Abstract
Background
In the first 5 years after their stroke, about a quarter of patients will suffer from a recurrent stroke. Digital health interventions facilitating interactions between a caregiver and a patient from a distance are a promising approach to improve patient adherence to lifestyle changes proposed by secondary prevention guidelines. Many of these interventions are not implemented in daily practice, even though efficacy has been shown. One of the reasons can be the lack of clear economic incentives for implementation. We propose to map all health economic evidence regarding digital health interventions for secondary stroke prevention.
Summary
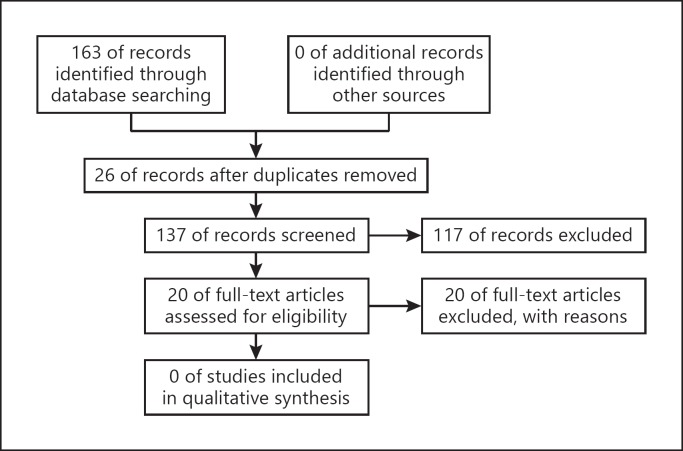
We performed a systematic search according to PRISMA-P guidelines and searched on PubMed, Web of Science, Cochrane, and National Institute for Health Research Economic Evaluation Database. Only digital health interventions for secondary prevention in stroke patients were included and all study designs and health economic outcomes were accepted. We combined the terms “Stroke OR Cardiovascular,” “Secondary prevention,” “Digital health interventions,” and “Cost” in one search string using the AND operator. The search performed on April 20, 2017 yielded 163 records of which 26 duplicates were removed. After abstract screening, 20 articles were retained for full-text analysis, of which none reported any health economic evidence that could be included for analysis or discussion.
Key Messages
There is a lack of evidence on health economic outcomes on digital health interventions for secondary stroke prevention. Future research in this area should take health economics into consideration when designing a trial and there is a clear need for health economic evidence and models.
Keywords: Telemedicine, Digital health interventions, Secondary prevention, Stroke, Health economics of stroke
Introduction
Stroke is the third cause of death worldwide and the second cause of disability-adjusted life years in high-income countries [1]. This condition poses a growing global health problem with major individual and societal impact [2]. In the first 5 years after their stroke, about a quarter of patients will suffer from a recurrent stroke [3] and about a fifth of patients will have a myocardial infarction or vascular death [4]. Internationally accepted guidelines provide evidence-based treatment targets to optimize secondary prevention after stroke [5]. These guidelines describe interventions like for example blood pressure control or dietary advice, but do not provide any guidance on how these interventions should be managed and implemented. Patients' adherence to key lifestyle modifications and compliance with pharmacological therapy is poor in current routine practice, with reported compliance rates of about 50% [6]. Digital health interventions (DHIs) that allow for remote interactions between a patient and a caregiver, like web-based interventions or the remote transmission of vital parameters, but mainly comprised of telephone interventions, have shown a mean difference of 6.14 blood pressure-lowering effects in stroke survivors [7]. In the broader field of cardiovascular diseases, DHIs have significantly reduced cardiovascular disease outcomes (relative risk, 0.61) and improved 10-year risk percentages [8]. Even though potential benefits have been shown, implementation of these new solutions in clinical practice has been limited. Most reviews to date have focused on clinical efficacy [7, 8] and lack a thorough search strategy for health economic information. Mapping the costs and cost-effectiveness of DHIs has been identified as a crucial aspect of the evaluation and rollout of DHIs [9]. We searched studies including a health economic analysis of DHIs for secondary prevention in stroke patients.
Methods
We performed and report on a systematic review according to the PRISMA guidelines [10]. A review protocol was drafted prior to the review and is available upon request.
Criteria for Considering Studies for Review
Types of Studies
In order to find all available evidence, all study types were accepted.
Types of Participants
We selected only studies that report on stroke patients, aged 18 years or older. All stroke types were accepted including but not limited to: ischemic strokes, hemorrhagic strokes, and transient ischemic attacks.
