Abstract
Purpose
Acute burn resuscitation in initial 24 h remains a challenge to plastic surgeons. Though various formulae for fluid infusion are available but consensus is still lacking, resulting in under resuscitation or over resuscitation. Parkland formula is widely used but recently its adequacy is questioned in studies. This study was conducted to see how closely the actual volume of fluid given in our center matches with that of calculated volume by Parkland formula.
Methods
All patients admitted with more than 20% flame burn injury and within 8 h of incident were included in this study. Crystalloid solution for infusion was calculated as per Parkland formula; however, it was titrated according to the urine output. Data on fluid infusion were collected from patient's inpatient records and analyzed.
Results
The study included a total of 90 patients, about 86.7% (n = 78) of the patients received fluid less than the calculated Parkland formula. Rate of fluid administered over 24 h in our study was 3.149 mL/kg/h. Mean hourly urine output was found to be 0.993 mL/kg/h. The mean difference between fluid administered and fluid calculated by Parkland formula was 3431.825 mL which was significant (p < 0.001).
Conclusion
The study showed a significant difference in the fluid infused based on urine output and the fluid calculated by Parkland formula. This probably is because fluid infused based on end point of resuscitation was more physiological than fluid calculated based on formulae.
Keywords: Burn resuscitation, Parkland formula, Urine output, Physiological curve
Introduction
Resuscitation of acute major burns is a challenge to the burn care providers especially in the first 24 h from the time of burns. It is one of the major determinants of survival of burn patients. Various resuscitation formulae are available at the behest of the burn care provider and many important advances have been made in the field of burn resuscitation, but none ensures smooth resuscitation. Problems of under resuscitation or over resuscitation related complications and the controversy in the choice of fluid i.e. crystalloid based resuscitation fluid, or the colloid based resuscitation fluid makes it difficult to choose the right guidelines for the early fluid resuscitation. As fluid volume depends on the burns size and the burns depth, inaccurate assessment of burn size can lead to inappropriate fluid volume infusion to the burn patient.1
Parkland formula has been the most widely used fluid resuscitation formula since it was first proposed by Baxter and Shires in 1968. It states infusion of Ringer Lactate solution at the rate of 3.7–4.2 mL per kilogram of body weight per percent burn. Early aggressive fluid replenishment in burn shock has been the mainstay of burns resuscitation, but recent studies have mentioned about burn injured patients being over-resuscitated, often with indistinct endpoint targets.2 More recently, fluid resuscitation in excess of the Parkland formula has been observed.3, 4, 5
The purpose of this study was to assess the effectiveness of Parkland formula in the estimation of resuscitation fluid volume in Adult thermal burns and to compare the resuscitation fluid calculated by Parkland formula and actual resuscitation fluid delivered to the burn patient based on end target of resuscitation in first 24 h of acute burn.
The Parkland formula is a time tested and valuable method for calculating the initial volume of fluid required for resuscitation of a burn victim. The study was not to disrepute the Parkland formula, but to see how closely the actual infused volume match the estimated volume calculated by Parkland formula.
Methods
The study was conducted in Christian Medical College, Vellore after obtaining ethical committee approval. This was a retrospective study to assess the fluid resuscitation in first 24 h from the time of burns. The data were obtained from the in-patient charts of the patient in the medical records department of the Christian Medical College, Vellore.
The study population included adults with burns above twenty percentage of total body surface area (TBSA) admitted in our institute within 8 h from the time of incident during the study period, 1st January 2010 to 31st December 2014.6 Our study included those patients who have referral sheet with recorded resuscitation fluid volumes prior to admission. The patients with electrical burns, chemical burns and those admitted after 8 h from the time of burns were excluded from the study. Patients with concomitant trauma were also excluded from the study.
Patients with history of burn in an enclosed space, facial burns, singeing of facial hairs, hoarseness of voice, stridor, carbonaceous sputum with breathlessness and presence of airway mucosal edema with soot in the airway were consider having inhalational injury.7, 8
The burn assessment was done to find the percentage of burns and the depth of burns. The Wallace rule of nine was applied to calculate the percentage of burns in the initial assessment and further accuracy in burns size estimation done by Lund and Browder chart. All burns were secured with a central venous access.
