Abstract
Rehabilitation therapy combined with nursing intervention in postoperative recovery of patients with hypertensive intracerebral hemorrhage was investigated. Retrospective analysis was carried out in 78 patients with severe HICH hematoma evacuation after treatment in Xuzhou No. 1 People's Hospital, Xuzhou Municipal Hospital Affiliated to Xuzhou Medical University from March 2014 to July 2017. The 28 patients who received routine treatment and nursing care were regarded as the control group, the 27 patients who underwent rehabilitation training based with routine treatment and nursing care were the rehabilitation training group. Moreover, the 23 patients who underwent rehabilitation training and nursing intervention based on routine treatment were regarded as the nursing intervention group. Systolic blood pressure, diastolic blood pressure, and Fugl-Meyer scores were compared immediately after surgery (T1), 4 weeks after treatment (T2) and 12 weeks after treatment (T3). During the period of T3, the total effective rate and adverse reactions were compared among the three groups of patients. The systolic blood pressure and diastolic blood pressure at T3 among the three groups were significantly lower than both T2 and T1, and the systolic and diastolic blood pressure of T2 was lower than T1 (P<0.05). Among the three groups of patients, the Fugl-Meyer score at T3 was significantly higher than both the T2 and T1, and the Fugl-Meyer score at T2 was higher than T1 (P<0.050). In the control group, the number of patients with shoulder-hand syndrome, hemorrhoids, and depression was significantly higher than both the rehabilitation training group and the nursing intervention group (P<0.050). The number of people with depression in the rehabilitation training group was significantly higher than the nursing intervention group (P<0.050). Rehabilitation therapy and nursing intervention are better than routine treatment and nursing for postoperative recovery of HICH patients, and has a lower adverse reaction rates after surgery, it is worthy of promotion clinically.
Keywords: rehabilitation therapy, nursing intervention, hypertensive cerebral hemorrhage, postoperative recovery
Introduction
Intracerebral hemorrhage (ICH), a non-traumatic and spontaneous brain parenchymal hemorrhage, has the characteristics of rapid onset and progression, with a high morbidity and mortality rates (1,2). Hypertensive intracerebral hemorrhage (HICH), is a critical disease and clinically common in middle-aged and elderly people, it is a type of blood circulation disorder that seriously endangers human health (3,4). The most serious pathological change in HICH is due to mechanical damage caused by bleeding and secondary damage to surrounding tissues, such as cerebral ischemia and edema (5). Lakhan et al (6) suggested that the degree of brain tissue damage caused by cerebral ischemia and edema after cerebral hemorrhage was similar to hematoma itself. However, the patients have a sharp increase of intracranial pressure in a short period of time causing an extremely high mortality rates, so efficient and timely treatment is clinically important (7). The current clinical goal of treating HICH is to remove the hematoma, reduce intracranial pressure, prevent or reduce the occurrence of secondary lesions after hemorrhage, and to apply more surgical treatments. However, due to different factors such as the severity of patients condition, location of hematoma, volume of hematoma and the extent of damage to the brain tissue, patients are prone to complications after surgery. Due to the above issues it has become medically important (8–10).
In recent years, with the improvement of clinical technology, the mortality rate after the surgery of HICH has decreased. However, due to the occurrence of different degrees of dysfunction in most patients after surgery, it seriously affects the prognosis and life quality of patients and impacts on both the patients and their families. Some reports have shown that the postoperative rehabilitation training has an important effect in patients with cerebrovascular disease (11,12). Moreover, according to the report of Li et al (13), active and effective nursing intervention is an important means of adjuvant treatment of HICH. It can reduce the disability rate, and improve the patients' life quality and mental state, which plays an important role in the clinical treatment of HICH. However, there are only a few reports on the rehabilitation and nursing interventions for patients after HICH surgery. Therefore, this study explored the comparison among patients of routine treatment and routine nursing intervention after HICH surgery with patients undergoing rehabilitation therapy and nursing intervention, with an aim to provide reference value for future clinical HICH treatment.