Types of Interventions
Studies that included DHIs [8], focused on secondary stroke prevention, were selected for this review. In this study, DHIs were defined as all interventions where digital communication between a patient and a caregiver is leveraged to support patient adherence to lifestyle guidelines to prevent stroke recurrence [5]. Adherence support to at least one lifestyle change or medication advice mentioned in the guidelines was enough for inclusion: (1) blood pressure reduction, (2) cholesterol lowering with a statin, (3) routine use of an antiplatelet agent unless anticoagulants are more appropriate, (4) smoking cessation, (5) reduction of alcohol consumption to 2 drinks per day for men and 1 drink per day for nonpregnant women, (6) for patients who are capable of engaging in physical activities: 3–4 sessions of aerobic exercise per week during 40 min at moderate to vigorous intensity, (7) dietary advice on low intake of saturated fat and salt but plenty of fish, poultry, olive oil, nuts, whole grains, fruit and vegetables, (8) weight reduction in obese individuals, (9) adequate glycemic control in patients with diabetes, and (10) compliance to prescribed medication. Holter monitoring and other long-term monitoring solely for the purpose of further diagnosis were excluded from this review.
Types of Outcome Measures
In order to find all available evidence, all health economic outcome measures were accepted and extracted for analysis and discussion. This includes – but is not limited to – cost-benefit analysis (monetary terms), cost-utility analysis (quality adjusted life years) and cost-effectiveness analysis (life years saved, or improvement in functional status).
Search Methods and Databases
We performed searches on PubMed, Web of Science, Cochrane, and the National Institute for Health Research Economic Evaluation Database (NHS EED). Only English language papers were included in the search. Studies published before 1990 were not included in the search, because we focused on modern applications that can be used in current clinical practice. Only papers published in peer-reviewed journals were considered. Papers could be published on-line ahead of print.
Search Strategy
We combined the terms “Stroke OR Cardiovascular,” “Secondary prevention,” “Digital health interventions,” and “Costs” in one search string using the AND operator. We used both Mesh terms (PubMed) and free words to maximize output. The search strings were adapted accordingly for each database and are available in supplementary files 1 and 2 (for all online suppl. material, see www.karger.com/doi/10.1159/000496107).
Searching Other Resources
The reference list of all relevant papers and reviews found was screened for additional papers.
Data Collection and Analysis
A first screening was performed by 3 independent screening reviewers based on title and abstract of all articles found by the database searches (after removal of duplicates). One reviewer (A.V.E.) screened all articles and each of the other 2 reviewers screened half the articles (S.S. and K.P.). In case of conflicting decisions, the cases were resolved in a discussion between all 3 reviewers. The remaining articles were screened based on the full texts following the same methodology.
Rayyan [11] was used for gathering all papers found by the searches, removing duplicates and for performing blinded assessment.
Because only health economic outcome parameters were considered, a lot of heterogeneity in the reported results were expected. A meta-analysis on the extracted evidence would be suboptimal and therefore all data was presented, analyzed and discussed descriptively.
Results
The search performed on April 20, 2017 yielded 163 records of which 26 duplicates were removed (Fig. 1). After abstract screening, 20 articles were retained for full-text analysis (Table 1). Eight articles were excluded mainly, but not exclusively, because they did not report on health economic outcome parameters [12, 13, 14, 15, 16, 17, 18, 19]. Three articles were excluded because the intervention was not a DHI aimed at secondary stroke prevention [20, 21, 22], 7 articles were excluded because they were reviews after thorough screening of the reference list [15, 23, 24, 25, 26, 27, 28], 1 article because it was a study protocol [29], and another article because the stroke patients were not the target population [30]. Zero papers were withheld for inclusion in this review.
Fig. 1.
Flow diagram of the search results.
Table 1.
