Abstract
OBJECTIVE
To determine the source of a healthcare-associated outbreak of Pantoea agglomerans bloodstream infections.
DESIGN
Epidemiologic investigation of the outbreak.
SETTING
Oncology clinic (clinic A).
METHODS
Cases were defined as Pantoea isolation from blood or catheter tip cultures of clinic A patients during July 2012-May 2013. Clinic A medical charts and laboratory records were reviewed; infection prevention practices and the facility’s water system were evaluated. Environmental samples were collected for culture. Clinical and environmental P. agglomerans isolates were compared using pulsed-field gel electrophoresis.
RESULTS
Twelve cases were identified; median (range) age was 65 (41–78) years. All patients had malignant tumors and had received infusions at clinic A. Deficiencies in parenteral medication preparation and handling were identified (eg, placing infusates near sinks with potential for splash-back contamination). Facility inspection revealed substantial dead-end water piping and inadequate chlorine residual in tap water from multiple sinks, including the pharmacy clean room sink. P. agglomerans was isolated from composite surface swabs of 7 sinks and an ice machine; the pharmacy clean room sink isolate was indistinguishable by pulsed-field gel electrophoresis from 7 of 9 available patient isolates.
CONCLUSIONS
Exposure of locally prepared infusates to a contaminated pharmacy sink caused the outbreak. Improvements in parenteral medication preparation, including moving chemotherapy preparation offsite, along with terminal sink cleaning and water system remediation ended the outbreak. Greater awareness of recommended medication preparation and handling practices as well as further efforts to better define the contribution of contaminated sinks and plumbing deficiencies to healthcare-associated infections are needed.
Pantoea species are members of the family Enterobacteriaceae and are generally identified from environmental samples, including soil and water. Although rarely a cause of human illness, isolated infections and clusters have been reported in adults and children, usually following a penetrating trauma involving plants or in association with immunosuppression and indwelling vascular devices.1–5 Healthcare-associated outbreaks of Pantoea spp. due to contaminated medical products have also been reported and have been attributed to contaminated total parenteral nutrition, propofol, blood products, and anticoagulant citrate dextrose solution.6–10
During August 2012-February 2013, 8 patients were diagnosed with Pantoea agglomerans bloodstream infections (BSIs) at an Illinois outpatient oncology clinic (clinic A) that had no such infections in the previous year. The majority of infected patients developed rigors while receiving an intravenous infusion at clinic A; the only common exposure identified was commercially manufactured normal saline flush syringes. On February 19, 2013, clinic A stopped using the product and sent a batch of unopened saline flush syringes to the Centers for Disease Control and Prevention (CDC) for sterility testing. A culture performed at the facility’s laboratory of a single, used flush syringe grew P. agglomerans; however, no organisms were cultured from any of the unopened flushes at CDC and there were no other reports of Pantoea infections linked to this particular saline flush product in Illinois or nationwide.
In May 2013, 2 additional patients were diagnosed with Pantoea spp. BSIs at clinic A, prompting a request from the Cook County Department of Public Health, the Illinois Department of Public Health, and clinic A for on-site assistance from CDC. This report describes the findings of the investigation.
METHODS
Case Definition, Case Finding, and Data Collection
A case was defined as P. agglomerans cultured from blood or a catheter tip from a patient examined at clinic A during July 2012–May 2013. Case finding was performed by reviewing microbiology records from clinic A’s affiliated hospital during the period of interest. Medical charts of case patients were reviewed to identify common exposures.
Infection Prevention Assessment and Facility Inspection
Clinic A nursing and pharmacy staff were interviewed. Observations of relevant procedures were performed, including central line access, handling and administration of infusion products, medication preparation, and compounding practices. The facility’s plumbing system was also evaluated. Residual chlorine testing of water from the clinic’s sinks was performed on site using both dipstick and reagent methods.
