Abstract
Background
Atrial fibrillation (AF) is associated with diminished cardiac function, and exercise tolerance.
Hypothesis
We sought to investigate the role of cardiac rehabilitation program (CR) in patients with AF.
Methods
The study included 2165 consecutive patients that participated in our CR program between the years 2009 to 2015. All were evaluated by a standard exercise stress test (EST) at baseline, and upon completion of at least 3 months of training. Participants were dichotomized according to baseline fitness and the degree of functional improvement. The combined primary end point was cardiac related hospitalization or all‐cause mortality.
Results
A total of 292 patients had history of AF, with a mean age of 68 ± 9 years old, 76% of which were males. The median predicted baseline fitness of AF patients was significantly lower compared to non‐AF patients (103% vs 122%, P < 0.001, respectively). Prominent improvement was achieved in the majority of the patients in both groups (64% among AF patients and 63% among those without AF). Median improvement in fitness between stress tests was significantly higher in patients with AF (124% vs 110%, P < 0.001, respectively). Among AF patients, high baseline fitness was associated with a lower event rates (HR 0.40; 95%CI 0.23‐0.70; P = 0.001). Moreover, prominent improvement during CR showed a protective effect (HR 0.83; 95% CI 0.69‐0.99; P = 0.04).
Conclusion
In patients with AF participating in CR program, low fitness levels at baseline EST are associated with increased risk of total mortality or cardiovascular hospitalization during long‐term follow‐up. Improvement on follow‐up EST diminishes the risk.
Keywords: atrial fibrillation, cardiac rehabilitation, exercise stress test, fitness level
1. INTRODUCTION
Atrial fibrillation (AF) is a common arrhythmia which is increasing yearly.1 Risk factors for developing AF include, among others, age, gender, obesity, and low fitness level.2, 3
The benefit of cardiac rehabilitation (CR) programs has been well‐established in many cardiac diseases, including heart failure, and coronary artery disease.4, 5, 6 Participation in multidisciplinary programs that include aerobic physical activity has been shown to be associated with a significant reduction in morbidity and mortality.7 Furthermore, fitness levels at baseline and the degree of improvement of fitness during rehabilitation are in correlation with outcomes.8, 9
The relationship between physical activity and risk of AF is preserved even when corrected for BMI, age, and comorbidities. In fact, the arrhythmia itself is associated with lower exercise capacity and physical fitness.10 While multiple studies showed benefit in increasing cardiovascular fitness in this patient population with subsequent decrease in incidence or recurrences of AF episodes,11, 12 only few have examined the impact of the arrhythmia on cardiac rehabilitation and fitness training without being able to evaluate the real impact of exercise based cardiac rehabilitation on mortality or cardiovascular adverse events.13
Accordingly, the aim of this study was to examine effects of AF on cardiac rehabilitation and associated outcomes. Specifically, we sought to evaluate the role of the fitness level at baseline as well as the degree of improvement among AF patients undergoing CR, and its effect on cardiac related morbidity and total mortality.
2. METHODS
2.1. Patients
Our CR cohort contains 5732 patients. The present study population was comprised of 2177 consecutive patients with and without AF who completed our CR program and who had a follow‐up EST between 2009 and April 2015. All are patients with established cardiovascular diseases who were admitted to our cardiac rehabilitation center after myocardial infarction, percutaneous coronary intervention, coronary artery by‐pass grafting operation, decompensated heart failure, or valve repair/replacement.
Participants were divided into two groups according to the existence of AF. Furthermore, the patients among the AF group were also dichotomized according to the degree of functional improvement, between the baseline and the follow‐up EST according to percent of predicted age and sex metabolic equivalent task (METs) score. The combined primary end point was cardiac related hospitalization and/or all‐cause mortality.
2.2. The diagnosis of AF
History of AF at baseline was based on medical records, self‐report during the initial physician examination, or electrocardiographic documentation of AF during the first exercise stress test. All atrial fibrillation events were adjudicated by two study investigators (Arwa Younis and AB (Anat Berkovitch)) who were blinded to patients' baseline characteristics.
2.3. Exercise protocol and clinical management
Patients participated in a 6‐month cardiac rehabilitation program, consisting of structured, 60 minutes, bi‐weekly ET sessions according to a predefined protocol individualized according to the ESC HF rehabilitation consensus paper.4 A maximal exercise stress test (EST) according to the Bruce protocol was performed and interpreted by a board certified cardiologist at the first visit.14 Exercise capacity and prescription was based on the results of the first EST, and were individually prescribed by senior exercise physiologists. In addition, all patients were consulted by cardiologists, dietitians, and nursing staff. Psychological support was available to all subjects.
