Abstract
Purpose: The primary tumor regression patterns of patients with esophageal squamous cell carcinoma (ESCC) treated with definitive chemoradiotherapy (CRT) were investigated to determine an optimal surveillance scheme.
Method: The clinical data and radiology images of patients before CRT, at completion of CRT and every 1–3 months for the subsequent 12 months or until disease progression were retrospectively reviewed to define the patterns of primary tumor regression after CRT. Survival rates were analyzed statistically in order to determine an optimal surveillance scheme.
Results: A total of 82 patients were enrolled in the present study for analysis. At the first surveillance visit date at the end of CRT, a total of 21 patients achieved complete response (early-CR), 29 patients reached incomplete response (IR), 25 patients maintained stable disease (SD) and 7 patients encountered progression of disease (PD). During subsequent surveillance, a total of 14 IR patients regressed continuously to CR (later-CR), 15 patients maintained IR (early-IR) and 9 SD patients gradually regressed to IR (later-IR). At full tumor regression (FTR), a total of 21, 14, 15, 9, 16 and 7 patients were defined as early-CR, later-CR, early-IR, later-IR, SD and PD, respectively. The median FTR time for later-CR and later-IR was 7.5 and 7 weeks, respectively. The 3-year overall survival rate of the early-CR group was 85.7% (P<0.001), which was higher compared with the later-CR (16.7%), early-IR (20%), later-IR (11.1%), SD (6.3%) and PD (0%) groups.
Conclusion: The early-CR following CRT is a robust prognostic predictor in patients with ESCC. To optimize the determination of tumor regression, ≥7 weeks after CRT is an optimal initial surveillance visit date. The surveillance of non-CR patients should concentrate on symptoms, nutrition and psychosocial support, rather than screening for recurrence of the disease.
Keywords: concurrent chemoradiotherapy, esophageal squamous cell carcinoma, surveillance, survival, tumor regression
Background
Definitive concurrent chemoradiotherapy (CRT) is considered to be the predominant treatment for patients with unresectable esophageal cancer.1 Tumor regression following CRT is regarded as not only a predictor of prognosis,2,3 but also a reference for optimal surveillance scheme establishment and determination of further treatment, such as salvage surgery or adjuvant chemotherapy.4,5
However, due to variation in tumor responses to radiation, prolonged radiation efficacy and side effects of radiation on normal tissue, including radiation-induced local inflammation or fibrotic changes, evaluating post-radiation tumor regression can be complicated.6 Until now, few studies on elucidating tumor regression patterns in patients with ESCC treated with CRT have been performed. An optimal surveillance scheme has not been established and varies somewhat arbitrarily worldwide.
The guidelines of both the National Comprehensive Cancer Network (NCCN) and the Japan Esophageal Society (JES) recommend that patients should be examined 3–4 weeks after completion of CRT to evaluate the tumor short-term response, then subsequently surveilled every 3 months during the first year, and every 4–6 months thereafter.7,8 By contrast, the European Society for Medical Oncology (ESMO) considers that, with the exception of patients who are potential candidates for “salvage surgery”, it does not appear that regular follow-up after definitive CRT has an impact on survival.9 However, all of these guidelines are lacking in sufficient evidence. So far, no definite consensus on what surveillance scheme is most effective has been adopted.
In this retrospective study, we attempt to determine an optimal surveillance scheme by investigating the patterns of primary tumor regression after CRT in patients with esophageal squamous cell carcinoma (ESCC).
Materials and methods
Patient selection criteria
The current study extends on our previous research10 and is based on the clinical data of patients obtained during our previous retrospective study, which was approved by Fujian Province Cancer Hospital (No. K201427) Institutional Review Board. Patients who fulfilled the following inclusion criteria were selected: i)histologically confirmed ESCC patients with no distant metastases except supraclavicular lymph node metastasis; ii)Eastern Cooperative Oncology Group (ECOG) performance status ≤2; iii)treated initially with CRT without neoadjuvant chemotherapy and/or salvage surgery; and iv)computed tomography (CT) and barium esophagography images available for defining clinical stage and evaluating tumor regression, from pre-CRT, at completion of CRT, and every 1–3 months subsequently. Patients who succumbed to acute radiation-induced pneumonitis following CRT were excluded.