Environmental Sampling and Laboratory Analysis
Environmental samples collected from clinic A included swab samples of high-touch surfaces in the infusion room and pharmacy; an ice machine; sink composite samples consisting of faucet, adjacent countertop, basin, and drain of each sink; and 1-liter tap water samples from each clinic sink. Surface samples were collected using sterile sponge sticks (3M). Water samples were collected in sterile containers with sodium thiosulfate tablets. Hand cultures were obtained from clinic nursing and pharmacy staff using established methods (Handi Wipes; Clorox).11
All environmental samples and hand cultures were sent to the CDC for bacterial testing. Surface samples were processed by high-volume homogenization, concentrated by centrifugation, plated, and cultured for gram-negative organisms. Bacteriologic water testing was performed using heterotrophic plate counts and conventional culture. Suspect isolates were identified as P. agglomerans using an automated biochemical identification system (Vitek 2; bioMérieux). Pulsed-field gel electrophoresis was performed on all available patient and environmental isolates of P. agglomerans to determine genetic relatedness. Genomic DNA was restricted with the XbaI enzyme; electrophoresis conditions included switch times of 2 and 40 seconds for 22 hours. A dendrogram comparing the resulting band patterns was generated using Bionumerics, version 6.6 (Applied Maths).
RESULTS
Description of Cases
In total, 12 cases were identified; the first case occurred in August 2012 and the last in May 2013 (Figure 1). All 12 had at least one positive blood culture for P. agglomerans; one also had a positive catheter tip culture. Seven (58%) of the case-patients were female; the median (range) age was 65 (41–78) years (Table 1). All case patients had been diagnosed with a malignant tumor. Eleven case patients had a documented fever within 48 hours of their first positive P. agglomerans culture; 9 (75%) required hospitalization. None of the case patients died within 30 days of their first positive culture.
FIGURE 1.
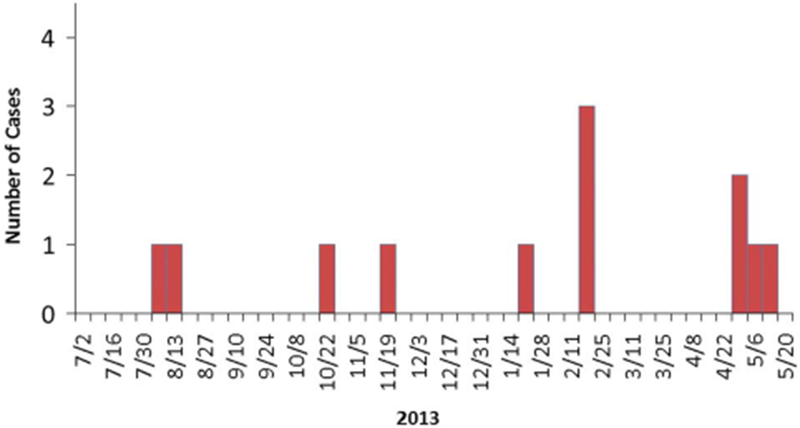
Epidemic curve for 12 Pantoea agglomerans cases at clinic A by week of first positive blood or catheter tip culture, July 2012-May 2013.
TABLE 1.
Demographic and Clinical Characteristics and Healthcare Exposures of 12 Pantoea agglomerans Case Patients at Clinic A in Illinois, 2012-2013
| Characteristic | Value |
|---|---|
| Demographic characteristics | |
| Female sex | 7 (58) |
| Age, median (range), y | 65 (41–78) |
| Clinical characteristics | |
| Diagnosis of malignant tumor | 12 (100) |
| Solid organ | 9 (75) |
| Hematologic | 3 (25) |
| Presence of central line (ie, implanted port) | 11 (92) |
| Time central line in place at time of positive culture, median (range), months | 4 (2–30) |
| Documented fever (temperature ≥100.4°F) within 48 hours of first positive culture | 11 (92) |
| Chills or rigors during presentation | 10 (83) |
| Blood culture positive for P. agglomerans infectiona | 12 (100) |
| Hospitalized for P. agglomerans infection | 9 (75) |
| Treated with antibiotics | 11 (92) |
| Central line removed | 7/11 (64) |
| Death within 30 days of initial culture | 0 (0) |
| Healthcare exposuresb | |
| Any infusion product (excluding saline or heparin flush) | 12 (100) |
| Chemotherapy infusion (prepared at clinic A) | 11 (92) |
| Blood transfusion | 2 (17) |
| Receipt of heparin flush | 11 (92) |
| Receipt of normal saline flush | 12 (100) |
| Number of infusion visits, median (range) | 2 (0–8) |
| Time since most recent chemotherapy infusion, median (range), days | 14 (0–54) |
note. Data are no. (%) of case-patients, unless otherwise indicated.
