Abstract
Background
Childhood maltreatment is a transdiagnostic risk factor for later psychopathology and has been associated with altered brain circuitry involved in the processing of threat and safety. Examining threat generalization mechanisms in young adults with childhood maltreatment and psychiatric symptoms may elucidate a pathway linking early-life adversities to the presence of subclinical psychopathology
Methods
We recruited youth aged 16–25 years with subclinical psychiatric symptomatology and healthy controls. They were dichotomized into 2 groups: 1 with a high level of childhood maltreatment (n = 58) and 1 with no or a low level of childhood maltreatment (n = 55). Participants underwent a functional MRI threat generalization paradigm, measuring self-reported fear, expectancy of an unconditioned stimulus (US) and neural responses.
Results
We observed interactions between childhood maltreatment and threat generalization indices on subclinical symptom load. In individuals reporting high levels of childhood maltreatment, enhanced generalization in self-reported fear and US expectancy was related to higher levels of psychopathology. Imaging results revealed that in the group with high levels of childhood maltreatment, lower activation in the left hippocampus during threat generalization was associated with a higher symptom load. Associations between threat generalization and psychopathology were nonsignificant overall in the group with no or low levels of childhood maltreatment.
Limitations
The data were acquired in a cross-sectional manner, precluding definitive insight into the causality of childhood maltreatment, threat generalization and psychopathology.
Conclusion
Our results suggest that threat generalization mechanisms may moderate the link between childhood maltreatment and subclinical psychopathology during emerging adulthood. Threat generalization could represent a vulnerability factor for developing later psychopathology in individuals being exposed to childhood maltreatment.
Introduction
Children who experience maltreatment are at increased risk for developing psychopathology, including depression, anxiety and psychosis, later in life.1,2 These symptoms often emerge during adolescence and early adulthood3 and are thought to be relatively diffuse and nonspecific for any mental disorder in the early stages of expression.4,5 Childhood maltreatment has been shown to increase the likelihood of a mixture of these symptoms, rather than isolated symptoms.1 The mechanisms underlying the link between childhood maltreatment and this later expression of psychopathology during emerging adulthood, however, remain poorly understood.
Childhood maltreatment has been associated with alterations in threat- and safety-processing mechanisms. Several studies have shown that children or adults who were exposed to childhood maltreatment exhibit blunted physiological responses to threat and a reduced ability to differentiate between threat and safety during differential fear conditioning.6–8 These alterations could be the result of perturbations of neural networks important for threat and safety processing.9 Childhood maltreatment has indeed been linked to structural and functional alterations in several brain regions critical for threat–safety discrimination, including the ventromedial prefrontal cortex (vmPFC), dorsal anterior cingulate cortex (dACC), dorsolateral prefrontal cortex (dlPFC), amygdala, insula and hippocampus.10–13
Disruptions in threat processing and threat–safety discrimination have also been reported in various types of psychopathology. In fact, anxiety, depression and psychosis have all been associated with an attention bias to potential threats or ambiguous stimuli.14,15 In addition, these symptoms have also been associated with a cognitive bias to interpret neutral information as threatening or negatively valenced,16–18 which may be indicative of enhanced threat generalization or negative generalization. Recent research has investigated threat generalization experimentally, examining the transfer of the threat value of a conditioned threat stimulus (CS) to stimuli that resemble that CS. In several types of psychopathology, including generalized anxiety disorder (GAD), posttraumatic stress disorder (PTSD) and panic disorder,19–21 indications of enhanced threat generalization have been observed. By using a design containing several ambiguous stimuli along a continuum of similarity to a CS, neuroimaging studies in PTSD and GAD have additionally reported flatter or more gradual generalization gradients in several brain regions, including in the vmPFC, hippocampus, anterior insula and dACC.19,22 The dACC and anterior insula are known for their respective roles in the expression of fear responses23 and interoceptive awareness, 24 with increasing activation along the similarity continuum to the CS.25,26 The hippocampus and vmPFC have been implicated in stimulus discrimination and safety processing, 27,28 respectively, with decreasing activation along the similarity continuum.25,26 Overall, the results therefore seem to indicate reduced threat–safety discrimination on a neural level in patients with anxiety and PTSD.19,22 Furthermore, generalization gradients in the vmPFC have been associated with symptoms of both anxiety and depression in those with GAD.22 Psychosis has also been associated with aberrant neural responses to safety cues during fear conditioning, suggesting aberrant threat processing and threat–safety discrimination. 16,29 Furthermore, intolerance of uncertainty, a disposition affecting how individuals cope with uncertain situations, is predictive of threat generalization30 and is a risk factor for anxiety, depression and the experience of psychosis.31,32
Overall, work to date indicates that overgeneralization of threat or negative responding may confer a general vulnerability to psychopathology and that childhood maltreatment is associated with altered response to threat. Therefore, one may hypothesize that threat generalization may mediate the association between childhood maltreatment and psychopathology. Yet, an alternative model could be proposed in which threat generalization moderates the association between childhood maltreatment and psychopathology. Such a moderation model suggests that individuals who are exposed to childhood maltreatment and show enhanced threat generalization are at increased risk for psychopathology. Indeed, not all individuals experience negative consequences of childhood maltreatment exposure.33 Therefore, it is possible that reduced threat generalization, or better threat–safety discrimination, may actually confer resilience to the development of psychopathology. Experimental data have provided support for a moderating role of several processes, including reward-related processes and emotional-valence processing in the association of childhood maltreatment with PTSD and depression, respectively.34,35 In addition, stress reactivity has been shown to moderate the link between childhood maltreatment and an admixture of psychosis, depression and anxiety symptoms.36
Examining behavioural and neural threat-generalization mechanisms in young adults who experienced childhood maltreatment and are at an early stage of expressing psychopathology may elucidate either a pathway or a vulnerability factor, linking early-life adversities to the emergence of psychopathology during adolescence. Therefore, in the present study, we examined, to our knowledge for the first time, associations between childhood maltreatment, threat generalization and psychiatric symptoms during emerging adulthood. More specifically, using cross-sectional data as a first step, the study aimed to examine whether threat generalization mediates or moderates the association between childhood maltreatment and psychiatric symptoms in emerging adulthood. We hypothesized that threat generalization moderates the association between childhood maltreatment and psychiatric symptoms. In particular, we expected that individuals with higher levels of childhood maltreatment combined with enhanced threat generalization (i.e., more gradual generalization gradients in both self-report scores and in neural activation in the vmPFC, hippocampus, anterior insula and dACC) would report higher levels of psychopathology, whereas individuals with higher levels of childhood maltreatment combined with low threat generalization would report lower levels of psychopathology.