The clinical TNM stage of enrolled patients was re-assessed according to the 8th American Joint Committee on Cancer (AJCC) TNM staging system based on CT scanning findings analyzed by at least two radiologists.11 The details of CRT, including concurrent chemotherapy regimen, gross tumor volume (GTV), clinical target volume (CTV) and organs at risk (OARs) of radiotherapy, target doses and doses limitations of OARs were defined and adjusted as described in our previous study.3 All enrolled patients were treated with three-dimensional conformal radiation therapy (3D-CRT) or intensity modulated radiation therapy (IMRT).
Tumor regression evaluation
The pattern of primary tumor regression was evaluated firstly at the end of CRT and re-assessed every 1–3 months subsequently by CT and barium esophagography until the primary tumor did not regress any further (termed “full tumor regression”, FTR) or until disease progression. Tumor regression was defined as clinically complete response (CR, the disappearance of all primary lesions evaluated by endoscopy and CT), incomplete response (IR, the persistence lesions on endoscopy and at least a 30% decrease in the greatest width of primary tumor on CT scanning), stable disease (SD, neither IR nor PD) and progression of disease (PD, the appearance of one or more new lesions and/or unequivocal progression in existing non-target lesions) using the Japanese Classification of Esophageal Cancer guidelines by two experienced radiologists. In the case of CR, histology confirmed by endoscopic biopsy was required.12
Surveillance and statistical analysis
The follow-up schedule for patients was as previously reported.3 In brief, patients were evaluated every 1–3 months for the first 2 years after CRT, every 6 months for the next 3 years, and then once annually. All patient outcomes were evaluated in March 2018. The primary endpoint was FTR time. The secondary endpoints were overall survival (OS), locoregional failure-free survival (LFFS) and distant failure-free survival (DFFS). Locoregional failure was defined as an increase in the size of primary tumor and regional node (including the supraclavicular lymph node) or the appearance of new lesions within the radiation field. Distant failure was defined as evidence of tumor in any other area.
The time to FTR was calculated from the date of RT completion to the date of FTR. The OS time was calculated from the date of diagnosis to the date of mortality or last follow-up. The LFFS and DFFS were defined as the duration between the date of diagnosis to locoregional progression, and distant progression, respectively.
Data were analyzed using IBM SPSS version 18.0 (SPSS, Inc., Chicago, IL, USA). Actuarial rates and survival curves were produced using the Kaplan-Meier estimator method and compared with the log-rank test. The correlation of tumor regression with clinical characteristics (including gender, age, ECOG score, tumor location, maximum tumor length and width, clinical TNM stages and the radiotherapy dose of GTV and CTV) was evaluated using Pearson correlation analysis. P≤0.05 was considered to indicate a statistically significant difference.
Results
Patient characteristics
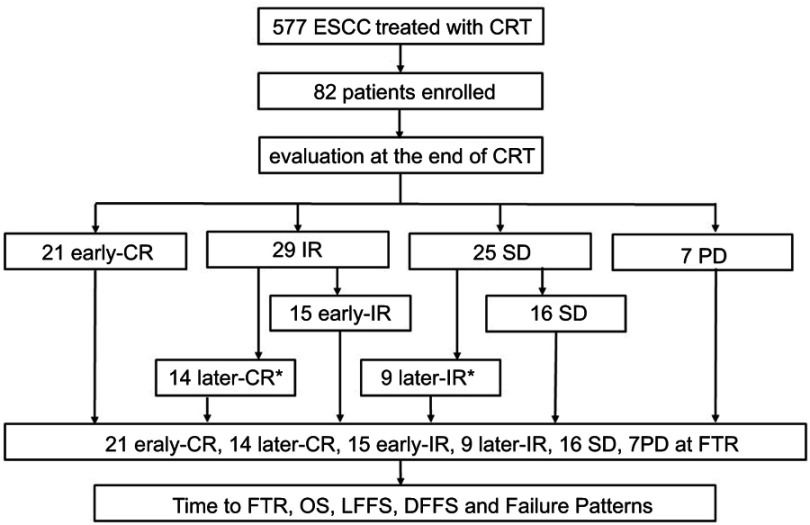
Between September 1, 2004 and December 31, 2015, a total of 577 patients treated with definitive CRT at Fujian Province Cancer Hospital were reviewed. A total of 82 of these patients met the inclusion criteria and were collected for analysis (Figure 1). The patient characteristics are presented in Table 1.
Figure 1.