Patients and methods
Patient information
Retrospective analysis was performed of 78 patients with severe HICH hematoma evacuation after treatment in Xuzhou No. 1 People's Hospital, Xuzhou Municipal Hospital Affiliated to Xuzhou Medical University (Xuzhou, China) from March 2014 to July 2017. Among them, 28 patients who received routine treatment and routine nursing were regarded as the control group, including 19 cases of males, 9 cases of females, average age of 68±4.67 years; 27 patients who underwent rehabilitation training based on routine treatment and routine nursing care were regarded as the rehabilitation training group, including 19 cases of males, 8 cases of females, with an average age of 67.54±5.21 years. Twenty-three patients who underwent rehabilitation training based on routine treatment and nursing intervention were regarded as nursing intervention group, including 14 cases of males and 9 cases of females, with an average age of 69.95±5.06 years. Inclusion criteria were: Patients diagnosed with HICH, and who underwent surgery; patients with a bleeding volume between 30–50 ml; complete medical records; not received treatment in other hospitals. Exclusion criteria were: Patients who were unwilling to cooperate with medical treatment; patients who have had hospitalization transfer; patients with other hemorrhage diseases; patients with liver, kidney, coagulopathy or other basic severe diseases; patients with tumors; patients with mental disorders and cognitive impairment.
All subjects and their families signed an informed consent and cooperated with medical staff to complete relevant medical treatment. The study was approved by the Ethics Committee of Xuzhou No. 1 People's Hospital, Xuzhou Municipal Hospital Affiliated to Xuzhou Medical University (Xuzhou, China).
Methods of treatment and nursing care
All the patients in the three groups underwent routine treatments such as nutritional brain cells, diuresis, hemostasis, dehydration, and hypotension; both the control group and rehabilitation group adopted routine nursing care method. On the basis of a stable condition, rehabilitation training was given to patients in both the rehabilitation training group and the nursing intervention group after the cerebral edema gradually subsided. Also targeted treatment was applied based on individual dysfunction of the patient, the main treatments are daily life ability training, bath technology and sports re-learning training. The main details are as follows: i) Good limb position placement and joint passive activity training: assisting the patient to perform appropriate passive exercise during bed rest, take the method of alternate replacement of supine position, healthy lateral position, the way to change lateral position and instruct the patient to turn over on the bed; also focus on how to maintain each joint position and the functional position, and take passive exercise in joint activity. ii) Swallowing and speech function training: assisting the patient in the lateral position, raising the head of the bed 15–30°, use a syringe to inject warm water from the corner of the healthy side into the mouth, exercise the patient's swallowing function; also employ language and hearing training for aphasia patients. iii) Station, walking and balance training: Assist patients in standing and gait training according to the patient's condition. After the patient's muscle strength reached grade 3 or above, the patient's single leg standing balance and normal gait training were performed. Practice the above training 10–20 min/time, 2 times/day.
The nursing intervention group teaches patients relevant knowledge on the basis of rehabilitation training, and patiently answers questions and understands the patient's inner needs. Develop an appropriate psychological guidance according to different patient characteristics, allow patients to express their inner depression and anxiety as much as possible, and provide psychological guidance. Helping patients to exercise dining, dressing and toileting and improve their self-care ability, reduce their dependence on psychology and depression. In addition, set up an activity room in the ward, and improve the entertainment venues such as TV and music for patients, this helps to reduce their depression.
Evaluation methods and criteria
The systolic blood pressure, diastolic blood pressure, and Fugl-Meyer score among the three groups were compared immediately after surgery (T1), 4 weeks after treatment (T2), and 12 weeks after treatment (T3). During the period of T3, the total effective rate and adverse reactions (shoulder-hand syndrome, hemorrhoids, depression) among the three groups of patients were compared.
Evaluation methods of Fugl-Meyer: the scores were taken by the same rehabilitation staff, with a total score of 100. The higher the score, the better the recovery.
Overall efficiency criteria: Significantly effective: The Fugl-Meyer score for patients during the period of T3 increased by 91–100% compared with T1, with a 0 degree of disability. Effective: During the period of T3, Fugl-Meyer score has increased by 46–90% compared with T1, with a 1–3 degree of disability. Progressed: Patients during the period of T3, Fugl-Meyer score has increased by 18–45% compared with T1, with nothing changed in the degree of disability. Non-effective: Patients during the period of T3, Fugl-Meyer score has increased less than 18% compared with T1. Overall efficiency = (significantly effective number + effective number) / total number of people.