Articles retained for full-text analysis
| Authors | Described intervention | Reason for exclusion |
|---|---|---|
| Banner et al. [19] | Virtual rehabilitation program | Reported outcomes: no health economic data |
| Bashshur et al. [23] | Telemedicine interventions for chronic disease management | Review: no additional papers withheld after screening |
| Clark et al. [25] | Alternative methods for cardiac rehabilitation | Review: no additional papers withheld after screening |
| Corazza et al. [16] | Telemedicine platform for rehabilitation | Reported outcomes: no health economic data |
| Pfaeffli Dale et al. [18] | Text message and internet support for disease self-management | Reported outcomes: no health economic data |
| Devi et al. [15] | Internet-based interventions | Review: no additional papers withheld after screening |
| Dregan et al. [17] | Secondary prevention using electronic health records | Reported outcomes: no health economic data |
| Franklin et al. [24] | Personal health technology | Review: no additional papers withheld after screening |
| Lazzaro et al. [13] | Detection of atrial fibrillation with telemetric Holter monitoring | Reported outcomes: no health economic data |
| Mayer et al. [20] | 7-day Holter monitoring | Intervention: not a DHI aimed at secondary stroke prevention |
| Mittag et al. [12] | Phone-based follow-up intervention for cardiac rehabilitation | Reported outcomes: no health economic data |
| Neubeck et al. [27] | Telehealth interventions for secondary prevention | Review: no additional papers withheld after screening |
| Perera et al. [26] | Strategies for monitoring lipid levels | Review: no additional papers withheld after screening |
| Pietrzak et al. [28] | Internet-based interventions | Review: no additional papers withheld after screening |
| Reena et al. [31] | Web-based program | Reported outcomes: no health economic data |
| Schweier et al. [14] | Web-based peer-modeling intervention | Reported outcomes: no health economic data |
| Southard et al. [30] | Internet-based case management system | Target population: no stroke patients |
| Vegter et al. [21] | Community pharmacy intervention program | Intervention: not a DHI aimed at secondary stroke prevention |
| Yan et al. [29] | Caregiver-delivered nurse-organized service programs | Study protocol |
| Yong et al. [22] | Ambulatory cardiac rhythm monitoring | Intervention: not a DHI aimed at secondary stroke prevention |
Discussion
We report the first health economic systematic review for DHIs aimed at secondary stroke prevention. Despite the growing field of secondary (stroke) prevention, no studies exist on the health economic aspects of DHIs in contemporary literature. Consequently, no studies met the inclusion criteria for our review.
Although we set broad inclusion criteria – all study designs and all possible health economic outcome parameters were eligible – we still might have missed some studies. We only looked for English literature and did not include articles published before 1990. But given the absence of any evidence found by our systematic search, it seems reasonable to assume that any other studies found would be too limited to be able to draw any conclusions on the cost-effectiveness of DHIs for secondary stroke prevention.
We found some evidence on the cost-effectiveness of monitoring solutions for the detection of atrial fibrillation [20, 22, 32]. Since they do not specifically target secondary stroke prevention, they were excluded from this review. Future designs for or models of DHIs for secondary stroke prevention could be taken into account or integrated with solutions for the detection of atrial fibrillation.
Because secondary prevention in stroke patients also entails secondary cardiovascular prevention, we included “cardiovascular” in our search term, in order to limit the chances of missing relevant studies. One paper withheld for full-text analysis provided some insights on health economic aspects of secondary cardiovascular prevention in general. The trial reports a return on investment of 2.13 for an internet-based case management system for secondary cardiovascular prevention [30]. However, the calculations were very basic and only took acute costs into account during the trial period. Yet, this may indicate that more health economic evidence might be available in the broader field of cardiovascular secondary prevention. Overlap exists between cardiovascular and secondary stroke prevention targets [5, 33, 34], but results may not be extrapolated from one domain to another.
A Cochrane review from 2013 on nonpharmacological interventions for secondary stroke prevention identified 5 ongoing studies [35], showing increasing interest in the field. When designing future trials on DHIs for secondary prevention in stroke patients it will be important to take health economic aspects into account. Most secondary prevention efficacy trials use surrogate endpoints such as adherence to one or more key parameters, like increased physical activity [36, 37]. Ideally trials would also use stronger endpoints, for instance prevalence of (re-)hospitalizations or cardiovascular events (including stroke). These clinical endpoints are more adequate for translation into health economic endpoints (e.g., quality-adjusted life years gained or lost). Obviously, there is also a lack of insights into the costs of organization of these interventions and potential associated savings compared to standard care. Therefore, we advise more transparent reporting on implementation and real-life costs and to collect data on resource use by patients. An important aspect, which can greatly influence the cost-effectiveness of DHIs are the usage and dropout rates. It has been shown that older patients have more trouble to adhere to digital health solutions for support of lifestyle changes [38] and given the advanced average age of stroke patients this might have a negative impact on the cost-effectiveness of DHIs for stroke patients. On the other hand, some evidence suggests that elderly people are well suited to be supported by DHIs for lifestyle changes [39]. Another potential health economic benefit with these types of interventions is the capability to virtually bring the patient in contact with the treating team, without the need for expensive transportation. In the situation that digital interventions would be provided on top of face-to-face visits, the intervention could entail an extra cost. On the other hand, if face-to-face visits can be fully replaced by digital interventions, then this will most likely result in cost savings. Cost transfers from health care systems to patients might be a negative externali ty – when patients need to install expensive ICT infrastructure or pay for larger mobile data plans. Implementation and cost-effectiveness of DHIs for secondary stroke prevention will also depend on the presence of a legal framework for DHIs, such as reimbursement and liability regulation. With current pursued savings in health care, the potential for reorganization of patient-centered care by the use of DHIs is huge. In order to improve the evaluation of DHIs, there is a need to consider sustainability and cost-effectiveness from the start of their conception and implementation [9]. Our review clearly indicates that this is lacking in the current development and research efforts. Therefore, it is mandatory that more care is given to health economic aspects in future research efforts in order to effectively drive the transformation of health care forward.
