Abstract
The goal of this 21-year naturalistic study of clozapine-treated patients was to examine the cardiovascular risk factors following clozapine initiation and resultant mortality estimates from cardiovascular disease. Data were collected from January 1992 to February 2012 medical records from clozapine-treated patients with schizophrenia or schizoaffective disorder. Demographics, clozapine dosage and laboratory results were extracted at 12-month intervals. At clozapine initiation, the mean age of the 96 patients was 36.4 years±7.6 years; n=27 (28%) were women. The mean duration of clozapine use was 13 years. The Kaplan-Meier estimate for 21-year cardiovascular events was 29%, while the Kaplan-Meier estimate for 21-year mortality from cardiovascular disease was 10%. The mean cardiovascular risk increased during the first ten years (p<.01), while a slight decrease occurred beyond ten years (p<.01). Patients involved in cardiometabolic research showed a greater decrease in cardiovascular risk factors over 21 years (p=.05). The Kaplan-Meier estimate for 21-year all-cause mortality was 22%. Forty-one patients were diagnosed with diabetes (42.7%), compared to a nationwide prevalence of 13.7% in a similar age group. These results support the hypothesis that clozapine-treated patients are at risk for cardiovascular events and death secondary to an increased risk of medical disorders. Interventions that target weight loss, smoking cessation, and lipid profile improvement may alleviate the increased risk of cardiovascular mortality.
Keywords: Clozapine, Schizophrenia, Cardiovascular Risk, Diabetes, Mortality
Introduction
High rates of medical morbidity and increased risk of mortality have long been associated with schizophrenia, with a life expectancy that is reduced by 15–25 years (1–3). Schizophrenia has been associated with an increased risk of cardiovascular disease (4–7), and the metabolic risk factors associated with antipsychotics are of growing concern. A countrywide study in Denmark showed that while the mortality from heart disease decreased in the general population between 1994 and 2006, mortality from heart disease actually increased in patients with schizophrenia (8). Clozapine remains the treatment of choice for treatment-resistant schizophrenia, but there is growing concern related to the increased risk of weight gain, metabolic syndrome, and cardiotoxicity associated with its use.
Patients with schizophrenia have higher rates of obesity (9). Weight gain is a well-known side effect of antipsychotic treatment (10, 11). Clozapine, together with olanzapine, has the greatest potential to induce weight gain in patients with schizophrenia treated with antipsychotic medications (12, 13). In our five-year naturalistic study, we found that weight gain with clozapine did not plateau until the fourth year (14). In our 10-year naturalistic study we found that some patients experienced a second period of weight gain that occurred when they improved enough to leave structured environments, such as residential settings, to move to independent apartments. Results from this study showed an increased risk of cardiovascular mortality associated with increased BMI over time (15).
Obesity is a risk factor for the development of type 2 diabetes. There is an increased risk for type 2 diabetes in people with schizophrenia both before (16) and after exposure to antipsychotic drugs (17, 18). In our 10-year cohort study we found that thirty-three out of ninety-six patients on clozapine had developed diabetes mellitus; increased BMI, total cholesterol level, and triglyceride levels were risk factors (15). A recent study of adults with psychosis in Australia showed that clozapine was a risk factor for type 2 diabetes, but not after adjusting for other predictors of diabetes including body mass index and hypercholesterolemia (19). Reducing body weight and improving lipid profiles have been a focus of recent efforts to reduce the cardiovascular risk and improve the physical health of those with serious mental illness (20, 21).
Despite known differences in risk profiles for weight gain and metabolic side effects in patients treated with clozapine, an increased risk of cardiovascular disease has not been clearly established compared to patients treated with more weight-neutral antipsychotics. In an autopsy study of patients with schizophrenia, no difference was found in cardiac-related measures (atherosclerosis, fibrosis, and hypertrophy) between those treated with clozapine and those treated with risperidone (22). A large retrospective cohort study of 1,084 patients found that cardiovascular mortality in schizophrenia did not differ between clozapine and risperidone (23). However, in this same cohort there was a trend toward higher cardiovascular mortality with clozapine in patients who started antipsychotic treatment at an older age (>55) (23).
The goal of this 21-year naturalistic study of clozapine-treated patients was to examine the change in cardiovascular risk factors following clozapine initiation and resultant mortality estimates from cardiovascular disease.
Methods
Following institutional review board approval, records of 96 patients with schizophrenia or schizoaffective disorder (DSM-IV criteria) who had been treated with clozapine for up to 21 years from January 1992 to February 2012 at the Freedom Trail Clozapine Clinic were reviewed for known cardiovascular risk factors (24). Patients were excluded if they were treated with clozapine prior to joining the clinic and if their baseline data could not be obtained. Patients in the dataset were numbered 1–100. Only 96 patients had data (66 patients with schizophrenia and 30 patients with schizoaffective disorder). Cardiovascular risk was tabulated using known risk factors for cardiac heart disease (24) according to the following criteria: race (African American, Hispanic/Latino American, Asian American)=1 point; BMI ≥27 kg/m2=1 point; hypertension (systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg)=1 point; diabetes mellitus=1 point; cigarette smoking=1 point; history of left ventricular hypertrophy, myocardial infarction, or cerebrovascular accident=1 point; total cholesterol level ≥200 mg/dL or serum triglyceride level ≥150 mg/dL=1 point; and male gender=1 point (24). This is the same risk assessment used in our five-year (14) and ten-year (15) studies. Cardiovascular risk factors were tabulated at 1-year intervals over a 21-year period.
