Abstract
Background
Statins are first‐line for cholesterol lowering and prevention of atherosclerotic cardiovascular disease (ASCVD), but their use is complicated by side effects and potential for drug–drug interactions. Provider‐patient communication is the basis of the recommended shared decision‐making, but relatively little is known about this in the context of statin use.
Methods
We surveyed 5014 US adults prescribed a statin for hypercholesterolemia to learn their perspectives on communication with their provider.
Results
Ninety‐four percent reported currently taking a statin while 6% had stopped. Past users vs current users were more likely to be female, age < 65 years, and to have fewer cardiovascular disease–related comorbidities (hypertension, type 2 diabetes mellitus, and coronary heart disease, respectively). Although 93% of current statin users were taking ≥1 other prescription medications (median of 4), 76% were “not at all”/“not very concerned” about potential drug–drug interactions with their statin, and fewer than one‐quarter recalled mention of these from their provider. Ninety‐five percent of subjects said it was “extremely”/“somewhat” important that their healthcare provider take “an individualized approach to selecting the right statin,” but 73% and 76%, respectively, said their statin choice was made with little or no input from them. Only 25% were told that “some statins might be more likely than others to interact with other medications,” and only 18% (and only 20% of past users) were told that “their particular statin might interact with other medications.”
Conclusion
Provider‐patient communication regarding statin therapy appears inadequate, by patient recall, and efforts to improve it are warranted.
Keywords: Cholesterol, HMG‐CoA Reductase Inhibitors, Hypercholesterolemia, Low‐Density Lipoprotein Cholesterol, Statin Adherence, Statins
1. INTRODUCTION
Statins (3‐hydroxy‐3‐methyglutaryl coenzyme A reductase inhibitors) are the cornerstone of hypercholesterolemia management, having been proven safe and effective in lowering elevated low‐density lipoprotein cholesterol (LDL‐C) and reducing the risk of atherosclerotic cardiovascular disease (ASCVD), the leading cause of death in the United States.1 Unfortunately, however, a large percentage of patients stop taking their statin therapy within 1 year, or less, of starting it.2, 3, 4 This is concerning, because, as would be expected, nonadherence to statin therapy is associated with an excess of myocardial infarction and cardiovascular morbidity.5
Previous research has addressed certain aspects of the reasons why patients discontinue statin therapy—in part because of myalgia and other side effects.6 These studies of statin adherence analyzed large insurance and pharmacy databases, based on objective data regarding pharmacy refills and diagnoses.7 The database studies, however, did not assess the subjective experience of statin‐taking patients, including their perception of related provider‐patient communication and patient understanding of the issues surrounding adherence to or discontinuation of this therapy.
The Understanding Statin Use in America and Gaps in Education (USAGE) internet survey was the first large US‐based study to address the patient perspective on statin therapy. USAGE assessed the attitudes, beliefs, practices, and behavior of 10 138 US adults age ≥ 18 years who were current and former statin users.8, 9, 10, 11, 12, 13 USAGE focused primarily on patient reasons for switching and stopping statins, and the survey results provided important insights into statin nonadherence, one of the largest barriers to effective treatment of hypercholesterolemia.
The current study, the Understanding Patient Adherence and Concerns with STatins and MedicatION Discussions with Physicians (ACTION) survey, is an effort to further explore, beyond the extent of the USAGE survey, patient reports of provider‐patient communication regarding statin therapy and the impact of this communication on patient knowledge of and attitudes toward statin therapy. This internet‐based survey included >5000 Americans age ≥ 45 years, selected for having been prescribed a statin for a diagnosis of high cholesterol levels. Further, the ACTION survey patient sample was not only selected for participation by sex, age, race, education, income, and regional area of residence representative of the US population of adults age ≥ 45 years, but the responses were weighted to even better approximate the population of interest.
2. SURVEY METHODOLOGY
The ACTION survey was conducted within the United States from July 7, 2017, to August 4, 2017, and consisted of an internet‐based, self‐administered questionnaire of 88 questions. It was conducted by the Harris Poll on behalf of Kowa Pharmaceuticals America, Inc. Respondents for the survey (primarily termed “patients” in the current report) were recruited from multiple online panels composed of millions of individuals who had agreed to participate in online survey research. To conduct this study, an email with a link to the survey was sent to a random sample of tens of thousands of these individuals, believed to be US adults age ≥ 45 years, inviting them to participate. They were not told the nature of the survey, nor was it indicated in the initial set of screening questions, which asked about 9 common health conditions (including high cholesterol) and several major medication classes (including statins), thus masking the intended focus on cholesterol and statin treatment in the full survey. Respondents to the screening questions who (1) indicated that they were residing in the United States, (2) confirmed that they were age ≥ 45 years, (3) reported having received a diagnosis of high cholesterol by a healthcare provider, and (4) reported having used a statin to treat their high cholesterol, were then identified as qualified and directly led to the full survey. After taking the full survey, a set of demographic questions was asked, as at the end of the screening questions for those not qualifying by the above 4 criteria. Among 18 202 panelists who completed the screening questions, 5014 qualified patients completed the full survey, the survey having been closed as soon as possible after reaching the prespecified quota of 5000 qualified respondents. The responses of the 5014 individuals who entered and completed the full survey during its open period constitute the final dataset used in this report.
