Abstract
Background
Transient pacing failure caused by transient increased pacing threshold has been reported in patients with transient left ventricular apical dysfunction (Takotsubo cardiomyopathy [TC]). Normal pacing thresholds usually recover after normalization of systolic dysfunction.
Hypothesis
Pacing failure correlates with clinics of TC.
Methods
We report the case of a 76‐year‐old man with a dual chamber pacemaker, admitted for acute chest pain and dyspnea and final diagnosis of TC. One month after index admission, the patient came back complaining again of chest pain. Unexpectedly, admission electrocardiogram showed ventricular pacing failure and an increased pacing threshold. In the following weeks, pacing threshold gradually recovered with left ventricular ejection fraction and QTc values.
Results
Ventricular pacing threshold correlated directly to QTc values and inversely to left ventricular ejection fraction over time (P < 0.05).
Conclusions
This is one of the first cases of delayed transient ventricular pacing failure in a male patient with transient left ventricular apical ballooning, in the presence of spared right ventricular function. Given the possibility of acute transient anomalies in myocardial impedance and pacing failure even in the subacute phase of TC several weeks after clinical onset of transient systolic dysfunction, pacing threshold should be carefully monitored in subjects with TC, both during the acute phase of the disease and in first months of follow‐up after discharge. Ventricular pacing threshold correlated directly to QTc values and inversely to left ventricular ejection fraction over time.
Keywords: male gender, myocardial edema, pacing failure, Takotsubo cardiomyopathy
1. INTRODUCTION
Transient pacing failure caused by transient increased pacing threshold has been reported in patients with transient left ventricular apical dysfunction, Takotsubo cardiomyopathy (TC).1 Normal pacing thresholds usually recover after normalization of systolic dysfunction.
2. CASE REPORT
We report the case of a 76‐year‐old man with history of coronary artery disease (prior coronary angioplasty 6 years earlier), sick sinus node disease, and paroxysmal atrial fibrillation, which was implanted with a dual chamber pacemaker. The patient was treated with ramipril, bisoprolol, aspirin, atorvastatin, and tamsulosin. Left ventricular function was found normal in all prior controls.
The patient was admitted to acute cardiac care unit complaining of acute chest pain and dyspnea. Admission electrocardiogram was non‐diagnostic in the presence of paced rhythm (Figure 1, negative T‐waves and QT prolongation); echocardiogram showed systolic dysfunction, left ventricular apical ballooning (left ventricular ejection fraction 35%), basal hyperkinesis, mild mitral regurgitation, and spared right ventricular function.
Figure 1.
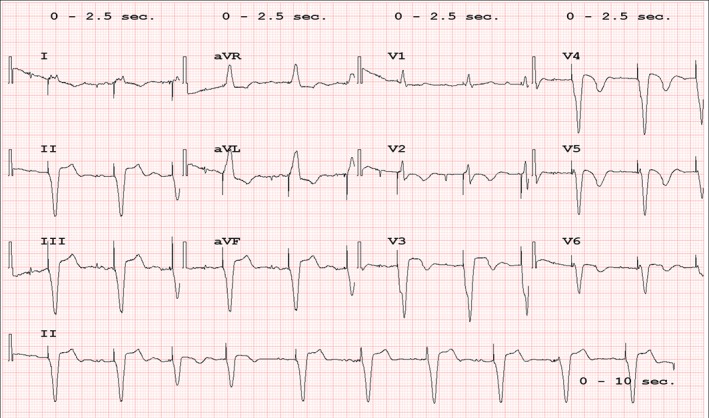
Admission electrocardiogram showing dual chamber paced rhythm, negative T‐waves, prolonged QTc, not conclusive for acute myocardial infarction
Coronary angiography did not reveal significant coronary stenosis or spasm and the final diagnosis was therefore TC. The patient was discharged 1 week later after partial recovery of left ventricular function (ejection fraction 40%). Peak troponin level was 1.62 ng/mL, C‐reactive protein 8.6 mg/L (n.v. <5), CA‐125 151 U/mL (n.v. <35), NT‐proBNP 9020 pg/mL (<125), potassium 3.4 mEq/L.
