Abstract
Background:
People experiencing homelessness are disproportionately affected by alcohol use disorder (AUD). Abstinence-based treatment, however, does not optimally engage or treat this population. Thus, Harm Reduction Treatment for Alcohol (HaRT-A) was developed together with people with lived experience of homelessness and AUD and community-based agencies that serve them. HaRT-A is a compassionate and pragmatic approach that aims to help people reduce alcohol-related harm and improve quality of life (QoL) without requiring abstinence or use reduction. A three-month, two-arm randomized controlled trial was conducted to test the initial efficacy of HaRT-A compared to a services-as-usual control condition.
Methods:
People experiencing homelessness and AUD (N = 168; 24% women) were recruited in community-based clinical and social services settings. Self-reported alcohol use, alcohol-related harm, motivation, and QoL as well as urinary ethyl glucuronide were assessed over a 3-month follow-up. Participants were randomized to receive HaRT- or services as usual. Over four sessions, HaRT-A interventionists delivered three components: a) collaborative tracking of participant-preferred alcohol metrics, b) elicitation of harm-reduction and QoL goals, and c) discussion of safer-drinking strategies.
Results:
Compared to control participants, HaRT-A participants reported significantly greater increases in confidence to engage in harm reduction and decreases in peak alcohol use, alcohol- related harm, AUD symptoms, and positive urinary ethyl glucuronide tests (ps < .05). Findings were inconclusive regarding group differences on QoL (ps > .12).
Conclusion:
A low-barrier, low-intensity, patient-driven, harm-reduction approach has at least short-term efficacy in improving AUD outcomes in this population. Future studies are needed to establish its longer-term efficacy.
Keywords: drinking, alcohol-related harm, alcohol treatment, harm reduction, homelessness, quality of life
Based on 2017 estimates, 549,928 people in the US are homeless on any given night (US Department of Housing and Urban Development, 2017), and over 1.4 million people – or 1 in 230 Americans – spent at least one night in a shelter in 2017 (US Department of Housing and Urban Development, 2018). The homeless population is disproportionately affected by medical, psychiatric, and substance-use problems (Fazel,Geddes,&Kushel,2014;Greenberg & Rosenheck, 2010; Krausz et al., 2013), among which alcohol use disorder (AUD) is one of the most prevalent and physically debilitating. A US population-based study indicated that about 40% of homeless people meet criteria for AUD (North, Eyrich-Garg, Pollio, & Thirthalli, 2010), which is over 7 times higher than the prevalence of AUD in the general population (Center for Behavioral Health Statistics and Quality, 2016). This disproportionate impact of AUD is associated with correspondingly high levels of alcohol-related mortality: People experiencing homelessness die of alcohol-attributable causes at rates 6 to 10 times higher than the general population in North American samples (Baggett et al., 2015; Hwang, Wilkins, Tjepkema, O’Campo,&Dunn,2009).
Existing Treatments Do Not Optimally Engage this Population
AUD treatment can be a part of a positive solution for this issue moving forward. In fact, one large-scale epidemiological study indicated that increasing treatment coverage to 40% of all people with severe AUD could substantially reduce alcohol-attributable mortality (Rehm, Shield, Gmel, Rehm, & Frick, 2013). he cornerstone of existing AUD treatment, particularly for more severely affected populations (NIAAA, 2005; Willenbring, 2014), is abstinence. Although studies suggest that abstinence-based treatments for homeless people are associated with modest improvements in alcohol outcomes (Hwang, Tolomiczenko, Kouyoumdjian, & Garner, 2006; Smith, Meyers, & Delaney, 1998; Zerger, 2002), these improvements are only experienced by the few who are engaged and retained in treatment (Zerger, 2002). The few studies addressing the topic show that a minority of homeless people start treatment (15–28%; Rosenheck et al., 1998; Wenzel et al., 2001), and even fewer complete it (2.5–33%; Orwin, Garrison-Mogren, Jacobs, & Sonnefeld, 1999). An NIAAA review of substance use treatment programs in the US showed that treatment engagement in this population decreased as program demands—particularly abstinence from substances—increased (Orwin et al., 1999).
Harm-reduction Approaches Are Preferred by and Are Promising for People experiencing homelessness and AUD
Harm-reduction approaches are a diverse set of compassionate and pragmatic strategies applied on policy, population, community or individual levels that aim to minimize substance-related harm and enhance quality of life (QoL) without requiring or advising abstinence or use reduction (Collins et al., 2011; Marlatt & Witkiewitz, 2010). In the homeless population, community-level harm-reduction approaches, such as low-barrier, nonabstinence-based housing or shelter paired with harm-reduction service provision, are associated with improved alcohol outcomes (Collins, Malone, et al., 2012; Larimer et al., 2009; Podymow, Turnbull, Coyle, Yetisir, & Wells, 2006; Stockwell et al., 2017; Vallance et al., 2016). Further, members of this population have expressed a preference for approaches that value their autonomy and priorities over alcohol abstinence (Collins, Clifasefi, et al., 2012; Collins et al., 2016). It thus stands to reason that harm-reduction approaches applied at the individual level could be similarly engaging and effective.
Under the larger harm-reduction umbrella, harm-reduction treatment is individual-level behavioral counseling that entails accepting people “where they’re at” while helping them make informed decisions to reduce their substance-related harm and improve their quality of life (Collins et al., 2011). It assumes an ecological systems framework (Bronfenbrenner, 1979), which holds that substance use is not only influenced by individual-level factors, but also larger familial, community, and even geopolitical factors. Given its stance that substance use disorder does not reside solely within the individual, harm-reduction treatment avoids pathologizing or placing moral value on substance use (Denning & Little, 2012).
There has been some disagreement about what differentiates harm-reduction treatment from other approaches (Heather, 2006). It is, however, the primary therapeutic intention—harm reduction versus use reduction or abstinence—that provides the clearest point of differentiation (Collins et al., 2011; Heather, 2006). Second, even in its name, the therapeutic intention of harm reduction is transparent and explicit, whereas the abstinence or use-reduction treatment goal is often assumed or implied in most other approaches. Finally, harm-reduction treatment is less directive in its style than most alcohol treatments in practice, which typically utilize different strategies to engage people with AUDs with a predetermined goal (i.e., abstinence or use reduction). While the name does convey its agenda, harm reduction is more broadly construed and thus can easily and must necessarily accommodate nearly any client-driven goal that can reduce substance-related harm (e.g., reduced blackouts, avoiding withdrawal, abstinence) and/or improve QoL (e.g., reconnecting with family, making art, going to the library) within a person’s own context (Collins, Grazioli, et al., 2015).
Harm-reduction approaches applied on the individual level have garnered an evidence base for other substance use disorders (e.g., opioids; Des Jarlais, Feelemyer, Modi, Abdul-Quader, & Hagan, 2013; Mattick, Breen, Kimber, & Davoli, 2014; Nielsen et al., 2016), and for risky drinking in nonclinical populations (e.g., college drinkers; Marlatt et al., 1998; Pearson, 2013). Best practices, however, still indicate abstinence as the recommended goal and desired outcome for people with AUD (NIAAA, 2005; Willenbring, 2014), and abstinence is the required focus of most publicly funded AUD treatment in the US (e.g., according to Washington state law where the current study was conducted; “Washington State Counselor Credentialing Standards,” 2008). Perhaps for these reasons, no studies to date have tested the efficacy of AUD treatment focusing explicitly on harm reduction.
Harm-Reduction Treatment for Alcohol (HaRT-A)
In this study, we tested the 3-month efficacy of harm-reduction treatment for alcohol (HaRT-A) in nontreatment-seeking people experiencing homelessness and AUD. HaRT-A was developed using a three-phase community-based participatory research approach ( BPR). CBPR is a public health research paradigm that strives to equitably involve affected community members in research planning, implementation and evaluation (Minkler & Wallerstein, 2008). CBPR is well-positioned for developing treatments that take communities’ needs into account, fit into more accessible community-based settings, and engender positive behavior change on participants’ own terms (Collins et al., 2018).
In the first phase, 50 people with lived experience of homelessness and AUD were interviewed to understand their perspectives on available and, de facto, abstinence-based treatments as well as their suggestions for improving treatment (Collins et al., 2016). These findings indicated preferences for participant-driven, nonjudgmental, nonabstinence-based approaches that emphasize engagement in meaningful activities, personal goal-setting, and discussions of ways to stay safer and healthier, even when using substances. Participants were not interested in currently available abstinence-based treatment or treatment in which the primary focus was on alcohol behavior change (Collins et al., 2016). These findings echoed those of our prior qualitative studies with people with lived experience of homelessness and AUD regarding their preferences on programming content and treatment goals (i.e., 95% preferred nonabstinence-based goals) (Clifasefi, Collins, Torres, Grazioli, & Mackelprang, 2016; Collins, Clifasefi, et al., 2012; Collins, Grazioli, et al., 2015).