Autopsy reports and all medical records were reviewed by a research psychiatrist (D.C.H.) to determine the cause of death. When cardiovascular disease was identified, all records were carefully reviewed to determine if any evidence of clozapine-associated myocarditis or cardiomyopathy was present prior to the death such as persistent tachycardia, left ventricular hypertrophy, a prolonged corrected QT interval, eosinophilia, dyspnea on exertion, exercise intolerance, or edema. Patients with cerebrovascular accidents, myocardial infarctions, and symptomatic left ventricular hypertrophy were considered to have cardiovascular disease. This definition of cardiovascular disease was determined prior to study initiation.
Statistical Analysis
Baseline demographic and clinical characteristics were calculated for the sample. We then summarized the cardiovascular and metabolic events and related clinical characteristics that occurred in the sample over the 21-year follow-up period including the type of cardiovascular event, incidence of diabetes mellitus after clozapine initiation, and other demographic and clinical characteristics of these cases. Time to development of diabetes mellitus, cardiovascular disease, cardiovascular-related mortality and all-cause mortality associated with clozapine treatment at 12-month intervals over a 21-year period was calculated using Kaplan-Meier survival functions in Stata, Version 14.
To explore risk factor trajectories, we constructed mixed-effects models with a random intercept and slope for each patient as well as a fixed effect of time (in months) on the risk factors of interest: BMI, cardiovascular risk score, diabetes risk, weight, serum cholesterol level, serum triglyceride level and smoking status. The fixed effect estimates the mean trajectory of the change from baseline, and the random effects allow a separate trajectory for each patient. We then constructed a piecewise linear mixed-effect model to examine the difference in slope during the 2nd 10-year interval as compared to the first 10 years as reported in Henderson et al. (2005) (15). A plot of the mean number of cardiovascular risk factors and standard errors at each time point was produced using Stata, Version 14. We also evaluated whether research participation would moderate the trajectories of the aforementioned cardiovascular and metabolic risk factors over time by adding the main effect of research participation and an interaction term (research participation x time) to these longitudinal mixed-effect models.
Cox proportional hazards models were used to test the association between the aforementioned risk factors as well as key demographic characteristics and the development of the events of interest (incidence of diabetes, cardiovascular disease, cardiovascular-related mortality, all-cause mortality). Age, race, and sex were analyzed as fixed covariates, and BMI, total cholesterol level, clozapine total daily dose, serum triglyceride level, smoking status and weight were analyzed as time-varying covariates. Each covariate was analyzed separately. Time was used as the stratum and ties were handled using the exact partial likelihood method. All p-values are 2-tailed, and a p-value of .05 was considered evidence of statistical significance.
Results
Characteristics of the Sample
Baseline demographic and laboratory measures are presented in Table 1. Sixty-nine subjects (72%) were men and 27 (28%) were women. The mean age at clozapine initiation was 36.4±7.6 years; six subjects (6%) were African Americans, four (4%) were Hispanic Americans, and one (1%) was an Asian American. The mean length of treatment with clozapine was 13 years (mean 150.3 months; SD 68.1 months) ranging from 6–246 months. Some subjects initiated clozapine after their first assessment, while three discontinued early. Deaths also contributed to a shorter mean duration of clozapine treatment.
Table 1.
Demographic Characteristics and Baseline Values for 96 Patients with Schizophrenia Treated with Clozapine Over a 21-Year Period
| Variable | N (%) | Mean (SD) |
|---|---|---|
| Age | 36.4 (7.6) | |
| Gender | ||
| Male | 69 (72) | |
| Female | 27 (28) | |
| Race | ||
| White | 85 (89) | |
| African American | 6 (6) | |
| Hispanic American | 4 (4) | |
| Asian American | 1 (1) | |
| Diagnosis | ||
| Schizophrenia | 66 (69) | |
| Schizoaffective disorder | 30 (31) | |
| Smoking status | ||
| Smoker | 61 (63.5) | |
| Nonsmoker | 35 (36.5) | |
| Baseline measures | ||
| Weight, lb | 174.2 (35.5) | |
| Body mass index, kg/m2 | 27.3 (5.2) | |
| Glucose level, mg/dL | 93 (12) | |
| Blood pressure, mmHg | ||
| Systolic | 114 (13) | |
| Diastolic | 76 (9) | |
| Total cholesterol level, mg/dL | 196 (47) | |
| Serum triglyceride level, mg/dL | 180 (136) | |
| Cardiovascular risk factors | 2.0 | |
Cardiovascular risk was tabulated using the following criteria: race (African American, Hispanic/Latino American, Asian American)=1 point; BMI ≥27 kg/m2=1 point; hypertension (systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg)=1 point; diabetes mellitus=1 point; cigarette smoking=1 point; history of left ventricular hypertrophy, myocardial infarction, or cerebrovascular accident=1 point; total cholesterol level ≥200 mg/dL or serum triglyceride level ≥150 mg/dL=1 point; and male gender=1 point.
