Abstract
Background
The rate of pacemaker (PM) implantations is constantly growing. Since life expectancy of the population is projected to increase, a large number of nonagenarian patients will need PM implantation. We aimed at analyzing short‐ and long‐term outcomes after PM implantation in nonagenarians.
Methods
Patients aged ≥90 years referred for PM implantation from 2004 to 2017 were included. The primary clinical endpoint was total mortality. Secondary endpoints included procedure‐related and in‐hospital complications.
Results
A total of 172 patients were included (92.6 ± 2.1 years, from 90.0 to 101.4 years). Procedure duration was 50.0 ± 19.7 minutes. Most of the patients had VVI devices implanted (143 pts, 83.1%) and mean hospital stay was 3.5 ± 1.5 days. Nine patients (5.2%) had short‐term device‐related complications and 29 patients (16.8%) had post‐procedural complications, non‐related to the implantation, including four leading to patients' death. During a follow‐up of 22.5 months (interquartile range: 7.3‐38.0), 94 patients (54.7%) died. Survival rates were 82.9% (95% confidence interval [CI]: 76.0‐88.0), 73.7% (95% CI: 65.7‐80.1) and 37.5% (95% CI: 27.5‐47.5) after 1, 2, and 5 years, respectively. The Charlson comorbidity index was a predictive factor of procedural complications (odds ratio = 1.33; 95% CI: 1.05‐1.69, P = 0.02) while having a complication (hazard ratio [HR] = 4.04; 95% CI: 1.79‐9.11, P = 0.001) and atrial fibrillation (HR = 1.63; 95% CI: [1.02‐2.63], P = 0.043) were predictors of post‐implantation death.
Conclusion
PM implantation in nonagenarians is safe, with a low risk of procedural complications, but many comorbidities‐related complications can occur. Caution should be taken in this old and frail population since complications significantly impact patients' survival.
Keywords: complications, nonagenarian, pacemaker
ABBREVIATIONS
- AF
atrial fibrillation
- AV
atrioventricular
- CCI
Charlson comorbidity index
- CI
confidence interval
- CRT
cardiac resynchronization therapy
- CRT‐P
cardiac resynchronization therapy‐Pacemaker
- OR
odds ratio
- HR
hazard ratio
1. INTRODUCTION
The implantation rate of pacemakers (PM) is increasing significantly each year exceeding 1 million devices implanted in 2016.1 This increase is because in part to the aging of the population, which causes an increased risk to develop atrioventricular (AV) block and sinus node dysfunction, and also related to the expansion of cardiac resynchronization therapy (CRT) indications or His ablation for heart rate control in patients with atrial fibrillation (AF).
The mean age at device implantation is currently 80.2, 77, and 75.5 years old for single‐chamber, dual‐chamber and CRT devices, respectively.2 In 2016, life expectancy at birth in Europe was 81 years for the general population, reaching 83.6 and 78.2 years for women and men, respectively.3 Over the past 50 years, it has increased by about 10 years. By 2060, life expectancy is projected to be 89.1 and 84.6 years for female and male, respectively, and the number of patients aged 80 and more is expected to be double. Currently, only few studies specifically reported the long‐term outcome of PM implantation in elderly patients. Mandawat et al. evaluated the short‐term mortality and complications of PM implantation in elderly patients, reporting 1.87% and 6.31% mortality and complications rates in nonagenarians, respectively.4 Also, Udo et al. studied outcome of PM recipients aged >80 and reported a cumulative 5‐year survival of around 50% after implantation, with an 18.1% complication rate.5 More recently, Loirat et al. described short‐ and long‐term outcomes of PM replacement in nonagenarians, reporting AF and non‐physiological pacing as predictors of mortality.6 However, no studies specifically evaluated the short‐ and long‐term outcomes of PM primo‐implantation in nonagenarian. Therefore, in the present study, we aimed at analyzing the procedural characteristics, survival rate, and causes of deaths in nonagenarians.
2. METHODS
2.1. Study population and data collection
Consecutive patients aged >90 years referred to our tertiary center for device implantation from January 2004 to December 2017 were retrospectively enrolled. The study was approved by local ethical committee and all patients gave their informed consent to participate.
Clinical information was obtained from patients' medical records, which included patient demographics, medical history, and medication use. “Physiological pacing” was defined as the implantation of a dual‐chamber PM or CRT in patients in sinus rhythm and single‐chamber PM for patients in AF, while “non‐physiological pacing” was defined as the implantation of a VVI chamber device in patients in sinus rhythm. The Charlson comorbidity index (CCI), a validated score to assess patients' comorbidities, was evaluated using dedicated scales available online.7, 8 Various CCI have been proposed, depending on the number of variables included. We decided, as previously performed by Mandawat et al. in their study about elderly PM recipients, to use the one not including age, since all our patients were >90 years.4
Procedural characteristics of the device implantation were recorded, including indication of pacing, the type of PM implanted, the hospital length stay, and the procedural complications. Procedural complications included lead‐related re‐interventions for displacement or dysfunction, hematoma requiring re‐intervention, pneumothorax requiring drainage, hemothorax, pericardial effusion because of cardiac perforation, and PM‐related systemic infections or endocarditis.
