Abstract
Purpose: To determine the prevalence and underlying pathology of abnormal glucose homeostasis in Chinese patients with non-transfusion-dependent thalassemia (NTDT).
Patients and methods: In this study, we enrolled 211 patients aged 4–63 years with NTDT, including 79 β thalassemia intermedia patients, 114 Hb H disease patients and 18 Hb E/β thalassemia patients. All had oral glucose tolerance test, serum ferritin (SF), homeostasis model assessment (HOMA) and liver iron concentration (LIC) measurement. One hundred and twenty healthy age-matched controls were also used for the comparative purpose. Iron load was assessed by using SF and hepatic load by LIC using validated MRI techniques.
Results: The 211 patients were divided into three groups according to their fasting and 2 hrs postprandial blood glucose levels: hypoglycemic, normal glucose tolerance (NGT) and hyperglycemic groups. In this study, 149 patients had NGT, 33 had hypoglycemia, 4 had diabetes and 25 had impaired glucose tolerance (IGT). None had impaired fasting glucose. There was a significant correlation between 2 hrs postprandial blood glucose levels and age, PINS120, HOMA-IR, alanine aminotransferase and LIC (P<0.05). Risk factors for IGT in NTDT patients were older age (≥24 years) and SF concentration of ≥2,500 ng/mL.
Conclusion: Age ≥24 years and SF ≥2,500 ng/mL of NTDT patients were at a greater risk for impaired glucose tolerance.
Keywords: glucose homeostasis, non-transfusion-dependent thalassemia, liver iron overload, postprandial hyperglycemia
Introduction
Thalassemia is the commonest monogenic global disorder which results from a defect in the synthesis of the globin chain.1,2 It constitutes a significant health-care burden with marked morbidity and mortality in South East (SE) Asia, Middle East, Africa and a public health problem with drainage of health-care resources.1,2 In China, the prevalence of thalassemia in the southern regions (such as Yunnan, Guangdong, Guangxi, Fujian and Sichuan provinces) is particularly high.3
Thalassemia can be divided into: transfusion-dependent thalassemia (TDT) and non-transfusion-dependent thalassemia (NTDT). NTDT usually encompasses three clinical subtypes β thalassemia intermedia (β-TI), Hb H disease and Hb E/β thalassemia with significant phenotypic heterogeneity.1 These patients do not need a blood transfusion for survival unlike thalassemia major (TM), but may require occasional or even frequent transfusion to prevent or treat organ damage. Hemoglobin levels in these patients remain mostly between 7 and 10 g/dL.4
NTDT patients have clinical symptoms after adulthood, including growth retardation, thalassemia-related skeletal deformities, splenomegaly, moderate and severe hepatomegaly.5 Glycaemic disorders including diabetes have been studied comprehensively in TM and TI patients.4,6 The prevalence of diabetes mellitus (DM) and impaired glucose tolerance (IGT) in β-TI patients varied from 1.7% to 2% and 2.9% to 24%.4,5 It is shown that DM in β-TI patients is mainly due to decreased insulin secretion and insulin resistance.7 Iron overload in liver and muscle can cause insulin resistance, which plays a crucial part in abnormal glucose homeostasis.
Hence we undertook this prospective case-controlled cross-sectional study to understand the prevalence and pathophysiology of glycemic disorders in relation to anemia and hepatic iron overload in a cohort of NTDT in three subsets (β-TI, Hb H and Hb E/β patients in Southern China). This information is mandatory for better understanding and management including prevention of diabetes in NTDT.
Patients and methods
This was a cross-sectional study of all NTDT patients registered at the hematology department of the First Affiliated Hospital of Guangxi Medical University, China. The study followed the ethical standards outlined in the Declaration of Helsinki, and was approved by the Medical Ethics Committee of the First Affiliated Hospital of Guangxi Medical University. All patients or their legal guardians provided written informed consent to participate. These samples included 211 patients with NTDT and 120 healthy controls from April 2013 to October 2016.
All patients received blood transfusions or chelation therapy irregularly. Subjects with a history of cancer, known liver disease were excluded from the study. Methods on glycemic markers and iron load were validated and were described in our previously published work.8 A physical examination of the subjects was performed, and medical history was recorded in detail. Age, gender, weight and height were recorded in the clinic. Body mass index (BMI) was calculated as body weight in kilograms divided by height in meters squared.
After at least 8 hrs of overnight fasting, we measured plasma glucose concentration, fructosamine, aspartate aminotransferase (AST), alanine aminotransferase (ALT), albumin, insulin and serum ferritin levels by collecting blood samples early in the next morning. All participants underwent a standard 2 hrs OGTT test. Blood samples were drawn at 30 and 120 mins after the subjects drank 300 mL of warm water containing 75 g of anhydrous glucose in order to determine glucose concentrations and serum insulin levels. These measurements were made within 5 mins of obtaining the blood samples. The glucose intake of children should be 1.75 g per kilogram of body weight to a maximum of 75 g.9
Homoeostasis model assessment was used to assess basal beta cell secretory function and systemic insulin resistance. The early phase insulinogenic index (IGI30) was an indicator of early insulin secretion.10 The delayed phase insulinogenic index (IGI120) was an indicator of late insulin secretion. We also calculated the area under the curve of total insulin secretion (AUC-I). The above indices were calculated using the following formulae:11
Plasma glucose and fructosamine were determined by the glucose oxidase method (Hitachi 7600 automated biochemical analyzer, Hitachi, Japan). Serum insulin and ferritin levels were measured using a human insulin radioimmunoassay (Beckman Coulter access analyzer, California, United States). Liver iron concentrations (LICs) were measured by MRI examination and the results were expressed as mg/g dry weight. However, we did not measure pancreas T2* because its value was not always measured routinely during clinical examinations. We collected the LIC from 103 of the patients.
According to the diabetes diagnostic criteria of the World Health Organization in 1999, the diagnosis of glucose metabolism disorders was as follows:9 NGT was defined as fasting blood glucose (FBG) <6.1 mmol/L and 2 hrs postprandial blood glucose (PBG120) <7.8 mmol/L; impaired fasting glucose(IFG) was defined as 6.1≤ FBG <7.0 mmol/L and PBG120<7.8 mmol/L; IGT was defined as FBG <7.0 mmol/L and 7.8≤ PBG120<11.1 mmol/L; and diabetes was defined as FBG ≥7.0 mmol/L and (or) PBG120≥11.1 mmol/L. Hypoglycemia was defined as FBG <2.8 mmol/L. The above diagnosis was based on two blood glucose test results. The clinically relevant thresholds of patients treated with deferasirox were shown as below: threshold to guide chelator dose interruption was defined as SF <300 ng/mL or LIC <3 mg Fe/g dw; the initiation of chelation therapy was defined as SF >800 ng/mL or LIC ≥7 mg Fe/g dw; and dose escalation was defined as SF ≥2,500 ng/mL or LIC ≥15 mg Fe/g dw.12 LIC ≥3 mg Fe/g dw and SF ≥300 ng/mL were considered as iron overload.