One month later, the patient came back complaining again of chest pain. Unexpectedly, admission electrocardiogram showed ventricular pacing failure (Figure 2) and an increased pacing threshold was found (2.2 V at 0.4 milliseconds with bipolar pacing while 6 months earlier the same figures were 0.6 V at 0.4 milliseconds at last control). Pacing output was accordingly increased to 4.4 V at 0.4 milliseconds as a precaution; other parameters were left unchanged in the presence of stable sensing threshold and catheter impedance (9 mV, 370‐400 Ω, Figure 3). Two weeks later, pacing threshold decreased to 1.7 V at 0.4 milliseconds and, finally, 2 weeks later to 1.5 V (Figure 3). Accordingly, left ventricular ejection fraction increased from 40% to 45%. QTc values directly and left ventricular ejection fraction values inversely correlated to ventricular pacing threshold over time (P < 0.05, Figure 4).
Figure 2.
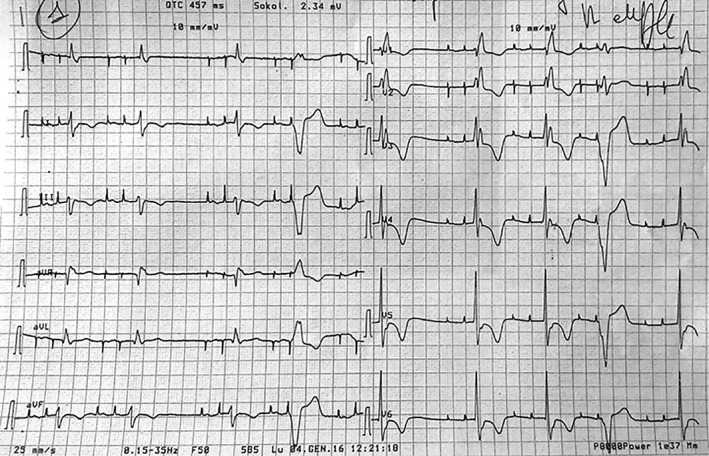
Admission electrocardiogram 1 month later showing transient ventricular pacing failure, right bundle branch block, negative T‐waves and QT‐prolongation
Figure 3.
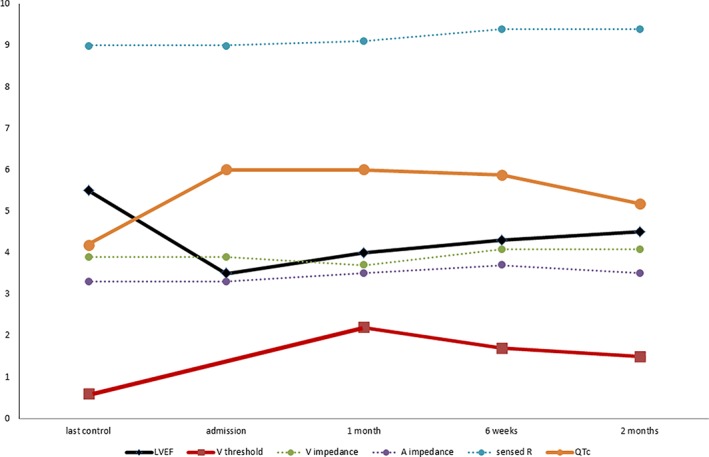
Pacing threshold, sensed R‐waves, ventricular lead impedance, and QTc values over time (ventricular pacing threshold in V, sensed R waved in mV, ventricular and atrial leads impedance in ×100 Ω, left ventricular ejection fraction in ×10%, QTc in ×100 milliseconds)
Figure 4.