Time To Development of Diabetes Mellitus, Cardiovascular Disease, Cause-Specific (Cardiovascular-Related) Mortality and All-Cause Mortality
Diabetes Mellitus
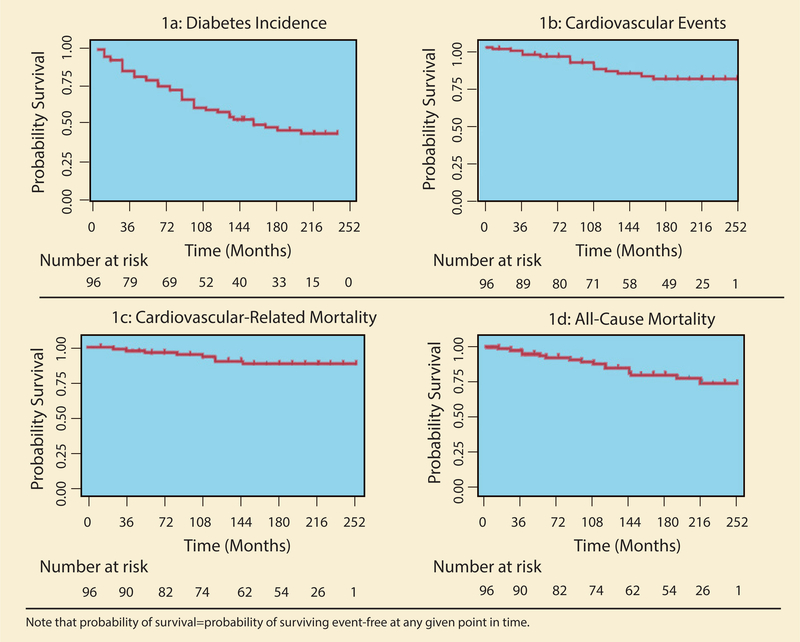
Forty-one patients were diagnosed with diabetes (42.7%) over the 21-year period. Thirty-three patients were diagnosed within 10 years of clozapine initiation, with an additional 8 diagnosed during the 10–21 year follow-up period. The probability of remaining diabetes free at the 10- and 21-year follow-up was 0.63 and 0.50, respectively (see Figure 1a; Table 2).
Figure 1. Time to Diabetes Incidence, Cardiovascular Events, Cardiovascular-Related Mortality, and All-Cause Mortality.
Note that probability of survival=probability of surviving event-free at any given point in time.
Table 2.
Survival Functions for Events of Interest (N=96)
| Event | Probability of Survival (Event-Free) |
Number of Events |
||
|---|---|---|---|---|
| 10-Year | 21-Year | 10-Year | 21-Year | |
| Incident Diabetes Mellitus | 0.630 | 0.503 | 33 | 8 |
| Cardiovascular Event | 0.858 | 0.811 | 12 | 3 |
| Cardiovascular-Related Mortality | 0.915 | 0.899 | 7 | 1 |
| All-Cause Mortality | 0.873 | 0.782 | 11 | 5 |
Cardiovascular Disease and Related Mortality
There were 17 cardiovascular events experienced by 15 patients (2 patients experienced 2 events each) during the 21-year period (see Table 3), with 4 of them occurring in the second decade. The Kaplan-Meier estimate for surviving without a cardiovascular event over the 10- and 21-year period was 0.86 and 0.81, respectively (see Figure 1b; Table 2). The Kaplan-Meier survival estimates for 10- and 21-year mortality from cardiovascular disease were 0.92 and 0.90, respectively (see Figure 1c; Table 2). One patient died secondary to a cardiovascular event in the second decade, while there were 7 cardiovascular deaths in the first decade after clozapine initiation.
Table 3.
Cardiovascular Events Over a 21-Year Period in Clozapine-Treated Patients
| Patient No. in Dataset | Patient Not in 10-Yr Paper | Duration of Clozapine Treatment, Months | ICD-9 Diagnosis | Gender | Cardiovascular Event | Race | Age at Time of Event, Year | Clozapine Dose (mg/d) | BMI (kg/m2) | Diabetes after Clozapine Initiation | Smoking Status |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 5 | 1 | 36 | 295.3 | Male | Non-fatal MI | White | 50 | 525 | 26.48 | No | Yes |
| 5 | 146 | 295.3 | Male | Fatal MI | White | 57 | |||||
| 8 | 132 | 295.7 | Male | Non-fatal CVA | White | 37 | 500 | 36 | Yes | ||
| 9 | 11 | 84 | 295.9 | Male | Non-fatal CVA | White | 45 | 400 | 17 | Yes | Yes |
| 18 | 54 | 295.3 | Female | Fatal CVD | White | 59 | |||||
| 19 | 2 | 108 | 295.9 | Male | Non-fatal MI | White | 49 | 450 | 35 | Yes | Yes |
| 23 | 108 | 295.3 | Female | Non-fatal LVH | White | 50 | 500 | No | Yes | ||
| 23 | 6 | 120 | 295.3 | Female | Fatal MI | White | 51 | 500 | 51 | No | Yes |
| 26 | 84 | 295.3 | Male | Fatal MI | White | 50 | 550 | 26 | No | Yes | |
| 30 | 156 | 295.7 | Male | Non-fatal MI | White | 63 | 500 | 26 | No | Yes | |
| 35 | 6 | 295.3 | Male | Non-fatal LVH | White | 27 | 400 | 27 | No | No | |
| 37 | 36 | 295.3 | Female | Fatal CVD | White | 45 | 125 | 31 | Yes | Yes | |
| 70 | 160 | 295.7 | Female | Non-fatal LVH | White | 38 | 550 | 35 | Yes | No | |
| 75 | 8 | 108 | 295.7 | Male | Fatal CVD | Hispanic | 29 | 43 | Yes | Yes | |
| 79 | 4 | 24 | 295.3 | Female | Fatal CVD | African American | 26 | 175 | 39 | Yes | No |
| 94 | 120 | 295.3 | Male | Fatal MI | White | 49 | 27 | No | Yes | ||
| 98 | 3 | 84 | 295.1 | Female | Non-fatal MI | White | 42 | 350 | 29 | No | Yes |
ICD: International classification of diseases; 295.1: disorganized type schizophrenia; 295.3: paranoid type schizophrenia; 295.7: schizoaffective disorder; 295.9: unspecified schizophrenia; BMI: Body Mass Index; CVA: cerebrovascular accident; CVD: MI cardiovascular disease; MI: myocardial infarction; LVH: left ventricular hypertrophy; MVI: multivitamin.
