Recently, the increased prevalence of depression largely affects people's quality life and raises social suicide rate. Meanwhile, depression has been reported associated with lipid abnormalities, one of the major risks of cardiovascular disease and diabetes.1 Hence, the improvement of lipid metabolism is of critical for depressive patients’ health care. Meditation, an ancient mind training to improve one's attention and emotional self‐regulation,2 has demonstrated as a promising alternative or complementary therapeutics for depression.3 Previous studies on healthy or patients with medical illnesses have implicated that meditation could balance serum lipid concentrations.4, 5, 6, 7, 8, 9 However, few studies investigate its effect on metabolic profiles in depression population. To clarify this issue, this preliminary study compared the effect of an 8‐week mindfulness meditation on serum lipids, glucose, and renal parameters between healthy and participants with depression symptoms.
This clinical trial was conducted in Shanghai Mental Health Center (SMHC) from August, 2015 to February, 2017 and approved by the Institutional Review Board, SMHC. It has been registered on the Chinese Clinical Trial Registry (ChiCTR‐RPC‐17011590).
This meditation training consisted of three modules: (i) sitting in seven points of lotus posture, (ii) breathing in abdominal respiration, and (iii) concentrating on breath. In each Saturday class, participants were engaged in a 120‐minute teacher delivering, 20‐30 minutes meditation practice, and 40‐minute group discussion. Participants complete daily home meditation practice for at least 20 minutes for two months.
Participants interested in meditation were included if met all of the following criteria: (i) adults aged 18 to 65 years, Han Chinese; (ii) normal systolic and diastolic blood pressure; (iii) BMI≤28; (iv) were able to attend the 8‐week program on each Saturday and conduct daily practice at home; (v) no current administration of psychoactive medication and substance dependence; (vi) not involved in psychotherapy programs or extensive practice of any form of meditation (>15 minutes per day); (vii) no severe physical illnesses, such as infection, diabetes, hepatitis C, cardiovascular disease, and cancer. All subjects gave their written informed consent to participate. Participants with a HAM‐D17 score ≥8 were considered with depressive symptoms10 (case group), and the left were in healthy group. Both groups received meditation. Only those who completed all pre‐ and postclinical scale and biochemical measures and attended at least six training classes and completed≥45 daily home practices (75% of intervention) were deemed as completers and included in statistical analyses.
Student t test and chi‐squared test were used to compare the means of continuous variable and frequencies between two groups, respectively. Repeated measures of ANOVA were used to examine changes in depression and anxiety symptoms, PSQI scores, and metabolic parameters between two conditions and pre‐postintervention. Paired t test was further used to compare the pre‐ and postdifference within groups.
Finally, a total of 76 of 107 (71.02%) recruited participants completed the program, 61 of which were heathy and 15 were with depression symptoms (Figure 1A). No significant group differences were found at baseline for sex, age, marriage status, education, BMI, waist circumference, systolic and diastolic blood pressure, and heart rate for all completers. No significant demographic differences were observed between completers and those who dropped out.
Figure 1.
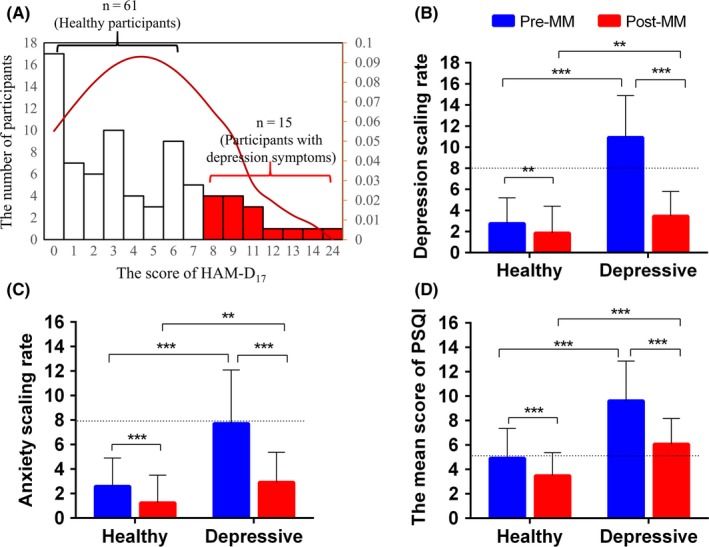
The rating scale of depression, anxiety, and sleep quality from pre‐ to postintervention between two groups. (A) Participant distribution of HAM‐D17 rating scale. Participants with rating score ≥8 were considered with depression symptoms (B) Scores on depression (C) Scores on anxiety (D) Estimated PSQI score. Data are shown as mean ± SD. Statistical analysis was performed by repeated measures of ANOVA. Paired t test was further used to compare the mean difference between groups, ***P < 0.001 and **P < 0.01. The dash line indicates the cutoff score of depression, anxiety risk, and sleep disorders.