Patients were resuscitated with crystalloid solution (Ringer lactate) in first 24 h and the resuscitation fluid required for the patient was calculated as per Parkland formula – 4 mL/kg of body weight/percentage of TBSA burns. The fluid administered to patient prior to admission was included in the calculated volume of fluid. However, to avoid fluid overload the initial fluid administered is only 1/8 of the first 50% of the volume calculated and the urine output is measured at the end of 1 h.
The fluid infusion to the patient was adjusted to achieve an hourly urine output of 0.5–1.0 mL/kg/h and mean arterial pressure values greater than 70 mmHg.9, 10, 11 A fall in the parameters was adjusted with bolus dose of crystalloid infusion. An hourly critical care flow chart was used to determine the actual crystalloid resuscitation volume received by the patient, the hourly urine output over the first 24 h, the central venous pressure and the mean arterial blood pressure (MAP) recorded for each hour during fluid resuscitation.
The data collected from the patient's record included age, sex, etiology of burns, total body surface area burn size, burn depth, inhalational injury, admission weight, fluid received by the patient and any evidence of fluid overload. The data was analyzed using SPSS 16.0 software.
Results
A total of 251 patients were admitted in our burns unit, of which 150 patients had sustained thermal burns injury involving more than 20% total body surface area (TBSA). Rest of the admitted patients had sustained either electrical burns or chemical burns or scald burns. Out of the 150 patients with thermal burns, 90 patients met the inclusion criteria.
Majority (70%) of the burn injuries were due to accidental fire injuries in kitchen commonly due to burst of kerosene stove which is still widely used in this part of the country. The study showed a younger population with majority comprising female population. These burns in an enclosed space led to many inhalational injuries (Table 1).
Table 1.
Patient demography (n = 90).
| Demographic variables | n (%) | Mean ± SD |
|---|---|---|
| Age (year) | 29.4 ± 11 | |
| Gender incidence | ||
| Female | 49 (54) | |
| Male | 41 (46) | |
| Etiology of burns | ||
| Kitchen accident | 63 (70) | |
| Self-immolation | 19 (22) | |
| Factory accident | 5 (5) | |
| Road accident | 3 (3) | |
| Percentage of burns TBSA (%) | 55 ± 24 | |
| Full thickness burns (%) | 40 ± 22 | |
| Inhalational burns | 36 (40) | |
| Reporting after initial burn (h) | 5.3 ± 3 | |
The extent of the burn in the study population ranged from 20% to 95% TBSA burns with a mean of 55% ± 24%. Most of the burn involved the trunk and the lower limb. No mortality was reported in the first 48 h from the time of burns. No cases of burn shock were reported. No signs of over resuscitation or under resuscitation were noticed.
The mean duration taken by the patient to reach hospital was (5.3 ± 3.1) h and the median was 4.4 h (Table 1). The delay in the presentation to hospital was due to the time taken for travel. There was big difference in the fluid calculated as per the Parkland formula (13030.7 mL) and actual fluid (9598.87 mL) administered to the patient (Difference = 3431.825 mL, p < 0.001). The fluid administered prior to admission was included in the total fluid calculation.
About 86.7% (n = 78) of the patients received fluid less than the calculated Parkland formula.
Patients who received fluid lesser than Parkland formula had higher burn size and greater percentage of full thickness burns whereas the percentage of inhalational injury was higher in patients who received fluid above Parkland formula (Table 2).
Table 2.
Different resuscitation fluid volume and the average percentage of TBSA burns and full thickness burns and inhalational injury in each group.
| Fluid administered | n (%) | Average percentage of TBSA burn (%) | Deep burns (average burns in %TBSA) | Inhalational injury (%) |
|---|---|---|---|---|
| >Parkland formula | 10 (11.1) | 45 | 32.8 | 6/10 (60) |
| <Parkland | 78 (86.7) | 56.9 | 42.1 | 28/78 (35.9) |
| = Parkland | 2 (2.2) | 45 | 30 | 2/2 (100) |
TBSA: Total body surface area.