In order to account for differences in expected METs according to age and gender, and neutralize their effect in our statistical analyses, we expressed the fitness of patients as a percentage of the expected METs for age and gender, as established by normograms from the literature.15 An improvement was defined as delta predicted METs ({[predicted METs 2−predicted METS1]/ predicted METs 1} * 100) that is greater than 5.
After a median of 8 ± 5 months of program participation, subjects underwent a second symptom limited stress test and clinical evaluation by a rehabilitation physician. Following the active training period, most patients continued exercise in the community, under the care of their family physician and cardiologist, while some continued to exercise in a hospital based setting.
2.4. Study design and endpoints
The primary outcome of the current study was the first composite event of cardiovascular related hospitalization or all‐cause mortality. Cardiac related hospitalizations were identified from hospital records of discharge letters from the internal medicine or cardiology wards with the ICD‐9 discharge diagnoses being one of the diagnoses of CHF or MACE (cardiovascular mortality, myocardial infarction, stroke, and cardiovascular related hospitalization). Mortality data was available for all subjects from the National Israeli Population Register up to middle of 2016.
2.5. Statistical analyses
Continuous parameters of the study groups were compared using the two‐sample Student t‐test. For comparison of categorical data we used the Fisher exact test. The probability of outcome according to the presence or absence of AF was graphically displayed according to the method of Kaplan and Meier, with comparison of cumulative survival across strata by the log‐rank test. Cox proportional hazards regression modeling was used to determine the hazard ratio (HR) for our primary outcome.
Multivariable linear regression models were conducted with metabolic equivalents as the dependent variable, and independent predictors were selected for inclusion using backward selection methodology. All potentially significant univariate predictors of exercise capacity (P < 0.10) were included in the model, and least significant covariates were removed individually until all remaining covariates were statistically significant predictors of improvement. Two and three‐way interaction terms between independent predictors in the final models were further tested for statistical significance.
Statistical significance was declared for a two‐sided P < 0.05. The statistical analysis was performed with IBM SPSS version 20.0 (Chicago, Illinois) and SAS version 9.2 (SAS institute Inc.).
3. RESULTS
3.1. Population characteristics
This study included 2177 consecutive patients that participated in our CR program and who had a follow‐up EST between 2009 and April 2015. The study group included 304 (15%) patients with a history of AF, while the control group included 1873 (85%) patients without it. Baseline characteristics of patients are summarized in Table 1.
Table 1.
Baseline characteristics, echocardiography, and cardiac stress test findings of the study population by the two pre‐specified groups
| Variable | None AF; n = 1873 | AF; n = 304 | P value |
|---|---|---|---|
| Male | 1537 (0.82) | 223 (0.76) | 0.02 |
| Age (years) | 62 (±12) | 68 (±9) | <0.001 |
| Weight (kg) | 81 (±15) | 83 (±16) | 0.57 |
| Smoking | 266 (0.16) | 32 (0.11) | 0.16 |
| Ischemic heart disease | 1535 (0.82) | 203 (0.7) | <0.001 |
| Congestive heart failure (NYHA ≥ II) | 165 (0.09) | 79 (0.27) | <0.001 |
| Prior CABG | 450 (0.24) | 102 (0.35) | <0.001 |
| Valvular disease | 282 (0.15) | 114 (0.39) | <0.001 |
| Cerebrovascular accident | 102 (0.05) | 29 (0.1) | 0.003 |
| Dyslipedemia | 986 (0.53) | 165 (0.57) | 0.218 |
| Hypertension | 887 (0.47) | 197 (0.68) | <0.001 |
| Diabetes mellitus | 493 (0.26) | 89 (0.31) | 0.136 |
| Renal impairment (eGFR < 60) | 100 (0.05) | 50 (0.17) | <0.001 |
| Chronic obstructive pulmonary disease | 30 (0.02) | 18 (0.06) | <0.001 |
| Chronic resynchronization therapy | 37 (0.02) | 6 (0.02) | 0.928 |
| Implantable cardioverter defibrillator | 69 (0.04) | 22 (0.08) | 0.002 |
| Pacemaker | 109 (0.06) | 45 (0.15) | <0.001 |
| Echocardiography findings | |||
| Left ventricular ejection fraction | 51% (±17) | 54% (±10) | <0.001 |
| Left atrial area (cm2) | 21 (±6) | 27 (±5) | <0.001 |
| Systolic pulmonary artery pressure (mm Hg) | 33 (±9) | 39 (±8) | <0.001 |
| Ergometrie findings | |||
| Heart rate at rest (bpm) | 69 (±11) | 69 (±14) | 0.325 |
| Max effort pulse (bpm) | 125 (±23) | 111 (±23) | <0.001 |
| One‐min recovery pulse (bpm) | 101 (±19) | 94 (±20) | <0.001 |
Abbreviations: CABG, coronary artery bypass grafting; eGFR, estimated glomerular filtration rate calculated based on the modification of diet in renal disease study equation; NYHA, New York Heart Association Score.
