Abstract
Introduction
Patients with atrial fibrillation (AF) receiving non-vitamin K oral anticoagulants (NOAC) have a slower decline in renal function than those taking warfarin. Moreover, a warfarin-related nephropathy has been described.
Aim
We assessed variation of estimated glomerular filtration rate (eGFR) and occurrence of contrast-induced nephropathy (CIN) after percutaneous coronary intervention (PCI) in patients with AF taking warfarin compared with NOAC.
Material and methods
We retrospectively enrolled consecutive patients taking oral anticoagulation for AF undergoing PCI. The primary endpoint was variation in eGFR and serum creatinine levels within 48–72 h after PCI. The secondary endpoint was occurrence of CIN, defined as a ≥ 25% relative increase, or a ≥ 0.5 mg/dl absolute increase, in serum creatinine levels within 48–72 h.
Results
We enrolled 420 patients (mean age: 75.0 ±5.5 years, 272 (64.7%) male), 124 (29.5%) treated with NOAC and 296 (70.5%) with warfarin. NOAC patients showed a reduced decline in renal function (eGFR change: –2.8 ±7.9 ml/min/1.73 m2 vs. –4.5 ±6.5 ml/min/1.73 m2, respectively, p = 0.02) and a smaller increase in serum creatinine levels (0.026 ±0.112 vs. 0.055 ±0.132, p = 0.032) after PCI compared with warfarin. In the multivariate linear regression model independent predictors of eGFR changes were diabetes, baseline eGFR ≤ 60 ml/min/1.73 m2 and warfarin use. Occurrence of CIN did not differ between NOAC and warfarin patients (13 (10.5%) vs. 46 (15.5%), p = 0.22).
Conclusions
Patients with AF taking NOAC have a reduced decline in renal function after PCI compared with warfarin. The NOAC may be a reasonable option for patients with a high risk of developing CIN.
Keywords: percutaneous coronary intervention, warfarin, atrial fibrillation, non-vitamin K oral anticoagulants, contrast-induced nephropathy
Summary
Patients with atrial fibrillation (AF) receiving non-vitamin K oral anticoagulants (NOAC) have a slower decline in renal function than those taking warfarin. Moreover, a warfarin-related nephropathy has been described. Our study demonstrated that patients with AF taking NOAC have a reduced decline in renal function after percutaneous coronary intervention compared with warfarin. The NOAC may be a reasonable option for patients with a high risk of developing contrast-induced nephropathy.
Introduction
Percutaneous coronary interventions (PCI) in patients with atrial fibrillation (AF) requiring oral anticoagulation account for up to 5–10% of all PCI procedures [1, 2]. Although warfarin has been commonly used for more than 60 years in patients with AF, its harmful effects on renal function, so-called warfarin-related nephropathy (WRN), have only recently been recognized [3–5]. Indeed, it is estimated that as many as 20.5% of all patients taking warfarin have experienced at least an episode of WRN during their treatment course [4, 6]. In recent years, non-vitamin K oral anticoagulants (NOAC) have been increasingly used for the prevention of ischemic stroke and systemic embolism in patients with AF as a safer alternative to warfarin with a lower risk of intracranial hemorrhage and other causes of major bleeding [7–11]. Interestingly, a post-hoc analysis of the RE-LY trial [5] indicated that patients with AF receiving dabigatran exhibited a slower decline in renal function than those taking warfarin, and another study demonstrated that among Asians with AF, dabigatran was associated with a lower risk of acute kidney injury (AKI) than warfarin [12]. Moreover, a recent large registry showed that renal function decline is common among patients with AF treated with oral anticoagulant agents. However, NOAC, particularly dabigatran and rivaroxaban, were associated with a slower decline in renal function and with lower risks of adverse renal outcomes than warfarin [13].
Contrast-induced nephropathy (CIN) is a prevalent but underdiagnosed complication of PCI that is associated with increased in-hospital morbidity and mortality [14, 15]. The importance of this complication is being increasingly recognized, with an incidence that ranges from 2.0% in patients with normal baseline renal function to as high as 20–30% in patients with a baseline creatinine > 176 μM (or 2.0 mg/dl) prior to PCI [14]. Nash et al. [16] reported that 11% of hospital-acquired renal insufficiency cases are due to contrast media, with coronary angiograms and PCI being the leading causes. Nevertheless, there are no data about the risk of CIN according to different types of oral anticoagulation in patients undergoing PCI.
Aim
In this study, we aimed to asses variation of estimated glomerular filtration rate (eGFR) and the occurrence of CIN after PCI in patients with AF taking warfarin compared with patients taking NOAC.