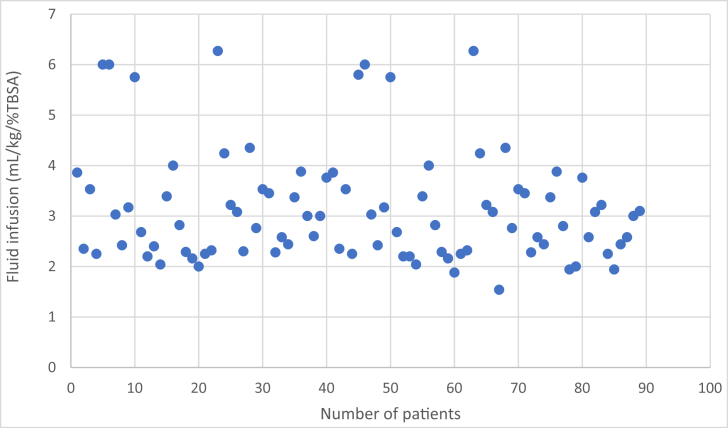
The scattered diagram (Fig. 1) shows the rate of fluid infusion among the patients which were clustered in the range of 2–4 mL/kg/percentage of burns. Mean rate of fluid administered over 24 h in our study was 3.149 mL/kg/h. There was no evidence of resuscitation morbidities in the study. Mean urine output was found to be 1424.05 mL/day. The mean hourly urine output was found to be 0.993 mL/kg/h, which was within the normal range of 0.5–1.0 mL/kg/h. Hourly urine output above 1.5 mL/kg/h was taken as criteria of over-resuscitation.
Fig. 1.
Fluid infusion (mL) per body weight (kg) per total body surface area (mL/kg/%TBSA). The above scattered plotting shows the distribution of the rate of fluid infused. The majority are clustered in the range of 2–4 mL/kg/percentage of burns.
Thirty-six (36/90) patients had inhalational injury. The significant number of inhalational injuries has been due to higher incidence of accidents in an enclosed space and self-immolation (Table 1). The rate of fluid administered in the burn patients with inhalational injury (3.36 mL/kg/%TBSA) was higher in comparison the average study value of 3.14 mL/kg/%TBSA.
Discussion
The crystalloid based resuscitation fluid is widely used for the acute burns, the commonest is the Parkland formula. Recently the accuracy of the Parkland formula is being questioned.12, 13 According the study by Luo et al. resuscitation commencing 8 h after injury has been shown to have greater complications and requirement of increase fluid resuscitation volume.6
The study showed a young group of the population involved in major burns with majority of the patient being female. The reasons for the predominant female population were related to occupation they are employed in this part of the country, cooking and house hold activities. Their susceptibility to fire accident was due to traditional dress (saree) they wear and the placement of cooking stoves on the floor. In the male population, factory accident has been the major cause.
The goal of resuscitation of the burned patient is to provide enough fluid to maintain organ function, whilst avoiding the complications of over-resuscitation. Cartotto et al.12 recently reported that fluid volumes administered during burn resuscitation frequently are in excess of what was estimated by the Parkland formula. In their study, resuscitation fluid volume exceeded Parkland formula in 45% of the patients. In the study by Chung et al.,13 comparison of Parkland formula and modified Brooke formula, patient on Parkland Formula received more volume of fluid as compared to Brooke formula based patient. Luo et al.6 in their study of TMMU (Third Military Medical University) protocol reported average amount of fluid actually infused was 2.33 mL/kg/percentage of TBSA burns in the first 24 h of resuscitation period with highest being 3.12 mL. In our study we found that the Parkland formula over estimates the resuscitation fluid volume required for the patient. Majority (87%) of our patients received fluid in the range of 3.14 mL/kg/percentage TBSA burns which was less than the Parkland formula of 4 mL/kg/percentage of burns. The fluid infusion was titrated based on the hourly urine output. No evidence of fluid overload was reported in the study. No evidence of hypoperfusion noted in the study. Only 11% of the patients received fluid more than Parkland formula and higher percentage of these patients were associated inhalational injury (Table 2). The hourly urine output was maintained in the range 0.5–1.0 mL/kg/h.
The significant difference in the resuscitation fluid questions our resuscitation protocol- Have we under resuscitated our patients?