The mean age at baseline was significantly higher in the AF group (68 ± 9 years old vs 62 ±12 years old, P < 0.001, respectively). In addition, the rates of comorbidities were higher in the AF group. Interestingly, patients with AF had higher LVEF compared to other participants (54 ±10% vs 51 ±17%, P < 0.001, respectively).
3.2. Follow‐up exercise stress test and improvement capacity
Both groups showed high rates of improvement in their fitness level adjusted for the age and sex predicted METs between the baseline and follow‐up EST. Significant improvement (delta > 5%) was achieved among 194 (64%) patients with AF, and among 1180 (63%) patients without AF (P = 0.37 for the comparison). The initial predicted METs was significantly lower among patients with AF (103% vs 122%; P < 0.001) (Figure 1A). The delta for improvement in fitness relative to age and gender predicted value was significantly more prominent in patients with AF (24% vs 10%, P < 0.001) (Figure 1B).
Figure 1.
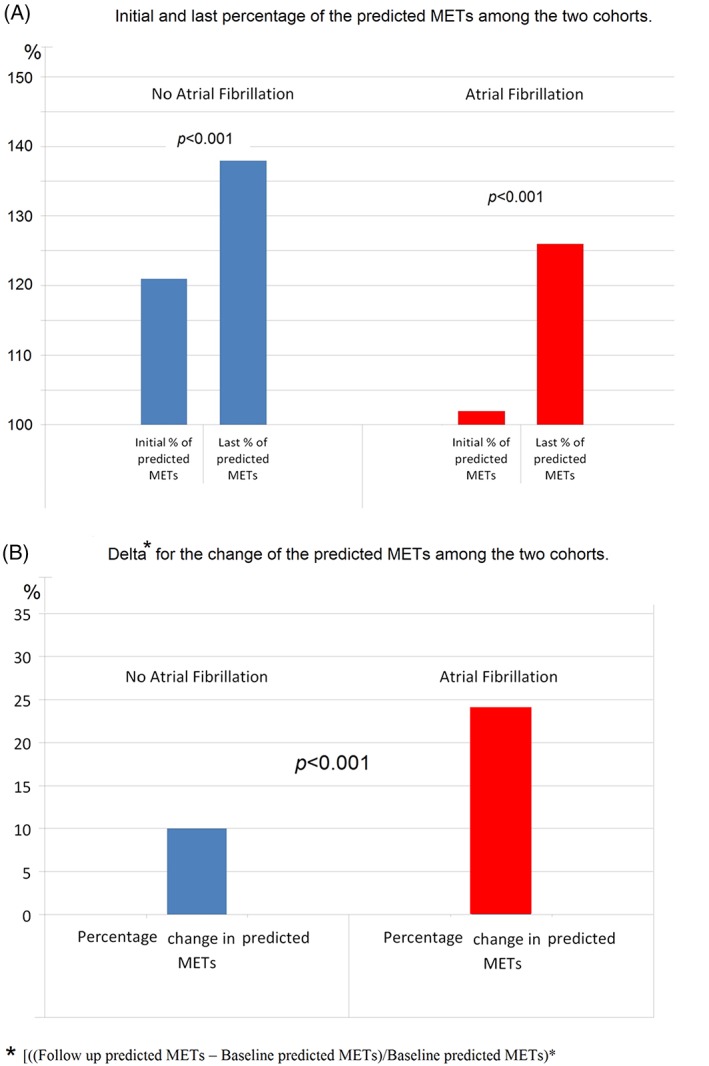
A, Initial and last percentage of the predicted METs among patients wit and without AF undergoing cardiac rehabilitation. B, The percentage change [([Follow‐up predicted METs−Baseline predicted METs]/Baseline predicted METs) * 100] among patients with AF and those without it
3.3. Predictors for improvement among patients with AF
In multivariate analyses, female sex, non‐DM, low maximal pulse effort, and preserved LVEF (>30%) were all significant independent predictors of remarkable improvement in exercise capacity after CR among AF patients (Figure S1, Supporting information). There was a statistically significant interaction between DM status, sex, and ejection fraction.