Methods
Participants
We recruited youth aged 16–25 years — the age at which psychopathology most often emerges3 — as part of a large randomized controlled trial investigating the effect of a psychological intervention on subclinical psychopathology (Dutch Trial Register number: NTR3808). They were recruited via posters in schools and public places and via advertisements in local news magazines. Participants with either no or low levels of psychopathology, or with subclinical depressive symptoms (Montgomery–Åsberg Depression Rating Scale [MADRS]37 ≥ 10) and/or subclinical psychotic experiences (Community Assessment Psychic Experiences [CAPE]38, positive distress subscale ≥ 2) were included. Exclusion criteria for the group with no or low levels of psychopathology were a history of psychiatric diagnosis or treatment, or a current DSM-IV axis I disorder as screened with the MINI International Neuropsychiatric Interview (MINI)39 For the group with subclinical depressive symptoms (MADRS ≥ 10) and/or subclinical psychotic experiences (CAPE, positive distress subscale ≥ 2), individuals with current psychiatric treatment or a significant need for care were excluded. For both groups, other exclusion criteria were lefthandedness, alcohol and substance dependence, current use of psychotropic drugs, a history of neurological disease, severe head trauma, organic brain disease and MRI contraindications. The Maastricht University Medical Centre ethics committee approved the study. All participants provided written informed consent; parental consent was additionally obtained for minors (age < 18 yr). We measured childhood maltreatment with the Childhood Trauma Questionnaire-short form (CTQ-SF).40 As childhood maltreatment scores were highly skewed, we used a median split procedure to categorize all participants into either the group with no/low levels of childhood maltreatment or the group with high levels of childhood maltreatment.41
Subclinical symptom load
We measured symptoms of anxiety, depression and psychotic experiences with the trait subscale of the State-Trait Anxiety Inventory (STAI),42 the MADRS and the Structured Interview for Schizotypy – Revised (SIS-R) – positive symptom scale,43 respectively. Scale scores were formed into a single composite subclinical symptom load score, because the questionnaire scores were strongly intercorrelated (all r > 0.53, all p < 0.001); the scores loaded on a single factor; and previous research has shown that childhood maltreatment increases the risk of an admixture of symptoms of anxiety, depression and psychosis rather than isolated symptoms.1 The subclinical symptom load was calculated as the average of z-transformed scale scores (see Appendix 1, available at jpn.ca/180053-a1 for further details).
Threat generalization neuroimaging task
Threat generalization was assessed using a validated functional MRI (fMRI) paradigm25 (adapted from Lissek and colleagues26), measuring both the affective expression (i.e., fear) and the cognitive expression of threat processing (i.e., expectancy of an aversive unconditioned stimulus [US]; US expectancy) as well as neural generalization responses (see Appendix 1, Fig. S1 for more details). Participants were presented 8 geometrical shapes, which were either rings or rectangles and a triangle. The largest and smallest rings/rectangle were the conditioned threat stimulus (CS+) and safety stimulus (CS−). The US, an electrical pulse, followed the CS+ in 6 of 12 occurences. A triangle served as a second CS− (vCS−) as a measure independent of perceptual generalization. The 5 intermediate-sized rings/rectangles served as generalization stimuli (GS); GS1 was perceptually most similar and GS5 was the least similar to the CS+. Behavioural outcome scores were online ratings of US expectancy obtained during the task phase and retrospective measures of fear, valence and arousal obtained after the task phase.
Statistical analysis
Behavioural data
Behavioural data were analyzed using SPSS version 23. Data were checked for normality and outliers. To test whether groups (no/low levels of childhood maltreatment, high levels of childhood maltreatment) differed in demographic characteristics (age, sex, education) and US intensity, we used independent samples t tests for continuous data and χ2 tests for categorical data. To confirm that childhood maltreatment groups differed in the CTQ-SF total score and subscales, we conducted nonparametric Mann–Whitney U tests. We considered results to be significant at p < 0.05. All further analyses were corrected for age and sex.
Mediating effects of behavioural generalization indices
As a requirement for a mediation model, we first examined interrelationships between childhood maltreatment, threat generalization and subclinical symptom load.
For the relationship between childhood maltreatment and symptom load, we conducted an analysis of covariance ( ANCOVA) with childhood maltreatment group (no/low levels of childhood maltreatment, high levels of childhood maltreatment) as the between-subjects variable and symptom load as the dependent variable. We also conducted a partial correlation analysis to test for a continuous association.
To examine the relationship between childhood maltreatment and threat generalization, for each self-report measure (fear and US expectancy), we conducted a mixed analysis of variance (ANOVA), with childhood maltreatment group as the between-subjects factor and stimulus type (7 levels; CS−, GS5, GS4 GS3, GS2, GS1 and CS+) as the within-subjects factor, along with a quadratic trend analysis. Greenhouse–Geisser correction and Bonferroni-corrected post hoc t tests were run when appropriate. A higher quadratic trend in the generalization gradient reflects a sharper gradient and is less indicative of stimulus generalization, whereas a flatter or more gradual generalization gradient indicates more widespread generalization.44
To examine the relationship between threat generalization and symptom load, similar to van Meurs and colleagues,45 we incorporated the generalization gradient shape into a continuous measure: the linear departure score (LDS; see Appendix 1 for details). A positive LDS reflects a more gradual gradient (enhanced generalization), whereas a negative value reflects a sharp gradient (lower generalization). The LDSs were regressed on the symptom load.
Moderating effects of behavioural generalization indices
We tested moderation using regression analyses, testing the interaction between childhood maltreatment and the LDSs in the models of symptom load.
Neural data
As a manipulation check, we first assessed whether generalization gradients in neural activation could be observed in our regions of interest (ROIs; the vmPFC, dACC, insula and hippocampus; Appendix 1). All group-level analyses were conducted in FSL software, both in functional ROIs as well as the whole brain, with FLAME1 at a cluster significance level of Z > 3.1 and p < 0.05 with Gaussian random field (GRF) correction for multiple comparisons.
