Abstract
Background
Little is known about variation in use of rehabilitation services provided in acute care hospitals for people who have had a stroke.
Objective
The objective was to examine patient and hospital sources of variation in acute care rehabilitation services provided for stroke.
Design
This was a retrospective, cohort design.
Methods
The sample consisted of Medicare fee-for-service beneficiaries with ischemic stroke admitted to acute care hospitals in 2010. Medicare claims data were linked to the Provider of Services file to gather information on hospital characteristics and the American Community Survey for sociodemographic data. Chi-square tests compared patient and hospital characteristics stratified by any rehabilitation use. We used multilevel, multivariable random effect models to identify patient and hospital characteristics associated with the likelihood of receiving any rehabilitation and with the amount of therapy received in minutes.
Results
Among 104,295 patients, 85.2% received rehabilitation (61.5% both physical therapy and occupational therapy; 22.0% physical therapy only; and 1.7% occupational therapy only). Patients received 123 therapy minutes on average (median [SD] = 90.0 [99.2] minutes) during an average length of stay of 4.8 [3.5] days. In multivariable analyses, male sex, dual enrollment in Medicare and Medicaid, prior hospitalization, ICU stay, and feeding tube were associated with lower odds of receiving any rehabilitation services. These same variables were generally associated with fewer minutes of therapy. Patients treated by tissue plasminogen activator, in limited-teaching and nonteaching hospitals, and in hospitals with inpatient rehabilitation units, were more likely to receive more therapy minutes.
Limitation
The findings are limited to patients with ischemic stroke.
Conclusion
Only 61% of patients with ischemic stroke received both physical therapy and occupational therapy services in the acute setting. We identified considerable variation in the use of rehabilitation services in the acute care setting following a stroke.
Stroke, a leading cause of hospitalization, is associated with high hospital readmission rates, postacute care use, and long-term disability.1–3 Early mobilization during the acute hospitalization following a stroke is recommended to prevent immobility-related deconditioning.4,5 Rehabilitation services including physical therapy and occupational therapy play important roles in promoting functional recovery and preventing deconditioning during acute hospitalizations, particularly when the patient is in the intensive care unit (ICU) and/or has a prolonged stay.6–9 Likewise in patients with a short length of stay, having consultation with a rehabilitation provider can improve the transition to postacute care or to home.10,11 Current recommendations on the use of rehabilitation services during acute hospitalization in patients with ischemic stroke are ambiguous.12 For example, the American Heart Association/American Stroke Association recommends early mobilization after stroke, but does not provide clear recommendations on the optimal dosage of therapy during acute hospitalizations.12 A recent editorial in PTJ strongly highlighted the lack of evidence-based guidance on the appropriate dosage of rehabilitation service.13 This information is currently lacking for the treatment of most conditions, in all settings (including acute hospitals and postacute settings, whether skilled nursing facilities, inpatient rehabilitation facilities, or home health care).
With bundling of acute and postacute payments, the need to understand the use and contributions of rehabilitation services in acute and postacute settings is important.14 To date, the majority of studies on use of health services following an acute care admission for stroke have shown that variation in the processes of care, such as thrombolysis treatment, hospital arrival times, and emergency department waiting time, is due to both patient- and hospital-level factors.15–17 The examination of patient- and hospital-level factors contributing to variation in the use of rehabilitation services in patients with stroke during acute care has not been thorough. This is primarily due to lack of development of methods to extract data associated with use of rehabilitation services in acute care hospitals. There is some evidence to suggest that many patients with stroke do not receive hospital-based physical therapy services.18–20 Freburger and colleagues found that some of the variation in physical therapy use is attributable to hospital characteristics such as profit status and teaching status.19 However, this study used data from a single state, North Carolina, therefore limiting generalizability.19 Andrews et al used data from 2 US states and found that 33% of patients with stroke did not receive any hospital-based physical therapy, and 34% received a low dosage of therapy (based on quartile distribution of hospital charges). They also found that the amount of therapy received was inversely related to risk of hospital readmission.18 Another recent study by Freburger et al, using a 20% random sample of national Medicare claims data in patients with stroke, found that 21.6% of patients did not receive any hospital-based therapy.20 All the aforementioned studies used hospital charges for rehabilitation services to quantify rehabilitation use, highlighting the methodological challenges in using charge information associated with hospital-based services because these charges vary by region.
Unlike in postacute settings, patient functional status is not a quality measure for the acute setting. Currently, there is no incentive for hospitals to report functional status to the Centers for Medicare and Medicaid Services. We hypothesized that in the absence of clear evidence-based practice guidelines and no incentive to report patient functional status, there would be marked variation in the provision of hospital-based rehabilitation services in patients with stroke and that factors other than need would be associated with use. Thus, the objectives of this study were: (1) to examine factors associated with receipt of rehabilitation services in the acute care hospital for patients with ischemic stroke, and (2) to examine the factors associated with amount of rehabilitation therapy delivery.
Methods
Data Sources
Data sources for this study were the 2010 100% Medicare inpatient claims data using the Standard Analytical File (SAF) format, linked to the Master Beneficiary Summary File. The SAF file contains claims for all inpatient stays, including acute hospitals and information about diagnostic conditions, surgical procedures, length of stay, and separate revenue center codes for evaluation and use of rehabilitation services (occupational therapy and physical therapy) as well as the number of rehabilitation therapy units delivered. The Master Beneficiary Summary File comprises Medicare enrollment indicators and beneficiary sociodemographic characteristics. Hospital-level factors were retrieved from the Provider of Services file. The Chronic Condition Data Warehouse (CCW) was used to retrieve the number of chronic conditions for the study cohort.21 We obtained median household income and household educational information for the patient's zip code of residence from the American Community Survey data (2010). Our study was reviewed and approved by the Institutional Review Board of Brown University, and a Data Use Agreement was approved by Centers for Medicare & Medicaid Services (DUA RSCH-2017-51217).