2.2. Follow‐up and outcomes
Clinical follow‐up data were obtained from clinical visits, or telephone interviews of patients or their families, general practitioners or nurses. The primary clinical endpoint was total mortality over the follow‐up period.
Causes of death were obtained through hospital discharge notes, inquiries made with the family, the general practitioner or nursing homes, and classified using the International Statistical Classification of Diseases and Related Health Problems classification (ICD‐10), as cardiovascular cause (I00‐I99), pulmonary cause (J00‐J99), digestive cause (K00‐K93), neoplasic cause (C00‐D48), renal cause (N00‐N99), because of a multiple organ dysfunction (R65‐10) or from an unknown origin (R99). Deaths were classified as unknown when no specific cause could be identified. Patients lost to follow‐up were censored as alive the day of the last visit. Secondary endpoints included procedure‐related and in‐hospital complications.
2.3. Statistical analyses
Data are summarized as frequencies and percentages for categorical variables. Quantitative variables are expressed as mean ± SD or median (interquartile range [IQR]) for non‐normally distributed variables. Qualitative data were compared using Fisher exact test, while quantitative data were compared using the Mann‐Whitney test. Survival curves were estimated using the Kaplan‐Meier method, with log‐rank tests for comparisons. The prognostic relevance of different characteristics on long‐term survival was assessed in univariate and multivariate fashion using Cox's proportional hazards regression analysis. All the values with a P ≤ 0.2 in univariate analysis were used for multivariate analysis. All tests were two‐sided at the 0.05 significance level. All statistical analyses were carried out with the SPSS for Windows, version 16.0 (SPSS Inc., Chicago, Illinois).
3. RESULTS
3.1. Study population
From January 2004 to December 2017, 172 nonagenarian patients were referred for PM implantation. Patients' characteristics are described in Table 1. The median age of patients included was 91.9 years (IQR 90.9‐93.7; from 90.0 to 101.4 years) at the time of PM implantation, and 67 (39.8%) were male. A total of 45 patients (26.2%) were living in nursing homes at the time of implantation and the median CCI was 2.0 (1.0‐3.5).
Table 1.
Characteristics and comparison between nonagenarians with and without complication during hospitalization
| General population N = 172 | No complication N = 136 | Complication N = 36 | P | |
|---|---|---|---|---|
| Age (years) | 91.9 (90.9‐93.7) | 92.1 (90.9‐94.1) | 91.5 (90.9‐93.4) | 0.584 |
| Male, n (%) | 67(39.0%) | 54 (39.7%) | 13 (36.1%) | 0.593 |
| Patients living in nursing home, n (%) | 45 (26.2%) | 36 (26.5%) | 9 (25.0%) | 0.972 |
| Body mass index (kg/m2) | 23.0 (21.1‐25.9) | 23.1 (21.1‐25.8) | 22.4 (20.8‐26.0) | 0.693 |
| Indication of implantation, n (%) | ||||
| High degree AV block | 144 (83.7%) | 114 (82.8%) | 30 (83.3%) | 0.923 |
| Sinus node dysfunction | 14 (8.1%) | 10 (7.4%) | 4 (11.1%) | |
| Sick‐sinus syndrome | 8 (4.7%) | 7 (5.2%) | 1 (2.8%) | |
| High rate AF with AV junction ablation | 4 (2.3%) | 3 (2.2%) | 1 (2.3%) | |