To ensure that the resulting participants (termed “patients” in this report) were as representative as possible of the US population of statin‐prescribed patients age ≥ 45 years, of which the demographic details are poorly known, results from all 18 202 US respondents age ≥ 45 years completing the survey were weighted according to several factors simultaneously to best approximate the well‐known demographic details of this adult population. These factors included race/ethnicity, age, sex, highest educational attainment, household income, and US region of residence. Responses were weighted upward if under‐represented vs the US general population of adults age ≥ 45 years (as much as 5.0‐fold, depending on the degree of under‐representation) or weighted downward if over‐represented (as much as 0.2‐fold, again depending on the degree of over‐representation). Once the 18 202 respondents were weighted, the 5014 qualified respondents who met the survey criteria were pulled out of the total group that was weighted, therefore allowing these qualified respondents to retain the representativeness benefit of having been weighted as part of that larger group. All values in this report are the result of that weighting process, such that none of the data shown are the actual “raw” responses.
After weighting, among the qualified respondents, 76% were Caucasian, 9% were Hispanic (of any race), 8% were African American, 5% were Asian, 1% were Native American/Alaska Native, 1% were mixed race, and 1% declined to answer (Table 1 and Supporting Information, Table S28, in the online version of this article). Half were male (52%), the mean age was 64 years, and the age range was 45 to 95 years (Table 1).
Table 1.
Patients' demographic characteristics and comorbidities
| Characteristic | Total Patients, N = 5014 | Current Statin Users, n = 4706 | Past Statin Users, n = 308 |
|---|---|---|---|
| Sex | |||
| M | 52 | 53a | 36 |
| F | 48 | 47 | 64a |
| Mean age, y | 64 | 64.1 | 63.1 |
| Age group | |||
| 45–54 y | 20 | 19 | 28a |
| 55–64 y | 30 | 30 | 28 |
| 65–74 y | 37 | 38a | 27 |
| ≥ 75 y | 14 | 13 | 16 |
| Race/ethnicity | |||
| White | 76 | 76 | 76 |
| Black/African American | 8 | 8 | 6 |
| Hispanic | 9 | 9 | 8 |
| Asian | 5 | 4 | 6 |
| Comorbidity | |||
| HTN | 68 | 69a | 58 |
| Arthritis | 35 | 35 | 41 |
| T2DM | 27 | 27a | 17 |
| Cancer | 13 | 13 | 10 |
| Prediabetes | 10 | 10 | 9 |
| CHD | 9 | 9a | 4 |
| T1DM | 1 | 1 | 1 |
| Chronic liver disease (including HBV) | 1 | 1 | <1 |
Abbreviations: CHD, coronary heart disease; F, female; HBV, hepatitis B virus; HTN, hypertension; M, male; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus. Data are presented as %.
Significant difference between current and former statin users, P < 0.05.
Regarding health status, patients were asked if they had ever been diagnosed by a healthcare provider with any of the following health conditions, and they could choose all that applied to them: 100% chose high cholesterol (by study design), 68% selected hypertension, 35% selected arthritis, 27% selected type 2 diabetes mellitus (T2DM), 13% selected cancer, 10% selected prediabetes, 9% selected coronary heart disease (CHD), 1% selected type 1 diabetes mellitus, and 1% selected chronic liver disease (Table 1 and Supporting Information, Table S21, in the online version of this article).
Differences between current and past statin users were determined by t test with P < 0.05 considered statistically significant, without correction for multiple comparisons. Except as noted below, responses did not differ statistically between current statin users and past statin users.
3. SURVEY RESULTS
3.1. Current vs past statin users
All study patients, by entry criterion, had been prescribed a statin, and 94% said they were currently using one. The remaining 6% of all patients said they were not using a statin at the time of the survey, and are thus termed past statin users in this report. A majority of the analyses in this report are divided according to current vs past statin use. Current users were asked if they had “delayed taking a statin after it was prescribed, sometimes miss a dose, or [otherwise] do not take their treatment as prescribed,” to which 21% said yes (see Supporting Information, Table S23, in the online version of this article). That 21% (n = 1043) were then asked “why,” by choosing ≥1 of several options: 76% responded “I simply forgot,” 12% said “I was experiencing side effects,” 9% said “I was worried about potentially experiencing muscle/joint pain,” 10% said “I was worried about potentially experiencing other side effects,” 6% said “I didn't know it was important to take statins as prescribed,” 4% said “the treatment was too expensive for me,” 1% said “I wasn't experiencing the results I wanted in terms of lowering my LDL‐C,” 7% said “other,” and 2% said “don't know/can't remember” (see Supporting Information, Table S24, in the online version of this article). In addition, all patients were asked several questions about activities regarding their statin use, for most of which the answers were very similar between past and current users: 9% and 11%, respectively, said they had stopped their statin for a period of time and then resumed it; 5% and 6% said they had cut back on their statin dose without first discussing it with their healthcare provider; 3% and 3% had “not told [their] healthcare provider about challenges” with their statin; and 2% and 3% said “I asked my healthcare provider to prescribe a specific statin but they chose to prescribe a different one” (see Supporting Information, Table S25, in the online version of this article). For one of these activities, however, the response differed greatly: 6% of current users vs 39% of past users said “I stopped taking my statin without talking with my doctor” (P < 0.05; Supporting Information, Table S25).
3.2. Patient demographics
Among current statin users, 53% were male and their mean age was 64.1 years (Table 1 and Supporting Information, Table S26, in the online version of this article). In contrast, past users differed greatly from current users by sex, as only 36% were male (P < 0.05; Table 1 and Supporting Information, Table S26). The mean age of current users differed little from past users at 64.1 years vs 63.2 (P = NS), but 38% of current users were age 65 to 74 years and 51% were age > 65 years, vs only 27% and 43% of past users, respectively (P < 0.05; Table 1 and Supporting Information, Table S27, in the online version of this article). Among current and past statin users, race/ethnicity did not differ appreciably: 76% and 76% were Caucasian, 9% and 8% were Hispanic, 8% and 6% were African American, 4% and 6% were Asian, 1% and < 1% were Native American/Alaskan Native, 1% and 1% were mixed race, and 1% and 0% declined to answer, respectively (Table 1 and Supporting Information, Table S28, in the online version of this article).