Study Population
The study sample consisted of Medicare beneficiaries with fee-for-service plans aged 66 years and older who were admitted to acute or critical access hospitals in 2010 for a new, primary diagnosis of ischemic stroke using the International Classification of Diseases, Ninth Revision (ICD-9) codes 433.x1, 434.x1, and 436. To obtain a complete medical history and health services use, the sample was restricted to patients who had 12 months of continuous Medicare fee-for-service enrollment prior to and 3 months after the index hospitalization. Patients enrolled in Medicare based on disability, who had a history of prior stroke in the past 3 months, who left the hospital against medical advice, transferred to another acute care hospital, or died during the index hospitalization were excluded from our sample (Fig. 1). We excluded patients who transferred from another hospital and nonemergent admissions because there would be incomplete information on their therapy use and they would have different severities of condition and could have a different process of care.
Figure 1.
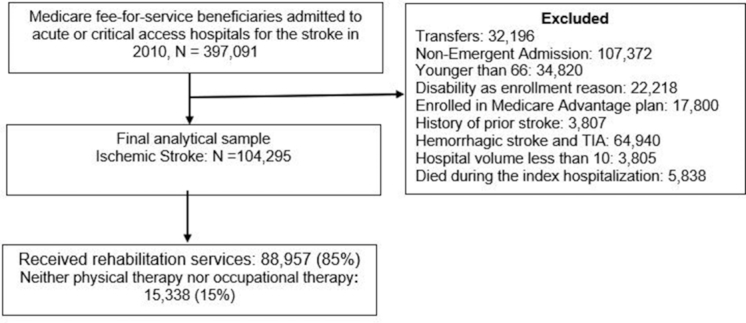
The derivation of the cohort.
Outcome variable
Hospital-based rehabilitation service was the primary dependent variable of interest. It was categorized using the revenue center codes for occupational therapy and physical therapy services described in Table 1. The SAF file contains separate revenue center codes for evaluation and use of rehabilitation services (occupational therapy and physical therapy) as well as the number of rehabilitation therapy units delivered. We assigned 15 minutes for each therapy unit and 30 minutes for each evaluation unit at the time of admission. We created 4 mutually exclusive groups categorizing the type of rehabilitation services received. The first group included those patients who received both physical therapy and occupational therapy. The second group included those patients who received physical therapy only (evaluation and/or therapy). The third group included patients who received occupational therapy only (evaluation and/or therapy). The fourth group included patients who did not receive either physical therapy or occupational therapy evaluation or therapy. Also, to estimate total rehabilitation services provided, we summed physical therapy and occupational therapy minutes recorded during the entire hospital stay. For multilevel analysis, we created 2 outcomes. The first outcome was receipt of any rehabilitation services (combining 3 groups: both physical therapy and occupational therapy, physical therapy only, occupational therapy only versus neither physical therapy nor occupational therapy), and the second outcome was the amount of rehabilitation therapy services (in minutes) during the entire stay.
Table 1.
Revenue Center Codes for Rehabilitation Services in the Standard Analytical File
| Rehabilitation Services | Revenue Center Code |
|---|---|
| Occupational therapy evaluation | 0434 |
| Physical therapy evaluation | 0424 |
| Occupational therapy: consultation, visit charge, hourly charge, group rate | 0430, 0431, 0432, 0433, 0439 |
| Physical therapy: consultation, visit charge, hourly charge, group rate | 0420, 0421, 0422, 0423, 0429 |
Study Covariates
Demographic variables
The study covariates included patient-level variables (eg, age, sex, and race). Age was categorized into 5 levels: 66–70, 71–75, 76–80, 81–85, and >85 years. Because 83% of the study sample was non-Hispanic white, race/ethnicity was categorized into non-Hispanic white, non-Hispanic black, and other races. Covariates also included several indicators of socioeconomic status such as Medicare-Medicaid dual eligibility, education, and income. Dual eligibility was dichotomized into “yes” and “no” categories and classified as “yes” if the beneficiary was enrolled in both Medicare and Medicaid. These variables were extracted from the Master Beneficiary Summary File. We also included patients’ residential zip code median household income and household education by zip code. Zip-code–level income and zip-code–level education were categorized into 4 levels based on quartile distribution.
Hospital-level variables
We obtained hospital-level information from the Provider of Services file, which includes organizational information about Medicare-certified hospitals. Hospital-level variables included location (urban/rural), profit status, teaching status, stroke volume, and hospital with inpatient rehabilitation unit or swing beds. Prior studies reported that hospital characteristics, including volume,22,23 affiliation to a medical school,24,25 and having a separate rehabilitation unit26 were associated with processes of care and patient outcomes. We dichotomized hospitals’ ownership (for-profit versus nonprofit). Consistent with methods from other studies,27 hospital teaching status was classified into 3 categories: major teaching hospitals, limited teaching hospitals, and no affiliation. Hospitals were also classified into quartiles based on annual volumes of patients with stroke (quartile 1: ≤123 cases per year; quartile 2: 124 to 228; quartile 3: 229 to 370, and quartile 4: ≥371). We identified hospitals with inpatient rehabilitation units if the hospital or health care system owned inpatient rehabilitation facilities.28 Hospital swing beds are transitional care beds in acute hospitals that can be used for postacute skilled nursing care.
Case-mix/severity variables
To control for condition severity/case-mix differences that might influence use of rehabilitation services at baseline, we also included, from the inpatient SAF file, patient-level variables related to comorbidities, length of stay, prior hospitalization, length of ICU stay, receipt of tissue plasminogen activator (tPA), and feeding tube insertion. Previous studies have shown that some of our case-mix variables, including clinical and processes of care variables retrieved from claims data, can be good proxies for stroke severity.29,30 Because comorbidities and comorbidity indexes from inpatient claims do not fully capture chronic conditions or predict patient functional status or hospital readmission,31,32 we decided to use data from the CCW to capture comorbidities. The CCW has developed an algorithm based on particular diagnosis and procedure codes found on institutional and noninstitutional claims across multiple care settings within a specified reference period to identify chronic conditions.21 We used the following chronic conditions flags from the CCW: acquired hypothyroidism, acute myocardial infarction, Alzheimer disease, Alzheimer disease–related disorders or senile dementia, anemia, asthma, atrial fibrillation, benign prostatic hyperplasia, colorectal cancer, endometrial cancer, breast cancer, lung cancer, prostate cancer, cataract, chronic kidney disease, chronic obstructive pulmonary disease, depression, diabetes, glaucoma, heart failure, hip/pelvic fracture, hyperlipidemia, hypertension, ischemic heart disease, osteoporosis, and rheumatoid arthritis/osteoarthritis. Length of stay in hospital was used as continuous variable. We identified tPA use using ICD-9 procedure codes 4311, 4319, and 4432 from the SAF file. We created a dichotomous variables ICU stay and for prior hospitalization if the patient had any hospitalization in the last 12 months.