| Carotid sinus hypersensitivity | 1 (0.6%) | 1 (0.74%) | 0 (0%) | |
| CRT‐P for heart failure | 1 (0.6%) | 1 (0.74%) | 0 (0%) | |
| Type of PM, n (%) | ||||
| Single chamber VVI | 143 (83.1%) | 112 (82.4%) | 31 (86.1%) | 0.926 |
| Dual chamber DDD | 26 (15.1%) | 21 (15.4%) | 5 (13.9%) | |
| Single chamber AAI | 1 (0.6%) | 1 (0.7%) | 0 (0%) | |
| VDD | 1 (0.6%) | 1 (0.7%) | 0 (0%) | |
| CRT‐P | 1 (0.6%) | 1 (0.7%) | 0 (0%) | |
| Physiologic stimulation, n (%) | 58 (33.7%) | 47 (34.6%) | 11 (30.6%) | 0.800 |
| Subclavian puncture, n (%) | 61 (35.5%) | 51 (37.5%) | 10 (27.8%) | 0.374 |
| Duration of procedure (minutes) | 50.0 (35.0‐60.0) | 49.0 (35.0‐60.0) | 50.0 (38.5‐70.0) | 0.202 |
| Mean hospital stay (days) | 3.5 (2.0‐7.0) | 3.0 (2.0‐6.0) | 6.5 (3.0‐9.0) | <0.001 |
| Heart rhythm at the time of implantation, n (%) | ||||
| Sinus rhythm | 136 (79.1%) | 107 (78.7%) | 29 (80.6%) | 0.987 |
| AF | 36 (20.9%) | 29 (21.3%) | 7 (19.4%) | |
| Cardiomyopathy, n (%) | ||||
| Valvular | 35 (20.3%) | 28 (20.6%) | 7 (19.4%) | 0.931 |
| Ischemic | 31 (18.0%) | 23 (16.9%) | 8 (22.2%) | |
| Hypertrophic | 14 (8.1%) | 11 (8.1%) | 3 (8.3%) | |
| Primary dilated | 8 (4.7%) | 7 (5.2%) | 1 (2.8%) | |
| Tachycardia‐induced cardiomyopathy | 1 (0.6%) | 1 (0.7%) | 0 (0.0%) | |
| Pulmonary hypertension | 1 (0.6%) | 1 (0.7%) | 0 (0.0%) | |
| Unknown (no TTE performed) | 48 (27.9%) | 35 (25.7%) | 13 (36.1%) | |
| Comorbities, n (%) | ||||
| History of AF | 58 (33.7%) | 45 (33.1%) | 13 (36.1%) | 0.870 |
| Diabetes mellitus | 17 (9.9%) | 13 (9.6%) | 4 (11.1%) | 0.971 |
| Hypertension | 107 (62.2%) | 84 (61.8%) | 23 (63.9%) | 0.968 |
| History of stroke | 29 (16.9%) | 22 (16.2%) | 7 (19.4%) | 0.829 |
| Heart failure | 56 (32.6%) | 42 (30.9%) | 14 (38.9%) | 0.477 |
| Valvular disease | 43 (25.0%) | 34 (25.0%) | 9 (25.0%) | 0.829 |
| Coronary artery disease | 41 (23.8%) | 32 (23.5%) | 9 (25.0%) | 0.971 |
| Cardiac surgery | 15 (8.7%) | 10 (7.4%) | 5 (13.9%) | 0.366 |
| Median Charlson comorbidity index | 2.0 (1.0‐3.5) | 2.0 (1.0‐3.0) | 3.0 (1.5‐4.0) | |
| Charlson comorbidity index | ||||
| 0 | 33 (19.2%) | 33 (24.3%) | 0 (0%) | 0.003 |
| 1 | 37 (21.5%) | 28 (20.6%) | 11 (29.7%) | |
| 2 | 25 (14.5%) | 22 (16.2%) | 3 (8.1%) | |
| 3 | 34 (19.8%) | 21 (15.4%) | 13 (35.1%) | |
| 4 | 21 (12.2%) | 17 (12.5%) | 4 (10.8%) | |
| 5 | 14 (8.1%) | 11 (8.1%) | 3 (8.1%) | |
| 6 | 1 (0.5%) | 1 (0.7%) | 0 (0%) | |
| 7 | 6 (1.7%) | 3 (2.2%) | 3 (8.1%) | |
| 8 | 1 (0.5%) | 0 (0%) | 0 (0%) | |
| Treatments, n (%) | ||||
| No antithrombotic treatment | 55 (32.0%) | 45 (33.1%) | 10 (27.8%) | 0.713 |
| Anticoagulants | 43 (25.0%) | 32 (23.5%) | 11 (30.6%) | |
| Antiplatlet agents | 82 (47.7%) | 65 (47.8%) | 17 (47.2%) | |
| Association AC and AP agent | 8 (4.7%) | 6 (4.4%) | 2 (5.6%) | |
| Number of medications | 5.0 (3.0‐7.0) | 5.0 (3.0‐7.0) | 6.5 (4.5‐8.0) | 0.02 |
| Blood work | ||||
| Hemoglobin level (g/dL) | 12.2 (11.3‐13.0) | 12.2 ± 1.4 | 11.8 ± 1.7 | 0.166 |
| Creatinine level (μmol/L) | 102.5 (80.0‐132.0) | 101.0 (81.0‐131.5) | 111.0 (73.8‐143.8) | 0.543 |
Abbreviations: AF, atrial fibrillation; AV, atrio‐ventricular; CRT‐P, cardiac resynchronization therapy‐pacemaker; PM, pacemaker.
