Abstract
Background
Tumor hypoxia is associated with metastasis and resistance to chemotherapy and radiotherapy. Genes involved in oxygen-sensing are clinically relevant and have significant implications for prognosis. In this study, we examined the pan-cancer prognostic significance of oxygen-sensing genes from the 2-oxoglutarate-dependent oxygenase family.
Methods
A multi-cohort, retrospective study of transcriptional profiles of 20,752 samples of 25 types of cancer was performed to identify pan-cancer prognostic signatures of 2-oxoglutarate-dependent oxygenase gene family (a family of oxygen-dependent enzymes consisting of 61 genes). We defined minimal prognostic gene sets using three independent pancreatic cancer cohorts (n = 681). We identified two signatures, each consisting of 5 genes. The ability of the signatures in predicting survival was tested using Cox regression and receiver operating characteristic (ROC) curve analyses.
Results
Signature 1 (KDM8, KDM6B, P4HTM, ALKBH4, ALKBH7) and signature 2 (KDM3A, P4HA1, ASPH, PLOD1, PLOD2) were associated with good and poor prognosis. Signature 1 was prognostic in 8 cohorts representing 6 cancer types (n = 2627): bladder urothelial carcinoma (P = 0.039), renal papillary cell carcinoma (P = 0.013), liver cancer (P = 0.033 and P = 0.025), lung adenocarcinoma (P = 0.014), pancreatic adenocarcinoma (P < 0.001 and P = 0.040), and uterine corpus endometrial carcinoma (P < 0.001). Signature 2 was prognostic in 12 cohorts representing 9 cancer types (n = 4134): bladder urothelial carcinoma (P = 0.039), cervical squamous cell carcinoma and endocervical adenocarcinoma (P = 0.035), head and neck squamous cell carcinoma (P = 0.038), renal clear cell carcinoma (P = 0.012), renal papillary cell carcinoma (P = 0.002), liver cancer (P < 0.001, P < 0.001), lung adenocarcinoma (P = 0.011), pancreatic adenocarcinoma (P = 0.002, P = 0.018, P < 0.001), and gastric adenocarcinoma (P = 0.004). Multivariate Cox regression confirmed independent clinical relevance of the signatures in these cancers. ROC curve analyses confirmed superior performance of the signatures to current tumor staging benchmarks. KDM8 was a potential tumor suppressor down-regulated in liver and pancreatic cancers and an independent prognostic factor. KDM8 expression was negatively correlated with that of cell cycle regulators. Low KDM8 expression in tumors was associated with loss of cell adhesion phenotype through HNF4A signaling.
Conclusion
Two pan-cancer prognostic signatures of oxygen-sensing genes were identified. These genes can be used for risk stratification in ten diverse cancer types to reveal aggressive tumor subtypes.
Electronic supplementary material
The online version of this article (10.1186/s40880-019-0369-5) contains supplementary material, which is available to authorized users.
Keywords: Oxygen-sensing gene, 2-Oxoglutarate-dependent oxygenase, Pan-cancer, Prognosis, Hypoxia, KDM8, HNF4A
Background
Solid tumors demand a considerable amount of oxygen due to their unique vasculature systems [1]. Rapid neoplastic cell proliferation and overexpression of angiogenic factors leading to the formation of disorganized blood vessels result in insufficient oxygen supply to tumor cells [2, 3]. Hence, there is a requirement for tumors to evolve systems that detect changes in oxygen homeostasis [4]. The discovery of hypoxia-inducible factor (HIF), a key oxygen-sensing gene, represents a quantum leap forward in tumor biology [5, 6]. Its discovery has led to the development of drugs used to treat cancer [7, 8].
In addition to HIF, 2-oxoglutarate (2OG)-dependent oxygenases represent another family of oxygen-sensing proteins. As suggested by the name, this group of enzymes has an absolute requirement for molecular oxygen. They catalyze a range of oxidative modifications, and their activities are affected by nutrient and oxygen availability [9], both of which are altered within the tumor microenvironment. Several members from this gene family have been implicated in cancer. For example, 10–11 translocation 2 is frequently found to be mutated in leukemia [10] and other solid malignancies [11]. In addition, the epigenetic alterations and inactivating mutations of the Jumonji-C domain-containing lysine demethylase (KDM) family are frequently observed in multiple cancers such as multiple myeloma, esophageal squamous cell carcinoma, renal cell carcinoma, breast cancer, colorectal cancer, and glioblastoma [12, 13].
We hypothesized that detecting the expression of 2OG-dependent oxygenases could help predict prognosis in solid malignancies that are characteristically oxygen-deprived. Additionally, we hypothesized this would be applicable to different types of cancer as they share a uniform need to overcome hypoxia for survival. Starting from an initial set of 61 genes encoding 2OG-dependent oxygenases, we developed two prognostic gene signatures, each consisting of a minimal 5 genes that could facilitate risk stratification and predict overall survival (OS) in cancer patients, and further confirmed their prognostic performance through a multi-cohort pan-cancer validation process.
Methods
Datasets and processing
Datasets used in this study consist of the expression profiles of 20,752 tumor samples and 881 non-tumor samples that were obtained from The Cancer Genome Atlas (TCGA) [14], International Cancer Genome Consortium (ICGC) [15], and Gene Expression Omnibus (GEO), representing 25 cancer types. The cohort descriptions are listed in Additional file 1. TCGA datasets were downloaded from Broad Institute GDAC Firehose (https://gdac.broadinstitute.org/), which included gene expression profiles of 19,781 tumor samples and 881 non-tumor samples. ICGC datasets were downloaded from the ICGC data portal (https://icgc.org/), which included 729 tumor samples. A GEO dataset was downloaded from the GEO data portal (https://www.ncbi.nlm.nih.gov/geo/), which included 242 tumor samples. TCGA transcriptome datasets were represented as the normalized gene expression RSEM (RNA-seq by expectation maximization) values [16] obtained from GDAC Firehose. ICGC transcriptome datasets were represented as normalized read counts. The GEO dataset was generated by Affymetrix microarray profiling using the Affymetrix Human Genome U133A 2.0 Array [17]. All expression profiles were converted to log2(x + 1) scale.
KDM8 differential expression analysis
TCGA liver cancer cohort (LIHC; Additional file 1) was used in KDM8 differential expression analysis. A total of 371 cancer patients in this cohort were median dichotomized into low and high KDM8 expression groups. To determine differentially expressed genes between the two groups, the Bayes method and linear model were implemented using the R package limma (version 3.8) [18]. P values were adjusted using the false discovery rate controlling procedure of Benjamini–Hochberg. Genes with log2 fold change of > 1 or < − 1 and adjusted P values < 0.05 were considered significant.
Gene signatures and risk scores
Expression scores for gene signatures 1 and 2 were calculated for each patient by taking the average log2 expression values of signature genes. Signature 1 genes: KDM8, KDM6B, P4HTM, ALKBH4, and ALKBH7. Signature 2 genes: KDM3A, P4HA1, ASPH, PLOD1, and PLOD2. Tumor hypoxia scores were calculated as the average log2 expression values of 52 hypoxia signature genes [19]: ESRP1, CORO1C, SLC2A1, UTP11, CDKN3, TUBA1B, ENO1, NDRG1, PGAM1, CHCHD2, SLC25A32, SHCBP1, KIF20A, PGK1, BNIP3, ANLN, ACOT7, TUBB6, MAP7D1, YKT6, PSRC1, GPI, PGAM4, GAPDH, MRPL13, SEC61G, VEGFA, MIF, TPI1, MAD2L2, HK2, AK4, CA9, SLC16A1, KIF4A, PSMA7, LDHA, MRPS17, PNP, TUBA1C, HILPDA, LRRC42, TUBA1A, MRGBP, MRPL15, CTSV, ADM, DDIT4, PFKP, P4HA1, MCTS1, and ANKRD37. The risk score for each patient was calculated by taking the sum of Cox regression coefficient for each signature gene multiplied with its corresponding expression value. Nonparametric Spearman’s rank correlation analysis was employed to assess the relationship of expression scores and risk scores with tumor hypoxia (hypoxia score).