3.4. Improvement in fitness and the primary outcome among both groups
During study follow‐up a total of 544 (25%) patients met the primary endpoint. Fifty‐four patients (2.5%) died, and another 490 (97.5%) were hospitalized for any cardiac reason. Among patients with AF, Kaplan‐Mayer survival analysis showed a strong trend for lower event rates of the primary endpoint at 5 years in patients with significant improvement in fitness (log‐rank P value = 0.06) (Figure 2A). Among patients without AF, Kaplan‐Mayer survival analysis showed a significant lower events rate of the primary endpoint at 5 years in patients with significant improvement in fitness (log‐rank P value < 0.001) (Figure 2B).
Figure 2.
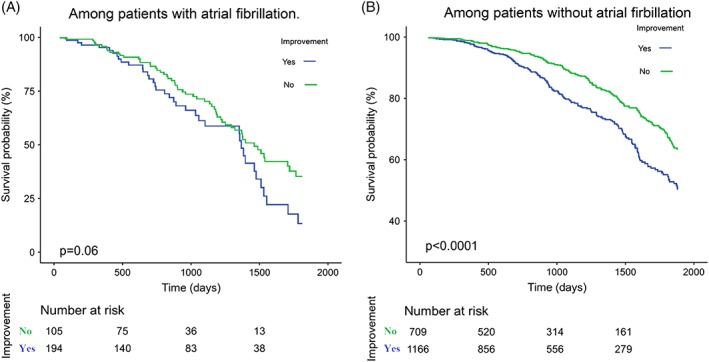
Kaplan Meier survival analyses showing the risk for MACE and/or all‐cause mortality among patients with AF (A) and without AF (B) based on their improvement
3.5. Improvement in fitness and the primary outcome only in patients with AF
Accordingly, multivariate cox modeling among only those with AF, adjusted for age, gender and comorbidities, demonstrated that prominent improvement was associated with a lower significant risk for the primary endpoint (HR 0.83; 95% CI 0.69‐0.98; P = 0.04). High baseline fitness was associated with the lowest significant risk for the primary endpoint (HR 0.41; 95% CI 0.24‐0.70; P < 0.001) (Table 2). Similar results were obtained also among patients without AF.
Table 2.
Independent MACE and all‐cause mortality risk predictors in patients with and without atrial fibrillation undergoing cardiac rehabilitation—a multivariate cox model regression
| Variable | Atrial fibrillation n. 304 | No atrial fibrillation n. 1873 | ||||
|---|---|---|---|---|---|---|
| HR | 95.0% CI | P value | HR | 95.0% CI | P value | |
| High baseline fitness | 0.41 | 0.24‐0.70 | <0.001 | 0.67 | 0.53‐0.85 | <0.001 |
| Improvementa | 0.83 | 0.69‐0.98 | 0.04 | 0.58 | 0.46‐0.72 | <0.001 |
| Age > 75 years | 1.29 | 0.81‐2.05 | 0.28 | 1.50 | 1.13‐1.98 | 0.005 |
| Men | 1.1 | 0.65‐1.86 | 0.73 | 1.05 | 0.78‐1.39 | 0.738 |
| Ischemic heart disease | 1.04 | 0.64‐1.71 | 0.87 | 1.03 | 0.77‐1.38 | 0.827 |
| Congestive heart failure | 1.22 | 0.77‐1.91 | 0.4 | 2.06 | 1.54‐2.75 | <0.001 |
| Prior cerebrovascular accident | 0.85 | 0.42‐1.71 | 0.64 | 1.23 | 0.82‐1.85 | 0.310 |
| Hypertension | 1.13 | 0.70‐1.83 | 0.62 | 1.18 | 0.93‐1.51 | 0.170 |
| Dyslipidemia | 0.63 | 0.40‐1.01 | 0.05 | 0.76 | 0.60‐0.96 | 0.022 |
| Diabetes mellitus | 1.45 | 0.93‐2.29 | 0.11 | 1.40 | 1.10‐1.78 | 0.006 |
| Renal impairmentb | 1.66 | 1.01‐2.73 | 0.05 | 1.50 | 1.04‐2.16 | 0.029 |
| Chronic obstructive pulmonary disease | 1.54 | 0.72‐3.27 | 0.27 | 1.20 | 0.60‐2.38 | 0.612 |
Improvement is ({[predicted METs 2—predicted METS1]/predicted METs 1} * 100) > 5.