In the second phase, a community advisory board, which comprised people with lived experience of homelessness and AUD and the staff and management who serve them, was engaged to cocreate the treatment based on the phase 1findings.Theresultingtreatmententailed a community-driven and pragmatic mindset that stemmed from the harm-reduction philosophy and tradition. For example, HaRT-A entails no abstinence requirements, a low number of expected treatment contacts, community-based treatment provision, and participant-driven goal-setting. HaRT-A also entails a compassionate heartset, founded in the spirit, processes and communication skills of motivational interviewing (Miller & Rollnick, 2012). For example, HaRT-A interventionists used only strengths-based reflections and affirmations and avoided advice-giving or judgment about alcohol use (Miller & Rollnick, 2012). Specific treatment components included a) collaborative tracking of participant-preferred alcohol metrics, b) elicitation of harm-reduction and QoL goals, and c) discussion of safer-drinking strategies (see Appendix A for treatment manual).
In the third phase, we conducted a 2-arm randomized controlled trial to test HaRT-A’s initial efficacy. In a priori, directional hypotheses, we expected that, compared to participants in a services-as-usual control condition, HaRT-A participants would evince reduced peak alcohol quantity, drinking to intoxication, number of endorsed AUD symptoms, and alcohol-related harm as well as increased motivation for alcohol harm reduction and improved QoL. To place HaRT-A efficacy in the context of the larger alcohol research literature and typical clinical practice, we conducted exploratory analyses testing HaRT-A effects on more conventional abstinence-oriented outcomes, including a biological outcome (i.e., urinary ethyl glucuronide [EtG] < 500ng/ml) and self-reported abstinence.
Methods
Participants
Participants were 169 people experiencing homelessness and AUD who were recruited from three community-based healthcare and social service agencies in Seattle, Washington. The proposed sample size (N = 160) was determined using a priori power analyses but was exceeded during recruitment. Inclusion criteria comprised a) being at least 21 years of age, b) being homeless as defined by the McKinney-Vento Act (“The McKinney-Vento Homeless Assistance Act,” 2009) for at least 6 of the last 12 months, and c) meeting AUD criteria. Exclusion criteria were refusal or inability to consent to participation and constituting a risk to the safety and security of other clients or staff. Additionally, we excluded from analyses one individual who, due to administrative errors, received the treatment and subsequent follow-up assessments far outside of the time window stipulated by the protocol (see Figure 1 for participant flowchart).
Figure 1.
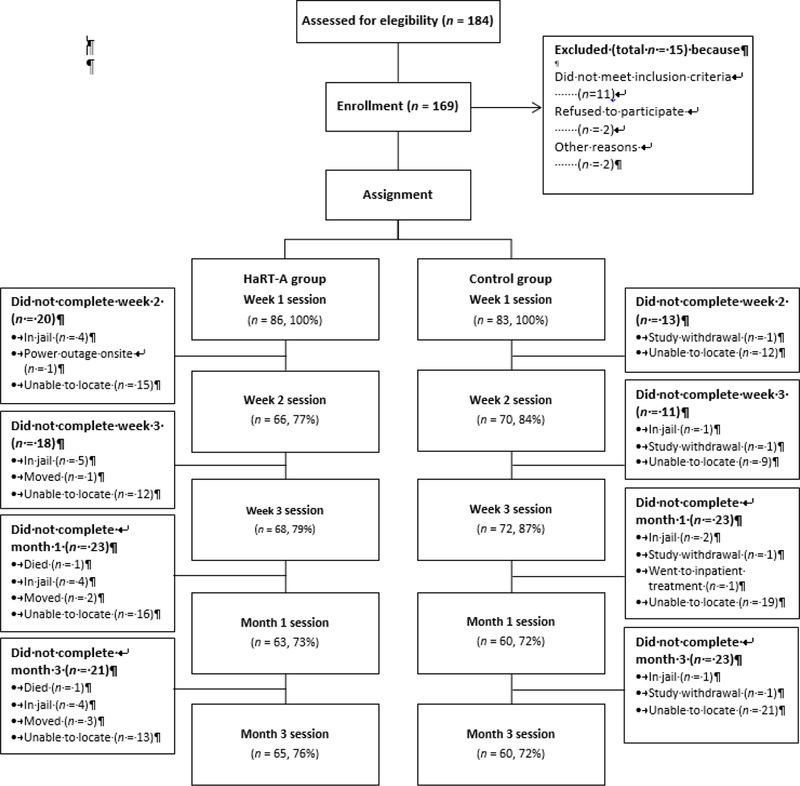
Participant flowchart.
Measures
Sociodemographic questions assessed age, sex assigned at birth, race, ethnicity, current housing status, and substance-use treatment and mutual-help group attendance.
Motivation to change was measured using three, 10-point “readiness rulers” (Center for Substance Abuse Treatment, 1999), which assessed participants’ readiness for, confidence about, and perception of the importance of changing drinking behavior to reduce its “negative side effects,” where 0 = not at all ready/confident/important and 10 = totally ready/confident/ important. Readiness rulers have been shown to be associated with alcohol outcomes and have evinced adequate psychometric properties (Bertholet, Gaume, Faouzi, Daeppen, & Gmel, 2012; Heather, Smailes, & Cassidy, 2008; LaBrie, Shiffman, & Earleywine, 2005; Maisto et al., 2011).
The Alcohol Quantity and Use Assessment (AQUA) is an open-ended, single-item, self-report measure of alcohol quantity (Collins, Duncan, et al., 2015; Collins, Malone, et al., 2012; Collins et al., 2014; Larimer et al., 2009) that was used together with the Blood Alcohol Concentration Calculation System (BACCUS; Markam, Miller, & Arciniega, 1993) to record the number of standard drinks consumed on participants’ heaviest drinking day (peak alcohol use) in the past 2 weeks.
Frequency of alcohol use was assessed using the psychometrically sound Addiction Severity Index – 5th Edition (McLellan, Kushner, Metzger, & Peters, 1992). Number of “days on which [you] drank to intoxication” in the past 2 weeks was converted to a dichotomous rating of no days drinking to intoxication. We transformed this outcome for two primary reasons. First, it serves as a close parallel to a measure of no heavy drinking days, an accepted, nonabstinence-based measure in the literature (Falk et al., 2010). Second, the data were extreme in their early positive skewness and later shift to a bimodal presentation (0/14 for days of use in past 2 weeks). Thus, as in a prior study with this population and similar data pattern (Collins, Malone, et al., 2012), dichotomization was deemed the most readily analyzable and parsimonious representation of the data.
The Structured Clinical Interview for the DSM-5 (SCID-5) is a validated assessment of DSM-5 criteria for psychiatric disorders (First, Williams, Karg, & Spitzer, 2015). The AUD portion of this measure documented the presence of AUD, a key criterion for study inclusion, as well as number of AUD symptoms, a primary outcome.
The Short Inventory of Problems (SIP-2A) is a psychometrically reliable and valid, 15-item, Likert-scale questionnaire that measures the extent of one’s experience with social, occupational, and psychological harms related to alcohol use (Miller, Tonigan, & Longabaugh, 1995). The summary score for the past 2 weeks served as a primary outcome variable.
Ethyl glucuronide (EtG) is a metabolite of ethyl alcohol formed in the body by glucuronidation after ethanol exposure and may be detected in urine up to 80 hours after exposure (Wurst, Skipper, & Weinmann, 2003). A cut-off of 500ng/ml was used asitis commonly encountered in clinical and forensic settings and has good sensitivity and specificity (Armer, Gunawardana, & Allcock, 2017), particularly when used to detect heavier alcohol use (McDonell et al., 2015).
The RAND 36-Item Short Form Health Survey Version 2 (SF-36) is a psychometrically sound measure of physical and mental health QoL (Ware, Kosinski, & Dewey, 2000). Scaled scores for the physical functioning and mental health scales were used in primary analyses.
The Participant Feedback Form comprises qualitative, open-ended prompts that ascertained participants’ feedback regarding HaRT-A: what participants liked or did not like about HaRT-A, how HaRT-A measured up to their expectations, how they felt their drinking compared pre to post, and what suggestions they had for enhancing HaRT-A.