3.3. Medical comorbidities
As expected for patients with ASCVD risk and cholesterol levels both high enough to warrant a statin prescription, certain comorbidities were common among ACTION patients; however, they were less common in past vs current statin users: hypertension, 58% vs 69%; T2DM, 17% vs 27%; and CHD, 4% vs 9%, respectively (all P < 0.05; Table 1 and Supporting Information, Table S1, in the online version of this article).
3.4. Use of statins and other medications
Certain details of statin use were queried among patients. Both current and past statin users were on average nearly 15 years out from first being told they had high cholesterol for which they subsequently received a statin (Table 2). As would be expected, current statin users had been on their current statin agent longer than past users had been on their most recent statin (mean of 8.4 years vs 3.5 years, respectively, P < 0.05; Table 2). Also, unsurprisingly, 39% of current users vs only 14% of past users had been on their current vs most recent statin (respectively) for ≥10 years (P < 0.05; Table 2). Among current statin users, 57% had taken only 1 statin since being diagnosed, 26% had taken 2 statins, 11% had taken 3 statins, and 5% had taken ≥4 statins (Table 2 and Supporting Information, Table S13, in the online version of this article). Past statin users had a generally similar distribution of having taken 1, 2, and 3 statins (53%, 28%, and 8%, respectively), except, interestingly, more past users had taken ≥4 statins (10% vs 5% of current users, P < 0.05; Table 2 and Supporting Information, Table S13).
Table 2.
Patients' use of statins
| Total Patients, N = 5014 | Current Statin Users, n = 4706 | Past Statin Users, n = 308 | |
|---|---|---|---|
| Years since hypercholesterolemia diagnosis by healthcare provider | 14.8 | 14.8 | 14.9 |
| Mean years on current or most recent statin therapy | 8.1 | 8.4a | 3.5 |
| On current/most recent statin for ≥10 years, % | 38 | 39a | 14 |
| No. of statins taken since diagnosis of hypercholesterolemia, % | |||
| 1 | 57 | 57 | 53 |
| 2 | 26 | 26 | 28 |
| 3 | 11 | 11 | 8 |
| ≥ 4 | 5 | 5 | 10a |
| Taking a high‐intensity statin, %b | N/A | 30 | N/A |
Abbreviations: ACC/AHA, American College of Cardiology/American Heart Association; LDL‐C, low‐density lipoprotein cholesterol; N/A, not applicable
Significant difference between current and past statin users, P < 0.05.
Defined as such by 2013 ACC/AHA Cholesterol Guidelines (eg, a statin that aims to lower LDL‐C by ≥50%, such as atorvastatin 40–80 mg or rosuvastatin 20–40 mg daily).14
Among current statin takers, 30% reported they were on a high‐intensity statin (atorvastatin 40–80 mg or rosuvastatin 20–40 mg daily), 42% reported they were not on a high‐intensity statin (implying that they were taking moderate‐ to low‐intensity statins), and 28% said they were not sure (Table 2 and Supporting Information, Table S4, in the online version of this article). Past users were not queried about the intensity of their (prior) statin use.
Relatively few current or past statin users said they were currently using or had ever used any one class of lipid‐lowering medication besides a statin. As might be expected, fewer current users were currently taking nonstatin lipid therapy: <1% to 3% for each of the various classes vs 1% to 6% for past statin users (higher in past users, P < 0.05 for nearly all class comparisons; see Supporting Information, Tables S2 and S3, in the online version of this article).
Nearly all current statin users (93%) were taking ≥1 other prescription medication (Table 3), a median of 4 agents per patient (Supporting Information, Table S5, in the online version of this article). Among current statin users, 37% were taking ≥1 of the following: a prescription medication for DM or 9 major classes of medications with the potential to interact adversely with a statin (calcium channel blockers, warfarin, amiodarone, azole antifungals, human immunodeficiency virus antiretrovirals, cyclosporine, digoxin, fibrates, and niacin), ranging from 1% to 7% of patients (Table 3 and Supporting Information, Tables S2 and S5, in the online version of this article). Unfortunately, however, neither (1) the use of 5 other medication classes with potential to interact adversely with statins (macrolide antibiotics, danazol, enalapril, rifampin, and colchicine), nor (2) the percentage of patients taking ≥1 of these 14 classes was queried. Thus, the number of ACTION patients currently taking a statin and another agent putting them potentially at risk for an adverse drug–drug interaction is unknown.
Table 3.
Patients' use of other prescription medications in addition to a statin
| Current Statin Users, n = 4706 | |
|---|---|
| Taking ≥1 other prescription medication + statin | 93 |
| Other medications patients were taking | |
| T2DM medications | 24 |
| Antiplatelet medications | 7 |
| CCBs | 6 |
| Warfarin | 5 |
| Amiodarone | 2 |
| Azole antifungals, antivirals (HIV/HCV), cyclosporine, digoxin | 1 |
| None of the above categories | 63 |
Abbreviations: CCB, calcium channel blocker; HCV, hepatitis C virus; HIV, human immunodeficiency virus; T2DM, type 2 diabetes mellitus. Data are presented as %.
In addition to prescription medications, 69% of current statin users reported taking ≥1 over‐the‐counter medication, a mean of 1.9 per patient; and 56% reported taking ≥1 vitamin or other dietary supplement, a mean of 1.6 per patient (see Supporting Information, Table S6, in the online version of this article). Overall, 99% of current statin users were taking a mean of 7.7 other medications plus supplements (Supporting Information, Table S6). Past statin users were not queried about other medications they were currently taking, nor about those they had taken when they were on a statin.