All-Cause Mortality
The probability of survival was 0.87 and 0.78 at 10 and 21 years, respectively (see Figure 1d; Table 2). The majority of deaths occurred during the first decade (n=11) as compared to the second decade (n=5). Five patients, ages 47–54, died from cancer-related causes, two of which were lung cancer related. The remaining causes of death included cardiovascular disease (n=8), perforated bowel (n=1) and unknown causes (n=2).
Cardiovascular and Metabolic Risk Trajectories
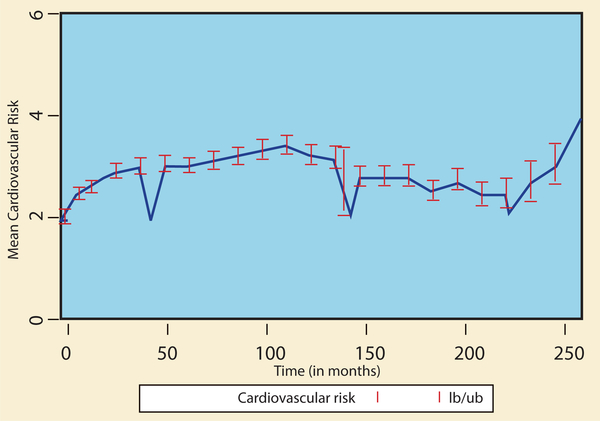
There was a significant increase in weight, BMI, diabetes risk and cardiovascular risk factors over the 21-year period, and an overall decrease in cholesterol levels (p<.001). While there was no significant overall change in serum triglyceride levels over the 21-year period, there was a significant decrease in triglyceride levels during the 2nd decade (linear coefficient of −1.1 mg/dL/month, SE=0.423, p=0.007). Results from the piecewise linear models suggest that the increases in cardiovascular risk (see Figure 2), cholesterol, triglycerides and weight were significantly attenuated during the 2nd decade relative to the first decade of the study. Probability of smoking did not change over time (see Table 4). Patients who were involved in metabolic research studies showed a decrease in cardiovascular risk factors, including decreased cholesterol (p=0.049), triglycerides (p=0.007) and weight (p=0.057) over a 21-year period compared to those who were not involved in research.
Figure 2.
Mean Cardiovascular Risk (±SE) for 96 Patients on Clozapine
Table 4.
The Effect of Time (Slope) on CVD and Metabolic Risk Factors
| DV: | Months 0–120 |
Months 121–252 |
Months 0–252 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | z | p | B | SE | z | p | B | SE | z | p | |
| BMI* | 0.027 | 0.004 | 6.73 | <.001 | −0.011 | 0.006 | −1.87 | 0.061 | 0.018 | 0.004 | 4.69 | <.001 |
| Cardiovascular Risk* | 0.009 | 0.001 | 8.67 | <.001 | −0.009 | 0.001 | −6.19 | <.001 | 0.004 | 0.001 | 3.88 | <.001 |
| Cholesterol | −0.152 | 0.052 | −2.93 | 0.003 | −0.348 | 0.128 | −2.71 | 0.007 | −0.188 | 0.044 | −4.26 | <.001 |
| Diabetes Risk | 0.012 | 0.001 | 10.27 | <.001 | 0.009 | 0.012 | 0.74 | 0.456 | 0.012 | 0.001 | 10.36 | <.001 |
| Triglycerides* | 0.195 | 0.167 | 1.17 | 0.241 | −1.143 | 0.423 | −2.70 | 0.007 | −0.102 | 0.121 | −0.84 | 0.399 |
| Weight* | 0.169 | 0.025 | 6.64 | 0.000 | −0.082 | 0.038 | −2.15 | 0.032 | 0.110 | 0.024 | 4.57 | 0.000 |
| Smoking Status (Y/N) | −0.001 | 0.002 | −0.95 | 0.344 | 0.004 | 0.004 | 1.09 | 0.274 | 0.001 | 0.002 | 0.33 | 0.745 |
Cardiovascular risk was tabulated using the following criteria: race (African American, Hispanic/Latino American, Asian American)=1 point; BMI ≥27 kg/m2=1 point; hypertension (systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg)=1 point; diabetes mellitus=1 point; cigarette smoking=1 point; history of left ventricular hypertrophy, myocardial infarction or cerebrovascular accident=1 point; total cholesterol level ≥200 mg/dL or serum triglyceride level ≥150 mg/dL=1 point; and male gender=1 point.
Effect of time (slope) is significantly different between the first and second decade.