Survival analyses
Cox proportional hazards regression analysis was employed to investigate the association between patient survival and risk factors, e.g., signature 1 or signature 2 score, tumor stage, and other clinical variables. Univariate analyses were performed to determine the influence of individual risk factors on OS. Multivariate analyses were performed by including risk factors that were identified in univariate analyses (P < 0.05). Hazard ratios (HR) were determined from Cox models. Cox regression analyses were performed using the R survival (version 2.43-3) [20] and survminer (version 0.4.3) [21] packages. Proportional hazards assumption was supported by a non-significant relationship between scaled Schoenfeld residuals and time using the R survival package. In addition, Kaplan–Meier and log-rank tests were used in univariate analyses of the gene signatures in relation to patient survival and were performed using the survival and survminer packages. Patients were median-dichotomized into low and high-score groups based on median expression scores of signature genes. Differences between high and low-score groups were tested using the log-rank test implemented with the survival package.
Time-dependent receiver operating characteristic (ROC) curve analysis was used to assess the predictive performance of both signatures 1 and 2 in comparison with standard tumor staging parameters. The R survcomp (version 3.8) package [22] was employed to compute time-dependent ROC curves [22].
Biological enrichment analysis
Analysis of biological pathway enrichment on the 745 differentially expressed genes between KDM8-low and -high groups was conducted using GeneCodis against the Kyoto Encyclopedia of Genes and Genomes (KEGG) (https://www.genome.jp/kegg/) and Gene Ontology (GO) databases (http://geneontology.org/) [23]. The Enrichr tool was used to identify transcription factors from the ENCODE database (https://www.encodeproject.org/) as potential regulators of these 745 genes [24, 25].
HNF4A loss-of-function analysis
A total of 148 genes were identified as HNF4A targets in the HepG2 hepatoma cell line determined using the Enrichr tool [24, 25]. Differential expression analysis between HNF4A wild-type and null mice livers (GSE3126) performed using the GEO2R tool [26] identified 110 differentially expressed genes from the initial 745-gene set identified previously (Fig. 5h). Of these 110 genes, 45 were identified as direct HNF4A targets and were down-regulated in the HNF4A-null mice (Fig. 5i).
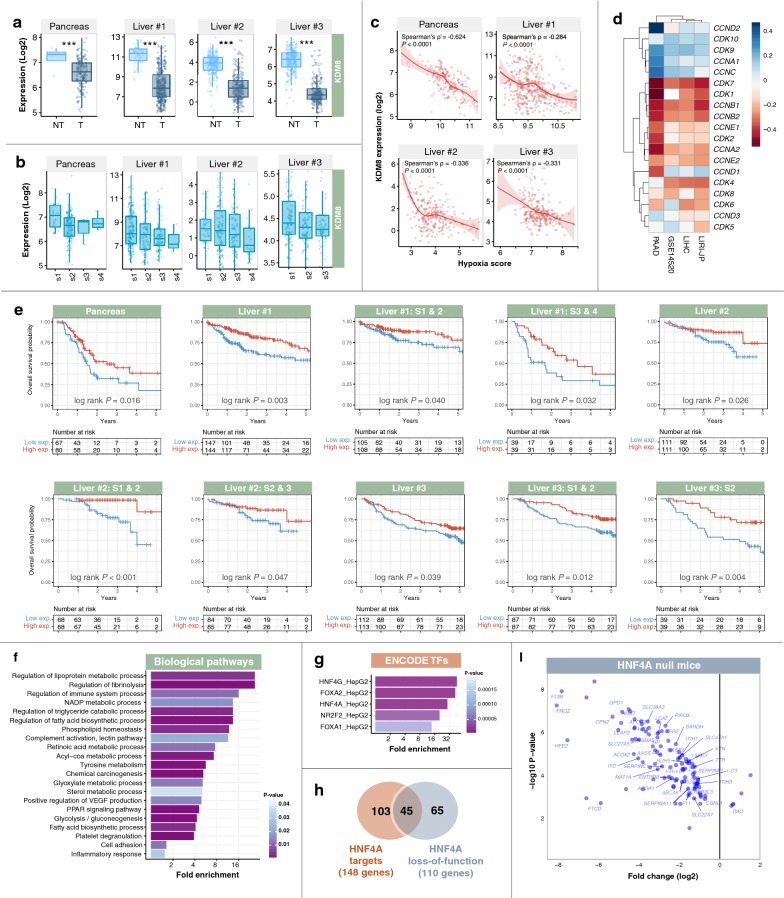
Fig. 5.
Putative tumor suppressive functions of KDM8 occur through processes related to cell cycle regulation and cell adhesion. a Expression of KDM8 was significantly lower in tumor (T) samples than in non-tumor (NT) samples in liver and pancreatic cancer cohorts. Mann–Whitney–Wilcoxon tests were used to compare T and NT samples. Asterisks represent significant P values: *** < 0.0001. b Expression levels of KDM8 decreased with disease progression and malignant grade in liver and pancreatic cancer cohorts. c Significant negative correlation between patients’ KDM8 expression and tumor hypoxia (hypoxia score) in liver and pancreatic cancer cohorts. d Correlation between KDM8 expression and canonical cell cycle regulators in patients with liver or pancreatic cancers. A majority of genes involved in cell-cycle regulation are negatively correlated with KDM8 expression. Liver #1 = LIHC cohort; Liver #2 = LIRI-JP cohort; and Liver #3 = GSE14520 cohort (Additional file 1). e Kaplan–Meier analysis of patients stratified by KDM8 expression. Patients were median-dichotomized into low- and high-expression groups. Patients with low KDM8 expression had significantly shorter overall survival. This was consistent in patients analyzed as a full cohort or sub-categorized according to TNM stage. Liver #1 = LIHC cohort; Liver #2 = LIRI-JP cohort; and Liver #3 = GSE14520 cohort (Additional file 1). f Patients were median-stratified according to KDM8 expression. Differential expression analysis between KDM8-high- and -low groups in liver cancer cohorts revealed 745 differentially expressed genes (DEGs; fold-change > 2 or < − 2). Enrichment of biological pathways associated with DEGs, which include processes related to cell adhesion, inflammation, metabolism, and signal transduction pathways in cancer. g Enrichment of transcription factors (TFs) from the ENCODE database that are potential regulators of KDM8 DEGs. These TFs were predicted to bind near KDM8 DEGs. h Venn diagram depicts the overlap between HNF4A targets (as identified by ENCODE chromatin-immunoprecipitation sequencing dataset) and genes affected by HNF4A loss-of-function (as identified in HNF4A-null mice). Of the 745 DEGs, 148 were identified as direct HNF4A targets, and 110 genes were affected by HNF4A loss-of-function. In the Venn intersection, 45 genes were both HNF4A targets and altered in HNF4A-null mice. i Scatter plot depicts expression patterns of 110 genes affected by HNF4A loss-of-function. Gene names of the 45 HNF4A targets are annotated on the plot. A majority of KDM8-associated genes were down-regulated in the HNF4A-null mice
Somatic mutation identification
Level 3 mutation datasets were downloaded from GDAC (https://gdac.broadinstitute.org/). Kaplan–Meier analysis and log-rank tests were employed to determine the association of somatic mutations, in combination with signature 1 or 2, on OS.
All graphs were generated using the ggplot2 package in R (version 3.1.0) [27].
Statistical analysis
Comparisons of gene expression levels between tumor and non-tumor samples or between high- and low-score groups were performed using the non-parametric Mann–Whitney–Wilcoxon test implemented in R (version 3.3.3) [28].