Statistical analysis was performed by using SPSS 22.0. Normally distributed data were expressed as average±SD, and non-normally distributed data were expressed as median (IQR) range. The nonparametric Kruskal–Wallis H test was used to analyze the independent variables. Spearman correlation was used to test the relationship between markers of iron overload and other variables. Multivariate analysis was performed using the stepwise logistic regression analysis to calculate odds ratios (ORs) with 95% confidence interval (CI) for the independent risk factors. Statistically significant differences were set at bilateral P-values<0.05.
Results
Patient characteristics
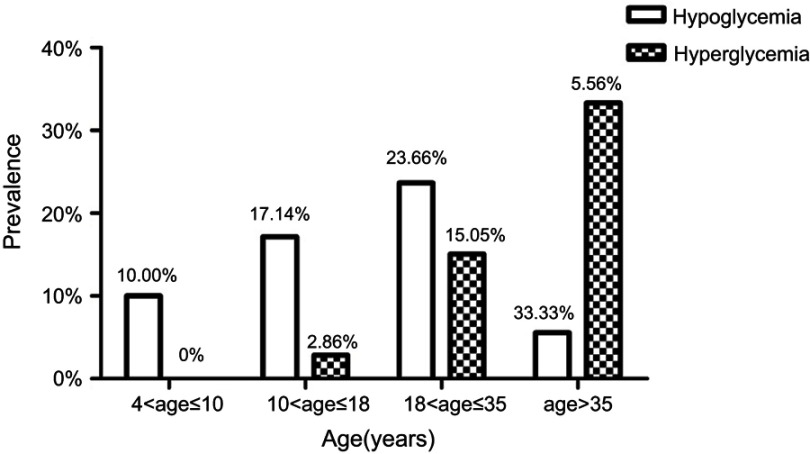
The clinical and physiological characteristics of the 211 patients with NTDT (including 79 β-TI, 114 Hb H and 18 Hb E/β patients) and the control subjects in this study are shown in Table 1. There were 31 patients with HbH disease had Constant Spring mutation. There were 115 (54.50) male patients and 96 (45.50) female patients. The average age of the patients was 24.31 years (range: 4–63 years). Weights and BMI of NTDT patients were significantly lower than those of controls. Thalassemia patients have separated the following age groups: 4–10 years; 10–18 years; 18–35 years; 35–50 years and >50 years. The prevalence of hyperglycemia gradually increased with age (Figure 1). According to the type of disease, patients were divided into two subgroups: E/beta thalassemia plus beta thalassemia intermedia as one subgroup, and Hb H disease as the other.
Table 1.
Clinical and physiological characteristics of patients with nontransfusion-dependent thalassemia and control subjects
| Variables | TI (n=211) | Control (n=120) | P-value | |
|---|---|---|---|---|
| β-TI and Hb E/β (n=97) | Hb H (n=114) | |||
| Disease, n (%) | ||||
| β thalassaemia intermedia | 79 (37.44) | |||
| Hb H disease | 114 (54.03) | |||
| Hb E/β thalassaemia | 18 (8.53) | |||
| Male: female, n (%) | 54 (55.67): 43 (44.33) | 61 (53.51): 53 (46.49) | 67 (55.83): 53 (44.17) | |
| Mean age ± SD, years | 22.93±11.18 | 23.63±13.29 | 23.98±12.71 | |
| Age category, n (%) | ||||
| 4–≤10 years | 18 (18.56) | 21 (18.42) | 20 (16.67) | |
| >10–≤18 years | 16 (16.49) | 25 (21.92) | 24 (20.00) | |
| >18–≤35 years | 48 (49.48) | 48 (42.11) | 52 (43.33) | |
| >35–≤50 years | 14 (14.43) | 17 (14.91) | 22 (18.33) | |
| >50 years | 1 (1.03) | 3 (2.63) | 2 (1.67) | |
| Mean height ± SD, cm | 151.48±19.78 | 149.47±18.75 | 148.51±13.84 | |
| Mean weight ± SD, kg | 44.13±14.82 | 43.14±14.45 | 45.97±9.86 | * |
| Mean BMI ± SD, kg/m2 | 18.60±3.39 | 18.60±3.23 | 20.97±1.71 | * |
| Median LIC (IQR, range) mg/g | 13.70 (14.30, 0.60–43.00) | 7.70 (12.58, 0.60–43.00) | ||
| LIC category, n (%) | ||||
| <3 mg/g | 3 (5.66) | 12 (24.00) | ||
| ≥3–≤7 mg/g | 12 (2.26) | 12 (24.00) | ||
| >7–≤15 mg/g | 18 (33.96) | 12 (24.00) | ||
| >15 mg/g | 20 (37.74) | 14 (28.00) | ||
| Median serum ferritin (IQR, range) ng/mL |
922.00 (1455.44, 26.88–8,300.00) | 564.51 (985.93, 30.75–7,440.78) | ||
| Serum ferritin category, n (%) | ||||
| <300 ng/mL | 15 (15.79) | 29 (26.85) | ||
| ≥300–≤800 ng/mL | 26 (27.37) | 39 (36.11) | ||
| >800–≤2,500 ng/mL | 37 (38.95) | 30 (27.78) | ||
| >2,500 ng/mL | 17 (17.89) | 10 (9.26) | ||
| Liver function | ||||
| Median AST(IQR, range), U/L | 30.50 (21.00, 13.00–122.00) | 29.00 (20.00, 13.00–96.00) | ||
| Median ALT (IQR, range), U/L | 20.00 (29.75, 4.00–120.00) | 29.00 (20.00, 13.00–96.00) | ||
| Median ALB (IQR, range), g/L | 47.00 (4.37, 35.60–49.30) | 47.40 (5.00, 27.00–50.00) | ||
| Glucose homeostasis | ||||
| Median FBG (IQR, range), mmol/L | 3.63 (1.07, 1.39–7.42) | 3.79 (1.49, 1.98–5.60) | 4.52 (0.76, 1.25–6.80) | * |
| Median PBG30 (IQR, range), mmol/L | 6.73 (1.94, 3.03–11.05) | 7.33 (2.76, 2.10–12.51) | ||
| Median PBG120 (IQR, range), mmol/L | 5.73 (1.92, 2.73–10.20) | 5.74 (1.73, 2.65–14.03) | ||
| Median FINS (IQR, range), pmol/L | 27.71 (27.18, 1.75–197.30) | 27.52 (28.44, 4.64–164.50) | 32.74 (29.42, 5.12–138.70) | |
| Median PINS30 (IQR, range), pmol/L | 213.30 (196.15, 24.19–1,292.00) | 194.85 (261.06, 13.89–1224.00) | ||
| Median PINS120 (IQR, range), pmol/L | 130.60 (201.44, 12.86–806.40) | 133.00 (178.74, 14.62–1196.00) | ||
| Median FA (IQR, range), umol/L | 193.00 (51.00, 90.00–300.00) | 188.00 (54.00, 106.00–364.67) | ||
| Median HOMA-IR (IQR, range) | 0.67 (0.62, 0.04–4.73) | 0.66 (0.71, 0.08–4.37) | 0.89 (0.87, 0.12–4.86) | * |
| Median HOMA-B (IQR, range) | 196.11 (30.89, 11.42–1,664.51) | 136.09 (183.40, 3.51–1596.55) | 82.30 (95.35, 14.09–632.19) | * |
| Median ISI (IQR, range) | 0.07 (0.07, 0.01–0.33) | 0.07 (0.07, 0.01–0.38) | 0.89 (1.05, 0.01–4.82) | * |