Material and methods
Study design and patient population
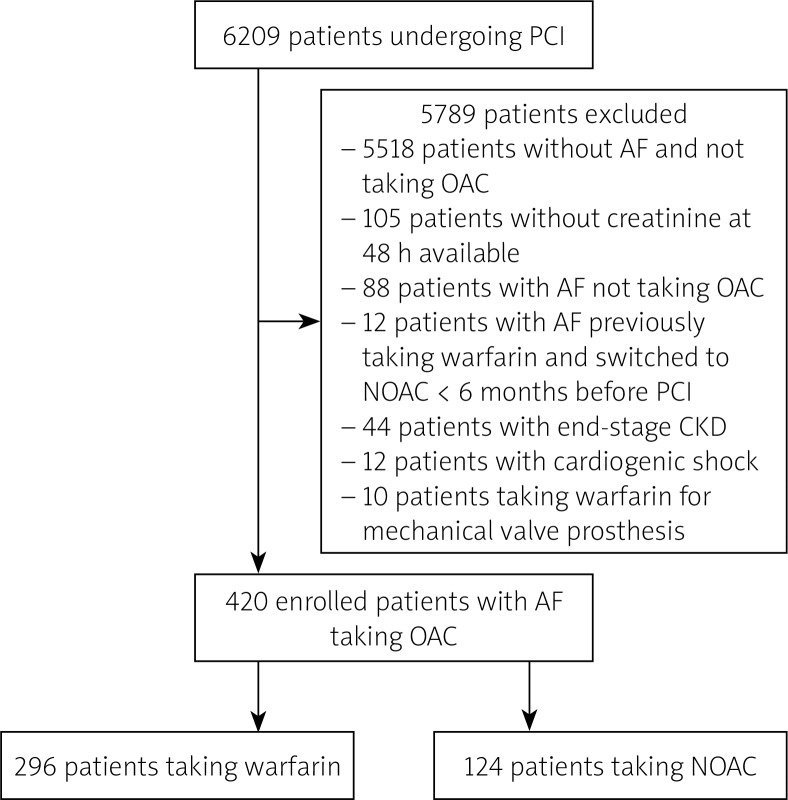
We retrospectively enrolled consecutive patients undergoing PCI in three hospitals in Italy and taking oral anticoagulation for AF. The enrolment period was from January 2015 to September 2017. Exclusion criteria were: end-stage renal disease with an eGFR < 30 ml/min/1.73 m2 (n = 44 patients); patients had started taking warfarin and then switched to NOAC < 6 months before PCI (n = 12 patients); emergent PCI with cardiogenic shock (defined as prolonged hypotension with systolic blood pressure < 90 mm Hg for at least 30 min or requiring inotropic support medication and/or intra-aortic balloon pump to maintain systolic blood pressure > 90 mm Hg) (n = 12 patients) (Figure 1).
Figure 1.
Study flow chart of enrolled patients
AF – atrial fibrillation, CKD – chronic kidney disease, NOAC – non-vitamin K oral anticoagulants, OAC – oral anticoagulation, PCI – percutaneous coronary intervention.
Procedure protocol
Coronary stenting with either bare-metal or drug-eluting stents was performed according to standard practice [17]. Radial access was the preferred choice in order to reduce bleeding complications [17]. In non-urgent patients taking warfarin PCI was performed without interrupting oral anticoagulation; in non-urgent NOAC patients PCI was performed stopping NOAC 48 h before the procedure without bridging therapy [18]. Urgent patients underwent PCI without stopping oral anticoagulation. After PCI all patients were treated with aspirin (75–100 mg/day) and clopidogrel (75 mg/day) for at least 1–6 months, along with oral anticoagulation, according to recommendations of guidelines [18]. Other drugs, including angiotensin converting enzyme inhibitors/angiotensin II receptor blockers, β-blockers, calcium channel blockers, diuretics and statin, were left to the discretion of the cardiologists according to the clinical requirements or recommendations of guidelines.
All patients undergoing elective PCI and with an eGFR < 60 ml/min/1.73 m2 received intravenous pre-hydration with NaCl 0.9% (1–1.5 ml/kg/h) for 12 h before PCI and continuing for 12–24 h after the procedure. Metformin was discontinued 48 h before in all diabetic patients. Patients undergoing urgent PCI for acute coronary syndrome received an infusion of NaCl 0.9% (3 ml/kg/h) for one hour followed by 1 ml/kg/h for 12 h. In patients with an eGFR < 60 ml/min/1.73 m2 N-acetylcysteine was administered in all elective PCI (1200 mg per o.s. b.i.d. for 24 h before and 48 h after PCI) and urgent PCI (1200 mg per o.s. b.i.d. for 48 h after PCI) [19].
Endpoint definition
The predefined primary endpoint of our study was the variation in eGFR and serum creatinine levels after PCI. Serum creatinine (SCr) levels were assessed before PCI and at 48–72 h and eGFR was calculated using the Modification of Diet in Renal Disease (MDRD) study group equation [20].
The secondary endpoint was the occurrence of CIN, defined as a ≥ 25% relative increase, or a ≥ 0.5 mg/dl (44 mmol/l) absolute increase, in SCr levels within 48–72 h of contrast exposure [15].
We also recorded the need for use of renal replacement therapy (RRT) after PCI during the index admission. The decision to use RRT was made in patients with oligo-anuria (urine output < 20 ml/h for 24 h) despite the administration of more than 1 γ of intravenous furosemide and presence of volume overload. Moreover, episodes of peri-procedural major bleeding according to the Bleeding Academic Research Consortium (BARC) classification defined as BARC ≥ class 2 were also recorded [21].
Statistical analysis
Data distribution was assessed according to the Kolmogorov-Smirnov test. Continuous variables were compared using the unpaired Student’s t-test or Mann-Whitney U-test, as appropriate, and data were expressed as mean ± standard deviation (SD) or as median (range). Categorical data were evaluated using the c2 test or Fisher’s exact test as appropriate. All tests were two-sided, and a p-value ≤ 0.05 represented statistically significant differences.