The main indication for implantation was high‐degree AV block (144 patients, 83.7%). The other indications were sinus node dysfunction, sick‐sinus syndrome, high‐rate AF with AV junction ablation, carotid sinus hypersensitivity, and CRT for heart failure.
3.2. Procedural characteristics and short‐term outcome
Procedures were short, lasting for a median time of 50.0 (IQR 35.0‐60.0) minutes, and all were performed with local anesthesia using mild sedation. Median hospital stay was 3.5 days (IQR 2.0‐7.0, from 1 to 30 days). Most of the patients had single‐chamber PM implanted (143 patients, 83.1%) and pacing was considered as “physiologic” only for 58 (33.7%), since most of the patients were in sinus rhythm on time of implantation (136 patients, 79.1%) and devices implanted mostly VVI PMs (83.1%).
To note, at the time of device implantation, many of the patients were under antithrombotic therapy with anticoagulant, antiplatelet therapies, or both (25.0%, 47.7%, and 4,7% respectively), and the median number of drugs taken by the patients was 5.0 (3.0‐7.0).
Regarding the complications of the procedure (Table 2), four patients had a pocket hematoma, none of them requiring a surgical revision. Three patients had a lead displacement requiring a redo intervention, and one got a pneumothorax. One patient had a hemothorax and needed a surgical drainage and a prolonged hospitalization (24 days).
Table 2.
Procedure and in‐hospital related complications, mortality and causes of death during the follow‐up
| Complications/number of patients, n (%) | 36 (20.9%) |
| Procedure‐related | |
| Lead displacement | 3 (8.3%) |
| Hematoma | 3 (8.3%) |
| Pericardial effusion | 2 (5.6%) |
| Hemothorax | 1 (2.8%) |
| Pneumothorax | 0 (0%) |
| In‐hospital | |
| Congestive heart failure | 9 (25.6%) |
| Transient confusion | 3 (8.3%) |
| Stroke | 2 (5.6%) |
| Acute myocardial infarction | 1 (2.8%) |
| Fall | 1 (2.8%) |
| Pneumonia | 4 (11.1%) |
| Urinary tract infection | 1 (2.8%) |
| Renal failure | 4 (11.1%) |
| Geriatric cachexia | 1 (2.8%) |
| Delayed | |
| Endocarditis | 1 (2.8%) |
| Deaths/number of patients, n (%) | 94 (54.7%) |
| Causes of deaths | |
| Unknown | 52 (55.3%) |
| Cardiac | 17 (18.1%) |
| Pulmonary | 5 (5.3%) |
| Digestive | 3 (3.2%) |
| Stroke | 7 (7.5%) |
| Severe infection | 4 (4.3%) |
| Neoplasia | 2 (2.1%) |
| Multiple organ dysfunction syndrome | 1 (1.1%) |
| Renal failure | 1 (1.1%) |
| Geriatric cachexia | 1 (1.1%) |
Twenty‐six patients (16.2%) had post‐procedural complications, non‐related to the implantation (Table 2): nine patients had congestive heart failure (8.0%) regressive after medical therapy, but leading to one death. The other complications were transient confusion for two patients, pneumonia for two patients, and renal failure for one patient. A 97‐year‐old woman had a femoral fracture after a fall following PM implantation and one patient in AF had an embolic stroke. For all these patients, the complication extended the duration of hospital stay to 6.5 days (IQR 3.0‐9.0, P < 0.001). There was a significant difference in CCI between nonagenarians with or without procedure complication (Table 1). Indeed, as shown in Figure 1A, the higher the CCI, the higher the risk of per‐ or post‐procedural complications. Furthermore, the CCI was found to be the only predictor of post‐implantation complications (Table 3) in multivariate analysis (odds ratio (OR) = 1.33; 95% confidence interval (CI): (1.05‐1.69) per 1 unit increase, P = 0.02).
Figure 1.
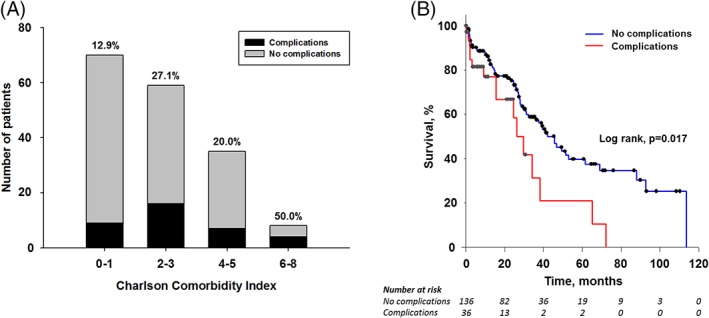
A, Complication rate depending of Charlson comorbidity index and Kaplan B, Meier survival curve depending of the occurrence of a per‐ or post‐procedural complication
Table 3.