Study flowchart. *Later-CR and later-IR patients were applied for time to FTR analysis.Abbreviations: CR, complete response; CRT, chemoradiotherapy; DFFS, distant failure-free survival; ESCC, esophageal squamous cell carcinoma; FTR, full tumor regression; IR, incomplete response; LFFS, locoregional failure-free survival; OS, overall survival; PD, progression of disease; SD, stable disease.
Table 1.
Clinical characteristics of patients
| Tumor regression (n=82) | ||||
|---|---|---|---|---|
| Characteristics | n | % | Correlation Coefficient | p-value |
| Gender | 0.1197 | 0.284 | ||
| Male | 69 | 84.1 | ||
| Female | 13 | 15.9 | ||
| Median age (y, range) | 59 (39–76) | −0.1179 | 0.291 | |
| ECOG scoring | 0.1307 | 0.242 | ||
| 0 | 16 | 19.5 | ||
| 1 | 66 | 80.5 | ||
| Tumor location | −0.2183 | 0.049 | ||
| Cervical | 9 | 11.0 | ||
| Upper | 31 | 37.8 | ||
| Middle | 38 | 40.3 | ||
| Lower | 4 | 4.9 | ||
| Clinical T stage | 0.0571 | 0.393 | ||
| T2 | 11 | 13.4 | ||
| T3 | 38 | 46.3 | ||
| T4 | 33 | 40.3 | ||
| Clinical N stage | 0.3932 | 0.001 | ||
| N0 | 24 | 29.3 | ||
| N1 | 58 | 70.7 | ||
| Clinical M stage | 0.1646 | 0.140 | ||
| M0 | 63 | 76.8 | ||
| M1 | 19 | 23.2 | ||
| Clinical stage | 0.2600 | 0.018 | ||
| II | 21 | 25.6 | ||
| III | 15 | 18.3 | ||
| IVA | 27 | 32.9 | ||
| IVB | 19 | 23.2 | ||
| Maxim tumor length (cm) | 5.5(2.5–14) | −0.0984 | 0.385 | |
| Maxim tumor width (cm) | 1.6(0.5–5.1) | −0.0745 | 0.512 | |
| Dose (Gy, range) | ||||
| GTV | 61.5 (50–66) | 0.0672 | 0.539 | |
| CTV | 50 (45–54) | −0.1269 | 0.256 |
Abbreviations: CTV, clinical target volume; ECOG, Eastern Cooperative Oncology Group; GTV, gross tumor volume.
Tumor regression, failure pattern and survival
At the first surveillance visit date at the end of CRT, a total of 21 patients achieved CR (early-CR), 29 patients reached IR, 25 patients maintained SD and 7 patients encountered PD. During subsequent surveillance, a total of 14 IR patients regressed continuously to CR (later-CR), the remaining 15 IR patients maintained IR (early-IR) and 9 SD patients gradually regressed to IR (later-IR). No patients with tumor regression from SD to CR or from PD to SD were observed. At FTR, a total of 21, 14, 15, 9, 16 and 7 patients were defined as early-CR, later-CR, early-IR, later-IR, SD and PD, respectively. The median time to FTR for later-CR (from IR to CR, TIC) and later-IR (from SD to IR, TSI) was 7.5 weeks (range, 5–41 weeks) and 7 weeks (range, 3–29 weeks), respectively. Tumor location, clinical N stage and clinical stage were considered to be correlated with tumor regression.
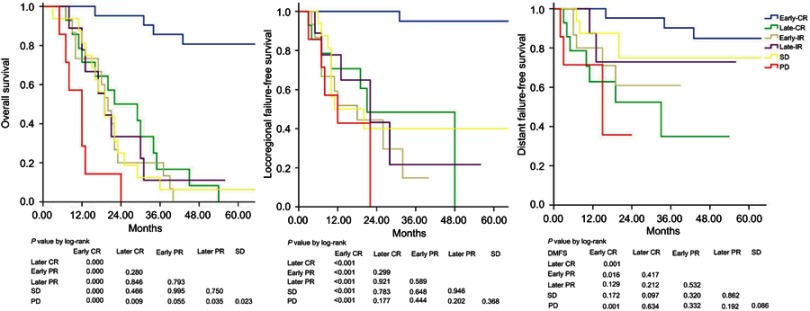
At the last surveillance visit, a total of 18 patients had survived, 62 patients had succumbed to disease progression and 2 had succumbed for unknown reasons. The median follow-up time of the cohort patients was 22 months (range, 3–108 months). The 1, 2, 3-year OS, LFFS and DFFS of early-CR, later-CR, early-IR, later-IR, SD and PD patients are summarized in Table 2. The survival of early-CR, in terms of OS, LFFS or DFFS, was significantly improved compared with the other subgroups (P<0.001). There were no significant differences in survival among later-CR, early-IR, later-IR and SD patients (termed “non-early-CR”). However, non-early-CR patients has significantly improved OS compared with PD patients (Table 2; Figure 2).