Association Between Demographic and Cardiometabolic Risk Factors and Incidence of Diabetes, Cardiovascular Disease, Cardiovascular-Related Mortality and All-Cause Mortality
Demographic factors (age, sex and race) were not related to cardiovascular events, cardiovascular-related mortality or all-cause mortality. As compared to Caucasians, African Americans (HR=11.4, 95% CI: 3.6, 36.4) and Hispanics (HR=3.7, 95% CI: 1.0, 13.2) were more likely to develop diabetes mellitus over the follow-up period. Moreover, the hazard of diabetes was also greater for individuals with higher body mass index (BMI; HR=1.11, 95% CI: 1.1, 1.2). Lastly, having diabetes mellitus was associated with experiencing a cardiovascular event (HR=3.8, 95% CI: 1.3, 11.4) and all-cause mortality (HR=3.94, 95% CI: 1.2, 13.0). All other cardiometabolic risk factors (cholesterol, triglycerides, blood pressure, clozapine dose, smoking status) were not significantly associated with the events of interest. See Table 5.
Table 5.
Hazard of Experiencing Events of Interest During the 21-Year Follow-Up Period by Demographic and Clinical Covariates
| Diabetes Incidence |
Cardiovascular Events |
Cardiovascular-Related Mortality |
All-Cause Mortality |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | HR | 95% CI | p | |
| Age (in years) | 1.01 | 0.97, 1.05 | 0.660 | 1.00 | 0.93, 1.07 | 0.957 | 1.03 | 0.93, 1.14 | 0.571 | 1.07 | 0.99, 1.15 | 0.090 |
| African American (ref: White) | 11.44 | 3.59, 36.39 | 0.000 | 1.33 | 0.17, 10.36 | 0.784 | 2.92 | 0.35, 24.54 | 0.323 | 2.99 | 0.66, 13.48 | 0.155 |
| Hispanic (ref: White) | 3.69 | 1.03, 13.15 | 0.044 | 2.02 | 0.26, 16.00 | 0.504 | 5.01 | 0.59, 42.91 | 0.141 | 2.25 | 0.29, 17.53 | 0.437 |
| Male | 1.08 | 0.54, 2.18 | 0.829 | 0.77 | 0.26, 2.28 | 0.642 | 0.36 | 0.09, 1.46 | 0.155 | 0.48 | 0.18, 1.30 | 0.150 |
| BMI | 1.11 | 1.05, 1.18 | 0.000 | 0.98 | 0.89, 1.07 | 0.594 | 1.14 | 1.00, 1.29 | 0.051 | 1.04 | 0.95, 1.15 | 0.397 |
| Cholesterol | 1.00 | 0.99, 1.01 | 0.882 | 1.00 | 0.98, 1.01 | 0.692 | 1.00 | 0.96, 1.03 | 0.756 | 0.99 | 0.98, 1.01 | 0.314 |
| Triglycerides | 1.00 | 1.00, 1.00 | 0.073 | 0.99 | 0.99, 1.00 | 0.242 | 1.00 | 0.99, 1.01 | 0.685 | 1.00 | 1.00, 1.00 | 0.826 |
| Systolic Blood Pressure | 1.01 | 0.99, 1.04 | 0.245 | 1.01 | 0.97, 1.05 | 0.619 | 1.02 | 0.97, 1.08 | 0.353 | 1.02 | 0.98, 1.07 | 0.292 |
| Diastolic Blood Pressure | 1.01 | 0.98, 1.05 | 0.536 | 1.02 | 0.96, 1.07 | 0.590 | 1.09 | 1.00, 1.18 | 0.059 | 1.07 | 1.00, 1.14 | 0.067 |
| Clozapine Dose | 1.00 | 1.00, 1.00 | 0.696 | 1.00 | 1.00, 1.00 | 0.889 | 1.00 | 0.99, 1.00 | 0.247 | 1.00 | 0.99, 1.00 | 0.222 |
| Smoking Status | 1.20 | 0.61, 2.36 | 0.597 | 1.92 | 0.52, 7.04 | 0.324 | 2.97 | 0.35, 25.55 | 0.321 | 1.10 | 0.33, 3.68 | 0.875 |
| Diabetes Mellitus | -- | -- | -- | 3.78 | 1.26, 11.36 | 0.018 | 3.85 | 0.75, 19.92 | 0.108 | 3.94 | 1.20, 12.96 | 0.024 |
Discussion
Clozapine is the only antipsychotic medication approved for treatment-resistant schizophrenia, but its use is often limited due to its adverse cardiometabolic risk profile. In addition to the low risk of myocarditis and cardiomyopathy (25, 26), clozapine is known to induce weight gain and may contribute to the risk of developing diabetes mellitus and other metabolic abnormalities (27–29). These risks are of particular concern in a population that is already predisposed to cardiovascular disease (30, 31) and metabolic dysfunction (32, 33).
Our results support the hypothesis that clozapine-treated patients are at risk for cardiovascular events and death secondary to clozapine-associated medical disorders such as obesity, diabetes, and hyperlipidemia. Fifteen of the 96 patients in our cohort (15.6%) experienced a cardiovascular event over a 21-year period, with eight patients dying from a cardiac event. While data on the 21-year risk of cardiovascular events in a healthy population of the same age are not available, the 30-year risk of a cardiovascular event in patients age 20–29 is 2.5% for women and 5% for men (34). A significant increase in BMI, weight, and cardiovascular risk factors was seen over the 21-year period. Forty-three percent of patients were diagnosed with diabetes mellitus—far more than would be expected based on the nationwide prevalence of 13.7% in those ages 45–64 (35).