Predefined subgroup analysis evaluating the occurrence of CIN according to the presence of a baseline eGFR ≤ 60 ml/min/1.73 m2, diabetes, age > 75 years, contrast volume > 150 ml, ACS as clinical presentation or CHA2DS2-VASc score ≥ 4 was planned.
Univariate linear regression analysis was applied to assess the relation of individual variables with change in eGFR. A multivariate linear regression model was then performed to identify variables independently associated with change in eGFR; to this aim we included in the multivariate model only variables showing a p-value ≤ 0.05 in univariate analysis. All analyses were performed using SPSS version 20 (SPSS Inc., Chicago, IL, USA).
Results
Baseline clinical characteristics according to type of oral anticoagulation
We enrolled 420 patients (mean age: 75.0 ±5.5 years, 272 (64.7%) male) taking oral anticoagulation for AF and undergoing PCI. In particular, 124 (29.5%) patients were treated with NOAC and 296 (70.5%) patients with warfarin. Main clinical and procedural characteristics were similar between patients taking NOAC or warfarin (Table I). Baseline eGFR (67.5 ±18.4 vs. 68.1 ±16.5, p = 0.74) and number of patients with baseline eGFR ≤ 60 ml/min/1.73 m2 (28 (22.6%) vs. 61 (20.6%), p = 0.65) were similar between NOAC and warfarin patients. Of importance, among NOAC patients dabigatran etexilate was the most commonly used oral anticoagulant (59.7%), followed by apixaban (21.0%), rivaroxaban (18.7%), and edoxaban (0.8%) (Table I).
Table I.
Clinical and procedural characteristics of overall study population and according to type of oral anticoagulation
| Variables | All patients (n = 420) | Patients taking NOAC (n = 124) | Patients taking warfarin (n = 296) | P-value |
|---|---|---|---|---|
| Clinical characteristics: | ||||
| Age, mean ± SD [years] | 75.0 ±5.5 | 75.7 ±5.8 | 74.7 ±5.3 | 0.09 |
| Male, n (%): | 272 (64.7) | 75 (60.4) | 197 (66.5) | 0.24 |
| Clinical presentation, n (%): | 0.66 | |||
| ACS | 163 (38.8) | 46 (37.1) | 117 (39.5) | |
| Stable angina | 257 (61.2) | 78 (62.9) | 179 (60.5) | |
| Risk factors, n (%): | ||||
| Smoking | 185 (44.0) | 55 (44.3) | 130 (43.9) | 0.93 |
| Hypertension | 354 (84.3) | 105 (84.7) | 249 (84.1) | 0.89 |
| Hypercholesterolemia | 230 (54.8) | 64 (51.6) | 166 (56.1) | 0.40 |
| Diabetes mellitus | 145 (34.5) | 47 (37.9) | 98 (33.1) | 0.37 |
| Obesity (BMI > 30 kg/m2) | 75 (17.9) | 24 (19.4) | 51 (17.2) | 0.60 |
| Family history of CAD | 113 (26.9) | 29 (23.4) | 84 (28.4) | 0.29 |
| Previous history, n (%): | ||||
| Previous ACS | 31 (7.3) | 10 (8.1) | 21 (7.1) | 0.56 |
| Previous PCI | 95 (22.6) | 31 (25.0) | 64 (21.6) | 0.47 |
| Previous CABG | 13 (3.1) | 4 (3.2) | 9 (3.0) | 1.0 |
| Congestive heart failure | 65 (15.5) | 20 (16.1) | 45 (15.2) | 0.88 |
| eGFR, mean ± SD [ml/min/1.73 m2] | 67.9 ±18.8 | 67.5 ±18.4 | 68.1 ±16.5 | 0.74 |
| Patients with eGFR < 60 ml/min/1.73 m2, n (%) | 132 (31.4) | 39 (31.4) | 93 (31.4) | 1.0 |
| CHA2DS2-VASc, mean ± SD | 3.94 ±1.95 | 3.89 ±1.88 | 3.96 ±1.56 | 0.69 |
| Medications at admission, n (%): | ||||
| Antiplatelet therapy | 138 (32.9) | 48 (38.7) | 90 (30.4) | 0.11 |
| β-Blockers | 313 (74.5) | 98 (79.0) | 215 (72.6) | 0.14 |
| ACE inhibitors/ARB | 273 (65.0) | 80 (64.5) | 193 (65.2) | 0.91 |
| Statins | 268 (63.8) | 77 (62.0) | 191 (64.5) | 0.66 |
| Insulin | 55 (13.1) | 19 (15.3) | 36 (12.1) | 0.43 |
| Oral hypoglycemic agents | 108 (25.7) | 35 (28.2) | 73 (24.7) | 0.46 |
| NOAC type: | ||||
| Dabigatran etexilate | 74 (17.6) | 74 (59.7) | – | |
| Rivaroxaban | 23 (5.5) | 23 (18.5) | – | |
| Apixaban | 26 (6.2) | 26 (21.0) | – | |
| Edoxaban | 1 (0.2) | 1 (0.8) | – | |
| Procedural characteristics: | ||||
| Access type: | 0.60 | |||
| Femoral | 88 (21.0) | 24 (19.4) | 64 (21.2) | |
| Radial | 331 (78.8) | 100 (80.6) | 231 (78.0) | |
| Other | 1 (0.2) | 0 (0.0) | 1 (0.8) | |
| Primary PCI | 44 (10.5) | 13 (10.4) | 31 (10.5) | 1.0 |
| Multivessel PCI | 37 (8.8) | 12 (9.7) | 25 (8.4) | 0.71 |
| Contrast volume, mean ± SD [ml] | 164.9 ±80.5 | 160.7 ±82.6 | 166.7 ±80.8 | 0.49 |
| Pre-PCI i.v. hydration [ml] | 427 ±231 | 445 ±243 | 420 ±205 | 0.13 |
| Peri-procedural major bleeding | 26 (6.2) | 8 (6.4) | 18 (6.1) | 0.83 |
ACS – acute coronary syndrome, ACE – angiotensin-converting enzyme, ARB – angiotensin-receptor blockers, BMI – body mass index, CABG – coronary artery bypass grafting, eGFR – estimated glomerular filtration rate, i.v. – intravenous, PCI – percutaneous coronary intervention.