Table 2.
Survival and failure patterns in various subgroup patients
| OS (%) | LFFS (%) | DFFS (%) | Failure patterns (n, %) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subgroups | Total | 1-y | 2-y | 3-y | p-value | 1-y | 2-y | 3-y | p-value | 1-y | 2-y | 3-y | p-value | LF | DF | LDF | p-value | MTF median (range) | p-value |
| Early-CR | 21 | 100 | 95.2 | 85.7 | <0.001a | 100 | 100 | 100 | <0.001a | 100 | 95.2 | 90.2 | 0.012 a | 1 (4.8) | 3 (14.3) | 1 (4.8) | 0.439a | 23.5 (11–43) | 0.152a |
| Later-CR | 14 | 71.4 | 50 | 16.7 | 0.828 b | 70.7 | 48.5 | 48.5 | 0.816 b | 62.9 | 52.4 | 34.9 | 0.266b | 6 (42.9) | 6 (42.9) | 1 (7.1) | 0.442b | 11 (3–48) | 0.179b |
| Early-IR | 15 | 73.3 | 20 | 20 | 51.9 | 44.4 | 14.8 | 80 | 61 | 61 | 10 (66.7) | 5 (33.3) | 0 (0) | 11 (5–12) | |||||
| Later-IR | 9 | 77.8 | 33.3 | 11.1 | 77.8 | 43.2 | 21.6 | 87.5 | 72.9 | 72.9 | 4 (44.4) | 1 (11.1) | 1 (11.1) | 11 (5–12) | |||||
| SD | 16 | 81.3 | 25 | 6.3 | 0.003 c | 50 | 40 | 40 | 0.219 c | 87.5 | 75 | 75 | 0.170 c | 8 (50.0) | 2 (12.5) | 1 (6.3) | 0.857c | 11 (7–20) | |
| PD | 7 | 28.6 | 0 | 0 | 42.9 | 0 | 0 | 71.4 | 35.7 | 0 | 4 (57.1) | 2 (28.6) | 1 (14.3) | ||||||
Notes: ap-value of early-CR vs non-early-CR. bp-value among non-early-CR. cp-value of non-early-CR vs PD.
Abbreviations: CR, complete response; IR, incomplete response; SD; stable disease; PD, progression of disease; OS, overall survival; LFFS, locoregional failure-free survival; DFFS, distant failure-free survival; LF, locoregional failure; DF, distant failure; LDF, locoregional and distant failure; MTF, median time to failure.
Figure 2.
Survival in different subgroups.
Abbreviations: CR, complete response; IR, incomplete response; SD, stable disease; PD, progression of disease; OS, overall survival; LFFS, locoregional failure-free survival; DFFS, distant failure-free survival.
The failure patterns of treatment in early-CR, later-CR, early-IR, later-IR, SD and PD patients are presented in Table 2. The median times to failure (MTF) after CRT in early-CR, later-CR, early-IR, later-IR and SD were 23.5 (range, 11–43), 11 (range, 3–48), 11 (range, 5–12), 11 (range, 5–12), and 11 (range, 7–20) months, respectively, with no significant difference among groups. Locoregional failure (LF) was the predominant failure pattern in all patients and no significant difference was observed among different subgroups. However, it was notable that distant metastasis (60%, 3/5 patients) rather than locoregional recurrence (20%, 1/5 patients) was the major failure pattern developed in early-CR patients.
Discussion
Our previous study3,10 indicated that in the majority of cases, failure of patients with ESCC treated with CRT occurred very early after CRT (>50% of cases within 9 months, >70% within one year and >90% within two years).13 This suggested that following up within the first 2 years after CRT is the subject of surveillance for patients with ESCC treated with CRT.7 However, the optimal surveillance scheme for patients with ESCC within the first 2 years after CRT, including the optimal first surveillance visit date for tumor regression evaluation and the interval between subsequent surveillance visits, has yet not been established.