| Median IGI30 (IQR, range) | 0.45 (0.50, 0.01–2.70) | 0.38 (0.62, 0.01–2.85) | ||
| Median IGI120 (IQR, range) | 0.37 (0.57, 0.01–3.59) | 0.37 (0.48, 0.01–4.72) | ||
| Median AUC-I (≤120 mins) (IQR, range) | 303.26 (371.35, 36.92–1,953.08) | 326.43 (404.74, 54.78–1785.73) | ||
Notes: LIC is measured in mg Fe/g dw; serum ferritin is measured in ng/mL; *P<0.05.
Abbreviations: TI, thalassemia intermedia; dw, dry weight; LIC, liver iron concentration; SD, standard deviation; IQR, interquartile range; BMI, body mass index; AST, aspartate aminotransferase; ALT, alanine aminotransferase; ALB, albumin; AUC-I, area under the curve of total insulin secretion; FBG, fasting blood glucose; PBG30, half-hour postprandial blood glucose; PBG120, 2 hrs postprandial blood glucose; FINS, fasting insulin; PINS30, half-hour postprandial insulin; PINS120, 2 hrs postprandial insulin; FA, fructosamine; HOMA-IR, homeostatic model assessment of insulin resistance; HOMA-β, homeostatic model assessment beta cell function; ISI, insulin sensitivity index; IGI30, early phase insulinogenic index; IGI120, delayed phase insulinogenic index.
Figure 1.
The percentage of patients with abnormal glucose homeostasis in nontransfusion-dependent thalassemia according to age distribution.
Glucose metabolism
In the NTDT group, 149/211 (70.62%) patients had normal glucose tolerance (NGT), 33/211 (15.64%) patients had hypoglycemia, 4/211 (1.90%) patients had diabetes and 25/211 (11.85%) patients had IGT. None of them had IFG. In the control group, none had IFG, IGT or diabetes. In the NTDT group, the median HOMA-B was higher than those in the control group, and the median ISI was higher than those in the control group. The 211 patients with NTDT were divided into three groups according to their fasting and 2 hrs postprandial blood glucose levels: hypoglycemic, NGT and hyperglycemic groups (IFG, IGT, DM). As Table 2 shows, the hyperglycemic group had higher age, height, weight and BMI compared with the NGT group (P<0.01).
Table 2.
Characteristics of nontransfusion-dependent thalassemia patients according to the presence of disorders of glucose metabolism
| Parameters | NGT (n=149) | Hypoglycemia (n=33) | Hyperglycemia (n=29) | P-value |
|---|---|---|---|---|
| Age (years)a | 21.44±12.29 | 22.79±8.10 | 33.50±11.89*,# | <0.001 |
| Height (cm)a | 146.95±20.59 | 158.91±13.32* | 158.24±10.73* | 0.004 |
| Weight (kg)a | 40.57±14.82 | 48.38±10.75 | 53.58±11.20* | <0.001 |
| BMI (kg/m2)a | 18.02±3.27 | 18.86±2.21 | 21.29±3.15*,# | <0.001 |
| FBG (mmol/L)b | 3.92 (1.08) (2.83,5.67) | 2.43 (0.43) (1.39,2.76)* | 3.88 (1.73) (2.70,7.42)# | <0.001 |
| PBG30 (mmol/L)b | 6.89 (1.93) (2.10,10.96) | 6.19 (2.62) (3.20,8.91) | 9.42 (1.42) (5.86,12.51)*,# | <0.001 |
| PBG120 (mmol/L)b | 5.62 (1.67) (2.65,7.68) | 5.17 (1.66) (2.73,7.52) | 8.81 (1.64) (6.73,14.03)*,# | <0.001 |
| FINS (pmol/L)b | 28.09 (27.11) (1.75,193.80) | 22.42 (18.15) (3.77,113.30) | 34.40 (53.25) (6.76,197.30) | 0.212 |
| PINS30 (pmol/L)b | 182.30 (259.71) (13.89,1292.00) | 257.47 (182.58) (35.00,823.10) | 211.50 (251.70) (54.57,1036.00) | 0.458 |
| PINS120 (pmol/L)b | 112.90 (156.19) (12.86,962.90) | 109.70 (184.00) (19.28,1016.00) | 272.85 (279.35) (84.96,1196.00)*,# | <0.001 |
| HOMA-IRb | 0.70 (0.60) (0.04,4.44) | 0.34 (0.34) (0.06,1.90)* | 0.81(1.46) (0.19,4.73)# | <0.001 |
| HOMA-βb | 187.40 (258.92) (11.42,1664.51) | 59.02 (65.42) (12.03,373.96)* | 160.67 (217.43) (3.51,1322.33)# | <0.001 |
| ISIb | 0.06 (0.05) (0.01,0.38) | 0.13 (0.11) (0.02,0.35)* | 0.06 (0.08) (0.01,0.23)# | <0.001 |
| IGI30b | 0.45 (0.71) (0.01,2.85) | 0.43 (0.46) (0.04,2.70) | 0.29 (0.36) (0.07,1.11)* | 0.029 |
| IGI120b | 0.36 (0.66) (0.01,4.72) | 0.40 (0.46) (0.01,2.37) | 0.42 (0.47) (0.07,3.56) | 0.773 |
| AUC-I (≤120 mins)b | 276.22 (381.73) (36.92,1785.73) | 369.70 (230.58) (64.60,1472.85) | 456.50 (535.11) (138.75,1953.08)* | 0.039 |
| FA (umol/L)b | 190.00 (55.00) (90.00,280.00) | 195.00 (154.00) (133.00,251.00) | 181.50 (63.75) (133.00,364.67) | 0.632 |
| SF (ng/mL)b | 680.23 (1284.00) (27.15,7440.78) | 652.55 (1097.00) (161.55,6130.07) | 1108.00 (2955.71) (26.88,8300.00)*,# | 0.012 |
| LIC (mg Fe/g dw)b | 9.05 (14.48) (0.60,43.00) | 8.75 (9.15) (0.80,35.30) | 17.10 (31.30) (5.80,43.00)*,# | 0.003 |
| AST (U/L)b | 28.00 (20.00) (13.00,119.00) | 30.00 (9.00) (13.00,84.00) | 34.00 (23.00) (18.00,122.00) | 0.178 |
| ALT (U/L)b | 18.00 (24.50) (4.00,120.00) | 17.00 (15.00) (5.00,101.00) | 26.00 (30.00) (9.00,76.00)* | 0.034 |
| ALB (g/L)b | 47.00 (4.17) (35.00,67.30) | 49.40 (3.67) (41.50,68.00)* | 46.90 (4.05) (27.00,52.00)# | 0.002 |
Notes: *P<0.05, compared with the NGT group; #P<0.05 compared with the hypoglycemia group; a expressed as average ± SD; b expressed as median (IQR)(range).