Despite the above finding that virtually all current statin users were taking ≥1 other medication or supplement, 76% reported they were “not very concerned” or “not at all concerned” (45% and 30%, respectively) about the possibility that the statin they were currently taking could interact with other medications or supplements (see Supporting Information, Table S17, in the online version of this article). In contrast, only 20% were “somewhat concerned,” and only 4% were “extremely concerned” about this possibility (Supporting Information, Table S17). Along the same line, when asked how much they agreed or disagreed with the statement “I have not/had not given much thought to how my statin may interact with other medications and supplements I take,” 59% of current statin users vs 51% of past users said they “strongly/somewhat agree” (P < 0.05), whereas 41% of current users and 49% of past users said they “strongly/somewhat disagree” (P < 0.05; see Supporting Information, Table S18, in the online version of this article).
3.5. Patient communication with healthcare providers
Patients were asked what they recalled being told by their healthcare provider when they were first prescribed a statin, and they could choose all options that applied to them. Only 33% of current users and 29% of past users said their healthcare provider explained “why the particular statin was being prescribed to me.” Further, only 25% of current users and 22% of past users were told “how the particular statin worked,” and, remarkably, only 22% of current users and 15% of past users could recall even being told “that there are different types of statins.” Additionally, only 18% of current users and 20% of past users were told “that their particular statin could potentially interact with other medications and supplements,” and only 10% of current users and 9% of past users were told “how the particular statin prescribed was different than others.” Thirty‐six percent of current users and 34% of past users said they couldn't remember what, if anything, they were told (at the time of their initial statin prescription) in this regard, and 15% percent of current users and 19% of past users chose none of the options offered (Table 4 and Supporting Information, Table S10, in the online version of this article). In a separate question, only 25% of current statin users responded affirmatively that “my [current] healthcare provider has explained that some statins are more likely than others to interact with other medications and supplements” (see Supporting Information, Table S15, in the online version of this article). Past statin users were not asked this question.
Table 4.
Patients given specific information about their statin by their healthcare provider at time of first prescription
| Total Patients, N = 5014 | Current Statin Users, n = 4706 | Past Statin Users, n = 308 | |
|---|---|---|---|
| Why the particular statin was being prescribed to me | 33 | 33 | 29 |
| How the particular statin worked | 24 | 25 | 22 |
| That there are different types of statins | 21 | 22 | 15 |
| That the particular statin could potentially interact with other medications and supplements | 18 | 18 | 20 |
| How the particular statin prescribed was different than others | 10 | 10 | 9 |
| Cannot remember | 36 | 36 | 34 |
| None of these | 15 | 15 | 19 |
Data are presented as %.
Patients were also asked how much input they had, compared with their healthcare provider, in choosing their current or past statin. These answers generally did not differ by current or past user status, respectively: 45% and 43% said “my healthcare provider told me which statin to take, without input from me”; 28% and 33% said “my healthcare provider was the primary decision‐maker, with some input from me”; and 20% vs 13% said “my healthcare provider and I were equally involved in the decision” (P < 0.05 for this one only). Thus, for both current and past users, 73% and 77% of choice of statin was entirely or at least largely driven by the provider. Given this result, very few patients reported primary input into this choice, whether they were current or past statin users: only 3% and 3% said “I was the primary decision‐maker with some input from my healthcare provider,” and only 4% and 7% said “I was the sole decision‐maker” (P < 0.05 for the latter difference only; Table 5 and Supporting Information, Table S16, in the online version of this article).
Table 5.
Patient input into choice of statin
| Total Patients, N = 5014 | Current Statin Users, n = 4706 | Past Statin Users, n = 308 | |
|---|---|---|---|
| Healthcare provider driven | 74 | 73 | 77 |
| My healthcare provider told me which statin to take without input from me | 45 | 45 | 43 |
| My healthcare provider was the primary decision‐maker with some input from me | 29 | 28 | 33 |
| My healthcare provider and I were equally involved in the decision | 19 | 20a | 13 |
| Patient driven | 7 | 7 | 10 |
| I was the primary decision‐maker with some input from my healthcare provider | 3 | 3 | 3 |
| I was the sole decision‐maker | 4 | 4 | 7a |
Data are presented as %.
Significant difference between current and former statin users, P < 0.05.
In separate questions solely asked of current statin users, only 45% responded that “I communicate openly with my healthcare provider about any challenges I face when I am on a statin”; only 25% said “my healthcare provider has explained that some statins are more likely than others to interact with other medications and supplements”; and fully 39% said “I usually don't ask my healthcare provider any questions about my statin and just take whatever they recommend” (see Supporting Information, Table S15, in the online version of this article). Past statin users were not asked these questions.
Patients were asked additional related questions about what they did at or around the time they were first prescribed a statin; they could choose all options that applied to them. Only 27% of current users and 27% of past users reported that “I asked my healthcare provider general questions about various statin options,” only 11% of current users and 14% of past users said “I questioned my healthcare provider's statin recommendation,” and only 8% of current users and 8% of past users said “I had read about statins and asked to be prescribed a specific one by name” (see Supporting Information, Table S11, in the online version of this article). Unfortunately, the potential impact of this set of results was weakened somewhat by the fact that 19% of current users and 24% of past users said they could not remember what they did at the time of their first statin prescription, and 45% of current statin users and 38% of past users chose none of these options (Supporting Information, Table S11).