Results
Multi-cohort analyses revealed two prognostic 2OG-dependent oxygenases signatures
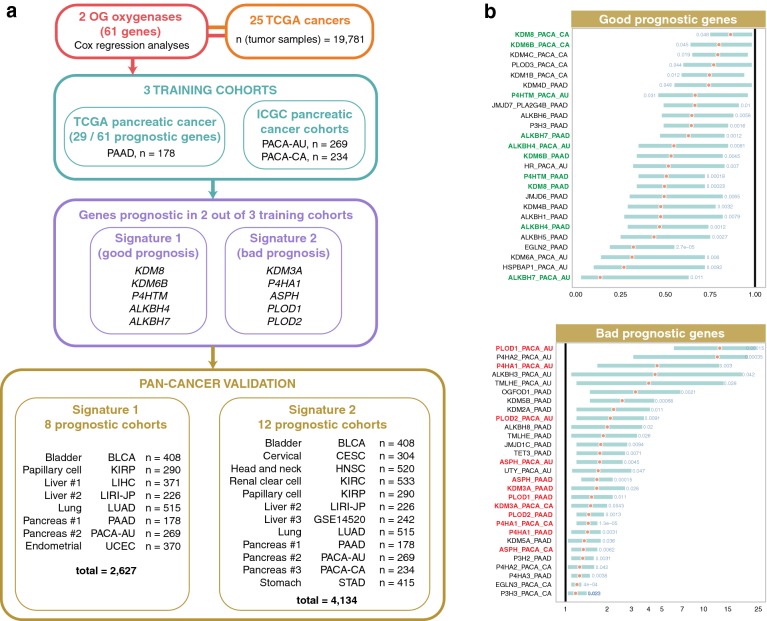
We analyzed the prognostic significance of 61 2OG-dependent oxygenase genes (Additional file 2) in 19,781 tumor samples from multiple TCGA cohorts [14] covering 25 cancer types (Additional file 1). Prognostic genes were defined as those whose expression levels were significantly correlated with patients’ OS. Pancreatic cancer is difficult to treat. Since the highest number of prognostic genes (29 genes) was observed in the pancreatic cancer cohort (PAAD; 178 samples), two additional pancreatic cancer cohorts from ICGC (PACA-AU and PACA-CA; 269 and 234 samples) were used in combination as training cohorts (Fig. 1a). We defined two gene signatures (signatures 1 and 2) as favorable and unfavorable prognostic factors by taking into consideration genes that were significant in univariate Cox regression analyses in 2 out of 3 pancreatic cancer cohorts (Fig. 1a, b). Signature 1 included KDM8, KDM6B, P4HTM, ALKBH4, and ALKBH7. Likewise, KDM3A, P4HA1, ASPH, PLOD1, and PLOD2 made up signature 2 (Fig. 1a).
Fig. 1.
Schematic diagram of the study design and development of signatures derived from 61 2-oxoglutarate-dependent oxygenase genes. a Three pancreatic adenocarcinoma cohorts were used to define both signatures 1 and 2. Genes found to be prognostic in univariate Cox regression analysis in 2 out of 3 pancreatic adenocarcinoma cohorts were included in signatures 1 and 2. Signature 1 is a marker of good prognosis and consists of 5 genes (KDM8, KDM6B, P4HTM, ALKBH4, and ALKBH7). Signature 2 is a marker of adverse prognosis and consists of 5 genes (KDM3A, P4HA1, ASPH, PLOD1, and PLOD2). Prognosis of both signatures was further confirmed in 10 cancer types using Kaplan–Meier, Cox regression, and receiver operating characteristic analyses. b Forest plots of prognostic genes found to be significant by univariate Cox regression analysis in pancreatic adenocarcinoma cohorts abbreviated as PAAD, PACA-AU, and PACA-CA. Genes were separated into two groups, good and bad prognostic genes. Hazard ratios were denoted as red circles, and turquoise bars represent 95% confidence interval. Significant Wald test P values are indicated in blue. Y-axes represent gene symbols followed by cohort abbreviations. Signature 1 genes are marked in green. Signature 2 genes are marked in red. Full description of cancers is listed in Additional file 1. 2OG, 2-oxoglutarate; TCGA, The Cancer Genome Atlas; ICGC, International Cancer Genome Consortium
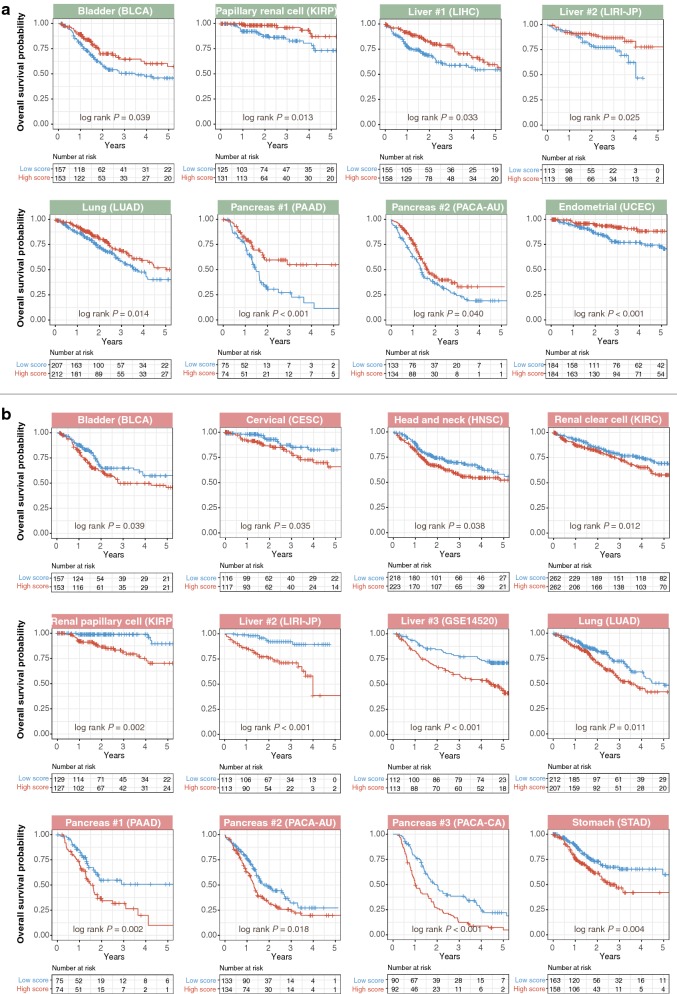
Patients were median-dichotomized based on mean expression scores of signatures 1 and 2 genes. Cox regression analyses revealed that patients with high expression of signature 1 genes had significantly better OS in 6 cancer types (Additional file 3): bladder urothelial carcinoma (BLCA: HR, 0.662; 95% confidence interval [CI] 0.450–0.974; P = 0.036), renal papillary cell carcinoma (KIRP: HR, 0.370; 95% CI 0.157–0.871; P = 0.023), liver cancer (LIHC: HR, 0.656; 95% CI 0.424–0.915; P = 0.048 and LIRI-JP: HR, 0.490; 95% CI 0.259–0.938; P = 0.031), lung adenocarcinoma (LUAD: HR, 0.625; 95% CI 0.443–0.879; P = 0.007), pancreatic adenocarcinoma (PAAD: HR, 0.454; 95% CI 0.278–0.741; P = 0.002), and uterine corpus endometrial carcinoma (UCEC: HR, 0.401; 95% CI 0.229–0.702; P = 0.002). Similar results were obtained using log-rank tests, consistent with the fact that signature 1 was a marker of good prognosis (Fig. 2a). In contrast, patients with high expression of signature 2 genes had significantly worse prognosis in 9 cancers: bladder urothelial carcinoma (BLCA: HR, 1.459; 95% CI 1.096–2.137; P = 0.042), cervical squamous cell carcinoma and endocervical adenocarcinoma (CESC: HR, 1.972; 95% CI 1.003–3.877; P = 0.045), head and neck squamous cell carcinoma (HNSC: HR, 1.479; 95% CI 1.056–2.072; P = 0.023), renal clear cell carcinoma (KIRC: HR, 1.483; 95% CI 1.096–2.007; P = 0.011), renal papillary cell carcinoma (KIRP: HR, 3.862; 95% CI 1.565–9.526; P = 0.003), liver cancer (LIRI-JP: HR, 5.271; 95% CI 2.429–11.440; P < 0.001 and GSE14520: HR, 2.285; 95% CI 1.458–3.580; P < 0.001), lung adenocarcinoma (LUAD: HR, 1.562; 95% CI 1.116–2.188; P = 0.009), pancreatic adenocarcinoma (PAAD: HR, 1.969; 95% CI 1.217–3.186; P = 0.006), and gastric adenocarcinoma (STAD: HR, 1.725; 95% CI 1.142–2.605; P = 0.009) (Fig. 2b and Additional file 3).
Fig. 2.