Treatment integrity was assessed using the HaRT-A Adherence and Competence Coding Scale. This coding system was adapted from procedures used in prior, large-scale alcohol treatment trials (O’Malley, Corbin, almer, Leeman, & Romano, 2006; Pettinati et al., 2004) and harm-reduction studies (Collins, Duncan, et al., 2015; Collins et al., 2014). We used 5 dimensions that measure interventionists’ adherence to and competence with HaRT-A (i.e., informativeness, authoritativeness, direction, warmth, adherence to manualized components). Dimensions were rated by trained, postbaccalaureat research assistants on 7-point Likert scales, where 0 = absence of the characteristic and 6 = very high levels of the characteristic (within the top 10%), except adherence, which was a ratio of observed to expected session components. Double coding was conducted on a randomly selected set of 8% of the sessions for calibration. Once adequate intraclass correlations were achieved (ICC = .84), raters independently coded a randomly selected set of 32% of sessions for treatment integrity analyses.
Treatment Conditions
Services-as-usual control.
Control participants did not receive HaRT-A but attended assessment sessions at each time point and thus experienced the same number of meetings with research staff. Services as usual at the three study sites were not withheld or limited and were thus available across both conditions during the study. The sites’ services are low-barrier and tailored to individuals’ needs. They included provision of outreach; case management; nursing/medical care; access to external service providers; and assistance with basic needs (i.e., food, clothing, income, housing). The active treatment condition, HaRT- , did not overlap with sites’ existing services because no formalized AUD treatment, much less harm-reduction treatment, was offered onsite.
HaRT-A.
This treatment was developed using an iterative, CBPR process by a team comprising researchers, people with lived experience of homelessness and AUD, and providers serving this population (Collins et al., 2018). See Appendix A for the complete treatment manual.
The HaRT-A mindset honors the long-standing grassroots movements that have advocated for community representation in harm-reduction intervention development (Friedman, 2007; Grund, Kaplan, & Adriaans, 1991). Specifically, community voices, values and belief systems were centered in the development of HaRT-A, and likewise, participants’ voices are centered in individual HaRT-A sessions. The HaRT-A mindset also acknowledges the larger familial, community, and even geopolitical forces that are at play in substance use (Collins et al., 2011; Marlatt, 1998), and thus emphasizes the wisdom of the participant in defining their own pathway to recovery.
The HaRT-A heart-set entails a compassionate way of being and communicating with a participant, which are embodied through the motivational interviewing spirit, processes and communication skills (Miller & Rollnick, 2012). In this case, compassion refers to “feeling with” the participant coupled with an unconflicted desire to support the participant on their own chosen trajectory. Thus, the HaRT-A heart-set is an application of motivational interviewing within a harm-reduction treatment context (W. R. Miller, personal communication, May 15, 2018).
Specific HaRT-A components that are administered in each HaRT-A session were codeveloped with community members. They include a) collaborative tracking of participant-preferred alcohol-related metrics, b) elicitation of participants’ own harm-reduction and/or QoL goals as the primary treatment focus, and c) discussion of safer-drinking strategies.
Staff training
Research staff completed online trainings on the ethical conduct of human subjects research as well as manualized, in-person, study-specific training using protocols developed during prior evaluations (Collins, Duncan, et al., 2015; Collins et al., 2014). Assessment interviewers were postbaccalaureate psychology research assistants who received at least 20 hours of training, including a review of written protocols (e.g., probe instructions, skip patterns, crisis de-escalation), mock interviews with feedback, and onsite shadowing, before they began independently recruiting and assessing participants. Interventionists included a registered nurse (NM), psychologist (SLC), and social worker (ET) who received 20 hours of in-person training, including review of the manual, role plays, shadowing and feedback. All staff received weekly supervision, including review of audio-recorded sessions, with a licensed clinical psychologist with over 20 years of experience conducting alcohol intervention research (SEC). Additional consultation was provided by other collaborators, as needed.
Procedures
Between October 2015 and February 2017, participants were recruited from three community-based agencies that serve marginalized and homeless populations and provide clinical and social services (i.e., medical, nursing, case management services). Interested individuals were identified by agency staff and via screening conducted in waiting rooms by research staff. Research staff approached individuals to briefly describe the study and screen participants for fulfilment of inclusion and exclusion criteria. Interested individuals who met initial screening criteria were provided with an explanation of the purpose and procedures of the study, as well as their rights and roles as participants.
After obtaining written, informed consent, research staff conducted 45-minute baseline (week one) interviews using the above measures. Participants were then individually randomized using permuted, stratified block randomization (Hedden, Woolson, & Malcolm, 2006) to either the HaRT-A or services-as-usual control conditions (see Appendix B for detail). HaRT-A participants received their first 20–30 minute treatment session immediately following week one assessments, when possible. All participants were then scheduled for their next sessions one week later and received a $20 payment. All participants attended additional assessment sessions at week two and three (posttest) and one and three months after the posttest session (see flowchart in Figure 1). In all, HaRT-A participants attended three weekly treatment sessions plus a one-month booster session. Procedures were approved by the Institutional Review Board at the University of Washington and followed principles outlined in the Declaration of Helsinki.
Data Analysis Plan
Preliminary analyses.
Analyses were conducted to test for potential group differences at baseline using t-tests and Mann-Whitney U tests for count and continuous data and chi-square tests of independence for dichotomous data. For missingness analyses, we used a series of logistic regressions with robust standard errors to test potential group differences on missing responses for primary outcomes across the follow-up period.
Primary outcome analyses.
Analyses testing the effects of HaRT-A on alcohol, motivation, and QoL outcomes were conducted in Stata 13 and comprised a series of generalized linear models (i.e., extensions of the general linear model that can accommodate outcomes with nonnormal error distributions; Nelder & Baker, 1972) with robust standard errors to account for clustered data. Models included a) centered linear time, to control for simple time effects reflecting regression to the mean (0 = week 1, 1 = week 3, 3 = 1-month follow-up, 7 = 3-month follow-up); b) centered quadratic time, to control for the curvilinear trend shown across most outcomes; c) treatment group, where 0 = control and 1 = HaRT - A; d) the centered linear time x treatment group interaction; and e) the centered quadratic time x treatment group interaction.
Outcome variables were selected to assess the efficacy of HaRT-A in precipitating its intended outcomes: alcohol harm reduction and QoL improvement. Alcohol outcomes included quantity-frequency variables that reflected higher/lower risk for harm (i.e., peak alcohol quantity, no days drinking to intoxication); experience of alcohol-related harm (i.e., SIP summary score); and AUD symptoms. We assessed participants’ motivation for alcohol harm reduction using three readiness rulers (readiness, confidence and importance) and QoL improvement using physical and mental health-related QoL scales from the SF-36. Secondary, exploratory analyses were conducted using more traditional, abstinence-oriented outcomes: self-reported abstinence and urinary toxicology testing (positive EtG > 500 ng/ml). These secondary analyses were conducted to place HaRT-A outcomes in the context of the existing alcohol treatment literature.
When outcomes were coded dichotomously (i.e., no days drinking to intoxication, abstinence, EtG), were nonnormally distributed (i.e., AUD symptoms), or were positively skewed, zero-inflated, overdispersed counts/integers (i.e., peak alcohol quantity, alcohol-related harm, reflected readiness ruler scores), we used Bernoulli (logit link), partial-proportional odds (ordered logit), and negative binomial (log link) models, respectively (Hardin & Hilbe, 2012). We addressed data nonindependence using the modified sandwich estimate of variance, which is robust to the clustering that results from repeated measures. As appropriate, we used diagnostics in modeling, including assessing link functions, overdispersion, standardized residual plots, and fulfillment of proportional-odds/parallel lines assumptions (Hardin & Hilbe, 2012). To enhance interpretability of the treatment effect sizes, exponentiated coefficients (e.g., odds ratios, incident rate ratios) are presented for logistic and negative binomial models, where IRR/OR < 1 indicates an inverse association, IRR/OR = 1 indicates no association, and IRR/OR > 1 indicates a positive association. Alpha was set to p = .05, and confidence intervals were set to 95%.
Results
Preliminary Analyses
Sample descriptive statistics.
Participants had an average age of 47.86 (SD = 9.56) years and were predominantly male (24% female; n = 40). Of the overall sample, 58% self-identified as Black/African American, 22% as white/European American, 12% as American Indian/Alaska Native/First Nations, 5% as Multiracial, 1% as Native Hawaiian/Pacific Islander, and 3% as “Other.” Additionally, 8% of the sample identified as Hispanic/Latinx.