HAM‐D17 and HAM‐A were used to assess the severity of depression and anxiety. After meditation, there was a larger drop of HAM‐D17 score in case group, resulting in a much smaller score difference between two groups, and all meditators with depression symptoms reached to a normal range of HAM‐D17 (Figure 1B). Results on anxiety assessment between two groups were similar to depression (Figure 1C). All of participants with depression symptoms reported poor sleep quality (PSQI score≥5) prior to meditation compared to 21.31% healthy participants. After meditation, each of them improved sleep quality and this group achieved a larger significant decrease in PSQI score (Figure 1D), resulting in a comparable well state to healthy group.
At baseline, there was no significant difference in metabolic variables between healthy and case groups, except for ApoA, which was higher in healthy group (Figure 2). After meditation, a significant decrease in uric acid, total cholesterol, HDL‐c, triglyceride, ApoA, ApoB, ApoE, and blood glucose was achieved in healthy group (Figure 2A‐E). Only triglyceride, ApoB, and ApoE were significantly reduced in case group (Figure 2F‐H). Although no significant difference, uric acid, total cholesterol, HDL‐c, ApoA, and blood glucose reduced to a comparable level to healthy group who received meditation, indicating a parallel physiological status as healthy controls after meditation. There was no correlation between the changes in triglyceride, ApoB, ApoE, and the change in HAM‐D17 score in case group.
Figure 2.
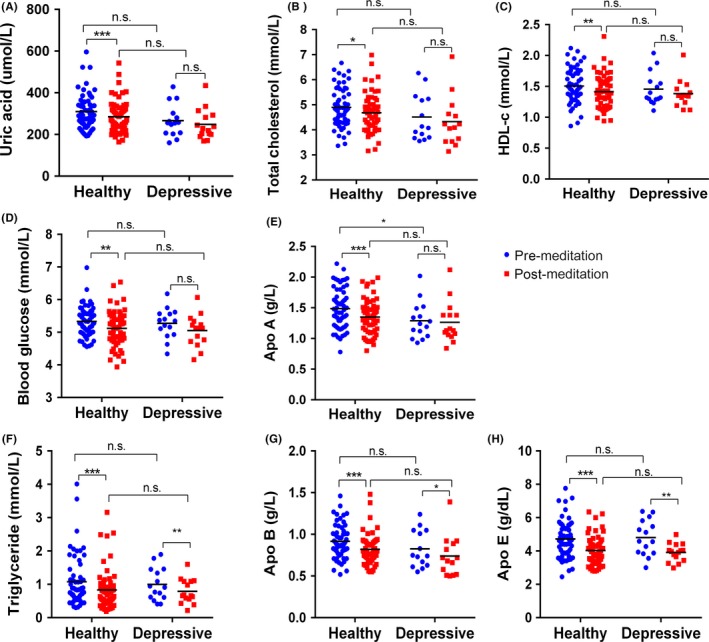
Metabolic profiles pre‐ and postmeditation practice between two groups. Data are shown as mean ± SD. Statistical analysis was performed by repeated measures of ANOVA. Paired t test was further used to compare the mean difference between groups, ***P < 0.001 and **P < 0.01.