Logistic regression for all‐cause complications in pacemaker recipients above 90 years of age
| Logistic regression for complications | Univariate OR (95% CI) | P | Multivariable OR (95% CI) | P |
|---|---|---|---|---|
| Number of medications | 1.17 (1.02‐1.34)a | 0.022 | 1.10 (0.94‐1.29)a | 0.22 |
| Charlson score | 1.35 (1.11‐1.64)b | 0.003 | 1.33 (1.05‐1.69)b | 0.02 |
| Hemoglobin on admission | 0.84 (0.65‐1.09)c | 0.19 | 0.95 (0.71‐1.27) | 0.72 |
| Sub‐clavian approach | 0.55 (0.24‐1.25) | 0.15 | 0.55 (0.22‐1.36) | 0.20 |
Abbreviation: OR, odds ratio.
Per each additional treatment, reference: 1.
Per 1 unit increase.
Per 1 g/dL increase.
Four nonagenarians (2.3%) died before the leaving hospital: two patients of severe geriatric cachexia, one of a myocardial infarction and one of a cerebral hemorrhage.
3.3. Long‐term follow‐up
The median time of follow‐up was 22.5 months (IQR 7.1‐37.1). Twelve patients (6.7%) were lost of follow‐up, and censored as alive the day of the last visit.
During the follow‐up, 94 patients died (54.7%), and one patient was still alive after more than 9 years of follow‐up. Causes of death are described in Table 2. The median time of survival was 22.5 months (95% CI 7.3‐38 months). The survival at 1, 2, and 5 years were 82.9% (95% CI: 76.0‐88.0%), 73.7% (95% CI: 65.7‐80.1%), and 37.5% (95% CI: 27.5‐47.5%), respectively. Seventeen patients (18.1%) died from a cardiovascular cause, mainly because of heart failure (14 patients, among which pacing was considered “physiologic” in only 6). Despite inquiries made with the general practitioner or medical service in case of patients living in nursing homes, 52 deaths remained of unknown cause (55.3%). To note, one patient with an aortic mechanic valve had an endocarditis (Streptococcus gallolyticus) 3 months after the implantation of the PM, leading to patients' death few weeks later.
3.4. Predictors of mortality
Predictors for all‐cause mortality in univariate and multivariate analysis are shown in Table 4. In univariate analysis, there was an increased mortality risk depending on a history of AF (hazard ratio [HR] = 1.80, 95%CI: 1.17‐2.77, P = 0.08), on the presence of an ischemic or a valvular cardiomyopathy (HR = 2.48, 95% CI: 1.18‐5.24 P = 0.0.17 and HR = 2.13, 95% CI: 1.07‐4.26, P = 0.032) and on complications after PM procedure (HR = 2.17, 95% CI: 1.31‐3.61, P = 0.003). Moreover in univariate analysis, the number of medications (HR = 1.12, 95% CI: 1.03‐1.22, P = 0.01) per each additional treatment, the CCI (HR = 1.19 per unit increase, 95% CI: 1.06‐1.33, P = 0.003) and AF (HR = 1.80, 95% CI: 1.17‐2.77, P = 0.008) were significant predictors of mortality.
Table 4.
Cox regression for all‐cause mortality in pacemaker recipients above 90 years of age
| Cox regression for mortality | Univariate HR(95% CI) | P | Multivariable HR (95% CI) | P |
|---|---|---|---|---|
| Male sex | 1.37 (0.90‐2.08) | 0.14 | 0.96 (0.60‐1.55) | 0.87 |
| Physiological pacing | 1.55 (0.995‐2.44) | 0.052 | 1.12 (0.67‐1.87) | 0.67 |
| Cardiomyopathy | — | 0.09 | — | 0.27 |
| Ischemic | 2.48 (1.18‐5.24) | 0.017 | 2.09 (0.94‐4.66) | 0.07 |
| Valvular | 2.13 (1.07‐4.26) | 0.032 | 1.94 (0.93‐4.04) | 0.08 |
| Other | 1.79 (0.96‐3.35) | 0.069 | 1.68 (0.88‐3.20) | 0.12 |
| Atrial fibrillation | 1.80 (1.17‐2.77) | 0.008 | 1.63 (1.02‐2.63) | 0.043 |
| Prior stroke | 1.53 (0.92‐2.54) | 0.10 | 1.40 (0.78‐2.51) | 0.26 |
| Complication during index hospitalization | 2.17 (1.31‐3.61) | 0.003 | 4.04 (1.79‐9.11) | 0.001 |
| Number of medications | 1.12 (1.03‐1.22)a | 0.01 | 1.06 (0.97‐1.16)a | 0.24 |
| Charlson score | 1.19 (1.06‐1.33)b | 0.003 | 1.08 (0.95‐1.24) ) | 0.24 |
| Timea complications interaction | — | — | 0.96 (0.92‐1.002) | 0.059 |
Abbreviation: HR, hazard ratio.
