.
| COPE (N = 54) | RP (N = 27) | Total (N = 81) | ||||
|---|---|---|---|---|---|---|
| Characteristic | ||||||
| Mean | SD | Mean | SD | Mean | SD | |
| Age (years) | 39.7 | 11.0 | 41.9 | 10.3 | 40.4 | 10.7 |
| Education (years) | 14.0 | 2.1 | 13.8 | 1.8 | 13.9 | 2.0 |
| Average years of military service | 10.1 | 8.7 | 9.2 | 6.2 | 9.8 | 7.9 |
| N | % | N | % | N | % | |
| Sex (male) | 50 | 92.6 | 23 | 85.2 | 73 | 90.1 |
| Hispanic ethnicity | 2 | 3.7 | 1 | 3.7 | 3 | 3.7 |
| Divorced/Annulled | 21 | 38.9 | 9 | 33.3 | 30 | 37.0 |
| Student | 2 | 3.8 | 1 | 3.7 | 3 | 3.8 |
| Served in OEF/OIF/ONDa | 37 | 68.5 | 14 | 53.8 | 51 | 64.6 |
| Military-related index traumaa | 44 | 83.0 | 20 | 76.9 | 64 | 81.0 |
| Substance Use | ||||||
| Alcohol use disorder only | 33 | 61.1 | 18 | 66.7 | 51 | 63.0 |
| Alcohol and drug use disorder | 15 | 27.8 | 7 | 25.9 | 22 | 27.2 |
| Drug use disorder only | 6 | 11.1 | 2 | 7.4 | 8 | 9.9 |
| Cigarette smoker | 32 | 59.3 | 14 | 51.9 | 46 | 56.8 |
| Goal of abstinencea | 26 | 50.0 | 17 | 65.4 | 43 | 55.1 |
| History of chronic pain treatment | 35 | 64.8 | 14 | 51.9 | 49 | 60.5 |
| Psychotropic medicationa | 34 | 65.4 | 17 | 63.0 | 51 | 64.6 |
| Current major depressionb | 21 | 38.9 | 3 | 11.1 | 24 | 29.6 |
| Lifetime suicidal ideation | 26 | 48.1 | 8 | 29.6 | 34 | 42.0 |
| Lifetime suicide attempt | 16 | 29.6 | 6 | 22.2 | 22 | 27.2 |
Note. COPE=Concurrent Treatment of PTSD and Substance Use Disorders Using Prolonged Exposure; RP=Relapse Prevention; OEF=Operation Enduring Freedom; OIF=Operation Iraqi Freedom; OND=Operation New Dawn.
Some information was missing for one to three participants.
Significantly higher proportion of participants meeting criteria for current major depression in COPE group, Fisher’s exact p = .01.
Table 2.
Lifetime traumatic events and combat-related experiences
| Lifetime traumatic events | % yes(N) |
|---|---|
| Natural disaster | 63.5 (47) |
| Fire or explosion | 54.7 (41) |
| Transportation accident (e.g., car accident, train wreck) | 73.3 (55) |
| Serious accident at work, home or during recreation | 47.9 (35) |
| Exposure to toxic substances | 39.2 (29) |
| Physical assault (e.g., being attacked, hit, beaten up) | 69.7 (53) |
| Assault with a weapon (e.g., shot, stabbed, threatened with a knife, gun, bomb) | 66.7 (50) |
| Sexual assault (e.g., rape, attempted rape, made to perform sexual act through force or threat of harm) | 24.7 (18) |
| Other unwanted or uncomfortable sexual experience | 25.0 (18) |
| Combat or war-zone exposure | 82.4 (61) |
| Captivity (e.g., kidnapped, held hostage, prisoner of war) | 6.9 (5) |
| Life-threatening illness or injury | 38.2 (29) |
| Severe human suffering | 22.7 (17) |
| Sudden violent death of someone close (e.g., suicide, homicide) | 24.7 (20) |
| Sudden unexpected death of someone close | 58.1 (43) |
| Serious injury, harm or death you caused to someone | 44.4 (32) |
| Other very stressful event or experience | 44.4 (28) |
| Combat-related traumatic events during deployment | % yes(N) |
| Went on combat patrols or mission | 73.0 (54) |
| Encountered land or water mines | 58.1 (43) |
| Received hostile incoming fire (e.g., artillery, rockets, mortars, bombs) | 78.4 (58) |
| Received hostile “friendly fire” | 33.8 (25) |
| Was in vehicle (e.g., tank, helicopter, truck) that was under fire | 56.8 (42) |
| Unit was attacked by terrorists or civilians | 68.5 (50) |
| Part of land/naval artillery unit that fired on enemy | 41.9 (31) |
| Part of assault on entrenched or fortified positions | 37.8 (28) |
| Part of an invasion involving land or naval forces | 44.6 (33) |
| Unit suffered causalities from battle | 51.4 (38) |
| Witnessed someone from unit seriously wounded or killed | 60.8 (45) |
| Witnessed enemy troops being seriously wounded or killed | 62.2 (46) |
| Was wounded or injured in combat | 28.8 (21) |
| Fired weapon at the enemy | 58.1 (43) |
| Killed someone in combat | 49.3 (37) |
Note. Some events/experiences included missing values. Percentages reflect the proportion of participants completing each item who endorsed it positively.
3.2. Retention
Participants attended an average of 8 sessions [M = 8.8 for COPE (SD = 4.1) vs. 7.4 for RP (SD = 5.0); p = .21]. Over half (53.7%) completed all 12 sessions of COPE and 48.1% completed all 12 sessions of RP (p = .64). Previous studies report the percentage who attended at least 8 out of 12 sessions (Brady et al., 2001), which was 63% in this study (COPE = 66.7% vs. RP = 55.6%, p = .33). Divorced/annulled participants were more likely than married individuals to complete 12 sessions (p = .03). No other baseline differences between completers and noncompleters were observed.