Estimated glomerular filtration rate < 60 mL/min/1.73 m2, based on the Modification of Diet in Renal Disease study equation.
Further analysis, only in patients with AF, incorporating the improvement upon baseline fitness showed a gradation in outcomes. Kaplan‐Mayer analysis showed that patients with high baseline fitness and major improvement had the lowest event rate of the primary endpoint. Furthermore, patients with high baseline fitness and minor improvement or low baseline fitness with a major improvement had intermediate outcomes. The worst outcome, in fact, was demonstrated in patients with poor baseline fitness and minor improvement in follow‐up (log‐rank P value < 0.001, Figure 3).
Figure 3.
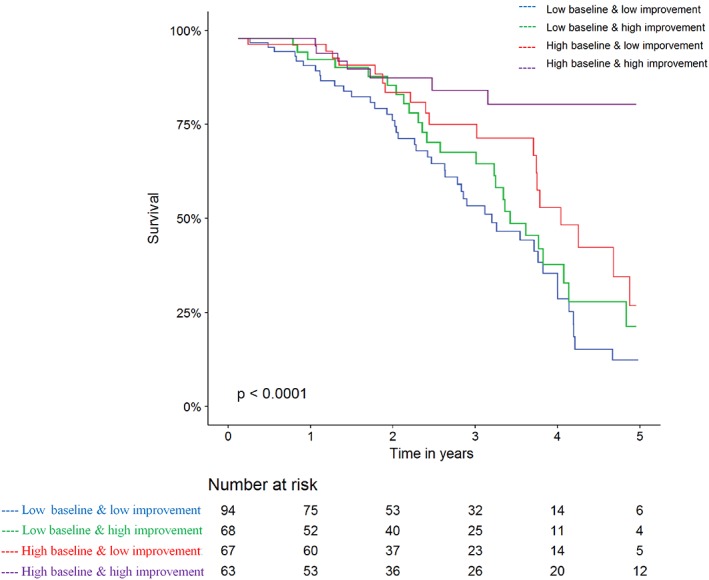
Kaplan‐Meier survival analysis showing the risk for MACE and/or all‐cause mortality among patients with AF based on their baseline fitness level and their percentage of improvement
While comparing to AF patients with low baseline fitness and minor improvement (the reference group), those with low baseline fitness and major improvement showed no significant risk reduction in clinical outcomes (P = 0.75). Interestingly, a significant decreased risk was observed in patients with high baseline fitness albeit a minor improvement (HR 0.55, 0.32‐0.94, P = 0.03). As predicted, the most prominent risk reduction was observed in patients with high baseline fitness and a major improvement in follow‐up EST (HR 0.18, 0.08‐0.39, P < 0.0001) (Figure S2).
4. DISCUSSION
Our study evaluated the significance of AF among patients with cardiovascular illnesses undergoing CR. The main finding of the present study is that among patients with AF undergoing CR, high baseline fitness levels are independently associated with decreased risk of MACE or mortality.
In keeping with previous studies16 patients with a history of AF had a lower baseline fitness levels compared to their non‐atrial fibrillation peers. Interestingly, these patients showed a higher degree of improvement throughout the rehabilitation program. This could be potentially related to the fact that starting at a lower level of fitness allows more room for improvement, whilst patients who start rehabilitation closer to their maximal fitness level have to work harder to achieve similar degree of improvements. Martin et al reported similar results showing that improvement in fitness level was most strongly among those who started with low fitness levels.7 Previous studies have shown also consistent results.17, 18 In fact, the positive effect on physical fitness level and capacity is of a paramount importance, since these are independent predictors of cardiovascular events and all‐cause mortality.19, 20 Several large cohort studies showed that for every one MET increase in physical capacity the mortality rates decrease for men by 17%, and for women by 14%.17 Indeed we also showed that there is an association between baseline fitness level, the degree of improvement and morbidity and mortality in patients with a history of AF. Participants in the rehabilitation program that exhibited no or little improvement in fitness levels at the six‐month evaluation had increased risk of the cardiac related hospitalization or total mortality. Those who showed an improvement did better during the follow‐up period. Nevertheless, the strongest predictor of this primary end point was fitness level at baseline: Those at highest risk were patients with low baseline fitness level, with no or low improvement. In contrary, patients with high baseline fitness levels, regardless of their improvement over time, had less adverse events or mortality.