One patient also had a positive catheter tip culture for P. agglomerans.
Occurring within 3 weeks or 3 infusion visits prior to the date of the first positive Pantoea culture.
All 12 case-patients had received an infusion at clinic A before the onset of their P. agglomerans BSI (Table 1). Eleven case patients (92%) had an implanted port, and all 11 had received a chemotherapy infusion prepared at clinic A’s on-site pharmacy during the 3 weeks preceding their first positive culture.
Infection Prevention Assessment and Facility Inspection
Clinic A staff included 3 physicians, 3 registered nurses, and 3 pharmacy staff. The clinic provided infusions to 20–30 patients per day, with non-infusion visits accounting for an additional 40–50 patients per day. Chemotherapy, blood products, and other intravenous fluids were administered in an infusion room with 12 patient chairs and 5 sinks; all central lines were accessed exclusively by nursing staff. Limited observations of hand hygiene and port access revealed no systematic deficiencies. However, infusion products were sometimes noted to be placed on countertops immediately adjacent to sinks with the tubing of the infusate bags draping over the sink rim, creating the potential for splash-back of water onto the infusate bags and tubing.
The on-site pharmacy contained a small medication preparation room (“clean room”), separated from the rest of the pharmacy by a doorway, with 2 laminar airflow workbenches (“hoods”), one of which was primarily used for chemotherapy preparation. Several concerns with medication preparation in the pharmacy were noted, including occasional rinsing of hands without soap or adequate drying, gloved hands entering the hood without adequate disinfection, and occasional inadequate disinfection of medication vial septa. Most notably, the pharmacy clean room contained a sink that was located close to both hoods and next to a countertop where recently prepared infusion products were placed; the presence of a sink in the clean room is contrary to published guidelines.12,13
The facility inspection revealed substantial dead-end piping in vacant areas of the building where clinic A was located. These included an out-of-use upstairs clinic, as well as a former radiation oncology suite adjacent to clinic A that had been vacated several months before the start of the outbreak. The radiation oncology suite had dead-end piping associated with equipment used for radiation treatments. This dead-end piping reduced water pressure to clinic A and depleted residual chlorine levels. Residual chlorine testing of water indicated levels below the accepted end-use level of 0.2 ppm (parts per million) in the clean room sink and 4 of the 5 infusion room sinks. Staff also indicated that water from the pharmacy and infusion room sinks had a yellow discoloration some mornings, especially after heavy rainstorms.
Laboratory Analysis
Fifty-one environmental samples and handwipe cultures were collected. P. agglomerans was isolated from composite samples of sinks in several rooms, including the infusion room (4 of 5 sinks), the pharmacy clean room, the staff bathroom, and a patient examination room. P. agglomerans was also isolated from a composite sample of the ice machine in the staff break room. No Pantoea were isolated from handwipe specimens, from surface samples, or directly from water samples. However, water samples from all 8 sinks exceeded the US Environmental Protection Agency’s ceiling heterotrophic plate count of 500 colony-forming units/mL, with counts ranging from 550 to more than 3,000 colony-forming units/mL from infusion room sinks and from 1,070 to more than 3,000 colony-forming units/mL from pharmacy sinks.