3.3. PTSD diagnostic remission and severity
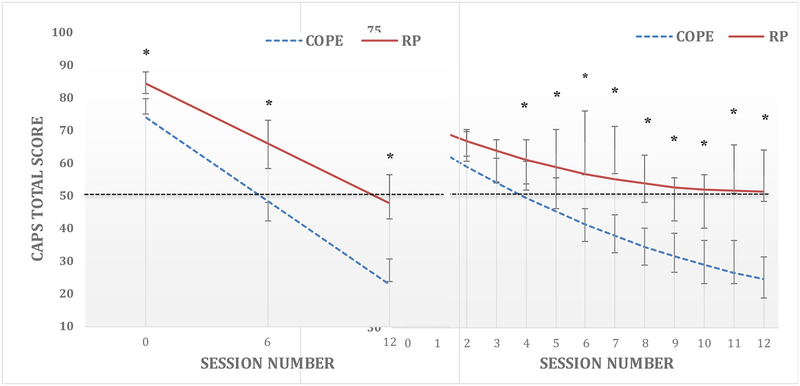
In the ITT sample, a significantly higher proportion of participants in COPE, as compared to RP, achieved diagnostic remission and no longer met criteria for PTSD [59.3% vs. 22.2%, p = .002; OR = 5.3; 95% CI (1.8, 15.7)]. Similarly, among completers, rates of PTSD diagnostic remission were significantly higher in COPE than RP [82.8% vs. 38.5%, p = .004; OR = 7.7; 95% CI (1.8, 33.6)]. PTSD severity improved in both groups (see Figure 2); however, participants in COPE improved significantly more on the CAPS [Mwithin-groupΔ = −51.2; 95% CI (−59.7, −42.8)] and PCL-M [Mwithin-groupΔ = −22.3; 95% CI (−29.3, −15.3)] than participants in RP [CAPS Mwithin-groupΔ = −35.9; 95% CI (−48.8, −23.0) and PCL-M Mwithin-groupΔ = −10.9; 95% CI (−18.0, −3.9)]. At session 12, COPE participants scored approximately 25.6 points lower on the CAPS (d = 1.4) and 13.3 points lower on the PCL-M (d = 1.3) than RP participants (see Table 5).
Figure 2.
Change in (a) Clinician Administered PTSD Scale (CAPS) and (b) PTSD Checklist-Military (PCL-M) from baseline to end of treatment by group.
Figure 2a-2b: raw mean scores, standard errors, and mean estimated effect of the treatment condition by session interaction in predicting PTSD symptoms from baseline (time 0) to session 12. Dashed lines indicate standard cut-off scores of 50 for severity and diagnostic thresholds. Asterisks indicate significant group differences (p < .05).
Table 5.
Intent-to-Treat Differences (RP - COPE) on Primary and Secondary Outcomes at Baseline, Mid-, and Posttreatment
| Measure | B [95% CI] | p | ES [95% CI] |
|---|---|---|---|
| CAPS-Total | |||
| Baseline | 10.3 [1.7, 18.9] | .02 | 0.6 [0.1, 1.0] |
| Midtreatment | 18.0 [8.6, 27.4] | < .001 | 1.0 [0.5, 1.5] |
| Posttreatment | 25.6 [11.3, 49.0] | < .001 | 1.4 [0.6, 2.2] |
| CAPS -Re- experiencing | |||
| Baseline | −0.6 [−4.1, 2.8] | .73 | −0.1 [−0.5, 0.4] |
| Midtreatment | 4.2 [0.2, 8.1] | .04 | 0.6 [0.0, 1.2] |
| Posttreatment | 8.9 [3.3, 14.6] | .00 | 1.2 [0.4, 1.9] |
| CAPS-Avoidance/Numbing | |||
| Baseline | 6.6 [2.5, 10.6] | .00 | 0.7 [0.3, 1.2] |
| Midtreatment | 11.2 [6.1, 16.2] | < .001 | 1.2 [0.7, 1.8] |
| Posttreatment | 15.8 [7.6, 24.0] | < .001 | 1.8 [0.8, 2.7] |
| CAPS-Hyperarousal | |||
| Baseline | 1.9 [−0.9, 4.8] | .19 | 0.3 [−0.3, 0.7] |
| Midtreatment | 4.6 [2.1, 7.1] | < .001 | 0.8 [0.8, 1.3] |
| Posttreatment | 7.3 [3.8, 10.9] | < .001 | 1.3 [0.7, 2.0] |
| PCL-M | |||
| Baseline | 2.0 [−3.1, 7.1] | .44 | 0.2 [−0.6, 1.3] |
| Midtreatment | 6.8 [−0.6, 14.2] | .07 | 0.7 [0.2, 1.3] |
| Posttreatment | 13.3 [4.0, 22.7] | .01 | 1.2 [0.4, 2.2] |
| PDU Any Substance | |||
| Baseline | 3.0 [−11.0, 16.9] | .68 | 0.1 [−0.3, 0.5] |
| Midtreatment | −0.9 [−13.2, 11.3] | .88 | −0.0 [−0.4, 0.3] |
| Posttreatment | −4.8 [−22.3, 12.7] | .59 | −0.1 [−0.6, 0.4] |
| PDU Alcohol | |||
| Baseline | −4.1[−18.0, 9.7] | .56 | −0.1 [−0.5, 0.3] |
| Midtreatment | −2.3 [−14.1, 9.5] | .71 | −0.1 [−0.4, 0.3] |
| Posttreatment | −0.5 [−15.7, 14.7] | .95 | −0.0 [−0.5, 0.4] |
| Drinks Per Drinking Day | |||
| Baseline | 1.8 [−0.6, 4.2] | .15 | 0.4 [−0.2, 1.0] |
| Midtreatment | 1.1 [−0.5, 2.7] | .18 | 0.3 [−0.1, 0.6] |
| Posttreatment | 0.4 [−1.3, 2.1] | .64 | 0.1 [−0.3, 0.5] |
| BDI-II | |||
| Baseline | 2.2 [−2.8, 7.3] | .38 | 0.2 [−0.2, 0.6] |
| Midtreatment | 5.1 [0.4, 9.9] | .04 | 0.4 [0.0, 0.9] |
| Posttreatment | 9.0 [2.2, 15.7] | .01 | 0.8 [0.2, 1.4] |
Note. Models are adjusted for current major depressive episode at baseline. RP = Relapse Prevention. COPE = Concurrent Treatment of PTSD and Substance Use Disorders Using Prolonged Exposure; CAPS = Clinician-Administered PTSD Scale; CI = confidence interval; PCL-M = PTSD Checklist-Military; PDU = percent days using; BDI-II = Beck Depression Index-II.