Kaplan–Meier analyses confirming that gene signatures were associated with patients’ overall survival. a Validation of signature 1 (green panels) across multiple cancer types. Kaplan–Meier plots of overall survival in cancer patients stratified based on signature 1 mean expression scores. Patients were median-dichotomized into high- and low-score groups. Signature 1 is a marker of good prognosis, and hence patients with high signature 1 scores had high survival rates. b Validation of signature 2 (red panels) across multiple cancer types. Kaplan–Meier plots of overall survival in cancer patients stratified based on signature 2 mean expression scores. Patients were median-dichotomized into high- and low-score groups. Signature 2 is a marker of adverse prognosis, and hence patients with high signature 2 scores had low survival rates. P values were calculated from the log-rank test. Pancreas #1 = PAAD cohort; Pancreas #2 = PACA-AU cohort; Pancreas #3 = PACA-CA cohort; Liver #1 = LIHC cohort; Liver #2 = LIRI-JP cohort; and Liver #3 = GSE14520 cohort (Additional file 1)
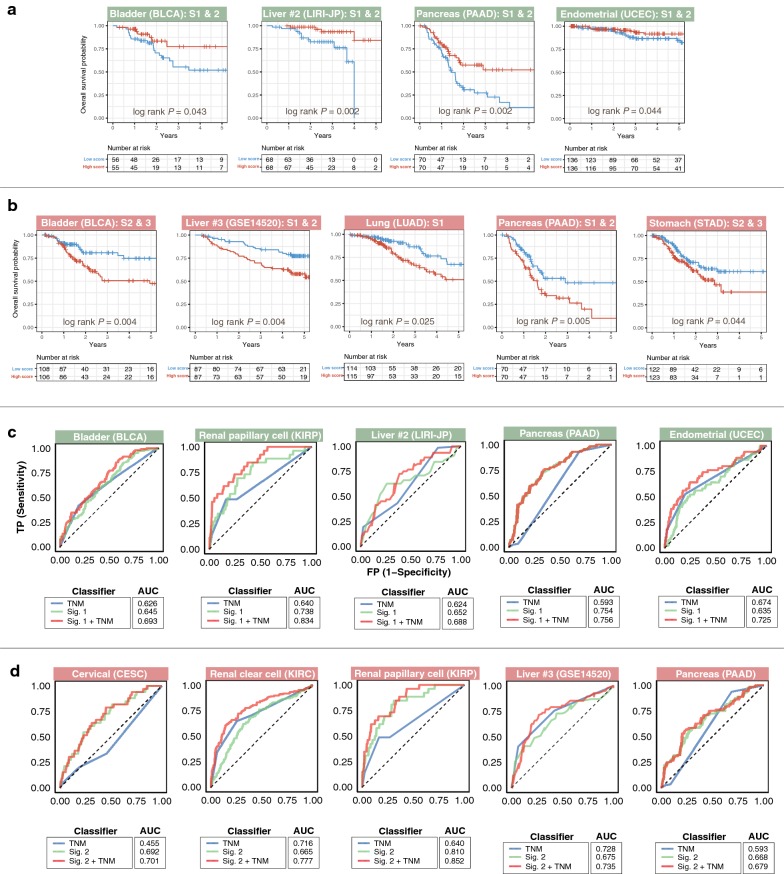
Cross-platform subgroup and multivariate analyses confirmed the validity of signatures 1 and 2 as independent prognostic factors
To assess the independence of signatures 1 and 2 over current tumor staging systems, we performed subgroup analyses of their prognostic effects in patients with early (stages I and/or II), intermediate (stages II and/or III), and late (stages III and/or VI) cancer stages. Kaplan–Meier analyses revealed that signature 1 successfully identified high-risk (low-expression score) and low-risk (high-expression score) patients with early (bladder urothelial carcinoma, liver cancer, lung adenocarcinoma, pancreatic adenocarcinoma, and uterine corpus endometrial carcinoma), intermediate (liver cancer and uterine corpus endometrial carcinoma), and late (renal papillary cell carcinoma) disease stages (Fig. 3a and Additional file 4A). Signature 2 was also independent of disease stage as it successfully predicted survival in early (liver cancer, lung adenocarcinoma, and pancreatic adenocarcinoma), intermediate (bladder urothelial carcinoma, liver cancer, and gastric adenocarcinoma), and late (bladder urothelial carcinoma, head and neck squamous cell carcinoma, renal papillary cell carcinoma, liver cancer, and gastric adenocarcinoma) stages (Fig. 3b and Additional file 4B).
Fig. 3.
Tumor subgroup analyses and evaluation of prognosis predictive performance of gene signatures across different malignant grades. Kaplan–Meier plots show independence of a signature 1 (green panels) and b signature 2 (red panels) over the current TNM staging system in predicting prognosis in different cancer cohorts. Patients were sub-grouped according to TNM stages and further stratified using either signature 1 or signature 2 scores. Both signatures successfully identified high-risk patients in different TNM stages. P values were calculated from the log-rank test. Analysis of specificity and sensitivity of c signature 1 (green panels) and d signature 2 (red panels) in predicting prognosis in different cancer cohorts using receiver operating characteristic (ROC) curves. Plots depict comparison of ROC curves of signature 1 or 2 and clinical TNM staging. Both signatures demonstrate incremental values over the current TNM staging system. AUC: area under the curve. TNM: tumor, node, metastasis staging. Liver #2 = LIRI-JP cohort and Liver #3 = GSE14520 cohort (Additional file 1). Representative plots are depicted in this figure. Additional plots are available in Additional file 4
ROC analyses were employed to determine the predictive performance (sensitivity and specificity) of signatures 1 and 2 on 5-year OS. Signature 1 performed the best, as measured by area under the curve (AUC), in pancreatic adenocarcinoma (PAAD: AUC = 0.754) followed by renal papillary cell carcinoma (KIRP: AUC = 0.738), liver cancer (LIRI-JP: AUC = 0.652 and LIHC: AUC = 0.613), bladder urothelial carcinoma (BLCA: AUC = 0.645), uterine corpus endometrial carcinoma (UCEC: AUC = 0.635), and lung adenocarcinoma (LUAD: AUC = 0.625) (Fig. 3c and Additional file 4C). Signature 2 performance in renal papillary cell carcinoma (KIRP: AUC = 0.810) was the best, followed by cervical squamous cell carcinoma and endocervical adenocarcinoma (CESC: AUC = 0.692), liver cancer (GSE14520: AUC = 0.675 and LIRI-JP: AUC = 0.625), pancreatic adenocarcinoma (PAAD: AUC = 0.668), renal clear cell carcinoma (KIRC: AUC = 0.665), head and neck squamous cell carcinoma (HNSC: AUC = 0.632), lung adenocarcinoma (LUAD: AUC = 0.623), gastric adenocarcinoma (STAD: AUC = 0.618), and bladder urothelial carcinoma (BLCA: AUC = 0.605) (Fig. 3d and Additional file 4D). Performance of both signatures 1 and 2 was superior to current tumor-node-metastasis (TNM) staging except for the following: signature 1 in liver cancer, lung adenocarcinoma, and uterine corpus endometrial carcinoma and signature 2 in bladder urothelial carcinoma, renal clear cell carcinoma, liver cancer, and lung adenocarcinoma (Fig. 3c, d and Additional file 4C, D). Remarkably, when used in combination with TNM staging, both signatures consistently outperformed each of the individual classifiers, reinforcing their incremental prognostic values (Fig. 3c, d and Additional file 4C, D). Significantly, while TNM staging could not predict outcome in cervical squamous cell carcinoma and endocervical adenocarcinoma patients (CESC: AUC = 0.455), signature 2 sufficiently served as an adverse prognostic factor (CESC: AUC = 0.692) (Fig. 3d).
Univariate Cox regression analyses revealed that TNM stage was associated with patient survival in different cancer types except for cervical squamous cell carcinoma and endocervical adenocarcinoma, and pancreatic adenocarcinoma (Additional file 3). This was expected given the low AUC values for TNM stage in both pancreatic adenocarcinoma (PAAD: AUC = 0.593) and cervical squamous cell carcinoma and endocervical adenocarcinoma (CESC: AUC = 0.455), suggesting that current TNM staging system for these cancers are inadequate (Fig. 3c, d). Multivariate Cox regression analyses after adjusting for TNM stage showed that signatures 1 and 2 remained significantly associated with survival (Additional file 3). For 2 liver cancer cohorts, we considered additional clinicopathological features. The GSE14520 cohort consisted of Chinese patients with hepatitis B-associated hepatocellular carcinoma [17], whereas LIRI-JP was a Japanese-based cohort of mixed etiology [29]. Tumor size, cirrhosis, TNM stage, Barcelona Clinic Liver Cancer (BCLC) stage, and alpha-fetoprotein (AFP) levels were all significantly associated with survival in the GSE14520 cohort; tumor size could also predict survival in the LIRI-JP cohort (Additional file 3). When these significant covariates along with signatures 1 or 2 were included in multivariate Cox models, the signatures remained significant risk factors: signature 1 (LIRI-JP: HR, 0.541; 95% CI 0.283–0.904; P = 0.043) and signature 2 (LIRI-JP: HR, 4.539, 95% CI 2.055–10.029; P < 0.001 and GSE14520: HR, 2.012; 95% CI 1.267–3.195; P = 0.003) (Additional file 3). These results highlight the potentially superior prognostic ability of our signatures: signatures 1 and 2 identified high- and low-risk patients in 8 and 12 independent cohorts covering 10 cancer types (Fig. 1a).