An adequate resuscitation can be judged by the tissue perfusion and the end point target like the urine output. Rate of urine output is considered as indirect measure of cardiac output. In our study patient's fluid infusion was titrated with hourly urine output. The mean urine output over 24 h was (1424 ± 750) mL. The rate of urine output was (0.99 ± 0.49) mL/kg/h which was in the desired range of 0.5–1.0 mL/kg/h. There was no evidence of signs of under -resuscitation in the patient. The Parkland formula divides the fluid resuscitation volume into two parts, half of the volume calculated is given in the first 8 h from the time of incident and next half in next 16 h. While in the study the fluid was administered as per the hourly urine output, this helps to assess the patient on hourly basis and infuse fluid continuously in physiological manner.
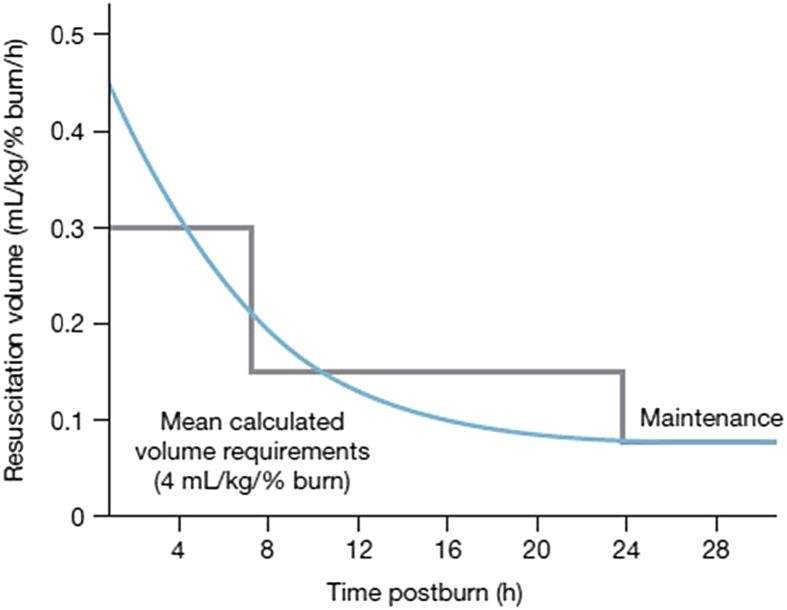
The relationship between fluid volume required and time since the burn injury is depicted by a smooth curve.14 This physiological curve (Fig. 2) represents the influence of temporal changes in microvascular permeability and tissue edema as well as fluid needs in the first 24 h of burn injury. The curve contrasts with abrupt changes in fluid infusion rate as prescribed by the Parkland formula. This avoids bolus of fluid over a period. Subsequently the Parkland formula decreases the fluid infusion in next 16 h to half which is an abrupt change in fluid infusion rate and not depended on the tissue perfusion. While the fluid infusion based on urine output follows a physiological curve as hourly urine output is monitored to titrate the infusion rate.
Fig. 2.
Physiological curve of fluid infusion requirements15 shows rate of fluid requirement against time post burn.
In hypovolemic shock there is decrease in capillary pressure due arteriolar vasoconstriction. In burns shock the capillary pressure doubles in first half an hour and then returns to baseline.15 So an aggressive infusion of crystalloids might extend the period of increased capillary pressure, causing continuous fluid extravasation and prolonged ‘‘feeding’’ of the burn edema.16 During the Parkland resuscitation of burns, there is aggressive fluid infusion in the first 8 h post burn, which if not monitored and titrated on timely basis may cause fluid creep. A strict titration on the fluid infusion based on end target of resuscitation could help avoid over-resuscitation.
The end point of the resuscitation was within the normal range to suggest that the fluid resuscitation was adequate in the study group. Even in the large burns the fluid infused was far less than calculated Parkland formula, the urine output was maintained at normal range. There was no mortality in the first 48 h from the time of burn injury. Patients in our study received only crystalloid fluid. Boluses of crystalloid were given when indicated but colloid was avoided in first 24 h. Only after 24 h plasma was transfused at the rate of 0.5 mL/kg/h. Extremity edema was seen on the patient, but none required escharotomy or fasciotomy in the first 48 h and treated with splinting and elevation.
Our study suggests that any formula serves only as a starting or guiding point. We should evaluate the circulation comprehensively and adjust the resuscitation according to heart rate, blood pressure, urine output, central venous pressure (CVP), blood routine examination, respiration and any signs of extremity compartment. The study showed the fluid requirement was 3.14 mL/kg/percentage of TBSA, which was less than the parkland formula. The Parkland formula overestimates the fluid requirement in the first 24 h of acute burns.
