Abstract
Background
Smoking cessation is correlated with several psychological, social, biological, and pharmacological aspects. The combined tendency to experience negative emotions and to inhibit the expression of these emotions is indicated as “type D personality,” an independent risk marker for clinical outcome in cardiac disease. Despite this effect of type D personality on cardiovascular disease, it is still unclear whether this personality trait may influence smoking cessation after a myocardial infarction.
Hypothesis
we hypothesized that there is a relationship between type D personality and smoking persistence in acute coronary syndrome patients, and this association may predict a worse long‐term prognosis.
Methods
The study enrolled 231 patients with ST‐segment elevation myocardial infarction, treated with primary percutaneous coronary intervention. Type D scale 14 (ds 14) was administered upon admission to the hospital.
Results
After controlling for demographic and clinical confounders, non–type D patients reported statistically significant higher frequencies of smoking cessation when compared with the type D group. In addition, the presence of this psychological factor anticipates significantly the onset of smoking during adolescence. Furthermore, current type D smokers had a higher incidence of cardiovascular events during long‐term follow‐up.
Conclusions
Type D personality and smoking status increase the risk of cardiac events. An emotionally stressed personality and persistence of smoking after the first cardiac event, and mostly their mutual influence, indicate a population at high cardiovascular risk.
Keywords: Acute Myocardial Infarction, Primary Percutaneous Coronary Intervention, Smoke Cessation, Smoking, Type D Personality
1. INTRODUCTION
Smoking is a well‐known risk factor for coronary artery disease (CAD) and is associated with increased rates of myocardial infarction (MI) and cardiovascular (CV) death.1 As reported by some authors, smokers had a higher chance of developing an acute MI >10 years earlier than nonsmokers, with similar risk of death at 1 year when adjusted for age and sex.2 It has been shown that the percentage of smokers is greater among subjects with anxiety or depression,3 and the correlation between these variables increases the risk of acute cardiac events.4 In addition, early depressive and anxious symptoms occur with high frequencies among patients suffering from acute coronary syndrome (ACS)5 related to Type D personality, with adverse effects on the cardiac outcome.6 The patients with this trait simultaneously tend to experience distress and inhibit the expression of emotions, with a negative impact on clinical outcomes.7 Patients affected by Type D personality often have unexplained poor clinical outcomes. It is still unclear what mechanisms link Type D personality with poor clinical outcomes in these patients.8 Mediating mechanisms may include both physiological and behavioral factors.9 The most remarkable behavioral linking factor could be the nonadherence to the need to modify individual risk factors (eg, smoking cessation).
The aim of the present study was to investigate the relationship between type D personality and smoking persistence in ACS patients and to explore whether this association may predict a worse long‐term prognosis.
2. METHODS
2.1. Subjects and measures
A sample of 231 consecutive post–ACS patients were recruited from June 2012 to December 2014 (follow‐up: 3.5 ± 1.1 years) during their hospitalization in our Department of Cardiology for ST‐segment elevation myocardial infarction. To select a homogeneous group of patients, they were eligible if they met the criteria for ACS proposed by the Joint European Society of Cardiology/American College of Cardiology Committee,10 if they underwent immediate coronary revascularization procedures (primary percutaneous coronary intervention [PCI]) due to a single‐culprit‐vessel coronary artery disease (CAD), and if they were current smokers. The atherosclerotic coronary burden was calculated as the ratio between stenosis degree and the number of vessels, in relation to the presence of any intermediate stenosis of other vessels not amenable to percutaneous treatment.
Patients were excluded if they had an antecedent ACS or an ongoing ACS with no ST‐segment elevation, PCI that followed coronary artery bypass graft surgery, left ventricular dysfunction (left ventricular ejection fraction <50%), were never smokers, or self‐reported a history of psychiatric illness. All participants were administered the Type D Scale‐14 (DS14) when they were medically stable, within 48 hours following primary PCI. Assessments took place for each individual under the superintendence of a researcher. The DS14 is a standardized measure that assesses 2 subscales, negative affectivity (NA) and social inhibitions (SI).11 Total scores on both subscales range from 0 to 28 (≥10 on NA and SI required to confirm type D personality). Participants were informed that the questionnaire was voluntary and anonymous, were assured that there were no right or wrong answers, and were assured of the confidentiality of their responses.