Of the 9 case patients from whom P. agglomerans isolates were available, 7 had a pulsed-field gel electrophoresis pattern indistinguishable from the isolate recovered from the sink composite sample in the pharmacy clean room (Figure 2). The isolate from a used syringe, which also matched the patient cluster, was deemed to have likely been contaminated by patient blood or tubing. The other patient and environmental isolates had distinct pulsed-field gel electrophoresis patterns.
FIGURE 2.
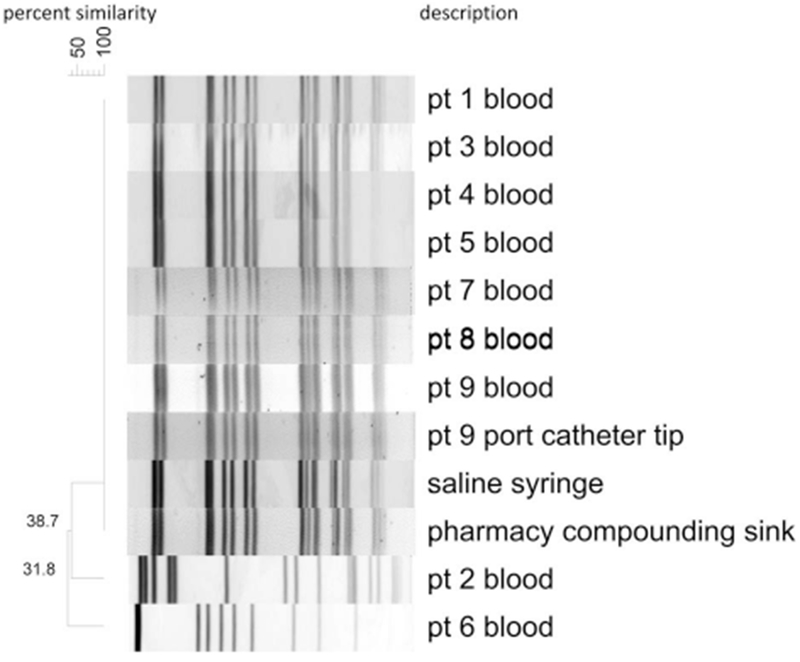
Pulsed-field gel electrophoresis dendrogram of Pantoea isolates from clinic A patients and select environmental cultures. For ease of display, 7 environmental Pantoea isolates from clinic A not matching the outbreak strain were not included in this figure. Pharmacy compounding sink in the figure refers to the sink located in the on-site pharmacy clean room sink.
Control Measures
Recommendations to clinic A included immediate terminal cleaning, focusing on sink areas in all rooms, and consultation with state and local experts to improve the facility’s water system, including rectifying the inadequate residual chlorine and dead-end piping. Clinic A staff were advised to refrain from placing any infusion products in or adjacent to sinks and to ensure strict adherence to national standards for safe compounding.12,13 This included reinforcing proper hand hygiene and medication preparation practices as well as implementing appropriate environmental controls in the pharmacy, including the removal of the clean room sink and the avoidance of any source of water near the hoods. Clinic A immediately moved chemotherapy preparation off-site and improved the building water system (cutting and capping many dead-end areas of piping back to the main line, increasing water system pressure, and regularly testing residual chlorine levels to ensure adequacy). Apart from 1 additional case of Pantoea BSI in a patient exposed before these interventions, no further cases were identified during the following year.
DISCUSSION
We describe a large outbreak of P. agglomerans BSIs at a single oncology clinic that was linked to a contaminated pharmacy sink. We identified aspects of the pharmacy layout and the preparation and handling of medications that likely facilitated the exposure of locally compounded infusates and/or associated tubing to water or splash from the sink. These included the presence of the sink in the cluttered pharmacy clean room, placement of infusate bags on counters adjacent to the sink, and inadequate hand drying by pharmacy personnel immediately prior to compounding. P. agglomerans was not directly recovered from any of the water samples; however, the elevated heterotrophic plate counts of water samples from all the sinks and growth of P. agglomerans strains from multiple sink composite samples throughout the facility suggest tap water could have been the source. A possible overgrowth of P. agglomerans in tap water could have been facilitated by the dead-end piping and low residual chlorine levels related to out-of-use building space and equipment. Alternatively, P. agglomerans could have been introduced into the sink drains and p-traps by an exogenous source, followed by splash-back out of the sinks to contaminate the surrounding environment. In this scenario, the problems with the facility’s water distribution system would have been unrelated to the outbreak.