To determine the optimal first surveillance visit date to evaluate tumor regression, an understanding of tumor regression patterns in ESCC after CRT is required. Several studies on tumor regression patterns after RT or CRT have been performed in other cancer types.14–16 However, to the best of our knowledge, few comparable studies have been conducted in ESCC treated with CRT.17 Findings inferred from other cancer types after CRT may provide some insight into the pattern of tumor regression in ESCC after CRT. Kong et al performed a study on tumor regression patterns in head and neck squamous cell carcinoma after RT or CRT.14 It was identified that 87.1% of patients demonstrated primary tumor regression at more than 2 months after RT, as well as at the completion of CRT. Therefore, the authors suggested that the optimal initial surveillance visit date for tumor regression evaluation should be ≥2 months after RT completion. Kwak et al conducted a study of timely tumor response after preoperative CRT in rectal cancer, and identified that regression rates peaked between 6 and 7 weeks after CRT and subsequently declined.18 The current study demonstrated that compared with tumor regression evaluation at the end of CRT completion, nearly half (14/29) of IR patients regressed to CR (later-CR) and one third (9/25) of SD patients regressed to IR (later-IR) during surveillance, with median TIC of 7.5 weeks (range, 5–41) and TSI of 7 weeks (range, 3–29), respectively. These results indicate that ≥7 weeks after CRT may be the optimal initial surveillance visit date to evaluate tumor regression for ESCC treated with CRT.
However, besides tumor regression, tumor regrowth is also an important consideration in determining the initial surveillance visit date for tumor regression evaluation. Kelly et al reported that if plotted, the odds of regression of esophageal cancer tumor after CRT and prior to surgical resection resembled an inverted U shape. The peak odds, which implied full tumor regression, were at the time interval of 85 to 98 days after CRT, and the odds decreased if the surgical procedure was delayed too long.19 As demonstrated in our previous10 and current study, the first locoregional recurrence, or tumor regrowth, occurred as early as three months (12 weeks) after CRT completion. Regarding the risk of complications during surgery owing to radiation-induced fibrosis, we recommend that the optimal initial surveillance visit date to define tumor regression should be no later than 12 weeks after CRT, to maximize surgical fitness.
When evaluating the optimal surveillance interval, tumor regression evaluation at the first surveillance visit date and tumor resection potential are both important. For operable disease, patients were recommended to opt for surgery after CRT and the subsequent postoperative surveillance was not the issue of the current study.20 For non-operable disease, for example due to tumor location, physical condition or patient wishes, there are discrepancies in surveillance between CR and non-CR subgroups.
Sudo et al conducted a study of relapse patterns in ESCC patients achieving CR after definitive CRT. They concluded that 14% of CR patients experienced luminal relapse after CRT. Of these, 100% could be observed by esophagogastroduodenoscopy (EGD) while only 11% of these patients could be determined by CT scanning. Furthermore, if local treatment were applied to patients with luminal relapse alone, this appeared to prolong median overall survival by 49.2 months. Consequently, a 3-month intensive follow-up based on using endoscopy to detect early luminary recurrence was recommended for improving patient survival.17
However, although there were no significant differences in failure patterns among various subgroups, a notable result in the current study was that distant metastases, rather than locoregional recurrence (14.3 vs 4.8%) were the major failure patterns in early-CR patients, indicating that not only local but also system failure is a necessary subject for surveillance in CR patients.21 Similarly, this suggests that it is worth considering intensive system chemotherapy to eliminate occult micrometastases for early-CR patients after CRT.22 However, several studies on intensive system chemotherapy in ESCC treated with CRT, including neoadjuvant, concurrent and adjuvant chemotherapy,3,5,23,24 have for the most part failed to demonstrate a survival advantage.25
Furthermore, although no significant difference was identified owing to the small number of patients in the current study, the time from CRT completion to locoregional or distant recurrence was longer in early-CRT patients compared with non-early-CR patients, with a median of 23.5 months and a wide range from 11 to 43 months. In other words, the earliest failure in early-CRT patients was at least 11 months after CRT completion, suggest that intensive follow-up in the first year of surveillance may not be necessary in these patients.