Mediating effects of neural generalization substrates
Interrelationships between childhood maltreatment and threat generalization and between threat generalization and subclinical symptom load were first examined as required for further mediation tests. For the relationship between childhood maltreatment and neural threat generalization, we conducted a 2-sample unpaired t test to compare the childhood maltreatment groups on the neural LDS contrast (average [GS1–5] > average [CS−, CS+]). For the relationship between threat generalization and symptom load, we used regression analyses to examine the association between subclinical symptom load and the neural LDS contrast.
Moderating effects of neural generalization substrates
Similar to the behavioural data, we conducted a whole-brain interaction analysis. Parameter estimates of significant clusters were extracted to assess associations between threat generalization and symptom load per childhood maltreatment group and to visualize neural generalization gradients.
Results
Participants
Our final sample included 113 participants: 55 participants in the group with no/low levels of childhood maltreatment and 58 participants in the group with high levels of childhood maltreatment. Table 1 shows sample characteristics of both childhood maltreatment groups. The groups did not differ in age (t111 = 0.93, p = 0.35), sex (χ2 2,113 = 2.15, p = 0.34), educational level (χ2 4,114 = 2.38, p = 0.67), or chosen US intensity (t111 = 0.61 p = 0.54). Analyses confirmed that childhood maltreatment groups differed in the CTQ-SF total score (Mann–Whitney U < 0.001, p < 0.001) and all subscale scores (all p < 0.04).
Table 1.
Demographic and clinical characteristics of study participants
| Characteristic | Group; mean ± SD* | |
|---|---|---|
|
| ||
| No/low levels of CM (n = 55) | High levels of CM (n = 58) | |
| Age yr | 21.00 ± 2.10 | 20.64 ± 2.03 |
| Sex, no. (%) | ||
| Male | 11 (20) | 11 (19) |
| Female | 44 (80) | 47 (81) |
| Educational level, no. (%) | ||
| Low | 0 (0) | 1 (2) |
| Medium | 6 (11) | 5 (9) |
| High | 49 (89) | 52 (90) |
| CTQ total score† | 28.05 ± 2.05 | 40.78 ± 7.91 |
| Symptom load† | −0.45 ± 0.69 | 0.41 ± 0.81 |
| MADRS | 5.33 ± 5.93 | 11.47 ± 7.46 |
| STAI | 34.45 ± 12.16 | 47.84 ± 11.41 |
| SIS-R | 0.47 ± 0.34 | 0.82 ± 0.50 |
| US intensity, mA | 24.92 ± 18.21 | 22.84 ± 17.38 |
CM = childhood maltreatment; CTQ = Childhood Trauma Questionnaire; MADRS = Montgomery-Asberg Depression Rating Scale; SD = standard deviation; SIS-R = Structured Interview for Schizotypy – Revised; STAI = State and Trait Anxiety Inventory; US = unconditioned stimulus.
Unless indicated otherwise.
p < 0.001.
Childhood trauma and psychopathology
The group with high levels of childhood maltreatment reported a higher symptom load than the group with no/low levels of childhood maltreatment (F3, 109 = 37.01, p < 0.001).
Childhood maltreatment and generalization outcomes
Behaviour
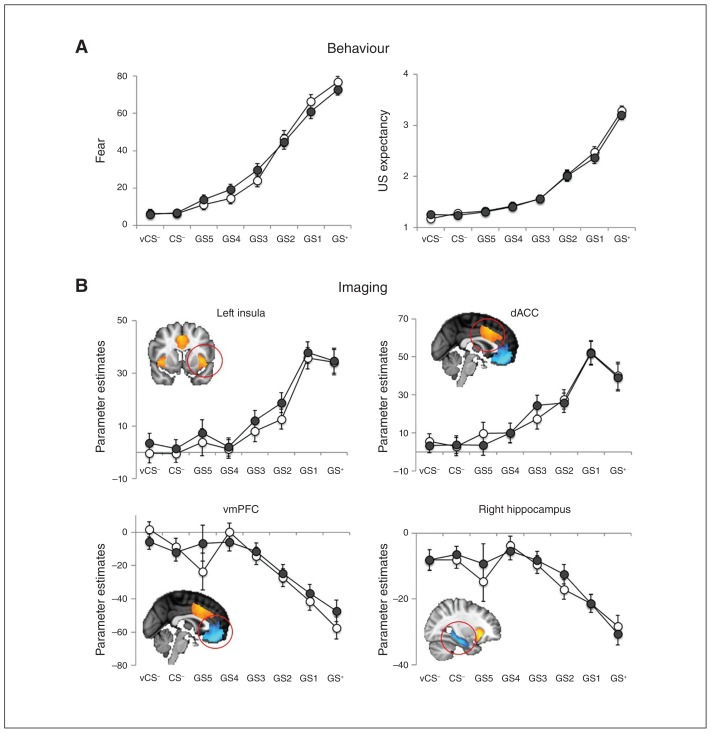
Both groups showed a positive generalization gradient in fear scores as well as US expectancy scores, as these scores increased with similarity to the CS+ (all p < 0.0001; Fig. 1). There were, however, no differences in threat generalization between the childhood maltreatment groups, as neither the group × stimulus type interactions (fear: F3.90,413.86 = 1.54, p = 0.19; US expectancy: F3.50,367.20 = 0.23, p = 0.90), the the group × quadratic trend analysis (fear: F1,106 = 1.83, p = 0.18; US expectancy: F1,106 = 0.39, p = 0.53), nor the group comparison of the LDS (fear: F3,106 = 0.94, p = 0.34; US expectancy: F3,106 = 0.14, p = 0.71) were significant.
Fig. 1.
Generalization gradients in behavioural data and in activation in functional regions of interest in the entire sample. (A) Generalization gradients in fear and unconditioned stimulus (US) expectancy ratings. (B) Generalization gradients in neural activation in the left insula, dorsal anterior cingulate cortex (dACC), ventromedial prefrontal cortex (vmPFC) and right hippocampus. Error bars represent standard errors of the mean. White circles represent the group with no/low levels of childhood maltreatment; grey circles represent the group with high levels of childhood maltreatment.