Conclusions
There is a lack of evidence on health economic data on DHIs for secondary stroke prevention. Even taking into account very broad inclusion criteria in terms of study design, no studies were included, and no models were found. Future research in this area should take health economics into consideration when designing a trial, and there is a clear need for health economic evidence and models.
Disclosure Statement
Alain Dupont, Pierter Cornu, Koen Putman, and Stephane Steurbaut report no disclosures. Raf Brouns is co-founder of Zebra Academy. Alexis Valenzuela Espinoza, Robbert-Jan van Hooff, and Raf Brouns are holders of a patent on in-ambulance telestroke.
Funding Sources
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Supplementary Material
Supplementary data
Supplementary data
References
- 1.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012 Dec;380((9859)):2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Truelsen T, Piechowski-Jozwiak B, Bonita R, Mathers C, Bogousslavsky J, Boysen G. Stroke incidence and prevalence in Europe: a review of available data. European journal of neurology : the official journal of the European Federation of Neurological Societies. 2006;13:581–598. doi: 10.1111/j.1468-1331.2006.01138.x. [DOI] [PubMed] [Google Scholar]
- 3.Mohan KM, Wolfe CD, Rudd AG, Heuschmann PU, Kolominsky-Rabas PL, Grieve AP. Risk and cumulative risk of stroke recurrence: a systematic review and meta-analysis. Stroke. 2011 May;42((5)):1489–94. doi: 10.1161/STROKEAHA.110.602615. [DOI] [PubMed] [Google Scholar]
- 4.Dhamoon MS, Tai W, Boden-Albala B, Rundek T, Paik MC, Sacco RL, et al. Risk of myocardial infarction or vascular death after first ischemic stroke: the Northern Manhattan Study. Stroke. 2007 Jun;38((6)):1752–8. doi: 10.1161/STROKEAHA.106.480988. [DOI] [PubMed] [Google Scholar]
- 5.Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014 Jul;45((7)):2160–236. doi: 10.1161/STR.0000000000000024. [DOI] [PubMed] [Google Scholar]
- 6.Ovbiagele B, Saver JL, Bang H, Chambless LE, Nassief A, Minuk J, et al. VISP Study Investigators Statin treatment and adherence to national cholesterol guidelines after ischemic stroke. Neurology. 2006 Apr;66((8)):1164–70. doi: 10.1212/01.wnl.0000208403.18885.0e. [DOI] [PubMed] [Google Scholar]
- 7.Kraft P, Hillmann S, Rücker V, Heuschmann PU. Telemedical strategies for the improvement of secondary prevention in patients with cerebrovascular events-A systematic review and meta-analysis. Int J Stroke. 2017 Aug;12((6)):597–605. doi: 10.1177/1747493017706188. [DOI] [PubMed] [Google Scholar]
- 8.Widmer RJ, Collins NM, Collins CS, West CP, Lerman LO, Lerman A. Digital health interventions for the prevention of cardiovascular disease: a systematic review and meta-analysis. Mayo Clin Proc. 2015 Apr;90((4)):469–80. doi: 10.1016/j.mayocp.2014.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray E, Hekler EB, Andersson G, Collins LM, Doherty A, Hollis C, et al. Evaluating digital health interventions: key questions and approaches. Am J Prev Med. 2016 Nov;51((5)):843–51. doi: 10.1016/j.amepre.2016.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International journal of surgery (London, England) 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dec;5((1)):210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mittag O, China C, Hoberg E, Juers E, Kolenda KD, Richardt G, et al. Outcomes of cardiac rehabilitation with versus without a follow-up intervention rendered by telephone (Luebeck follow-up trial): overall and gender-specific effects. Int J Rehabil Res. 2006 Dec;29((4)):295–302. doi: 10.1097/MRR.0b013e328010ba9a. [DOI] [PubMed] [Google Scholar]