It is well known that CR after CRT is a good predictor of prognosis.2,21,26 Shaikh et al performed a study of ESCC treated with neoadjuvant chemoradiotherapy (NCRT) followed by surgery to define prognosis prediction efficacy of CR after CRT. It was identified that a longer interval time between NCRT and surgery was associated with a higher rate of pathology CR. Unfortunately, pathology CR achieved via extending CRT to surgery interval time (later-CR) did not translate into OS improvement.27 Similarly, the current study indicated that CR patients after CRT had superior survival to non-CR patients. However, when a stratified analysis was performed in different subgroups, the present study identified that, consistent with Shaikh et al compared with IR or SD patients, only early-CR but not later-CR patients, achieved notable survival improvement, which implied tumor radiosensitivity in those patients. This indicates that to predict the survival of patients with ESCC treated with CRT, early-CR after CRT but not later-CR should be a robust prognostic predictor.
For non-resection-eligible patients who encounter non-CR, which is a serious problem in the clinic and describes the majority of ESCC patients treated with CRT, an optimal surveillance interval is less clear. NCCN and Japanese guidelines suggest that these patients should undergo surveillance routinely, whereas ESMO guidelines recommend that follow-up visits in these patients should concentrate on symptoms, nutrition and psychosocial support, rather than survival.9 The current study indicated that the survival of patients with later-CR, early-IR, later-IR, SD and PD was very poor, with a 3-year survival of 16.7, 20, 11.1, 6.3 and 0%, respectively. Our previous study also indicated that adjuvant chemotherapy with current regimens did not benefit patients treated with CRT in terms of improving survival.10 Therefore, we suggest that, except for clinical trials, according to the currently available alternative treatments for non-CR and non-resection patients after CRT, the ESMO guidelines for surveillance in those patients may be more appropriate than NCCN or JES guidelines.
One notable result of the current study was the unexpected differences in survival rates among later-CR, IR (early or later) and SD patients, particularly between later-CR and early-IR patients. The survival of later-CR patients, who were theoretically deemed to have improved survival compared with non-CR patients, were on the contrary inferior to early-IR in the current study. There was no obvious explanation for this unexpected result. However, the current study was limited by potential biases in patient selection and small sample sizes in each cohort due to the retrospective nature of the study.
Conclusion
In summary, the current study identified that early-CR rather than later-CR after CRT may serve as a robust prognostic predictor in patients with ESCC treated with CRT. To optimize determination of tumor regression after CRT, a surveillance visit date ≥7 weeks after CRT is recommended as the optimal initial date. To improve fitness for surgery, the surveillance and surgery date should not be later than 12 weeks after CRT. For non-early-CR patients who are expected to have poor survival, the subject of surveillance after CRT should be concentrated on symptoms, nutrition and psychosocial support, rather than screening for recurrence of the disease.
The current study had certain limitations due to its retrospective nature, including the inherent biases of patient selection and the suboptimal assessment of tumor regression by CT scanning, which makes it difficult for us to make firm conclusions from the findings. However, in reporting on the tumor regression pattern in ESCC after CRT, the current study provides some evidence for determining an optimal initial surveillance visit date and establishing a surveillance scheme.
Acknowledgments
The authors thank all patients who participated in the present study. This study was supported in part by grants from the Fujian Provincial Health & Family Planning Commission (Project Number: 2016-ZQN-32), the Fujian Provincial Department of Science & Technology (Project Number: 2018J01306), Joint Funds for the Innovation of Science and Technology, Fujian province (Project Number: 2017Y9079), the Fujian Provincial Platform for Medical Laboratory Research, Key Laboratory for Tumor Individualized Active Immunity (Project Number: FYKFKT- 2017015), and the Science and Technology Program of Fujian Province (Project Number: 2018Y2003).
Ethics approval and consent to participate
This retrospective study was approved by the Institutional Review Board of Fujian Province Cancer Hospital (No. K201427). All patients provided written informed consent prior to treatment, and all information was anonymized prior to analysis.
Abbreviation list
3D-CRT, three-dimensional conformal radiation therapy; AJCC, American Joint Committee on Cancer; CR, complete response; CRT, chemoradiotherapy; CT, computed tomography; CTV, clinical target volume; DFFS, distant failure-free survival; ECOG, Eastern Cooperative Oncology Group; ESCC, esophageal squamous cell carcinomas; ESMO, European Society for Medical Oncology; FTR, full tumor regression; GTV, gross tumor volume; IMRT, intensity modulated radiation therapy; IR, incomplete response; JES, Japan Esophageal Society; LFFS, locoregional failure-free survival; MTF, median time to failure; NCCN, National Comprehensive Cancer Network; OAR, organs at risk OS, overall survival; PD, progression of disease; RT, radiotherapy; SD, stable disease.