Statistical analysis
SPSS 19.1 [Bo Yi Zhixun (Beijing) Information Technology Co. Ltd., Beijing, China] software system was applied for statistical analysis. The enumeration data were expressed as a percentage [n (%)], the difference between the groups was compared by Chi-square test. Difference between multiple groups was compared by ANOVA with LSD post hoc test. The difference between the three groups was compared by F test. Measurement data was expressed as mean ± standard deviation. P<0.05 was considered to indicate a statistically significant difference.
Results
Comparison of clinical data of patients
In order to make the experimental results accurate and credible, the patients' sex, age, weight, condition of psychomotor agitation, pathological changes of small arteries and hemorrhage location were compared among the three groups, the difference was not statistically significant (P>0.05). This indicates that it is comparable among the three groups. Table I shows basic patient clinical data.
Table I.
Basic data of patients in the three groups [n (%)].
| Characteristics | Control group (n=28) | Rehabilitation training group n=27) | Nursing intervention group (n=23) | Chi-square test | P-value |
|---|---|---|---|---|---|
| Sex | 0.532 | 0.766 | |||
| Male | 19 (67.86) | 19 (70.37) | 14 (60.87) | ||
| Female | 9 (32.14) | 8 (29.63) | 9 (39.13) | ||
| Age (years) | 0.191 | 0.909 | |||
| ≤60 | 5 (17.86) | 6 (22.22) | 5 (21.74) | ||
| >60 | 23 (82.14) | 21 (77.78) | 18 (78.26) | ||
| Weight (kg) | 0.655 | 0.721 | |||
| ≤60 | 13 (46.43) | 11 (40.74) | 12 (52.17) | ||
| >60 | 15 (53.57) | 16 (59.26) | 11 (47.83) | ||
| Psychomotor agitation | 1.990 | 0.370 | |||
| Yes | 4 (14.29) | 8 (29.63) | 6 (26.09) | ||
| No | 24 (85.71) | 19 (70.37) | 17 (73.91) | ||
| Pathological changes of small arteries | 1.042 | 0.594 | |||
| Glassy | 22 (78.95) | 18 (66.67) | 16 (69.57) | ||
| Fibrous | 6 (21.05) | 9 (33.33) | 7 (30.43) | ||
| Hemorrhage location | 1.659 | 0.798 | |||
| Basal ganglia | 18 (64.29) | 14 (51.85) | 11 (47.83) | ||
| Thalamus | 6 (21.43) | 7 (25.93) | 7 (30.43) | ||
| Lobar | 4 (14.29) | 6 (22.22) | 5 (21.74) |
Changes of systolic blood pressure at T1-T3 in the three groups of patients
The systolic blood pressure at T1, T2, and T3 in the control group was 173.72±22.61, 164.56±16.57, and 156.25±8.13 mmHg. The systolic blood pressure at T1, T2 and T3 in the rehabilitation training group was 174.61±23.54, 156.35±15.94, and 149.36±7.48 mmHg. The systolic blood pressure at T1, T2, and T3 in the nursing intervention group was 173.27±23.15, 154.16±14.86, and 148.21±7.73 mmHg.
During the period of T1, there was no statistically significant difference in systolic blood pressure among the three groups (P>0.050). At T2 and T3, the systolic blood pressure in both the rehabilitation training group and the nursing intervention group were lower than the control group, and the difference was statistically significant (P<0.050). There was no significant difference in systolic blood pressure between the rehabilitation training group and the nursing intervention group (P>0.050). The systolic blood pressure at T3 in the three groups was significantly lower than T2 and T1, and the systolic blood pressure at T2 was lower than T1. The difference was statistically significant (P<0.050) (Fig. 1).
Figure 1.