Most of the risk for cardiovascular morbidity and mortality was engendered during the first decade of our study. Increased BMI, cardiovascular risk, triglycerides, and weight seen during the first 10 years were significantly attenuated during the second decade. There was, in fact, a decrease in cardiovascular risk factors in the second decade. This was paralleled by lower rates of cardiovascular events and death. The probability of smoking remained relatively consistent over the 21-year period. While rates of smoking in schizophrenia are known to be 2–3 times higher than the general population (36), risk of tobacco use is lower in patients treated with clozapine (37). Our data set did not include quantity of tobacco use within the subset of patients who smoked, but there is evidence that smokers decrease their daily use of cigarettes after clozapine initiation (38).
The reason for the decline in rates of cardiovascular morbidity, mortality, and risk factors in the second decade relative to the first is likely multifactorial. The rapid weight gain seen within the first three months of treatment with clozapine has been reported to increase at a slower rate for a year or longer and eventually plateau (39, 40). In our cohort, we observed an increase in weight during the first decade that was associated with the development of diabetes mellitus and cardiovascular mortality, followed by a leveling off of BMI during the second decade. Additionally, clinicians have become increasingly vigilant for the cardiometabolic side effects of antipsychotic medication during recent years. Patients who were enrolled in metabolic research studies in our cohort had a decrease in cardiovascular risk factors compared to those who were not. These patients were often enrolled in studies that included dietary and lifestyle interventions and were seen by clinicians regularly. While it is possible that there were baseline differences between these groups—including functional status and disease severity—the only difference in cardiovascular disease risk factors between the groups was a higher baseline cholesterol level in the research group.
The number of cancer-related deaths in our sample was alarming. Five patients, ages 48–54, passed away from cancer. Two of these patients had lung cancer and three of these patients had widely metastatic disease of unknown source. Population-based studies from several countries have shown that individuals with schizophrenia are 1.5 to 2 times more likely to die of cancer than patients without mental illness (41–43). Contributing factors at the level of the patient, the provider, and the healthcare system likely influence this increase in mortality (44). In a large Swedish study, cancer mortality in schizophrenia patients was primarily explained by under detection—despite the fact that these patients had increased contacts with the healthcare system (41). The relationship between antipsychotic use and cancer has not been examined, though antipsychotic continuity has been associated with overall decreased mortality (45).
There are several limitations to the current study. First, it is possible that other unknown factors affected the rates of cardiovascular events and development of diabetes mellitus. These include family history, diet and exercise habits, and frequency of healthcare screening. In addition, there are measures that are now known to be associated with increased cardiovascular risk, including low HDL cholesterol, and measures known to be associated with increased metabolic risk, including increased waist circumference, which were not included in our database as they were not recognized as major risk factors when data collection was started. Many patients participated in interventions that may have reduced the overall incidence of new-onset diabetes or cardiovascular death in this cohort. Finally, although medical records and autopsy reports were carefully reviewed, it is possible that undetected cardiomyopathy or myocarditis contributed to the cardiovascular deaths.
Schizophrenia is associated with high rates of medical comorbidity and mortality associated with cardiovascular disease and metabolic dysfunction, and this risk may be compounded by the use of atypical antipsychotic medications including clozapine. An increased risk of cardiovascular events, mortality, and development of diabetes was seen in this cohort of patients over a 21-year period. This risk was highest in the first decade. Screening and interventions that target weight loss, smoking cessation, and lipid profile improvement may mitigate the increased risk of cardiovascular morbidity and mortality associated with clozapine use. Increased vigilance with regards to cancer screening and detection is necessary for this high-risk population.
Acknowledgment
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Footnotes
Conflict of Interests
None declared.