PTSD treatment gains were maintained during follow-up with only slight decay at 3-months [CAPS, Mwithin-groupΔ = 7.6 (SD = 22.3); PCL-M, Mwithin-groupΔ = 3.3 (SD = 11.2)], and 6-months follow-up [CAPS, Mwithin-groupΔ = 4.1 (SD = 33.6); PCL-M, Mwithin-groupΔ = 2.4 (SD = 12.0)], with no significant group differences.
3.4. Substance use severity
Substance use decreased significantly in both groups, with improvement occurring more rapidly early in treatment (MΔ = −29.3%, −36.5% for any substance use and alcohol use, respectively). In the ITT sample, 40.7% of participants in COPE and 25.9% in RP reported abstinence during the last two weeks of treatment. Similarly, 42.6% of participants in COPE and 25.9% in RP reported three consecutive weeks of abstinence during treatment. Among completers, the findings were slightly higher for the last two weeks of abstinence (COPE = 51.7%, RP = 38.5%) and three consecutive weeks of abstinence (COPE = 51.7%, RP = 30.8%). BAC tests were positive in approximately 1.5% of COPE and 2.5% of RP participants across treatment sessions, with no between-group differences. UDS tests were positive for any drug in approximately 16.2% of COPE and 19.1% of RP participants across all treatment sessions, which was not significantly different by group.
Reductions in substance use were generally maintained during follow-up in both groups. In comparison to end of treatment, the average number of standard drinks per drinking day was similar at 3-months [Mwithin-groupΔ = −0.09 (SD = 3.5)] and 6-months follow up [Mwithin-groupΔ = 0.5 (SD = 3.6)]. At 3-months there was a trend (p = .07) and at 6-months a significant group difference in the average number of drinks per drinking day (COPE M = 4.5 vs. RP M = 8.3, p = .05).
3.5. Therapeutic alliance
Patients rated the therapeutic alliance positively at sessions 6 (COPE M = 5.3, RP M = 5.5) and 12 (COPE M = 5.2, RP M = 5.4). Positive perceptions of therapeutic alliance were also reported by therapists at sessions 6 (COPE M = 5.0, RP M = 4.9) and 12 (COPE M = 5.2, RP = 5.0). No group differences in therapeutic alliance were observed.
3.6. Depression
Depression improved in both groups (see Table 4) with a trend toward greater improvement in COPE (p = .07) on the BDI-II [COPE, Mwithin-groupΔ = −16.0; 95% CI (−21.4, −10.6); RP, Mwithin-groupΔ = −9.4; 95% CI (−15.3, −3.6)]. At session 12, the BDI-II score was significantly lower in COPE than RP (p = .01).
Table 4.
Conditional Intent-to-Treat Models of PTSD Symptoms and Substance Use
| PTSD Symptoms | CAPS Total Score | CAPS Re-experiencing | CAPS Avoidance/Numbing | CAPS Hyperarousal | PCL-M | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | B | SE | B | SE | ||
| Intercept (Baseline) | 74.1*** | 2.7 | 21.7*** | 1.1 | 34.9*** | 1.3 | 18.0 | 0.9 | 59.7*** | 1.75 | |
| Group | 10.3* | 4.4 | −0.6 | 1.8 | 6.6** | 2.1 | 1.9 | 1.5 | 2.0 | 2.61 | |
| Session (linear) | −4.3*** | 04 | −1.4*** | 0.1 | −1.9*** | 0.2 | −0.9*** | 0.1 | −2.8*** | 0.48 | |
| Session2 (quadratic) | -- | -- | -- | -- | -- | -- | -- | -- | 0.1* | 0.03 | |
| Group by session | 1.3* | 0.6 | 0.8*** | 0.2 | 0.8* | 0.3 | 0.5** | 0.2 | 1.0* | 0.39 | |
| Substance Use | Any Substance Use | Any Alcohol Use | PDU Any Substance | PDU Alcohol | Drinks per Drinking Da | ||||||
| B | SE | B | SE | B | SE | B | SE | B | SE | ||
| Threshold/Intercept | −3.7*** | 0.9 | −3.0*** | 0.7 | 52.5*** | 5.2 | 53.0*** | 5.4 | 6.9 | 0.6 | |
| Group | 0.3 | 1.2 | 0.6 | 1.0 | 3.0 | 7.1 | −4.1 | 7.1 | 1.8 | 1.2 | |
| Session (linear) | −0.7 | 0.1 | −0.8*** | 0.1 | −4.0* | 1.4 | −4.8** | 1.2 | −0.7*** | 0.2 | |
| Session2 (quadratic) | 0.0*** | 0.0 | 0.0*** | 0.0 | 0.2* | 0.1 | 0.3** | 0.1 | 0.1*** | 0.0 | |
| Group by session | 0.0 | 0.2 | 0.1 | 0.1 | −0.7 | 0.9 | 0.3 | 0.7 | −0.1 | 0.1 | |
| Depression | BDI-II | ||||||||||
| B | SE | ||||||||||
| Intercept | 26.5*** | 1.8 | |||||||||
| Group | 2.2 | 2.6 | |||||||||
| Session (linear) | −1.3*** | 0.2 | |||||||||
| Session2 | -- | -- | |||||||||
| Group by session | 0.6† | 0.3 | |||||||||
Note. Continuous outcomes are modeled among those reporting any use. Intercepts and session slopes are adjusted for current major depressive episode at baseline. Substance/alcohol use (0 = no use, 1 = any use). Treatment condition (0 = COPE, 1 = RP). PTSD = posttraumatic stress disorder; CAPS = Clinician Administered PTSD Scale; PCL-M = PTSD Checklist-Military; PDU = percent days use; BDI-II = Beck Depression Index-II; SE = standard error.