Changes in renal function according to type of oral anticoagulation
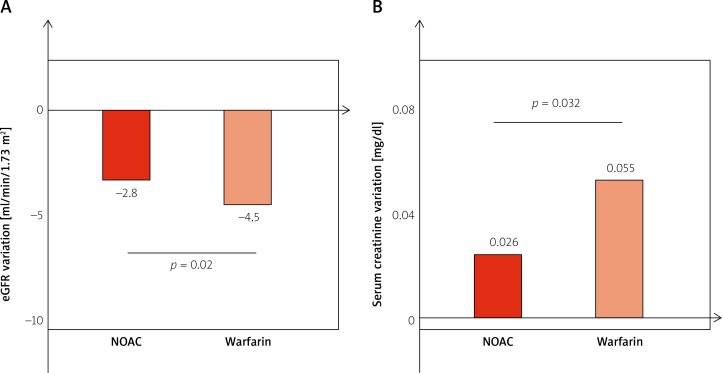
Patients in the NOAC group had a reduced decline in renal function after PCI compared with patients in the warfarin group (Table II). In particular, the eGFR change was –2.8 ±7.9 ml/min/1.73 m2 in the NOAC group and –4.5 ±6.5 ml/min/1.73 m2 in the warfarin group (p = 0.02) (Figure 2). Accordingly, SCr levels after PCI had a smaller increase in NOAC patients compared with warfarin patients (0.026 ±0.112 vs. 0.055 ±0.132, p = 0.032) (Figure 2).
Table II.
Occurrence of endpoints in overall population and according to type of oral anticoagulation
| Variables | All patients (n = 420) | Patients taking NOAC (n = 124) | Patients taking warfarin (n = 296) | P-value |
|---|---|---|---|---|
| Change in eGFR, mean ± SD [ml/min/1.73 m2] | –3.96 ±6.9 | –2.8 ±7.9 | –4.5 ±6.5 | 0.02 |
| Change in SCr, mean ± SD [mg/dl] | 0.046 ±0.109 | 0.026 ±0.112 | 0.055 ±0.132 | 0.032 |
| Occurrence of CIN, n (%) | 59 (14.0) | 13 (10.5) | 46 (15.5) | 0.22 |
| Need for RRT, n (%) | 9 (2.1) | 2 (1.6) | 7 (2.3) | 1.0 |
CIN – contrast-induced nephropathy, eGFR – estimated glomerular filtration rate, RRT – renal replacement therapy, SCr – serum creatinine.
Figure 2.
Mean post-procedural change in eGFR (A) and serum creatinine levels (B) according to type of oral anticoagulation
In univariate linear regression analysis, predictors of decline in eGFR were diabetes (β = –4.01, 95% CI: –5.36 – –2.66, p = 0.001), baseline eGFR ≤ 60 ml/min/1.73 m2 (β = –3.56, 95% CI: –4.96 – –2.17, p = 0.001), CHA2DS2-VASc score ≥ 4 (β = –1.44, 95% CI: –2.80 – –0.08, p = 0.038), contrast volume (β = –1.53, 95% CI: –4.24 – –0.27, p = 0.022), ACS as clinical presentation (β = –1.50, 95% CI: –2.86 – –0.14, p = 0.031), and warfarin use (β = –1.66, 95% CI: –3.11 – –0.20, p = 0.025) (Table III). Of note, prior metformin use and statin therapy at admission did not predict eGFR changes after PCI.
Table III.
Variables associated with eGFR variation in univariate and multivariate linear regression analysis
| Parameter | Univariate analysis | Multivariate analysis (R2 = 0.11) | ||
|---|---|---|---|---|
| β (95% CI) | P-value | β (95% CI) | P-value | |
| Diabetes | –4.01 (–5.36 – –2.66) | 0.001 | –3.08 (–4.76 – –1.40) | 0.001 |
| CHA2DS2-VASc score ≥ 4 | –1.44 (–2.80 – –0.08) | 0.038 | – | NS |
| Baseline eGFR < 60 ml/min/1.73 m2 | –3.56 (–4.96 – –2.17) | 0.001 | –1.64 (–3.29 – –0.003) | 0.05 |
| Contrast volume > 150 ml | –2.67 (–4.57 – –0.77) | 0.006 | – | NS |
| ACS as clinical presentation | –1.50 (–2.86 – –0.14) | 0.031 | – | NS |
| Warfarin vs. NOAC therapy | –1.66 (–3.11 – –0.20) | 0.025 | –1.59 (–2.99 – –0.18) | 0.027 |
ACS – acute coronary syndrome, eGFR – estimated glomerular filtration rate, NOAC – non-vitamin K oral anticoagulant. Regression coefficients (β) with 95% confidence intervals (95% CI) and p-values for the univariate and multivariate analysis. R2 displayed for the multivariate model.