Significance of somatic mutations in risk-stratified patients
Patients were risk stratified into low- and high-risk groups using signatures 1 and 2. For signature 1, high-risk patients had significantly lower expression levels of good prognosis genes ALKBH4, ALKBH7, KDM8, KDM6B, and P4HTM (Additional file 5A). In contrast, high-risk patients as stratified by signature 2 had significantly higher expression levels of adverse prognosis genes ASPH, KDM3A, P4HA1, PLOD1, and PLOD2 (Additional file 5B). To ascertain the relationship between tumor hypoxia and expression of signature genes, hypoxia scores were computed for each patient as mean expression values (log2) of 52 hypoxia signature genes [19]. Signature 1 expression scores in patients negatively correlated with hypoxia score (Additional file 6A). Since tumor hypoxia is associated with distant metastasis, recurrence, and reduced therapeutic response [30], high expression of signature 1 genes (low hypoxia score) was correlated with less advanced disease states consistent with it being a marker of good prognosis (Additional file 6A).
Conversely, signature 2 scores positively correlated with tumor hypoxia and hence poor survival outcomes (Additional file 7A). We anticipated that patients’ individual risks of death, as determined from signatures 1 and 2, would positively correlate with tumor hypoxia. Indeed, the risk score for each patient, as calculated by taking the sum of Cox regression coefficient for each of the individual genes multiplied with its corresponding expression value [31], was correlated with the hypoxia score (Additional files 6B, 7B). Hence, high-risk patients had more hypoxic tumors, suggesting that our gene signatures are efficient and adequate in predicting death.
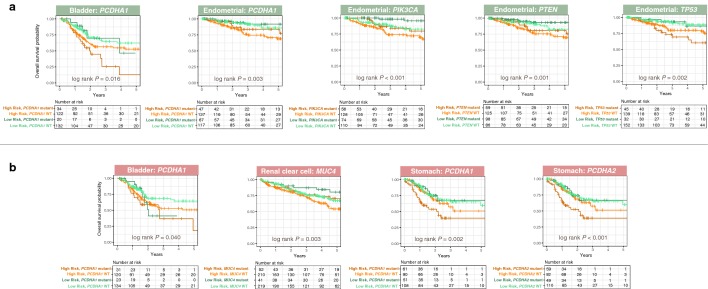
To ascertain the association between patients’ risks, as determined by our gene signatures, and somatic mutations, we retrieved the five most commonly mutated genes for each cancer. Mutations in PCDHA1, a cell adhesion gene from the cadherin superfamily, were associated with short survival in bladder urothelial carcinoma (BLCA: HR, 1.649; 95% CI 1.058–2.569; P = 0.027) and gastric adenocarcinoma (STAD: HR, 1.525; 95% CI 1.007–2.307; P = 0.046) but with prolonged survival in uterine corpus endometrial carcinoma (UCEC: HR, 0.516; 95% CI 0.272–0.978; P = 0.042) (Additional file 3). Mutations in another gene from the protocadherin alpha cluster, PCDHA2, were also associated with adverse outcomes in gastric adenocarcinoma (STAD: HR, 1.604; 95% CI 1.061–2.427; P = 0.025) (Additional file 3). Mutations in TTN and the tumor suppressor TP53 were associated with short survival in bladder urothelial carcinoma (BLCA: HR, 1.610; 95% CI 1.091–2.376; P = 0.016) and uterine corpus endometrial carcinoma (UCEC: HR, 1.780; 95% CI 1.025–3.090; P = 0.041) (Additional file 3). Interestingly, another tumor suppressor PTEN, when mutated, was linked to better outcomes in uterine corpus endometrial carcinoma (UCEC: HR, 0.427; 95% CI 0.234–0.781; P = 0.006) (Additional file 3). Similar observations were made for a lipid kinase gene PIK3CA in uterine corpus endometrial carcinoma (UCEC: HR, 0.362; 95% CI 0.190–0.689; P = 0.002) (Additional file 3). Likewise, MUC4 mutations prolonged survival in renal clear cell carcinoma patients (KIRC: HR, 0.570; 95% CI 0.370–0.880; P = 0.012) (Additional file 3), an observation that is consistent with another study [32].
Multivariate Cox regression analyses on signatures 1 and 2 while controlling for significant somatic mutation variables revealed that the gene signatures were independent survival predictors for bladder urothelial carcinoma (signature 1: HR, 0.686; 95% CI 0.466–0.912; P = 0.047 and signature 2: HR, 1.411; 95% CI 1.062–2.070; P = 0.048), renal clear cell carcinoma (signature 2: HR, 1.520; 95% CI 1.123–2.056; P = 0.007), gastric adenocarcinoma (signature 2: HR, 1.800; 95% CI 1.184–2.737; P = 0.006), and uterine corpus endometrial carcinoma (signature 1: HR, 0.519; 95% CI 0.293–0.920; P = 0.024) (Additional file 3). Signatures 1 or 2 and mutation status were collectively associated with OS (Fig. 4). In bladder urothelial carcinoma, high-risk patients (low signature 1 score) harboring mutant alleles of PCDHA1 had ~ 50% increased mortality at 5 years compared to low-risk patients (high signature 1 score) with wild-type PCDHA1 (P = 0.016; Fig. 4). Although results were less dramatic for PCDHA1 and signature 2, we still observed a ~ 25% elevated mortality at 5 years for these two patient groups with bladder urothelial carcinoma (P = 0.040; Fig. 4). In gastric adenocarcinoma, high-risk patients (high signature 2 scores) with mutant PCDHA1 had the worst outcomes (P = 0.002; Fig. 4). Conversely, PCDHA1 mutation was associated with good prognosis in uterine corpus endometrial carcinoma, hence high-risk patients with wild-type PCDHA1 had the lowest survival rates while survival was prolonged by ~ 20% in low-risk patients with mutant PCDHA1 (P = 0.003; Fig. 4). PIK3CA (P < 0.001) and PTEN mutations (P = 0.001) were associated with good outcomes in uterine corpus endometrial carcinoma (Fig. 4). Mutations in another cadherin gene PCDHA2 when considered alongside signature 2 were also associated with survival in gastric adenocarcinoma (P < 0.001; Fig. 4). Survival rates were reduced by ~ 37% in high-risk patients with mutant PCDHA2 (Fig. 4). Joint relation between TP53 mutations and signature 1 significantly influenced survival in uterine corpus endometrial carcinoma (P = 0.002; Fig. 4). Since MUC4 mutations were associated with good outcomes, survival rates were the lowest in high-risk patients (high signature 2 scores) with wild-type MUC4 (P = 0.003; Fig. 4).
Fig. 4.
Relationship between patients’ risks as determined by gene signatures and common genetic mutations. Patients were median-stratified into low or high-risk groups using a signature 1 (green panels) and b signature 2 (red panels). Since signature 1 is a marker of good prognosis, high-risk patients had a lower mean expression of signature 1 genes. Signature 2 is a marker of poor prognosis, hence high-risk patients had a higher mean expression of signature 2 genes. Kaplan–Meier plots depict combined relation of somatic mutations with signatures 1 or 2 on overall survival in cancer patients. P values were calculated from the log-rank test
Tumor suppressive roles of KDM8 through cell cycle regulation and cell adhesion maintenance
Of all the signature genes, KDM8 was identified as one of the most down-regulated genes in tumors (Fig. 5a). Patients with high KDM8 levels had a significantly lower risk of death in pancreatic and liver cancer cohorts (Fig. 5e). Prognostic significance of KDM8 was also independent of tumor stage (Fig. 5e). KDM8 expression decreased as tumor malignant grade increased in that stage 1 tumors had the highest median KDM8 values (Fig. 5b). Moreover, KDM8 expression was negatively correlated with hypoxia score, indicating that patients with low levels of KDM8 had more hypoxic tumors and poorer survival outcomes (Fig. 5c). Together, these observations suggest that KDM8 may function as a tumor suppressor. This hypothesis is corroborated by an independent report on the role of KDM8 in cell cycle regulation [33]. Indeed, we observed that KDM8 expression was negatively correlated with the expression levels of canonical cell cycle genes: cyclins (CCNA2, CCNB1, CCNB2, CCND1, CCNE1, and CCNE2) and cyclin-dependent kinases (CDK1, CDK2, CDK4, CDK6, CDK7, and CDK8), which were consistent across all liver and pancreatic cancer cohorts (Fig. 5d). This implied that KDM8 is required for tight control of the cell cycle machinery and its reduction may lead to aberrant proliferation commonly seen in cancer cells.