p<.05,
p<.01,
p<.001,
p = .07.
3.7. Adverse Events
Three serious adverse events occurred during the study: 1) one COPE participant was hospitalized for suicidal ideation, 2) one RP participant made a suicide attempt, and 3) one individual who had not yet completed the baseline assessment, and therefore had not been randomized, died unexpectedly due to cardiac problems. None of these events were deemed study related.
4. Discussion
This is the first study to evaluate the efficacy of an integrated, exposure-based treatment for co-occurring SUD and PTSD among military veterans. To date, prior studies of integrated treatments for SUD/PTSD, including prior studies of COPE, have focused on non-veteran samples. In this study, the majority of participants were OEF/OIF/OND veterans with military-related traumas. The findings from this study provide critical information to help inform clinical practice guidelines regarding the treatment of comorbid SUD and PTSD, two of the most common mental health disorders afflicting our nation’s military veterans.
As hypothesized, COPE was associated with significantly greater reduction in PTSD severity and higher rates of PTSD diagnostic remission than RP. Among participants who completed COPE, 83% no longer met criteria for PTSD, and among the more conservative ITT sample, 59% of COPE participants no longer met criteria for PTSD. These outcomes are similar or higher than diagnostic remission rates observed in PTSD-only patients (no comorbid SUD) treated with cognitive behavioral therapies (Hoffman et al., 2018). Based on this and other studies examining exposure-based treatments in comorbid populations, the presence of a current SUD should not be regarded as a contraindication to receiving exposure-based treatment for PTSD (Brady et al., 2001; Foa et al., 2013; Foa et al., 2017; Mills et al., 2012; Najavits et al., 2018; Norman & Hamblen, 2017; Persson et al., 2017; Ruglass et al., 2017; Simpson et al., 2017). Although the greatest reductions in PTSD symptoms were observed in the COPE group, participants in the RP group also reported improvements in PTSD, and approximately 22% of the ITT sample who received RP no longer met criteria for PTSD. This finding is consistent with previous investigations (e.g., Simpson, Lehavot & Petrakis, 2017), and may be due, in part, to the fact that manualized RP therapy, provided by a well-trained clinician receiving weekly expert supervision can address negative emotions, cognitions and behaviors that overlap with PTSD symptoms. Although PTSD was not discussed during RP therapy sessions, the cognitive-behavioral skills learned in RP could conceivably generalize to PTSD-related symptoms.
The trauma history of participants in this study is notable. Most participants endorsed a variety of military-related and non-military related traumatic events with exposure to an average of 8 different types of traumas. Previous studies of COPE among civilians with complex trauma histories have also found substantial pre- to post-treatment reductions in SUD and PTSD. Mills and colleagues (2012) evaluated COPE among 103 outpatients in Australia who were mostly female, heroin injection drug users with childhood trauma (79%) and exposure to an average of 6 different trauma types. Mills et al. (2012) found that COPE, in comparison to treatment as usual in the community, significantly reduced PTSD symptoms and yielded comparable SUD outcomes. In a more recent, open-label study of COPE among women with alcohol use disorder and PTSD in Sweden, Persson and colleagues (2017) found that COPE led to significant reductions in both SUD and PTSD severity, despite the fact that almost all of the women (91%) reported childhood trauma and exposure to an average of 7 different trauma types. Taken together, the findings indicate that integrated, exposure-based treatment is effective in reducing SUD and PTSD severity across multiple types of traumas, including military-related events.
Contrary to our hypothesis, both treatment groups evidenced significant and comparable reductions in substance use during treatment. One possible explanation for why the COPE group did not demonstrate significantly greater reductions in SUD outcomes, as compared to the RP group, is that the COPE group received approximately half the amount of the RP intervention. That is, approximately 45 minutes of each COPE session was dedicated to substance use, while the full 90 minutes of each RP session was dedicated to substance use. Despite this, significant group differences emerged with COPE participants consuming fewer drinks per drinking day (approximately 4 fewer drinks per day) than RP participants at the final time point. On the one hand, the lack of group differences in SUD outcomes during treatment may be seen as disappointing. On the other hand, this finding may be viewed as encouraging in that a 12-session integrated SUD/PTSD treatment resulted in as much reduction in SUD severity as an evidence-based, SUD-only treatment, while also conferring the additional benefit of reducing PTSD severity. This highlights a major advantage of integrated treatments in efficiently addressing two disorders in the same amount of time. Reductions in SUD observed in the current study were similar to findings from previous studies of COPE in civilians (Mills et al., 2012; Ruglass et al., 2017) and comparable to findings observed in randomized controlled trials of SUD-only patients (Anton et al., 2006; Dutra et al., 2008). The findings from this study converge with those of previous investigations (Coffey et al., 2006; Foa et al., 2013; Mills et al., 2012; Norman et al., 2016; Peck et al., 2018; Persson et al., 2017; Ruglass et al., 2017) and show that PE delivered in the context of an integrated or comprehensive SUD treatment is beneficial, even among individuals who continue to use substances. The findings also highlight that there is room for improvement, particularly with regard to SUD outcomes, and suggest that the addition of pharmacotherapies or other interventions to further reduce craving and substance use may be benefit some patients with SUD/PTSD.