Per each additional treatment, reference: 1.
Per 1 unit increase.
In multivariate analysis, a complication during hospitalization (OR = 4.04, 95% CI: 1.79‐9.11, P = 0.001) and a history of AF (OR = 1.63, 95% CI: 1.02‐2.63, P = 0.043) were the only predictive factors of mortality. Neither the other comorbidities nor CCI was predictors of mortality. Kaplan‐Meier survival curves depending on the occurrence of complications are shown in the figure, panel B.
4. DISCUSSION
4.1. Main results
The main findings of this study are the following: (a) PM implantation in nonagenarians is a straightforward procedure in patients >90 years, but carries a significant risk of pre‐ and post‐procedural complications, (b) many comorbidities can affect post‐operative period and prolong the hospitalization, (c) The CCI is a predictive factor of post‐operative complications, and (d) post‐operative complications and AF are predictors of mortality.
4.2. Nonagenarians in the general population
The percentage of nonagenarians is expected to increase in next decades, and according to the American Social Security Administration, one out of every four 65‐year olds today will live past age 90, and one out of 10 will live past 95. In the United States, the number of nonagenarians has increased from approximately 230 000 in 1960 to approximately 1.8 million in 2010, and in the five biggest countries in the European Union (Germany, France, the United Kingdom, Italy, and Spain) the number has increased from approximately 250.000 to 1.6 million.9 This frail population is at high risk of symptomatic high degree AV block and sinus node dysfunction requiring PM implantation.
4.3. Safety of the procedure
Many short‐term complications are described after PM implantation like hematoma, device‐related infection, lead dislodgment, device extrusion, or pericardial effusion.5 They affect approximately up to 9.5% of device recipients.10 Kirkfeldt et al. analyzed all procedure of electronic device implantations in Denmark regardless of age. Lead‐related re‐intervention was the most common complication (2.4%).10 In elderly patients (>80 years), the risk of any lead‐related re‐intervention was lower than for patients between 60 and 79 years (1% vs 3.1%, P < 0.001).Similarly, Udo et al. reported a significant 9.8% and 6.9% rate of complications in octagenarians, mostly lead‐related, within 2 months and during long‐term follow‐up, respectively.5 Similarly, very elderly patients did not seem to have more complications than younger patients in other studies.10, 11 On the contrary, Ozcan et al. demonstrated that the complication rate for elderly patients who had a permanent PM implantation was statistically lower than in patients who were <70 years.12 However, in the largest epidemiologic study published so far about PM implantations, in the nonagenarians subgroup, including more than 12 000 patients from the Healthcare Cost and Utilization Project Nationwide Inpatient Sample administrative database, Mandawat et al. demonstrated 1.87% and 6.31% mortality and complication rates, respectively, modestly but significantly more than in septuagenarians and octogenarians. These frail patients also had a significantly longer hospital stay than younger patients, whose cost was estimated to be more than $41 000. Severe comorbidities and older age were strong predictors of mortality.4 Various parameters may explain the higher rate of complications observed in elderly patients, including tortuous venous anatomy making lead placement sometimes challenging.13 This may explain the higher rate of pneumothorax observed in the PASE trial in patients aged >75 years.14 Elderly patients also have a thinner right ventricular wall, increasing the risk of cardiac perforation. Ventricular lead should be carefully placed to reduce this risk. In our study, 5.2% had early complications. No hematoma requiring re‐intervention was noted during the follow‐up period. Three patients had a lead displacement requiring a redo intervention and one had a hemothorax needing a surgical drainage and a prolonged hospitalization. Twenty‐six patients (15.1%) had post‐procedural complications, non‐related to the implantation. This important rate of complications was related to nonagenarians' fragility, directly correlated to the CCI. As described, nearly 50% of the nonagenarians with a CCI between 6 and 8 had post‐procedural complication. For all these patients, the complication extended the duration of hospital stay.