In the overall sample, 8% met criteria for mild, 10% for moderate, and 82% for severe levels of AUD. Most participants (78%) reported at least one day of polysubstance use at baseline (i.e., alcohol plus at least one other substance), with cannabis (59%), crack cocaine (40%), and methamphetamine (18%) comprising the top 3 other substances used. All other substances had a self-reported 2-week baseline prevalence of less than10%.
Baseline group differences.
Treatment groups did not differ significantly on baseline demographic (i.e., age, birth sex, race, ethnicity) or outcome variables (ps > .08; see Table 1 for descriptive statistics on outcomes).
Table 1.
Raw Descriptive Statistics for Outcome Variables by Group Over Time
|
M(SD)/% Mdn |
||||
|---|---|---|---|---|
| Variables | Baseline | Posttest | 1-Month Follow-up | 3-Month Follow-up |
| Peak alcohol quantity | ||||
| HaRT-A | 23.22(16.94) 19.53 |
14.84(17.65) 10.26 |
10.83(8.94) 8.8 |
10.12(10.36) 6.6 |
| Control | 22.27(18.22) 16.91 |
19.28(22.92) 12.96 |
15.30(16.90) 11.30 |
14.53(12.80) 12.96 |
| No days drinking to intoxication | ||||
| HaRT-A | 11.76% | 35.29% | 46.03% | 52.38% |
| Control | 10.84% | 30.56% | 46.67% | 38.33% |
| Alcohol-related harm | ||||
| HaRT-A | 23.28(10.98) 24 |
15.99(12.58) 11.5 |
12.78(11.67) 8 |
12.02(11.89) 7 |
| Control | 20.10(12.76) 21 |
16.04(12.93) 13.5 |
12.83(12.51) 11.5 |
14.40(14.11) 11.5 |
| Alcohol use disorder symptoms | ||||
| HaRT-A | 7.87(2.49) 8 |
5.07(3.60) 5 |
4.59(3.48) 4 |
3.97(3.51) 3 |
| Control | 7.70(2.53) 8 |
5.79(3.34) 6 |
5.27(3.64) 5 |
5.03(3.79) 5 |
| Readiness for harm reduction | ||||
| HaRT-A | 6.99(2.92) 8 |
7.26(3.06) 8 |
7.11(2.92) 7 |
7.87(2.54) 8 |
| Control | 6.75(3.02) 7 |
6.92(3.08) 8 |
7.28(3.20) 8.5 |
7.22(3.11) 8 |
| Confidence for engaging in harm reduction | ||||
| HaRT-A | 6.35(3.05) 7 |
7.32(2.55) 8 |
7.43(2.63) 8 |
7.89(2.07) 8 |
| Control | 7.04(2.89) 7 |
7.67(2.58) 8.5 |
7.27(2.88) 8 |
7.33(3.01) 9 |
| Importance of harm reduction | ||||
| HaRT-A | 8.14(2.50) 10 |
8.00(2.85) 10 |
7.54(3.21) 9 |
8.08(2.76) 10 |
| Control | 7.96(2.89) 10 |
7.68(2.92) 9 |
7.90(2.84) 9 |
7.75(3.19) 10 |
| Physical health-related QoL | ||||
| HaRT-A | 67.59(23.24) 65 |
69.04(25.45) 75 |
70.08(25.01) 75 |
65.57(26.10) 70 |
| Control | 63.98(29.52) 65 |
67.15(29.42) 70 |
70.59(30.33) 85 |
69.67(27.80) 75 |
| Mental health-related QoL | ||||
| HaRT-A | 50.59(26.08) 48 |
58.94(21.21) 64 |
62.67(22.84) 64 |
61.46(22.84) 64 |
| Control | 52.90(21.38) 52 |
60.22(22.04) 62 |
58.67(26.55) 60 |
57.67(25.69) 58 |
| Ethyl Glucoronide (EtG) > 500 ng/ml | ||||
| HaRT-A | 50.00% | 53.13% | 34.43% | 40.00% |
| Control | 44.30% | 54.29% | 48.15% | 52.73% |
| Abstinence achievement | ||||
| HaRT-A | 2.35% | 8.82% | 14.52% | 25.40% |
| Control | 0% | 15.28% | 23.33% | 16.67% |
Notes. Peak alcohol quantity refers to the number of standard drinks (i.e., 12oz beer, 5oz glass of wine, 1.5oz hard liquor) participants reported drinking on their heaviest drinking day. Alcohol-related harm refers to the summary score of the Short Inventory of Problems (SIP; see manuscript body for full description). Alcohol use disorder symptoms refer to the number of DSM-5 criteria fulfilled (American Psychiatric Association, 2013). The readiness, importance and confidence scores were measured using single, 10-point Likert-type scales, with higher scores indicating higher readiness, importance and confidence, respectively (see manuscript body for full description). Quality of life (QoL) was measured using the SF-36 (see manuscript body for full description). Abstinence achievement and EtG >500ng/ml (abstinence biomarker) were dichotomous measures where 0=negative and 1=positive for alcohol use. Percentages in this table indicate the number of participants who specified “1” or positive for the variable in question.
Retention and satisfaction.
Of HaRT-A participants, 100%, 77%, 79% and 73% attended sessions 1, 2, 3 and 4, respectively. Overall, participant retention rates for each assessment session were 83%, 73% and 74% at the posttest, 1- and 3-month follow-ups, respectively (see Figure 1 for retention by group). Content analysis showed that 92% of participants in the active treatment group expressed a predominantly positive view of HaRT-A, whereas 8% expressed predominantly neutral views,and0%expressednegative views.
Missing data analyses.
Missingness on the outcome variables was not associated with group (ps > .79). Missingness occurring completely at random (MCAR) cannot be directly tested because the probability of missingness on the outcome variable is assessed as a function of the values of both predictors and outcomes. These analyses, however, suggested that the missingness mechanism may be considered “ignorable” for primary analyses (Allison, 2001).
HaRT-A adherence and competence.
Using a two-way mixed effects model, interrater consistency using absolute agreement was adequate for single ratings of adherence and competence (ICC = .84). Across the four competence scales (i.e., informativeness, direction, authoritativeness, warmth), ratings ranged between the “high” and “top 10% of clinicians” levels of the characteristic (M = 5.16–5.88). Adherence was also high, with interventionists providing 99% (SD = .06) of expected components on average per session.
Primary Outcome Analyses
Peak alcohol quantity.
The model testing treatment effects on peak alcohol quantity was significant, Wald χ2(6, N=548) = 56.25, p < .001. Taking the control group into account, HaRT-A participants’ peak alcohol quantity decreased by 10% for each two-week period that passed (see Table 2 for parameter statistics).
Table 2.