Information concerning demographics variables (sex and age), disease classification and severity, traditional CAD risk factors (smoking: current smoking and smoking cessation; hypertension: values of arterial pressure and hypertension treatment; dyslipidemia: values of lipid and lipid‐lowering medication; diabetes mellitus: blood glucose value and antidiabetic therapies; body mass index), and type of coronary percutaneous treatment performed were gathered from medical records, whereas data concerning educational level (elementary, higher education) and family status (living alone/widowed, married/living with partner) were collected by self‐report from participants. The participants also reported their habitual cigarette consumption. At the presentation, patients who stopped smoking and did not start again during the observation period were classified as “stop smoker.”
A written informed consent was obtained from each participant before any study‐related procedure was started. The study protocol was approved by the research review board of the participating hospital units.
2.2. Study outcomes
Clinical outcome was evaluated by monitoring major adverse cardiovascular events (death, reinfarction, re–percutaneous transluminal coronary angioplasty) and rehospitalization, seen as cumulative cardiovascular (cCV) events for all statistical analyses.
2.3. Statistical analysis
Data are presented as mean ± SD and frequency of occurrence (%). The level of statistical significance was set at P < 0.05. Differences in demographics and clinical variables observed in type D and non–type D subjects were analyzed by χ2 test (categorical variables) or independent t tests and multivariate analysis of variance (continuous variables). The same analyses were administered to examine basic differences between current smoking and stop‐smoking patients. Then, the association of type D personality with smoking status (current smoking = 1, stop smoking = 0), until the end of observation period, was assessed with χ2 analysis. Furthermore, multivariate adjusted hazard ratios of cCV events were calculated using Cox proportional hazards models for significant covariates, previously assessed by bivariate correlation; and type D personality and smoking status, separately as first step; and both variables merged, finally. Significant or trend variables on univariate analysis were entered in each multivariable model. The difference in rates of cCV events between groups, according to type D/non–type D and current/stop smoking categorization, during the follow‐up period was assessed by the Kaplan–Meier method by means of the log‐rank test. SPSS 20 statistical software was used for the analysis (SPSS Inc., Chicago, IL).
3. RESULTS
The patients' baseline characteristics are shown in Table 1. Particularly, current smokers had a worse lipid profile, especially as regards high‐density lipoprotein cholesterol values, which were significantly lower in the group of patients with type D personality. Furthermore, the presence of this psychological factor anticipates significantly the onset of smoking during adolescence. There were no significant differences in severity of CAD and therapy among the groups. The prevalence of type D personality was 34%, and 55 out of 78 (71%) of these patients have continued to smoke (Figure 1).
