Abstract
Chronic kidney disease (CKD) is considered an independent risk factor for cardiovascular disease, with increased cardiovascular morbidity and mortality seen even in the early stages of CKD. Several studies have shown a high prevalence of vitamin D deficiency in individuals with CKD. Low vitamin D levels upregulate the renin-angiotensin-aldosterone system (RAAS), cause endothelial dysfunction and increase inflammation. Epidemiological studies show an association between vitamin D deficiency and risk factors for cardiovascular disease, but a causal relationship has not been established. The high cardiovascular morbidity and mortality associated with CKD in adults requires therapies to decrease this elevated risk. However, results from several meta-analyses and randomized clinical trials in adults have not shown convincing evidence for the use of vitamin D therapy in improving cardiovascular outcomes. Lack of high quality evidence from randomized clinical trials in children regarding the effectiveness and long-term safety of vitamin D treatment, precludes any recommendations on its use to mitigate the cardiovascular burden of CKD.
Keywords: chronic kidney disease, children, cardiovascular risk, ergocalciferol, cholecalciferol, active vitamin D analogues
Introduction
Vitamin D is an essential steroid hormone with effects extending beyond its classical role in bone-mineral disease. Recently, the importance of vitamin D in the kidneys, cardiovascular disease, immune system, and cancer has been recognized [1, 2]. With these new roles being studied, there is growing interest in the therapeutic potential of vitamin D.
According to the 2011 report on dietary requirements for calcium and vitamin D from the Institute of Medicine (IOM), vitamin D deficiency has been defined as 25(OH)D levels <20 ng/ml (50 nmol/l) and adequacy as levels ≥30 ng/ml (75 nmol/l). Serum concentrations of 25(OH)D above 50 ng/ml (125 nmol/liter) should be prevented, since risks have been identified for some outcomes [3]. Vitamin D deficiency is highly prevalent in the general population in the US and prevalence varies by geographical location, diet and comorbidities [1].
The spectrum of cardiovascular disease (CVD) in adult CKD patients includes ischemic heart disease, congestive heart failure, arrhythmias and peripheral vascular disease. Vitamin D deficiency has been linked to cardiovascular mortality, both in the general population and in adult patients with CKD [4, 5].
In adult patients with mild to moderate CKD the incidence of cardiovascular mortality is much higher than the incidence of kidney failure, making it the more important reason for increased morbidity seen in CKD [6–8].
It is imperative to focus on therapies that reduce the cardiovascular risk to decrease the morbidity and mortality of CKD.
Vitamin D Metabolism
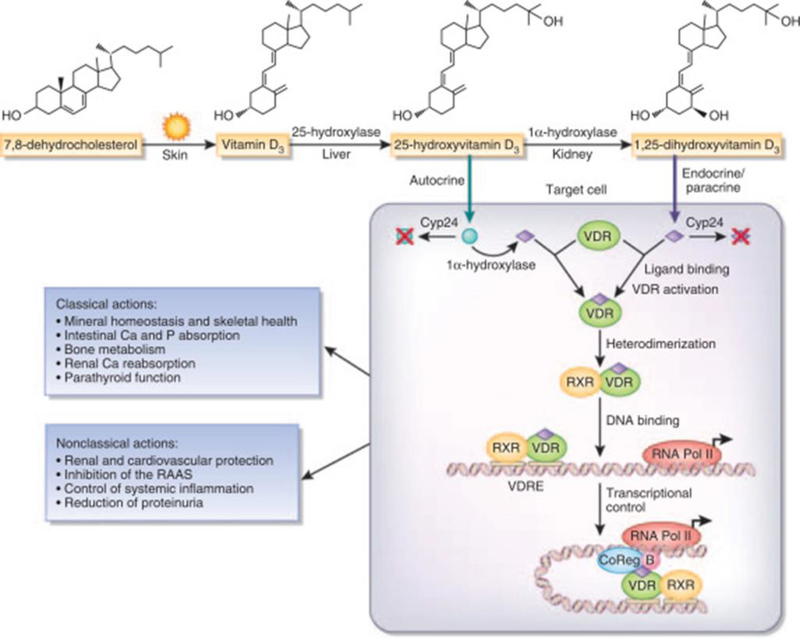
Vitamin D is a prohormone which plays a vital role in bone metabolism, cardiovascular disease, the immune system, and the kidneys [9] (Fig. 1).
Figure 1. Vitamin D bioactivation and actions.
Classical and nonclassical vitamin D actions require vitamin D conversion to 25-hydroxyvitamin D (25(OH)D, open circle), and its bioactivation to its hormonal form 1,25-dihydroxyvitamin D (calcitriol, diamond) by renal and extrarenal 1-hydroxylase and calcitriol binding to and activation of its receptor, the vitamin D receptor (VDR). Calcitriol-activated VDR binds its partner the retinoic X receptor (RXR, heterodimerization) and vitamin D-responsive elements (VDRE) in the promoter of VDR-responsive genes (DNA binding), and recruits basal transcription factors (B) and co-activator and corepressor molecules (CoReg) to induce or repress the transcription of vitamin D-responsive genes by RNA polymerase II (transcriptional regulation). The net balance between cellular uptake of calcitriol and/or 25(OH)D, the rate of 25(OH)D conversion to calcitriol versus the activity of 24-hydroxylase (cyp24), responsible for the inactivation of 25(OH)D and calcitriol (crossed blue circle and purple diamond), determines the degree of VDR activation by intracellular calcitriol. Most of these steps are impaired in kidney disease. Ca, calcium; P, phosphate; RAAS, renin-angiotensin-aldosterone system. Reproduced from Dusso et al. [96], used with permission.
Vitamin D is unique, as it can be obtained from certain foods and also be synthesized in the human body. The term ‘Vitamin D’ includes ergocalciferol (Vitamin D2), a plant and fungal derived calciferol and cholecalciferol (Vitamin D3). These are inactive precursors and sometimes referred to as “nutritional or inactive” vitamin D. Ergocalciferol and cholecalciferol need to be hydroxylated twice in order to become active. Ultraviolet irradiation accounts for approximately 80% of the daily Vitamin D (D3) synthesis, whereas nutritional intake accounts for approximately 20%, consisting of both D2 and D3 [10, 11]. Cholecalciferol is synthesized endogenously when the epidermal layer of the skin is exposed to ultraviolet B radiation. In the epidermis, 7dehydrocholesterol undergoes photolytic cleavage and produces pre-vitamin D3, which undergoes isomerization to produce cholecalciferol [12, 13]. Vitamin D2 and D3 are found in the bloodstream where they bind to vitamin D binding protein (DBP) a carrier molecule responsible for systemic transport. Upon transport to the liver D2 and D3 undergo the first hydroxylation into 25(OH)D (calcifediol) by a hydroxylase enzyme known as CYP2R1 (cytochrome P4502R1) forming stable 25(OH)D-DBP complex. This complex undergoes a second hydroxylation after it is excreted into the urine and reabsorbed via megalin/cubilin at the proximal tubule cells, where it is converted into the active form of vitamin D, 1,25(OH)2D (calcitriol), by the enzyme 1α-hydroxylase (CYP27B1) [2, 14].
The final hydroxylation step is highly regulated. 1α-hydroxylase is upregulated by factors such as low calcium, low phosphate, high parathyroid hormone (PTH), calcitonin, growth hormone (GH), and insulin-like growth factor (IGF). 1α-hydroxylase is down-regulated by high phosphate, high Fibroblast growth factor 23 (FGF23), and 1,25(OH)2D itself [15, 16]. Both 25(OH)D and 1,25(OH)2D are inactivated by the enzyme 24-hydroxylase (CYP24A1). CYP24A1 expression and 24-hydroxylase production are induced most strongly by 1,25(OH)2D, as part of a negative feedback loop. In addition to the kidney, cells from the skin, immune system, gastrointestinal tract, brain and endothelium among others, also express the 1α-hydroxylase enzyme and are able to produce 1,25(OH)2D, which accounts for the paracrine/non-classical actions of active vitamin D. In these tissues the activity of 1α-hydroxylase enzyme is under cell-function-specific control, rather than the mineral metabolism hormones.
Mechanism of action of 1,25(OH)2D
The actions of 1,25(OH)2D are mediated via the nuclear vitamin D receptor (VDR). VDR acts as a ligand-active transcription factor playing an imperative role in the regulation of expression of several genes involved in calcium phosphate homeostasis. VDR is distributed throughout the body in various cells and tissues, such as the epithelium cells of the small intestine, large intestine, distal tubule of kidneys, parathyroid, bronchus, thymus, prostate gland, mammary gland, and the cells of the osteoblasts in bones. The 1,25(OH)2D3 binds to VDR and allows the heterodimerization of VDR with the retinoid X receptor (RXR), forming the VDR-RXR complex. This complex is able to recognize specific DNA sequences known as vitamin D response elements (VDRE). When the 1,25(OH)2D/VDR/RXR complex binds to VDREs, it is able to recruit transcription factors and increase or decrease transcription of genes involved in bone and calcium metabolism, and a multitude of signaling pathways affecting cellular proliferation, differentiation and function. It has also been suggested that 1,25(OH)2D has rapid, non-genomic effects by activating apical voltage-dependent calcium channels and increasing intracellular calcium, a process that may or may not require the VDR [17]. The non-genomic effects also include triggering of downstream signaling pathways in diverse tissues that affect cell differentiation, apoptosis and proliferation [18].