4.4. Long‐term survival
Among the study population, 92 patients (54.7%) died, mainly from unknown or cardiovascular causes, and survival rates were 82.9%, 73.7%, and 37.5% after 1, 2, and 5 years, respectively, and median time of survival was 22.5 (95% CI: 7.1‐37.1 months). These survival rates are quite similar to what has been previously described by Udo et al. in a population of octogenarians and nonagenarians implanted with PMs (86%, 75%, and 49% after 1, 2 and 5 years, respectively),4 In a prospective community‐based study, Formiga et al. found that better cognitive status and lesser comorbidities (evaluated by the CCI) were the best predictors to identify which nonagenarians will die after a 5‐year follow‐up period.15 In the present study, univariable analysis showed that CCI, number of medication, AF, and complications during hospitalization are predictors of mortality. In multivariable analysis, the CCI was the only predictive factor of post‐procedure complications. AF and complications were significant predictive factors of mortality for nonagenarians.
4.5. Pacing mode in nonagenarians
The optimal pacing mode has been, for a while, a matter of debate. In 2005, the United Kingdom Pacing and Cardiovascular Events (UKPACE) study showed that in elderly (>75 years) patients with high‐degree AV block, the pacing mode (VVI or DDD) did not influence the rate of deaths from all causes and the incidence of cardiovascular events.16 Healey et al. published a meta‐analysis about pacing modes to analyze whether an atrial‐based pacing mode was associated with better long‐term outcomes in device recipients, including UKPACE16 and four large studies (Canadian Trial of Physiological Pacing (CTOPP),17 Mode Selection Trial (MOST),18 Pacemaker Selection in the Elderly (PASE)14 and the Danish trial19, 20). The authors showed that compared with ventricular pacing, the use of atrial‐based pacing does not improve survival or reduce heart failure or cardiovascular death. Jahangir et al.21 describe that in very elderly patients (≥80 years), the mode of pacing was not found to be a predictor of all‐cause mortality. However, these results were contradicted by Krzemień‐Wolska et al. in a recent paper22 that showed that DDD mode pacing decreased mortality among patients aged >80 years in long‐term follow‐up, and by Loirat et al. found that non‐physiological pacing was a predictor of mortality in nonagenarians scheduled for PM replacement,6 In the present study, only 58 patients (33.7%) had a physiological stimulation, but there was no significant difference in terms of mortality between non‐physiological stimulation in univariate analysis neither in multivariate analysis.
4.6. Limitations
We acknowledge some limitations in our study. Our analysis was performed as a retrospective review of a cohort of patients, with the inherent limitations of such studies (ie, some patients were lost of follow‐up). Because of the retrospective nature of the study, only in‐hospital complications could be carefully collected and described. Out‐of‐hospital complications, except device‐related endocarditis in one patient, could not be gathered and detailed in the manuscript. Furthermore, the limited number of patients may not allow a precise determination of predictive factors of mortality.
As stated above, some patients developed heart failure during the study period. However, none of them were scheduled for CRT‐P implantation, and all were treated medically. Although this attitude is questionable, patients were considered too frail and/or too elderly to undergo a left ventricular lead implantation, and so, we cannot draw conclusions about device upgrade in nonagenarians. Moreover, a potential deleterious effect of right ventricular pacing on left ventricular function cannot be excluded in these patients. The pacing burden was not collected in the present study, so we cannot incriminate with certainty the pacing as the cause of heart failure development.
The rate of VVI, DDD or other device type was similar among groups (P = 0.926). One would probably expect higher risk of complications in patients with more than one single lead implanted, but our study was probably underpowered to show such effect.
Lastly, despite inquiries made with the general practitioner or medical service in case of nursing homes, 52 (55.3%) deaths remained from unknown cause, patients for whom the devices were not interrogated post‐mortem.
5. CONCLUSION
PM implantation in nonagenarians is a straightforward procedure, but carries a significant risk of complications occurring during the hospitalization. Many comorbidities‐related complications can occur in this old and frail population, that eventually major the risk of mortality.
CONFLICTS OF INTERESTS
The authors declare no potential conflict of interests.
Dang D, Galand V, Loirat A, et al. Procedural safety and long‐term follow‐up after pacemaker implantation in nonagenarians. Clin Cardiol. 2018;41:1315–1321. 10.1002/clc.23083
REFERENCES
- 1. https://www.statista.com/statistics/800794/pacemakers-market-volume-in-units-worldwide/.