References
- 1.Brown S Excess mortality of schizophrenia. A meta-analysis. Br J Psychiatry 1997;171:502–508. [DOI] [PubMed] [Google Scholar]
- 2.Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis 2006;3(2):A42. [PMC free article] [PubMed] [Google Scholar]
- 3.Hennekens CH, Hennekens AR, Hollar D, Casey DE. Schizophrenia and increased risks of cardiovascular disease. Am Heart J 2005;150(6):1115–1121. doi: 10.1016/j.ahj.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 4.De Hert M, Dekker JM, Wood D, Kahl KG, Holt RI, Moller HJ. Cardiovascular disease and diabetes in people with severe mental illness position statement from the European Psychiatric Association (EPA), supported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC). Eur Psychiatry 2009;24(6):412–424. doi: 10.1016/j.eurpsy.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 5.Fleischhacker WW, Cetkovich-Bakmas M, De Hert M, Hennekens CH, Lambert M, Leucht S, et al. Comorbid somatic illnesses in patients with severe mental disorders: clinical, policy, and research challenges. J Clin Psychiatry 2008;69(4):514–519. [DOI] [PubMed] [Google Scholar]
- 6.Leucht S, Burkard T, Henderson J, Maj M, Sartorius N. Physical illness and schizophrenia: a review of the literature. Acta Psychiatr Scand 2007;116(5):317–333. doi: 10.1111/j.1600-0447.2007.01095.x. [DOI] [PubMed] [Google Scholar]
- 7.Mitchell AJ, Malone D. Physical health and schizophrenia. Curr Opin Psychiatry 2006;19(4):432–437. doi: 10.1097/01.yco.0000228767.71473.9e. [DOI] [PubMed] [Google Scholar]
- 8.Laursen TM, Nordentoft M. Heart disease treatment and mortality in schizophrenia and bipolar disorder - changes in the Danish population between 1994 and 2006. J Psychiatr Res 2011;45(1):29–35. doi: 10.1016/j.jpsychires.2010.04.027. [DOI] [PubMed] [Google Scholar]
- 9.Saarni SE, Saarni SI, Fogelholm M, Heliovaara M, Perala J, Suvisaari J, et al. Body composition in psychotic disorders: a general population survey. Psychol Med 2009;39(5):801–810. doi: 10.1017/S0033291708004194. [DOI] [PubMed] [Google Scholar]
- 10.Marder SR, Essock SM, Miller AL, Buchanan RW, Casey DE, Davis JM, et al. Physical health monitoring of patients with schizophrenia. Am J Psychiatry 2004;161(8):1334–1349. doi: 10.1176/appi.ajp.161.8.1334. [DOI] [PubMed] [Google Scholar]
- 11.Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet 2009;373(9657):31–41. doi: 10.1016/S0140-6736(08)61764-X. [DOI] [PubMed] [Google Scholar]
- 12.Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante MC, et al. Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry 1999;156(11):1686–1696. [DOI] [PubMed] [Google Scholar]
- 13.Newcomer JW. Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs 2005;19 Suppl 1:1–93. [DOI] [PubMed] [Google Scholar]
- 14.Henderson DC, Cagliero E, Gray C, Nasrallah RA, Hayden DL, Schoenfeld DA, et al. Clozapine, diabetes mellitus, weight gain, and lipid abnormalities: A five-year naturalistic study. Am J Psychiatry 2000;157(6):975–981. [DOI] [PubMed] [Google Scholar]
- 15.Henderson DC, Nguyen DD, Copeland PM, Hayden DL, Borba CP, Louie PM, et al. Clozapine, diabetes mellitus, hyperlipidemia, and cardiovascular risks and mortality: results of a 10-year naturalistic study. J Clin Psychiatry 2005;66(9):1116–1121. [DOI] [PubMed] [Google Scholar]
- 16.Cohen D, De Hert M. Endogenic and iatrogenic diabetes mellitus in drug-naive schizophrenia: the role of olanzapine and its place in the psychopharmacological treatment algorithm. Neuropsychopharmacology 2011;36(11):2368–2369. doi: 10.1038/npp.2011.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nielsen J, Skadhede S, Correll CU. Antipsychotics associated with the development of type 2 diabetes in antipsychotic-naive schizophrenia patients. Neuropsychopharmacology 2010;35(9):1997–2004. doi: 10.1038/npp.2010.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yood MU, DeLorenze G, Quesenberry CP Jr, Oliveria SA, Tsai AL, Willey VJ, et al. The incidence of diabetes in atypical antipsychotic users differs according to agent--results from a multisite epidemiologic study. Pharmacoepidemiol Drug Saf 2009;18(9):791–799. doi: 10.1002/pds.1781. [DOI] [PubMed] [Google Scholar]
- 19.Foley DL, Mackinnon A, Morgan VA, Watts GF, McGrath JJ, Castle DJ, et al. Predictors of type 2 diabetes in a nationally representative sample of adults with psychosis. World Psychiatry 2014;13(2):176–183. doi: 10.1002/wps.20130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Daumit GL, Dickerson FB, Wang NY, Dalcin A, Jerome GJ, Anderson CA, et al. A behavioral weight-loss intervention in persons with serious mental illness. N Engl J Med 2013;368(17):1594–1602. doi: 10.1056/NEJMoa1214530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yarborough BJ, Leo MC, Stumbo S, Perrin NA, Green CA. STRIDE: a randomized trial of a lifestyle intervention to promote weight loss among individuals taking antipsychotic medications. BMC Psychiatry 2013;13:238. doi: 10.1186/1471-244X-13-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kelly DL, Wehring HJ, Linthicum J, Feldman S, McMahon RP, Love RC, et al. Cardiac-related findings at autopsy in people with severe mental illness treated with clozapine or risperidone. Schizophr Res 2009;107(2–3):134–138. doi: 10.1016/j.schres.2008.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kelly DL, McMahon RP, Liu F, Love RC, Wehring HJ, Shim JC, et al. Cardiovascular disease mortality in patients with chronic schizophrenia treated with clozapine: a retrospective cohort study. J Clin Psychiatry 2010;71(3):304–311. doi: 10.4088/JCP.08m04718yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilson PW, Culleton BF. Epidemiology of cardiovascular disease in the United States. Am J Kidney Dis 1998;32(5 Suppl 3):S56–65. [DOI] [PubMed] [Google Scholar]