Vitamin D Deficiency in Chronic Kidney Disease
Controversy exists regarding the optimal 25(OH)D level. According to the 2011 report on dietary requirements for calcium and vitamin D from the Institute of Medicine (IOM), vitamin D deficiency has been defined as 25(OH)D levels <20 ng/ml, as this level was considered adequate for bone health in most of the population. The Endocrine Society disagrees with the recommendations of the IOM and consider a level of 30 ng/ml as the lower limit of acceptable [19]. This is based on the studies that have shown decrease in osteoporotic fractures by 33% when the 25(OH)D level was raised from 20 to 21–29 ng/ml [19], meta analyses that have shown no appreciable decrease in fracture rates with 25(OH)D levels below 30 ng/ml [20, 21] and an abnormal osteoid seam width in 6 of 28 subjects in an autopsy study with 25(OH)D levels between 20 to 30 ng/ml [22]. Although controversy exists regarding the definition of vitamin D deficiency, generally levels between 21–29 ng/ml are considered insufficient and levels below 20 ng/ml are considered deficient [23]. We found a 9% prevalence of 25(OH)D deficiency (<15 ng/ml) and 61% prevalence of insufficiency (levels between 16–29 ng/ml) in a nationally representative sample of healthy children and young adults aged 1 to 21 years in the National Health and Nutrition Examination Survey 2001–2004 [24]. This study was done prior to the IOM guidelines being released and used the cut off as <15 ng/ml to define deficiency.
In the Chronic Kidney Disease in Children (CKiD) cohort study, the largest study of children with CKD in North America, we found a 28% prevalence of 25(OH)D levels <20 ng/ml and a 50% prevalence of levels <30 ng/ml [25]. In both the general pediatric and CKD populations, deficiency of 25(OH)D was associated with older age, non-white race, higher BMI, lower milk intake and absence of vitamin D supplement use. The CKD-specific risk factor for deficiency was nephrotic range proteinuria [24, 25]. We did not find an association between severity of CKD and 25(OH)D deficiency, but others have reported a higher prevalence with lower glomerular filtration rate (GFR) [26, 27]. We also evaluated the determinants of 1,25(OH)2D deficiency in the CKiD cohort and found serum 25(OH)D and GFR to be significantly positively associated, and age, FGF23 levels and proteinuria to be inversely associated with 1,25(OH)2D levels [25].
Both the classical effects on bone/mineral metabolism and non-classical actions of vitamin D can be affected by its deficiency.
Increased Cardiovascular Risk in Chronic Kidney Disease
Impaired kidney function has been associated with a wide spectrum of cardiovascular diseases. The causes for increased cardiovascular morbidity in CKD are many, including traditional cardiovascular risk factors such as hypertension, diabetes mellitus, left ventricular hypertrophy (LVH), coronary artery disease, dyslipidemia as well as factors such as chronic inflammation, increased activity of the renin-angiotensin-aldosterone system (RAAS) and sympathetic nerve activity. However, increased cardiovascular risk in CKD is not just due to the high prevalence of hypertension and diabetes. Meta-analyses of several studies [7, 8], involving more than 1.4 million individuals, showed that after adjustment for traditional cardiovascular risk factors and albuminuria the risk for cardiovascular mortality increased linearly with decreasing estimated GFR below 75 ml/min/1.73m2. Cardiovascular mortality was about twice as high in patients with stage 3 CKD (estimated GFR 30–59 mL/min/1.73 m2) and three times higher at stage 4 (15–29 mL/min/1·73 m2) than in individuals with normal kidney function. The association of albuminuria with cardiovascular risk was even more significant. After adjustment for traditional cardiovascular risk factors and estimated GFR, the adjusted risk of cardiovascular mortality more than doubled at the upper end of the microalbuminuria category (30–299 mg/g) compared with the risk in individuals with no albuminuria. Even slight increases in albuminuria have significant clinical consequences. This was studied in a large population cohort in Canada. Life expectancy for 30-year-old subjects with CKD stage 3B and 4 was reduced by 17 and 25 years, respectively. Similarly, in 30-year-olds with albuminuria, minimally elevated (30–299 mg/g) and ≥300 mg/g albuminuria, was associated with a 10 and 18 year shorter life expectancy, respectively [6].
Children with CKD too have a shortened life span and cardiovascular disease is the main cause of this increase in mortality, especially in children on dialysis. Even after a kidney transplant the increased risk persists and the average life span of a child with a transplant is 10–15 years less than the general population [28]. Processes that contribute to this increased risk include, uncontrolled hypertension, dyslipidemia, vascular endothelial dysfunction, medial arterial calcification, increased carotid artery intima-media thickness and cardiac dysfunction [29–32]. In children, fewer approved therapies are available to manage the above complications and there are few if any randomized clinical trials to assess the long-term benefits in terms of overall and cardiovascular morbidity and mortality in this vulnerable population.
Vitamin D deficiency and increased cardiovascular risk
Observational studies have mostly evaluated the associations between 25(OH)D levels (the inactive form of vitamin D) and cardiovascular outcomes, whereas most clinical trials have used both inactive vitamin D supplements (ergocalciferol or cholecalciferol) or active vitamin D analogues (calcitriol, paricalcitol, doxercalciferol and 1-α calcidiol) as an intervention to assess the effects of vitamin D on cardiovascular outcomes.
Observational studies have shown associations between 25(OH)D deficiency and increased cardiovascular events in the general population. In evaluation of vitamin D deficiency in the normal pediatric population, using the NHANES cohort, we and others have shown that lower 25(OH)D levels were more likely to be associated with lower HDL cholesterol levels, diabetes mellitus, hypertension and the metabolic syndrome [24, 33]. Similarly in adults, using the NHANES III database it was shown that the adjusted prevalence of hypertension (OR, 1.30), diabetes mellitus (OR, 1.98), obesity (OR, 2.29), and high serum triglyceride levels (OR, 1.47) were significantly higher in the first than in the fourth quartile of serum 25(OH)D levels (P<0.001 for all) [34]. In the CKD and end-stage renal disease (ESRD) populations too low 25(OH)D levels have been associated with increased cardiovascular morbidity and mortality [35–37].
Vitamin D may have cardiovascular effects via several mechanisms. 25(OH)D is a known regulator of the RAAS and treatment with calcitriol leads to renin suppression in experimental studies [38]. VDR is present on vascular smooth muscle cells and calcitriol can affect proliferation of these cells [39]. VDR agonists can increase the expression of calcification inhibitors, such as matrix-gla protein and osteopontin, in vascular cells and decrease the expression of pro-inflammatory cytokines [40].
Vitamin D may act by the above and multiple other ways, like decreasing proteinuria and lowering blood pressure to mitigate the increased cardiovascular risk seen in CKD patients [41].
Vitamin D and Hypertension
Preclinical studies suggest a role for vitamin D in modulating the RAAS, vascular smooth muscle cells and the endothelium [38, 42–44]. Hence, a biological plausibility exists for the associations seen between 25(OH)D and blood pressure in observational studies.
Ke et al. performed a mixed effects meta-analysis of observational studies published between 2007 to 2014. Ten prospective studies (n=58,262) and 19 cross-sectional studies (n=90,535) were included. Pooled risk for incident hypertension when comparing the highest vs. lowest category of 25(OH)D showed a relative risk of 0.76 (0.63–0.90) for the prospective studies and an odds ratio of 0.79 (0.73–0.87) for the cross-sectional studies [45]. These observational data, although significant, could not prove causality between 25(OH)D and hypertension.
Intervention studies of vitamin D supplementation, both inactive (cholecalciferol or ergocalciferol) and active vitamin D analogues (calcitriol, 1-α calcidiol, paricalcitol, and doxercalciferol) for hypertension have shown conflicting results so far [46, 47], with some showing decrease in blood pressure, while some showing no effect. A recent systematic review investigated whether supplementation with vitamin D2 (ergocalciferol), vitamin D3 (cholecalciferol), calcitriol (1,25-hydroxyvitamin D3), 1-α-hydroxylated vitamin D, paricalcitol, and doxerocalciferol may reduce blood pressure [48]. It included 46 randomized placebo-controlled clinical trials with 4,541 participants from 1966 to 2014. Trials that used vitamin D supplementation for a minimum of 4 weeks for any indication and reported blood pressure data were part of the analyses. Co-interventions were permitted if identical in all treatment arms. At the trial level, no effect of vitamin D supplementation was seen on systolic blood pressure (effect size, 0.0 [95% CI, −0.8 to 0.8] mm Hg; P = 0.97; I 2 = 21%) or diastolic blood pressure (effect size, −0.1 [95% CI, −0.6 to 0.5] mm Hg; P = 0.84; I 2 = 20%). Similar results were found analyzing individual patient data for systolic blood pressure (effect size, −0.5 [95% CI, −1.3 to 0.4] mm Hg; P = 0.27; I 2 = 0%) and diastolic blood pressure (effect size, 0.2 [95% CI, −0.3 to 0.7] mm Hg; P = 0.38; I 2 = 0%). Subgroup analysis did not reveal any baseline factor predictive of a better response to therapy. The authors concluded that vitamin D supplementation, active or inactive, is not effective as a treatment for decreasing blood pressure and is not recommended as an antihypertensive drug.
Studies evaluating effects of vitamin D supplementation in the CKD population are very few and most of them have hypertension only as a secondary outcome. A small study compared blood pressure reduction and insulin sensitivity in 7 pediatric patients on hemodialysis and 7 controls after pharmacological doses of IV calcitriol (2 μg/m2). There was a significant reduction in mean arterial blood pressure (from 108 ± 2 to 96 ± 3 mmHg, p <0.05) in the dialysis patients when compared to the controls [49].