- 2. Tuppin P, Neumann A, Marijon E, et al. Implantation and patient profiles for pacemakers and cardioverter‐defibrillators in France (2008‐2009). Arch Cardiovasc Dis. 2011;104:332‐342. [DOI] [PubMed] [Google Scholar]
- 3. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Mortality_and_life_expectancy_statistics#Life_expectancy_at_birth_increased_in_2016
- 4. Mandawat A, Curtis JP, Njike VY, Lampert R. Safety of pacemaker implantation in nonagenarians: an analysis of the healthcare cost and utilization project‐nationwide inpatient sample. Circulation. 2013;127:1453‐1465. 65e1‐2. [DOI] [PubMed] [Google Scholar]
- 5. Udo EO, van Hemel NM, Zuithoff NPA, et al. Long‐term outcome of cardiac pacing in octogenarians and nonagenarians. Europace. 2012;14:502‐508. [DOI] [PubMed] [Google Scholar]
- 6. Loirat A, Fénéon D, Behaghel A, et al. Pacemaker replacement in nonagenarians: procedural safety and long‐term follow‐up. Arch Cardiovasc Dis. 2015;108(6–7):367‐374. [DOI] [PubMed] [Google Scholar]
- 7. Charlson ME, Pompei P, Ales KL, CR MacKenzie. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373‐83. [DOI] [PubMed] [Google Scholar]
- 8. Hall WH, Ramachandran R, Narayan S, Jani AB, Vijayakumar S. An electronic application for rapidly calculating Charlson comorbidity score. BMC Cancer. 2004;4:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Thinggaard M, McGue M, Jeune B, Osler M, Vaupel JW, Christensen K. Survival prognosis in very old adults. J Am Geriatr Soc. 2016. Jan;64(1):81‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kirkfeldt RE, Johansen JB, Nohr EA, Jorgensen OD, Nielsen JC. Complications after cardiac implantable electronic device implantations: an analysis of a complete, nationwide cohort in Denmark. Eur Heart J. 2014;35:1186‐1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Eberhardt F, Bode F, Bonnemeier H, et al. Long term complications in single and dual chamber pacing are influenced by surgical experience and patient morbidity. Heart. 2005;91:500‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ozcan KS, Osmonov D, Altay S, et al. Pacemaker implantation complication rates in elderly and young patients. Clin Interv Aging. 2013;8:1051‐1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Armaganijan LV, Toff WD, Nielsen JC, et al. Are elderly patients at increased risk of complications following pacemaker implantation? A meta‐analysis of randomized trials. Pacing Clin Electrophysiol. 2012;35:131‐134. [DOI] [PubMed] [Google Scholar]
- 14. Lamas GA, Orav EJ, Stambler BS, et al. Quality of life and clinical outcomes in elderly patients treated with ventricular pacing as compared with dual‐chamber pacing. Pacemaker selection in the elderly investigators. N Engl J Med. 1998;338:1097‐1104. [DOI] [PubMed] [Google Scholar]
- 15. Formiga F, Ferrer A, Chivite D, Rubio‐Rivas M, Cuerpo S, Pujol R. Predictors of long‐term survival in nonagenarians: the NonaSantfeliu study. Age Ageing. 2011;40:111‐116. [DOI] [PubMed] [Google Scholar]
- 16. Toff WD, Camm AJ, Skehan JD, United Kingdom Pacing and Cardiovascular Events Trial Investigators . Single‐chamber versus dual‐chamber pacing for high‐grade atrioventricular block. N Engl J Med. 2005;353:145‐155. [DOI] [PubMed] [Google Scholar]
- 17. Kerr CR, Connolly SJ, Abdollah H, et al. Canadian trial of physiological pacing: effects of physiological pacing during long‐term follow‐up. Circulation. 2004;109:357‐362. [DOI] [PubMed] [Google Scholar]
- 18. Lamas GA, Lee KL, Sweeney MO, et al. Ventricular pacing or dual‐chamber pacing for sinus‐node dysfunction. N Engl J Med. 2002;346:1854‐1862. [DOI] [PubMed] [Google Scholar]
- 19. Andersen HR, Nielsen JC, Thomsen PEB, et al. Long‐term follow‐up of patients from a randomised trial of atrial versus ventricular pacing for sick‐sinus syndrome. Lancet. 1997;350:1210‐1216. [DOI] [PubMed] [Google Scholar]
- 20. Andersen HR, Thuesen L, Bagger JP, Vesterlund T, Thomsen PEB. Prospective randomised trial of atrial versus ventricular pacing in sick‐sinus syndrome. Lancet. 1994;344:1523‐1528. [DOI] [PubMed] [Google Scholar]
- 21. Jahangir A, Shen WK, Neubauer SA, et al. Relation between mode of pacing and long‐term survival in the very elderly. J Am Coll Cardiol. 1999;33:1208‐1216. [DOI] [PubMed] [Google Scholar]
- 22. Krzemień‐Wolska K, Tomasik A, Wojciechowska C, Barańska‐Pawełczak K, Nowalany‐Kozielska E, Jacheć W. Prognostic factors in patients with an implanted pacemaker after 80 years of age in a 4‐year follow‐up. Gerontology. 2018;64:107‐117. [DOI] [PubMed] [Google Scholar]