Abbreviations: BMI, body mass index; ALT, alanine aminotransferase; AST, aspartate aminotransferase; ALB, albumin; AUC-I, area under the curve of total insulin secretion; SF, serum ferritin; FBG, fasting blood glucose; PBG30, half-hour postprandial blood glucose; PBG120, 2 hr postprandial blood glucose; FINS, fasting insulin; PINS30, half-hour postprandial insulin; PINS120, 2 hr postprandial insulin; FA, fructosamine; HOMA-IR, homeostatic model assessment of insulin resistance; HOMA-β, homeostatic model assessment beta cell function; ISI, insulin sensitivity index; IGI30, early phase insulinogenic index; IGI120, delayed phase insulinogenic index; LIC, liver iron concentration.
Patients in the hyperglycemic group had higher PINS120, AUC-I, SF, LIC and ALT than those in the NGT group (P<0.05). IGI30 in the hyperglycemic group was lower than those in the NGT group (P<0.05). The hypoglycemic group had lower HOMA-IR and HOMA-B compared with the NGT and hyperglycemic groups (P<0.01). There was no significant difference in fructosamine, fasting insulin (FINS) and IGI120 between the three groups.
In the NTDT group, 4/211 (1.90%) patients had diabetes, including two women and two men. They were between 35 and 50 years old, all suffering from HbH disease, and the BMI of them were in the normal range. Two of them had LIC≥15 mg/g and SF≥2,500 ng/mL and received blood transfusion and chelation therapy. The other two patients had LIC and SF in the normal range and received irregular chelation therapy, with no history of blood transfusion. Only one of the four patients had a family history of diabetes.
Iron metabolism
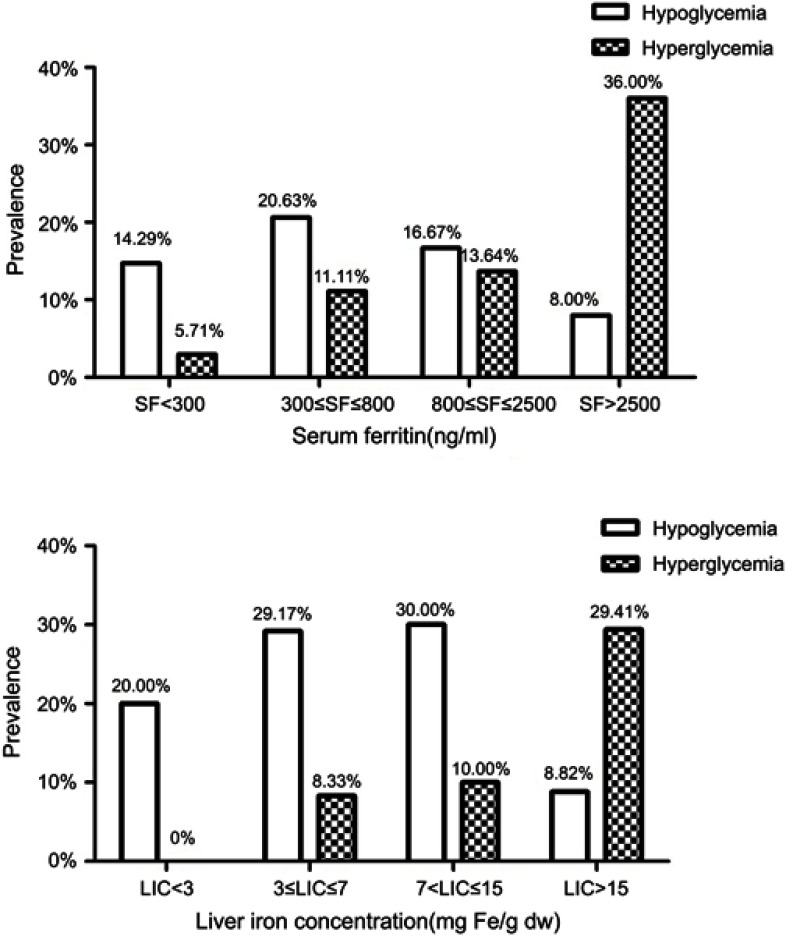
In 203 patients with NTDT, the median SF was 707.00 ng/mL. 44/203 (21.67%) patients had normal serum ferritin, 65/203 (32.02%) patients had serum ferritin levels of 300–800 ng/mL, 67/203 (33.00%) patients had serum ferritin levels of 800–2,500 ng/mL and 27/203 (13.30%) patients had serum ferritin levels higher than 2,500 ng/mL. In the 103 patients with NTDT, the median LIC was 10.30 mg/g, in which 15/103 (14.56%) had normal LIC, 24/103 (23.30%) patients had LIC levels of 3–7 mg/g, 30/103 (29.13%) patients had LIC levels of 7–15 mg/g and 34/103 (33.01%) patients had LIC levels higher than 15 mg/g. Hb H disease group had decreased serum ferritin and LIC compared with Hb E/β plus β-TI group. However, no significant differences were found in glucose metabolism between them. With the increase of serum ferritin and LIC, the proportion of hyperglycemic patients showed a gradual increase (Figure 2).