Of importance, in the multivariate linear regression model independent predictors of eGFR changes at 48–72 h were diabetes (β = –3.08, 95% CI: –4.76 – –1.40, p = 0.001), baseline eGFR ≤ 60 ml/min/1.73 m2 (β = –1.64, 95% CI: –3.29 – –0.003, p = 0.05) and warfarin use (β = –1.59, 95% CI: –2.99 – –0.18, p = 0.027).
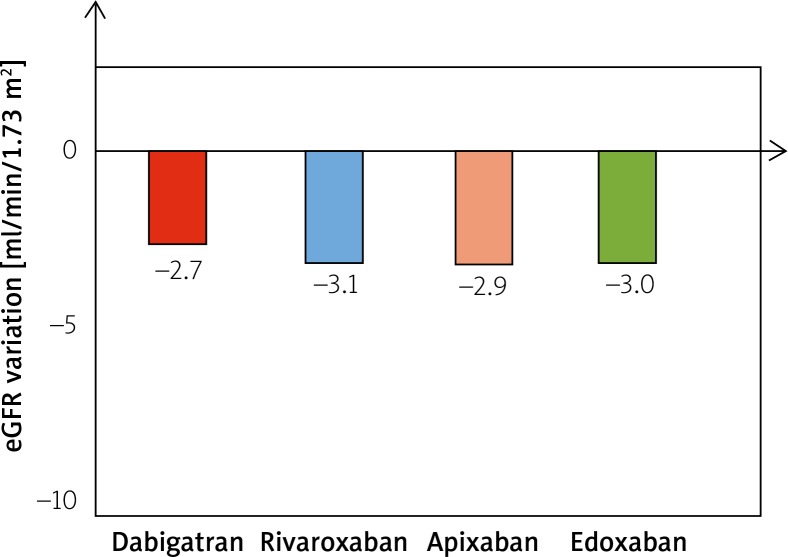
Finally, among NOAC patients a subgroup analysis did not show significant differences in eGFR change according to type of NOAC used (Figure 3).
Figure 3.
Mean post-procedural change in eGFR across different types of NOAC. P-values are not significant for all comparisons between groups
Occurrence of contrast-induced nephropathy and need for renal replacement therapy according to type of oral anticoagulation
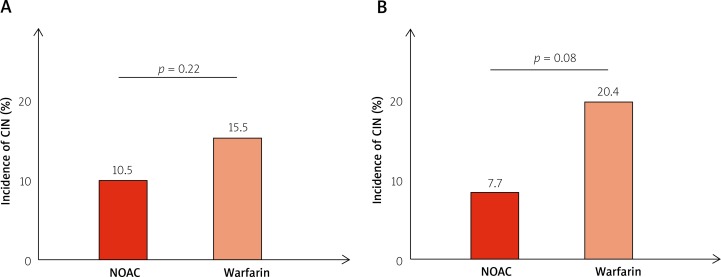
In the overall population, occurrence of CIN did not differ between NOAC and warfarin patients (13 (10.5%) vs. 46 (15.5%), p = 0.22, respectively). In a predefined subgroup analysis considering only patients with impaired renal function (eGFR ≤ 60 ml/min/1.73 m2), the occurrence of CIN was higher, although not significantly, among warfarin patients compared with NOAC patients (3 (7.7%) vs. 19 (20.4%), p = 0.08, respectively) (Figure 4). Of note, clinical characteristics of patients with baseline eGFR ≤ 60 ml/min/1.73 m2 were not different between NOAC and warfarin patients. No significant differences in the occurrence of CIN were observed between NOAC and warfarin patients in predefined subgroup analysis according to the presence of diabetes, age > 75 years, contrast volume > 150 ml, ACS as clinical presentation or CHA2DS2-VASc score ≥ 4.
Figure 4.
Incidence of contrast-induced nephropathy according to type of oral anticoagulation in the overall population (A) and in patients with baseline eGFR ≤ 60 ml/min/1.73 m2 (B)
Finally, there was no difference in the need for RRT between NOAC and warfarin patients (2 (1.6%) vs. 7 (2.3%), p = 1.0).
Discussion
Our study represents the first study evaluating the changes in renal function in patients with AF and undergoing PCI according to the type of oral anticoagulation. We demonstrated that patients taking warfarin have a significantly greater decline in renal function after PCI compared with patients taking NOAC. In multivariate analysis warfarin use, the presence of diabetes and a baseline eGFR ≤ 60 ml/min/1.73 m2 were independent predictors of an increased decline in renal function. Moreover, occurrence of CIN and need for RRT were similar between NOAC and warfarin patients, although rates of CIN were non-significantly higher among warfarin patients when considering only patients with an impaired baseline renal function (eGFR ≤ 60 ml/min/1.73 m2).