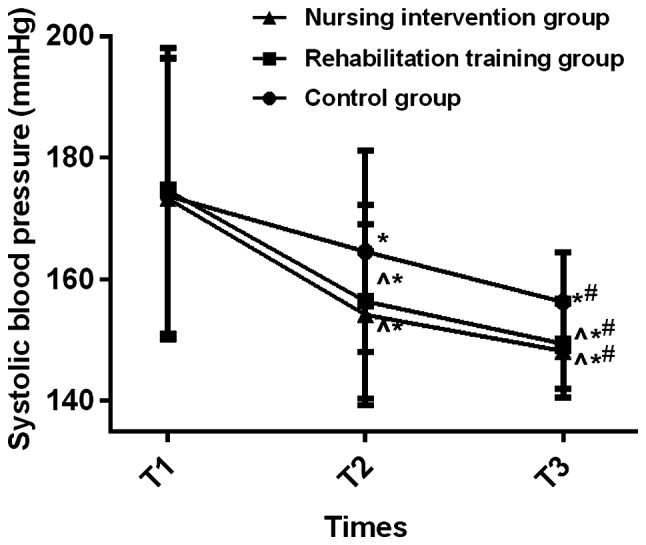
Changes in systolic blood pressure at T1-T3 in the three groups of patients, there was no statistically significant difference in systolic blood pressure in the three groups (P>0.050). During the period of T2 and T3, the systolic blood pressure of in the rehabilitation training group and the nursing intervention group were lower than the control group, the difference was statistically significant (P<0.050). There was no significant difference in systolic blood pressure between the rehabilitation training group and the nursing intervention group (P>0.050). The systolic blood pressure at T3 in the three groups was significantly lower than both T2 and T1, and the systolic blood pressure at T2 was lower than T1, the difference was statistically significant (P<0.050). ^P<0.050, the difference is statistically significant compared with the control group; *P<0.050, the difference is statistically significant compared to T1; #P<0.050, the difference is statistically significant compared to T2.
Changes of diastolic blood pressure at T1-T3 among the three groups of patients
The diastolic blood pressures of T1, T2, and T3 in the control group were 108.36±12.97, 99.24±10.75, and 92.08±8.36 mmHg. The diastolic blood pressure in the rehabilitation training group at T1, T2, and T3 was respectively 107.24±13.02, 94.11±9.28, and 86.35±6.15 mmHg. The diastolic blood pressure at T1, T2, and T3 in the nursing intervention group was 107.82±12.63, 92.86±8.84, and 85.21±7.73 mmHg.
During the period of T1, there was no statistically significant difference in diastolic blood pressure among the three groups (P>0.050). During the period of T2 and T3, the diastolic blood pressure in the rehabilitation training group and the nursing intervention group were lower than the control group and the difference was statistically significant (P<0.050). There was no significant difference in diastolic blood pressure between the rehabilitation training group and the nursing intervention group (P>0.050). The diastolic blood pressure at T3 in the three groups was significantly lower than both T2 and T1. The diastolic blood pressure at T2 was lower than T1, and the difference was statistically significant (P<0.050) (Fig. 2).
Figure 2.
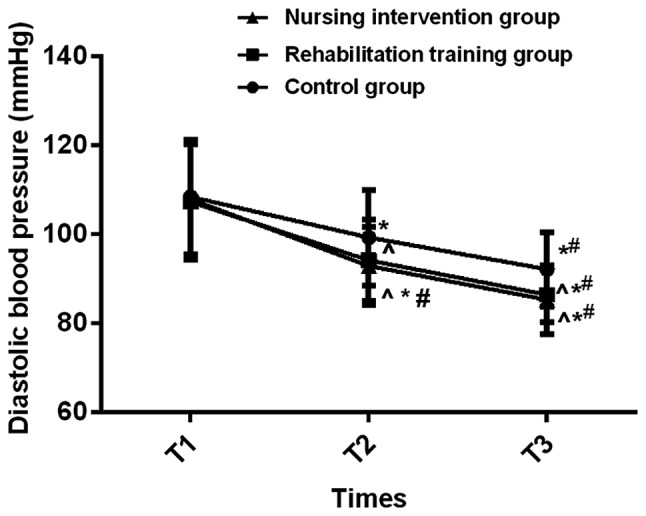
Changes in diastolic blood pressure at T1-T3 in the three groups of patients, there was no statistically significant difference in diastolic blood pressure in the three groups (P>0.050). During the period of T2 and T3, the diastolic blood pressure in the rehabilitation training group and the nursing intervention group were lower than the control group, and the difference was statistically significant (P<0.050). There was no significant difference in diastolic blood pressure between the rehabilitation training group and the nursing intervention group (P>0.050). The diastolic blood pressure at T3 among the three groups was significantly lower than both T2 and T1. The diastolic blood pressure at T2 was lower than T1, and the difference was statistically significant (P<0.050). ^P<0.050, the difference is statistically significant compared with the control group; *P<0.050, the difference is statistically significant compared to T1; #P<0.050, the difference is statistically significant compared to T2.