Figure 2.
The percentage of patients with abnormal glucose homeostasis in nontransfusion-dependent thalassemia with according to their serum ferritin levels (SF) and liver iron concentrations (LIC).
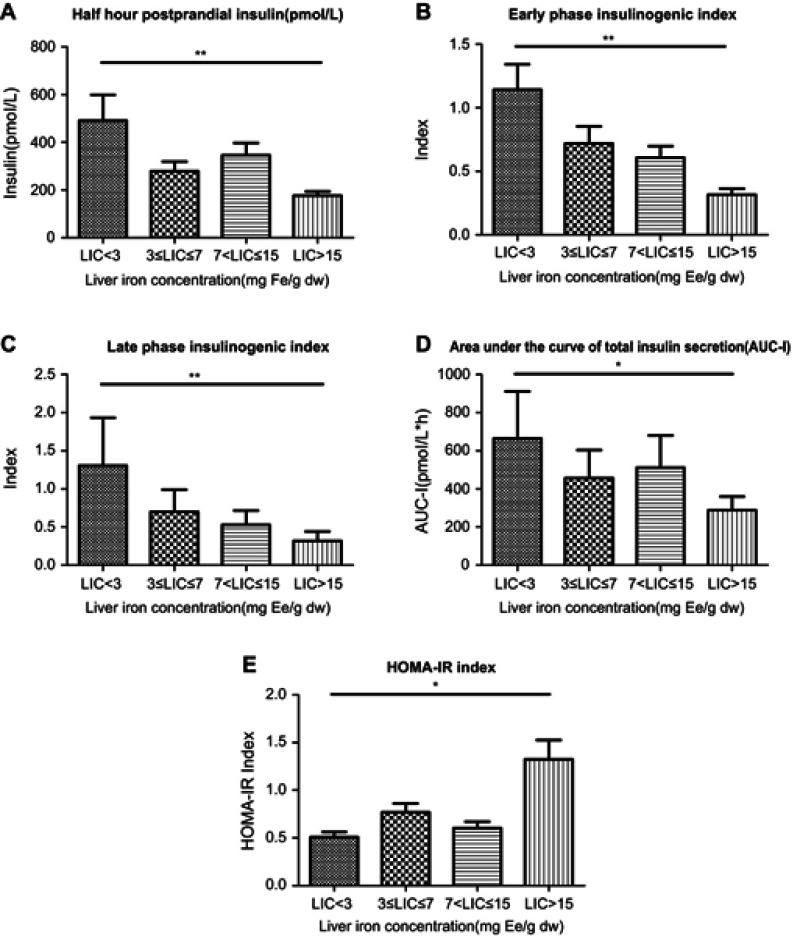
PINS30, IGI30, IGI120 and AUC-I was lower in LIC≥15 mg/g group than in LIC<3 mg/g group (P<0.05). There was no significant difference in FBG, FA and HOMA-B between the three groups (Figure 3).
Figure 3.
Compare (A) half-hour postprandial insulin (PINS30); (B) early phase insulinogenic index (IGI30); (C) late phase insulinogenic index (IGI120); (D) area under the curve of total insulin secretion (AUC-I) and (E) HOMA-IR index in nontransfusion-dependent thalassemia patients according to levels of LIC. *P<0.05, **P<0.01.
Relationship between 2 hrs postprandial glucose levels and other variables
There was a significant correlation between 2 hrs postprandial blood glucose levels and age (r=0.49; P<0.01), 2 hrs postprandial insulin levels (r=0.55; P<0.01), HOMA-IR index (r=0.17; P<0.05), ISI (r=−0.19; P<0.05), AUC-I (r=0.30; P<0.01), LICs (r=0.30; P<0.01) and ALT levels (r=0.15; P<0.05; Figure 4).
Figure 4.

Correlation between 2 hrs postprandial glucose and (A) age (r=0.49; P<0.01); (B) 2 hrs postprandial insulin (r=0.55; P<0.01); (C) HOMA-IR index (r=0.17; P<0.05); (D) insulin sensitivity index (r=−0.19; P<0.05); (E) alanine aminotransferase (r=0.15; P<0.05); (F) liver iron concentration (r=0.30; P<0.01); (G) area under the curve of total insulin secretion (AUC-I) (r=0.30; P<0.01) in nontransfusion- dependent thalassemia patients.
Risk factors for IGT in NTDT patients
Stepwise logistic regression analysis was used to calculate the ORs with 95% CI for the independent risk factors. This showed that age of ≥24 years (OR 14.94; 95% CI 1.60 to 139.35; P<0.05) and serum ferritin levels of ≥2,500 ng/mL (OR 8.13; 95% CI 1.45 to 45.55; P<0.05) had independent effects on the IGT observed in the NTDT subjects (Table 3).
Table 3.
Odds ratios for clinical and demographic factors associated with abnormal glucose homeostasis in nontransfusion dependent thalassemia patients
| Variables | Hyperglycemia | Hypoglycemia | ||
|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | |
| Age (≥24 years) | 14.94 (1.60–139.35) | 0.018* | 1.01 (0.35–2.90) | 0.993 |
| Serum ferritin (≥2,500 ng/mL) | 8.13 (1.45–45.55) | 0.017* | 0.33 (0.03–3.62) | 0.329 |
| Serum ALT (>50IU/L) | 1.03 (0.15–7.04) | 0.973 | 0.64 (0.12–3.34) | 0.643 |
| LIC (≥15 mg Fe/g dw) | 1.60 (0.38–6.61) | 0.519 | 0.39 (0.10–1.57) | 0.386 |
Note: *P<0.050.
Abbreviations: CI, confidence interval; OR, odds ratio; ALT, alanine transaminase; LIC, liver iron concentration.
Discussion
This was the first study which aimed at evaluation of the prevalence and underlying cause of abnormal glucose homeostasis in Chinese patients with NTDT. The results of this study indicated that 15.64% of patients with NTDT had hypoglycemia, 1.90% of patients had diabetes and 11.85% of patients had IGT.