Analysis
We used χ2 tests to compare the percentage of patients receiving any rehabilitation service (physical therapy and/or occupational therapy) by individual patient and hospital characteristics. To account for the clustering of patients nested within hospitals in our data, we used multilevel, multivariable random effect models. In the first model, we assessed the likelihood of receiving rehabilitation (yes/no) across hospitals and factors associated with receipt of any rehabilitation services. In the second model, using the linear mixed model, we estimated the association of hospital and patient-level factors with total therapy minutes among those patients who received some amount of therapy. The models were adjusted for age, sex, race, dual Medicare and Medicaid enrollment, income, education, comorbidities, prior hospitalization in the 12 months before index hospital admission, length of stay, ICU stay, feeding tube insertion, tPA administration, and hospital characteristic (urban/rural, profit status, hospital stroke volume, affiliation to medical school, rehabilitation unit, and swing bed unit). All the statistical significance tests were 2-sided and tested at the .05 significance level. We tested for multicolinearity among covariates in our model. All the coefficient and variable inflation factor values were in the very low range (0.25 for coefficient and 2.63 for variable inflation factor ). All the statistical analyses were performed using SAS 9.4 (SAS Inc., Cary, NC, USA).
Sensitivity analyses
We conducted multilevel logistic regression analyses to identify predictors of receiving only physical therapy (yes/no). We limited our analyses to the subgroup of patients who received physical therapy only (22%) and did not create an occupational therapy–only subgroup due to the small number (1.7% of sample). The results of the subgroup analysis are reported in the eTable (available at https://academic.oup.com/ptj). This study is reported as per the STROBE guidelines (S2 STROBE Checklist).
Role of the Funding Source
Sponsors had no role in the study design, analysis, interpretation of the data, or in the writing of the manuscript.
Results
Table 2 presents the characteristics of patients receiving rehabilitation services by type of service received. The mean [SD] age for all patients was 80.6 [7.7] years (data not shown) and the mean hospital length of stay was 4.8 [3.5] days. Patients with ischemic stroke received a mean of 123.2 [99.2] minutes, (median = 90.0) of rehabilitation therapy during the stay. For this cohort, 61.5% received both physical therapy and occupational therapy services, 22.0% received only physical therapy, 1.7% received only occupational therapy, and 15.0% did not receive either physical therapy or occupational therapy.
Table 2.
Sociodemographic, Clinical, and Hospital Characteristics, by Physical Therapy and Occupational Therapy Servicea
| Overall totals, n (%) | Total Sample, N (%) | Both Physical Therapy and Occupational Therapy, % | Physical Therapy Only, % | Occupational Therapy Only, % | Neither Physical Therapy nor Occupational Therapy, % | Pb |
|---|---|---|---|---|---|---|
| 104,295 (100) | 64,159 (61.5) | 23,014 (22.0) | 1784 (1.7) | 15,338 (15.0) | ||
| Patient-level characteristics (%) | ||||||
| Age group | ||||||
| 66–70 | 12,903 (12.37) | 58.97 | 20.10 | 2.36 | 18.56 | <.0001 |
| 71–75 | 16,573 (15.89) | 60.14 | 21.26 | 2.12 | 16.48 | |
| 76–80 | 21,021 (20.16) | 61.73 | 21.84 | 1.84 | 14.59 | |
| 81–85 | 24,461 (23.45) | 63.38 | 22.66 | 1.34 | 12.62 | |
| 85+ | 29,337 (28.13) | 61.71 | 23.05 | 1.41 | 13.83 | |
| Gender | ||||||
| Male | 42,163 (40.43) | 61.19 | 21.57 | 1.86 | 15.37 | .0020 |
| Female | 62,132 (59.57) | 61.74 | 22.40 | 1.61 | 14.25 | |
| Race/ethnicity | ||||||
| White | 86,653 (83.08) | 61.75 | 21.68 | 1.73 | 14.83 | <.0001 |
| Black | 10,633 (10.20) | 63.30 | 21.76 | 1.72 | 13.21 | |
| Other | 7009 (6.72) | 55.90 | 27.29 | 1.41 | 15.39 | |
| Dual-eligible | ||||||
| Yes | 15,172 (14.55) | 55.89 | 25.92 | 1.54 | 16.66 | <.0001 |
| No | 89,123 (85.45) | 62.48 | 21.41 | 1.74 | 14.37 | |