These findings demonstrate that improvement in fitness level has a modest protective effect, among those with low baseline fitness levels. Low exercise capacity or fitness as assessed by standard exercise test or cardiopulmonary test is a well‐established and independent predictor of all‐cause mortality, coronary artery disease, or cardiovascular events. This association was established in several large population studies and further validated by meta‐analysis.21 Actually, these findings apply for healthy subjects22 and as well as for patients with ischemic heart disease, or heart failure patients.16 Our results also support and expand this data, showing consistent result in a real life unselected cohort of AF patients.
Based on our findings, the most important predictor for cardiac related adverse events or total mortality in patients with a history of AF undergoing CR is their baseline fitness capacity. Yet, CR can reduce the risk of morbidity and mortality in patients with AF, although this effect is relatively modest, identification of patients at increased risk could be easily assessed by a baseline exercise test prior to initiating rehabilitation programs. In those, it may be helpful to perform an intense rehabilitation in order to increase their fitness level, and maybe improve their outcomes.
Our study has some limitations most of which stem from the retrospective and observational nature of the analysis which limits our ability to control for unmeasured confounders. Furthermore the data are derived from the experience of a single center, limiting the generalization of our results and conclusions. While our study cohort comprised subjects with a history of AF participating in CR in our institution, it is likely that this group still reflects selection bias by referring physicians. Furthermore, subjects who chose to attend and adhere to a CR program are probably more compliant and health conscious than subjects unwilling to do so. Nevertheless, our study describes a cohort of AF patients attending a structured CR program in a real life setting and presents long‐term outcome.
5. CONCLUSION
Among our cohort of AF patients participating in CR program, improvement in cardiovascular fitness, as measured by standard EST, was associated with reduced risk of mortality or hospitalization during follow‐up. Nevertheless, the baseline fitness level overshadows the improvement capacity in determining the primary outcome.
Conflict of interest
The authors declare no potential conflict of interests.
Supporting information
Figure S1. Predictors for improvement in fitness capacity among patients with AF
Figure S2. Multivariate analysis comparing patients with AF based on their baseline and improvement, taking patients with low baseline fitness level and low improvement as the reference group
Younis A, Shaviv E, Nof E, et al. The role and outcome of cardiac rehabilitation program in patients with atrial fibrillation. Clin Cardiol. 2018;41:1170–1176. 10.1002/clc.23001
REFERENCES
- 1. Chugh SS, Havmoeller R, Narayanan K, et al. Worldwide epidemiology of atrial fibrillation: a global burden of disease 2010 study. Circulation. 2014;129(8):837‐847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Anderson L, Thompson DR, Oldridge N, Zwisler AD, Rees K, et al. Exercise‐based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2016;1:CD001800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lau DH, Nattel S, Kalman JM, Sanders P. Modifiable risk factors and atrial fibrillation. Circulation. 2017;136(6):583‐596. [DOI] [PubMed] [Google Scholar]
- 4. Piepoli MF, Conraads V, Corra U, Dickstein K, Francis DP, et al. Exercise training in heart failure: from theory to practice. A consensus document of the heart failure association and the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Heart Fail. 2011;13(4):347‐357. [DOI] [PubMed] [Google Scholar]
- 5. Taylor RS, Sagar VA, Davies EJ, Briscoe S, Coats AJ, et al. Exercise‐based rehabilitation for heart failure. Cochrane Database Syst Rev. 2014;4:CD003331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Reibis R, Voller H, Gitt A, Jannowitz C, Halle M, et al. Management of patients with ST‐segment elevation or non‐ST‐segment elevation acute coronary syndromes in cardiac rehabilitation centers. Clin Cardiol. 2014;37(4):213‐221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Martin BJ, Arena R, Haykowsky M, et al. Cardiovascular fitness and mortality after contemporary cardiac rehabilitation. Mayo Clin Proc. 2013;88(5):455‐463. [DOI] [PubMed] [Google Scholar]