DM is one of the endocrine complications of thalassemia major patients.13 Pancreatic iron overload occurs in children with thalassemia major in the early days of the disease.14 In China, the data on glucose metabolism disorders in TDT is diverse. A study involving 57 transfusion-dependent β-TM patients from Sun Yat-sen Memorial Hospital showed that 7% with β-TM was diagnosed with DM, and 24% had impaired fasting glucose.15 A study of 200 children with alpha-thalassemia discovered that DM was identified in 14 patients and 71.4% of them were 6 years old with no significant difference identified between males and females.16 In our previous study of adolescent, TM patients we found that the overall prevalence of diabetes and IFG in thalassaemic children under 18 years was 2% and 30%, respectively.8
Glucose tolerance abnormalities and DM are common complications in NTDT patients.5 In Milan, Baldini et al, found that only two had IGT and one had diabetes in a study of 70 β-TI adult patients.10 Taher et al, conducted a study of 584 thalassemia intermedia patients from six countries including Lebanon, Italy, Iran, Egypt, United Arab Emirates and Oman and reported that the mean age was 24.39±12.24 years, with the prevalence of diabetes being 1.7%.17 The prevalence of diabetes in patients with NTDT in this study was similar to those found outside China. But it occurred at a very early age as young as 8 years unlike the European and Middle Eastern patients, due primarily to hepatic siderosis. Our results indicated that, except for DM, abnormal glucose metabolism in NTDT patients was characterized by hypoglycemia and IGT, which has not been reported before. This might be related to the irregular blood transfusions or chelation therapy in Chinese subjects. The specific mechanism needs to be further studied.
Our data also suggested that there was an age-dependent increase in glycemic disorders in the age group of 24.39 years (range: 4–63 years). However, the youngest with IGT was only 8 years old which was novel. We have previously published data in a similar cohort of TM adolescents under 18 years with glycaemic disorders.8 Interestingly in our previous study of adolescent patients with transfusion-dependent thalassemia major, we found a very high incidence of diabetes and IGT, and patients were affected as early as 3 years.8
Little was known about IGT in NTDT children as young as 8 years of age. His father also suffered from beta thalassemia intermedia and IGT. The BMI of this child was 17.8, which was normal but close to the overweight threshold. Moreover, literature in Chinese patients was sparse. The exact reason for IGT in the 8-year-old NTDT patient was speculative. Family history and potential obesity may be the main causes. But iron load with hepatic siderosis and hypoxia might also be contributors. The LIC level and hemoglobin level in this patient was 12.1 mg Fe/g and 85 g/L, respectively. This was very worrying as it could be to be a forerunner of diabetes in due course. It was known that IGT may be reversible with intensified chelation therapy. In a previous study, we also showed that DFP-treated patients had a lower prevalence of abnormal glucose homeostasis.8 It was speculative that during the process of pancreatic siderosis, once the pancreas became atrophic, the process became irreversible. IGT probably could be ameliorated by strict diabetic diet, appropriate weight reduction and intensive chelation therapy (monotherapy or dual therapy with deferoxamine (DFO) and DFP).18 It was proposed that with DFP regime, full blown DM could be preventable more as siderosis is a slow process in NTDT. Therefore, early diagnosis and proper treatment are important in the younger patient population with NTDT.
The cause of abnormal glucose metabolism in thalassemia was not yet fully understood. Patients with β-thalassemia major were shown to have insulin resistance and β-cell dysfunction.19 In addition, decreased insulin sensitivity and IGT with hyperinsulinemia can contribute to insulin resistance in these patients.13,19 Tangvarasittichai et al observed that insulin resistance was associated positively with oxidative stress as measured by increased concentrations of MDA among the β-TM patients.20 Insulin deficiency secondary to iron-induced pancreatic β-cell defects was another possible cause of glucose abnormalities.19,21,22 NTDT patients lacked regular blood transfusions, but ineffective erythropoiesis and chronic hemolysis would cause the inhibition of hepcidin, resulting in an increase in the intestinal compensatory absorption of iron, eventually leading to body iron overload.23 Iron accumulation occurred more slowly in NTDT patients compared to TDT patients, and complications did not arise until later in life.24 Iron overload increased with age and was more common in patients who received transfusions.25 In patients with TM, most of the iron from the blood transfusion was distributed in the reticuloendothelial system and parenchyma, while in NTDT patients iron was mainly accumulated in the liver cells.26 Under-expression of hepcidin resulted in body iron overload, which triggered the production of reactive oxygen species simultaneously thought to play a major role in diabetes pathogenesis mediated both by β-cell failure and insulin resistance.27
The mechanism of the iron load is likely to be associated with gastro-intestinal (GI) absorption. With increased GI absorption of iron, iron overload occurs late in NTDT patients, leading to a series of complications linked to endocrine disorders including glucose metabolism disorder,4,8 adrenal insufficiency,28 vitamin D deficiency and low bone mass.29,30 It is known that abnormal glucose homeostasis is a fairly common complication of this disease.6 However, unlike Italian, Middle Eastern European18 and other cohorts who were affected at a late stage in life, we have shown that Chinese children and adolescents are more vulnerable.
We cannot measure iron deposition in the pancreas, but hepatic siderosis can indirectly reflect iron content in the visceral organ. In this study, with the aggravation of liver iron deposition, PINS30, IGI30, IGI120 and AUC-I levels were further reduced, HOMA-IR index was increased. Therefore, pancreatic iron overload can reduce early phase insulin secretion and increase insulin resistance, leading to postprandial hyperglycemia. Our findings suggested that the independent risk factors for IGT found in NTDT patients were the age of ≥24 years and serum ferritin levels of ≥2,500 ng/mL, which was similar to other findings.31
Iron overload was associated closely with the incidence of hyperglycemia. Iron overload can cause elevated blood glucose in patients with thalassemia intermedia, resulting in the development of IGT or diabetes. The mechanism for iron overload leading to IGT and diabetes is still unknown. Iron overload can cause insulin resistance and decreased pancreatic β-cell secretion. There was a positive correlation between iron overload, oxidative stress and insulin resistance in patients with β-TM.20 Excessive iron deposition in the liver and muscles due to iron overload leads to impaired insulin-mediated glucose uptake and utilization and peripheral insulin resistance. At the same time, iron deposition in pancreatic β cells decreased the early phase insulin secretion, induces increased apoptosis and promotes the occurrence of diabetes.13 Due to the expansion of erythrocytes, inhibition of hepcidin production resulted in the increased iron release from macrophages and increased intestinal iron absorption, leading eventually to iron overload in the liver.32
In this study, with the increase of serum ferritin and LIC, the proportion of hyperglycemic patients showed a gradual increase. In the patients with SF≥2,500 ng/mL or LIC≥15 mg Fe/g dw group, the prevalence of hyperglycemia was significantly higher than in patients with SF<300 ng/mL or LIC<3 mg Fe/g dw. PINS30, IGI30, IGI120 and AUC-I were lower in patients with LIC≥15 mg/g than in those with LIC<3 mg/g (P<0.05). Musallam et al, demonstrated that patients with an LIC≥5 mg/g have a significantly higher prevalence of several serious vascular and endocrine/bone morbidities than patients with LIC<5 mg/g.33 A study from six racial/ethnic groups of 97,470 participants has shown that serum ferritin levels are significantly associated with diabetes, even though levels are lower than those associated with hemochromatosis or iron overload.34 Chern et al, also found that serum ferritin concentration was one of the risk factors for abnormal glucose tolerance in thalassemia intermedia.35 Karimi et al, discovered that serum ferritin levels were correlated negatively with T2 hepatic MRI and correlated positively with LIC in the patients with thalassemia intermedia.36 Our finding is consistent with previous studies in children and adolescents with thalassemia.