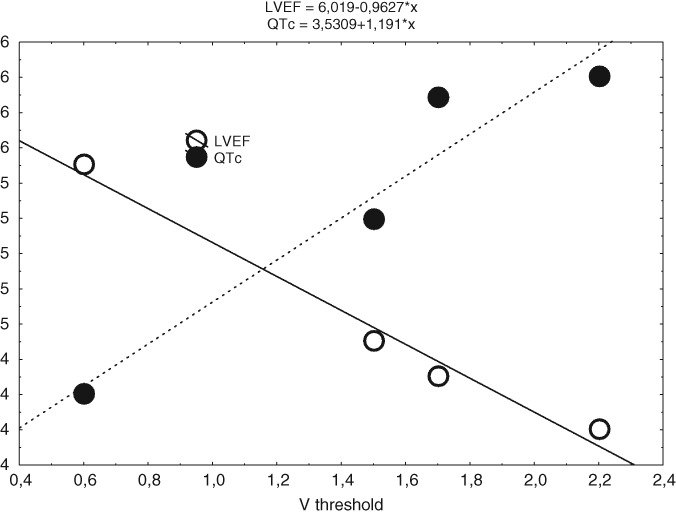
Linear regression between ventricular threshold, QT corrected and left ventricular ejection fraction (P < 0.05)
3. DISCUSSION
To the best of our knowledge, we report one of the first cases of delayed transient ventricular pacing failure in a male patient with transient left ventricular apical ballooning (TC), in the presence of spared right ventricular function.
Several cases of TC following pacemaker implantation have been reported,2, 3, 4 while just few cases of pacing failure during an episode of TC have been published so far, and all in female patients. In 2008, Wissner et al. described a case of reversible pacemaker dysfunction in a patient with transient cardiac apical ballooning syndrome, which responded to conservative therapy1; an 81‐year‐old woman with a dual‐chamber pacemaker and prior radiofrequency catheter ablation of the atrio‐ventricular node for the treatment or refractory atrial tachyarrhythmias. Her electrocardiogram showed ST‐segment elevation during the acute phase of TC and deeply inverted T‐waves. Ventricular dysfunction involved both the left and right apex. Pacing threshold doubled from 1.2 to 2.7 V, while sensed R‐wave amplitude halved from 8.9 to 5.2 mV, and ventricular pacing lead impedance from 1210 to 740 Ω. Pacing threshold and pacing lead impedance normalized a couple of weeks later.
Chikata et al. reported a case of repeated pacemaker dysfunction in a patient with recurrent TC precipitated by hyponatremia.5 Acute phase of TC was featured by negative T‐waves and marked QT‐prolongation.
Despite pacing failure is often precipitated by hyperkalemia,6 in our case, pacing failure was associated with lower potassium levels; either conditions (hypokalemia and hyperkalemia) have been reported in TC.7
We hypothesize that myocardial edema commonly found in TC8, 9 may have transiently influenced pacing threshold, which gradually improved with the recovery of left ventricular function. Significant correlation between QTc, a sign of myocardial edema, and ventricular pacing threshold seems to support this possible link. Local myocardial edema in dysfunctional areas of TC is considered responsible for acute electrocardiogram anomalies in TC (T‐wave inversion, QT‐prolongation, QRS complexes attenuation8, 10). There is evidence, indeed, that myocardial edema may increase local tissue impedance; thus, possibly accounting for increased pacing threshold, particularly, with bipolar pacing.11
The case also shows that right ventricular dysfunction in TC may be not essential for pacing failure, since myocardial edema of left ventricular wall may easily extend to right ventricular areas through inter‐ventricular septum and cardiac apex, where ventricles are strictly “in contact” and where pacemaker leads are usually placed.
Interestingly, we report a delayed case of pacing failure following after 4 weeks the clinical presentation of TC. Probably, delayed evidence of pacing failure may coincide with further delayed QT prolongation, which usually peaks in the subacute phase of TC rather than in the acute phase.12 Episodes of pacing failure may have anticipated second hospital admission, going possibly undiagnosed in the absence of continuous electrocardiogram monitoring after first hospital discharge. Alternatively, we must hypothesize that other conditions beyond QTc prolongation, presently not completely known and occurred after first hospital discharge, may have influenced ventricular threshold interacting with QT prolongation and leading to pacing failure (electrolyte anomalies, dehydration). A recurrent episode of TC should be excluded, in the absence of any worsening of ventricular function and any rise in troponin levels.