Healthcare-associated outbreaks attributed to a water source have been commonly reported.14–21 These clusters have often involved Legionella, non-tuberculous mycobacteria, or certain gram-negative pathogens, such as Pseudomonas aeruginosa and Acinetobacter baumannii. Sink p-traps and drains are increasingly recognized as sources for healthcare-associated outbreaks.22–24 Even organisms less commonly associated with an environmental source, like multidrug-resistant Enterobacteriaceae, have been recovered from the sink basin, drain, or trap during an outbreak, suggesting that contaminated sinks and the drainage system (as a result of contaminated fluid waste going down the drain) might be an environmental reservoir for these organisms.23,24 Previous reports have indicated the potential for splash-back from sink drains to contaminate the surrounding environment, thereby serving as a source for transmission.22,25,26 In one study, the use of fluorescent marker revealed that splashes originating from sink drains were visible at least 1 meter from the sink, and that smaller particles might have traveled farther.25
During outbreaks involving waterborne organisms, a direct link to a water source for individual patients can sometimes be difficult to establish since some of these organisms can also be transmitted patient-to-patient from contact with contaminated environmental surfaces or equipment or via hands of healthcare personnel.14,27 Solving these outbreaks often involves isolation of the organism from tap water, faucets or aerators, or other sink components and the identification of opportunities for contamination of medications or equipment.17–19,23,24 The fact that 7 of the 9 patient isolates in this outbreak were the same strain as the isolate from the pharmacy clean room sink strongly implicated that sink as the source. Not surprisingly, other P. agglomerans strains were detected in the environment, and the isolation of distinct strains in 2 patients could point to additional pathways of infection from an environmental source.
To prevent healthcare-associated outbreaks related to a water source, interventions should focus on minimizing exposure to splash of droplets or aerosols from sinks or other water sources. Although in some situations this might be achieved with the use of splash barriers, another approach would be to avoid performing patient procedures and medication preparation, as well as storing medications and patient supplies and equipment, in the vicinity of a sink or other water sources. In addition, enhanced daily cleaning and disinfection of surfaces that might be contaminated by splash (eg, counters) or that might serve as a reservoir for organisms (eg, sink basins) might decrease the risk of transmission. Other interventions that could reduce the burden of contamination in and around sinks or other water sources might need to target facility premise plumbing, including drainage systems, as well as upstream pipe and water system. Because of the difficulty in eradicating biofilms with disinfectants, some facilities have replaced sinks or plumbing systems,23,24,28 although recontamination can occur. Current guidelines for the decontamination and maintenance of healthcare facility water system are primarily focused on preventing Legionella outbreaks.29 As healthcare-associated outbreaks related to water contamination occur with increasing frequency, evidence-based recommendations for maintenance of facility water systems will need to target other organisms.