To ascertain the biological consequences of deregulated KDM8 expression, we conducted differential expression analysis on liver cancer patients categorized into KDM8-low and -high groups. A total of 745 genes were differentially expressed (DEGs) between the two groups (fold change > 2 or < − 2, P < 0.05) (Additional file 8). Significant enrichments of biological pathways involved in metabolism, immune regulation, VEGF production, inflammation, and cell adhesion were observed (Fig. 5f and Additional file 9). Furthermore, DEGs were overexpressed as targets of HNF4A, HNF4G, FOXA1, FOXA2, and NR2F2 transcription factors (TFs) (Fig. 5g). These TFs play central roles in cell polarity maintenance and epithelial differentiation [26, 34, 35], hence down-regulation of KDM8 may drive epithelial–mesenchymal transition (EMT) and tumor progression. HNF4A is a key TF responsible for regulating a myriad of hepatic functions including cell junction assembly [26, 36]. Pathway analysis of KDM8 DEGs revealed enrichment of processes related to cell adhesion, suggesting potential crosstalk between KDM8 and HNF4A. Of the 745 DEGs, analysis on a hepatoma-based HNF4A chromatin immunoprecipitation-sequencing dataset demonstrated that 148 genes were directly bound by HNF4A [37]. To further reinforce the interplay between HNF4A and KDM8, we observed that 110 of the 745 DEGs were overrepresented in HNF4A-null mice [26] and 45 of these genes were direct HNF4A targets (Fig. 5h). Differential expression analysis between HNF4A-deficient and wild-type mice showed that a majority of the 45 genes were down-regulated, as expected, suggesting that HNF4A directly activates their gene expression, many of which are involved in a multitude of cell adhesion processes (Fig. 5i).
Discussion
The present multi-cohort retrospective study identified two novel pan-cancer prognostic gene signatures derived from oxygen-sensing genes. Cross-platform validations confirmed prognosis in 10 cancer types to collectively include 6761 patients spanning 20 diverse cohorts (Fig. 1a). The gene signatures had opposing prognostic values: signature 1 is a marker of good prognosis, whereas signature 2 is associated with poor outcomes. The key strengths of our signatures as powerful prognostic tools are (1) pan-cancer utility, (2) involvement of a mere 5 genes each that provide continuous assessment of death risks, and (3) superiority over current TNM staging. Our results suggest that dysregulated oxygen sensing in diverse cancer types may activate other oncogenic pathways such as the loss of cell polarity and cell cycle regulation, which collectively influenced clinical outcomes in patients.
Anti-tumorigenic functions have been reported for several genes from signature 1. Loss of KDM6B resulted in more aggressive pancreatic ductal adenocarcinoma [38]. In colorectal cancer, high KDM6B expression predicted good prognosis, and knock-down of KDM6B was associated with augmented cell proliferation and inhibited apoptosis [39]. Yet, KDM6B function is enigmatic. Others have reported that high KDM6B expression is associated with increased metastasis and invasion of renal clear cell carcinoma [40]. KDM6B also promotes TGF-β-induced EMT and invasiveness in breast cancer [41]. While we could neither confirm nor deny the validity of these studies, it is striking that our observation of favorable prognosis associated with high KDM6B expression in pancreatic ductal adenocarcinoma was consistent with the report from Yamamoto et al. [38]. We also did not observe any prognostic significance of signature 1, which includes KDM6B, in either breast or renal clear cell cancer, which indirectly substantiates findings from two other reports on KDM6B not being a marker of good prognosis [40, 41]. Several other gene signatures have been reported for gastrointestinal cancers [42–46]. Interestingly, there is no overlap between our signature genes and those identified in these studies. This is perhaps not surprising since our signatures were identified based on prognostic information in pancreatic cancer, whereas those studies employed very different approaches for gene signature discovery.
KDM8 is a gene associated with favorable prognosis. Our results suggest determinative crosstalk between KDM8 and HNF4A, particularly in the context of morphogenesis, cell adhesion, maintenance of cell polarity, and epithelial formation. Moreover, 5-year survival rates dropped to ~ 12% in bladder cancer patients with low expression of signature 1 genes (high-risk), which included KDM8 and PCDHA1 mutations. Additive effects conferred by mutations in this cell-adhesion protein supports the hypothesis that KDM8 is likely a tumor suppressor and down-regulation of this gene may lead to a loss of epithelial phenotype and cell adhesion to promote cancer invasion. Additionally, loss of KDM8 expression is correlated with increased expression of cell cycle genes that may contribute to deranged cell cycle regulation and tumor progression (Fig. 5d). Like KDM6B, the function of KDM8 appears to be cell type-dependent. While KDM8 expression is down-regulated in liver and pancreatic tumor samples compared to adjacent non-tumor samples (Fig. 5a), it is overexpressed in breast cancer to induce EMT and invasion [47]. Nonetheless, KDM8 roles are not limited to cell cycle regulation. KDM8 exerts tumor suppressive functions in hematopoietic cancer by mediating DNA repair [48]. Collectively, imbalance in the Jumonji-C subfamily of lysine demethylases such as KDM8 and KDM6B is likely to result in broad-ranging but cell type-specific biological effects.
Conclusions
Overall, our gene signatures would enhance decision making in clinic by stratifying patients according to their tumor biology. This may maximize treatment efficacy and prolong lifespan by directing resources to those most in need. This technology may be incorporated into existing diagnostic pathways to achieve a more individualized standard of care by revealing molecular changes that allow further discrimination of otherwise similarly staged tumors. As each signature only consists of 5 genes, we anticipate that they can be implemented immediately, even in modestly sized centers that are using PCR-based technology. Consequently, therapeutic options can be allocated more decisively based upon this additional personalized information to ensure that patients with the most aggressive cancers get the most robust treatments.
Additional files
Additional file 1. Cancer cohort descriptions.
Additional file 2. List of 61 2OG-dependent oxygenases.
Additional file 3. Univariate and multivariate Cox proportional hazards analysis of risk factors associated with overall survival in multiple cancers. Univariate values of TNM stage were in accordance with our previous report utilizing TCGA datasets [4].
Additional file 4. Additional tumor subgroup analyses and evaluation of prognosis predictive performance of gene signatures across different malignant grades. Kaplan–Meier plots show independence of (A) signature 1 (green panels) and (B) signature 2 (red panels) over current TNM staging system in predicting prognosis in different cancer cohorts. Patients were sub-grouped according to TNM stages and further stratified using either signature 1 or signature 2 scores. Both signatures successfully identified high-risk patients in different TNM stages. P values were calculated from the log-rank test. Analysis of specificity and sensitivity of (C) signature 1 (green panels) and (D) signature 2 (red panels) in predicting prognosis in different cancer cohorts using receiver operating characteristic (ROC) curves. Plots depict comparison of ROC curves of signature 1 or 2 and clinical TNM staging. Both signatures demonstrated incremental values over current TNM staging system. AUC: area under the curve. TNM: tumor, node, metastasis staging. Liver #1 = LIHC cohort; Liver #2 = LIRI-JP cohort and Liver #3 = GSE14520 cohort (Additional file 1).
Additional file 5. Distribution of expression of signature genes in low- and high-risk patients. (A) signature 1 (green panels) and (B) signature 2 (red panels). Patients were median-stratified into low- and high-risk groups based on mean expression scores of signature genes. Box plots depict expression distribution of each of the 5 genes in both signatures in these two patient groups. (A) Since signature 1 is a marker of good prognosis, high-risk patients show significantly lower expression of individual signature genes. (B) In contrast, signature 2 is a marker of poor prognosis, hence high-risk patients show significantly higher expression of individual signature genes. Nonparametric Mann–Whitney–Wilcoxon tests were used to compare low- and high-risk patients. Asterisks represent significant P values: * < 0.01, ** < 0.001 and *** < 0.0001. LR = low risk. HR = high risk.
Additional file 6. Correlation of patients’ risk scores derived from signature 1 with tumor hypoxia. (A) Significant negative correlation between signature 1 expression scores and tumor hypoxia. (B) Significant positive correlation between signature 1 risk scores and tumor hypoxia. Calculations of expression scores, risk scores, and hypoxia scores are explained in the methods. Liver #1 = LIHC cohort and Liver #2 = LIRI-JP cohort.