Worsening of renal function after exposure to contrast medium is a common drawback for patients undergoing PCI. Previous studies reported an incidence of CIN that ranged from 2.0% in patients with normal baseline renal function to as high as 20–30% in patients with impaired renal function prior to PCI [14, 22]. Indeed, when renal integrity is already impaired by disease, the kidney is less likely to tolerate the additional stresses conferred by excreting contrast medium. Therefore, one of the strongest risk factors associated with CIN is a pre-existing CKD [22, 23]. In this context, our study provides the first evidence suggesting that WRN may represent an underlying, often unrecognized, clinical condition that may predispose AF patients to a greater decline in renal function after PCI.
Of interest, a recent large registry [13] demonstrated that renal function decline is common among patients with AF treated with oral anticoagulant agents. Approximately 1 in 4 patients had at least a 30% decline in eGFR, and 1 in 7 had an episode of AKI within 2 years. In comparison with warfarin, treatment with NOAC was related to lower risks of ≥ 30% decline in eGFR, doubling of SCr, and AKI. The risk of kidney failure was also numerically lower in patients treated with NOAC compared with warfarin, but this was not statistically significant. In particular, the lower risk in renal outcomes was more evident for dabigatran and rivaroxaban patients. Of note, in a subgroup analysis, warfarin-treated patients with an average INR > 3 had much higher rates of eGFR decline of at least 30%, doubling of SCr, and AKI. However, in comparison with warfarin-treated patients whose mean INR was < 2 or 2 to 3, NOAC may still be associated with lower risks, suggesting that differential renal outcomes are not attributable solely to poor INR control with warfarin and that other mechanisms may be involved [13]. Of note, differences in the pattern of excretion of different NOAC do not seem to be involved in determining renal outcomes, probably because patients with end-stage renal disease are not included in clinical studies and because the choice of NOAC dosage is also determined by baseline renal function in order to avoid drug accumulation and over-anticoagulation.
Of importance, a post-hoc analysis from the RE-LY trial indicated that warfarin was associated with a greater decline in eGFR at follow-up than either low-dose or standard-dose dabigatran [5], in particular among patients with INR above the target range and in patients with diabetes. Moreover, a recent study enrolling Asian patients with AF demonstrated that dabigatran was associated with a lower risk of AKI at follow-up compared with warfarin, whether or not patients had any prior kidney disease [12]. Of interest, patients who took warfarin had an increased risk of AKI as the CHA2DS2-VASc score increased in both the CKD-free and CKD cohorts. Conversely, the annual incidence of AKI for dabigatran users remained stable despite the increase in CHA2DS2-VASc score [12]. In contrast, a recent meta-analysis demonstrated that the risk of renal failure deriving from the use of NOAC (dabigatran, apixaban, or rivaroxaban) was similar to that with warfarin or low molecular-weight heparin [24]; however, it was noted that rivaroxaban was associated with an increased risk of creatinine elevation in the J-ROCKET and RECORD 1–2 trials [25–27], probably suggesting a different effect in renal function according to the type of NOAC.
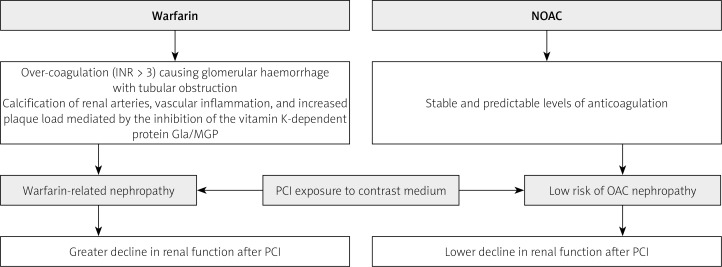
Previous studies showed that warfarin might directly induce a nephropathy due to different pathogenic mechanisms (Figure 5). In particular, severe glomerular hemorrhage caused by over-coagulation seems to play a major role. Indeed, pathological studies showed that kidney biopsies of patients taking warfarin and with INR > 3 presented severe glomerular hemorrhage and consequent tubular obstruction with many renal tubular cross sections filled with red blood cells, including red blood cell casts. Remarkably, the glomeruli were normal or nearly normal by light, immunofluorescence, and electron microscopy, suggesting that the massive glomerular hemorrhage was not explained by traditional measures of glomerular injury [4, 28, 29]. However, the finding that NOAC patients had a slower decline in renal function compared with warfarin patients having a mean INR < 2 or 2 to 3 suggests that mechanisms other than glomerular hemorrhage induced by over-coagulation are involved [13]. Indeed, warfarin may also induce calcification of renal arteries, vascular inflammation, and increased plaque load mediated by the inhibition of the vitamin K-dependent protein γ carboxyglutamic acid (matrix Gla protein) [30, 31]. Moreover, the decline in eGFR may be amplified by several atherosclerotic factors, including diabetes, and warfarin use has been correlated with other rare renal complications, including allergic interstitial nephritis, spontaneous atheromatous embolism, and renal pelvis/ureteral hematomas [32]. Of importance, occurrence of WRN is associated with a higher risk of mortality and kidney morbidity [4, 6].
Figure 5.
Mechanisms explaining the greater decline in renal function after PCI in warfarin-treated patients compared with NOAC patients
NOAC – non-vitamin K oral anticoagulants, OAC – oral anticoagulant, PCI – percutaneous coronary intervention.