The 89% and 86% of current and past statin users, respectively, who did not state that they questioned their provider's recommendation for a statin (see above and Supporting Information, Table S11, in the online version of this article) were then asked to give reasons for not questioning that recommendation by choosing all options that applied to them. Current vs past users differed somewhat in the following: 81% vs 74% said “I trusted their recommendation” (P < 0.05), and 16% vs 22% said “I assumed all statins are essentially the same” (P < 0.05; see Supporting Information, Table S12, in the online version of this article). On the other hand, current and past users did not differ in the following: 19% and 20% said “I didn't realize there were different statins to choose from,” 2% and 2% said “I [had] asked my friends and/or family members which statins they took, and assumed the same one would work for me,” and 3% and 6% chose “other” unspecified reasons (Supporting Information, Table S12).
Patients were also asked about actions they took to find out more about statin treatments after they were first diagnosed with high cholesterol, in addition to talking to their healthcare provider; they could choose all options that applied to them. Current users differed somewhat vs past users in that 26% vs 34%, respectively, said they “researched online/did a web search” (P < 0.05; see Supporting Information, Table S14, in the online version of this article), whereas there was little or no difference between current and past users, respectively, in the other choices: 16% and 20% “talked to a friend or family member who is taking a statin”; 12% and 8% “consulted a pharmacist”; 11% and 13% “visited that drug's website”; 6% and 6% “talked to a friend or family member who is not taking a statin”; 6% and 7% “consulted another healthcare provider”; and 2% and 2% said “other.” A number of patients, especially current users, chose none of these options (41% and 30%; P < 0.05) and 14% and 15% said they could not remember (Supporting Information, Table S14).
Several actions of healthcare providers were cited by a vast majority of both current and past statin users as being “extremely” or at least “somewhat” important when recommending a statin to prescribe: (1) that their healthcare provider “takes an individualized approach to selecting the right statin for me” (95% and 94%, respectively), (2) “recommends the lowest dose option possible” (90% and 93%, respectively), (3) “recommends a statin that is compatible with my diet” (88% and 88%, respectively), and (4) “helps me find a statin I can afford” (77% and 81%, respectively; see Supporting Information, Table S19, in the online version of this article).
3.6. Switching and stopping statins
As noted above, 43% of current statin users had switched statins at least once, but whether this involved an immediate change, without interruption of statin treatment, or occurred after whatever period of time off statins, was not queried. Similarly, 47% of past statin users had switched statins at least once before stopping, and the duration of time off statins again was not queried (Table 2).
Patients were asked several questions about their reasons for switching to their most recent statin, in the case of current users, and for stopping their last statin, in the case of past users. Strikingly, among current statin users, only 22% reported switching for side effects, including muscle/joint pain (17%) and/or other side effects (9%), whereas in sharp contrast, 55% of past users reported stopping due to symptoms, muscle/joint pain (42%), and/or non–muscle/joint pain (29%, all P < 0.05; Table 6; Supporting Information, Table S21, in the online version of this article; and Figure 1, part A). “Risk of interfering with other medications” was also a reason given for switching/stopping, more commonly by past users (9%) than current users (3%), and “other” reasons were given far more commonly by past users (26%) than current users (9%, P < 0.05 for both comparisons; Table 6; Supporting Information, Table S21; and Figure 1, part A). In contrast, “it was recommended to me” was a far more common reason for switching/stopping among current users (27%) than among past users (8%, P < 0.05 for this and the next 6 comparisons; Table 6 and Supporting Information, Table S21), as were medication costs (14% vs 7%), lack of insurance coverage (10% vs 2%), desire for a generic statin (14% vs 2%), lack of cholesterol efficacy (13% vs 6%), lack of triglyceride efficacy (11% vs 5%), and “don't know/can't remember” (13% vs 6%; Table 6; Supporting Information, Table S21; and Figure, 1 part B).
Table 6.
Patients' reasons for stopping or switching a statin
| Total Patients, N = 2306 | Current Statin Users Who Have Switched, n = 1998 | Past Statin Users, n = 308 | |
|---|---|---|---|
| Side effects experienced while on the medication | 27 | 22 | 55a |
| Muscle/joint pain | 20 | 17 | 42a |
| Side effects other than muscle/joint pain | 11 | 9 | 29a |
| It was recommended to me | 25 | 27a | 8 |
| The medication did not lower my LDL‐C (“bad cholesterol”) level enough | 13 | 13 | 15 |
| The cost of the medication | 13 | 14a | 7 |
| I wanted to switch from a brand‐name to a generic statin | 12 | 14a | 2 |
| The medication was not effective in managing my high cholesterol | 12 | 13a | 6 |
| The medication did not lower my TG level enough | 10 | 11a | 5 |
| The medication was not covered by my insurance | 9 | 10a | 2 |
| The medication did not address my overall cholesterol levels | 8 | 8 | 10 |
| The risk of interfering with other medications I was taking | 4 | 3 | 9a |
| I wanted to switch from a generic to a brand‐name statin | 1 | 2 | 0 |
| Other | 11 | 9 | 26a |
| Do not know/cannot remember | 12 | 13a | 6 |
Abbreviations: LDL‐C, low‐density lipoprotein cholesterol; TG, triglycerides. Data are presented as %.
Significant difference between current and former statin users, P < 0.05.
Figure 1.