| Resident zip income quartile | ||||||
| 1 (low) | 17,440 (16.72) | 58.21 | 24.64 | 1.50 | 15.65 | <.0001 |
| 2 | 24,331 (23.33) | 60.94 | 21.82 | 1.67 | 15.57 | |
| 3 | 26,936 (25.83) | 63.55 | 20.46 | 1.82 | 14.17 | |
| 4 (high) | 35,588 (34.12) | 62.00 | 22.19 | 1.76 | 14.06 | |
| Resident zip education quartile | ||||||
| 1 (low) | 17,746 (17.02) | 56.07 | 26.32 | 1.54 | 16.07 | <.0001 |
| 2 | 27,753 (26.61) | 60.26 | 22.90 | 1.68 | 15.17 | |
| 3 | 32,387 (31.05) | 62.73 | 21.24 | 1.73 | 14.31 | |
| 4 (high) | 26,409 (25.32) | 65.02 | 19.35 | 1.83 | 13.80 | |
| Number of CCW chronic conditions | ||||||
| 0 | 9534 (9.14) | 63.65 | 20.57 | 1.91 | 13.89 | <.0001 |
| 1 | 8511 (8.16) | 63.89 | 19.67 | 1.77 | 14.66 | |
| 2 | 12,049 (11.55) | 61.50 | 21.43 | 1.86 | 15.21 | |
| 3 | 15,364 (14.73) | 62.02 | 21.10 | 1.80 | 15.09 | |
| 4 | 16,117 (15.45) | 60.89 | 22.58 | 1.79 | 14.73 | |
| 5 | 14,144 (13.56) | 61.41 | 22.47 | 1.66 | 14.46 | |
| 6+ | 28,576 (27.40) | 60.24 | 23.58 | 1.50 | 14.68 | |
| Prior hospitalization (last 12 mo) | ||||||
| Yes | 35,429 (33.97) | 60.33 | 23.00 | 1.66 | 15.01 | <.0001 |
| No | 68,866 (66.03) | 62.13 | 21.59 | 1.74 | 14.55 | |
| Length of stayc | 4.8 (3.5) | 4.3 (3.3) | 3.3 (2.9) | 3.2 (2.8) | 4.7 (3.5) | <.0001 |
| ICU stayc | ||||||
| Yes | 52,916 (50.74) | 64.88 | 20.44 | 1.60 | 13.08 | <.0001 |
| No | 51,379 (49.26) | 58.05 | 23.75 | 1.82 | 16.38 | |
| Feeding tube | ||||||
| Yes | 4443 (4.26) | 74.48 | 15.85 | 1.15 | 8.53 | <.0001 |
| No | 99,852 (95.74) | 60.94 | 22.34 | 1.74 | 14.98 | |
| Tissue plasminogen activator (tPA) | ||||||
| Yes | 5016 (4.81) | 76.93 | 13.60 | 1.59 | 7.86 | <.0001 |
| No | 99,279 (95.19) | 60.74 | 22.49 | 1.72 | 15.05 | |
| Hospital characteristics | ||||||
| Location | ||||||
| Urban | 91,705 (87.93) | 63.22 | 21.00 | 1.75 | 14.03 | <.0001 |
| Rural | 12,590 (12.07) | 49.12 | 29.83 | 1.40 | 19.65 | |
| Profit status | ||||||
| Yes | 13,440 (12.89) | 54.84 | 28.07 | 1.23 | 15.86 | <.0001 |
| No | 90,855 (87.11) | 62.50 | 21.18 | 1.78 | 14.54 | |
| Teaching status | ||||||
| Major | 23,696 (22.72) | 63.81 | 20.01 | 2.28 | 13.90 | <.0001 |
| Limited | 24,757 (23.74) | 63.69 | 20.56 | 1.68 | 14.06 | |
| No affiliation | 55,842 (53.54) | 59.58 | 23.60 | 1.48 | 15.33 | |
| Hospital volume | ||||||
| 1 (≤123) | 23,268 (22.31) | 50.72 | 29.16 | 1.61 | 18.51 | <.0001 |
| 2 (124–228) | 27,348 (26.22) | 61.13 | 22.72 | 1.48 | 14.67 | |
| 3 (229–370) | 26,498 (25.41) | 65.68 | 18.98 | 1.68 | 13.65 | |
| 4 (≥371) | 27,181 (26.06) | 67.09 | 18.34 | 2.06 | 12.51 | |
| Hospital with rehabilitation unit | ||||||
| Yes | 52,245 (50.09) | 67.55 | 16.88 | 1.85 | 13.72 | <.0001 |
| No | 52,050 (49.91) | 55.46 | 27.27 | 1.57 | 15.70 | |
| Hospital with swing bed | ||||||
| Yes | 3932 (3.77) | 46.08 | 31.56 | 1.25 | 21.11 | <.0001 |
| No | 100,363 (96.23) | 62.12 | 21.69 | 1.73 | 14.46 | |
aCCW = Chronic Conditions Data Warehouse; ICU = intensive care unit.
bThe P value was compared between patient and hospital characteristics with the 4 groups.
cDepicted as mean and standard deviation.
Table 3 presents the results of separate multivariate models associated with receipt of any rehabilitation services (physical therapy only, occupational therapy only, or both physical therapy and occupational therapy) and amount of rehabilitation services. Patients who were older (>70 years), had longer lengths of stay, and received tPA were more likely to receive any rehabilitation services. Patients who were dually enrolled in Medicare and Medicaid (dual patients) were 16% less likely to receive any rehabilitation services (odds ratio [OR] = 0.84; 95% confidence interval [CI] = 0.79–0.88) compared with nondual patients. Patients with a recent prior history of hospitalization were 11% less likely to receive any rehabilitation services (OR = 0.89; 95% CI = 0.85–0.93). Stroke severity as indicated by having an ICU stay (OR = 0.90; 95% CI = 0.86–0.94) or having a feeding tube inserted (OR = 0.47; 95% CI = 0.41–0.53) were significantly less likely to receive any rehabilitation services.
Table 3.