This outbreak also highlights ongoing concerns about medication preparation and handling in outpatient settings, where awareness of recommended practices can vary greatly. Currently, most outpatient facilities, including oncology clinics, are not regulated by a state or federal licensing/certification agency and thus are not routinely inspected for adherence to recommended infection prevention practices. Outpatient oncology facilities might be particularly concerning because they often treat an immunocompromised population and handle a high volume of injectable medications that require more complex compounding procedures (eg, preparation of chemotherapy infusions). Several outbreaks involving outpatient oncology facilities have been reported,30–34 and in some instances, injectable medications were prepared by personnel without formal training or in a facility without appropriate environmental controls (eg, placement of chemotherapy hood next to an open window).30,31 Clinic A had an on-site pharmacy with professionally trained staff to perform compounding of sterile medications in a dedicated clean room; however, deficiencies in medication preparation and handling were still identified. These findings underscore the continued need to increase awareness of existing guidelines for the safe preparation and handling of injectable medications and to expand infection control oversight across all outpatient settings.12,13,35 In 2015, the CDC released a policy guide to assist health departments and policymakers to identify gaps in oversight of outpatient settings in their jurisdictions and pursue potential solutions.36 The CDC is also working with state and federal partners to expand the uptake of infection prevention guidance materials in outpatient settings.37,38
Our investigation had several limitations. Patient data were collected through retrospective medical chart reviews instead of patient interviews, and incomplete documentation in charts might have limited our ability to identify all potential exposures. Our investigation was conducted several months after the outbreak onset, and the practices and conditions that contributed to the risk of developing P. agglomerans infection might have changed. Isolates from 3 of the 12 cases were not available for molecular characterization; however, isolate data from the remaining cases supported a point-source outbreak. Because composite samples were used to collect environmental cultures from the sink and adjacent countertops, we could not definitively determine the specific sink components or countertop areas that were contaminated. We also could not determine the primary source of the P. agglomerans associated with the pharmacy clean room sink. P. agglomerans was not recovered from any of the tap water samples, but this could have been due to the transient contamination of water or sparse colony counts of this fastidious bacterium.
In conclusion, our investigation provides additional evidence for transmission of bacteria from contaminated sinks, resulting in substantial morbidity to patients. Further evaluation is needed to characterize the burden of healthcare-associated infections that result from water-related environmental contamination and the most effective interventions to address this mechanism of transmission, including recommendations for sink and plumbing system maintenance. Interventions that affect the placement of sinks in healthcare facilities must balance the impact on hand hygiene adherence of healthcare personnel with the risk for transmission from these sources.
ACKNOWLEDGMENTS
Financial support. None reported.
Footnotes
Previous presentation: CDC’s 2014 Epidemic Intelligence Service Conference; Atlanta, Georgia; May 1, 2014; and the 2014 Council of State and Territorial Epidemiologists’ Conference; Nashville, Tennessee; June 23, 2014 (Abstract #3255).
Potential conflicts of interest. All authors report no conflicts of interest relevant to this article.
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of CDC.
REFERENCES