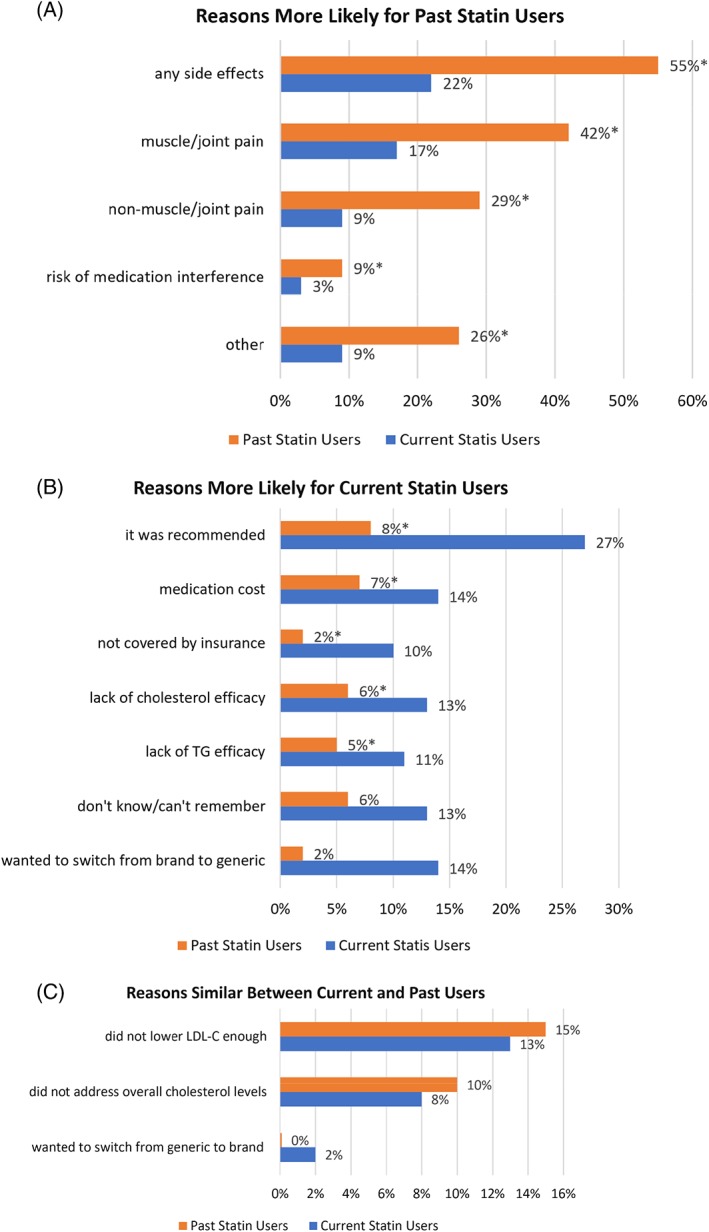
Reasons current users gave for switching statins and reasons past users gave for stopping statins: (A) reasons more likely for past users, (B) reasons more likely for current users, and (C) reasons of comparable importance to past and current users. Patients were allowed to choose as many options as applicable to them. (P < 0.05 for all comparisons in parts A and B; P = NS for all in part C.) Abbreviations: LDL‐C, low‐density lipoprotein cholesterol; NS, not significant; TG, triglycerides
Those who had discontinued a given statin were asked about the circumstances surrounding that discontinuation and could choose all options that applied to them. Tellingly, 49% of current statin users but only 12% of past users reported “I discussed any issues I was having with that statin with my healthcare provider and we decided on a better statin for me” (P < 0.05; see Supporting Information, Table S22, in the online version of this article). It is also striking to note that only 7% of current users but 35% of past users “stopped taking the statin before discussing with my healthcare provider” (P < 0.05; Supporting Information, Table S22). Among past users, 36% said “I told my healthcare provider I no longer wished to take a statin and I am now managing my high cholesterol with lifestyle modifications only,” whereas 21% said “I decided to stop taking medication to manage my high cholesterol altogether [no mention of ongoing diet],” and 10% said “I told my healthcare provider I no longer wished to take a statin and am now managing my high cholesterol with a different type of medicine other than a statin” (Supporting Information, Table S22). Of course, the last 3 choices did not apply to current users.
Interestingly, among the 30% of current statin users reporting to be on a high‐intensity statin (Table 2 and Supporting Information, Table S4, in the online version of this article), 56% “strongly or somewhat agreed” that they wished they “could take a lower‐intensity statin” to manage their hypercholesterolemia.
3.7. Patient issues less or unlikely related to provider communication
Interestingly, current and past statin users differed very little in their concern about their LDL‐C, with 10% and 10%, respectively, “extremely concerned”; 42% and 46%, respectively, “somewhat concerned”; 37% and 38%, respectively, “not very concerned”; and 12% and 6%, respectively, “not at all concerned” (see Supporting Information, Table S8, in the online version of this article). Further, neither current nor past statin users tended to be overly concerned about their LDL‐C level compared with other specific medical conditions, with only 14% to 31% more concerned, 34% to 54% equally concerned, and 22% to 52% less concerned, depending on the specific comparator condition (see Supporting Information, Table S9, in the online version of this article).
In sharp contrast, current vs past statin users differed greatly regarding whether they “had challenges with the first statin I took”: 11% vs 44% “strongly agreed” (P < 0.05) and 13% and 17% “somewhat agreed,” for a total of 24% vs 62% “strongly/somewhat agreed” among current vs past users, respectively (P < 0.05; see Supporting Information, Table S18, in the online version of this article).