Additional exploratory analyses on valence and arousal scores did not indicate group differences in generalization, as the valence and arousal LDSs (all p > 0.29) and the quadratic trend of the gradients (all p > 0.21) did not differ across groups. However, we found significant group × stimulus interactions for the valence and arousal scores ( Appendix 1, Fig. S2), reflecting that the group with high levels of childhood maltreatment showed less variation in self-reported valence/arousal scores across stimuli than the group with no/low levels of childhood maltreatment (all p < 0.02).
Imaging
The task induced neural generalization gradients in each of the ROIs (all p < 0.001), with positive generalization gradients in the dACC and insular cortices, and negative generalization gradients in the vmPFC and hippocampi (Fig. 1 and Appendix 1, Table S1). Exploration of the neural LDS contrast across the childhood maltreatment groups did not reveal any group differences.
Generalization outcomes and psychopathology
Behaviour
Neither the fear LDS nor the US expectancy LDS showed significant associations with symptom load (fear: r = 0.10, p = 0.27; US expectancy: r = 0.08, p = 0.39).
Imaging
We found no associations between neural activation for the LDS contrast and symptom load.
Threat generalization as a moderator of the association between childhood maltreatment and psychopathology
As no significant associations were observed between childhood maltreatment and threat generalization, or between threat generalization and subclinical symptoms, no mediation analyses were conducted. Moderation analyses were conducted testing the interaction between childhood maltreatment and threat generalization on subclinical symptom load.
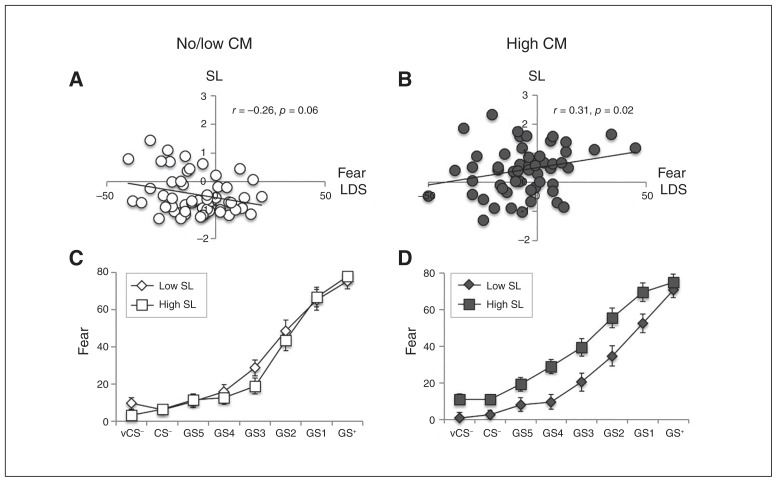
Behaviour
Regression analyses revealed significant interactions between childhood maltreatment and the fear LDS on subclinical symptom load (Fig. 2), reflecting that in the group with high levels of childhood maltreatment, the association between fear generalization and symptom load was more positive than in the group with no/low levels of childhood maltreatment (β = 0.36, p = 0.008). Further exploration of within-group correlation analyses revealed that only in the group with high levels of childhood maltreatment, a higher fear LDS was positively associated with an increased symptom load (r = 0.31, p = 0.02). In the group with no/low levels of childhood maltreatment, we observed a trend toward a negative association (no childhood maltreatment: r = −0.26, p = 0.06). To illustrate the generalization gradient shape per symptom load level within each childhood maltreatment group, we followed up with a median-split symptom load score × quadratic trend interaction analysis on the fear generalization gradient. As expected, in the group with high levels of childhood maltreatment, individuals with low symptom load showed a stronger quadratic trend, and thus a shaper fear generalization gradient, than individuals with a high symptom load (F1,53 = 6.84, p = 0.01). In the group with low levels of childhood maltreatment, no difference in the quadratic trend of the generalization gradient was found between individuals with a high or low symptom load (F1,49 = 2.52, p = 0.28).
Fig. 2.
Threat generalization moderates the link between childhood maltreatment and psychopathology. (A) Correlation between the fear linear departure score (LDS) and symptom load (SL) in the group with no/low levels of childhood maltreatment (CM). (B) Correlation between the fear LDS and SL in the group with high levels of CM. (C) Fear generalization gradient in the group with no/low levels of CM and low versus high SL (median split). (D) Fear generalization gradient in the group with high levels of CM and low versus high SL (median split). Errors bars represent standard errors of the mean.
Results of the US expectancy LDS were similar to those of the fear LDS, as we found a significant interaction between childhood maltreatment group and US expectancy LDS on subclinical symptom load (β = 0.58, p < 0.0001). Findings on post hoc tests were also comparable (see Appendix 1 for US expectancy LDS results).
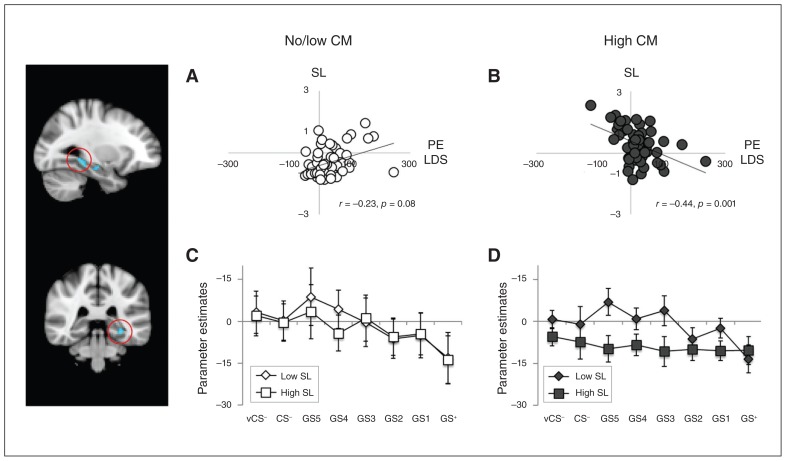
Imaging
The ROI analysis showed a significant interaction in 2 clusters in the left hippocampus (anterior: Montreal Neurological Institute [MNI] coordinates x, y, z = −30, −18, −16; k = 18, Z = 3.53, p = 0.02; posterior: MNI coordinates x, y, z = −30, −38, −10; k = 41, Z = 4.38, p = 0.008; Fig. 3). This interaction reflected that, in the group with high levels of childhood maltreatment, the association between symptom load and LDS-related activation in these clusters was more negative than in the group with no/low levels of childhood maltreatment. Correlational analyses with extracted parameter estimates of the LDS contrast revealed that there was a negative association between hippocampal activation and symptom load in the group with high levels of childhood maltreatment in both clusters (anterior: r = −0.37, p = 0.005; posterior: r = −0.44, p = 0.001), whereas there were no significant associations in the group with no/low levels of childhood maltreatment (anterior: r = 0.24, p = 0.10; posterior: r = 0.25, p = 0.08). The generalization gradient shape in these clusters per symptom-load level within each childhood maltreatment group was further tested by a median-split symptom load score × quadratic trend interaction analysis. In the group with high levels of childhood maltreatment, individuals with a low symptom load showed a sharper hippocampal generalization gradient, as reflected by a stronger quadratic trend in the gradient, than individuals with a high symptom load (F1,52 = 4.32, p = 0.04; F1,52 = 5.75, p = 0.02). No difference in the quadratic trend of the generalization gradient between individuals with a low versus a high symptom load were found in the group with low levels of childhood maltreatment (F1,49 = 0.06, p = 0.82; F1,49 = 0.17, p = 0.20).