Fugl-Meyer scores at T1-T3 time points in the three groups of patients
During the period of T1, there was no significant difference in Fugl-Meyer score in the three groups (P>0.050). During the period of T2 and T3, the Fugl-Meyer scores in the rehabilitation training group and the nursing intervention group were higher than the control group, the difference was statistically significant (P<0.050). There was no significant difference in Fugl-Meyer score between the rehabilitation training group and the nursing intervention group (P>0.050). The Fugl-Meyer score at T3 in the three groups was significantly higher than both T2 and T1, and the Fugl-Meyer score at T2 was higher than T1. The difference was statistically significant (P<0.050) (Table II).
Table II.
Comparison of Fugl-Meyer scores at T1-T3 in the three groups of patients.
| Item | Control group (n=28) | Rehabilitation training group (n=27) | Nursing intervention group (n=23) | F value | P-value |
|---|---|---|---|---|---|
| T1 | 26.83±5.79 | 27.19±5.54 | 27.02±6.11 | 0.027 | 0.974 |
| T2 | 34.17±8.61a | 41.59±9.03a,b | 43.07±8.67a,b | 7.825 | 0.001 |
| T3 | 43.51±8.84a,c | 58.37±10.15a–c | 60.08±10.45a–c | 23.100 | <0.001 |
| F value | 31.600 | 95.030 | 103.600 | ||
| P-value | <0.001 | <0.001 | <0.001 |
P<0.050, the difference is statistically significant compared with the control group
P<0.050, the difference is statistically significant compared to T1
P<0.050, the difference is statistically significant compared to T2.
Comparison of overall efficiency at T3 among the three groups of patients
The number of significantly-effective, effective, progressed and non-effective patients in the control group were 13, 8, 5, and 2, respectively. The number of significantly-effective, effective, progressed and non-effective patients in the rehabilitation training group was 16, 10, 1 and 0, respectively; The number of significantly effective, effective, progressed, and non-effective patients in the nursing intervention group was 15, 7, 1 and 0, respectively.
The total effective rate in the control group was 75.00%, the total effective rate in the rehabilitation training group was 96.30% and the total effective rate in the nursing intervention group was 95.65%. The total effective rate in the rehabilitation training group and the nursing intervention group was significantly higher than the control group, and the difference was statistically significant (P<0.050). There was no significant difference in total effective rate between the rehabilitation training group and the nursing intervention group (P>0.050) (Table III).
Table III.
Comparison of total effective rate at T3 in the three groups of patients.
| Item | Significantly effective | Effective | Progressed | Non-effective | Total effective rate |
|---|---|---|---|---|---|
| Control group (n=28) | 13 (46.43) | 8 (28.57) | 5 (17.86) | 2 (7.14) | 21 (75.00) |
| Rehabilitation group (n=27) | 16 (59.26) | 10 (37.03) | 1 (3.70) | 0 (0.00) | 26 (96.30) |
| Nursing intervention group (n=23) | 15 (65.22) | 7 (30.43) | 1 (4.35) | 0 (0.00) | 22 (95.65) |
| Chi-square test | – | – | – | – | 7.379 |
| P-value | – | – | – | – | 0.025 |
Comparison of adverse reactions at T3 in the three groups of patients
In the control group, the number of patients with shoulder-hand syndrome, hemorrhoids, and depression was significantly higher than both the rehabilitation training group and the nursing intervention group, the difference was statistically significant (P<0.050). There was no significant difference in the number of patients with shoulder-hand syndrome and hemorrhoids in the rehabilitation training group or nursing intervention group (P>0.050). The number of people with depression in the rehabilitation training group was significantly higher than the nursing intervention group, and the difference was statistically significant (P<0.050) (Table IV).
Table IV.
Comparison of adverse reactions in the three groups of patients n (%)].
| Groups | Control group (n=28) | Rehabilitation training group (n=27) | Nursing intervention group (n=23) | Chi-square test | P-value |
|---|---|---|---|---|---|
| Shoulder-hand syndrome | 21 (75.00) | 3 (11.11)a | 4 (17.39)a | 29.240 | <0.001 |
| Decubitus | 13 (46.43) | 5 (18.52)a | 4 (17.39)a | 7.171 | 0.028 |
| Depression | 23 (82.14) | 14 (51.85)a | 5 (21.74)a,b | 18.600 | <0.001 |
P<0.050, the difference is statistically significant compared with the control group
P<0.050, the difference was statistically significant compared with the rehabilitation training group.