Patient and Hospital Characteristics Associated With Receipt of Any Therapy and With Minutes of Therapy:a Results of 2 Separate Models
| Characteristics | Odds Ratio (95% CI) | Estimates (95% CI)b |
|---|---|---|
| Any Rehabilitation (Yes/No) | Minutes of Rehabilitation During Entire Stay | |
| Patient characteristics | ||
| Age categories | ||
| 66–70 | Ref | Ref |
| 71–75 | 1.17 (1.09–1.25) | 2.99 (1.12–4.87) |
| 76–80 | 1.30 (1.22–1.39) | 3.80 (2.00–5.61) |
| 81–85 | 1.53 (1.43–1.63) | 5.95 (4.18–7.72) |
| >85 | 1.35 (1.27–1.42) | 4.50 (2.76–5.24) |
| Sex | ||
| Female | Ref | Ref |
| Male | 0.95 (0.92–0.99) | −1.15 (−2.16 to −0.14) |
| Race/ethnicity | ||
| White | Ref | Ref |
| Black | 1.21 (1.12–1.30) | −0.02 (−1.89 to 1.18) |
| Other | 1.12 (1.03–1.21) | 0.58 (−1.68 to 2.85) |
| Dual eligibility | ||
| No | Ref | Ref |
| Yes | 0.84 (0.79–0.88) | −5.07 (−6.60 to −3.53) |
| Resident zip income quartile | ||
| 1 (low) | Ref | Ref |
| 2 | 0.99 (0.92–1.05) | −1.05 (−2.83 to 0.74) |
| 3 | 1.02 (0.95–1.00) | −0.62 (−2.51 to 1.27) |
| 4 (high) | 0.96 (0.89–1.04) | −0.43 (−2.55 to 1.69) |
| Resident zip education quartile | ||
| 1 (low) | Ref | Ref |
| 2 | 1.00 (0.94–1.07) | −0.18 (−1.93 to 1.58) |
| 3 | 1.01 (0.94–1.09) | 0.19 (−1.74 to 2.10) |
| 4 (high) | 0.98 (0.91–1.06) | 0.78 (−1.39 to 2.96) |
| Number of CCW chronic conditions | ||
| 0 | Ref | Ref |
| 1 | 0.90 (0.82–0.98) | 0.55 (−2.89 to 1.78) |
| 2 | 0.89 (0.82–0.97) | −1.17 (−3.32 to 0.99) |
| 3 | 0.87 (0.80–0.94) | −2.22 (−4.28 to −0.16) |
| 4 | 0.90 (0.83–0.97) | −1.77 (−3.82 to 0.28) |
| 5 | 0.89 (0.82–0.97) | −1.83 (−3.95 to 0.28) |
| 6+ | 0.85 (0.79–0.92) | −2.99 (−4.95 to −1.03) |
| Length of stay | 1.29 (1.27–1.30) | 14.20 (14.04–14.36) |
| Prior hospitalization | ||
| No | Ref | Ref |
| Yes | 0.89 (0.85–0.93) | −3.71 (−4.81 to −2.61) |
| ICU stay | ||
| No | Ref | Ref |
| Yes | 0.90 (0.86–0.94) | 0.04 (−1.29 to 1.37) |
| Feeding tube | ||
| No | Ref | Ref |
| Yes | 0.47 (0.41–0.53) | 5.71 (3.14–8.27) |
| tPA | ||
| No | Ref | Ref |
| Yes | 1.51 (1.40–1.76) | 16.57 (14.27–18.86) |
| Hospital characteristics | ||
| Urban | Ref | Ref |
| Rural | 1.25 (1.11–1.41) | 4.56 (−1.52 to 10.64) |
| Profit status | ||
| No | Ref | Ref |
| Yes | 0.92 (0.82–1.03) | 5.58 (−0.29 to 11.45) |
| Teaching status | ||
| Major | Ref | Ref |
| Limited | 1.12 (0.97–1.28) | 19.74 (12.53–26.97) |
| No affiliation | 1.12 (0.98–1.26) | 20.96 (14.55–27.38) |
| Hospital stroke volume | ||
| 1 (≤123) | Ref. | Ref. |
| 2 (124–228) | 1.20 (1.08–1.34) | 0.64 (−4.97 to 6.12) |
| 3 (229–370) | 1.29 (1.13–1.46) | −1.94 (−8.66 to 4.77) |
| 4 (≥371) | 1.40 (1.21–1.63) | −6.09 (−14.17 to 1.98) |
| Hospital with rehabilitation unit | ||
| No | Ref | Ref |
| Yes | 1.10 (1.01–1.20) | 8.65 (4.13–13.18) |
| Hospital with swing bed unit | ||
| No | Ref | Ref |
| Yes | 0.85 (0.72–1.04) | 5.96 (−2.61 to 14.52) |
aPhysical therapy only, occupational therapy only, or both physical therapy and occupational therapy. CCW= Chronic Conditions Data Warehouse; CI = confidence interval; ICU = intensive care unit; Ref = reference group; tPA = tissue plasminogen activator.
bInterpretation of estimate among those patients who received any rehabilitation therapy. For example, patients treated in hospital with inpatient rehabilitation unit provides 8.65 more minutes of therapy (8.65; 95% CI = 4.13–13.18) compared with hospital without rehabilitation unit.
Among patients who received rehabilitation therapy, dual-eligible patients received 5 minutes less therapy (−5.07; 95% CI = −6.60 to −3.53) over the entire episode of care, compared with non–dual-eligible patients, and patients receiving tPA received 16 more minutes of therapy (16.57; 95% CI = 14.27–18.86). Patients with a feeding tube received 5 more minutes of therapy (5.71; 95% CI = 3.14–8.27). Each 1-day increase in length of stay was associated with getting 14 more minutes of therapy (14.20; 95% CI = 14.04–14.36).
Some of the hospital characteristics were associated with higher odds of receiving rehabilitation services. Patients treated in a rural hospital, treated in a hospital with a higher volume of patients with stroke, or treated in a hospital with an inpatient rehabilitation unit were more likely to have received rehabilitation. Among those who received any rehabilitation therapy, patients treated in a limited teaching hospital received 19 more minutes of therapy (19.74; 95% CI = 12.53–26.97), and those served by nonteaching hospitals received 20 more minutes of therapy (20.96; 95% CI = 14.55–27.38), compared with teaching hospitals. Similarly, patients treated in a hospital with an inpatient rehabilitation unit received 8 more minutes of therapy (8.65; 95% CI = 4.13–13.18). Results from the sensitivity analysis for patients receiving only physical therapy were similar to patients receiving rehabilitation services, except for patients treated in nonteaching hospitals, who had higher odds of receiving physical therapy only.
Figure 2 illustrates the variation in hospital-based rehabilitation services minutes provided across all acute care hospitals in the United States, after adjusting for patient and hospital characteristics. The horizontal lines show the adjusted mean of total rehabilitation minutes provided across all hospitals. Each vertical line represents the adjusted mean with 95% CI for each of the 2224 hospitals. Approximately 38% of hospitals provided total rehabilitation services minutes significantly below the national average, and 22.4% of hospitals provided total rehabilitation services minutes significantly above the national average.
Figure 2.