4. DISCUSSION
The ACTION survey is one of the largest internet‐based surveys of current and past users of statins. A very important contribution is its insights into provider‐patient communication in general, and specifically regarding choices among individual statin agents and the potential impact of those choices on possible drug–drug interactions. First of all, certain responses indicating poor patient‐provider communication were far more common among past vs current statin users. As a prime example, only 12% of past users (vs fully 49% of current users who had switched their statin) reported discussing with their healthcare provider the issues they were having with the statin that they had discontinued or would soon discontinue, and decided on a better statin for themselves. As a result, the vast majority of the healthcare providers of past users were likely unaware of challenges the patient faced, thus preventing them from working with the patient to choose a better statin for their circumstances. Remarkably, more than one‐third of past users (35% vs only 7% of current users who had switched their statin) actually stopped statin use before even mentioning it to their healthcare provider, again precluding the provider from helping continue statin treatment. In addition, a lack of communication between the patient and provider was reported by past users; more than one‐third (36%) said “I told my healthcare provider I no longer wished to take a statin and I am now managing my high cholesterol with lifestyle modifications only,” whereas at least 1 in 5 said that they decided to stop taking any medication (21%), or at least stop taking statins (10%), to manage their high cholesterol. These findings in ACTION seem to complement those in USAGE in which past statin users were less satisfied with provider‐patient discussions than current users (65% vs 83%; P < 0.05).8
ACTION further showed that certain aspects of the patient end of provider‐patient communication were poor among both current and past users. Just barely over one‐quarter (27%) of either group asked their provider any questions about the various statin options when first prescribed a statin; not even half of current users (45%) said that they communicate “openly” with their provider regarding challenges related to taking a statin; and fully 2 of 5 (39%) said they usually do not ask any questions about their statin, simply taking whatever their provider recommends.
This lack of patient‐initiated dialogue appears likely related to a lack of provider‐initiated education of their patients, whether current or past statin users. When first prescribed a statin, only one‐third of patients recalled being told “why the particular statin was being prescribed,” and only about one‐fifth could recall being told “that there are different types of statins.” Further, one‐fifth or fewer recalled being told about potential statin interactions with other medications and supplements, and only one‐tenth recalled being told how their particular statin might differ from others. Although more than one‐third (36% and 34%) said they “can't remember” these points of those conversations, held years ago, this lack of memory suggests a lack of adequate communication, at least when judged by patient recall. In a similar manner, only one‐quarter of current statin users reported that their provider explained “that some statins are more likely than others to interact with other medications and supplements.” In line with this lack of patient education, providers also seemed infrequently to have solicited patient input into the choice of a statin, from either current or past statin users. Three‐quarters of patients said that their provider told them which statin to take “without” or with only “some” input from them.
The above remarkable lack of provider education and outreach, at least by patient perspective and recall, contrasts sharply with how important the vast majority of patients (whether current or past statin users) said it is that their providers “individualize” their selection of the “right statin” for them (95% and 94%), recommend “the lowest dose possible” (90% and 93%), and find one “compatible” with their diet (88% each) and affordable (77% and 81%). In a related response, among the nearly one‐third of current statin users who reported taking a high‐intensity statin, ≥50% said that they wished they could “take a lower‐intensity statin” to manage their hypercholesterolemia.
Although healthcare providers are likely confident that the particular statin they are prescribing for a particular patient is appropriate for that patient's characteristics and situation, the ACTION study results discussed above clearly show a need for better provider‐patient communication regarding many aspects of statin therapy. These include discussion of the various statin options; the rationale for the choice of a particular statin; and solicitation of patient concerns, questions, and input into the treatment decision. This “shared decision‐making” approach is strongly encouraged in the 2013 American College of Cardiology/American Heart Association (ACC/AHA) Cholesterol Guidelines14 and has been mentioned in several other contemporary guidelines, including the NLA Task Force on Lipid Safety–2014 update15 and the American Association of Clinical Endocrinologists (AACE) Expert Lipid Statement of 2017.16 The process of greater patient engagement promises to not only better provide information about any adverse effects or concerns about possible adverse effects, but, perhaps most important, to encourage and promote adherence to the regimen thus mutually selected. This is especially important for patients who have already had challenges or concerns sufficient to consider stopping their statin.
Two additional ACTION findings regarding high‐intensity statin dosing, discussed above, show patient reluctance to accept that dosing, despite its endorsement in the 2013 ACC/AHA Cholesterol Guidelines.14 First, the vast majority of all ACTION patients want their provider to recommend the “lowest [statin] dose option possible”; and second, a majority of patients who reported taking a high‐intensity statin dosage stated their desire to take lower‐intensity statins. Because high‐intensity statin use is medically desirable in most high‐risk patients, ACTION makes clear that achieving patient buy‐in for such treatment constitutes a challenge in statin‐related provider‐patient communication.
ACTION also focused on the potential for drug interactions with statins. Nearly all current statin users (93%) were taking ≥1 other prescription medication, a median of 4 such per patient, and essentially all (99%) were taking ≥1 prescription agent, over‐the‐counter medication, and/or vitamin or supplement, with a median of 7 separate products. Although the percentage of current statin users taking any one of the 14 major classes of medications with potential for adverse statin interaction was not completely queried, between 1% and 7% were taking each of 9 such classes, and so the total percentage who were taking ≥1 of the 14 was likely relatively high. Of concern given this setting, three‐quarters of current statin users (99% of whom were taking ≥1 other medication) said they were “not at all” or “not very” concerned about possible statin interactions with other medications. USAGE found that 84% of statin patients were taking ≥1 medication with the potential for an adverse interaction with a statin,8 whereas those on such medications had a 42% or 28% increase in the likelihood of experiencing muscle pain or stopping a statin for that reason, respectively.11 Thus, these ACTION results complement those of the USAGE survey in exploring possible contributors to statin nonadherence, which constitutes a major portion of the distance between ideal and actual statin use.