Fig. 3.
Hippocampal activation during generalization moderates the link between childhood maltreatment (CM) and psychopathology. (A) Correlation between the average parameter estimate (PE) of the linear departure score (LDS) contrast and symptom load (SL) in the group with no/low levels of CM. (B) Correlation between the average PE of the LDS contrast and SL in the group with high levels of CM. (C) Hippocampal generalization gradient in the group with no/low levels of CM and low versus high SL (median split). (D) Hippocampal generalization gradient in the group with high levels of CM group and low versus high SL (median split). Errors bars represent standard errors of the mean.
Further whole-brain analyses revealed an interaction effect in a cluster encompassing the left hippocampus, parahippocampal gyrus and temporal fusiform gyrus, with similar results (Appendix 1).
Discussion
Childhood maltreatment is a transdiagnostic risk factor for development of psychopathology. To our knowledge, this is the first study exploring interrelationships between threat generalization (behavioural and neural), childhood maltreatment and psychopathology during emerging adulthood. As expected, our results showed that childhood maltreatment was linked to increased subclinical psychopathology (i.e., a mixture of depression, anxiety and psychotic experiences) in young adults. Furthermore, we found that threat generalization moderated the link between childhood maltreatment and psychopathology. More specifically, we observed a high clinical symptom load only in individuals who reported high levels of childhood maltreatment and showed enhanced levels of threat generalization. Similarly, our neural data revealed that a high level of childhood maltreatment in combination with lower activation in the hippocampus during presentation of generalization stimuli was associated with a higher subclinical symptom load. The results cautiously suggest that, after exposure to childhood maltreatment, threat generalization may function as a vulnerability factor for the development of psychopathology during emerging adulthood.
Overall, in the group reporting high levels of childhood maltreatment, individuals with a high subclinical symptom load showed enhanced levels of threat generalization in several generalization indices (i.e., LDS for fear ratings, US expectancy and hippocampal activation) than those with a low symptom load. Our results further confirmed that in the group with high levels of childhood maltreatment, individuals with a high subclinical symptom load showed more gradual gradients in fear ratings, US expectancy and hippocampal activation than those with a low symptom load, which reflects lower stimulus discrimination and more widespread generalization.46 Subclinical symptoms of interest were anxiety, depression and psychotic experiences, as childhood maltreatment is associated with an admixture of these symptoms,1 and they are thought to be highly interrelated at a subclinical level,4 as confirmed by the present data. With careful consideration of the cross-sectional nature of our study, these results may imply that young adults with a history of childhood maltreatment are at risk for subclinical psychopathology when they also show higher levels of threat generalization. Many individuals who were exposed to maltreatment during childhood do not transition to psychopathology. 33 As such, lower levels of threat generalization may contribute to resilience in these individuals. Although this is, to our knowledge, the first study linking threat generalization indices to a continuous measure of subclinical psychopathology, previous case–control studies have provided evidence for higher threat anticipation and lower threat–safety discrimination not only in individuals with psychosis, anxiety disorders (including panic disorder and GAD with depression) and PTSD, but also in healthy individuals with increased psychotic experiences and higher trait anxiety.16,19–22,47,48 Our study adds childhood maltreatment to these findings, suggesting that threat generalization could play a moderating role in the association between childhood maltreatment and psychopathology.
Results in the hippocampus paralleled our behavioural findings. Our behavioural findings showed positive generalization gradients in US expectancy and self-reported fear ratings. The activation in the hippocampus followed a negative generalization gradient, with the highest activation in response to the safest stimuli (vCS− and CS−) and decreasing reactivity to stimuli that were perceptually more similar to the conditioned threat stimulus. The negative generalization gradient observed in the hippocampus has been reported in previous studies.49,50 The hippocampus has been proposed to be centrally implicated in threat generalization26 via its role in stimulus discrimination and safety processing,27,28,51 thereby influencing reactivity in fear-inhibition regions such as the vmPFC. Our results may indicate that, in individuals with a history of childhood maltreatment, reduced hippocampal responses to ambiguous threats can promote threat overgeneralization, which could contribute to the development of psychiatric symptoms. Previous work has focused mainly on hippocampal morphological changes and functional alterations measured with resting-state fMRI, suggesting that such alterations may mediate the association between childhood maltreatment and psychopathology.9 In addition, a recent meta-analysis reported reduced left hippocampal activation to socioaffective cues in adults with exposure to childhood maltreatment.13 Yet, how functional activations during threat processing are associated with the development of psychiatric symptoms after exposure to childhood maltreatment needs further examination.
Of note, inspection of the fear-generalization gradient (Fig. 2) in the group reporting high levels of childhood maltreatment also showed that individuals with a high symptom load reported greater fear in response to all stimuli except the CS+ than those with a low symptom load. This result may indicate enhanced sensitization in addition to enhanced threat generalization.