- 13.Lazzaro MA, Krishnan K, Prabhakaran S. Detection of atrial fibrillation with concurrent holter monitoring and continuous cardiac telemetry following ischemic stroke and transient ischemic attack. J Stroke Cerebrovasc Dis. 2012 Feb;21((2)):89–93. doi: 10.1016/j.jstrokecerebrovasdis.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 14.Schweier R, Romppel M, Richter C, Hoberg E, Hahmann H, Scherwinski I, et al. A web-based peer-modeling intervention aimed at lifestyle changes in patients with coronary heart disease and chronic back pain: sequential controlled trial. J Med Internet Res. 2014 Jul;16((7)):e177. doi: 10.2196/jmir.3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Devi R, Singh SJ, Powell J, Fulton EA, Igbinedion E, Rees K. Internet-based interventions for the secondary prevention of coronary heart disease. Cochrane Database Syst Rev. 2015 Dec;((12)):CD009386. doi: 10.1002/14651858.CD009386.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corazza I, Bianchini D, Urbinati S, Zannoli R. REHAL®, a telemedicine platform for home cardiac rehabilitation. Minerva Cardioangiol. 2014 Oct;62((5)):399–405. [PubMed] [Google Scholar]
- 17.Dregan A, van Staa TP, McDermott L, McCann G, Ashworth M, Charlton J, et al. Trial Steering Committee. Data Monitoring Committee Point-of-care cluster randomized trial in stroke secondary prevention using electronic health records. Stroke. 2014 Jul;45((7)):2066–71. doi: 10.1161/STROKEAHA.114.005713. [DOI] [PubMed] [Google Scholar]
- 18.Pfaeffli Dale L, Whittaker R, Jiang Y, Stewart R, Rolleston A, Maddison R. Text Message and Internet Support for Coronary Heart Disease Self-Management: Results From the Text4Heart Randomized Controlled Trial. J Med Internet Res. 2015 Oct;17((10)):e237. doi: 10.2196/jmir.4944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Banner D, Lear S, Kandola D, Singer J, Horvat D, Bates J, et al. The experiences of patients undertaking a ‘virtual' cardiac rehabilitation program. Stud Health Technol Inform. 2015;209:9–14. [PubMed] [Google Scholar]
- 20.Mayer F, Stahrenberg R, Gröschel K, Mostardt S, Biermann J, Edelmann F, et al. Cost-effectiveness of 7-day-Holter monitoring alone or in combination with transthoracic echocardiography in patients with cerebral ischemia. Clin Res Cardiol. 2013 Dec;102((12)):875–84. doi: 10.1007/s00392-013-0601-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vegter S, Oosterhof P, van Boven JF, Stuurman-Bieze AG, Hiddink EG, Postma MJ. Improving adherence to lipid-lowering therapy in a community pharmacy intervention program: a cost-effectiveness analysis. J Manag Care Spec Pharm. 2014 Jul;20((7)):722–32. doi: 10.18553/jmcp.2014.20.7.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yong JH, Thavorn K, Hoch JS, Mamdani M, Thorpe KE, Dorian P, et al. EMBRACE Steering Committee Potential Cost-Effectiveness of Ambulatory Cardiac Rhythm Monitoring After Cryptogenic Stroke. Stroke. 2016 Sep;47((9)):2380–5. doi: 10.1161/STROKEAHA.115.011979. [DOI] [PubMed] [Google Scholar]
- 23.Bashshur RL, Shannon GW, Smith BR, Alverson DC, Antoniotti N, Barsan WG, et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemed J E Health. 2014 Sep;20((9)):769–800. doi: 10.1089/tmj.2014.9981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Franklin NC, Lavie CJ, Arena RA. Personal health technology: A new era in cardiovascular disease prevention. Postgrad Med. 2015 Mar;127((2)):150–8. doi: 10.1080/00325481.2015.1015396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clark RA, Conway A, Poulsen V, Keech W, Tirimacco R, Tideman P. Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol. 2015 Jan;22((1)):35–74. doi: 10.1177/2047487313501093. [DOI] [PubMed] [Google Scholar]
- 26.Perera R, McFadden E, McLellan J, Lung T, Clarke P, Pérez T, et al. Optimal strategies for monitoring lipid levels in patients at risk or with cardiovascular disease: a systematic review with statistical and cost-effectiveness modelling. Health Technol Assess. 2015 Dec;19((100)):1–401. doi: 10.3310/hta191000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Neubeck L, Redfern J, Fernandez R, Briffa T, Bauman A, Freedman SB. Telehealth interventions for the secondary prevention of coronary heart disease: a systematic review. Eur J Cardiovasc Prev Rehabil. 2009 Jun;16((3)):281–9. doi: 10.1097/HJR.0b013e32832a4e7a. [DOI] [PubMed] [Google Scholar]