Pediatric data is available from one of the few randomized clinical trials in pediatric CKD: The Effect of Strict Blood Pressure Control and ACE Inhibition on Progression of CKD in Pediatric Patients (ESCAPE) study. This randomized controlled study showed that strict blood pressure control with a fixed dose of ACE inhibition slowed the progression of renal disease. A post hoc analysis of this data was done to determine whether 25(OH)D levels influence proteinuria and CKD progression. In the 167 children included in the analysis it was shown that there was an inverse association between the diastolic blood pressure before the start of ACE inhibitor treatment and baseline serum 25(OH)D levels (P=0.014, r=–0.19 and P=0.038, r=–0.16 for diastolic blood pressure (mmHg) and diastolic blood pressure standard deviation score, respectively). Patients with 25(OH)D levels <20 ng/ml had higher diastolic blood pressure than those with levels ≥20 ng/ml (P=0.004). The association between diastolic blood pressure and 25(OH)D persisted even on ACE inhibitor treatment (P=0.004, r=–0.22). The systolic blood pressure and 24-hour mean arterial blood pressure at baseline and follow-up did not show any association with 25(OH)D levels at any time point [50].
The Vitamin D Receptor Activator for Albuminuria Lowering (VITAL) was a randomized, placebo-controlled study that evaluated the effect of different doses of an active vitamin D analogue, paricalcitol (2 μg daily or 1 μg daily) on proteinuria over 24 weeks compared to placebo, in 281 patients with diabetic CKD and albuminuria. The subjects were randomized to receive placebo (n=93), 1 μg paricalcitol (n=93), or 2 μg paricalcitol (n=95) [51]. There was a dose-dependent decrease in systolic blood pressure in the paricalcitol group compared with placebo (range −3 to −9 mmHg, p=0.03). Another randomized controlled trial, the Paricalcitol Capsule Benefits in Renal Failure-Induced Cardiac Morbidity (PRIMO) trial included 227 patients with stage 3 and 4 CKD and LVH who were randomized to paricalcitol (2μg daily) or matching placebo for 48 weeks. There was no difference in the primary outcome (left ventricular mass index (LVMI)) or in systolic or diastolic blood pressure (P=0.87 and 0.97, respectively) [52]. Both the above studies did not require patients to be vitamin D deficient; all patients were being treated for hypertension and antihypertensive medication doses were either not available or were not included in the analysis.
As the above variable results suggest, it is still unclear whether inactive or active vitamin D supplementation affect blood pressure or not. Currently ongoing clinical trials such as Vitamin D and Omega-3 Hypertension Trial (VITAL Hypertension) is evaluating if cholecalciferol (2000 units daily) and omega-3 fatty acids (fish oil, 1 gram daily) supplementation lowers blood pressure and decreases the risk of incident hypertension compared to placebo. This study might provide additional insights into the link between 25(OH)D and blood pressure.
Randomized controlled studies in the pediatric CKD and ESRD populations are needed to delineate the effect of vitamin D supplementation on blood pressure and other hard outcomes, like decreased cardiovascular mortality over long-term follow-up.
Vitamin D and Cardiac Structure and Function
Vitamin D can affect cardiac structure and function via its effects on the RAAS system, cardiac myocytes and vascular calcification [53, 54].
In the CKD population, observational studies have reported an association between vitamin D and LVH in both pediatric and adult patients. Patange et al. in a small cross-sectional study of 34 children with CKD (20 on dialysis and 14 with pre-dialysis CKD) explored the relationship between various parameters of calcium-phosphorus metabolism including 25(OH)D and cardiovascular structure and function [55]. Pearson’s correlation analysis showed that increased LVMI was negatively correlated with 25(OH)D (r = –0.54; p <0.05) and GFR (r = −0.31; p <0.05). A positive correlation was observed with systolic blood pressure (r = 0.36; p <0.05). Multiple regression analysis showed that low 25(OH)D and systolic hypertension were the only independent predictors of increased LVMI in children with CKD.
In the Hoorn Study, a population-based cohort from Netherland, low serum 25(OH)D levels were only associated with higher LVMI at 8-year follow-up in subjects without prior cardiovascular disease and median estimated GFR ≤77.5 ml/min/1.73m2. This association attenuated after adjustments for parathyroid hormone [56].
One of the earliest intervention studies treated 15 adult patients undergoing hemodialysis with intravenous calcitriol over 15 weeks. It showed reduced interventricular wall thickness (13.9±3.6 mm vs.12.8±3.1 mm; P=0.01), left ventricular posterior wall thickness (12.5±2.4 mm vs. 11.3±1.8 mm; P=0.05), and LVMI (178±73 g/m2 vs. 155±61 g/m2; P=0.01). Serum levels of atrial natriuretic peptide and angiotensin II were also reduced after calcitriol treatment [57].
However, more recent larger randomized control trials have failed to show any benefit of active vitamin D analogues on cardiac structure and function. In the PRIMO study, a double-blind, randomized placebo-controlled trial of 227 patients with CKD, mild to moderate LVH, and preserved left ventricular ejection fraction, participants were randomly assigned to receive oral paricalcitol, 2 μg/d (n=115), or matching placebo (n=112). Change in LVMI was assessed over 48 weeks by cardiac magnetic resonance imaging. Secondary end-points included echocardiographic changes in left ventricular diastolic function. Treatment with paricalcitol reduced parathyroid hormone levels within 4 weeks and maintained levels within the normal range throughout the study duration. At 48 weeks, the change in LVMI did not differ between the two groups. Doppler measures of diastolic function also did not differ. However, paricalcitol did decrease the number of cardiovascular hospitalizations [52]. Similarly, the OPERA study, a prospective, double-blind, randomized, placebo-controlled trial to determine whether 52 weeks of 1 μg oral paricalcitol reduces left ventricular mass in patients with stages 3–5 CKD with LVH did not show any decrease in LVMI, left ventricular volume and ejection fraction, but did show a decrease in the number of cardiovascular-related hospitalizations compared with placebo [58].
A post hoc analysis of data from the PRIMO study showed a significant decrease in left atrial volume index (LAVi, an indicator of diastolic dysfunction) in the paricalcitol group compared with the placebo, despite similar blood pressure control and RAAS inhibitor use. There was a synergistic effect between RAAS inhibitors and paricalcitol with the greatest decline in LAVi seen in patients receiving both medications. LAVi continued to improve in weeks 24 to 48 of the study, suggesting that longer therapy might be of further benefit. Brain natriuretic peptide (BNP), a marker for heart failure, was also evaluated. BNP levels increased throughout the study in both groups, however the rise was attenuated in the paricalcitol group. The change in LAVi correlated with log transformed BNP change. Limitations of this study include potential for false positive results due to the post hoc analysis, exclusion of patients with severe CKD, severe LVH or left ventricular dysfunction and the small number of cardiovascular events which precluded the evaluation of any benefits of LAVi reduction on hard outcomes like heart failure [59].
In pediatric CKD patients there is a significant burden of hypertension and LVH. The Cardiovascular Comorbidity in Children with CKD Study (4 C) is a multicenter, prospective, observational study in children aged 6–17 years old with initial GFR of 1060 ml/min/1.73 m2 in Europe. This study showed that at baseline 26.1% of children had uncontrolled hypertension (24-hour ambulatory blood pressure monitoring; n=545), and the prevalence increased from 24.4% in CKD stage 3, to 47.4% in CKD stage 5. The prevalence of LVH was higher with each CKD stage, from 10.6% in CKD stage 3a to 48% in CKD stage 5 [60]. In the CKiD cohort study, 1 year after study entry (n=332), only half of the subjects had a normal ambulatory blood pressure monitoring. Blood pressure load was elevated (>25%) in 52% (n=172), while mean blood pressure was elevated in 32% (n=105) [61]. At baseline, 17% of children had LVH (11% eccentric and 6% concentric) and 9% had concentric remodeling of the left ventricle [62].
Given the above reports, apart from effective control of hypertension, other treatments, such as vitamin D analogues, also need to be evaluated in children with advanced CKD. The effects of vitamin D on FGF23 and in turn LVH also need to be delineated, as studies have shown increases in FGF23 levels with vitamin D supplementation [63].
Vitamin D and Vascular dysfunction in CKD
Vascular dysfunction in CKD includes a combination of endothelial dysfunction, medial arterial calcification and intimal thickening. Progressive vascular calcifications are linked to altered bone and mineral metabolism. Changes in vessels are assessed by measuring carotid artery intima-media thickness (cIMT) and pulse wave velocity that determine loss of compliance or stiffness.
Inflammation and endothelium:
The endothelium is a single vessel layer between blood and the vascular supply to tissues. It is responsible for regulating vascular tone (vasoconstriction vs. vasodilation), angiogenesis, smooth muscle cell proliferation, inflammation and wound healing. The endothelial cells also activate 25(OH)D to 1,25(OH)2D which has autocrine, paracrine, and endocrine effects, particularly on vascular tone, preventing vascular inflammation and oxidative stress [64–67].
Endothelial dysfunction can be detected even at early stages of CKD. The Hoorn study revealed that it independently contributed to a higher cardiovascular mortality [68]. Methods to assess endothelial dysfunction include functional response to ischemia, Flow-mediated vasodilation (FMD) and measurement of certain biomarkers released during endothelial injury, e.g. ICAM, VCAM, E-selectin and von Willebrand factor [69–73]. However, these markers only partially reflect the complex nature of endothelial dysfunction. They do not encompass in entirety the impaired nitric oxide synthesis in patients with decreased renal function [74].
In a randomized, double-blind, placebo-controlled trial, the effect of cholecalciferol supplementation on vascular function in 120 adult patients with nondiabetic CKD stage 3–4 and 25(OH)D levels ≤20 ng/ml was evaluated. Patients were randomized to either two directly observed oral doses of cholecalciferol (300,000 IU) or matching placebo at baseline and 8 weeks. The primary outcome was change in endothelium-dependent brachial artery flow-mediated dilation at 16 weeks. Secondary outcome measures included changes in pulse wave velocity and circulating biomarkers. Cholecalciferol supplementation significantly increased endothelium-dependent brachial artery flow-mediated dilation at 16 weeks, whereas placebo did not (between-group difference in mean change: 5.49%; 95% CI, 4.34% to 6.64%; P <0.001). Intervention also led to significant favorable changes in pulse wave velocity and circulating IL-6 levels [75].