Additional file 7. Correlation of patients’ risk scores derived from signature 2 with tumor hypoxia. (A) Significant positive correlation between signature 2 expression scores and tumor hypoxia. (B) Significant positive correlation between signature 2 risk scores and tumor hypoxia. Calculations of expression scores, risk scores and hypoxia scores are explained in the methods. Liver #2 = LIRI-JP cohort and Liver #3 = GSE14520 cohort.
Additional file 8. Differentially expressed genes between KDM8-high and -low groups in the liver cancer cohort (LIHC).
Additional file 9. Significantly enriched biological pathways of differentially expressed genes.
Authors’ contributions
AGL had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: WHC and AGL. Data acquisition and analysis: WHC and AGL. Data interpretation: all authors. Drafting the manuscript: WHC and AGL. Critical revision of the manuscript for important intellectual content: all authors. Supervision: AGL. All authors read and approved the final manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and its additional files.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Funding
Not applicable.
Abbreviations
- HIF
hypoxia inducible factor
- 2OG
2-oxoglutarate
- OS
overall survival
- KDM
Jumonji-C domain-containing lysine demethylase
- TCGA
The Cancer Genome Atlas
- ICGC
International Cancer Genome Consortium
- GEO
Gene Expression Omnibus
- RSEM
RNA-seq by expectation maximization
- HR
hazard ratio
- CI
confidence interval
- ROC
receiver operating characteristic
- AUC
area under the curve
- KEGG
Kyoto Encyclopedia of Genes and Genomes
- GO
gene ontology
- BCLC
Barcelona Clinic Liver Cancer
- TNM
tumor, node, metastasis
- EMT
epithelial–mesenchymal transition
- DEG
differentially expressed gene
- TF
transcription factor
- AFP
alpha-fetoprotein
Contributor Information
Wai Hoong Chang, Email: changwaihoong@gmail.com.
Donall Forde, Email: donall.forde@ndm.ox.ac.uk.
Alvina G. Lai, Email: alvinagracelai@gmail.com
References
- 1.Zeng W, Liu P, Pan W, Singh SR, Wei Y. Hypoxia and hypoxia inducible factors in tumor metabolism. Cancer Lett. 2015;356:263–267. doi: 10.1016/j.canlet.2014.01.032. [DOI] [PubMed] [Google Scholar]
- 2.Denko NC. Hypoxia, HIF1 and glucose metabolism in the solid tumour. Nat Rev Cancer. 2008;8:705. doi: 10.1038/nrc2468. [DOI] [PubMed] [Google Scholar]
- 3.Nagy JA, Chang SH, Dvorak AM, Dvorak HF. Why are tumour blood vessels abnormal and why is it important to know? Br J Cancer. 2009;100:865. doi: 10.1038/sj.bjc.6604929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang WH, Forde D, Lai AG. A novel signature derived from immunoregulatory and hypoxia genes predicts prognosis in liver and five other cancers. J Transl Med. 2019;17:14. doi: 10.1186/s12967-019-1775-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Semenza GL, Wang GL. A nuclear factor induced by hypoxia via de novo protein synthesis binds to the human erythropoietin gene enhancer at a site required for transcriptional activation. Mol Cell Biol. 1992;12:5447–5454. doi: 10.1128/MCB.12.12.5447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ratcliffe PJ. Oxygen sensing and hypoxia signalling pathways in animals: the implications of physiology for cancer. J Physiol. 2013;591:2027–2042. doi: 10.1113/jphysiol.2013.251470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Semenza GL. Evaluation of HIF-1 inhibitors as anticancer agents. Drug Discov Today. 2007;12:853–859. doi: 10.1016/j.drudis.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 8.Melillo G. Inhibiting hypoxia-inducible factor 1 for cancer therapy. Mol Cancer Res. 2006;4:601–605. doi: 10.1158/1541-7786.MCR-06-0235. [DOI] [PubMed] [Google Scholar]
- 9.Ploumakis A, Coleman ML. OH, the places you’ll go! hydroxylation, gene expression, and cancer. Mol Cell. 2015;58:729–741. doi: 10.1016/j.molcel.2015.05.026. [DOI] [PubMed] [Google Scholar]
- 10.Ko M, An J, Pastor WA, Koralov SB, Rajewsky K, Rao A. TET proteins and 5-methylcytosine oxidation in hematological cancers. Immunol Rev. 2015;263:6–21. doi: 10.1111/imr.12239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang Y, Rao A. Connections between TET proteins and aberrant DNA modification in cancer. Trends Genet. 2014;30:464–474. doi: 10.1016/j.tig.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dalgliesh GL, Furge K, Greenman C, Chen L, Bignell G, Butler A, et al. Systematic sequencing of renal carcinoma reveals inactivation of histone modifying genes. Nature. 2010;463:360. doi: 10.1038/nature08672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van Haaften G, Dalgliesh GL, Davies H, Chen L, Bignell G, Greenman C, et al. Somatic mutations of the histone H3K27 demethylase gene UTX in human cancer. Nat Genet. 2009;41:521. doi: 10.1038/ng.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weinstein JN, Collisson EA, Mills GB, Shaw KRM, Ozenberger BA, Ellrott K, et al. The cancer genome atlas pan-cancer analysis project. Nat Genet. 2013;45:1113. doi: 10.1038/ng.2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang J, Baran J, Cros A, Guberman JM, Haider S, Hsu J, Liang Y, Rivkin E, Wang J, Whitty B, Wong-Erasmus M, Yao L, Kasprzyk A. International cancer genome consortium data portal—a one-stop shop for cancer genomics data. Database. 2011;2011:bar026. doi: 10.1093/database/bar026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li B, Dewey CN. RSEM: accurate transcript quantification from RNA-Seq data with or without a reference genome. BMC Bioinform. 2011;12:323. doi: 10.1186/1471-2105-12-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roessler S, Jia HL, Budhu A, Forgues M, Ye QH, Lee JS, et al. A unique metastasis gene signature enables prediction of tumor relapse in early-stage hepatocellular carcinoma patients. Cancer Res. 2010;70:10202–10212. doi: 10.1158/0008-5472.CAN-10-2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ritchie ME, Phipson B, Wu D, Hu Y, Law CW, Shi W, et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47. doi: 10.1093/nar/gkv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buffa FM, Harris AL, West CM, Miller CJ. Large meta-analysis of multiple cancers reveals a common, compact and highly prognostic hypoxia metagene. Br J Cancer. 2010;102:428–435. doi: 10.1038/sj.bjc.6605450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Therneau TM. A package for survival analysis in S. 2015. https://cran.r-project.org/package=survival.
- 21.Kassambara A, Kosinski M. survminer: drawing survival curves using “ggplot2”. 2018. https://cran.r-project.org/package=survminer.
- 22.Schroeder M, Culhane A, Quackenbush J, Haibe-Kains B. Survcomp: an R/bioconductor package for performance assessment and comparison of survival models. Bioinformatics. 2011;27(22):3206–3208. doi: 10.1093/bioinformatics/btr511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tabas-Madrid D, Nogales-Cadenas R, Pascual-Montano A. GeneCodis3: a non-redundant and modular enrichment analysis tool for functional genomics. Nucleic Acids Res. 2012;40:W478–W483. doi: 10.1093/nar/gks402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuleshov MV, Jones MR, Rouillard AD, Fernandez NF, Duan Q, Wang Z, et al. Enrichr: a comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res. 2016;44:W90–W97. doi: 10.1093/nar/gkw377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen EY, Tan CM, Kou Y, Duan Q, Wang Z, Meirelles GV, et al. Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinform. 2013;14:128. doi: 10.1186/1471-2105-14-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Battle MA, Konopka G, Parviz F, Gaggl AL, Yang C, Sladek FM, et al. Hepatocyte nuclear factor 4α orchestrates expression of cell adhesion proteins during the epithelial transformation of the developing liver. Proc Natl Acad Sci USA. 2006;103:8419–8424. doi: 10.1073/pnas.0600246103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wickham H. ggplot2: elegant graphics for data analysis. New York: Springer; 2016. https://ggplot2.tidyverse.org/.
- 28.R Core Team. R: A Language and Environment for Statistical Computing. Vienna: R Core Team; 2018. https://www.r-project.org/.