- 1.Cruz AT, Cazacu AC, Allen CH. Pantoea agglomerans, a plant pathogen causing human disease. J Clin Microbiol 2007;45:1989–1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Christakis GB, Perlorentzou SP, Aslanidou M, Savva L, Zarkadis IK. Bacteremia caused by Pantoea agglomerans and Enterococcus faecalis in a patient with colon cancer. J BUON 2007;12: 287–290. [PubMed] [Google Scholar]
- 3.Cheng A, Liu CY, Tsai HY, et al. Bacteremia caused by Pantoea agglomerans at a medical center in Taiwan, 2000–2010. J Microbiol Immunol Infect 2013;46:187–194. [DOI] [PubMed] [Google Scholar]
- 4.Achkar MA, Rogers JS, Muszynski MJ. Pantoea species sepsis associated with sickle cell crisis in a pregnant woman with a history of pica. Am J Case Rep 2012;13:26–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong KW. Pantoea agglomerans as a rare cause of catheter-related infection in hemodialysis patients. J Vasc Access 2013;14:306. [DOI] [PubMed] [Google Scholar]
- 6.Habsah H, Zeehaida M, Van Rostenberghe H, et al. An outbreak of Pantoea spp. in a neonatal intensive care unit secondary to contaminated parenteral nutrition. J Hosp Infect 2005; 61:213–218. [DOI] [PubMed] [Google Scholar]
- 7.Bennett SN, McNeil MM, Bland LA, et al. Postoperative infections traced to contamination of an intravenous anesthetic, propofol. N Engl J Med 1995;333:147–154. [DOI] [PubMed] [Google Scholar]
- 8.Boszczowski I, Nóbrega de Almeida Júnior J, Peixoto de Miranda EJ, et al. Nosocomial outbreak of Pantoea agglomerans bacteraemia associated with contaminated anticoagulant citrate dextrose solution: new name, old bug? J Hosp Infect 2012;80:255–258. [DOI] [PubMed] [Google Scholar]
- 9.Arduino MJ, Bland LA, Tipple MA, et al. Growth and endotoxin production of Yersinia enterocolitica and Enterobacter agglomerans in packed erythrocytes. J Clin Microbiol 1989;27:1483–1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stenhouse MA. Enterobacter agglomerans as a contaminant of blood. Transfusion 1992;32:86. [DOI] [PubMed] [Google Scholar]
- 11.Petersen NJ, Collins DE, Marshall JH. A microbiological assay technique for hands. Health Lab Sci 1973;10:18–22. [PubMed] [Google Scholar]
- 12.US Pharmacopeial Convention. USP35-NF 30 Pharmaceutical compounding—sterile preparations. Rockville, MD: US Pharmacopeial Convention; 2012:350–387. [Google Scholar]
- 13.American Society of Health-System Pharmacists. ASHP guidelines on compounding sterile preparations. Am J Health-Syst Pharm 2014;71:145–166. [DOI] [PubMed] [Google Scholar]
- 14.Williams MM, Armbruster CR, Arduino MJ. Plumbing of hospital premises is a reservoir for opportunistically pathogenic microorganisms: a review. Biofouling 2013;29:147–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Decker BK, Palmore TN. The role of water in healthcare-associated infections. Curr Opin Infect Dis 2013;26:345–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haupt TE, Heffernan RT, Kazmierczak JJ, et al. An outbreak of Legionnaires disease associated with a decorative water wall fountain in a hospital. Infect Control Hosp Epidemiol 2012;332:185–191. [DOI] [PubMed] [Google Scholar]
- 17.Livni G, Yaniv I, Samra Z, et al. Outbreak of Mycobacterium mucogenicum bacteraemia due to contaminated water supply in a paediatric haematology-oncology department. J Hosp Infect 2008;70:253–258. [DOI] [PubMed] [Google Scholar]
- 18.Ashraf MS, Swinker M, Augustino KL, et al. Outbreak of Mycobacterium mucogenicum bloodstream infections among patientsm with sickle cell disease in an outpatient setting. Infect Control Hosp Epidemiol 2012;33:1132–1136. [DOI] [PubMed] [Google Scholar]
- 19.Kline S, Cameron S, Streifel A, et al. An outbreak of bacteremias associated with Mycobacterium mucogenicum in a hospital water supply. Infect Control Hosp Epidemiol 2004;25:1042–1049. [DOI] [PubMed] [Google Scholar]
- 20.Aumeran C, Paillard C, Robin F, et al. Pseudomonas aeruginosa and Pseudomonas putida outbreak associated with contaminated water outlets in an oncohaematology paediatric unit. J Hosp Infect 2007;65:47–53. [DOI] [PubMed] [Google Scholar]
- 21.Durojaiye OC, Carbarns N, Murray S, Majumdar S. Outbreak of multidrug-resistant Pseudomonas aeruginosa in an intensive care unit. J Hosp Infect 2011;78:154–155. [DOI] [PubMed] [Google Scholar]