In the PENNY study, a double-blind randomized controlled trial, paricalcitol (2 μg/day) was given to 88 patients with stage 3–4 CKD for 12 weeks, and the effects on endothelium-dependent vasodilatation were studied. After 12 weeks of treatment, flow-mediated dilation rose in the paricalcitol but not in the placebo group, and the between-group difference in flow-mediated dilation changes was significant (1.8%, 95% CI, 0.33.1%, P=0.02), and the mean proportional change in flow-mediated dilation was 61% higher in paricalcitol-treated patients than in placebo-treated patients [76]. Another randomized clinical trial involving 60 patients with stage 3–4 CKD with type 2 diabetes found no improvement in FMD after 3 months of 1 μg paricalcitol treatment [77]. Similarly, a randomized clinical trial including 115 CKD patients given 6 months of oral cholecalciferol (2000 IU daily) or calcitriol (0.5mg daily) revealed no effect on FMD [78]. Supplementation with cholecalciferol 50,000 units once a week for 12 weeks in patients with CKD and 25(OH)D level <30 ng/ml, showed an increase in FMD after intervention, and decrease in soluble vascular cell adhesion molecule-1 (sVCAM-1) and sE-selectin [79].
Pharmacological interventions using vitamin D supplementation have shown variable effects on markers of endothelial dysfunction. The studies are difficult to compare due to varying inclusion criteria, e.g. enrollment of individuals with diabetes, varying cutoff for initial vitamin D levels (deficiency vs. insufficiency) and dosage/formulations of vitamin D used.
Atherogenesis
Increased inflammation and endothelial cell changes are implicated in the initiation of the atherothrombotic process, progressing to sub-endothelial low-density lipoprotein (LDL) accumulation, and chronic arterial wall inflammation with formation of a plaque [80, 81].
Epidemiologic studies revealed an inverse relationship between serum 25(OH)D levels and atherosclerotic changes in healthy individuals. According to the Framingham Offspring Study, there was a correlation between vitamin D deficiency and major adverse cardiovascular events. The Framingham Offspring Study included 1,739 participants (mean age 59 years; 55% women; all white) without prior cardiovascular disease. Individuals with 25(OH)D level <15 ng/mL had a multivariable-adjusted hazard ratio of 1.62 (95% confidence interval 1.11 to 2.36, P=0.01) for incident cardiovascular events compared with those with 25(OH)D ≥15 ng/mL. There was a graded increase in cardiovascular risk across categories of 25(OH)D, with multivariable-adjusted hazard ratios of 1.53 (95% CI1.00 to 2.36) for levels 10 to <15 ng/mL and 1.80 (95% CI1.05 to 3.08) for levels <10 ng/mL (P for linear trend=0.01) [82].
Carotid intima media thickness (cIMT) is a marker of large artery atherosclerosis and shown to be predictive of cardiovascular events [83]. A cross-sectional study involving 100 stage 3–4 CKD patients, however, showed no difference in common carotid artery intima-media thickness (CCA-IMT) between patients with and without 25(OH)D deficiency. It also showed no relationship or correlation between serum 25(OH)D levels and CCA-IMT or the presence of plaques [84]. Contrary to this, an observational study conducted in patients with more severe CKD (stage 4–5) reported an inverse association between serum 25(OH)D and CCA-IMT in CKD patients [85].
Data from the CKiD study showed that pediatric CKD patients had a 0.02 mm higher cIMT as compared to controls (P=0.03 for difference), and hypertension and dyslipidemia were significantly associated with the increased cIMT [32].
The effect of high dose cholecalciferol (300,000 units oral once) on vascular stiffness and endothelial dysfunction markers was compared between 41 children with CKD and 24 healthy controls. Comparisons were made with healthy children for LVH, cIMT, local arterial stiffness, and endothelium-dependent vasodilatation, C-reactive protein (CRP), fibrinogen, plasma concentrations of von Willebrand factor (vWf) and homocysteine levels. Children with CKD had higher LVMI and cIMT. Following cholecalciferol supplementation, a significant increase in FMD (p <0.001) and endothelium-independent FMD (p=0.004) was observed only in the CKD group. There was an increase in the distensibility coefficient and fall in the stiffness index [86].
Shroff et al. showed a bimodal association between 1,25(OH)2D levels and vascular disease in dialysis-dependent children [87]. 61 children on dialysis and 40 age-matched controls were included. Dialysis patients were prescribed daily oral 1-α hydroxyvitamin D3. Both cIMT and calcification scores showed a U-shaped distribution: patients with both low and high 1,25(OH)2D levels had significantly greater cIMT (P <0.0001) and calcification (P= 0.0002) than those with normal levels. 25(OH)D levels did not correlate with any vascular measure. The effects of 1,25(OH)2D on calcium-phosphate balance was thought to be responsible for this relationship. This study highlights the potential pitfalls of active vitamin D therapy and the possible increase in vascular calcifications as a potential adverse effect has to be monitored when designing trials in pediatric as well as adult CKD populations.
Vitamin D and Albuminuria
Albuminuria is an independent risk factor for increased cardiovascular morbidity and mortality [7]. There have been few randomized clinical trials in adult CKD patients that have examined the effect of vitamin D on proteinuria [88–90].
In the VITAL study described above there was a dose-dependent change in albumin/creatinine ratio, −3% (from 61 to 60 mg/mmol; 95% CI −16 to 13) in the placebo group; −16% (from 62 to 51 mg/mmol; −24 to −9) in the combined paricalcitol groups. Patients on 2 μg paricalcitol showed a reduction in albuminuria, ranging from −18% to 28% (p=0.014 vs placebo). Incidence of hypercalcaemia, adverse events, and serious adverse events was similar between groups receiving paricalcitol versus placebo [51].
These promising results need to be replicated in larger trials with longer follow up duration to assess both persistent efficacy as well as incidence of hypercalcemic adverse events that increase the risk for vascular calcifications.
Vitamin D and Inflammation
Chronic kidney disease is a state of low-grade inflammation and this is an important contributor to the increased cardiovascular risk seen in patients with CKD. Elevated levels of pro-inflammatory cytokines (CRP, IL-6, MCP-1 and TNF-α) are seen early in CKD [91, 92]. Low 25(OH)D and 1,25(OH)2D levels have been associated with higher cytokine levels in children and adults with pre-dialysis CKD and ESRD [27, 93]. Zehnder et al. measured vitamin D metabolites and markers of inflammation in 174 adult patients with CKD. Logistic regression analysis with urinary MCP-1 as binary outcome showed that a 10-unit increase in serum 1,25(OH)2D or 25(OH)D resulted in lower renal inflammation. Patients with acute renal inflammation had a significant increase in urinary and tissue MCP-1, macrophage infiltration, and macrophage and renal epithelial CYP27B1 expression, but significantly lower levels of serum 1,25(OH)2D in comparison to patients with chronic ischemic disease, despite similar levels of renal damage. In vitro, 1,25(OH)2D attenuated TNF α-induced MCP-1 expression by human proximal tubule cells [93].
Vitamin D supplementation studies in CKD and ESRD patients have shown a reduction in inflammatory cytokines in some but not all studies. 30 hemodialysis patients with iPTH levels of <300 pg/mL, not receiving any vitamin D therapy, and presenting with 25(OH)D levels of <30 ng/mL were prescribed cholecalciferol 50,000 IU once a week in the first 12 weeks and 20,000 IU in the last 12 weeks of the study. Inflammatory markers, such as high-sensitivity CRP, interleukin-6 and serum albumin, were evaluated. There was a significant reduction in high-sensitivity CRP levels after 3 months (median: 0.62 [0.05 to 29.6] mg/L vs. 0.32 [0.02 to 3.13] mg/L; P = 0.02) which persisted after 6 months (P=0.04) of cholecalciferol supplementation. Interleukin-6 levels also decreased (median: 6.44 pg/mL vs. 3.83 pg/mL; P = 0.018) after 6 months of supplementation [94].
A double-blind, randomized, placebo-controlled trial enrolled 46 adult subjects with early CKD (stages 2 and 3) and supplemented them with cholecalciferol (50000 IU weekly for 12 weeks followed by 50000 IU every other week for 40 weeks) or a matching placebo for 1 year. Serum tumor necrosis factor-α, interleukin-6, monocyte chemo-attractant protein-1 (MCP-1), interferon gamma-induced protein-10 and neutrophil gelatinase-associated lipocalin were measured at baseline, 12 weeks and 1 year. By 12 weeks, serum MCP-1 decreased in the cholecalciferol group (66.2±2.5 to 60.8±2.6 pg/ml, group-by-time interaction P <0.02) but was not different from baseline at 1 year. Other markers of inflammation did not change. The authors speculated that inflammation in early stages of CKD may not be as pronounced as in dialysis patients and that may have resulted in the null results with respect to other markers of inflammation [95].