The benefit in terms of renal function of NOAC compared with warfarin may be related to a more predictable dose-response effect and a lower risk of over-coagulation (Figure 5). However, a few case reports describing dabigatran-related AKI have been reported [33, 34]. Moreover, in a nephrectomy rat model with CKD dabigatran resulted in a dose-dependent increase in SCr and haematuria in both control and CKD rats [35]. Of note, both CKD and control rats took high doses of dabigatran, thus suggesting that nephropathy may also occur with NOAC in case of over-coagulation [28].
Our study has several limitations. First, our study has a retrospective design and we cannot exclude the presence of a selection bias between NOAC and warfarin patients. Second, we demonstrated a greater decline in post-PCI renal function among warfarin-treated patients. However, whether this finding translates into a different clinical outcome cannot be deduced from our study. Thus, larger prospective studies are needed in order to confirm our results. Third, we have no data about time in the therapeutic INR range prior to PCI for patients taking warfarin and the consequent individual risk of WRN related to over-coagulation. Finally, we have no data about life span in anticoagulant therapy prior to PCI. As a consequence, we cannot exclude a time-dependent effect on the renal function deriving from a different temporal exposure to anticoagulant therapy between NOAC and warfarin patients.
Conclusions
Our study shows for the first time that patients with AF taking warfarin have a significantly greater decline in renal function after PCI compared with patients taking NOAC. These findings suggest that patients taking warfarin should undergo accurate peri-procedural surveillance in order to avoid the occurrence of AKI. Moreover, the use of NOAC may be a reasonable option for patients with AF requiring oral anticoagulation and with a high risk of developing contrast-induced nephropathy.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Choi HI, Ahn JM, Kang SH, et al. Prevalence, management, and long-term (6-year) outcomes of atrial fibrillation among patients receiving drug-eluting coronary stents. JACC Cardiovasc Interv. 2017;10:1075–85. doi: 10.1016/j.jcin.2017.02.028. [DOI] [PubMed] [Google Scholar]
- 2.Sutton NR, Seth M, Ruwende C, Gurm HS. Outcomes of patients with atrial fibrillation undergoing percutaneous coronary intervention. J Am Coll Cardiol. 2016;68:895–904. doi: 10.1016/j.jacc.2016.05.085. [DOI] [PubMed] [Google Scholar]
- 3.Brodsky SV, Satoskar A, Chen J, et al. Acute kidney injury during warfarin therapy associated with obstructive tubular red blood cell casts: a report of 9 cases. Am J Kidney Dis. 2009;54:1121–6. doi: 10.1053/j.ajkd.2009.04.024. [DOI] [PubMed] [Google Scholar]
- 4.Brodsky SV, Nadasdy T, Rovin BH, et al. Warfarin-related nephropathy occurs in patients with and without chronic kidney disease and is associated with an increased mortality rate. Kidney Int. 2011;80:181–9. doi: 10.1038/ki.2011.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Böhm M, Ezekowitz MD, Connolly SJ, et al. Changes in renal function in patients with atrial fibrillation: an analysis from the RE-LY Trial. J Am Coll Cardiol. 2015;65:2481–93. doi: 10.1016/j.jacc.2015.03.577. [DOI] [PubMed] [Google Scholar]
- 6.An JN, Ahn SY, Yoon CH, et al. The occurrence of warfarin-related nephropathy and effects on renal and patient outcomes in Korean patients. PLoS One. 2013;8:e57661.. doi: 10.1371/journal.pone.0057661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Connolly SJ, Ezekowitz MD, Yusuf S, et al. RE-LY Steering Committee and Investigators Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 8.Granger CB, Alexander JH, McMurray JJ, et al. ARISTOTLE Committees and Investigators Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–92. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- 9.Patel MR, Mahaffey KW, Garg J, et al. ROCKET AF Investigators Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–91. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]
- 10.Giugliano RP, Ruff CT, Braunwald E, et al. ENGAGE AF-TIMI 48 Investigators Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–104. doi: 10.1056/NEJMoa1310907. [DOI] [PubMed] [Google Scholar]
- 11.Balsam P, Ozierański K, Tymińska A, et al. Comparison of clinical characteristics of real-life atrial fibrillation patients treated with vitamin K antagonists, dabigatran, and rivaroxaban: results from the CRAFT study. Kardiol Pol. 2018;76:889–98. doi: 10.5603/KP.a2018.0027. [DOI] [PubMed] [Google Scholar]
- 12.Chan YH, Yeh YH, See LC, et al. Acute kidney injury in Asians with atrial fibrillation treated with dabigatran or warfarin. J Am Coll Cardiol. 2016;68:2272–83. doi: 10.1016/j.jacc.2017.02.061. [DOI] [PubMed] [Google Scholar]
- 13.Yao X, Tangri N, Gersh BJ, et al. Renal outcomes in anticoagulated patients with atrial fibrillation. J Am Coll Cardiol. 2017;70:2621–32. doi: 10.1016/j.jacc.2017.09.1087. [DOI] [PubMed] [Google Scholar]