- 29.Fujimoto A, Furuta M, Totoki Y, Tsunoda T, Kato M, Shiraishi Y, et al. Whole-genome mutational landscape and characterization of noncoding and structural mutations in liver cancer. Nat Genet. 2016;48:500. doi: 10.1038/ng.3547. [DOI] [PubMed] [Google Scholar]
- 30.Vaupel P, Mayer A. Hypoxia in cancer: significance and impact on clinical outcome. Cancer Metastasis Rev. 2007;26:225–239. doi: 10.1007/s10555-007-9055-1. [DOI] [PubMed] [Google Scholar]
- 31.Kim SM, Leem SH, Chu IS, Park YY, Kim SC, Kim SB, et al. Sixty-five gene-based risk score classifier predicts overall survival in hepatocellular carcinoma. Hepatology. 2012;55:1443–1452. doi: 10.1002/hep.24813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.King RJ, Yu F, Singh PK. Genomic alterations in mucins across cancers. Oncotarget. 2017;8:67152. doi: 10.18632/oncotarget.17934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu B-H, Chen H, Cai C-M, Fang J-Z, Wu C-C, Huang L-Y, et al. Epigenetic silencing of JMJD5 promotes the proliferation of hepatocellular carcinoma cells by down-regulating the transcription of CDKN1A. Oncotarget. 2016;7:6847. doi: 10.18632/oncotarget.6867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang C, Han Y, Huang H, Qu L, Shou C. High NR2F2 transcript level is associated with increased survival and its expression inhibits TGF-β-dependent epithelial–mesenchymal transition in breast cancer. Breast Cancer Res Treat. 2014;147:265–281. doi: 10.1007/s10549-014-3095-3. [DOI] [PubMed] [Google Scholar]
- 35.Song Y, Washington MK, Crawford HC. Loss of FOXA1/2 is essential for the epithelial-to-mesenchymal transition in pancreatic cancer. Cancer Res. 2010;70:2115–2125. doi: 10.1158/0008-5472.CAN-09-2979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Odom DT, Zizlsperger N, Gordon DB, Bell GW, Rinaldi NJ, Murray HL, et al. Control of pancreas and liver gene expression by HNF transcription factors. Science. 2004;303:1378–1381. doi: 10.1126/science.1089769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Consortium EP An integrated encyclopedia of DNA elements in the human genome. Nature. 2012;489:57. doi: 10.1038/nature11247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yamamoto K, Tateishi K, Kudo Y, Sato T, Yamamoto S, Miyabayashi K, et al. Loss of histone demethylase KDM6B enhances aggressiveness of pancreatic cancer through downregulation of C/EBPα. Carcinogenesis. 2014;35:2404–2414. doi: 10.1093/carcin/bgu136. [DOI] [PubMed] [Google Scholar]
- 39.Tokunaga R, Sakamoto Y, Nakagawa S, Miyake K, Izumi D, Kosumi K, et al. The prognostic significance of histone lysine demethylase JMJD3/KDM6B in colorectal cancer. Ann Surg Oncol. 2016;23:678–685. doi: 10.1245/s10434-015-4879-3. [DOI] [PubMed] [Google Scholar]
- 40.Li Q, Hou L, Ding G, Li Y, Wang J, Qian B, et al. KDM6B induces epithelial–mesenchymal transition and enhances clear cell renal cell carcinoma metastasis through the activation of SLUG. Int J Clin Exp Pathol. 2015;8:6334. [PMC free article] [PubMed] [Google Scholar]
- 41.Ramadoss S, Chen X, Wang CY. Histone demethylase KDM6B promotes epithelial-mesenchymal transition. J Biol Chem. 2012;287:44508–44517. doi: 10.1074/jbc.M112.424903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kukita Y, Ohkawa K, Takada R, Uehara H, Katayama K, Kato K. Selective identification of somatic mutations in pancreatic cancer cells through a combination of next-generation sequencing of plasma DNA using molecular barcodes and a bioinformatic variant filter. PLoS ONE. 2018;13:e0192611. doi: 10.1371/journal.pone.0192611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Takeuchi S, Doi M, Ikari N, Yamamoto M, Furukawa T. Mutations in BRCA1, BRCA2, and PALB2, and a panel of 50 cancer-associated genes in pancreatic ductal adenocarcinoma. Sci Rep. 2018;8:8105. doi: 10.1038/s41598-018-26526-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Peters MLB, Tseng JF, Miksad RA. Genetic testing in pancreatic ductal adenocarcinoma: implications for prevention and treatment. Clin Ther. 2016;38:1622–1635. doi: 10.1016/j.clinthera.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 45.Li X, Xu W, Kang W, Wong SH, Wang M, Zhou Y, et al. Genomic analysis of liver cancer unveils novel driver genes and distinct prognostic features. Theranostics. 2018;8:1740. doi: 10.7150/thno.22010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Park J, Yoo HM, Jang W, Shin S, Kim M, Kim Y, et al. Distribution of somatic mutations of cancer-related genes according to microsatellite instability status in Korean gastric cancer. Medicine. 2017;96(25):e7224. doi: 10.1097/MD.0000000000007224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhao Z, Sun C, Li F, Han J, Li X, Song Z. Overexpression of histone demethylase JMJD5 promotes metastasis and indicates a poor prognosis in breast cancer. Int J Clin Exp Pathol. 2015;8:10325. [PMC free article] [PubMed] [Google Scholar]
- 48.Suzuki T, Minehata K, Akagi K, Jenkins NA, Copeland NG. Tumor suppressor gene identification using retroviral insertional mutagenesis in Blm-deficient mice. EMBO J. 2006;25:3422–3431. doi: 10.1038/sj.emboj.7601215. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Cancer cohort descriptions.
Additional file 2. List of 61 2OG-dependent oxygenases.
Additional file 3. Univariate and multivariate Cox proportional hazards analysis of risk factors associated with overall survival in multiple cancers. Univariate values of TNM stage were in accordance with our previous report utilizing TCGA datasets [4].
Additional file 4. Additional tumor subgroup analyses and evaluation of prognosis predictive performance of gene signatures across different malignant grades. Kaplan–Meier plots show independence of (A) signature 1 (green panels) and (B) signature 2 (red panels) over current TNM staging system in predicting prognosis in different cancer cohorts. Patients were sub-grouped according to TNM stages and further stratified using either signature 1 or signature 2 scores. Both signatures successfully identified high-risk patients in different TNM stages. P values were calculated from the log-rank test. Analysis of specificity and sensitivity of (C) signature 1 (green panels) and (D) signature 2 (red panels) in predicting prognosis in different cancer cohorts using receiver operating characteristic (ROC) curves. Plots depict comparison of ROC curves of signature 1 or 2 and clinical TNM staging. Both signatures demonstrated incremental values over current TNM staging system. AUC: area under the curve. TNM: tumor, node, metastasis staging. Liver #1 = LIHC cohort; Liver #2 = LIRI-JP cohort and Liver #3 = GSE14520 cohort (Additional file 1).
Additional file 5. Distribution of expression of signature genes in low- and high-risk patients. (A) signature 1 (green panels) and (B) signature 2 (red panels). Patients were median-stratified into low- and high-risk groups based on mean expression scores of signature genes. Box plots depict expression distribution of each of the 5 genes in both signatures in these two patient groups. (A) Since signature 1 is a marker of good prognosis, high-risk patients show significantly lower expression of individual signature genes. (B) In contrast, signature 2 is a marker of poor prognosis, hence high-risk patients show significantly higher expression of individual signature genes. Nonparametric Mann–Whitney–Wilcoxon tests were used to compare low- and high-risk patients. Asterisks represent significant P values: * < 0.01, ** < 0.001 and *** < 0.0001. LR = low risk. HR = high risk.
Additional file 6. Correlation of patients’ risk scores derived from signature 1 with tumor hypoxia. (A) Significant negative correlation between signature 1 expression scores and tumor hypoxia. (B) Significant positive correlation between signature 1 risk scores and tumor hypoxia. Calculations of expression scores, risk scores, and hypoxia scores are explained in the methods. Liver #1 = LIHC cohort and Liver #2 = LIRI-JP cohort.
Additional file 7. Correlation of patients’ risk scores derived from signature 2 with tumor hypoxia. (A) Significant positive correlation between signature 2 expression scores and tumor hypoxia. (B) Significant positive correlation between signature 2 risk scores and tumor hypoxia. Calculations of expression scores, risk scores and hypoxia scores are explained in the methods. Liver #2 = LIRI-JP cohort and Liver #3 = GSE14520 cohort.
Additional file 8. Differentially expressed genes between KDM8-high and -low groups in the liver cancer cohort (LIHC).
Additional file 9. Significantly enriched biological pathways of differentially expressed genes.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article and its additional files.