Table 1.
Baseline characteristics of the study patients
| Type D | Non–Type D | All P Valuea | |||||
|---|---|---|---|---|---|---|---|
| Current Smoker, n = 55 | Stop Smoker, n = 23 | P Valueb | Current Smoker, n = 18 | Stop Smoker, n = 135 | P Valueb | ||
| Age, y | 63.4 ± 10.5 | 60.3 ± 11.4 | NS | 60.1 ± 13.6 | 63.7 ± 11.3 | NS | NS |
| Male sex, % | 22.1 | 9.9 | NS | 6.5 | 56.2 | NS | NS |
| BMI, kg/m2 | 27.2 ± 3.4 | 28.1 ± 2.2 | NS | 27.7 ± 3.6 | 27.3 ± 4.5 | NS | NS |
| SBP, mm Hg | 142.3 ± 11.4 | 141.2 ± 10.9 | NS | 139.9 ± 12.2 | 141.5 ± 11.7 | NS | NS |
| Heart rate, bpm | 77.3 ± 2.4 | 75.7 ± 5.5 | NS | 79.1 ± 5.1 | 77.7 ± 4.9 | NS | NS |
| Burden of CAD, %c | 16.2 ± 7.6 | 15.4 ± 6.4 | NS | 14.7 ± 8.1 | 14.8 ± 5.5 | NS | NS |
| LVEF, % | 57.4 ± 3.3 | 58.2 ± 1.7 | NS | 57.1 ± 4.3 | 59.3 ± 2.2 | NS | NS |
| Cholesterol, mg/dL | 169.8 ± 43.6 | 171.4 ± 55.5 | NS | 171.4 ± 41.7 | 169.9 ± 43.7 | NS | NS |
| HDL‐C, mg/dL | 41.5 ± 10.1 | 50.2 ± 46.6 | 0.03 | 40.4 ± 15.5 | 45.4 ± 14.6 | NS | NS |
| TG, mg/dL | 119.4 ± 48.8 | 122.5 ± 58.4 | NS | 123.4 ± 46.2 | 118.5 ± 49.9 | NS | NS |
| Fasting glucose, mg/dL | 98.4 ± 11.1 | 101.3 ± 13.6 | NS | 103.3 ± 10.3 | 99.9 ± 12.1 | NS | NS |
| Cr, mg/dL | 0.9 ± 0.2 | 0.8 ± 0.6 | NS | 1.0 ± 0.2 | 0.9 ± 0.8 | NS | NS |
| Age at onset of smoking, y | 14.2 ± 3.8 | 16.8 ± 2.7 | 0.003 | 18.6 ± 8.8 | 16.6 ± 3.7 | NS | 0.001 |
| Mean daily cigarettes, n | 26.4 ± 14.3 | 24.6 ± 15.3 | NS | 26.9 ± 13.3 | 24.5 ± 11.1 | NS | NS |
| Antiplatelet therapy, % | 100 | 100 | NS | 100 | 100 | NS | NS |
| Statin, % | 98 | 99 | NS | 99 | 100 | NS | NS |
| ACEI, % | 95.2 | 96.6 | NS | 96.1 | 95.7 | NS | NS |
| β‐Blocker, % | 97.2 | 97.3 | NS | 98.1 | 97.4 | NS | NS |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; BMI, body mass index; CAD, coronary artery disease; Cr, creatinine; HDL‐C, high‐density lipoprotein cholesterol; LVEF, left ventricular ejection fraction; MANOVA, multivariate analysis of variance; NS, not significant; SBP, systolic blood pressure; SD, standard deviation; TG, triglycerides.
Data are presented as mean ± SD unless otherwise noted.
MANOVA between type D and non–type D groups.
MANOVA between current smoker and stop smoker groups.
Calculated as the ratio between degree of stenosis and number of vessels.
Figure 1.
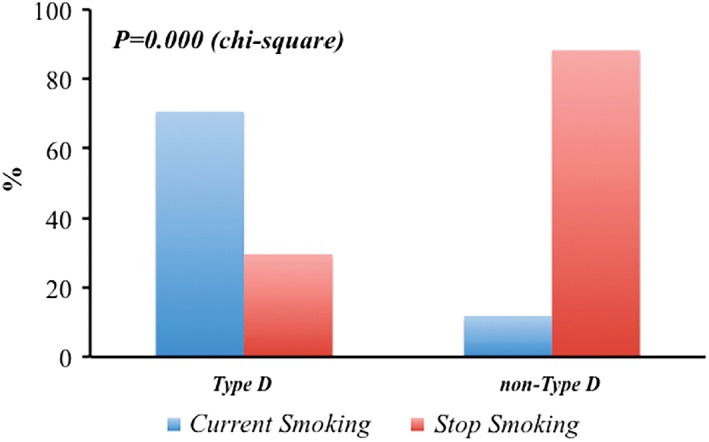
Change in smoking status according to type D personality
During 3.5 years of follow‐up, the rate of cCV events was 28.6 per 100 person‐years in all type D patients (78 events) and 29.1 per 100 person‐years in all current smokers (73 events). The rate of cCV events was lower in non–type D patients who stopped smoking compared with type D patients who continued to smoke after MI (0.36 vs 37.4 per 100 person‐years, respectively, P = 0.000; Figure 2). The Cox regression model is summarized in Table 2, reporting only the results of the 2 study variables, corrected by all principal parameters (age, sex, body mass index, onset of smoking, mean daily cigarettes, hemodynamic status, and metabolic and lipid profile, as previously described). Type D personality and current smokers, evaluated separately, were heavily exposed to a high risk of cCV recurrences (Table 2). When both variables were merged, the risk of cCV events remained significantly increased (Table 2).
Figure 2.