4. CONCLUSIONS
Given the possibility of acute transient anomalies in myocardial impedance and pacing failure even in the subacute phase of TC, several weeks after clinical onset of transient systolic dysfunction, pacing threshold should be carefully monitored in subjects with TC, both during the acute phase of the disease and in first months of follow‐up after discharge. Temporary increased pacing thresholds may be occasionally required to prevent pacing failure, when increased pacing threshold are found.
Ventricular pacing threshold correlated directly to QTc values and inversely to left ventricular ejection fraction over time.
CONFLICTS OF INTEREST
The authors declare no potential conflict of interests.
Brunetti ND, D'Arienzo G, Sai R, et al. Delayed ventricular pacing failure and correlations between pacing thresholds, left ventricular ejection fraction, and QTc values in a male with Takotsubo cardiomyopathy. Clin Cardiol. 2018;41:1487–1490. 10.1002/clc.23082
REFERENCES
- 1. Wissner E, Fortuin FD, Scott LR, Altemose GT. Reversible pacemaker dysfunction in a patient with transient cardiac apical ballooning syndrome: a case report. Europace. 2008;10:1105‐1107. [DOI] [PubMed] [Google Scholar]
- 2. Brunetti ND, Ieva R, Correale M, et al. Combined exogenous and endogenous catecholamine release associated with Tako‐Tsubo like syndrome in a patient with atrio‐ventricular block undergoing pace‐maker implantation. Acute Card Care. 2011;13:112‐114. [DOI] [PubMed] [Google Scholar]
- 3. Golzio PG, Anselmino M, Presutti D, Cerrato E, Bollati M, Gaita F. Takotsubo cardiomyopathy as a complication of pacemaker implantation. J Cardiovasc Med. 2011;12:754‐760. [DOI] [PubMed] [Google Scholar]
- 4. Dias A, Franco E, Usatii V. Stress‐induced cardiomyopathy shortly after pacemaker placement. J Invasive Cardiol. 2013;25:E207‐E209. [PubMed] [Google Scholar]
- 5. Chikata A, Omi W, Saeki T, Nagai H, Sakagami S. Repeated pacemaker dysfunction in a patient with recurrent Takotsubo cardiomyopathy precipitated by hyponatremia. Int J Cardiol. 2014;170:443‐444. [DOI] [PubMed] [Google Scholar]
- 6. Kahloon MU, Aslam AK, Aslam AF, Wilbur SL, Vasavada BC, Khan IA. Hyperkalemia induced failure of atrial and ventricular pacemaker capture. Int J Cardiol. 2005;105:224‐226. [DOI] [PubMed] [Google Scholar]
- 7. Santoro F, Ferraretti A, Ieva R, et al. Recurrent Tako‐Tsubo cardiomyopathy apparently induced by opposite triggers. Int J Cardiol. 2013;165:198‐199. [DOI] [PubMed] [Google Scholar]
- 8. Perazzolo Marra M, Zorzi A, Corbetti F, et al. Apicobasal gradient of left ventricular myocardial edema underlies transient T‐wave inversion and QT interval prolongation (Wellens' ECG pattern) in Tako‐Tsubo cardiomyopathy. Heart Rhythm. 2013;10:70‐77. [DOI] [PubMed] [Google Scholar]
- 9. Casavecchia G, Gravina M, Totaro A, et al. Role of cardiac magnetic resonance in the differential diagnosis of Takotsubo cardiomyopathy. Am J Emerg Med. 2015;33:983.e1‐983.e4. [DOI] [PubMed] [Google Scholar]
- 10. Madias JE. Transient attenuation of the amplitude of the QRS complexes in the diagnosis of Takotsubo syndrome. Eur Heart J Acute Cardiovasc Care. 2014;3:28‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Grauhan O, Müller J, Knosalla C, et al. Electric myocardial impedance registration in humoral rejection after heart transplantation. J Heart Lung Transplant. 1996;15:136‐143. [PubMed] [Google Scholar]
- 12. Matsuoka K, Okubo S, Fujii E, et al. Evaluation of the arrhythmogenecity of stress induced ‘Takotsubo cardiomyopathy’ from the time course of the 12‐lead surface electrocardiogram. Am J Cardiol. 2003;92:230‐233. [DOI] [PubMed] [Google Scholar]