The present study showed a high symptom load only in individuals with high levels of childhood maltreatment and higher levels of threat generalization, not in the complete sample. This finding was not in line with those of several (mostly case–control) studies that reported a direct link between threat generalization and psychopathology.19–23 Yet, some studies reported no association between threat generalization and anxiety symptoms,52,53 and some studies reported enhanced threat-safety discrimination in individuals with high levels of anxiety54 and greater differential threat conditioning in individuals with depression,55 which suggests reduced threat generalization. In line with these latter findings, our study showed that, in the group with no/low levels of childhood maltreatment, higher generalization in US expectancies was associated with lower levels of psychopathology. However, generalization in other measures (i.e., self-reported fear or in the neural data) was not significantly associated with psychopathology in this group. As the overall evidence on the link between threat generalization and anxiety/depression symptomatology is mixed, our study highlights the importance of taking into account early-life adversities in threat-generalization studies.
Across the sample, childhood maltreatment exposure could not be linked to enhanced threat generalization in either self-report ratings or neural data. Similarly, a recent study found that childhood maltreatment–related PTSD was not associated with altered generalization gradients in self-report ratings or physiological outcomes.56 Yet, a previous study did find an association between childhood maltreatment and reduced differential threat conditioning, 6 as observed with skin conductance responses, which is indicative of a generalized psychophysiological response. Furthermore, the reduced differential skin conductance response during conditioning seemed to be associated more with a blunted response to the CS+ than with enhanced reactivity to the CS−, which is consistent with the findings of previous studies reporting blunted threat reactivity in individuals exposed to childhood trauma.7 In the present study, we observed altered generalization gradients in valence and arousal ratings in the group with high levels of childhood maltreatment, which also reflected more overall bluntness in subjective responses. Thus, childhood maltreatment seems not be related to enhanced threat generalization, but may be associated with more blunted subjective arousal or psychophysiological responses to threat. Furthermore, our imaging data did not reveal any overall associations between childhood maltreatment and alterations in threat-related activations in our generalization task. Previous studies have reported altered fear circuitry in individuals exposed to childhood maltreatment; however, such findings have been reported based on structural MRI or resting-state fMRI.9,57,58
Strengths and limitations
Strengths of the present study were that we used validated measures of psychopathology, childhood maltreatment and threat generalization. However, the study had some limitations. The data were acquired in a cross-sectional manner, precluding definitive insight into the causality of childhood maltreatment, threat generalization and psychopathology. Our results should, therefore, be interpreted carefully, and further longitudinal examination is warranted. In addition, it would have been interesting to take into account maltreatment-related characteristics, including timing of exposure, chronicity and type. For instance, it has been hypothesized that abuse and neglect may have different effects on threat-processing outcomes.11 Measures of abuse and neglect were, however, highly intercorrelated in the present sample. Another limitation was that childhood trauma was reported retrospectively, which entails a risk of recall bias. Finally, we did not measure psychophysiological data, such as skin conductance responses or fear-potentiated startle, during the threat-generalization procedure. Such measures may provide additional information on threat responses.
Conclusion
Our results suggest that threat generalization moderates the association between childhood maltreatment and subclinical psychopathology in emerging adulthood. Individuals who were exposed to high levels of childhood maltreatment and showed enhanced threat generalization reported a higher subclinical symptom load. Our findings suggest that, after childhood maltreatment exposure, higher threat generalization may put individuals at risk for the development of psychopathology. As our study was cross-sectional, more definite insights into the mechanisms underlying the association between childhood maltreatment and later symptomatology should be investigated further in longitudinal designs. Our results could inform developmental models of latent mental vulnerability and comorbidity and provide directions for further exploration of vulnerability factors or resilience mechanisms. Furthermore, our results suggest that targeting threat-generalization mechanisms may lower the likelihood of young adults exposed to childhood maltreatment developing mental health problems. Whether threat-generalization mechanisms can be altered and whether this contributes to greater resilience in individuals exposed to childhood maltreatment needs exploration in future studies.
Acknowledgements
This study was funded by a research grant from Stichting the Weijerhorst and by a fellowship of the Dutch Brain Foundation to M. Wichers (Hersenstichting Nederland: 20121-03).
Footnotes
Competing interests: R. van Winkel reports personal fees from Johnson & Johnson, outside the submitted work. No other authors declared competing interests.
Contributors: I. Lange, L. Goossens, M. Marcelis, M. Wichers, J. van Os, T. van Amelsvoort and K. Schruers designed the study. I. Lange, J. Bakker and S. Michielse collected the data. I. Lange, L. Goossens, R. van Winkel, S. Lissek, N. Leibold and K. Schruers analyzed the data. I. Lange wrote the article, which all authors critically reviewed. All authors approved the final version to be published and can certify that no other individuals not listed as authors have made substantial contributions to the paper.