Model Parameters for Primary Analyses
| Predictors | Coefficients (IRR/OR/B) | Robust SE | CI(95%) | Z | p |
|---|---|---|---|---|---|
| Peak alcohol quantity | |||||
| Negative binomial processa | |||||
| Other treatment attendance | .73 | .08 | (.59, .90) | −3.00 | .003 |
| Time | .96 | .02 | (.93, 1.00) | −1.99 | .046 |
| Group | .58 | .09 | (.43, .78) | −3.54 | <.001 |
| Time x group | .90 | .03 | (.85, .95) | −3.68 | <.001 |
| Time2 | 1.00 | .01 | (.98, 1.02) | 0.00 | .998 |
| Time2 x group | 1.04 | .01 | (1.02, 1.06) | 3.33 | .001 |
| Constant | 21.53 | 2.47 | (17.19, 26.96) | 26.75 | <.001 |
| Zero-inflated processa | |||||
| Other treatment attendance | 1.60 | .36 | (.90, 2.31) | 4.47 | <.001 |
| Constant | −2.61 | .27 | (−3.13, −2.08) | −9.73 | <.001 |
| Alcohol-related harm | |||||
| Negative binomial processa | |||||
| Other treatment attendance | .96 | .09 | (.79, 1.16) | −0.45 | .656 |
| Time | .96 | .02 | (.93, 1.00) | −1.95 | .051 |
| Group | .88 | .13 | (.67, 1.16) | −0.89 | .373 |
| Time x group | .94 | .02 | (.89, .99) | −2.35 | .019 |
| Time2 | 1.01 | .01 | (1.00, 1.03) | 1.71 | .087 |
| Time2 x group | 1.01 | .01 | (.99, 1.03) | 1.08 | .281 |
| Constant | 16.73 | 1.85 | (13.47, 20.78) | 25.48 | <.001 |
| Zero-inflated processa | |||||
| Other treatment attendance | .67 | .34 | (.01, 1.34) | 1.99 | .047 |
| Constant | −2.23 | .23 | (−2.67, −1.78) | −9.71 | <.001 |
| Alcohol Use Disorder Symptoms | |||||
| Other treatment attendance | .39 | .14 | (.19, .80) | −2.58 | .010 |
| Time | .79 | .04 | (.72, .86) | −5.30 | <.001 |
| Group | .54 | .18 | (.28, 1.04) | −1.84 | .066 |
| Time x group | .87 | .06 | (.77, .99) | −2.17 | .030 |
| Time2 | 1.05 | .02 | (1.02, 1.09) | 2.98 | .003 |
| Time2 x group | 1.03 | .03 | (.98, 1.08) | 1.26 | .208 |
| Constant | 13.46 | 4.01 | (7.51, 24.12) | 8.73 | <.001 |
| Perceived confidence about engaging in harm reduction | |||||
| Other treatment attendance | .84 | .10 | (.67, 1.05) | −1.52 | .127 |
| Time | 1.00 | .02 | (.96, 1.05) | .21 | .830 |
| Group | .86 | .11 | (.67, 1.11) | −1.16 | .247 |
| Time x group | .93 | .03 | (.88, .98) | −2.58 | .010 |
| Time2 | 1.00 | .01 | (.99, 1.02) | .34 | .733 |
| Time2 x group | 1.00 | .01 | (.98, 1.02) | .23 | .820 |
| Constant | 4.37 | .42 | (3.62, 5.27) | 15.38 | <.001 |
| Ethyl glucuronide positive test (> 500ng/ml) | |||||
| Other treatment attendance | .31 | .11 | (.16, .60) | −3.42 | .001 |
| Time | 1.07 | .05 | (.97, 1.18) | 1.27 | .204 |
| Group | .45 | .16 | (.22, .92) | −2.18 | .029 |
| Time x group | .82 | .07 | (.70, .96) | −2.45 | .014 |
| Time2 | .98 | .02 | (.94, 1.02) | −.98 | .328 |
| Time2 x group | 1.06 | .03 | (1.00, 1.13) | 1.94 | .052 |
| Constant | 1.58 | .43 | (.92, 2.69) | 1.67 | .095 |
Notes.
For the negative binomial process, coefficients are represented as incident rate ratios (IRRs). For the zero-inflated process, raw coefficients (B) are presented.
In this partial-proportional odds model, the parallel lines assumption was relaxed for the other treatment attendance variable; thus, the parameters for that and the constant varied depending on how the outcome was dichotomized. The parameters presented in this table are those comparing people with no alcohol use disorder symptoms to all other individuals. Although it was too unwieldy to include in the current table, parameters for other dichotomizations are available from the first author upon request.
No days drinking to intoxication.
The model testing treatment effects on no days drinking to intoxication was significant, Wald χ2(6, N=553) = 79.88, p < .001. However, the time x treatment interaction effect was not (p = .79).
Alcohol-related harm.
The model testing treatment effects on alcohol-related harm was significant, Wald χ2(6, N=547) = 35.48, p < .001. Taking the control group into account, HaRT-A participants’ alcohol-related harm decreased by 6% for each two-week period after study enrollment(see Table 2).
AUD symptoms.
he model testing treatment effects on number of AUD symptoms was significant, Wald χ2(16, N=553) = 119.90, p < .001. Compared to the control group, HaRT-A participants were 13% less likely to experience an additional AUD symptom for each two-week period after study enrollment (see Table 2).
Motivation for harm reduction.
The model testing treatment effects on confidence in making changes in one’s drinking to reduce alcohol-related harm was significant, Wald χ2(6, N=553) = 21.32, p = .002. Taking the control group into account, HaRT-A participants’ confidence increased by 8% for each two-week period after study enrollment (see Table 2). The model testing treatment effects on importance of reducing alcohol-related harm was significant, Wald χ2(6, N=553) = 14.23, p = .03; however, the time x treatment interaction effect was not (p = .30), and the model testing treatment effects on readiness was not significant (p = .18).
Health-related QoL.
The omnibus model for QoL-physical functioning did not reach significance (p > .40). The model for QoL-emotional health was significant, F(6, 167) = 3.41, p = .003; however the time x treatment interaction effect was not (p > .12).
Secondary Outcome Analyses
EtG.
The logistic model testing treatment effects on urinary EtG was significant, Wald χ (6, N=526) = 16.70, p = .01. Taking the control group into account, HaRT-A participants’ likelihood of positive urinary EtG tests decreased by 18% for each two-week period (see Table 2).
Abstinence achievement.
A logistic model testing treatment effects on continuous abstinence was significant, Wald χ2(6, N=552) = 88.13, p < .001. However, the time x treatment interaction was not (p = .81).
Discussion
HaRT-IncreasedConfidenceforEngaging in Alcohol Harm Reduction
Compared to control participants, HaRT-A participants reported feeling increasingly more confident they could engage in alcohol harm reduction over the course of study. There were, however, no significant treatment group differences on measures of participants’ readiness for and perceived importance of alcohol harm reduction. Examination of baseline descriptive statistics showed that the preexisting median level of perceived importance of reducing alcohol-related harm was relatively high at baseline, indicating a potential ceiling effect. Overall, findings suggest that interest in reducing alcohol-related harm was high across participants but that HaRT-A increased participants’ confidence they could translate that interest into actual behavior change.
HaRT-A Resulted in Improved Alcohol Outcomes
We expected HaRT-A would precipitate improvements on alcohol outcomes. It is noteworthy, however, that this expectation is not universally held. There have been concerns that harm reductionists engage in “enabling behavior” (Denning & Little, 2012), which has been defined as an act that “may be reasonably thought to reinforce drinking or hinder recovery” (Rotunda, West, & O’Farrell, 2004). Research on this topic has primarily focused on behaviors of partners and families of people with AUD (e.g., encouraging partner to go to work despite a hangover, taking over neglected chores, or explaining partner’s impaired behavior to others; Rotunda & Doman, 2001). However, providers have also fielded concerns that they enable people’s substance use when they utilize harm-reduction interventions (Denning & Little, 2012), such as discussion of safer-use strategies or meeting with intoxicated clients. The implication is that a harm-reduction approach provides permission or even encouragement to drink, which are, in turn, believed to precipitate increased alcohol use and alcohol-related harm.
The present study provides initial evidence to allay these concerns. Compared to their services-as-usual control counterparts, HaRT-A participants showed statistically significant improvements on alcohol outcomes, including reductions in peak alcohol quantity, alcohol-related harm, number of AUD symptoms, and alcohol-positive EtG tests. These encouraging initial findings corresponded to those for other, albeit community-level harm-reduction approaches applied with this population, including the low-barrier, nonabstinence-based Housing First model (Collins, Malone, et al., 2012; Larimer et al., 2009) and alcohol management programs (Podymow et al., 2006; Stockwell et al., 2017; Vallance et al., 2016).
HaRT-A Was Not Associated with Improved QoL
The inconclusive finding regarding group differences for physical and mental health QoL has various potential explanations. First, the relative brevity of both the 4-session HaRT-A and the 3-month follow-up period may not be adequate to engender and register QoL changes, respectively. Further, the achievement of positive and sustained changes in QoL in this population likely also requires meeting people’s many other basic needs, including food security, permanent housing, and adequate medical and mental health services. Finally, one systematic review indicated that common QoL measures (e.g., SF-36) rarely show significant AUD treatment effects (Luquiens, Reynaud, Falissard, & Aubin, 2012). This finding could be attributable to the generic nature of such questionnaires, which is necessary to facilitate their use across a range of health conditions but may also fail to capture alcohol-specific aspects of QoL. easures to date also assess researcher-versus patient-defined QoL. Fortunately, alcohol researchers have recently developed and validated a participant-driven, alcohol-specific QoL measure that is a promising means of measuring this construct in future trials (Luquiens et al., 2016).
Limitations
Study limitations deserve mention. HaRT-A comprised four treatment sessions, and this brevity may, in part, explain the inconclusive tests for group differences on some alcohol and QoL outcomes. That said, its brevity may also be its strength: Briefer engagement strategies have been shown to be effective and manageable for people with AUD (Field & Caetano, 2010; Guth et al., 2008), as well as for members of this specific population (Wain et al., 2011). HaRT-A components may also be repeated cyclically in clinical practice and may thus be implemented as either a brief intervention or repeated across sessions in longer-term treatment contexts.