Over the past decade, our understanding of the molecular features, pathophysiology and complications of NTDT particularly β-TI has increased tremendously. The clinical manifestations and complications of β–TI are unique and different from well-treated β-TM patients but are similar to β-TM patients who are poorly transfused. Hence, it is plausible that the manifestation of TI is due to dyserythropoiesis. The triad of chronic anemia, ineffective erythropoiesis, and iron overload characterizes NTDT and is mostly responsible for its clinical sequelae.37,38
We recognized that one of the limitations of our study was the lack of cardiac and pancreatic iron values, but since MRI testing was not a routine examination in our hospital and expenditure of MRI was high, majority of the patients were unwilling to undergo this test.
Conclusion
In summary, our data suggested that the high prevalence of abnormal blood glucose in patients with NTDT could be attributed to increase insulin resistance and insufficient insulin secretion secondary to iron overload. Furthermore, the severity of IGT and diabetes was proportional to the severity of iron overload. It could affect patients at a very young age of 8 years.
Acknowledgment
This work was supported by research grants from Guangxi Scientific Research and Technology Development Plan Project (Grants No. 1598011-1) and the Guangxi Natural Science Foundation (Grant No. 2017GXNSFDA198010).
Disclosure
The authors report no conflicts of interests in this work.
References
- 1.Weatherall DJ. The definition and epidemiology of non-transfusion-dependent thalassemia. Blood Rev. 2012;26(Suppl 1):S3–S6. doi: 10.1016/S0268-960X(12)70003-6 [DOI] [PubMed] [Google Scholar]
- 2.De Sanctis V, Kattamis C, Canatan D, et al. beta-Thalassemia distribution in the old world: an ancient disease seen from a historical standpoint. Mediterr J Hematol Infect Dis. 2017;9(1):e2017018. doi: 10.4084/mjhid.2017.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lai K, Huang G, Su L, He Y. The prevalence of thalassemia in mainland China: evidence from epidemiological surveys. Sci Rep. 2017;7(1):920. doi: 10.1038/s41598-017-00967-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baldini M, Marcon A, Cassin R, et al. Beta-thalassaemia intermedia: evaluation of endocrine and bone complications. Biomed Res Int. 2014;2014:174581. doi: 10.1155/2014/174581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Inati A, Noureldine MA, Mansour A, Abbas HA. Endocrine and bone complications in beta-thalassemia intermedia: current understanding and treatment. Biomed Res Int. 2015;2015:813098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Sanctis V, Soliman AT, Elsedfy H, et al. Diabetes and glucose metabolism in thalassemia major: an update. Expert Rev Hematol. 2016;9(4):401–408. [DOI] [PubMed] [Google Scholar]
- 7.Tzoulis P, Shah F, Jones R, Prescott E, Barnard M. Joint diabetes thalassaemia clinic: an effective new model of care. Hemoglobin. 2014;38(2):104–110. [DOI] [PubMed] [Google Scholar]
- 8.Liang Y, Bajoria R, Jiang Y, et al. Prevalence of diabetes mellitus in Chinese children with thalassaemia major. Trop Med Int Health. 2017;22(6):716–724. [DOI] [PubMed] [Google Scholar]
- 9.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15(7):539–553. [DOI] [PubMed] [Google Scholar]
- 10.Huang Z, Liu J, Ma L, et al. Glucose metabolism, insulin sensitivity and beta-cell function in type A insulin resistance syndrome around puberty: a 9-year follow-up. Horm Metab Res. 2014;46(1):65–72. doi: 10.1055/s-0033-1357193 [DOI] [PubMed] [Google Scholar]
- 11.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–419. [DOI] [PubMed] [Google Scholar]
- 12.Taher A, Vichinsky E, Musallam K, et al. Iron overload and chelation therapy, Chap.5. In: Weatherall D, editor. Guidelines for the Management of Non Transfusion Dependent Thalassaemia (NTDT) [Internet]. Nicosia, Cyprus: Thalassaemia International Federation; 2013. Available from: https://www.ncbi.nlm.nih.gov/books/NBK190440/ [PubMed] [Google Scholar]
- 13.De Sanctis V, Soliman A, Yassin M. Iron overload and glucose metabolism in subjects with beta-thalassaemia major: an overview. Curr Diabetes Rev. 2013;9(4):332–341. [DOI] [PubMed] [Google Scholar]
- 14.Cario H, Holl RW, Debatin KM, Kohne E. Insulin sensitivity and beta-cell secretion in thalassaemia major with secondary haemochromatosis: assessment by oral glucose tolerance test. Eur J Pediatr. 2003;162(3):139–146. doi: 10.1007/s00431-002-1121-7 [DOI] [PubMed] [Google Scholar]
- 15.Ly L, Wq L, Meng Z, et al. Analysis of the influence of iron overload in glucose metabolism in thalassemia major patients. Zhonghua Er Ke Za Zhi. 2017;55(6):419–422. doi: 10.3760/cma.j.issn.0578-1310.2017.06.005 [DOI] [PubMed] [Google Scholar]
- 16.Luo HC, Luo QS, Huang FG, Wang CF, Wei YS. Impact of genotype on endocrinal complications of children with alpha-thalassemia in China. Sci Rep. 2017;7(1):2948. doi: 10.1038/s41598-017-03029-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taher AT, Musallam KM, Karimi M, et al. Overview on practices in thalassemia intermedia management aiming for lowering complication rates across a region of endemicity: the OPTIMAL CARE study. Blood. 2010;115(10):1886–1892. doi: 10.1182/blood-2009-09-243154 [DOI] [PubMed] [Google Scholar]