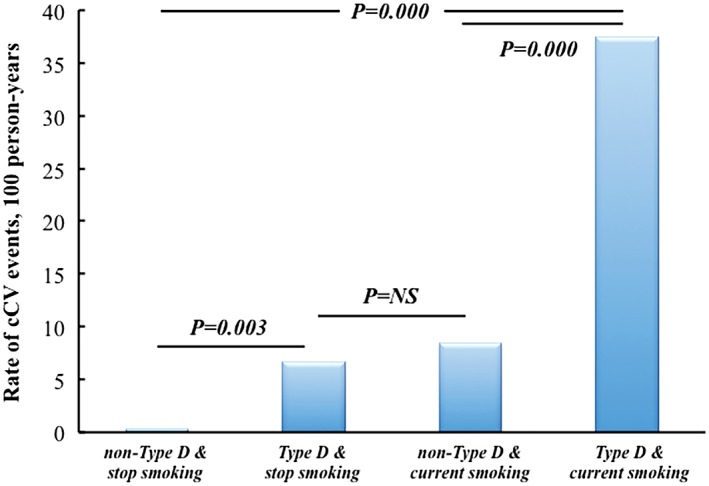
Rate of cCV events according to personality and smoking status. Abbreviations: cCV, cumulative cardiovascular
Table 2.
Cox regression modela
| Adjusted HR | 95% CI | P Value | |
|---|---|---|---|
| Type D | 72.28 | 23.91‐218.44 | 0.000 |
| Current smoking | 33.35 | 13.46‐82.62 | 0.000 |
| Type D + current smoking | 5.06 | 3.37‐7.60 | 0.000 |
Abbreviations: BMI, body mass index; CI, confidence interval; HR, hazard ratio.
Model corrected by all principal parameters (age, sex, BMI, onset of smoking, mean daily cigarettes, hemodynamic status, and metabolic and lipid profile).
During follow‐up, Kaplan–Meier curves showed higher incidence of cCV events in type D patients compared with the non–type D patients, and in current smokers compared with the stop smokers group, with additive effect when both variables were merged (Figure 3).
Figure 3.
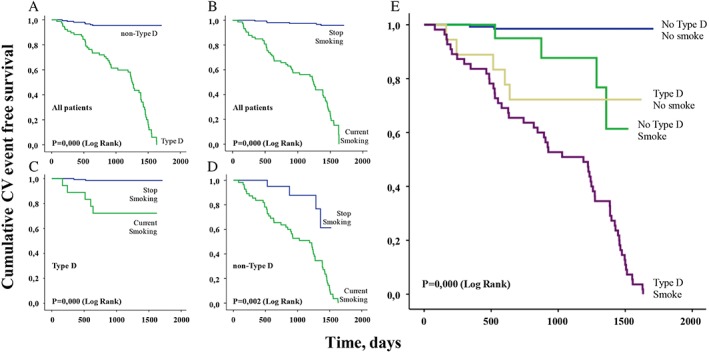
Kaplan–Meier survival curves comparing overall freedom of cumulative CV events between (A) type D and non–type D personality and (B) current smoking and stop smoking; comparing freedom of cumulative CV events between current smoking and stop smoking in (C) type D and (D) non–type D personality; and (E) comparing freedom of cumulative CV events among merged variables. Abbreviations: CV, cardiovascular
4. DISCUSSION
This is the first study assessing the impact of smoking persistence related to type D personality on long‐term CV outcome in patients undergoing primary PCI. Our results showed that type D subjects found it more difficult to quit smoking compared with non–type D patients, with an augmented (5×) risk of developing heart‐related diseases. Literature also confirmed this strict association between type D personality and smoking addiction.12 NA and SI contribute to the development of the distressed personality (type D),13 which gives itself a worse CV prognosis.14 Furthermore, the association between type D personality and CAD morbidity and mortality was highlighted in several studies,15 independently from conventional risk factors, disease severity,16 appropriate medical treatment,17 and other psychological factors.18 In fact, type D personality was not related to disease severity, as estimated by the number of coronary arteries affected by atherosclerotic disease.19 Furthermore, several authors confirmed that quitting smoking was associated with an increase in concentrations of high‐density lipoprotein cholesterol, although the mechanism was not fully understood.20 This observation was also present in our work, but improving patients' lipid profile seemed not to directly affect the prognosis in our population. These findings simply suggest that the association between type D personality and adverse CV prognosis21 may be explained by other pathways22 hypothesized in both biological and behavioral mechanisms.23 Biological pathways that were taken into account included elevated cortisol levels24 and pro‐inflammatory cytokines,25 whereas behavioral processes are thought to reside in negative health‐related behaviors26 and poor treatment adherence.27
Less is known about how potential mechanisms linking type D personality with smoking habit impact on the CV prognosis. Probably type D subjects find it more difficult to quit smoking due to their inclination to experience events in a more negative way, and smoking cessation may be viewed as an alarming and traumatic event; this tendency might therefore suggest their need for more support.28 The results of the present study indicate that type D patients differed significantly from non–type D patients in relation to smoking habit, adding to the evidence which has found that type D personality is associated with smoking behavior in both healthy participants and cardiac patients.29 It should be noted that important previous research had failed to establish such an association.26 The present study identified that type D patients not only were more likely than non–type D patients to be smokers, they also smoked before and a higher number of cigarettes. In addition to previous research that has outlined potential mechanisms linking type D personality to CV disease, the current findings indicate that type D patients may have poorer outcomes due to their wrong smoking behaviors regardless of the severity of baseline CAD. This finding is in accordance with previous results in CAD and congestive heart failure patients, where no association has been found between type D personality and indicators of disease severity, such as multivessel disease.30
4.1. Study limitations
Certain limitations restrict the interpretation of the present findings. First of all, the participant samples were not randomly selected. Yet the population included consecutive patients, which diminished greatly the risk of selection bias in that sample. Another limitation is the patients' self‐reporting of psychopharmacological medication use, previous mental health problems, and smoking.