The study showed a significant difference in the fluid infused based on urine output and the fluid calculated by Parkland formula. This probably is because fluid infused based on end point of resuscitation (urine output and CVP) was more physiological than fluid calculated based on formulae. There is smooth infusion of fluid based on the tissue need when resuscitated based on the end target of resuscitation and abrupt changes in fluid infused when boluses of fluid as seen in the existing resuscitation formulae.
The result shows that the resuscitation regimens are guidelines to estimate the starting fluid volume and fluid resuscitation in burns patient should be individually assessed and monitored.
Funding
None.
Ethical statement
IRB Min No: 9399 [OBSERVE] dated 02.04.2015.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Parvizi D., Kamolz L.P., Giretzlehner M. The potential impact of wrong TBSA estimations on fluid resuscitation in patients suffering from burns: things to keep in mind. Burns. 2014;40:241–245. doi: 10.1016/j.burns.2013.06.019. [DOI] [PubMed] [Google Scholar]
- 2.Baxter C.R. Management of fluid volume and electrolyte changes in the early post burn period. Geriatr Nurs. 1975:57–62. [PubMed] [Google Scholar]
- 3.Cartotto R.C., Innes M., Musgrave M.A. How well does the Parkland formula estimate actual fluid resuscitation volumes? J Burn Care Rehabil. 2002;23:258–265. doi: 10.1097/00004630-200207000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Dulhunty J.M., Boots R.J., Rudd M.J. Increased fluid resuscitation can lead to adverse outcomes in major-burn injured patients, but low mortality is achievable. Burns. 2008;34:1090–1097. doi: 10.1016/j.burns.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 5.Saffle J.R. The phenomenon of “Fluid Creep” in acute burn resuscitation. J Burn Care Res. 2007;28:382–395. doi: 10.1097/BCR.0B013E318053D3A1. [DOI] [PubMed] [Google Scholar]
- 6.Luo G., Peng Y., Yuan Z. Fluid resuscitation for major burn patients with the TMMU protocol. Burns. 2009;35:1118–1123. doi: 10.1016/j.burns.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 7.The Pathophysiology of inhalational injury . In: Total Burn Care. 4th edition. Herndon D.N., editor. Saunders Elsevier; Edinburgh, New York: 2012. pp. 229–237. [DOI] [Google Scholar]
- 8.Klein M.B., Hayden D., Elson C. The association between fluid administration and outcome following major burn: a multicenter study. Ann Surg. 2007;245:622–628. doi: 10.1097/01.sla.0000252572.50684.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cancio L.C. Initial assessment and fluid resuscitation of burn patients. Surg Clin. 2014;94:741–754. doi: 10.1016/j.suc.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 10.Diver A.J. The evolution of burn fluid resuscitation. Int J Surg. 2008;6:345–350. doi: 10.1016/j.ijsu.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Tricklebank S. Modern trends in fluid therapy for burns. Burns. 2009;35:757–767. doi: 10.1016/j.burns.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 12.Cartotto R. Fluid resuscitation of the thermally injured patient. Clin Plast Surg. 2009;36:569–581. doi: 10.1016/j.cps.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 13.Chung K.K., Wolf S.E., Cancio L.C. Resuscitation of severely burned military casualties: fluid begets more fluid. J Trauma. 2009;67:231–237. doi: 10.1097/TA.0b013e3181ac68cf. [DOI] [PubMed] [Google Scholar]
- 14.Warden G.D. Fluid resuscitation and early management. In: Herndon D.N., editor. Total Burn Care. 4th edition. Saunders Elsevier; Edinburgh, New York: 2012. pp. 115–124. [DOI] [Google Scholar]
- 15.Pitt R.M., Parker J.C., Jurkovich G.J. Analysis of altered capillary pressure and permeability after thermal injury. J Surg Res. 1987;42:693–702. doi: 10.1016/0022-4804(87)90013-8. [DOI] [PubMed] [Google Scholar]
- 16.Holm C., Mayr M., Tegeler J. A clinical randomized study on the effects of invasive monitoring on burn shock resuscitation. Burns. 2004;30:798–807. doi: 10.1016/j.burns.2004.06.016. [DOI] [PubMed] [Google Scholar]