Alborzi et al. conducted a pilot trial in 24 adult patients with CKD stage 2 and 3 to evaluate the effects of active vitamin D on endothelial function, blood pressure, albuminuria and inflammation. Patients were randomly allocated equally to 3 groups to receive 0, 1, or 2 μg of paricalcitol orally for 1 month. At 1 month, the treatment: baseline ratio of high sensitivity CRP was 1.5 (95% CI: 1.1 to 2.1; P=0.02) with placebo, 0.8 (95% CI: 0.3 to 1.9; P=0.62) with a 1 μg dose, and 0.5 (95% CI: 0.3 to 0.9; P=0. 03) with a 2 μg dose of paricalcitol. At 1 month, the treatment: baseline ratio of 24-hour albumin excretion rate was 1.35 (95% CI: 1.08 to 1.69; P=0.01) with placebo, 0.52 (95% CI: 0.40 to 0.69; P<0.001) with a 1-μg dose, and 0.54 (95% CI: 0.35 to 0.83; P=0. 01) with a 2 μg dose (P<0.001 for between group changes). No differences were observed in iothalamate clearance, flow-mediated dilation (a measure of endothelial function), 24h ambulatory blood pressure, or PTH with treatment or upon washout. The limitations of this trial include the small sample size and short duration. All patients had low 25(OH)D levels in this study; whether nutritional vitamin D replacement could have also improved albuminuria or inflammation is not known [88].
The above studies seem to suggest that both inactive and active vitamin D supplementation may result in a decrease in inflammatory markers, especially in the ESRD population. Active vitamin D compounds may be of benefit in the earlier stages of CKD, although this needs to be evaluated in large, longer duration randomized controlled trials using different vitamin D receptor agonists for comparison.
Recommendations for vitamin D supplementation in Chronic Kidney Disease
In 2017, KDIGO published an update to clinical practice guidelines for Chronic Kidney Disease-Mineral Bone Disorder in children and adults and the European Society for Pediatric Nephrology published clinical practice guidelines for native and active vitamin D therapy in children with CKD stage 2–5 and on dialysis. Most of these guidelines are based on low quality of evidence and hence are not strongly and unequivocally recommended.
Both groups recommend measuring 25(OH)D levels and correcting deficiency to maintain levels greater than 30 ng/ml. In children with CKD Stages 2–3, native vitamin D supplements could be used for the prevention or treatment of secondary hyperparathyroidism. Active vitamin D therapy was recommended only for severe and progressive secondary hyperparathyroidism and to maintain normal serum calcium levels in children.
No recommendations were made with regards to the extra-skeletal actions of vitamin D. The guidelines recommended evaluating cardiovascular outcomes of PTH lowering strategies as an area of future clinical research.
We agree with the recommendation for measuring 25(OH)D levels in early CKD and correcting deficiency to maintain levels greater than 30 ng/ml, as this can prevent and delay the onset of secondary hyperparathyroidism. Care must be taken to avoid levels greater than 50 ng/ml. It is more challenging to make recommendations for active vitamin D supplementation as we have no consensus on optimal PTH levels to target in children with CKD. Even less is known about the extra-skeletal benefits of vitamin D in pediatric CKD, precluding any recommendations at this point.
Conclusions
In summary, multiple observational studies have shown strong associations between vitamin D deficiency in CKD and cardiovascular diseases. However, given the wide variations in the study designs of randomized clinical trials (i.e., sample size, geographical variation, patient population selection, duration of intervention, and formulation of vitamin D supplementation used) and lack of beneficial effects in some trials, it becomes challenging to make definitive recommendations about vitamin D use for the prevention and treatment of cardiovascular outcomes. As illustrated by the above review, there are no randomized trials in children that have evaluated the effects of vitamin D supplementation on cardiovascular outcomes. The somewhat discouraging results from some of the adult randomized clinical trials makes it even more challenging to study these outcomes systematically in children. However, given that children stand to gain most if cardiovascular risk is mitigated, it is imperative that effects of vitamin D treatment, both nutritional and active be evaluated in well-designed clinical trials. There are several possible adverse effects of vitamin D therapies that have to be kept in mind; primary ones being the risk of vascular calcifications with active vitamin D supplementation, increase in FGF23 levels due to inactive vitamin D supplementation and the possible adverse effects of inactive vitamin D supplementation on the lipid profile in CKD patients. There are several large-scale randomized clinical trials currently being conducted (clinicaltrial.gov) in adult CKD patients that could provide more definitive answers about vitamin D and its role in decreasing the cardiovascular burden in CKD patients.
Table I.
Summary of the intervention studies of inactive and active vitamin D supplementation
| Author/(reference #) | Subjects | Study type | Vitamin D Intervention | Outcome evaluated | Results |
|---|---|---|---|---|---|
| Witham, MD et al. (46) | Non CKD adults | Meta-analysis of 11 RCTs | -Inactivated -Active -UVB radiation |
-Office BP -Ambulatory BP |
-Decrease in DBP -Greater decrease with inactivated vitamin D |
| Wu, SH et al. (47) | Normotensive and hypertensive non CKD adults | Meta analysis of 4 RCTs | -Cholecalciferol | -Change in SBP and DBP | -Decrease in SBP -No decrease in DBP |
| Beveridge, LA et al. (48) |
Non CKD adults | Meta analysis of 46 RCTS | -Inactive -Active |
-Change in SBP and DBP | -No effect |
| Mak, RH et al. (49) | Pediatric hemodialysis patients & healthy controls | Clinical trial | -IV calcitriol | -Change is BP -Change in insulin sensitivity |
-Decrease in mean arterial BP -Increase in insulin sensitivity |
| de Zeeuw, D et al. (51) | Adult diabetic CKD patients | RCT | -Paricalcitol | -BP -Albuminuria |
-Decrease in BP -Decrease in albuminuria |
| Thadani, R et al. (52) | Adult CKD patients | RCT | -Paricalcitol | -LVMI -BP |
-No change in LVMI -No change in BP -Decrease in left atrial volume index -Decrease in cardiovascular hospitalizations |
| Park, CW et al. (57) | Adult hemodialysis patients | Clinical trial | -IV calcitriol | -myocardial hypertrophy | Decrease in LVMI, LV posterior wall and interventricular wall thickness |
| Wang, AY et al. (58) | Adult CKD patients | RCT | -Paricalcitol | -LVMI | -No change in LVMI -Decrease in cardiovascular hospitalizations |
| Lerch, C et al. (63) | Pediatric CKD patients | Post-hoc analysis of an RCT and observational study | -ergocalciferol -cholecalciferol |
-sclerostin -Klotho -FGF23 |
-normalization of Klotho and Sclerostin -increase in FGF23 |
| Kumar, V et al. (75) | Adult non diabetic CKD | RCT | -cholecalciferol | -flow mediated dilation (FMD) | -increase in FMD |
| patients | -pulse wave velocity -IL-6 | -decrease in PWV -decrease in IL-6 levels |
|||
| Zoccali, C et al. (76) | Adult stage 3–4 CKD | RCT | -Paricalcitol | -FMD | -Improve in endothelium dependent FMD |
| Thethi, TK et al. (77) | Adult stage 3–4 CKD patients with diabetes | RCT | -Paricalcitol | -FMD | -no change in FMD |
| Kendrick, J et al. (78) | Adult CKD patients | RCT | -Cholecalciferol -Calcitriol |
-FMD | -No change in FMD |
| Zhang, Q et al. (79) | Adult CKD patients | RCT | -Cholecalciferol | -FMD -soluble vascular adhesion molecule-1 (sVCAM-1) -soluble Eselectin (sES) |
-increase in FMD -decrease in sVCAM and sES |
| Aytac, MB et al. (86) | Pediatric CKD patients | Intervention study with healthy controls | -Cholecalciferol | -cIMT -LVH -FMD homocysteine level |
-increase in FMD -decrease in homocysteine -no change in cIMT and LVH |
| Alborzi, P et al. (88) Agarwal, R et al. (89) Fishbane, S et al. (90) |
Adult CKD patients | RCTs | -Paricalcitol | -FMD -hsCRP -Albuminuria |
-increase in FMD -decrease in hsCRP and albuminuria |
| Bucharels, S (94) | Adult hemodialysis | Prospective interventional study | -Cholecalciferol | -hsCRP, IL-6 -LVH |
-decrease in LVH, IL-6 and hsCRP |
| Alvarez, JA (95) | Adult CKD stage 2, 3 | RCT | -Cholecalciferol | -TNF-α, IL-6, MCP-1, NGAL, IP-10 |
-decrease in MCP-1 -no change in others |
Key points.
Inadequate vitamin D levels (<30 ng/ml) are highly prevalent in the adult and pediatric chronic kidney disease populations
Vitamin D deficiency is associated with hypertension, diabetes, proteinuria cardiac dysfunction and dyslipidemia
Low vitamin D levels upregulate the renin-angiotensin-aldosterone system, increase inflammation and cause endothelial dysfunction leading to higher cardiovascular risk
Clinical trials and meta-analyses data in adults have failed to show a benefit of vitamin D therapy on cardiovascular outcomes
Lack of randomized clinical trials and high quality evidence in the pediatric CKD population make it difficult to recommend use of vitamin D therapy for reduction of cardiovascular disease burden
Questions.