References
- 1.van Nierop M, Viechtbauer W, Gunther N, et al. Childhood trauma is associated with a specific admixture of affective, anxiety, and psychosis symptoms cutting across traditional diagnostic boundaries. Psychol Med. 2015;45:1277–88. doi: 10.1017/S0033291714002372. [DOI] [PubMed] [Google Scholar]
- 2.Van Dam D, van Nierop M, Viechtbauer W, et al. Childhood abuse and neglect in relation to the presence and persistence of psychotic and depressive symptomatology. Psychol Med. 2015;45:1363–77. doi: 10.1017/S0033291714001561. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 4.Wigman JT, van Os J, Thiery E, et al. Psychiatric diagnosis revisited: towards a system of staging and profiling combining nomothetic and idiographic parameters of momentary mental states. PLoS One. 2013;8:e59559. doi: 10.1371/journal.pone.0059559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGorry P, Keshavan M, Goldstone S, et al. Biomarkers and clinical staging in psychiatry. World Psychiatry. 2014;13:211–23. doi: 10.1002/wps.20144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McLaughlin KA, Sheridan MA, Gold AL, et al. Maltreatment exposure, brain structure, and fear conditioning in children and adolescents. Neuropsychopharmacology. 2015;41:1956–64. doi: 10.1038/npp.2015.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D’Andrea W, Pole N, DePierro J, et al. Heterogeneity of defensive responses after exposure to trauma: blunted autonomic reactivity in response to startling sounds. Int J Psychophysiol. 2013;90:80–9. doi: 10.1016/j.ijpsycho.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 8.Busso DS, McLaughlin KA, Sheridan MA. Dimensions of adversity, physiological reactivity, and externalizing psychopathology in adolescence: deprivation and threat. Psychosom Med. 2017;79:162–71. doi: 10.1097/PSY.0000000000000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herringa RJ, Birn RM, Ruttle PL, et al. Childhood maltreatment is associated with altered fear circuitry and increased internalizing symptoms by late adolescence. Proc Natl Acad Sci U S A. 2013;110:19119–24. doi: 10.1073/pnas.1310766110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McCrory EJ, Gerin MI, Viding E. Annual research review: childhood maltreatment, latent vulnerability and the shift to preventative psychiatry–the contribution of functional brain imaging. J Child Psychol Psychiatry. 2017;58:338–57. doi: 10.1111/jcpp.12713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teicher MH, Samson JA, Anderson CM, et al. The effects of childhood maltreatment on brain structure, function and connectivity. Nat Rev Neurosci. 2016;17:652–66. doi: 10.1038/nrn.2016.111. [DOI] [PubMed] [Google Scholar]
- 12.Morey R, Dunsmoor J, Haswell C, et al. Fear learning circuitry is biased toward generalization of fear associations in posttraumatic stress disorder. Transl Psychiatry. 2015;5:e700. doi: 10.1038/tp.2015.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heany SJ, Groenewold NA, Uhlmann A, et al. The neural correlates of Childhood Trauma Questionnaire scores in adults: a meta-analysis and review of functional magnetic resonance imaging studies. Dev Psychopathol. 2018;30:1–11. doi: 10.1017/S0954579417001717. [DOI] [PubMed] [Google Scholar]
- 14.Den ML, Graham BM, Newall C, et al. Teens that fear screams: a comparison of fear conditioning, extinction, and reinstatement in adolescents and adults. Dev Psychobiol. 2015;57:818–32. doi: 10.1002/dev.21330. [DOI] [PubMed] [Google Scholar]
- 15.Lim MH, Gleeson JF, Jackson HJ. Selective attention to threat bias in delusion-prone individuals. J Nerv Ment Dis. 2011;199:765–72. doi: 10.1097/NMD.0b013e31822fc9e9. [DOI] [PubMed] [Google Scholar]
- 16.Holt DJ, Coombs G, Zeidan MA, et al. Failure of neural responses to safety cues in schizophrenia. Arch Gen Psychiatry. 2012;69:893–903. doi: 10.1001/archgenpsychiatry.2011.2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams LM, Gatt JM, Schofield PR, et al. ‘Negativity bias’ in risk for depression and anxiety: brain–body fear circuitry correlates, 5-HTT-LPR and early life stress. Neuroimage. 2009;47:804–14. doi: 10.1016/j.neuroimage.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 18.Fulford D, Rosen RK, Johnson SL, et al. Negative generalization and symptoms of anxiety disorders. J Exp Psychopathol. 2011;3 doi: 10.5127/jep.019811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaczkurkin AN, Burton PC, Chazin SM, et al. Neural substrates of overgeneralized conditioned fear in PTSD. Am J Psychiatry. 2017;174:125–34. doi: 10.1176/appi.ajp.2016.15121549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lissek S, Kaczkurkin AN, Rabin S, et al. Generalized anxiety disorder is associated with overgeneralization of classically conditioned fear. Biol Psychiatry. 2014;75:909–15. doi: 10.1016/j.biopsych.2013.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lissek S, Rabin S, Heller RE, et al. Overgeneralization of conditioned fear as a pathogenic marker of panic disorder. Am J Psychiatry. 2010;167:47–55. doi: 10.1176/appi.ajp.2009.09030410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Greenberg T, Carlson JM, Cha J, et al. Ventromedial prefrontal cortex reactivity is altered in generalized anxiety disorder during fear generalization. Depress Anxiety. 2013;30:242–50. doi: 10.1002/da.22016. [DOI] [PubMed] [Google Scholar]
- 23.Milad MR, Quirk GJ, Pitman RK, et al. A role for the human dorsal anterior cingulate cortex in fear expression. Biol Psychiatry. 2007;62:1191–4. doi: 10.1016/j.biopsych.2007.04.032. [DOI] [PubMed] [Google Scholar]
- 24.Singer T, Critchley HD, Preuschoff K. A common role of insula in feelings, empathy and uncertainty. Trends Cogn Sci. 2009;13:334–40. doi: 10.1016/j.tics.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 25.Lange I, Goossens L, Michielse S, et al. Behavioral pattern separation and its link to the neural mechanisms of fear generalization. Soc Cogn Affect Neurosci. 2017;12:1720–9. doi: 10.1093/scan/nsx104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lissek S, Bradford DE, Alvarez RP, et al. Neural substrates of classically conditioned fear-generalization in humans: a parametric fMRI study. Soc Cogn Affect Neurosci. 2013;9:1134–42. doi: 10.1093/scan/nst096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harrison BJ, Fullana MA, Via E, et al. Human ventromedial prefrontal cortex and the positive affective processing of safety signals. Neuroimage. 2017;152:12–8. doi: 10.1016/j.neuroimage.2017.02.080. [DOI] [PubMed] [Google Scholar]
- 28.Fullana M, Harrison B, Soriano-Mas C, et al. Neural signatures of human fear conditioning: an updated and extended meta-analysis of fMRI studies. Mol Psychiatry. 2016;21:500–8. doi: 10.1038/mp.2015.88. [DOI] [PubMed] [Google Scholar]