Author contributions
All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that the submitted work was not carried out in the presence of any personal, professional or financial relationships that could potentially be construed as a conflict of interest. The authors report no conflicts on interest in this work.
References
- 1.Cooper JS, Guo MD, Herskovic A, et al. Chemoradiotherapy of locally advanced esophageal cancer: long-term follow-up of a prospective randomized trial (RTOG 85-01). Radiation therapy oncology group. JAMA. 1999;281(17):1623–1627. [DOI] [PubMed] [Google Scholar]
- 2.Adenis A, Tresch E, Dewas S, et al. Clinical complete responders to definite chemoradiation or radiation therapy for oesophageal cancer: predictors of outcome. BMC Cancer. 2013;13(1):413. doi: 10.1186/1471-2407-13-413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen MQ, Lin QL, Chen YG, Guo JH, Xu BH, Tian Y. Neoadjuvant chemotherapy may not benefit esophageal squamous cell carcinoma patients treated with definitive chemoradiotherapy. Jcma. 2017;80(10):636–643. doi: 10.1016/j.jcma.2017.06.014 [DOI] [PubMed] [Google Scholar]
- 4.Wu SX, Li XY, Xu HY, et al. Effect of consolidation chemotherapy following definitive chemoradiotherapy in patients with esophageal squamous cell cancer. Sci Rep. 2017;7(1):16870. doi: 10.1038/s41598-017-17254-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen Y, Guo L, Cheng X, et al. With or without consolidation chemotherapy using cisplatin/5-FU after concurrent chemoradiotherapy in stage II-III squamous cell carcinoma of the esophagus: A propensity score-matched analysis. Radiother Oncol.2018;129(1):154–160. [DOI] [PubMed] [Google Scholar]
- 6.Saito N, Nadgir RN, Nakahira M, et al. Posttreatment CT and MR imaging in head and neck cancer: what the radiologist needs to know. Radiographics. 2012;32(5):1261–1282. doi: 10.1148/rg.325115160 [DOI] [PubMed] [Google Scholar]
- 7.Kuwano H, Nishimura Y, Oyama T, et al. Guidelines for diagnosis and treatment of Carcinoma of the Esophagus April 2012 edited by the Japan Esophageal Society. Esophagus. 2015;12:1–30. doi: 10.1007/s10388-014-0465-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ajani J, D’Amico TA, Baggstrom M, et al. Esophageal and esophagogastric junction cancers; 2018. Available from: https://wwwnccnorg/professionals/physician_gls/pdf/esophagealpdf. Accessed July 11, 2018.
- 9.Lordick F, Mariette C, Haustermans K, Obermannová R, Arnold D. Oesophageal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2016;27(suppl_5):v50–v57. doi: 10.1093/annonc/mdw329 [DOI] [PubMed] [Google Scholar]
- 10.Chen M, Shen M, Lin Y, et al. Adjuvant chemotherapy does not benefit patients with esophageal squamous cell carcinoma treated with definitive chemoradiotherapy. Radiat Oncol. 2018;13(1). doi: 10.1186/s13014-018-1086-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rice TW, Gress DM, Patil DT, Hofstetter WL, Kelsen DP, Blackstone EH. Cancer of the esophagus and esophagogastric junction—major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67(4):304–317. doi: 10.3322/caac.21399 [DOI] [PubMed] [Google Scholar]
- 12.Japan Esophageal S. Japanese classification of esophageal cancer, 11th edition: part II and III. Esophagus. 2017;14(1):37–65. doi: 10.1007/s10388-016-0556-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fang HY, Chao YK, Chang HK, Tseng CK, Liu YH. Survival outcomes of consolidation chemoradiotherapy in esophageal cancer patients who achieve clinical complete response but refuse surgery after neoadjuvant chemoradiotherapy. Dis Esophagus. 2017;30(2):1–8. doi: 10.1093/dote/dox100 [DOI] [PubMed] [Google Scholar]