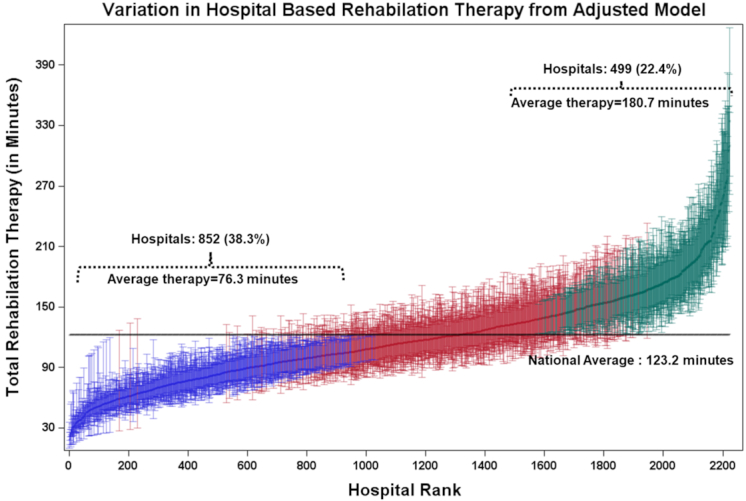
Hospital-level variation in total rehabilitation therapy minutes after adjusting for patients and hospital characteristics. Hospital rank for total rehabilitation amount given (in minutes) estimated by multilevel, multivariable random effect models adjusted for patient- and hospital-level characteristics. Horizontal lines present the unadjusted mean [SD] of total rehabilitation therapy minutes given (123.2 [99.0]). Each vertical line represents the adjusted mean with 95% confidence interval for each of the 2200 hospitals. Blue lines reflect the 852 (38.3%) hospitals where total rehabilitation therapy minutes provided (76.3 [19.2]) were lower than average rates. Green lines indicate the 499 (22.4%) hospitals where total rehabilitation therapy minutes (180.7 [36.1]) provided were above the average rates. Red lines reflect the 849 (38.5%) hospitals where total rehabilitation therapy minutes provided fell within a national average range.
Discussion
This study overcomes limitations of prior research by using a more precise method to measure the amount of rehabilitation services delivered in the acute care setting following an ischemic stroke. To our knowledge, this is the first study to quantify dosage and receipt of rehabilitation services in this manner. Our proposed method provided a robust estimation of minutes of rehabilitation service use over the episode of acute hospitalization, rather than relying on hospital charges. Recent research found that 21.6% of patients with new ischemic stroke in 2010 to 2013 did not receive any rehabilitation services, in a 20% random sample of Medicare beneficiaries.20 We found substantial variability in use of rehabilitation services across acute care hospitals, even after accounting for length of stay and other patient and hospital-level factors. Approximately 38% of hospitals provided significantly less (76.3 minutes during the whole length of stay) than the national average of rehabilitation services minutes (123 minutes), whereas 22.4% provided significantly more (180.7 minutes) than the national average. These findings are consistent with our hypothesis that there is considerable variation in the use of services due to the lack of clear practice guidelines on how much rehabilitation should be offered in the acute care setting.
In this study, we found that patient sociodemographic characteristics, condition severity (number of comorbidities, ICU, feeding tube insertion, tPA administration), as well as hospital-specific factors (teaching status, hospital with an inpatient rehabilitation unit) influenced provision of hospital-based rehabilitation services. We found that patients with risk factors such as ICU stay, number of prior hospitalizations, and feeding tube insertion were less likely to receive any therapy. These factors were proxy measures of stroke severity and suggest a missed opportunity for early mobilization/therapy to prevent deconditioning in persons with more severe conditions.
Our study found that persons dually enrolled in Medicare and Medicaid were less likely to receive any therapy and received fewer rehabilitation therapy minutes compared with persons enrolled in Medicare only. Medicare-Medicaid dually enrolled patients are known to have more complex clinical needs and have lower socioeconomic status compared with nonduals.33 Our finding of inequities by dual enrollment status underscores the need for standardized rehabilitation assessment in the acute setting. We also found that black patients were more likely to receive any therapy, a finding that is consistent with a recent research finding that black patients were more likely to receive rehabilitation therapy than white patients following stroke across all postacute settings.34
We found that older age and receiving tPA were associated with greater likelihood of getting any therapy and receipt of more rehabilitation minutes after stroke. One possible explanation is that older patients are complex to work with and have severe functional limitations and frailty, which require longer sessions of therapy services. In addition, tPAs are provided in primary and comprehensive stroke centers, which provide timely and complete care to patients with complex stroke and have trained rehabilitation expertise for taking care of patients with stroke.
We identified several hospital-level factors that were associated with use of rehabilitation services among those patients who received any rehabilitation therapy. For instance, patients treated in hospitals with a high volume of stroke admissions were more likely to receive any therapy. Numerous studies have demonstrated a volume-outcome (mortality) relationship in patients with stroke;22,35 however, few studies have examined the relationship between volume of stroke patients and receipt of rehabilitation services. We found that patients treated in limited-teaching and nonteaching hospitals received more rehabilitation minutes. Our study also found that patients treated in hospitals with inpatient rehabilitation units had a greater likelihood of getting any therapy and received more rehabilitation minutes. These hospitals are specialized in providing comprehensive postacute rehabilitation care and can use therapists from their rehabilitation facilities to meet their acute care needs. These therapists, in turn, can be proponents of providing upstream rehabilitation interventions to improve downstream outcomes. This type of influence could become more prevalent with value-based payment reforms such as bundled payments. In these reforms, acute hospitals are incentivized to have integrated postacute rehabilitation care, or to form some contractual agreements with postacute providers, so that they can establish or enhance coordination of care with postacute care providers by sharing medical records and sharing physical therapists and occupational therapists across settings. After the implementation of voluntary bundle payment models and the Hospital Readmissions Reduction Program, hospitals are cautiously increasing length of stays and prioritizing medical stabilization during acute hospitalization. Thus, we suspect that rehabilitation service provision during the acute stay can play a critical role in minimizing hospital-associated deconditioning, improving functional status, and could lead to better postacute discharge placement.