- 22.Peterson AE, Chitnis AS, Xiang N, et al. Clonally related Burkholderia contaminans among ventilated patients without cystic fibrosis. Am J Infect Control 2013;41:1298–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lowe C, Willey B, O’Shaughnessy A, et al. Outbreak of extended-spectrum β-lactamase-producing Klebsiella oxytoca infections associated with contaminated handwashing sinks. Emerg Infect Dis 2012;18:1242–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vergara-López S, Domínguez MC, Conejo MC, Pascual Á, Rodríguez-Baño J.Wastewater drainage systemas an occult reservoir in a protracted clonal outbreak due to metallo-β-lactamase-producing Klebsiella oxytoca. Clin Microbiol Infect 2013;19:E490–E498. [DOI] [PubMed] [Google Scholar]
- 25.Hota S, Hirji Z, Stockton K, et al. Outbreak of multidrug-resistant Pseudomonas aeruginosa colonization and infection secondary to imperfect intensive care unit room design. Infect Control Hosp Epidemiol 2009;30:25–33. [DOI] [PubMed] [Google Scholar]
- 26.La Forgia C, Franke J, Hacek DM, Thomson RB Jr, Robicsek A, Peterson LR. Management of a multidrug-resistant Acinetobacter baumannii outbreak in an intensive care unit using novel environmental disinfection: a 38-month report. Am J Infect Control 2010;38:259–263. [DOI] [PubMed] [Google Scholar]
- 27.Decker BK, Palmore TN. Waterborne pathogen detection: more than just “location, location, location…”. Infect Control Hosp Epidemiol 2014;35:130–131. [DOI] [PubMed] [Google Scholar]
- 28.Hong KB, Oh HS, Song JS, et al. Investigation and control of an outbreak of imipenem-resistant Acinetobacter baumannii infection in a pediatric intensive care unit. Pediatr Infect Dis J 2012;31:685–690. [DOI] [PubMed] [Google Scholar]
- 29.Sehulster L, Chinn RY. Healthcare Infection Control Practices Advisory Committee. Guidelines for environmental infection control in health-care facilities. MMWR Recomm Rep 2003;52:1–42. [PubMed] [Google Scholar]
- 30.See I, Nguyen DB, Chatterjee S, et al. Outbreak of Tsukamurella species bloodstream infection among patients at an oncology clinic, West Virginia, 2011–2012. Infect Control Hosp Epidemiol 2014;35:300–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dobbs TE, Guh AY, Oakes P, et al. Outbreak of Pseudomonas aeruginosa and Klebsiella pneumoniae bloodstream infections at an outpatient chemotherapy center. Am J Infect Control 2014;42:731–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greeley RD, Semple S, Thompson ND, et al. Hepatitis B outbreak associated with a hematology-oncology office practice in New Jersey, 2009. Am J Infect Control 2011;39:663–670. [DOI] [PubMed] [Google Scholar]
- 33.Macedo deOliveira A, White KL, Leschinsky DP, et al. An outbreak of hepatitis C virus infections among outpatients at a hematology/oncology clinic. Ann Intern Med 2005;142:898–902. [DOI] [PubMed] [Google Scholar]
- 34.Watson JT, Jones RC, Siston AM, et al. Outbreak of catheter-associated Klebsiella oxytoca and Enterobacter cloacae bloodstream infections in an oncology chemotherapy center. Arch Intern Med 2005;165:2639–2643. [DOI] [PubMed] [Google Scholar]
- 35.Siegel JD, Rhinehart E, Jackson M, Chiarello L. Healthcare Infection Control Practices Advisory Committee. 2007 guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings. Centers for Disease Control and Prevention website. http://www.cdc.gov/hicpac/pdf/isolation/Isolation2007.pdf Published 2007 Accessed March 25, 2016.
- 36.Centers for Disease Control and Prevention (CDC). Outpatient settings policy options for improving infection prevention. CDC website. http://www.cdc.gov/hai/pdfs/prevent/Outpatient-Settings-Policy-Options.pdf Published October 2015 Accessed March 25, 2016.
- 37.Centers for Disease Control and Prevention (CDC). Infection control assessment tools. CDC website. http://www.cdc.gov/hai/prevent/infection-control-assessment-tools.html Updated January 15, 2016 Accessed March 25, 2016.
- 38.Joint Commission. Topic library item: “Joint Commission, CDC collaborating on ambulatory infection prevention project.” Joint Commission website. http://www.jointcommission.org/joint_commission_cdc_collaborating_on_ambulatory_infection_prevention_project/ Updated March 10, 2016 Accessed March 25, 2016.