Discussion
According to statistics, in industrialized countries, cerebrovascular disease is the leading cause of death among women. Also the second leading cause of death in men, cerebrovascular disease is also an important cause of cognitive impairment and dementia (14,15). HICH is a parenchymal hemorrhage caused by rupture of small arteries when blood pressure rises suddenly. The incidence of HICH has increased significantly in recent years. It has a high disability and mortality rate, the mortality rate is approximately 35–52% (16). HICH is the main cause of functional disability, most patients with cerebral hemorrhage have neurological sequelae after treatment, and cannot restore the same level of daily living activities as before the disease (17,18). The number of patients with HICH worldwide is gradually declining due to early control of risk factors. However, many patients still require a long-term care after surgery, this has caused a great burden on the patient's family and society, therefore, early intervention is crucial (19,20). This study analyzed 78 patients with severe HICH hematoma evacuation after treatment in Xuzhou No. 1 People's Hospital. The efficacy and adverse reactions of different postoperative intervention methods were compared to provide reference for clinical diagnosis and treatment of HICH patients.
In this study, we found that the systolic blood pressure, diastolic blood pressure, Fugl-Meyer score, total effective rate and the number of patients with shoulder-hand syndrome and decubitus were not statistically significant in either the rehabilitation training group or the nursing intervention group. This indicates that there was no significant difference in the effect of postoperative intervention between the groups. However, the number of people with depression in the rehabilitation training group was significantly higher than the nursing intervention group. Lack of social support, disability and chronic diseases are the poor prognostic factors for depression, and has increased the mortality rate in patients (21). Scientific and effective care with positive and accurate clinical treatment are the key to improving the prognosis condition and cure rate. Traditional and conventional nursing models cannot fully adapt to patients in different situations because of their backward concepts and ways of thinking. This has caused less than ideal prognosis for patients, especially in the emotional direction of patients (22). Therefore, we need to be more focused on the emotional side of HICH patients. Some documentaries have shown that it is important to let cardiovascular patients know the relevant knowledge, further supporting our point view (23).
In this study, we also found that patients in the rehabilitation training group and the nursing intervention group had undergone rehabilitation training, so the systolic blood pressure, diastolic blood pressure, and the number of patients with shoulder-hand syndrome and decubitus were significantly lower than the control group. However, the Fugl-Meyer score and the overall effective rate were significantly higher than the control group. This indicates that each index of the patients who underwent rehabilitation training after HICH is better than those who did not undergo rehabilitation training. Some documents have shown that for patients with ischemic or cerebral vascular hemorrhage, should take therapeutic exercise, task-oriented training, gait training, balance training, restrictive exercise therapy, shoulder treatment and other rehabilitation training (24). According to a study by Bai et al (25) on patients with hemorrhagic stroke, it was found that the improvement of Fugl-Myere score in the rehabilitation group was significantly higher than the control group, and this further support our research results. However, according to Stern et al (26) in patients with non-traumatic subarachnoid hemorrhage, they found that rehabilitation physicians have developed the most appropriate rehabilitation program for these patients with the latest developments and potential complications, this can reduce the mortality rate in patients. However, there is currently only a few documents on the rehabilitation therapy in HICH patients. Therefore, this has made our study more innovative and valuable.
There are still some shortcomings in our investigation due to limited experimental conditions, such as small sample size; so statistical analysis of large data could not be performed. Also our research subjects were quite uniform, so there may be differences in the performance among different ethnicities.