Participants in this study completed an average of 8 therapy sessions, with no difference by treatment condition; this highlights that the addition of exposure-based trauma work does not lead to increased dropout. The majority of available COPE sessions (73.7%) and RP sessions (61.7%) were attended. Completion rates and attendance in this study were similar to or higher than previous studies of non-exposure based, integrated treatments (Hien et al., 2009; Myers, Browne, & Norman, 2015; Najavits et al., 2018) as well as exposure-based, integrated treatments (Coffey et al., 2016; Foa et al., 2013; Mills et al., 2012; Peck et al., 2018; Ruglass et al., 2017; Schacht et al., 2017). Improvements in retention observed in the current study may be due, in part, to modifications made to the treatment protocol. Most notably, the current version of the COPE therapy manual (Back et al., 2014), which was utilized in this study, initiates in vivo and imaginal exposures earlier in treatment (sessions 3 and 4, respectively), which is earlier than exposures were initiated in previous studies (e.g., Brady et al., 2001; Mills et al., 2012). The higher retention may also be due to the study sample which consisted of military veterans who often receive multiple services at the VA hospital (e.g., primary care, housing, occupational assistance), which allows research staff to schedule study visits around veterans’ other VA appointments. In addition, transportation problems are mitigated in this population, as veterans may be reimbursed by the VA for transportation costs to and from appointments, or offered transportation via a VA shuttle bus. Nonetheless, there remains significant room for improving retention in this population, as 54% of the COPE group and 48% of the RP group attended all 12 sessions of treatment. Retention of patients with either PTSD or SUD, conditions frequently characterized by avoidance coping, is challenging and it becomes even more challenging when both conditions are present (Zandberg et al., 2016a). Previous examination of dropout from COPE reveals that the highest probability of dropout occurs between sessions 9 and 10 (Szafranski et al., 2017b), and that a substantial proportion of individuals (40%−68%) who drop out before completing all 12 sessions evidence clinically significant improvement and/or met good end-state functioning with regard to SUD, PTSD, and depression prior to dropping out (Szanfranski et al., in press). Thus, it may not always be the case that dropout is due to a worsening or lack of symptom improvement (Szafranski et al., 2017a; Zanberg et al., 2016a), and more research in this area is needed.
Several limitations warrant consideration. The sample size was small, which may have underpowered the analyses. Although the percentage of women in the study is representative of women in the U.S. military service (Department of Defense, 2015), the small number of women limited our ability to evaluate gender differences. Despite these limitations, this study is the first to examine COPE in a military population and has several key strengths including the use of a randomized between-groups experimental design, comparison of two evidence-based treatments matched on time and therapeutic attention, intent-to-treat design, validated assessments, and inclusion of a substantial proportion of minority individuals (37% African American). Furthermore, minimal exclusion criteria were used and the sample is representative of real-world practice.
In summary, in this sample of veterans with extensive military-related trauma, COPE resulted in significantly greater reductions in PTSD severity, higher rates of PTSD diagnostic remission, and comparable reductions in SUD, as compared to RP. Importantly, there were no treatment group differences in measures of therapeutic alliance, retention, or number of adverse events. In conjunction with a growing body of literature on integrated treatments for SUD/PTSD, the findings raise important questions for clinical practice and future research in VA healthcare settings. First, it is recommended that all veterans with SUD be assessed for trauma exposure and PTSD. Veterans with both SUD and PTSD should be offered integrated, exposure-based treatment to address both conditions concurrently. Veterans wishing to receive integrated treatment should initiate treatment promptly; PTSD treatment should not be delayed until abstinence has been achieved. Although abstinence is the safest option, a significant proportion of veterans with SUD/PTSD do not endorse a goal of abstinence (Lozano et al., 2015) and PTSD treatment should not be delayed because of this. Future research is needed to identify ways to further increase treatment retention and reduce substance use in order to yield long-term positive outcomes in both SUD and PTSD.
Figure 1.
Flow of participants through the study.
Table 3.