- 28.Pietrzak E, Cotea C, Pullman S. Primary and secondary prevention of cardiovascular disease: is there a place for Internet-based interventions? J Cardiopulm Rehabil Prev. 2014 Sep-Oct;34((5)):303–17. doi: 10.1097/HCR.0000000000000063. [DOI] [PubMed] [Google Scholar]
- 29.Yan LL, Chen S, Zhou B, Zhang J, Xie B, Luo R, et al. A randomized controlled trial on rehabilitation through caregiver-delivered nurse-organized service programs for disabled stroke patients in rural china (the RECOVER trial): design and rationale. Int J Stroke. 2016 Oct;11((7)):823–30. doi: 10.1177/1747493016654290. [DOI] [PubMed] [Google Scholar]
- 30.Southard BH, Southard DR, Nuckolls J. Clinical trial of an Internet-based case management system for secondary prevention of heart disease. J Cardiopulm Rehabil. 2003 Sep-Oct;23((5)):341–8. doi: 10.1097/00008483-200309000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Devi R, Powell J, Singh S. A web-based program improves physical activity outcomes in a primary care angina population: randomized controlled trial. J Med Internet Res. 2014 Sep;16((9)):e186. doi: 10.2196/jmir.3340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sullivan PW, Arant TW, Ellis SL, Ulrich H. The cost effectiveness of anticoagulation management services for patients with atrial fibrillation and at high risk of stroke in the US. Pharmacoeconomics. 2006;24((10)):1021–33. doi: 10.2165/00019053-200624100-00009. [DOI] [PubMed] [Google Scholar]
- 33.Carlsson AC, Wändell PE, Gigante B, Leander K, Hellenius ML, de Faire U. Seven modifiable lifestyle factors predict reduced risk for ischemic cardiovascular disease and all-cause mortality regardless of body mass index: a cohort study. Int J Cardiol. 2013 Sep;168((2)):946–52. doi: 10.1016/j.ijcard.2012.10.045. [DOI] [PubMed] [Google Scholar]
- 34.Chow CK, Jolly S, Rao-Melacini P, Fox KA, Anand SS, Yusuf S. Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation. 2010 Feb;121((6)):750–8. doi: 10.1161/CIRCULATIONAHA.109.891523. [DOI] [PubMed] [Google Scholar]
- 35.Mackay-Lyons M, Thornton M, Ruggles T, Che M. Non-pharmacological interventions for preventing secondary vascular events after stroke or transient ischemic attack. Cochrane Database Syst Rev. 2013 Mar;((3)):CD008656. doi: 10.1002/14651858.CD008656.pub2. [DOI] [PubMed] [Google Scholar]
- 36.Reid RD, Morrin LI, Beaton LJ, Papadakis S, Kocourek J, McDonnell L, et al. Randomized trial of an internet-based computer-tailored expert system for physical activity in patients with heart disease. Eur J Prev Cardiol. 2012 Dec;19((6)):1357–64. doi: 10.1177/1741826711422988. [DOI] [PubMed] [Google Scholar]
- 37.Antypas K, Wangberg SC. E-Rehabilitation - an Internet and mobile phone based tailored intervention to enhance self-management of cardiovascular disease: study protocol for a randomized controlled trial. BMC Cardiovasc Disord. 2012 Jul;12((1)):50. doi: 10.1186/1471-2261-12-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kelders SM, Van Gemert-Pijnen JE, Werkman A, Nijland N, Seydel ER. Effectiveness of a Web-based intervention aimed at healthy dietary and physical activity behavior: a randomized controlled trial about users and usage. J Med Internet Res. 2011 Apr;13((2)):e32. doi: 10.2196/jmir.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aalbers T, Baars MA, Rikkert MG. Characteristics of effective Internet-mediated interventions to change lifestyle in people aged 50 and older: a systematic review. Ageing Res Rev. 2011 Sep;10((4)):487–97. doi: 10.1016/j.arr.2011.05.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data
Supplementary data