- 29.Romaniuk L, Honey GD, King JR, et al. Midbrain activation during Pavlovian conditioning and delusional symptoms in schizophrenia. Arch Gen Psychiatry. 2010;67:1246–54. doi: 10.1001/archgenpsychiatry.2010.169. [DOI] [PubMed] [Google Scholar]
- 30.Morriss J, Macdonald B, van Reekum CM. What is going on around here? Intolerance of uncertainty predicts threat generalization. PLoS One. 2016;11:e0154494. doi: 10.1371/journal.pone.0154494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carleton RN, Mulvogue MK, Thibodeau MA, et al. Increasingly certain about uncertainty: Intolerance of uncertainty across anxiety and depression. J Anxiety Disord. 2012;26:468–79. doi: 10.1016/j.janxdis.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 32.White R, Gumley A. Intolerance of uncertainty and distress associated with the experience of psychosis. Psychol Psychother. 2010;83:317–24. doi: 10.1348/147608309X477572. [DOI] [PubMed] [Google Scholar]
- 33.Taillieu TL, Brownridge DA, Sareen J, et al. Childhood emotional maltreatment and mental disorders: results from a nationally representative adult sample from the United States. Child Abuse Negl. 2016;59:1–12. doi: 10.1016/j.chiabu.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 34.Fonzo GA, Huemer J, Etkin A. History of childhood maltreatment augments dorsolateral prefrontal processing of emotional valence in PTSD. J Psychiatr Res. 2016;74:45–54. doi: 10.1016/j.jpsychires.2015.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dennison MJ, Sheridan MA, Busso DS, et al. Neurobehavioral markers of resilience to depression amongst adolescents exposed to child abuse. J Abnorm Psychol. 2016;125:1201. doi: 10.1037/abn0000215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van Nierop M, Lecei A, Myin-Germeys I, et al. Stress reactivity links childhood trauma exposure to an admixture of depressive, anxiety, and psychosis symptoms. Psychiatry Res. 2018;260:451–7. doi: 10.1016/j.psychres.2017.12.012. [DOI] [PubMed] [Google Scholar]
- 37.Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–9. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 38.Konings M, Bak M, Hanssen M, et al. Validity and reliability of the CAPE: a self-report instrument for the measurement of psychotic experiences in the general population. Acta Psychiatr Scand. 2006;114:55–61. doi: 10.1111/j.1600-0447.2005.00741.x. [DOI] [PubMed] [Google Scholar]
- 39.Overbeek I, Schruers K, Griez E. Mini International Neuropsychiatric Interview: Nederlandse versie 5.0. 0. DSM-IV [Dutch version] Maastricht, The Netherlands: Universiteit Maastricht; 1999. [Google Scholar]
- 40.Bernstein DP, Fink L, Handelsman L, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151:1132. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- 41.Aas M, Kauppi K, Brandt C, et al. Childhood trauma is associated with increased brain responses to emotionally negative as compared with positive faces in patients with psychotic disorders. Psychol Med. 2017;47:669–79. doi: 10.1017/S0033291716002762. [DOI] [PubMed] [Google Scholar]
- 42.Spielberger CD, Gorsuch RL, Lushene RE. Manual for the state-trait anxiety inventory. 1970. [Google Scholar]
- 43.Vollema MG, Ormel J. The reliability of the Structured Interview for Schizotypy–Revised. Schizophr Bull. 2000;26:619. doi: 10.1093/oxfordjournals.schbul.a033482. [DOI] [PubMed] [Google Scholar]
- 44.Dunsmoor JE, Mitroff SR, LaBar KS. Generalization of conditioned fear along a dimension of increasing fear intensity. Learn Mem. 2009;16:460–9. doi: 10.1101/lm.1431609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.van Meurs B, Wiggert N, Wicker I, et al. Maladaptive behavioral consequences of conditioned fear-generalization: a pronounced, yet sparsely studied, feature of anxiety pathology. Behav Res Ther. 2014;57:29–37. doi: 10.1016/j.brat.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dymond S, Dunsmoor JE, Vervliet B, et al. Fear generalization in humans: systematic review and implications for anxiety disorder research. Behav Ther. 2015;46:561–82. doi: 10.1016/j.beth.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 47.Haddad AD, Pritchett D, Lissek S, et al. Trait anxiety and fear responses to safety cues: Stimulus generalization or sensitization? J Psychopathol Behav Assess. 2012;34:323–31. [Google Scholar]
- 48.Reininghaus U, Kempton MJ, Valmaggia L, et al. Stress sensitivity, aberrant salience, and threat anticipation in early psychosis: an experience sampling study. Schizophr Bull. 2016;42:712–22. doi: 10.1093/schbul/sbv190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lissek S, Bradford DE, Alvarez RP, et al. Neural substrates of classically conditioned fear-generalization in humans: a parametric fMRI study. Soc Cogn Affect Neurosci. 2013;9:1134–42. doi: 10.1093/scan/nst096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Greenberg T, Carlson JM, Cha J, et al. Neural reactivity tracks fear generalization gradients. Biol Psychol. 2013;92:2–8. doi: 10.1016/j.biopsycho.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 51.De Shetler NG, Rissman J. Dissociable profiles of generalization/discrimination in the human hippocampus during associative retrieval. Hippocampus. 2017;27:115–21. doi: 10.1002/hipo.22684. [DOI] [PubMed] [Google Scholar]
- 52.Tinoco-González D, Fullana MA, Torrents-Rodas D, et al. Conditioned fear acquisition and generalization in generalized anxiety disorder. Behav Ther. 2015;46:627–39. doi: 10.1016/j.beth.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 53.Torrents-Rodas D, Fullana MA, Bonillo A, et al. No effect of trait anxiety on differential fear conditioning or fear generalization. Biol Psychol. 2013;92:185–90. doi: 10.1016/j.biopsycho.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 54.Glotzbach-Schoon E, Tadda R, Andreatta M, et al. Enhanced discrimination between threatening and safe contexts in high-anxious individuals. Biol Psychol. 2013;93:159–66. doi: 10.1016/j.biopsycho.2013.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Borelli JL, Sbarra DA, Crowley MJ, et al. Mood symptoms and emotional responsiveness to threat in school-aged children. J Clin Child Adolesc Psychol. 2011;40:220–32. doi: 10.1080/15374416.2011.546047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thome J, Hauschild S, Koppe G, et al. Generalisation of fear in PTSD related to prolonged childhood maltreatment: an experimental study. Psychol Med. 2018;48:2223–4. doi: 10.1017/S0033291717003713. [DOI] [PubMed] [Google Scholar]
- 57.Birn RM, Patriat R, Phillips ML, et al. Childhood maltreatment and combat posttraumatic stress differentially predict fear-related fronto-subcortical connectivity. Depress Anxiety. 2014;31:880–92. doi: 10.1002/da.22291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McLaughlin KA, Sheridan MA, Gold AL, et al. Maltreatment exposure, brain structure, and fear conditioning in children and adolescents. Neuropsychopharmacology. 2016;41:1956–64. doi: 10.1038/npp.2015.365. [DOI] [PMC free article] [PubMed] [Google Scholar]