This comparative study on metabolic profiles as well as depression and sleep quality could provide us views about how meditation could benefit health care for different populations, especially its potential therapeutic effect for psychiatric disorders. Meditation significantly improved metabolic profiles in both groups, while this effect was greater in heathy subjects. This could be due to that healthy participants might be more focused and behave better during meditation. Triglyceride, ApoB, and ApoE were robust and sensitive factors in response to meditation regardless of population. No correlations were found between the changes in triglyceride, ApoB, ApoE and HAM‐D17 score, indicating a complex regulation mechanisms between metabolism and symptoms. Meditators with depression symptoms had a significantly larger reduction in symptoms and greater improvement of sleep quality compared to healthy group. This might be the floor effect that healthy individuals with a low level at baseline may have a relatively smaller space of improvement.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGMENTS
This research was supported by the grants of National Key R&D Program of China (2017YFC0909200); National Natural Foundation of China (81671336); SJTU joint medical and engineering funding (YG2016ZD06), SJTU joint art and science funding (14JCRZ05), and Shanghai Key laboratory of Psychotic Disorders (13dz2260500). We gratefully acknowledge the contribution of all volunteers, the clinical staff, and postgraduate students in Shanghai Mental Health Center who contributed to data collection. We acknowledge prof. Xiang‐Yang Zhang, prof. Da‐Ke Qi, prof. Melvin G. McInnis, prof. Guan‐Ning Lin, and prof. Ti‐Fei Yuan help modify this manuscript.
REFERENCES
- 1. Lepine JP, Briley M. The increasing burden of depression. Neuropsychiatr Dis Treat. 2011;7(Suppl 1):3‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kabat‐Zinn J. Mindfulness‐based interventions in context: past, present, and future. Clin Psychol Sci Pract. 2003;10(2):144‐156. [Google Scholar]
- 3. Edenfield TM, Saeed SA. An update on mindfulness meditation as a self‐help treatment for anxiety and depression. Psychol Res Behav Manag. 2012;5:131‐141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Schneider RH, Nidich SI, Salerno JW, et al. Lower lipid peroxide levels in practitioners of the Transcendental Meditation program. Psychosom Med. 1998;60(1):38‐41. [DOI] [PubMed] [Google Scholar]
- 5. Mahajan AS, Reddy KS, Sachdeva U. Lipid profile of coronary risk subjects following yogic lifestyle intervention. Indian Heart J. 1999;51(1):37‐40. [PubMed] [Google Scholar]
- 6. Singh S, Kyizom T, Singh KP, Tandon OP, Madhu SV. Influence of pranayamas and yoga‐asanas on serum insulin, blood glucose and lipid profile in type 2 diabetes. Indian J Clin Biochem. 2008;23(4):365‐368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kim DH, Moon YS, Kim HS, et al. Effect of Zen Meditation on serum nitric oxide activity and lipid peroxidation. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29(2):327‐331. [DOI] [PubMed] [Google Scholar]
- 8. Bijlani RL, Vempati RP, Yadav RK, et al. A brief but comprehensive lifestyleeducation program based on yoga reduces risk factors for cardiovasculardisease and diabetes mellitus. J Altern Complement Med. 2005;11(2):267‐274. [DOI] [PubMed] [Google Scholar]
- 9. Ko GT, Tsang PC, Chan HC. A 10‐week Tai‐Chi program improved the blood pressure, lipid profile and SF‐36 scores in Hong Kong Chinese women. Med Sci Monit. 2006;12:CR196‐CR199. [PubMed] [Google Scholar]
- 10. Frank E, Prien RF, Jarrett RB, et al. Conceptualization and rationale for consensus definitions of terms in major depressive disorder. Remission, recovery, relapse, and recurrence. Arch Gen Psychiatry. 1991;48(9):851‐855. [DOI] [PubMed] [Google Scholar]