- The following are important determinants of 25(OH)D levels in patients with chronic kidney disease, EXCEPT
- age
- nutritional vitamin D supplement use
- gender
- proteinuria
- race
- 1,25 dihydroxyvitamin D levels in CKD are regulated by which one of the following:
- FGF23
- Klotho
- Sclerostin
- Osteopontin
- The production of 24-hydroxylase enzyme which inactivates both 25(OH)D and 1,25(OH)2D is induced most strongly by:
- 25(OH)D
- FGF23
- PTH
- 1,25(OH)2D
- A bimodal association is seen between 1,25 dihydroxy vitamin D and which of the following:
- Left ventricular mass index
- Pulse wave velocity
- Flow mediated dilation
- Fibrinogen
- Carotid intima media thickness
- In adult clinical trials, paricalcitol, a vitamin D receptor agonist has been shown to do all of the following, EXCEPT:
- Decrease proteinuria
- Decrease markers of inflammation (CRP)
- Decrease left ventricular mass index
- Decrease cardiovascular-related hospitalizations
Answers:
c
a
d
e
c
Acknowledgements
J.K. is funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01 HD009115) and Weill Cornell CTSC Pilot grant UL1-TR-002348.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281 [DOI] [PubMed] [Google Scholar]
- 2.Dusso AS, Brown AJ, Slatopolsky E (2005) Vitamin D. Am J Physiol Renal Physiol 289:F8–28 [DOI] [PubMed] [Google Scholar]
- 3.Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, Durazo-Arvizu RA, Gallagher JC, Gallo RL, Jones G, Kovacs CS, Mayne ST, Rosen CJ, Shapses SA (2011) The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab 96:53–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hajhosseiny R, Khavandi K, Goldsmith DJ (2013) Cardiovascular disease in chronic kidney disease: untying the Gordian knot. Int J Clin Pract 67:14–31 [DOI] [PubMed] [Google Scholar]
- 5.McCullough PA, Steigerwalt S, Tolia K, Chen SC, Li S, Norris KC, WhaleyConnell A (2011) Cardiovascular disease in chronic kidney disease: data from the Kidney Early Evaluation Program (KEEP). Curr Diab Rep 11:47–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hemmelgarn BR, Clement F, Manns BJ, Klarenbach S, James MT, Ravani P, Pannu N, Ahmed SB, MacRae J, Scott-Douglas N, Jindal K, Quinn R, Culleton BF, Wiebe N, Krause R, Thorlacius L, Tonelli M (2009) Overview of the Alberta Kidney Disease Network. BMC Nephrol 10:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, Coresh J, Gansevoort RT (2010) Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 375:2073–2081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van der Velde M, Matsushita K, Coresh J, Astor BC, Woodward M, Levey A, de Jong P, Gansevoort RT, Levey AS, de Jong PE, El-Nahas M, Eckardt KU, Kasiske BL, Ninomiya T, Chalmers J, Macmahon S, Tonelli M, Hemmelgarn B, Sacks F, Curhan G, Collins AJ, Li S, Chen SC, Hawaii Cohort KP, Lee BJ, Ishani A, Neaton J, Svendsen K, Mann JF, Yusuf S, Teo KK, Gao P, Nelson RG, Knowler WC, Bilo HJ, Joosten H, Kleefstra N, Groenier KH, Auguste P, Veldhuis K, Wang Y, Camarata L, Thomas B, Manley T (2011) Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality. A collaborative meta-analysis of high-risk population cohorts. Kidney Int 79:1341–1352 [DOI] [PubMed] [Google Scholar]
- 9.Verstuyf A, Carmeliet G, Bouillon R, Mathieu C (2010) Vitamin D: a pleiotropic hormone. Kidney Int 78:140–145 [DOI] [PubMed] [Google Scholar]
- 10.Grant WB, Wimalawansa SJ, Holick MF, Cannell JJ, Pludowski P, Lappe JM, Pittaway M, May P (2015) Emphasizing the health benefits of vitamin D for those with neurodevelopmental disorders and intellectual disabilities. Nutrients 7:1538–1564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wimalawansa SJ (2012) Vitamin D in the new millennium. Curr Osteoporos Rep 10:4–15 [DOI] [PubMed] [Google Scholar]
- 12.Holick MF, Frommer JE, McNeill SC, Richtand NM, Henley JW, Potts JT, Jr., (1977) Photometabolism of 7-dehydrocholesterol to previtamin D3 in skin. Biochem Biophys Res Commun 76:107–114 [DOI] [PubMed] [Google Scholar]
- 13.Pike JW, Meyer MB (2010) The Vitamin D Receptor: New Paradigms for the Regulation of Gene Expression by 1,25-Dihydroxyvitamin D(3). Endocrinol Metab Clin North Am 39:255–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nair R, Maseeh A (2012) Vitamin D: The “sunshine” vitamin. J Pharmacol Pharmacother 3:118–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu S, Tang W, Zhou J, Stubbs JR, Luo Q, Pi M, Quarles LD (2006) Fibroblast growth factor 23 is a counter-regulatory phosphaturic hormone for vitamin D. J Am Soc Nephrol 17:1305–1315 [DOI] [PubMed] [Google Scholar]
- 16.Yu X, White KE (2005) FGF23 and disorders of phosphate homeostasis. Cytokine Growth Factor Rev 16:221–232 [DOI] [PubMed] [Google Scholar]
- 17.Wali RK, Kong J, Sitrin MD, Bissonnette M, Li YC (2003) Vitamin D receptor is not required for the rapid actions of 1,25-dihydroxyvitamin D3 to increase intracellular calcium and activate protein kinase C in mouse osteoblasts. J Cell Biochem 88:794–801 [DOI] [PubMed] [Google Scholar]
- 18.Haussler MR, Jurutka PW, Mizwicki M, Norman AW (2011) Vitamin D receptor (VDR)-mediated actions of 1alpha,25(OH)(2)vitamin D(3): genomic and nongenomic mechanisms. Best Pract Res Clin Endocrinol Metab 25:543–559 [DOI] [PubMed] [Google Scholar]
- 19.Heaney RP, Holick MF (2011) Why the IOM recommendations for vitamin D are deficient. J Bone Miner Res 26:455–457 [DOI] [PubMed] [Google Scholar]
- 20.Bischoff-Ferrari HA, Willett WC, Wong JB, Giovannucci E, Dietrich T, Dawson-Hughes B (2005) Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA 293:2257–2264 [DOI] [PubMed] [Google Scholar]
- 21.Bischoff-Ferrari HA, Willett WC, Wong JB, Stuck AE, Staehelin HB, Orav EJ, Thoma A, Kiel DP, Henschkowski J (2009) Prevention of nonvertebral fractures with oral vitamin D and dose dependency: a meta-analysis of randomized controlled trials. Arch Intern Med 169:551–561 [DOI] [PubMed] [Google Scholar]
- 22.Priemel M, von Domarus C, Klatte TO, Kessler S, Schlie J, Meier S, Proksch N, Pastor F, Netter C, Streichert T, Puschel K, Amling M (2010) Bone mineralization defects and vitamin D deficiency: histomorphometric analysis of iliac crest bone biopsies and circulating 25-hydroxyvitamin D in 675 patients. J Bone Miner Res 25:305–312 [DOI] [PubMed] [Google Scholar]
- 23.Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM (2011) Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96:1911–1930 [DOI] [PubMed] [Google Scholar]
- 24.Kumar J, Muntner P, Kaskel FJ, Hailpern SM, Melamed ML (2009) Prevalence and associations of 25-hydroxyvitamin D deficiency in US children: NHANES 2001–2004. Pediatrics 124:e362–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kumar J, McDermott K, Abraham AG, Friedman LA, Johnson VL, Kaskel FJ, Furth SL, Warady BA, Portale AA, Melamed ML (2016) Prevalence and correlates of 25-hydroxyvitamin D deficiency in the Chronic Kidney Disease in Children (CKiD) cohort. Pediatr Nephrol 31:121–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Seeherunvong W, Abitbol CL, Chandar J, Zilleruelo G, Freundlich M (2009) Vitamin D insufficiency and deficiency in children with early chronic kidney disease. J Pediatr 154:906–911 e901 [DOI] [PubMed] [Google Scholar]
- 27.Kalkwarf HJ, Denburg MR, Strife CF, Zemel BS, Foerster DL, Wetzsteon RJ, Leonard MB (2012) Vitamin D deficiency is common in children and adolescents with chronic kidney disease. Kidney Int 81:690–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.(2017) U.S. Renal Data System, USRDS 2017 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States.