Overall, rehabilitation therapy and nursing intervention are better than routine treatment and nursing for postoperative recovery of HICH patients, also there are less adverse reactions post-operatively, thus it is worthy of promotion clinically.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Authors' contributions
XL and PZ were responsible for methods of treatment and nursing care. CG and JX collected and analyzed general data of patients. MH wrote the initial draft manuscript and helped with statistical analysis. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Xuzhou No. 1 People's Hospital, Xuzhou Municipal Hospital Affiliated to Xuzhou Medical University (Xuzhou, China). Patients who participated in this research had complete clinical data. Signed informed consents were obtained from the patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Hemphill JC, III, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, Fung GL, Goldstein JN, Macdonald RL, Mitchell PH, et al. American Heart Association Stroke Council; Council on Cardiovascular and Stroke Nursing and Council on Clinical Cardiology Guidelines for the management of spontaneous intracerebral hemorrhage: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:2032–2060. doi: 10.1161/STR.0000000000000069. [DOI] [PubMed] [Google Scholar]
- 2.Wang J, Wang G, Yi J, Xu Y, Duan S, Li T, Sun XG, Dong L. The effect of monascin on hematoma clearance and edema after intracerebral hemorrhage in rats. Brain Res Bull. 2017;134:24–29. doi: 10.1016/j.brainresbull.2017.06.018. [DOI] [PubMed] [Google Scholar]
- 3.Qureshi AI, Qureshi MH. Acute hypertensive response in patients with intracerebral hemorrhage pathophysiology and treatment. J Cereb Blood Flow Metab. 2018;38:1551–1563. doi: 10.1177/0271678X17725431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hong D, Stradling D, Dastur CK, Akbari Y, Groysman L, Al-Khoury L, Chen J, Small SL, Yu W. Resistant hypertension after hypertensive intracerebral hemorrhage is associated with more medical interventions and longer hospital stays without affecting outcome. Front Neurol. 2017;8:184. doi: 10.3389/fneur.2017.00184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang XQ, Zhang ZM, Yin XL, Zhang K, Cai H, Ling F. Exploring the optimal operation time for patients with hypertensive intracerebral hemorrhage: Tracking the expression and progress of cell apoptosis of prehematomal brain tissues. Chin Med J (Engl) 2010;123:1246–1250. [PubMed] [Google Scholar]
- 6.Lakhan SE, Kirchgessner A, Tepper D, Leonard A. Matrix metalloproteinases and blood-brain barrier disruption in acute ischemic stroke. Front Neurol. 2013;4:32. doi: 10.3389/fneur.2013.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ropper AE, Chi JH. Treatment of traumatic brain injury without direct intracranial pressure monitoring. Neurosurgery. 2013;72:N19–N20. doi: 10.1227/01.neu.0000428424.83867.87. [DOI] [PubMed] [Google Scholar]
- 8.Gavito-Higuera J, Khatri R, Qureshi IA, Maud A, Rodriguez GJ. Aggressive blood pressure treatment of hypertensive intracerebral hemorrhage may lead to global cerebral hypoperfusion: Case report and imaging perspective. World J Radiol. 2017;9:448–453. doi: 10.4329/wjr.v9.i12.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manno EM, Atkinson JL, Fulgham JR, Wijdicks EF. Emerging medical and surgical management strategies in the evaluation and treatment of intracerebral hemorrhage. Mayo Clin Proc. 2005;80:420–433. doi: 10.4065/80.3.420. [DOI] [PubMed] [Google Scholar]
- 10.Inamasu J, Nakae S, Adachi K, Hirose Y. Angiotensin II receptor blockers following intravenous nicardipine administration to lower blood pressure in patients with hypertensive intracerebral hemorrhage: A prospective randomized study. Blood Press Monit. 2017;22:34–39. doi: 10.1097/MBP.0000000000000225. [DOI] [PubMed] [Google Scholar]