This study’s generalizability may be limited by its geographic location as well as sociodemographics and substance-use patterns specific to the homeless population in this area. In particular, this study was implemented in low-barrier settings serving a nontreatment-seeking, homeless population in a large, resources-rich city in the US Pacific Northwest. Further, we did not exclude polysubstance users in order to provide a real-world assessment of the treatment effectiveness as well as embody harm reduction’s inclusive and low-barrier approach. Thus, these findings may not generalize to other communities where abstinence-based service settings or solely alcohol-using populations are the norm. Relatedly, the majority of the sample reported cannabis use, which is indicative of its legal status in Washington State where this study was conducted. Our safer-use strategy endorsing a switch-over from heavy alcohol use to cannabis use was deemed likely to result in relative harm reduction for people experiencing the physical sequelae (e.g., liver disease, pancreatitis) of severe AUD. However, this particular safer-use strategy resulted from our locally conducted community-based participatory research process, and could be tailored or dropped when more broadly disseminated to less severely affected populations or in areas where cannabis use is illegal. Finally, the sample was representative of the larger US homeless population in terms of race and age (US Department of Housing and Urban Development, 2017), and was representative of the local homeless, AUD-affected community. These findings, however, may not be generalizable to youth experiencing homelessness, communities with greater Latinx representation, and housed individuals.
Finally, there were important factors that were not assessed in the current study, including the experience of psychiatric and medical disorders, the relative performance of harm-reduction versus abstinence-based treatment, and potential underlying mechanisms of action. In this study, we sought to establish feasibility, desirability and initial, short-term outcomes. Future, larger-scale randomized controlled trials could include more comprehensive assessments of co-occurring disorders, an abstinence-based treatment comparison condition, as well as tests of mediators of the hypothesized treatment effects. Such next-steps would provide a more nuanced understanding of the population, relative treatment effects, and potential mechanisms of action.
Conclusions and Future Directions
Findings provide evidence that HaRT-A has short-term efficacy for improving alcohol outcomes—even on biological measures—in people experiencing homelessness and AUD. Future studies are needed to test the longer-term efficacy of HaRT-A, compare it to abstinence-based treatments, and explore its underlying mechanisms of action. Ultimately, it will be important to know if the self-reported reductions in alcohol-related harm documented in this study correspond to longer-term reductions in alcohol-related mortality, criminal justice system involvement, and health-related quality of life. If so, the harm-reduction mindset, heart-set and components could be adapted and evaluated across different sociodemographic and substance-using populations to address the needs of the 89% of Americans with substance use disorders in the general population who are not currently served by the existing abstinence-based treatment system (Center for Behavioral Health Statistics and Quality, 2016).
Supplementary Material
Highlights.
Harm reduction treatment for alcohol (HaRT-A) was codeveloped with people with lived experience of homelessness and alcohol use disorder (AUD).
HaRT-A prioritizes reduction in alcohol-related harm over abstinence or use reduction.
Compared to services as usual, HaRT-A is associated with statistically significantly less heavy alcohol use, alcohol-related harm, and AUD symptoms.
HaRT-A is also associated with increased confidence to engage in harm reduction.
Acknowledgments
This work was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) to Susan E. Collins (R34AA022077). Seema L. Clifasefi’s time was additionally supported by a grant from NIAAA (K01AA021147). NIAAA did not have a role in study design; collection, analysis and interpretation of the data; report writing; or decision to submit the article for publication.
We acknowledge our partners at the Downtown Emergency Service Center (DESC), Evergreen Treatment Services - REACH, and Pioneer Square Clinic, especially Molly Carney, Michael Donegan, Edward Dywer-O’Connor, Kelley Craig, Chloe Gale, Mary Mahar, Jaime Moss, and Dr. Nancy Sugg. We thank Tatiana Ubay and Greta Kaese for conducting assessment interviews, Dr. Emma Elliott-Groves for her support on the ground, and Angie Woodstock for data management and preparation. We thank student research assistants, including Sunny Chang, Alex Clark, Jingyan Gu, Robby Hardy, Gary Lee, Victoria Orfaly, Alex Vess, and Teresa Wu.
We thank our colleagues and mentors for their helpful advice in handling clinical and research challenges, including Drs. Patt Denning, Mary Larimer, and Michele Peake-Andrasik. We are grateful to Dr. G. Alan Marlatt, whose trailblazing work and mentorship inspired these efforts. We also thank Dr. William R. Miller for his work on the spirit of motivational interviewing, which forms the foundation of the HaRT-A heart-set, and for his help in drawing parallels and distinctions between motivational interviewing and harm-reduction treatment. Most of all, we thank participants in this study for expending their time and energy to support this research, decrease their alcohol-related harm, and improve future treatment options for their communities.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: None.
Contributor Information
Susan E. Collins, University of Washington – Harborview Medical Center
Seema L. Clifasefi, University of Washington – Harborview Medical Center
Lonnie A. Nelson, Washington State University
Joey Stanton, Downtown Emergency Service Center, University of Washington – Harborview edical Center.
Silvi C. Goldstein, University of Washington – Harborview Medical Center
Emily M. Taylor, University of Washington – Harborview Medical Center
Gail Hoffmann, University of Washington – Harborview Medical Center.
Victor L. King, University of Washington – Harborview Medical Center
Alyssa S. Hatsukami, University of Washington – Harborview Medical Center
Zohar Lev Cunningham, University of Washington – Harborview Medical Center.
Ellie Taylor, University of Washington – Harborview Medical Center.
Nigel Mayberry, University of Washington – Harborview Medical Center.
Daniel K. Malone, Downtown Emergency Service Center
T. Ron Jackson, Evergreen Treatment Services – REACH, University of Washington.
References
- Allison PD (2001). Missing data Thousand Oaks, CA: Sage. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Armer JM, Gunawardana L, & Allcock RL (2017). The Performance of Alcohol Markers Including Ethyl Glucuronide and Ethyl Sulphate to Detect Alcohol Use in Clients in a Community Alcohol Treatment Programme. Alcohol Alcohol, 52(1), 29–34. doi: 10.1093/alcalc/agw072 [DOI] [PubMed] [Google Scholar]
- Baggett TP, Chang Y, Singer D, Porneala B, Gaeta J, O’Connell J, & Rigotti N (2015). Tobacco-, alcohol-, and drug-attributable deaths and their contribution to mortality disparities in a cohort of homeless adults in boston. American Journal of Public Health, 105, 1189–1197. doi: 10.2105/AJPH.2014.302248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertholet N, Gaume J, Faouzi M, Daeppen J-B, & Gmel G (2012). Predictive value of readiness, importance, and confidence in ability to change drinking and smoking. Addiction Science & Clinical Practice, 7(Suppl 1), A28–A28. doi: 10.1186/1940-0640-7-S1-A28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U (1979). The ecology of human development Cambridge, MA: Harvard University Press. [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2016). Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16–4984, NSDUH Series H-51) Retrieved from http://www.samhsa.gov/data/.