Raw Scores on Primary and Secondary Outcomes by Treatment Groupa
| COPE | RP | ||||||
|---|---|---|---|---|---|---|---|
| Measure | n | SD | n | SD | |||
| CAPS Totalb | |||||||
| Baseline | 54 | 18.1 | 27 | 17.8 | |||
| Midtreatment | 41 | 18.5 | 15 | 28.6 | |||
| Posttreatment | 30 | 19.4 | 14 | 25.3 | |||
| CAPS Re-experiencing | |||||||
| Baseline | 54 | 7.6 | 27 | 7.7 | |||
| Midtreatment | 41 | 6.5 | 15 | 10.3 | |||
| Posttreatment | 30 | 7.1 | 14 | 10.7 | |||
| CAPS Avoidance/Numbing | |||||||
| Baseline | 54 | 9.1 | 27 | 7.1 | |||
| Midtreatment | 41 | 9.4 | 15 | 13.9 | |||
| Posttreatment | 30 | 9.7 | 14 | 13.4 | |||
| CAPS Hyperarousal | |||||||
| Baseline | 54 | 6.0 | 27 | 5.8 | |||
| Midtreatment | 41 | 8.0 | 15 | 7.4 | |||
| Posttreatment | 30 | 8.2 | 14 | 6.0 | |||
| PCL-M Totalb | |||||||
| Baseline | 54 | 11.0 | 27 | 8.9 | |||
| Midtreatment | 41 | 15.6 | 15 | 18.5 | |||
| Posttreatment | 30 | 17.2 | 14 | 14.5 | |||
| PDU Any Substancec | |||||||
| Baseline | 48 | 33.7 | 25 | 32.2 | |||
| Midtreatment | 25 | 26.2 | 10 | 26.1 | |||
| Posttreatment | 14 | 26.7 | 9 | 36.2 | |||
| PDU Any Alcoholc | |||||||
| Baseline | 44 | 30.4 | 25 | 31.5 | |||
| Midtreatment | 23 | 24.7 | 9 | 17.8 | |||
| Posttreatment | 14 | 22.8 | 9 | 36.0 | |||
| Drinks Per Drinking Dayc | |||||||
| Baseline | 44 | 7.0 | 25 | 6.7 | |||
| Midtreatment | 23 | 3.5 | 9 | 3.3 | |||
| Posttreatment | 14 | 3.6 | 9 | 4.1 | |||
| BDI-IId | |||||||
| Baseline | 54 | 12.3 | 25 | 9.7 | |||
| Midtreatment | 41 | 11.7 | 15 | 13.7 | |||
| Posttreatment | 30 | 11.0 | 14 | 12.3 | |||
| ASI - Alcohol Composite | |||||||
| Baseline | 54 | 0.26 | 27 | 0.29 | |||
| Midtreatment | 39 | 0.19 | 15 | 0.28 | |||
| Posttreatment | 29 | 0.18 | 14 | 0.17 | |||
| ASI - Drug Composite | |||||||
| Baseline | 54 | 0.06 | 27 | 0.12 | |||
| Midtreatment | 39 | 0.07 | 15 | 0.09 | |||
| Posttreatment | 29 | 0.04 | 14 | 0.06 | |||
| ASI - Psychiatric Composite | |||||||
| Baseline | 54 | 0.22 | 27 | 0.15 | |||
| Midtreatment | 39 | 0.17 | 15 | 0.74 | |||
| Posttreatment | 29 | 0.21 | 14 | 0.22 | |||
Note. COPE=Concurrent Treatment of PTSD and Substance Use Disorders Using Prolonged Exposure; RP=Relapse Prevention; CAPS=Clinician-Administered PTSD Scale; PCL-M=PTSD Checklist-Military; PDU=percent days using; BDI-II=Beck Depression Inventory-II; ASI=Addiction Severity Index.
Posttreatment ns include participants who did not complete all 12 sessions but completed assessments.
Diagnositc cut off for the DSM-IV CAPS and PCL total scores = 50.
Among participants reporting substance use during period covered by a given assessment.
Data is missing on baseline scores for two participants.
Highlights.
Posttraumatic stress disorder (PTSD) is common among individuals with addiction.
Rates of PTSD and addiction are particularly high among military veterans.
This study tested an integrated treatment for both disorders in military veterans.
The treatment included Prolonged Exposure (PE) for PTSD.
The treatment was effective and significantly reduced PTSD and substance use severity.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anton R, O’Malley S, Ciraulo D Cisler R, Couper D, Donovan D,…Zweben A (2006). Combined pharmacotherapies and behavioral interventions for alcohol dependence. The COMBINE study: A randomized controlled trial. JAMA, 295, 2003–2017. [DOI] [PubMed] [Google Scholar]
- Back S, Foa E, Killeen T, Mills K, Teeson M, Carroll K,…Brady K (2014). Concurrent treatment of PTSD and substance use disorders using prolonged exposure (COPE) Therapist Manual. New York, NY: Oxford University Press. [Google Scholar]
- Back SE, & Jones JL (2018). Alcohol Use Disorder and Posttraumatic Stress Disorder: An Introduction. Alcohol Clin Exp Res, 42(5), 836–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Back S,Killeen TE, Teer A, Hartwell E, Federline A, Beylotte F, & Cox E (2014). Substance use disorders and PTSD: An exploratory study of treatment preferences among military veterans. Addict Behav, 39, 369–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett E, Teeson M, & Mills K (2014). Associations between substance use, post-traumatic stress disorder and the perpetration of violence: A longitudinal investigation. Addict Behav, 39, 1075–1080. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory (2nd ed.). San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Blake D, Weathers F, Nagy L, Kaloupek D, Gusman F, Charney D,…Keane T (1995). The development of a Clinician-Administered PTSD Scale. J Trauma Stress, 8, 75–90. [DOI] [PubMed] [Google Scholar]
- Brady K, Dansky B, Back S, & Foa E, Carroll K (2001). Exposure therapy in the treatment of PTSD among cocaine-dependent individuals: Preliminary findings. J Subst Abuse Treat, 21, 47–54. [DOI] [PubMed] [Google Scholar]
- Carey K (1997). Reliability and validity of the time-line follow-back interview among psychiatric outpatients: A preliminary report. Psychol Addict Behav, 11, 26–33. [Google Scholar]