- 29.Mitsnefes MM (2005) Cardiovascular disease in children with chronic kidney disease. Adv Chronic Kidney Dis 12:397–405 [DOI] [PubMed] [Google Scholar]
- 30.Mitsnefes MM, Kimball TR, Kartal J, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2005) Cardiac and vascular adaptation in pediatric patients with chronic kidney disease: role of calcium-phosphorus metabolism. J Am Soc Nephrol 16:2796–2803 [DOI] [PubMed] [Google Scholar]
- 31.Shroff R, Weaver DJ, Jr., Mitsnefes MM (2011) Cardiovascular complications in children with chronic kidney disease. Nat Rev Nephrol 7:642–649 [DOI] [PubMed] [Google Scholar]
- 32.Brady TM, Schneider MF, Flynn JT, Cox C, Samuels J, Saland J, White CT, Furth S, Warady BA, Mitsnefes M (2012) Carotid intima-media thickness in children with CKD: results from the CKiD study. Clin J Am Soc Nephrol 7:1930–1937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reis JP, von Muhlen D, Miller ER, 3rd, Michos ED, Appel LJ (2009) Vitamin D status and cardiometabolic risk factors in the United States adolescent population. Pediatrics 124:e371–379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martins D, Wolf M, Pan D, Zadshir A, Tareen N, Thadhani R, Felsenfeld A, Levine B, Mehrotra R, Norris K (2007) Prevalence of cardiovascular risk factors and the serum levels of 25-hydroxyvitamin D in the United States: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med 167:1159–1165 [DOI] [PubMed] [Google Scholar]
- 35.Drechsler C, Pilz S, Obermayer-Pietsch B, Verduijn M, Tomaschitz A, Krane V, Espe K, Dekker F, Brandenburg V, Marz W, Ritz E, Wanner C (2010) Vitamin D deficiency is associated with sudden cardiac death, combined cardiovascular events, and mortality in haemodialysis patients. Eur Heart J 31:2253–2261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Boer IH, Kestenbaum B, Shoben AB, Michos ED, Sarnak MJ, Siscovick DS (2009) 25-hydroxyvitamin D levels inversely associate with risk for developing coronary artery calcification. J Am Soc Nephrol 20:1805–1812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abajo M, Betriu A, Arroyo D, Gracia M, Del Pino MD, Martinez I, Valdivielso JM, Fernandez E (2017) Mineral metabolism factors predict accelerated progression of common carotid intima-media thickness in chronic kidney disease: the NEFRONA study. Nephrol Dial Transplant 32:1882–1891 [DOI] [PubMed] [Google Scholar]
- 38.Li YC, Kong J, Wei M, Chen ZF, Liu SQ, Cao LP (2002) 1,25-Dihydroxyvitamin D(3) is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest 110:229–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cardus A, Parisi E, Gallego C, Aldea M, Fernandez E, Valdivielso JM (2006) 1,25-Dihydroxyvitamin D3 stimulates vascular smooth muscle cell proliferation through a VEGF-mediated pathway. Kidney Int 69:1377–1384 [DOI] [PubMed] [Google Scholar]
- 40.Zittermann A, Koerfer R (2008) Protective and toxic effects of vitamin D on vascular calcification: clinical implications. Mol Aspects Med 29:423–432 [DOI] [PubMed] [Google Scholar]
- 41.Zittermann A, Koerfer R (2008) Vitamin D in the prevention and treatment of coronary heart disease. Curr Opin Clin Nutr Metab Care 11:752–757 [DOI] [PubMed] [Google Scholar]
- 42.Carthy EP, Yamashita W, Hsu A, Ooi BS (1989) 1,25-Dihydroxyvitamin D3 and rat vascular smooth muscle cell growth. Hypertension 13:954–959 [DOI] [PubMed] [Google Scholar]
- 43.Weng S, Sprague JE, Oh J, Riek AE, Chin K, Garcia M, Bernal-Mizrachi C (2013) Vitamin D deficiency induces high blood pressure and accelerates atherosclerosis in mice. PLoS One 8:e54625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wong MS, Delansorne R, Man RY, Vanhoutte PM (2008) Vitamin D derivatives acutely reduce endothelium-dependent contractions in the aorta of the spontaneously hypertensive rat. Am J Physiol Heart Circ Physiol 295:H289–296 [DOI] [PubMed] [Google Scholar]
- 45.Ke L, Mason RS, Kariuki M, Mpofu E, Brock KE (2015) Vitamin D status and hypertension: a review. Integr Blood Press Control 8:13–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Witham MD, Nadir MA, Struthers AD (2009) Effect of vitamin D on blood pressure: a systematic review and meta-analysis. J Hypertens 27:1948–1954 [DOI] [PubMed] [Google Scholar]
- 47.Wu SH, Ho SC, Zhong L (2010) Effects of vitamin D supplementation on blood pressure. South Med J 103:729–737 [DOI] [PubMed] [Google Scholar]
- 48.Beveridge LA, Struthers AD, Khan F, Jorde R, Scragg R, Macdonald HM, Alvarez JA, Boxer RS, Dalbeni A, Gepner AD, Isbel NM, Larsen T, Nagpal J, Petchey WG, Stricker H, Strobel F, Tangpricha V, Toxqui L, Vaquero MP, Wamberg L, Zittermann A, Witham MD (2015) Effect of Vitamin D Supplementation on Blood Pressure: A Systematic Review and Meta-analysis Incorporating Individual Patient Data. JAMA Intern Med 175:745–754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mak RH (1992) Amelioration of hypertension and insulin resistance by 1,25dihydroxycholecalciferol in hemodialysis patients. Pediatr Nephrol 6:345–348 [DOI] [PubMed] [Google Scholar]
- 50.Shroff R, Aitkenhead H, Costa N, Trivelli A, Litwin M, Picca S, Anarat A, Sallay P, Ozaltin F, Zurowska A, Jankauskiene A, Montini G, Charbit M, Schaefer F, Wuhl E (2016) Normal 25-Hydroxyvitamin D Levels Are Associated with Less Proteinuria and Attenuate Renal Failure Progression in Children with CKD. J Am Soc Nephrol 27:314–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.de Zeeuw D, Agarwal R, Amdahl M, Audhya P, Coyne D, Garimella T, Parving HH, Pritchett Y, Remuzzi G, Ritz E, Andress D (2010) Selective vitamin D receptor activation with paricalcitol for reduction of albuminuria in patients with type 2 diabetes (VITAL study): a randomised controlled trial. Lancet 376:1543–1551 [DOI] [PubMed] [Google Scholar]
- 52.Thadhani R, Appelbaum E, Pritchett Y, Chang Y, Wenger J, Tamez H, Bhan I, Agarwal R, Zoccali C, Wanner C, Lloyd-Jones D, Cannata J, Thompson BT, Andress D, Zhang W, Packham D, Singh B, Zehnder D, Shah A, Pachika A, Manning WJ, Solomon SD (2012) Vitamin D therapy and cardiac structure and function in patients with chronic kidney disease: the PRIMO randomized controlled trial. JAMA 307:674–684 [DOI] [PubMed] [Google Scholar]
- 53.O’Connell TD, Berry JE, Jarvis AK, Somerman MJ, Simpson RU (1997) 1,25Dihydroxyvitamin D3 regulation of cardiac myocyte proliferation and hypertrophy. Am J Physiol 272:H1751–1758 [DOI] [PubMed] [Google Scholar]
- 54.Simpson RU, Hershey SH, Nibbelink KA (2007) Characterization of heart size and blood pressure in the vitamin D receptor knockout mouse. J Steroid Biochem Mol Biol 103:521–524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Patange AR, Valentini RP, Gothe MP, Du W, Pettersen MD (2013) Vitamin D deficiency is associated with increased left ventricular mass and diastolic dysfunction in children with chronic kidney disease. Pediatr Cardiol 34:536–542 [DOI] [PubMed] [Google Scholar]
- 56.van Ballegooijen AJ, Snijder MB, Visser M, van den Hurk K, Kamp O, Dekker JM, Nijpels G, Stehouwer CD, Henry RM, Paulus WJ, Brouwer IA (2012) Vitamin D in relation to myocardial structure and function after eight years of follow-up: the Hoorn study. Ann Nutr Metab 60:69–77 [DOI] [PubMed] [Google Scholar]
- 57.Park CW, Oh YS, Shin YS, Kim CM, Kim YS, Kim SY, Choi EJ, Chang YS, Bang BK (1999) Intravenous calcitriol regresses myocardial hypertrophy in hemodialysis patients with secondary hyperparathyroidism. Am J Kidney Dis 33:73–81 [DOI] [PubMed] [Google Scholar]
- 58.Wang AY, Fang F, Chan J, Wen YY, Qing S, Chan IH, Lo G, Lai KN, Lo WK, Lam CW, Yu CM (2014) Effect of paricalcitol on left ventricular mass and function in CKD--the OPERA trial. J Am Soc Nephrol 25:175–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tamez H, Zoccali C, Packham D, Wenger J, Bhan I, Appelbaum E, Pritchett Y, Chang Y, Agarwal R, Wanner C, Lloyd-Jones D, Cannata J, Thompson BT, Andress D, Zhang W, Singh B, Zehnder D, Pachika A, Manning WJ, Shah A, Solomon SD, Thadhani R (2012) Vitamin D reduces left atrial volume in patients with left ventricular hypertrophy and chronic kidney disease. Am Heart J 164:902–909.e902 [DOI] [PubMed] [Google Scholar]
- 60.Schaefer F, Doyon A, Azukaitis K, Bayazit A, Canpolat N, Duzova A, Niemirska A, Sozeri B, Thurn D, Anarat A, Ranchin B, Litwin M, Caliskan S, Candan C, Baskin E, Yilmaz E, Mir S, Kirchner M, Sander A, Haffner D, Melk A, Wuhl E, Shroff R, Querfeld U (2017) Cardiovascular Phenotypes in Children with CKD: The 4C Study. Clin J Am Soc Nephrol 12:19–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Samuels J, Ng D, Flynn JT, Mitsnefes M, Poffenbarger T, Warady BA, Furth S (2012) Ambulatory blood pressure patterns in children with chronic kidney disease. Hypertension 60:43–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mitsnefes M, Flynn J, Cohn S, Samuels J, Blydt-Hansen T, Saland J, Kimball T, Furth S, Warady B (2010) Masked hypertension associates with left ventricular hypertrophy in children with CKD. J Am Soc Nephrol 21:137–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lerch C, Shroff R, Wan M, Rees L, Aitkenhead H, Kaplan Bulut I, Thurn D, Karabay Bayazit A, Niemirska A, Canpolat N, Duzova A, Azukaitis K, Yilmaz E, Yalcinkaya F, Harambat J, Kiyak A, Alpay H, Habbig S, Zaloszyc A, Soylemezoglu O, Candan C, Rosales A, Melk A, Querfeld U, Leifheit-Nestler M, Sander A, Schaefer F, Haffner D; 4C study consortium; ESPN CKD-MBD working group (2018) Effects of nutritional vitamin D supplementation on markers of bone and mineral metabolism in children with chronic kidney disease. Nephrol Dial Transplant. DOI: 10.1093/ndt/gfy012 [DOI] [PubMed] [Google Scholar]