- Center for Substance Abuse Treatment. (1999). Enhancing motivation for change in substance abuse treatment: Treatment Improvement Protocol (TIP) Series 35 HHS publication No (SMA) 13–4212. Retrieved from http://ncadi.samhsa.gov/govpubs/bkd342/35l.aspx [PubMed]
- Clifasefi SL, Collins SE, Torres NI, Grazioli VS, & Mackelprang JL (2016). Housing First, but what comes second? A qualitative study of resident, staff and management perspectives on single-site Housing First program enhancement. Journal of Community Psychology, 44(7), 845–855. doi: 10.1002/jcop.21812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins SE, Clifasefi SL, Dana EA, Andrasik MP, Stahl NE, Kirouac M, … Malone DK (2012). Where harm reduction meets Housing First: Exploring alcohol’s role in a project-based Housing First setting. International Journal of Drug Policy, 23, 111–119. doi: 10.1016/j.drugpo.2011.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins SE, Clifasefi SL, Logan DE, Samples L, Somers J, & Marlatt GA (2011). Chapter 1 - Harm reduction: Current status, historical highlights and basic principles. In Marlatt GA, Witkiewitz K, & Larimer ME (Eds.), Harm reduction: Pragmatic strategies formanaginghigh-riskbehaviors (2nd ed). New York: Guilford; http://www.guilford.com/excerpts/marlatt2.pdf. [Google Scholar]
- Collins SE, Clifasefi SL, Stanton J, The LEAP Advisory Board, Straits KJE, Gil-Kashiwabara, ., … Wallerstein N (2018). Community-based participatory research ( BPR): Towards equitable involvement of community in psychology research. American Psychologist, 73, 884–898. doi: 10.1037/amp0000167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins S, Duncan MH, Smart BF, Saxon AJ, Malone D, Jackson T, & Ries R (2015). Extended-release naltrexone and harm reduction counseling for chronically homeless people with alcohol dependence. Substance Abuse, 36, 21–33. doi: 10.1080/08897077.2014.904838 [DOI] [PubMed] [Google Scholar]
- Collins SE, Grazioli V, Torres N, Taylor E, Jones C, Hoffman G, … Dean P (2015). Qualitatively and quantitatively defining harm-reduction goals among chronically homeless individuals with alcohol dependence. Addictive Behaviors, 45, 184–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins SE, Jones CB, Hoffmann G, Nelson LA,Hawes SM,Grazioli VS,… Clifasefi SL (2016). In their own words: Content analysis of pathways to recovery among individuals with the lived experience of homelessness and alcohol use disorders. Int J Drug Policy, 27, 89–96. doi: 10.1016/j.drugpo.2015.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins SE, Malone DK, Clifasefi SL, Ginzler J, Garner MD, Burlingham B, … Larimer ME (2012). Project-based Housing First for chronically homeless individuals with alcohol problems: Within-subjects analyses of two-year alcohol-use trajectories. American Journal of Public Health, 102, 511–519. doi: 10.2105/AJPH.2011.300403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins SE,Saxon AJ,Duncan MH, Smart BF, Merrill JO, Malone DK, … Ries RK (2014). Harm reduction with pharmacotherapy for homeless people with alcohol dependence: Protocol for a randomized controlled trial. Contemporary Clinical Trials, 38, 221–234. doi: 10.1016/j.cct.2014.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denning P, & Little J (2012). Practicing harm reduction psychotherapy: An alternative approach to addictions (2nd edition). New York: Guilford Press. [Google Scholar]
- Des Jarlais DC, Feelemyer JP, Modi SN, Abdul-Quader A, & Hagan H (2013). High coverage needle/syringe programs for people who inject drugs in low and middle income countries: a systematic review. BMC Public Health, 13, 53. doi: 10.1186/1471-2458-13-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk D, Wang XQ, Liu L, Fertig J, Mattson M, Ryan M, … Litten RZ (2010). Percentage of Subjects With No Heavy Drinking Days: Evaluation as an Efficacy Endpoint for AlcoholClinical Trials. Alcoholism: Clinical and Experimental Research, 34(12), 2022–2034. doi: 10.1111/j.1530-0277.2010.01290.x [DOI] [PubMed] [Google Scholar]
- Fazel S, Geddes JR, & Kushel M (2014) .The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet (London, England), 384(9953), 1529–1540. doi: 10.1016/S0140-6736(14)61132-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field CA, & Caetano R (2010). The effectiveness of brief intervention among injured patients with alcohol dependence: Who benefits from brief interventions. Drug Alcohol Depend, 111, 13–20. doi: 10.1016/j.drugalcdep.2009.11.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Williams JBW, Karg RS, & Spitzer RL (2015). Structured clinical interview for DSM-5, Research version (SCID-5 for DSM-5, Research Version; SCID-5-RV) Arlington,VA: American Psychiatric Association. [Google Scholar]
- Friedman SR, de Jong W, Rossi D, Touze G, Rockwell R, Des Jarlais DC, & Elovich R (2007). Harm reduction theory: Users’ culture, micro-social indigenous harm reduction, and the self-organization and outside-organization of users’ groups. International Journal of Drug Policy, 18, 107–117. doi: 10.1016/j.drugpo.2006.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg G, & Rosenheck RA (2010). Correlates of past homelessness in the National Epidemiological Survey on alcohol and related conditions. Administration and Policy in Mental Health, 37, 357–366. doi: 10.1007/s10488-009-0243 [DOI] [PubMed] [Google Scholar]
- Grund J-P, Kaplan CD, & Adriaans NFP (1991). Needle sharing in the Netherlands: An ethnographic analysis. American Journal of Public Health, 81, 1602–1607. doi: 10.2105/AJPH.81.12.1602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guth S, Lindberg SA, Badger GJ, Thomas CS, Rose GL, & Helzer JE (2008). Brief intervention in alcohol-dependent versus nondependent individuals. Journal of Studies on Alcohol and Drugs, 69, 243–250. [DOI] [PubMed] [Google Scholar]
- Hardin JW, & Hilbe JM (2012). Generalized linear models and extensions, 3nd Edition. College Station, TX: Stata Press. [Google Scholar]
- Heather N (2006). Controlled drinking, harm reduction and their roles in the response to alcohol- related problems. Addiction Research and Theory, 14, 7–18. doi: 10.1080/16066350500489170 [DOI] [Google Scholar]
- Heather N, Smailes D, & Cassidy P (2008). Development of a readiness ruler for use with alcohol brief interventions. Drug Alcohol Depend, 98, 235–240. doi: 10.1016/j.drugalcdep.2008.06.005 [DOI] [PubMed] [Google Scholar]
- Hedden SL, Woolson RF, & Malcolm RJ (2006). Randomization in substance abuse clinical trials. Substance Abuse Treatment, Prevention and Policy, 1, 6. doi: 10.1186/1747-597X-1-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang SW, Tolomiczenko G, Kouyoumdjian FG, & Garner RE (2006). Interventions to improve the health of the homeless. American Journal of Preventative Medicine, 29, 311–319. [DOI] [PubMed] [Google Scholar]
- Hwang SW, Wilkins R, Tjepkema M, O’Campo P, & Dunn JR (2009). Mortality among residents of shelters, rooming houses and hotels in Canada: 11 year follow-up. British Medical Journal, 339, b4036. doi: 10.1136/bmj.b4036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krausz RM, Clarkson AF, Strehlau V, Torchalla I, Li K, & Schuetz CG (2013). Mental disorder, service use, and barriers to care among 500 homeless people in 3 different urban settings. Soc Psychiatry Psychiatr Epidemiol, 48(8), 1235–1243. [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Shiffman JE, & Earleywine ME (2005). Performance of alcohol and safer sex Behaviors, 19, 112–115. doi: 10.1037/0893-164X.19.1.112 [DOI] [PubMed] [Google Scholar]
- Larimer ME, Malone DK, Garner MD, Atkins DC, Burlingham B, Lonczak HS, … Marlatt GA (2009). Health Care and Public Service Use and Costs Before and After Provision of Housing for Chronically Homeless Persons With Severe Alcohol Problems. Journal of the American Medical Association, 301, 1349–1357. doi: 10.1001/jama.2009.414 [DOI] [PubMed] [Google Scholar]
- Luquiens A, Reynaud M, Falissard B, & Aubin HJ (2012). Quality of life among alcohol-dependent patients: how satisfactory are the available instruments? systematic review. DrugAlcoholDepend,125(3),192–202. doi: 10.1016/j.drugalcdep.2012.08.012 [DOI] [PubMed] [Google Scholar]
- Luquiens A, Whalley D, Laramee P, Falissard B, Kostogianni N, Rehm J, … Aubin HJ (2016). Validation of a new patient-reported outcome instrument of health-related quality of life specific to patients with alcohol use disorder: the Alcohol Quality of Life Scale (AQoLS). Qual Life Res, 25(6), 1549–1560. doi: 10.1007/s11136-015-1190-5 [DOI] [PubMed] [Google Scholar]
- Maisto SA, Krenek M, Chung T, Martin CS, Clark D, & Cornelius J (2011). A comparison of the concurrent and predictive validity of three measurs of readiness to change alcohol use in a clinical sample of adolescents. Psychological assessment, 23, 983–994. doi: 10.1037/a0024136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markam MR, Miller WR, & Arciniega L (1993). BACCuS 2.01: Computer software for quantifying alcohol consumption. Behavior Research Methods, Instruments & Computers, 25, 420–421. [Google Scholar]
- Marlatt GA (1998). Basic principles and strategies of harm reduction. In Marlatt GA (Ed.), Harm reduction: Pragmatic strategies for managing high-risk behaviors (pp. 49–66).New York: The Guilford Press. [Google Scholar]
- Marlatt GA, Baer JS, Kivlahan DR, Dimeff LA, Larimer M, Quigley L, … Williams E (1998). Screening and brief intervention for high-risk college student drinkers: Results from a 2-year follow-up assessment. Journal of Consulting and Clinical Psychology, 66, 604–615. doi: 10.1037//0022-006X.66.4.604 [DOI] [PubMed] [Google Scholar]
- Marlatt GA, & Witkiewitz K (2010). Update on harm-reduction policy and intervention research. Annual Review of Clinical Psychology, 6, 591–606. doi: 10.1146/annurev.clinpsy.121208.131438 [DOI] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, & Davoli M (2014). Buprenorphine maintenance versusplacebo or methadone maintenance for opioid dependence. Cochrane Database of Systematic Reviews (2). doi: 10.1002/14651858.CD002207.pub4 [DOI] [Google Scholar]
- McDonell MG,Skalisky J, Leickly E, McPherson S, Battalio S, Nepom JR, … Ries RK (2015). Using ethyl glucuronide in urine to detect light and heavy drinking in alcohol dependent outpatients. Drug Alcohol Depend, 157, 184–187. doi: 10.1016/j.drugalcdep.2015.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The McKinney-Vento Homeless Assistance Act, 42 USC § 11302 (2009).