- 14.Rihal CS, Textor SC, Grill DE, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002;105:2259–64. doi: 10.1161/01.cir.0000016043.87291.33. [DOI] [PubMed] [Google Scholar]
- 15.Rear R, Bell RM, Hausenloy DJ. Contrast-induced nephropathy following angiography and cardiac interventions. Heart. 2016;102:638–48. doi: 10.1136/heartjnl-2014-306962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;39:930–6. doi: 10.1053/ajkd.2002.32766. [DOI] [PubMed] [Google Scholar]
- 17.Authors/Task Force members. Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Eur Heart J. 2014;35:2541–619. doi: 10.1093/eurheartj/ehu278. [DOI] [PubMed] [Google Scholar]
- 18.Lip GY, Windecker S, Huber K, et al. Management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary or valve interventions: a joint consensus document of the European Society of Cardiology Working Group on Thrombosis, European Heart Rhythm Association (EHRA), European Association of Percutaneous Cardiovascular Interventions (EAPCI) and European Association of Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm Society (HRS) and Asia-Pacific Heart Rhythm Society (APHRS) Eur Heart J. 2014;35:3155–79. doi: 10.1093/eurheartj/ehu298. [DOI] [PubMed] [Google Scholar]
- 19.Kang X, Hu DY, Li CB, et al. N-acetylcysteine for the prevention of contrast-induced nephropathy in patients with pre-existing renal insufficiency or diabetes: a systematic review and metaanalysis. Ren Fail. 2015;37:297–303. doi: 10.3109/0886022X.2015.1012985. [DOI] [PubMed] [Google Scholar]
- 20.Levey AS, Bosch JP, Lewis JB, et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–70. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 21.Mehran R, Rao SV, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123:2736–47. doi: 10.1161/CIRCULATIONAHA.110.009449. [DOI] [PubMed] [Google Scholar]
- 22.McCullough P. Outcomes of contrast-induced nephropathy: experience in patients undergoing cardiovascular intervention. Catheter Cardiovasc Interv. 2006;67:335–43. doi: 10.1002/ccd.20658. [DOI] [PubMed] [Google Scholar]
- 23.Parfrey PS, Griffiths SM, Barrett BJ, et al. Contrast material-induced renal failure in patients with diabetes mellitus, renal insufficiency, or both. A prospective controlled study. N Engl J Med. 1989;320:143–9. doi: 10.1056/NEJM198901193200303. [DOI] [PubMed] [Google Scholar]
- 24.Caldeira D, Gonçalves N, Pinto FJ, et al. Risk of renal failure with the non-vitamin K antagonist oral anticoagulants: systematic review and meta-analysis. Pharmacoepidemiol Drug Saf. 2015;24:757–64. doi: 10.1002/pds.3791. [DOI] [PubMed] [Google Scholar]
- 25.Hori M, Matsumoto M, Tanahashi N, et al. J-ROCKET AF study investigators Rivaroxaban vs. warfarin in Japanese patients with atrial fibrillation – the J-ROCKET AF study. Circ J. 2012;76:2104–11. doi: 10.1253/circj.cj-12-0454. [DOI] [PubMed] [Google Scholar]
- 26.Eriksson BI, Borris LC, Friedman RJ, et al. RECORD1 Study Group Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med. 2008;358:2765–75. doi: 10.1056/NEJMoa0800374. [DOI] [PubMed] [Google Scholar]
- 27.Kakkar AK, Brenner B, Dahl OE, et al. RECORD2 Investigators Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: a double-blind, randomised controlled trial. Lancet. 2008;372:31–9. doi: 10.1016/S0140-6736(08)60880-6. [DOI] [PubMed] [Google Scholar]
- 28.Brodsky SV, Hebert LA. Anticoagulant-related nephropathy: is an aki elephant hiding in plain view? J Am Coll Cardiol. 2016;68:2284–6. doi: 10.1016/j.jacc.2016.09.926. [DOI] [PubMed] [Google Scholar]
- 29.Brodsky SV, Collins M, Park E, et al. Warfarin therapy that results in an international normalization ratio above the therapeutic range is associated with accelerated progression of chronic kidney disease. Nephron Clin Pract. 2010;115:c142–6. doi: 10.1159/000312877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ware K, Brodsky P, Satoskar AA, et al. Warfarin-related nephropathy modeled by nephron reduction and excessive anticoagulation. J Am Soc Nephrol. 2011;22:1856–62. doi: 10.1681/ASN.2010101110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yanagita M. Gas6, warfarin, and kidney diseases. Clin Exp Nephrol. 2004;8:304–9. doi: 10.1007/s10157-004-0305-z. [DOI] [PubMed] [Google Scholar]
- 32.Wheeler DS, Giugliano RP, Rangaswami J. Anticoagulation-related nephropathy. J Thromb Haemost. 2016;14:461–7. doi: 10.1111/jth.13229. [DOI] [PubMed] [Google Scholar]
- 33.Shafi ST, Negrete H, Roy P, et al. A case of dabigatran-associated acute renal failure. WMJ. 2013;112:173–5. [PubMed] [Google Scholar]
- 34.Escoli R, Santos P, Andrade S, Carvalho F. Dabigatran-related nephropathy in a patient with undiagnosed IgA nephropathy. Case Rep Nephrol. 2015;2015:298261. doi: 10.1155/2015/298261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ryan M, Ware K, Qamri Z, et al. Warfarin-related nephropathy is the tip of the iceberg: direct thrombin inhibitor dabigatran induces glomerular hemorrhage with acute kidney injury in rats. Nephrol Dial Transplant. 2014;29:2228–34. doi: 10.1093/ndt/gft380. [DOI] [PubMed] [Google Scholar]