- 14.Kong M, Hong SE. Tumor regression patterns based on follow-up duration in patients with head and neck squamous cell carcinoma treated with radiotherapy or chemoradiotherapy. Clin Exp Otorhinolaryngol. 2015;8(4):416–421. doi: 10.3342/ceo.2015.8.4.416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanzaki H, Kataoka M, Nishijima N, Nagasaki K, Uwatsu K, Nishikawa A. Early tumor regression impacts on outcome in stage III non-small cell lung cancer treated with definitive radiation therapy. Int J Radiat Oncol Biol Phys. 2015;93(3):E447-E448. [Google Scholar]
- 16.Van Den Begin R, Kleijnen J-P, Engels B, et al. Tumor volume regression during preoperative chemoradiotherapy for rectal cancer: a prospective observational study with weekly MRI. Acta Oncol (Madr). 2018;57(6):723–727. [DOI] [PubMed] [Google Scholar]
- 17.Sudo K, Kato K, Kuwabara H, et al. Patterns of relapse after definitive chemoradiotherapy in stage II/III (Non-T4) esophageal squamous cell carcinoma. Oncology. 2018;94(1):47–54. doi: 10.1159/000480515 [DOI] [PubMed] [Google Scholar]
- 18.Kwak YK, Kim K, Lee JH, et al. Timely tumor response analysis after preoperative chemoradiotherapy and curative surgery in locally advanced rectal cancer: A multi-institutional study for optimal surgical timing in rectal cancer.Radiother Oncol. 2016;1119(3):512–518. [DOI] [PubMed] [Google Scholar]
- 19.Haisley KR, Laird AE, Nabavizadeh N, et al. Association of intervals between neoadjuvant chemoradiation and surgical resection with pathologic complete response and survival in patients with esophageal cancer. JAMA Surg. 2016;151(11):e162743. doi: 10.1001/jamasurg.2016.2743 [DOI] [PubMed] [Google Scholar]
- 20.Nomura M, Kato K, Ando N, et al. Comparison between neoadjuvant chemotherapy followed by surgery and definitive chemoradiotherapy for overall survival in patients with clinical Stage II/III esophageal squamous cell carcinoma (JCOG1406-A). Jpn J Clin Oncol. 2017;47(6):480–486. doi: 10.1093/jjco/hyx040 [DOI] [PubMed] [Google Scholar]
- 21.Jipping KM, Hulshoff JB, van Amerongen EA, Bright TI, Watson DI, Plukker JTM. Influence of tumor response and treatment schedule on the distribution of tumor recurrence in esophageal cancer patients treated with neoadjuvant chemoradiotherapy. J Surg Oncol. 2017;116(8):1096–1102. doi: 10.1002/jso.24786 [DOI] [PubMed] [Google Scholar]
- 22.Oppedijk V, van der Gaast A, van Lanschot JJ, et al. Patterns of recurrence after surgery alone versus preoperative chemoradiotherapy and surgery in the CROSS trials. J Clin Oncol. 2014;32(5):385–391. doi: 10.1200/JCO.2013.51.2186 [DOI] [PubMed] [Google Scholar]
- 23.Minsky BD, Neuberg D, Kelsen DP, et al. Final report of Intergroup Trial 0122 (ECOG PE-289, RTOG 90-12): phase II trial of neoadjuvant chemotherapy plus concurrent chemotherapy and high-dose radiation for squamous cell carcinoma of the esophagus. Int J Radiat Oncol Biol Phys. 1999;43(3):517–523. doi: 10.1016/S0360-3016(98)00463-5 [DOI] [PubMed] [Google Scholar]
- 24.Adelstein DJ, Rice TW, Rybicki LA, et al. Does paclitaxel improve the chemoradiotherapy of locoregionally advanced esophageal cancer? A nonrandomized comparison with fluorouracil-based therapy. J Clin Oncol. 2000;18(10):2032–2039. doi: 10.1200/JCO.2000.18.10.2032 [DOI] [PubMed] [Google Scholar]
- 25.van Meerten E. van der Gaast A. Systemic treatment for oesophageal cancer. Eur J Cancer. 2005;41(5):664–672. doi: 10.1016/j.ejca.2004.10.030 [DOI] [PubMed] [Google Scholar]
- 26.Berger AC, Farma J, Scott WJ, et al. Complete response to neoadjuvant chemoradiotherapy in esophageal carcinoma is associated with significantly improved survival. J Clin Oncol. 2005;23(19):4330–4337. doi: 10.1200/JCO.2005.05.017 [DOI] [PubMed] [Google Scholar]
- 27.Shaikh T, Ruth K, Scott WJ, et al. Increased time from neoadjuvant chemoradiation to surgery is associated with higher pathologic complete response rates in esophageal cancer. Ann Thorac Surg. 2015;99(1):270–276. doi: 10.1016/j.athoracsur.2014.08.033 [DOI] [PMC free article] [PubMed] [Google Scholar]