- McLellan AT, Kushner H, Metzger D, & Peters R (1992). The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment, 9, 199–213. doi: 10.1016/0740-5472(92)90062-S [DOI] [PubMed] [Google Scholar]
- Miller WR, & Rollnick S (2012). Motivational interviewing: Helping people change (3rd edition). New York: Guilford Press. [Google Scholar]
- Miller WR, Tonigan J, & Longabaugh R (1995). The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse Test manual (Vol. 4, Project MATCH Monograph Series). Rockville: National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- Minkler M, & Wallerstein N (2008). Chapter 1: Introduction to community-based participatory research. In Minkler M & Wallerstein N (Eds.), Community-based participatory research for health: From process to outcomes San Francisco: Jossey Bass. [Google Scholar]
- Nelder JA, & Baker RJ (1972). Generalized linear models. Journal of the Royal Statistical Society, 135, 370–384. doi: 10.2307/2344614 [DOI] [Google Scholar]
- NIAAA. (2005). Helping patients who drink too much: A clinician’s guide Bethesda, MD: NIAAA: NIH publication; no. 05–3769. [Google Scholar]
- Nielsen S, Larance B, Degenhardt L, Gowing L, Kehler C, & Lintzeris N (2016). Opioid agonist treatment for pharmaceutical opioid dependent people. Cochrane Database of Systematic Reviews(5). doi: 10.1002/14651858.CD011117.pub2 [DOI] [PubMed] [Google Scholar]
- North CS, Eyrich-Garg KM, Pollio DE, & Thirthalli J (2010). A prospective study of substance use and housing stability in a homeless population. Soc Psychiatry Psychiatr Epidemiol, 45(11), 1055–1062. doi: 10.1007/s00127-009-0144-z [DOI] [PubMed] [Google Scholar]
- O’Malley SS, Corbin WR, Palmer R, Leeman RF, & Romano D (2006). Manual for combining naltrexone with BASICS for the treatment of heavy alcohol use in young adults Yale University School of Medicine; New Haven, CT. [Google Scholar]
- Orwin RG, Garrison-Mogren R, Jacobs ML, & Sonnefeld LJ (1999). Retention of homeless clients in substance abuse treatment: Findings from the National Institute on Alcohol Abuse and Alcoholism Cooperative Agreement Program. Journal of Substance Abuse Treatment, 17, 45–66. [DOI] [PubMed] [Google Scholar]
- Pearson MR (2013). Use of Alcohol Protective Behavioral Strategies among College Students: A Critical Review. Clinical psychology review, 33(8), 10.1016/j.cpr.2013.1008.1006. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettinati HM, Weiss RD, Miller WR, Donovan D, Ernst DB, & Rounsaville BJ (2004). Medical Management Treatment Manual: Clinical Research Guide for Medically Trained Clinicians Providing Pharmacotherapy as Part of a Treatment for Alcohol Dependence. COMBINE Monograph Series, Volume 2 DHHS Publication No. (NIH) 04–5289 Bethesda, MD: NIAAA. [Google Scholar]
- Podymow T, Turnbull J, Coyle D, Yetisir E, & Wells G (2006). Shelter-based managed alcohol administration to chronically homeless people addicted to alcohol. Canadian Medical Association Journal, 174, 45–49. doi:doi: 10.1503/cmaj.1041350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Shield K, Gmel G, Rehm MX, & Frick U (2013). Modeling the impact of alcohol dependence on mortality burden and the effect of available treatment interventions in the European Union. Eur Neuropsychopharmacol, 23(2), 89–97. doi: 10.1016/j.euroneuro.2012.08.001 [DOI] [PubMed] [Google Scholar]
- Rosenheck RA, Morrissey J, Lam J, Calloway M, Johnsen M, Goldman H, … Teague G (1998). Service system integration, access to services, and housing outcomes in a program for homeless persons with severe mental illness. American Journal of Public Health, 88, 1610–1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotunda RJ, & Doman K (2001). Partner Enabling of Sub stance Use Disorders: Critical Review and Future Directions. The American Journal of Family Therapy, 29(4), 257–270. doi: 10.1080/01926180126496 [DOI] [Google Scholar]
- Rotunda RJ, West L, & O’Farrell TJ (2004). Enabling behavior in a clinical sample of alcohol-dependent clients and their partners. Journal of Substance Abuse Treatment, 26(4), 269–276. doi: 10.1016/j.jsat.2004.01.007 [DOI] [PubMed] [Google Scholar]
- Smith JE, Meyers RJ, & Delaney HD (1998). The Community Reinforcement Approach with homeless alcohol-dependent individuals. Journal of Consulting and Clinical Psychology, 66, 541–548. doi: 10.1037//0022-006X.66.3.541 [DOI] [PubMed] [Google Scholar]
- Stockwell T,Pauly B,Chow C,Erickson RA,Krysowaty B, Roemer A,…Zhao J (2017). Does managing the consumption of people with severe alcohol dependence reduce harm? A comparison of participants in six Canadian managed alcohol programs with locally recruited controls. Drug Alcohol Rev doi: 10.1111/dar.12618 [DOI] [PubMed] [Google Scholar]
- US Department of Housing and Urban Development. (2017. Retrieved from: https://www.hudexchange.info/resources/documents/2017-AHAR-Part-1.pdf). The 2017 annual homelessness assessment report to Congress: Part 1 Point-in-Time Estimates of Homelessness Washington, D.C. [Google Scholar]
- US Department of Housing and Urban Development. (2018. Retrieved from https://www.hudexchange.info/resources/documents/2017-AHAR-Part-2.pdf). The 2017 annual homeless assessment report (AHAR) to congress Part 2: Estimates of homelessness in the United States Washington, D.C: Author. [Google Scholar]
- Vallance K, Stockwell T, Pauly B, Chow C, Gray E, Krysowaty B, … Zhao J (2016). Do managed alcohol programs change patterns of alcohol consumption and reduce related harm? A pilot study. Harm Reduct J, 13(1),13.doi: 10.1186/s12954-016-0103-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wain RM, Wilbourne PL, Harris KW, Pierson H, Teleki J, Burling TA, & Lovett S (2011). Motivational interview improves treatment entry in homeless veterans. Drug Alcohol Depend, 115, 113–119. doi: 10.1016/j.drugalcdep.2010.11.006 [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, & Dewey JE (2000). How to score version two of the SF-36 Health Survey Lincoln, RI: QualityMetric, Inc. [Google Scholar]
- Washington State Counselor Credentialing Standards, § 15, RCW 18.205.020, c 135 Stat (2008).
- Wenzel SL, Burnam MA, Koegel P, Morton SC, Miu A, Jinnett KJ, & Sullivan JG (2001). Access to inpatient or residential substance abuse treatment among homeless adults withalcoholorotherdrug use disorders. Medical Care, 39, 1158–1169. doi: 10.1097/00005650-200111000-00003 [DOI] [PubMed] [Google Scholar]
- Willenbring ML (2014). reatment of heaving drinking and alcohol use disorder. In Ries RK, Fiellin DA, Miller SC, & Saitz R (Eds.), The ASAM principles of addiction medicine, Fifth Ed. (pp. 375–388). Philadelphia: Wolters Kluwer. [Google Scholar]
- Wurst FM, Skipper G., & Weinmann W (2003). Ethyl glucuronide - the direct ethanol metabolite on the threshold from science to routine use. Addiction, 98(suppl. 2), 51–61. [DOI] [PubMed] [Google Scholar]
- Zerger S (2002). Substance abuse treatment: What works for homeless people? A review of the literature Nashville, TN: National Health Care for the Homeless Council. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