The variation that we observed could be attributable to lack of clear guidance on rehabilitation timing and dosage in the acute care setting. It could also be due to the current reimbursement structure for hospitals, which is based on Diagnosis Related Groups.36 Unlike postacute payment, which is influenced by therapy needs and use, the provision of rehabilitation services in acute settings does not alter the Diagnosis Related Groups payment to a hospital. Thus, cost savings are incurred by decreasing length of stay and services that are deemed to be optional. Although Diagnosis Related Groups-based payments can accurately project the medical/surgical and nursing services that were provided to patients during acute stays, they are largely determined by medical diagnoses, not function-related measures.36 The cost of services that target improvements in function and the need for rehabilitation services is not currently included in the Diagnosis Related Groups formula. Therefore, lack of additional payment for rehabilitation services might discourage provision of such services during acute stays, which can negatively affect the intended outcomes for patients.
We know little about variability in hospital-based rehabilitation services and the cause of this variability. By identifying patient- and hospital-level factors associated with receipt of therapy, and the amount of therapy received, our findings are a first step toward standardizing rehabilitation practice in acute hospitals in the United States. Findings from this study fill gaps in knowledge regarding rehabilitation service use and have the potential to improve standardization of care after stroke in the acute settings. Although many of the relationships that we observed were statistically significant, the actual differences in minutes of therapy received were small. We are conducting a separate analysis to quantify the impact of therapy quantity on patient outcomes. This information will help us to understand the clinical significance of these differences.
Our study has several limitations. First, we were unable to directly control for patient functional status or stroke severity in our analyses because these variables are not captured in the Medicare data associated with acute hospitalization claims. The missing information on functional status and stroke severity in claims data could have had a residual confounding effect on our study outcomes. Second, our study cohort was limited to older Medicare fee-for-service enrollees. Thus, the results are not generalizable to younger patients and those covered under Medicare Advantage plans. The possibility of coding and reporting errors might exist with claims data, which could bias estimation of our primary variables of interest. Our analysis and results are limited to the year 2010. Several value-based initiatives and quality measures were implemented after 2010, and these could have influenced rehabilitation practice pattern in recent years. Future studies are needed to examine how care patterns have changed since 2010. Despite these limitations, we believe that our proposed method using Medicare claims data in the SAF format provides researchers with a new approach for examining use of rehabilitation services by using revenue center codes for physical therapy/occupational therapy evaluation and therapy, and better estimating minutes of therapy. Currently, the relationship between therapy minutes and patient-level outcomes is not clear. The revenue center code approach will allow us, and others, to test the association between acute care rehabilitation services and clinical outcomes using postacute assessment data in future work.
In conclusion, this study investigated the use of rehabilitation services in the acute care setting and examined variations in service delivery for patients with ischemic stroke using a new method for quantifying the use of rehabilitation services in Medicare claims data. We observed significant variation in the use of rehabilitation services across hospitals. Our findings show that a significant amount of variation in the use of hospital-based rehabilitation services is attributable to patient- and hospital-level factors. These results suggest a timely opportunity to standardize rehabilitation service delivery in acute settings for patients with ischemic stroke. The next step for this line of research is to quantify the relationship between rehabilitation service receipt and variation and patients’ clinical outcomes to inform the development of guidelines for optimal dosage of rehabilitation services in the acute setting.
Supplementary Material
Author Contributions
Concept/idea/research design: A. Kumar, D. Adhikari, A. Karmarkar, J.K. Freburger, P. Gozalo, V. Mor, L. Resnik
Writing: A. Kumar, D. Adhikari, A. Karmarkar, J.K. Freburger, P. Gozalo, V. Mor, L. Resnik
Data collection: A. Kumar, D. Adhikari
Data analysis: A. Kumar, D. Adhikari, J.K. Freburger, L. Resnik, P. Gozalo
Project management: A. Kumar
Fund procurement: A. Kumar, V. Mor, P. Gozalo
Providing facilities/equipment: V. Mor
Consultation (including review of manuscript before submitting): A. Kumar, A. Karmarkar, P. Gozalo, V. Mor, L. Resnik
Funding
This study was funded by the Foundation for Physical Therapy's Center on Excellence in Health Services and Health Policy Research and Training (CoHSTAR) Grant, a National Center for Medical Rehabilitation Research Grant (K01-HD086290, R03-HD096372), and a National Institute on Aging Grant (P01 AG027296).
Disclosure and Presentations
The authors completed the ICJME Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest. Results from this study were presented as an abstract at the American Congress of Rehabilitation Medicine conference, October 23–26, 2017, Atlanta, Georgia.