- 64.Apetrii M, Covic A (2016) Vitamin D and Endothelial Function in Chronic Kidney Disease In: Ureña Torres PA et al. (eds) Vitamin D in Chronic Kidney Disease Springer International Publishing, Switzerland: DOI 10.1007/978-3-319-32507-1_20(2) Vitamin D and Endothelial Function in Chronic Kidney Disease | Request PDF. Available from: https://www.researchgate.net/publication/308500307_Vitamin_D_and_Endothelial_Function_in_Chronic_Kidney_Disease [accessed Sept 13, 2018] [DOI] [Google Scholar]
- 65.Merke J, Milde P, Lewicka S, Hugel U, Klaus G, Mangelsdorf DJ, Haussler MR, Rauterberg EW, Ritz E (1989) Identification and regulation of 1,25dihydroxyvitamin D3 receptor activity and biosynthesis of 1,25-dihydroxyvitamin D3. Studies in cultured bovine aortic endothelial cells and human dermal capillaries. J Clin Invest 83:1903–1915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Molinari C, Uberti F, Grossini E, Vacca G, Carda S, Invernizzi M, Cisari C (2011) 1alpha,25-dihydroxycholecalciferol induces nitric oxide production in cultured endothelial cells. Cell Physiol Biochem 27:661–668 [DOI] [PubMed] [Google Scholar]
- 67.Zhong W, Gu B, Gu Y, Groome LJ, Sun J, Wang Y (2014) Activation of vitamin D receptor promotes VEGF and CuZn-SOD expression in endothelial cells. J Steroid Biochem Mol Biol 140:56–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Stam F, van Guldener C, Becker A, Dekker JM, Heine RJ, Bouter LM, Stehouwer CD (2006) Endothelial dysfunction contributes to renal function-associated cardiovascular mortality in a population with mild renal insufficiency: the Hoorn study. J Am Soc Nephrol 17:537–545 [DOI] [PubMed] [Google Scholar]
- 69.Deanfield J, Donald A, Ferri C, Giannattasio C, Halcox J, Halligan S, Lerman A, Mancia G, Oliver JJ, Pessina AC, Rizzoni D, Rossi GP, Salvetti A, Schiffrin EL, Taddei S, Webb DJ (2005) Endothelial function and dysfunction. Part I: Methodological issues for assessment in the different vascular beds: a statement by the Working Group on Endothelin and Endothelial Factors of the European Society of Hypertension. J Hypertens 23:7–17 [DOI] [PubMed] [Google Scholar]
- 70.Shechter M, Issachar A, Marai I, Koren-Morag N, Freinark D, Shahar Y, Shechter A, Feinberg MS (2009) Long-term association of brachial artery flow-mediated vasodilation and cardiovascular events in middle-aged subjects with no apparent heart disease. Int J Cardiol 134:52–58 [DOI] [PubMed] [Google Scholar]
- 71.Yeboah J, Crouse JR, Hsu FC, Burke GL, Herrington DM (2007) Brachial flow-mediated dilation predicts incident cardiovascular events in older adults: the Cardiovascular Health Study. Circulation 115:2390–2397 [DOI] [PubMed] [Google Scholar]
- 72.Yilmaz MI, Stenvinkel P, Sonmez A, Saglam M, Yaman H, Kilic S, Eyileten T, Caglar K, Oguz Y, Vural A, Cakar M, Altun B, Yenicesu M, Carrero JJ (2011) Vascular health, systemic inflammation and progressive reduction in kidney function; clinical determinants and impact on cardiovascular outcomes. Nephrol Dial Transplant 26:3537–3543 [DOI] [PubMed] [Google Scholar]
- 73.Zoccali C, Maio R, Tripepi G, Mallamaci F, Perticone F (2006) Inflammation as a mediator of the link between mild to moderate renal insufficiency and endothelial dysfunction in essential hypertension. J Am Soc Nephrol 17:S64–68 [DOI] [PubMed] [Google Scholar]
- 74.Wever R, Boer P, Hijmering M, Stroes E, Verhaar M, Kastelein J, Versluis K, Lagerwerf F, van Rijn H, Koomans H, Rabelink T (1999) Nitric oxide production is reduced in patients with chronic renal failure. Arterioscler Thromb Vasc Biol 19:1168–1172 [DOI] [PubMed] [Google Scholar]
- 75.Kumar V, Yadav AK, Lal A, Kumar V, Singhal M, Billot L, Gupta KL, Banerjee D, Jha V (2017) A Randomized Trial of Vitamin D Supplementation on Vascular Function in CKD. J Am Soc Nephrol 28:3100–3108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zoccali C, Curatola G, Panuccio V, Tripepi R, Pizzini P, Versace M, Bolignano D, Cutrupi S, Politi R, Tripepi G, Ghiadoni L, Thadhani R, Mallamaci F (2014) Paricalcitol and endothelial function in chronic kidney disease trial. Hypertension 64:1005–1011 [DOI] [PubMed] [Google Scholar]
- 77.Thethi TK, Bajwa MA, Ghanim H, Jo C, Weir M, Goldfine AB, Umpierrez G, Desouza C, Dandona P, Fang-Hollingsworth Y, Raghavan V, Fonseca VA (2015) Effect of paricalcitol on endothelial function and inflammation in type 2 diabetes and chronic kidney disease. J Diabetes Complications 29:433–437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kendrick J, Andrews E, You Z, Moreau K, Nowak KL, Farmer-Bailey H, Seals DR, Chonchol M (2017) Cholecalciferol, Calcitriol, and Vascular Function in CKD: A Randomized, Double-Blind Trial. Clin J Am Soc Nephrol 12:1438–1446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhang Q, Zhang M, Wang H, Sun C, Feng Y, Zhu W, Cao D, Shao Q, Li N, Xia Y, Tang T, Wan C, Liu J, Jin B, Zhao M, Jiang C (2018) Vitamin D supplementation improves endothelial dysfunction in patients with non-dialysis chronic kidney disease. Int Urol Nephrol 50:923–927 [DOI] [PubMed] [Google Scholar]
- 80.Libby P, Ridker PM, Hansson GK (2009) Inflammation in Atherosclerosis: From Pathophysiology to Practice. J Am Coll Cardiol 54:2129–2138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ross R (1999) Atherosclerosis--an inflammatory disease. N Engl J Med 340:115–126 [DOI] [PubMed] [Google Scholar]
- 82.Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E, Lanier K, Benjamin EJ, D’Agostino RB, Wolf M, Vasan RS (2008) Vitamin D deficiency and risk of cardiovascular disease. Circulation 117:503–511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE (1997) Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation 96:1432–1437 [DOI] [PubMed] [Google Scholar]
- 84.Ng YM, Lim SK, Kang PS, Kadir KA, Tai MS (2016) Association between serum 25-hydroxyvitamin D levels and carotid atherosclerosis in chronic kidney disease patients. BMC Nephrol 17:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Yadav AK, Banerjee D, Lal A, Jha V (2012) Vitamin D deficiency, CD4+CD28null cells and accelerated atherosclerosis in chronic kidney disease. Nephrology (Carlton) 17:575–581 [DOI] [PubMed] [Google Scholar]
- 86.Aytac MB, Deveci M, Bek K, Kayabey O, Ekinci Z (2016) Effect of cholecalciferol on local arterial stiffness and endothelial dysfunction in children with chronic kidney disease. Pediatr Nephrol 31:267–277 [DOI] [PubMed] [Google Scholar]
- 87.Shroff R, Egerton M, Bridel M, Shah V, Donald AE, Cole TJ, Hiorns MP, Deanfield JE, Rees L (2008) A bimodal association of vitamin D levels and vascular disease in children on dialysis. J Am Soc Nephrol 19:1239–1246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Alborzi P, Patel NA, Peterson C, Bills JE, Bekele DM, Bunaye Z, Light RP, Agarwal R (2008) Paricalcitol reduces albuminuria and inflammation in chronic kidney disease: a randomized double-blind pilot trial. Hypertension 52:249–255 [DOI] [PubMed] [Google Scholar]
- 89.Agarwal R, Acharya M, Tian J, Hippensteel RL, Melnick JZ, Qiu P, Williams L, Batlle D (2005) Antiproteinuric effect of oral paricalcitol in chronic kidney disease. Kidney Int 68:2823–2828 [DOI] [PubMed] [Google Scholar]
- 90.Fishbane S, Chittineni H, Packman M, Dutka P, Ali N, Durie N (2009) Oral paricalcitol in the treatment of patients with CKD and proteinuria: a randomized trial. Am J Kidney Dis 54:647–652 [DOI] [PubMed] [Google Scholar]
- 91.Munoz Mendoza J, Isakova T, Ricardo AC, Xie H, Navaneethan SD, Anderson AH, Bazzano LA, Xie D, Kretzler M, Nessel L, Hamm LL, Negrea L, Leonard MB, Raj D, Wolf M (2012) Fibroblast growth factor 23 and Inflammation in CKD. Clin J Am Soc Nephrol 7:1155–1162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Shlipak MG, Fried LF, Crump C, Bleyer AJ, Manolio TA, Tracy RP, Furberg CD, Psaty BM (2003) Elevations of inflammatory and procoagulant biomarkers in elderly persons with renal insufficiency. Circulation 107:87–92 [DOI] [PubMed] [Google Scholar]
- 93.Zehnder D, Quinkler M, Eardley KS, Bland R, Lepenies J, Hughes SV, Raymond NT, Howie AJ, Cockwell P, Stewart PM, Hewison M (2008) Reduction of the vitamin D hormonal system in kidney disease is associated with increased renal inflammation. Kidney Int 74:1343–1353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bucharles S, Barberato SH, Stinghen AE, Gruber B, Piekala L, Dambiski AC, Custodio MR, Pecoits-Filho R (2012) Impact of cholecalciferol treatment on biomarkers of inflammation and myocardial structure in hemodialysis patients without hyperparathyroidism. J Ren Nutr 22:284–291 [DOI] [PubMed] [Google Scholar]
- 95.Alvarez JA, Zughaier SM, Law J, Hao L, Wasse H, Ziegler TR, Tangpricha V (2013) Effects of high-dose cholecalciferol on serum markers of inflammation and immunity in patients with early chronic kidney disease. Eur J Clin Nutr 67:264–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Dusso AS, Tokumoto M (2011) Defective renal maintenance of the vitamin D endocrine system impairs vitamin D renoprotection: a downward spiral in kidney disease. Kidney Int 79:715–729 [DOI] [PubMed] [Google Scholar]