5. CONCLUSION
Type D personality was related to a higher smoking prevalence and smoking persistence. Type D personality was not related to other traditional risk factors, disease severity, or treatment administered in CAD patients. During the follow‐up, a worsening of CV prognosis occurred during long‐term observation in D type personality patients who started smoking again. More research needs to be conducted to clarify which mediating mechanisms are behind the type D personality association with adverse prognosis in cardiac patients, and to confirm whether smoking behavior play a significant role.
Conflicts of interest
The authors declare no potential conflicts of interest.
Imbalzano E, Vatrano M, Quartuccio S, et al. Effect of type D personality on smoking status and their combined impact on outcome after acute myocardial infarction. Clin Cardiol. 2018;41:321–325. 10.1002/clc.22865
REFERENCES
- 1. Kannel WB, Higgins M. Smoking and hypertension as predictors of cardiovascular risk in population studies. J Hypertens Suppl. 1990;8:S3–S8. [PubMed] [Google Scholar]
- 2. Rakowski T, Siudak Z, Dziewierz A, et al. Impact of smoking status on outcome in patients with ST‐segment elevation myocardial infarction treated with primary percutaneous coronary intervention. J Thromb Thrombolysis. 2012;34:397–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Campion J, Checinski K, Nurse J, et al. Smoking by people with mental illness and benefits of smoke‐free mental health services. Adv Psychiatr Treat. 2008;14:217–228. [Google Scholar]
- 4. Yusuf S, Hawken S, Ounpuu S, et al; INTERHEART Study Investigators . Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case‐control study. Lancet. 2004;364:937–952. [DOI] [PubMed] [Google Scholar]
- 5. De Fazio P, Caroleo M, Rizza P, et al. Specific personality traits and coping styles predict affective symptoms in early post–acute coronary syndrome inpatients. Int J Psychiatry Med. 2012;44:119–132. [DOI] [PubMed] [Google Scholar]
- 6. Van Melle JP, de Jonge P, Spijkerman TA, et al. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta‐analysis. Psychosom Med. 2004;66:814–822. [DOI] [PubMed] [Google Scholar]
- 7. Denollet J, Pedersen SS, Vrints CJ et al. Usefulness of type D personality in predicting five‐year cardiac events above and beyond concurrent symptoms of stress in patients with coronary heart disease. Am J Cardiol. 2006;97:970–973. [DOI] [PubMed] [Google Scholar]
- 8. Williams L, O'Connor RC, Howard S, et al. Type‐D personality mechanisms of effect: the role of health‐related behavior and social support. J Psychosom Res. 2008;64:63–69. [DOI] [PubMed] [Google Scholar]
- 9. Hamer M, Molloy GJ, Stamatakis E. Psychological distress as a risk factor for cardiovascular events: pathophysiological and behavioral mechanisms. J Am Coll Cardiol. 2008;52:2156–2162. [DOI] [PubMed] [Google Scholar]
- 10. Steg PG, James SK, Atar D, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST‐segment elevation. Eur Heart J. 2012;33:2569–2619. [DOI] [PubMed] [Google Scholar]
- 11. Denollet J. DS14: standard assessment of negative affectivity, social inhibition, and Type D personality. Psychosom Med. 2005;67:89–97. [DOI] [PubMed] [Google Scholar]
- 12. Pedersen SS, Denollet J, Ong AT, et al. Adverse clinical events in patients treated with sirolimus‐eluting stents: the impact of Type D personality. Eur J Cardiovasc Prev Rehabil. 2007;14:135–140. [DOI] [PubMed] [Google Scholar]
- 13. Denollet J, Sys SU, Stroobant N, et al. Personality as independent predictor of long‐term mortality in patients with coronary heart disease. Lancet. 1996;347:417–421. [DOI] [PubMed] [Google Scholar]