- Carroll K, Kiluk B, Nich C, DeVito E, Decker S, LaPaglia D, Duffey D, Babuscio T, & Ball S (2014). Toward empirical identification of a clinically meaningful indicator of treatment outcome: Features of candidate indicators and evaluation of sensitivity to treatment effects and relationship to one year follow up cocaine use outcomes. Drug Alcohol Depend, 137, 3–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll K, Nich C, Sifry R, Nuro K, Frankforter T, Ball S, Fenton L, Rounsaville B (2000). A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug Alcohol Depend, 57, 225–238. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Schumacher JA, Nosen E, Littlefield AK, Henslee AM, Lappen A, & Stasiewicz PR (2016). Trauma-focused exposure therapy for chronic posttraumatic stress disorder in alcohol and drug dependent patients: A randomized controlled trial. Psychol Addict Behav, 30(7), 778–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey S, Stasiewicz P, Hughes P.l, & Brimo M (2006). Trauma-focused imaginal exposure for individuals with comorbid posttraumatic stress disorder and alcohol dependence: Revealing mechanisms of alcohol craving in a cue reactivity paradigm. Psychol Addict Behav, 20, 425–435. [DOI] [PubMed] [Google Scholar]
- Department of Defense (DoD), Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy (September 2015). 2015 Demographics: Profile of the Military Community. http://download.militaryonesource.mil/12038/MOS/Reports/2015-Demographics-Report.pdf
- Dutra L, Stathopoulou G, Basden S, Leyro T, Powers M, & Otto M (2008). A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry, 165, 179–187. [DOI] [PubMed] [Google Scholar]
- Feingold A (2009). Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychol Methods, 14, 43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa E, Asnaani A, Rosenfield D, Zandberg L, Gariti P, & Imms P (2017). Concurrent varenicline and prolonged exposure for patients with nicotine dependence and PTSD: A randomized controlled trial. J Consult Clin Psychol, 85, 862–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa E, Hembree E, & Rothbaum B (2007). Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences therapist guide. Oxford University Press. [Google Scholar]
- Foa E, Yusko D, McLean C, Suvak M, Bux D, Oslin D,…Volpicelli J (2013). Concurrent naltrexone and prolonged exposure therapy for patients with comorbid alcohol dependence and PTSD: A randomized clinical trial. JAMA, 7, 488–495. [DOI] [PubMed] [Google Scholar]
- Folstein M, Folstein S, & McHugh P (1975). “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res, 12,189–198. [DOI] [PubMed] [Google Scholar]
- Grant B, Goldstein R, Saha T, Chou S, Jung J, Zhang H,…Hasin D (2015). Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry, 72, 757–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray M, Litz B, Hsu J, & Lombardo T (2004). Psychometric properties of the Life Events Checklist. Assessment, 11, 330–341. [DOI] [PubMed] [Google Scholar]
- Hien D, Wells E, Jiang H, Suarez-Morales L, Campebell A, Cohen L,…Nunes E (2009). Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. J Consult Clin Psychol, 77, 607–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge C (2015). Measuring the long-term impact of war-zone military service across generations and changing posttraumatic stress disorder definitions. JAMA Psychiatry, 72, 861–862. [DOI] [PubMed] [Google Scholar]
- Hoffman V, Middleton JC, Feltner C, Gaynes BN, Weber RP, Bann C, Viswanathan M, Lohr KN, Baker C, & Green J (2018). Psychological and pharmacological treatments for adults with postrraumatic stress disoder: A systematic review update. Comparative Effectivness Review No. 207. AHRQ Publication No 18-EHC011-EF. PCORI Publication No. 2018-SR-01. Rockville, MD: Agency for Healthcare Research and Quality. [PubMed] [Google Scholar]
- Kadden R, Carroll K, Donovan D, Cooney N, Monti P, Abrams D,…Hester R (1992). Cognitive–behavioral coping skills therapy manual. National Institute on Alcohol Abuse and Alcoholism, Rockville, MD. [Google Scholar]
- Kilpatrick D, Resnick H, Milanak M, Miller M, Keyes K, & Friedman M (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress, 26, 537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeman R, Hefner K, Frohe T, Murray A, Rosenheck R, Watts B, & Sofuoglu M (2017). Exclusion of participants based on substance use status: Findings from randomized controlled trials of treatments for PTSD. Behav Res Ther, 89, 33–40. [DOI] [PubMed] [Google Scholar]
- Lozano B, Gros D, Killeen T, Jaconis M, Beylotte F, Boyd S, & Back S (2015). To reduce or abstain? Substance use goals in the treatment of veterans with substance use disorders and comorbid PTSD. Am J Addict, 24, 578–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W, Yanos PT, Gottlieb JD, Duva SM, Silverstein SM, Xie H, … Mueser KT (2012). Use of fidelity assessments to train clinicians in the CBT for PTSD program for clients with serious mental illness. Psychiatric Services, 63(8), 785–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luborsky L, Barber J, Siqueland L, Johnson S, Najavits L, Frank A, & Daley D (1996). The revised Helping Alliance Questionnaire (HAq-II). J Psychother Pract Res, 5, 260–271. [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, & O’Brien CP (1980). An improved diagnostic evaluation instrument for substance abuse patients. The Addiction Severity Index. Journal of Nervous and Mental Disorders, 168 (1), 26–33. [DOI] [PubMed] [Google Scholar]
- Mills K, Teesson M, Back S, Brady K, Baker A, Hopwood S,…Ewer P (2012). Integrated exposure-based therapy for co-occurring posttraumatic stress disorder and substance dependence: a randomized controlled trial. JAMA, 308, 690–699. [DOI] [PubMed] [Google Scholar]
- Mills K, Teeson M, Ross J, & Peters L (2006). Trauma, PTSD, and substance use disorders: Findings from the Australian National Survey of Mental Health and Well-Being. Am J Psychiatry, 163, 652–658. [DOI] [PubMed] [Google Scholar]