- 18.Chatterjee R, Bajoria R. New concept in natural history and management of diabetes mellitus in thalassemia major. Hemoglobin. 2009;33(Suppl 1):S127–S130. doi: 10.3109/09553000903347880 [DOI] [PubMed] [Google Scholar]
- 19.Ghergherehchi R, Habibzadeh A. Insulin resistance and beta cell function in patients with beta-thalassemia major. Hemoglobin. 2015;39(1):69–73. doi: 10.3109/03630269.2014.999081 [DOI] [PubMed] [Google Scholar]
- 20.Tangvarasittichai S, Pimanprom A, Choowet A, Tangvarasittichai O. Association of iron overload and oxidative stress with insulin resistance in transfusion-dependent beta-thalassemia major and beta-thalassemia/HbE patients. Clin Lab. 2013;59(7–8):861–868. [DOI] [PubMed] [Google Scholar]
- 21.de Assis RA, Ribeiro AA, Kay FU, et al. Pancreatic iron stores assessed by magnetic resonance imaging (MRI) in beta thalassemic patients. Eur J Radiol. 2012;81(7):1465–1470. doi: 10.1016/j.ejrad.2011.03.077 [DOI] [PubMed] [Google Scholar]
- 22.Okita K, Iwahashi H, Kozawa J, et al. Homeostasis model assessment of insulin resistance for evaluating insulin sensitivity in patients with type 2 diabetes on insulin therapy. Endocr J. 2013;60(3):283–290. [DOI] [PubMed] [Google Scholar]
- 23.Shirley M, Plosker GL. Deferasirox: a review of its use for chronic iron overload in patients with non-transfusion-dependent thalassaemia. Drugs. 2014;74(9):1017–1027. doi: 10.1007/s40265-014-0238-0 [DOI] [PubMed] [Google Scholar]
- 24.Taher AT, Viprakasit V, Musallam KM, Cappellini MD. Treating iron overload in patients with non-transfusion-dependent thalassemia. Am J Hematol. 2013;88(5):409–415. doi: 10.1002/ajh.23405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vichinsky E, Cohen A, Thompson AA, et al. Epidemiologic and clinical characteristics of nontransfusion-dependent thalassemia in the United States. Pediatr Blood Cancer. 2018;65(7):e27067. doi: 10.1002/pbc.27067 [DOI] [PubMed] [Google Scholar]
- 26.Musallam KM, Cappellini MD, Wood JC, Taher AT. Iron overload in non-transfusion-dependent thalassemia: a clinical perspective. Blood Rev. 2012;26(Suppl 1):S16–S19. doi: 10.1016/S0268-960X(12)70006-1 [DOI] [PubMed] [Google Scholar]
- 27.Ambachew S, Biadgo B. Hepcidin in iron homeostasis: diagnostic and therapeutic implications in type 2 diabetes mellitus patients. Acta Haematol. 2017;138(4):183–193. doi: 10.1159/000481391 [DOI] [PubMed] [Google Scholar]
- 28.Nakavachara P, Viprakasit V. Adrenal insufficiency is prevalent in HbE/beta-thalassaemia paediatric patients irrespective of their clinical severity and transfusion requirement. Clin Endocrinol (Oxf). 2013;79(6):776–783. doi: 10.1111/cen.12235 [DOI] [PubMed] [Google Scholar]
- 29.Nakavachara P, Petchkul J, Jeerawongpanich K, et al. Prevalence of low bone mass among adolescents with nontransfusion-dependent hemoglobin E/beta-thalassemia and its relationship with anemia severity. Pediatr Blood Cancer. 2018;65:1. doi: 10.1002/pbc.26744 [DOI] [PubMed] [Google Scholar]
- 30.Baldini M, Marcon A, Ulivieri FM, et al. Bone quality in beta-thalassemia intermedia: relationships with bone quantity and endocrine and hematologic variables. Ann Hematol. 2017;96(6):995–1003. doi: 10.1007/s00277-017-2959-0 [DOI] [PubMed] [Google Scholar]
- 31.Tantiworawit A, Charoenkwan P, Hantrakool S, Choeyprasert W, Sivasomboon C, Sanguansermsri T. Iron overload in non-transfusion-dependent thalassemia: association with genotype and clinical risk factors. Int J Hematol. 2016;103(6):643–648. doi: 10.1007/s12185-016-1991-5 [DOI] [PubMed] [Google Scholar]
- 32.Frazer DM, Wilkins SJ, Mirciov CS, Dunn LA, Anderson GJ. Hepcidin independent iron recycling in a mouse model of beta-thalassaemia intermedia. Br J Haematol. 2016;175(2):308–317. doi: 10.1111/bjh.14206 [DOI] [PubMed] [Google Scholar]
- 33.Musallam KM, Cappellini MD, Taher AT. Evaluation of the 5mg/g liver iron concentration threshold and its association with morbidity in patients with β-thalassemia intermedia. Blood Cells Mol Dis. 2013;51(1):35–38. doi: 10.1016/j.bcmd.2013.01.015 [DOI] [PubMed] [Google Scholar]
- 34.Acton RT, Barton JC, Passmore LV, et al. Relationships of serum ferritin, transferrin saturation, and HFE mutations and self-reported diabetes in the Hemochromatosis and Iron Overload Screening (HEIRS) study. Diabetes Care. 2006;29(9):2084–2089. doi: 10.2337/dc05-1592 [DOI] [PubMed] [Google Scholar]
- 35.Chern JP, Lin KH, Lu MY, et al. Abnormal glucose tolerance in transfusion-dependent beta-thalassemic patients. Diabetes Care. 2001;24(5):850–854. [DOI] [PubMed] [Google Scholar]
- 36.Karimi M, Amirmoezi F, Haghpanah S, et al. Correlation of serum ferritin levels with hepatic MRI T2 and liver iron concentration in nontransfusion beta-thalassemia intermediate patients: a contemporary issue. Pediatr Hematol Oncol. 2017;34(5):292–297. doi: 10.1080/08880018.2017.1400135 [DOI] [PubMed] [Google Scholar]
- 37.Asadov C, Alimirzoeva Z, Mammadova T, Aliyeva G, Gafarova S, Mammadov J. beta-Thalassemia intermedia: a comprehensive overview and novel approaches. Int J Hematol. 2018;108(1):5–21. doi: 10.1007/s12185-018-2411-9 [DOI] [PubMed] [Google Scholar]
- 38.Vichinsky E. Non-transfusion-dependent thalassemia and thalassemia intermedia: epidemiology, complications, and management. Curr Med Res Opin. 2016;32(1):191–204. doi: 10.1185/03007995.2015.1110128 [DOI] [PubMed] [Google Scholar]