- 14. Denollet J, Sys SU, Brutsaert DL. Personality and mortality after myocardial infarction. Psychosom Med. 1995;57:582–591. [DOI] [PubMed] [Google Scholar]
- 15. Denollet J, Schiffer AA, Spek V. A general propensity to psychological distress affects cardiovascular outcomes: evidence from research on the type D (distressed) personality profile. Circ Cardiovasc Qual Outcomes. 2010;3:546–557. [DOI] [PubMed] [Google Scholar]
- 16. Pedersen SS, Denollet J. Is Type D personality here to stay? Emerging evidence across cardiovascular disease patient groups. Curr Cardiol Rev. 2006;2:205–213. [Google Scholar]
- 17. Denollet J, Vaes J, Brutsaert DL. Inadequate response to treatment in coronary heart disease: adverse effects of type D personality and younger age on 5‐year prognosis and quality of life. Circulation. 2000;102:630–635. [DOI] [PubMed] [Google Scholar]
- 18. Denollet J, Pedersen SS, Ong AT, et al. Social inhibition modulates the effect of negative emotions on cardiac prognosis following percutaneous coronary intervention in the drug‐eluting stent era. Eur Heart J. 2006;27:171–177. [DOI] [PubMed] [Google Scholar]
- 19. Svansdóttir E, Karlsson HD, Gudnason T, et al. Validity of Type D personality in Iceland: association with disease severity and risk markers in cardiac patients. J Behav Med. 2012;35:155–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Forey BA, Fry JS, Lee PN, et al. The effect of quitting smoking on HDL‐cholesterol—a review based on within‐subject changes. Biomark Res. 2013;1:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Svansdóttir E. Type D Personality Across General Population and Coronary Patient Samples in Iceland: Implications for Cardiovascular Health [doctoral thesis]. Tilburg University; 2012. [Google Scholar]
- 22. Beutel ME, Wiltink J, Till Y, et al. Type D personality as a cardiovascular risk marker in the general population: results from the Gutenberg health study. Psychother Psychosom. 2012;81:108–117. [DOI] [PubMed] [Google Scholar]
- 23. Kupper N, Denollet J. Type D personality as a prognostic factor in heart disease: assessment and mediating mechanisms. J Pers Assess. 2007;89:265–276. [DOI] [PubMed] [Google Scholar]
- 24. Whitehead DL, Perkins‐Porras L, Strike PC, et al. Cortisol awakening response is elevated in acute coronary syndrome patients with type‐D personality. J Psychosom Res. 2007;62:419–425. [DOI] [PubMed] [Google Scholar]
- 25. Denollet J, Conraads VM, Brutsaert DL, et al. Cytokines and immune activation in systolic heart failure: the role of Type D personality. Brain Behav Immun. 2003;17:304–309. [DOI] [PubMed] [Google Scholar]
- 26. Williams L, O'Connor RC, Howard S, et al. Type D personality mechanisms of effect: the role of health‐related behavior and social support. J Psychosom Res. 2008;64:63–69. [DOI] [PubMed] [Google Scholar]
- 27. Molloy GJ, Randall G, Wikman A, et al. Type D personality, self‐efficacy, and medication adherence following an acute coronary syndrome. Psychosom Med. 2012;74:100–106. [DOI] [PubMed] [Google Scholar]
- 28. Hooten WM, Ames SC, Vickers KS, et al. Personality correlates related to tobacco abstinence following treatment. Int J Psychiatry Med. 2005;35:59–74. [DOI] [PubMed] [Google Scholar]
- 29. Einvik G, Dammen T, Hrubos‐Strøm H, et al. Prevalence of cardiovascular risk factors and concentration of C‐reactive protein in Type D personality persons without cardiovascular disease. Eur J Cardiovasc Prev Rehabil. 2011;18:504–509. [DOI] [PubMed] [Google Scholar]
- 30. Martens EJ, Kupper N, Pedersen SS, et al. Type‐D personality is a stable taxonomy in post‐MI patients over an 18‐month period. J Psychosom Res. 2007;63:545–550. [DOI] [PubMed] [Google Scholar]