- 11.Knecht S, Roßmüller J, Unrath M, Stephan KM, Berger K, Studer B. Old benefit as much as young patients with stroke from high-intensity neurorehabilitation: Cohort analysis. J Neurol Neurosurg Psychiatry. 2016;87:526–530. doi: 10.1136/jnnp-2015-310344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shimamura N, Katagai T, Kakuta K, Matsuda N, Katayama K, Fujiwara N, Watanabe Y, Naraoka M, Ohkuma H. Rehabilitation and the Neural Network After Stroke. Transl Stroke Res. 2017;8:507–514. doi: 10.1007/s12975-017-0550-6. [DOI] [PubMed] [Google Scholar]
- 13.Li W, Gao J, Wei S, Wang D. Application values of clinical nursing pathway in patients with acute cerebral hemorrhage. Exp Ther Med. 2016;11:490–494. doi: 10.3892/etm.2015.2909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Phipps MS, Jastreboff AM, Furie K, Kernan WN. The diagnosis and management of cerebrovascular disease in diabetes. Curr Diab Rep. 2012;12:314–323. doi: 10.1007/s11892-012-0271-x. [DOI] [PubMed] [Google Scholar]
- 15.Kalaria RN. Cerebrovascular disease and mechanisms of cognitive impairment: Evidence from clinicopathological studies in humans. Stroke. 2012;43:2526–2534. doi: 10.1161/STROKEAHA.112.655803. [DOI] [PubMed] [Google Scholar]
- 16.Soustiel JF, Sviri GE, Mahamid E, Shik V, Abeshaus S, Zaaroor M. Cerebral blood flow and metabolism following decompressive craniectomy for control of increased intracranial pressure. Neurosurgery. 2010;67:65–72. doi: 10.1227/01.NEU.0000370604.30037.F5. [DOI] [PubMed] [Google Scholar]
- 17.Xu X, Chen X, Li F, Zheng X, Wang Q, Sun G, Zhang J, Xu B. Effectiveness of endoscopic surgery for supratentorial hypertensive intracerebral hemorrhage: A comparison with craniotomy. J Neurosurg. 2018;128:553–559. doi: 10.3171/2016.10.JNS161589. [DOI] [PubMed] [Google Scholar]
- 18.Biffi A, Anderson CD, Battey TW, Ayres AM, Greenberg SM, Viswanathan A, Rosand J. Association between blood pressure control and risk of recurrent intracerebral hemorrhage. JAMA. 2015;314:904–912. doi: 10.1001/jama.2015.10082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yu SX, Zhang QS, Yin Y, Liu Z, Wu JM, Yang MX. Continuous monitoring of intracranial pressure for prediction of postoperative complications of hypertensive intracerebral hemorrhage. Eur Rev Med Pharmacol Sci. 2016;20:4750–4755. [PubMed] [Google Scholar]
- 20.Li F, Chen QX. Risk factors for mental disorders in patients with hypertensive intracerebral hemorrhage following neurosurgical treatment. J Neurol Sci. 2014;341:128–132. doi: 10.1016/j.jns.2014.04.021. [DOI] [PubMed] [Google Scholar]
- 21.Lee LC, Tsai AC. Mini-nutritional assessment predicts functional decline of elderly Taiwanese: Result of a population-representative sample. Br J Nutr. 2012;107:1707–1713. doi: 10.1017/S0007114511004880. [DOI] [PubMed] [Google Scholar]
- 22.Waguchi H, Hidaka K, Shinoki K, Matsuoka M, Mito S, Doi S, Hata A, Ibata T, Komuro R, Iijima S. Coordination to assist with hospital-to-home discharge after cerebral hemorrhage - perspectives of a patient's family and nurse. Gan To Kagaku Ryoho. 2013;40(Suppl 2):216–218. (In Japanese) [PubMed] [Google Scholar]
- 23.Raitakari OT, Juonala M, Kähönen M, Taittonen L, Laitinen T, Mäki-Torkko N, Järvisalo MJ, Uhari M, Jokinen E, Rönnemaa T, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: The Cardiovascular Risk in Young Finns Study. JAMA. 2003;290:2277–2283. doi: 10.1001/jama.290.17.2277. [DOI] [PubMed] [Google Scholar]
- 24.Cavallo S, Brosseau L, Toupin-April K, Wells GA, Smith CA, Pugh AG, Stinson J, Thomas R, Ahmed S, Duffy CM, et al. Ottawa panel evidence-based clinical practice guidelines for structured physical activity in the management of juvenile idiopathic arthritis. Arch Phys Med Rehabil. 2017;98:1018–1041. doi: 10.1016/j.apmr.2016.09.135. [DOI] [PubMed] [Google Scholar]
- 25.Bai Y, Hu Y, Wu Y, Zhu Y, He Q, Jiang C, Sun L, Fan W. A prospective, randomized, single-blinded trial on the effect of early rehabilitation on daily activities and motor function of patients with hemorrhagic stroke. J Clin Neurosci. 2012;19:1376–1379. doi: 10.1016/j.jocn.2011.10.021. [DOI] [PubMed] [Google Scholar]
- 26.Stern M, Chang D, Odell M, Sperber K. Rehabilitation implications of non-traumatic subarachnoid haemorrhage. Brain Inj. 2006;20:679–685. doi: 10.1080/02699050600744269. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.