References
- 1. Benjamin EJ, Blaha MJ, Chiuve SE et al.. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135:e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Krumholz HM, Normand SL, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999–2011. Circulation. 2014;130:966–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lichtman JH, Leifheit-Limson EC, Jones SB, Wang Y, Goldstein LB. Preventable readmissions within 30 days of ischemic stroke among Medicare beneficiaries. Stroke. 2013;44:3429–3435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Craig LE, Bernhardt J, Langhorne P, Wu O. Early mobilization after stroke: an example of an individual patient data meta-analysis of a complex intervention. Stroke. 2010;41:2632–2636. [DOI] [PubMed] [Google Scholar]
- 5. Cumming TB, Thrift AG, Collier JM et al.. Very early mobilization after stroke fast-tracks return to walking: further results from the phase II AVERT randomized controlled trial. Stroke. 2011;42:153–158. [DOI] [PubMed] [Google Scholar]
- 6. Pollock A, Baer G, Campbell P et al.. Physical rehabilitation approaches for the recovery of function and mobility following stroke. Cochrane Database Syst Rev. 2014;(4):CD001920.doi:10.1002/14651858.CD001920.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Biernaskie J, Chernenko G, Corbett D. Efficacy of rehabilitative experience declines with time after focal ischemic brain injury. J Neurosci. 2004;24:1245–1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Diserens K, Moreira T, Hirt L et al.. Early mobilization out of bed after ischaemic stroke reduces severe complications but not cerebral blood flow: a randomized controlled pilot trial. Clin Rehabil. 2012;26:451–459. [DOI] [PubMed] [Google Scholar]
- 9. Cumming TB, Collier J, Thrift AG, Bernhardt J. The effect of very early mobilisation after stroke on psychological well-being. J Rehabil Med. 2008;40:609–614. [DOI] [PubMed] [Google Scholar]
- 10. Falvey JR, Burke RE, Malone D, Ridgeway KJ, McManus BM, Stevens-Lapsley JE. Role of physical therapists in reducing hospital readmissions: optimizing outcomes for older adults during care transitions from hospital to community. Phys Ther. 2016;96:1125–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Matmari L, Uyeno J, Heck CS. Physiotherapists' perceptions of and experiences with the discharge planning process in acute-care general internal medicine units in Ontario. Physiother Can. 2014;66:254–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Winstein CJ, Stein J, Arena R et al.. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47:e98–e169. [DOI] [PubMed] [Google Scholar]
- 13. Jette AM. The importance of dose of a rehabilitation intervention. Phys Ther. 2017;97:1043. [DOI] [PubMed] [Google Scholar]
- 14. Centers for Medicare & Medicaid Services. Bundled Payments for Care Improvement Advanced (BPCI Advanced) Initiative. https://innovation.cms.gov/initiatives/bpci-advanced/. Updated December 11, 2018 Accessed October 31, 2018. [Google Scholar]
- 15. Skolarus LE, Meurer WJ, Shanmugasundaram K, Adelman EE, Scott PA, Burke JF. Marked regional variation in acute stroke treatment among Medicare beneficiaries. Stroke. 2015;46:1890–1896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schwamm LH, Reeves MJ, Pan W et al.. Race/ethnicity, quality of care, and outcomes in ischemic stroke. Circulation. 2010;121:1492–1501. [DOI] [PubMed] [Google Scholar]
- 17. Springer MV, Labovitz DL, Hochheiser EC. Race-ethnic disparities in hospital arrival time after ischemic stroke. Ethn Dis. 2017;27:125–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Andrews AW, Li D, Freburger JK. Association of rehabilitation intensity for stroke and risk of hospital readmission. Phys Ther. 2015;95:1660–1667. [DOI] [PubMed] [Google Scholar]
- 19. Freburger JK, Heatwole Shank K, Knauer SR, Montmeny RM. Delivery of physical therapy in the acute care setting: a population-based study. Phys Ther. 2012;92:251–265. [DOI] [PubMed] [Google Scholar]
- 20. Freburger JK, Li D, Johnson AM, Fraher EP. Physical and occupational therapy from the acute to community setting after stroke: predictors of use, continuity of care, and timeliness of care. Arch Phys Med Rehabil. 2018;99:1077–1089. [DOI] [PubMed] [Google Scholar]
- 21. Centers for Medicare & Medicaid Services. Chronic condition data warehouse. 1999-2016; https://www.ccwdata.org/web/guest/condition-categories. Accessed October 31, 2018. [Google Scholar]
- 22. Saposnik G, Baibergenova A, O'Donnell M, Hill MD, Kapral MK, Hachinski V. Hospital volume and stroke outcome: does it matter? Neurology. 2007;69:1142–1151. [DOI] [PubMed] [Google Scholar]
- 23. Joynt KE, Orav EJ, Jha AK. The association between hospital volume and processes, outcomes, and costs of care for congestive heart failure. Ann Intern Med. 2011;154:94–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the hospital readmissions reduction program. JAMA. 2013;309:342–343. [DOI] [PubMed] [Google Scholar]
- 25. Vartak S, Ward MM, Vaughn TE. Do postoperative complications vary by hospital teaching status? Med Care. 2008;46:25–32. [DOI] [PubMed] [Google Scholar]
- 26. Graham JE, Prvu Bettger J, Middleton A, Spratt H, Sharma G, Ottenbacher KJ. Effects of acute-postacute continuity on community discharge and 30-day rehospitalization following inpatient rehabilitation. Health Serv Res. 2017;52:1631–1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Burke LG, Frakt AB, Khullar D, Orav EJ, Jha AK. Association between teaching status and mortality in US hospitals. JAMA. 2017;317:2105–2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bogasky S, Gage B, Morley M, Spain P, Ingber M. Examining post-acute care relationships in an integrated hospital system. URL:https://aspe.hhs.gov/sites/default/files/pdf/75761/report.pdf. Published February 1, 2009. Accessed October 31, 2018. [Google Scholar]
- 29. Sung SF, Chen SC, Hsieh CY, Li CY, Lai EC, Hu YH. A comparison of stroke severity proxy measures for claims data research: a population-based cohort study. Pharmacoepidemiol Drug Saf. 2016;25:438–443. [DOI] [PubMed] [Google Scholar]
- 30. Sung S-F, Hsieh C-Y, Kao Yang Y-H et al.. Developing a stroke severity index based on administrative data was feasible using data mining techniques. J Clin Epidemiol. 2015;68:1292–1300. [DOI] [PubMed] [Google Scholar]
- 31. Kumar A, Karmarkar AM, Graham JE et al.. Comorbidity indices versus function as potential predictors of 30-day readmission in older patients following postacute rehabilitation. J Gerontol A Bio Sci Med Sci. 2017;72:223–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kumar A, Graham JE, Resnik L et al.. Examining the association between comorbidity indexes and functional status in hospitalized Medicare fee-for-service beneficiaries. Phys Ther. 2016;96:232–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jacobson G,T, Damico A. Medicare's role for dual eligible beneficiaries [internet. Menlo Park(CA):Kaiser Family Foundation;2012 April (Issue Brief No.8138-02 Available from https://kaiserfamilyfoundation.files.wordpress.com/2013/01/8138-02.pdf.Published April 2012. Accessed October 31, 2018. [Google Scholar]
- 34. Skolarus LE, Feng C, Burke JF. No racial difference in rehabilitation therapy across all post-acute care settings in the year following a stroke. Stroke. 2017;48:3329–3335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O'Brien CR, Rubenfeld GD. Hospital volume and the outcomes of mechanical ventilation. N Eng J Med. 2006;355:41–50. [DOI] [PubMed] [Google Scholar]
- 36. Centers for Medicare & Medicaid Services. Medicare program; hospital inpatient prospective payment systems for acute care hospitals and the long term care hospital prospective payment system and policy changes and fiscal year 2018 rates. Fed Regist. 2017;82(155):37990–38589. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


