Abstract
Blue nevus is a congenital and acquired melanocytic proliferation that includes different histological types. The atypical cellular type has been rarely described and it classically has a benign course. However, because of its intermediate features between common blue nevus and malignant blue nevus, long-term clinical follow-up is required. Here we report the case of a 28-year-old woman who presented with an atypical cellular blue nevus on the right foot.
Keywords: Blue nevus, Atypical nevus
Case Presentation
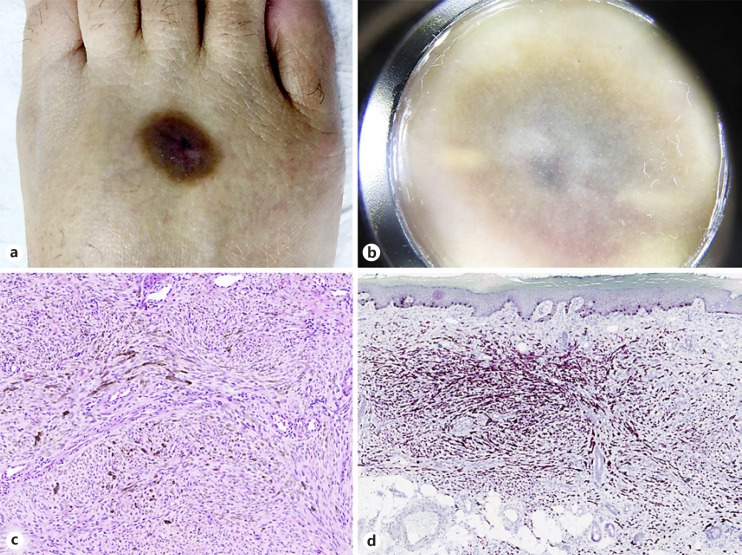
We report the case of a 28-year-old woman, with no medical history, who presented with a black skin lesion on the dorsum of the right foot which had appeared in 2009 after an insect bite during her holidays in Brazil. Since then, the lesion had slightly increased in size. Clinical examination revealed a brownish macule with a bluish center that was slightly infiltrated (Fig. 1a). Dermoscopy showed a blue-steel pigmentation in one part and a violaceous color in the other, with hypopigmented areas (Fig. 1b).
Fig. 1.
a Brownish macule with a bluish center on the dorsum of the right foot. b Dermoscopy showing a blue-steel pigmentation in one part and a violaceous color in the other, with hypopigmented areas. c Histology showing dermal proliferation of spindle cells organized in fascicles with a storiform pattern or in nests. H&E. Original magnification, ×10. d Melan-A was diffusely positive. Immunohistochemistry. Original magnification, ×5.
A biopsy of the lesion showed dermal proliferation of spindle cells organized in fascicles with a storiform pattern or in nests. Smaller epithelioid cells with nuclei similar to the spindle cells were also present. The lesion infiltrated the subcutaneous fat along with the septa (thickness: 1.9 mm). There were no mitoses. S100, SOX10, melan-A, and MITF were diffusely positive. Based on the morphological aspect (Fig. 1a–c) and immunohistochemical profile (Fig. 1d), the diagnosis of atypical blue nevus (BN) with hypercellularity was made. The lesion was surgically removed and exhibited an atypical cellular BN (ACBN).
Discussion and Conclusion
BN is a congenital and acquired melanocytic proliferation that includes different histological types: common, cellular, atypical cellular, desmoplastic cellular, combined, compound, and malignant [1, 2, 3]. First described by Tièche in 1906 [2, 3], this melanocytic lesion usually appears in childhood and rarely before birth [1, 3].
Few cases of ACBN have been described [4, 5]. The scalp, trunk, buttocks, and extremities are the main localizations reported, and it seems to be more common among women than among men [4]. It is a rare variant of cellular BN, with clinical features resembling classic BN and histological features similar to malignant BN [4]. Compared to common BN, ACBN often shows asymmetry on histology, an infiltrating border, and extension into subcutaneous tissue [6]. The lesion exhibits sheet-like growth. However, there is usually a pattern of nesting in the tumoral area that may be highlighted with the use of a reticulin stain. Furthermore, it has a higher proliferative index and higher mitotic rate [1, 6]. Because of the presence of atypical spindle cells with periadnexal or perineural infiltration and peri- or intratumoral lymphocytic infiltrates, ACBN can be misdiagnosed as malignant melanoma. The absence of a junctional malignant melanocytic component with an intraepidermal pagetoid spread or atypical mitoses helps in diagnosis [4].
A report on 9 cases published by Tran et al. [4] showed that ACBN classically have a benign clinical course, acting as common BN, but because of the intermediate features between common BN and malignant BN and their indeterminate nature, complete excision with a 1-cm margin and long-term follow-up are recommended [1, 4].
In conclusion, ACBN is a rare lesion that can be difficult to diagnose. Because of its intermediate features, long-term clinical follow-up is required.
Statement of Ethics
The case report was prepared in compliance with all ethical and confidentiality guidelines and principles.
Disclosure Statement
The authors declare no conflict of interest.
References
- 1.Daltro LR, Yaegashi LB, Freitas RA, Fantini BC, Souza CD. Atypical cellular blue nevus or malignant blue nevus? An Bras Dermatol. 2017 Jan-Feb;92((1)):110–2. doi: 10.1590/abd1806-4841.20174502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muñoz C, Quintero A, Sánchez JL, Ruiz-Santiago H. Persistent blue nevus simulating melanoma. J Am Acad Dermatol. 2004 May;50((5 Suppl)):S118–20. doi: 10.1016/j.jaad.2003.09.022. [DOI] [PubMed] [Google Scholar]
- 3.Matz H, Orion E, Ruocco V, Wolf R. Clinical simulators of melanoma. Clin Dermatol. 2002 May-Jun;20((3)):212–21. doi: 10.1016/s0738-081x(02)00232-8. [DOI] [PubMed] [Google Scholar]
- 4.Tran TA, Carlson JA, Basaca PC, Mihm MC. Cellular blue nevus with atypia (atypical cellular blue nevus): a clinicopathologic study of nine cases. J Cutan Pathol. 1998 May;25((5)):252–8. doi: 10.1111/j.1600-0560.1998.tb01729.x. [DOI] [PubMed] [Google Scholar]
- 5.Özdemir ED, Yalçınkaya C, Çoban G, Canpolat T, Okçu Heper A, Çelik H. A rare lesion of the clitoris: atypical cellular blue naevus: case report. J Obstet Gynaecol. 2017 Jan;37((1)):121–2. doi: 10.1080/01443615.2016.1225021. [DOI] [PubMed] [Google Scholar]
- 6.Shumway BS, Rawal YB, Allen CM, Kalmar JR, Magro CM. Oral atypical cellular blue nevus: an infiltrative melanocytic proliferation. Head Neck Pathol. 2013 Jun;7((2)):171–7. doi: 10.1007/s12105-012-0386-z. [DOI] [PMC free article] [PubMed] [Google Scholar]