- Myers U, Browne K, & Norman S (2015). Treatment engagement: Female survivors of intimate partner violence in treatment for PTSD and alcohol use disorder. J Dual Diagn, 11, 238–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najavits LM, Krinsley K, Waring ME, Gallagher MW, & Skidmore C (2018). A Randomized Controlled Trial for Veterans with PTSD and Substance Use Disorder: Creating Change versus Seeking Safety. Subst Use Misuse, 1–13. [DOI] [PubMed] [Google Scholar]
- Norman S, Davis B, Colvonen P, Haller M, Myers U, Trim R,…Robinson S (2016). Prolonged exposure with veterans in a residential substance use treatment program. Cogn Behav Pract, 23, 162–172. [Google Scholar]
- Norman S, & Hamblen J (2017). Promising directions for treating comorbid PTSD and substance use disorder. ACER, 41, 706–710. [DOI] [PubMed] [Google Scholar]
- Olsen M, & Schafer J (2001). A two-part random-effects model for semicontinuous longitudinal data. J Am Stat Assoc, 96, 730–45. [Google Scholar]
- Peck KR, Schumacher JA, Stasiewicz PR, & Coffey SF (2018). Adults with Comorbid Posttraumatic Stress Disorder, Alcohol Use Disorder, and Opioid Use Disorder: The Effectiveness of Modified Prolonged Exposure. J Trauma Stress, 31(3), 373–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persson A, Back S, Killen T, Brady K, Schwandt M, Heilig M, & Magnusson A (2017). Concurrent treatment of PTSD and substance use disorders using prolonged exposure (COPE): A pilot study in alcohol-dependent women. J Addict Med, 11, 119–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrakis I, Rosenheck R, & Desai R (2011). Substance use comorbidity among veterans with posttraumatic stress disorder and other psychiatric illness. Am J Addict, 20, 185–189. [DOI] [PubMed] [Google Scholar]
- Resick P, Williams L, Suvak M, Monson C, & Gradus J (2012). Long-term outcomes of cognitive-behavioral treatments for posttraumatic stress disorder among female rape survivors. J Consult Clin Psychol, 80, 201–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts N, Roberts P, Jones N, & Bisson J (2015). Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: A systematic review and meta-analysis. Clin Psychol Review, 38, 25–38. [DOI] [PubMed] [Google Scholar]
- Rounsaville B, Carroll K, & Onken L (2006). A stage model of behavioral therap ies research: Gettign started and moving on from stage 1. Clin Psychol Sci Pract, 8, 133–142. [Google Scholar]
- Ruglass L, Lopez-Castro T, Papini S, Killeen T, Back S, & Hien D (2017). Concurrent treatment with prolonged exposure for co-occurring full or subthreshold posttraumatic stress disorder and substance use disorders: A randomized clinical trial. Psychother Psychosom, 86, 150–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schacht R, Brooner R, King V, Kidorf M, & Peirce J (2017). Incentivizing attendence to prolonged exposure for PTSD in opioid use disorder patients: A randomized controlled trial. J Consult Clin Psychol, 85, 689–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan D, Lecrubier Y, Sheehan K, Amorim P, Janavs J, Weiller E,…, Dunbar G (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry, 59, 22–33. [PubMed] [Google Scholar]
- Simpson T, Lehavot K, & Petrakis I (2017). No wrong doors: Findings from a critical review of behavioral randomized clinical trials for individuals with co-occurring alcohol/drug problems and PTSD. ACER, 41, 681–702. [DOI] [PubMed] [Google Scholar]
- Sobell L, & Sobell M (1992). Timeline follow-back: A technique for assessing self-report ethanol consumption In Allen J & Litten R (Eds.), Measuring alcohol consumption: Psychosocial and biological mehtods (pp. 41–72). Totowa, NJ: Humana Press. [Google Scholar]
- Stein M, Campbell-Sills L, Gelernter J, He F, Heeringa S, Nock M,…Ursano R (2017). Alcohol misuse and co-occurring mental disorders among new soldiers in the U.S. army. ACER, 41, 139–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szafranski DD, Gros D, Acierno R, Brady K Killeen T, & Back S (in press). Heterogeneity of treatment dropout: PTSD, depression and alcohol use disorder reductions in PTSD and AUD/SUD treatment non-completers. Clinical Psychology and Psychotherapy. [DOI] [PubMed] [Google Scholar]
- Szafranski DD, Smith BN, Gros DF, & Resick PA (2017a). High rates of PTSD treatment dropout: A possible red herring? Journal of Anxiety Disorders, 47, 91–98. [DOI] [PubMed] [Google Scholar]
- Szafranski DD, Snead A, Allan NP, Gros DF, Killeen T, Flanagan J, Pericot-Valverde I, & Back SE (2017b). Integrated, exposure-based treatment for PTSD and comorbid substance use disorders: Predictors of treatment dropout. Addictive Behaviors, 73, 30–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeters JB, Lancaster CL, Brown DG, & Back SE (2017). Substance use disorders in military veterans: prevalence and treatment challenges. Subst Abuse Rehabil, 8, 69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F, Litz B, Huska J, & Keane T (1994). PTSD Checklist-Military (PCL-M) for DSM-IV. Boston: National Center for PTSD, Behavioral Science Division. [Google Scholar]
- Wei L, & Lachin J (1988). Properties of the urn randomization in clinical trials. Control Clin Trials, 9, 345–364. [DOI] [PubMed] [Google Scholar]
- Zandberg L, Rosenfield D, Alpert E, McLean CP & Foa EB (2016a). Predictors of dropout in concurrent treatment of posttraumatic stress disorder and acohol dependence: Rate of improvement matters. Behavior Research and Therapy, 80,1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandberg L, Rosenfield D, McLean C, Power M, Asnaani A, & Foa E (2016b). Concurrent treatment of posttraumatic stress disorder and acohol dependence: Predictors and moderators of outcome. J Consult Clin Psychol, 84, 43–56. [DOI] [PMC free article] [PubMed] [Google Scholar]