- 8. Hung RK, Al‐Mallah MH, McEvoy JW, Whelton SP, Blumenthal RS, et al. Prognostic value of exercise capacity in patients with coronary artery disease: the FIT (Henry ford ExercIse testing) project. Mayo Clin Proc. 2014;89(12):1644‐1654. [DOI] [PubMed] [Google Scholar]
- 9. Sarullo FM, Fazio G, Brusca I, et al. Cardiopulmonary exercise testing in patients with chronic heart failure: prognostic comparison from peak VO2 and VE/VCO2 slope. Open Cardiovasc Med J. 2010;4:127‐134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Qureshi WT, Alirhayim Z, Blaha MJ, et al. Response to letter regarding article, "cardiorespiratory fitness and risk of incident atrial fibrillation: results from the henry ford exercise testing (FIT) project". Circulation. 2015;132(25):e395. [DOI] [PubMed] [Google Scholar]
- 11. Proietti M, Boriani G, Laroche C, Diemberger I, Popescu MI, et al. Self‐reported physical activity and major adverse events in patients with atrial fibrillation: a report from the EURObservational research programme pilot survey on atrial fibrillation (EORP‐AF) general registry. Europace. 2017;19(4):535‐543. [DOI] [PubMed] [Google Scholar]
- 12. Zhu W, Shen Y, Zhou Q, et al. Association of physical fitness with the risk of atrial fibrillation: a systematic review and meta‐analysis. Clin Cardiol. 2016;39(7):421‐428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Risom SS, Zwisler AD, Johansen PP, Sibilitz KL, Lindschou J, et al. Exercise‐based cardiac rehabilitation for adults with atrial fibrillation. Cochrane Database Syst Rev. 2017;2:CD011197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Farrell SW, Finley CE, Radford NB, Haskell WL. Cardiorespiratory fitness, body mass index, and heart failure mortality in men: Cooper center longitudinal study. Circ Heart Fail. 2013;6(5):898‐905. [DOI] [PubMed] [Google Scholar]
- 15. Morris CK, Myers J, Froelicher VF, Kawaguchi T, Ueshima K, Hideg A. Nomogram based on metabolic equivalents and age for assessing aerobic exercise capacity in men. J Am Coll Cardiol. 1993;22(1):175‐182. [DOI] [PubMed] [Google Scholar]
- 16. Vanhees L, Schepers D, Defoor J, Brusselle S, Tchursh N, Fagard R. Exercise performance and training in cardiac patients with atrial fibrillation. J Cardpulm Rehabil. 2000;20(6):346‐352. [DOI] [PubMed] [Google Scholar]
- 17. Gulati M, Black HR, Shaw LJ, Arnsdorf MF, Merz CN, et al. The prognostic value of a nomogram for exercise capacity in women. N Engl J Med. 2005;353(5):468‐475. [DOI] [PubMed] [Google Scholar]
- 18. Taylor C, Tsakirides C, Moxon J, et al. Submaximal fitness and mortality risk reduction in coronary heart disease: a retrospective cohort study of community‐based exercise rehabilitation. BMJ Open. 2016;6(6):e011125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gulati M, Pandey DK, Arnsdorf MF, et al. Exercise capacity and the risk of death in women: the St James women take heart project. Circulation. 2003;108(13):1554‐1559. [DOI] [PubMed] [Google Scholar]
- 20. Myers J, Prakash M, Froelicher V, Do D, Partington S, Atwood JE. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med. 2002;346(11):793‐801. [DOI] [PubMed] [Google Scholar]
- 21. Kodama S, Saito K, Tanaka S, et al. Cardiorespiratory fitness as a quantitative predictor of all‐cause mortality and cardiovascular events in healthy men and women: a meta‐analysis. JAMA. 2009;301(19):2024‐2035. [DOI] [PubMed] [Google Scholar]
- 22. Ekelund LG, Haskell WL, Johnson JL, Whaley FS, Criqui MH, Sheps DS. Physical fitness as a predictor of cardiovascular mortality in asymptomatic north American men. The lipid research clinics mortality follow‐up study. N Engl J Med. 1988;319(21):1379‐1384. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Predictors for improvement in fitness capacity among patients with AF
Figure S2. Multivariate analysis comparing patients with AF based on their baseline and improvement, taking patients with low baseline fitness level and low improvement as the reference group