- 25.Merrill DB, Dec GW, Goff DC. Adverse cardiac effects associated with clozapine. J Clin Psychopharmacol 2005;25(1):32–41. [DOI] [PubMed] [Google Scholar]
- 26.Wehmeier PM, Heiser P, Remschmidt H. Myocarditis, pericarditis and cardiomyopathy in patients treated with clozapine. J Clin Pharm Ther 2005;30(1):91–96. doi: 10.1111/j.1365-2710.2004.00616_1.x. [DOI] [PubMed] [Google Scholar]
- 27.Ahmed M, Hussain I, O’Brien SM, Dineen B, Griffin D, McDonald C. Prevalence and associations of the metabolic syndrome among patients prescribed clozapine. Ir J Med Sci 2008;177(3):205–210. doi: 10.1007/s11845-008-0156-9. [DOI] [PubMed] [Google Scholar]
- 28.Lamberti JS, Olson D, Crilly JF, Olivares T, Williams GC, Tu X, et al. Prevalence of the metabolic syndrome among patients receiving clozapine. Am J Psychiatry 2006;163(7):1273–1276. doi: 10.1176/appi.ajp.163.7.1273. [DOI] [PubMed] [Google Scholar]
- 29.Wirshing DA. Schizophrenia and obesity: impact of antipsychotic medications. J Clin Psychiatry 2004;65 Suppl 18:13–26. [PubMed] [Google Scholar]
- 30.Gladigau EL, Fazio TN, Hannam JP, Dawson LM, Jones SG. Increased cardiovascular risk in patients with severe mental illness. Intern Med J 2014;44(1):65–69. doi: 10.1111/imj.12319. [DOI] [PubMed] [Google Scholar]
- 31.Ifteni P, Correll CU, Burtea V, Kane JM, Manu P. Sudden unexpected death in schizophrenia: autopsy findings in psychiatric inpatients. Schizophr Res 2014;155(1–3):727–726. doi: 10.1016/j.schres.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 32.Dasgupta A, Singh OP, Rout JK, Saha T, Mandal S. Insulin resistance and metabolic profile in antipsychotic naive schizophrenia patients. Prog Neuropsychopharmacol Biol Psychiatry 2010;34(7):1202–1207. doi: 10.1016/j.pnpbp.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 33.Thakore JH. Metabolic disturbance in first-episode schizophrenia. Br J Psychiatry Suppl 2004;47:S76–79. [DOI] [PubMed] [Google Scholar]
- 34.Pencina MJ, D’Agostino RB Sr, Larson MG, Massaro JM, Vasan RS. Predicting the 30-year risk of cardiovascular disease: the Framingham heart study. Circulation 2009;119(24):3078–3084. doi: 10.1161/CIRCULATIONAHA.108.816694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Center for Disease Control and Prevention. 2011 National Diabetes Fact Sheet 2011. [cited 2014 6 Jun]. Available from: http://www.cdc.gov/diabetes/pubs/estimates11.html.
- 36.de Leon J, Diaz FJ. A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophr Res 2005;76(2–3):135–157. Epub 2005/06/14. doi: 10.1016/j.schres.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 37.Wijesundera H, Hanwella R, de Silva VA. Antipsychotic medication and tobacco use among outpatients with schizophrenia: a cross-sectional study. Ann Gen Psychiatry 2014;13(1):7. doi: 10.1186/1744-859x-13-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.George TP, Sernyak MJ, Ziedonis DM, Woods SW. Effects of clozapine on smoking in chronic schizophrenic outpatients. J Clin Psychiatry 1995;56(8):344–346. Epub 1995/08/01. [PubMed] [Google Scholar]
- 39.Bai YM, Chen JY, Chen TT, Lin CY, Chou P, Su TP, et al. Weight gain with clozapine: 8-year cohort naturalistic study among hospitalized Chinese schizophrenia patients. Schizophr Res 2009;108(1–3):122–126. doi: 10.1016/j.schres.2008.10.023. [DOI] [PubMed] [Google Scholar]
- 40.Pai N, Deng C, Vella SL, Castle D, Huang XF. Are there different neural mechanisms responsible for three stages of weight gain development in anti-psychotic therapy: temporally based hypothesis. Asian J Psychiatr 2012;5(4):315–318. doi: 10.1016/j.ajp.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 41.Crump C, Winkleby MA, Sundquist K, Sundquist J. Comorbidities and mortality in persons with schizophrenia: a Swedish national cohort study. Am J Psychiatry 2013;170(3):324–333. doi: 10.1176/appi.ajp.2012.12050599. [DOI] [PubMed] [Google Scholar]
- 42.Guan NC, Termorshuizen F, Laan W, Smeets HM, Zainal NZ, Kahn RS, et al. Cancer mortality in patients with psychiatric diagnoses: a higher hazard of cancer death does not lead to a higher cumulative risk of dying from cancer. Soc Psychiatry Psychiatr Epidemiol 2013;48(8):1289–1295. doi: 10.1007/s00127-012-0612-8. [DOI] [PubMed] [Google Scholar]
- 43.Kisely S, Sadek J, MacKenzie A, Lawrence D, Campbell LA. Excess cancer mortality in psychiatric patients. Can J Psychiatry 2008;53(11):753–761. [DOI] [PubMed] [Google Scholar]
- 44.Irwin KE, Henderson DC, Knight HP, Pirl WF. Cancer care for individuals with schizophrenia. Cancer 2014;120(3):323–334. doi: 10.1002/cncr.28431. [DOI] [PubMed] [Google Scholar]
- 45.Cullen BA, McGinty EE, Zhang Y, Dosreis SC, Steinwachs DM, Guallar E, et al. Guideline-concordant antipsychotic use and mortality in schizophrenia. Schizophr Bull 2013;39(5):1159–1168. doi: 10.1093/schbul/sbs097. [DOI] [PMC free article] [PubMed] [Google Scholar]