A strength of ACTION is the fact that the respondents were selected and then their responses were weighted to reflect closely the demographics of US adults, with 76% Caucasian, 8% African‐American, 5% Asian, and 9% Hispanic. This contrasts with USAGE, in which 92% were Caucasian and only 4% were African‐American, 1% were Asian, and 1% were Hispanic.8 Similarly, ACTION patients were more balanced by sex, with 52% male and 48% female, vs 39% male and 61% female in USAGE.8 Although status as a current vs past statin user did not differ significantly by race/ethnicity in ACTION, it did differ by sex, with females disproportionately being past users (64% vs 48% of all patients, P < 0.05; Table 1). Also, in USAGE, females were more likely to have discontinued their statin than were males.9
As might be expected, patients with any of the 3 major comorbidities related to atherosclerosis risk—hypertension, T2DM, and CHD—were each significantly more likely to be current statin users than past users (69% vs 58%, 27% vs 17%, and 9% vs 4%, respectively). Thus, in summary, patients who were female and those who lacked major ASCVD‐related comorbidities were more likely to have stopped their statin, potentially indicating that they believed that statin adherence was less needed due to lower ASCVD risk.
Finally, the reasons patients gave for switching to their most recent statin (current users) or for stopping their last statin used (past users) are interesting and instructive (Table 6 and Figure 1). Strikingly, all side effects were a reason among current statin users for switching in fewer than one‐quarter, but side effects were a reason in a majority of past users (P < 0.05) for stopping a statin. Thus, ACTION shows that statin‐associated muscle symptoms and other statin side effects are not only an important reason for switching among statin agents among patients who continue statin use, but, more important, they appear to be a major reason for statin discontinuation in the United States. Interestingly, perception of a “risk of interfering with other medications” by their statin was also more likely among past vs current users (9% vs 3%, respectively; P < 0.05), although not a common reason for either. In contrast, current users reported that provider recommendation, cost, lack of insurance coverage, desire to switch from brand to generic, lack of cholesterol‐ or triglyceride‐lowering efficacy, and “don't know/can't remember” were all more common in current vs past users (2× to 7× times more common; all P < 0.05). These reasons for switching rather than discontinuing are revealing in that they involve provider initiation or issues most obviously addressable by a provider, or issues that were minor enough that the patient could not recall them.
Importantly, these key ACTION results confirm similar findings in USAGE, in which muscle‐related side effects were reported by 60% and 25% of former and current users, respectively (P < 0.05), and in which the primary reason for switching by current users was cost (32%) and the primary reason for discontinuation was side effects (62%).8
4.1. Survey limitations
A limitation of this study is the somewhat unusual finding that only 6% of patients reported being past statin users and 94% said they were currently using a statin. Considering that ACTION study patients were, on average, very nearly 15 years out from their initial diagnosis of a high cholesterol level and current users had been taking their current statin agent for an average of 8.4 years, their reported statin use is far greater than that noted in most studies, in which discontinuation of statin therapy is roughly one‐half after 6 months to 1 year.2, 3, 4 There are several possible explanations for this large apparent discrepancy.
First and likely foremost is the fact that self‐reporting of statin use is likely to be higher than by objective determination. We are aware, however, of no study of substantial size that has had both subjective and objective data regarding statin use in the same patients, so this likelihood remains unconfirmed and not quantified. Second, ACTION does suggest some lack of compliance even among “current users,” 21% of whom said they “sometimes miss a dose, or [otherwise] do not take their treatment as prescribed.” These omissions were said to occur mainly because they “simply forgot” (76%), but about 1 in 10 said they had or worried about having side effects in the muscles/joints or elsewhere. Third, 6% of current users and nearly 2 in 5 past users said they had stopped taking a statin without talking to their provider.
Another possible explanation of the unusually high reported statin use in ACTION is the fact that the study population was, by design, somewhat older, and also was slightly over half male and with a high prevalence of major lipid‐related comorbidities, all of which are predictors of greater likelihood of reporting current statin use in this study. Another possible reason for the high percentage of ACTION patients reporting current statin use may have been the willingness of their providers to work to find a statin that they tolerated and that was suitable to their circumstances. Nearly half of current users reported having switched statin medication at least once, and many did several times, so current users may have been more common due to extra effort by providers. Finally, the nature of the survey, which included only a fraction of invitees, those who volunteered their time and did so relatively quickly, may have inadvertently and indirectly selected for individuals who, being more quick to volunteer for a study, were also by nature more compliant than the average patient in taking provider‐prescribed medication.
Another limitation of the ACTION survey is its online nature, which limited participation to individuals who had access to the internet and facility with its use. The generalizability of the survey findings is further limited by the fact that survey participation was limited to members of several panels who had agreed to participate in online surveys. Importantly, however, the topic of the survey was not disclosed to the subjects beforehand, reducing the selection bias that would occur from obtaining only patients who felt a desire to communicate about their experience with statin therapy. Individuals who choose to participate in surveys may differ from those who choose not to participate. Because the sample is based on those who agreed to participate, no estimates of theoretical sampling error can be calculated. Further, the survey did not provide an opportunity for participants to ask questions to clarify or explain the meaning of the questions. Also, the fact that the questions were multiple choice instead of “free text” meant that survey participants were given only limited opportunity to express their experience and opinions.
A final, obvious limitation is related to the self‐report nature of the survey data. Self‐reporting of medication choice and adherence is subject to recall bias.17 Importantly, we do not know the actual content of the provider‐patient discussions, only the patient recall of those conversations, and the survey was conducted an average of 15 years after the initial diagnosis took place. This point is, however, also a potential strength of the survey, because patient recall of a conversation is in some ways more important than what the provider actually said, because so much of the success or failure of statin therapy (or any chronic medical therapy) depends on what the patient can recall after the visit, even long after the visit.
5. CONCLUSION
ACTION provides evidence that patients starting statin therapy often are not told by their provider about the potential for adverse drug interactions between the statin they are taking and other prescription agents, even though such potential existed in a reasonable percentage of our patients. Further, patients often recalled not having been informed (or could not recall being informed) by their provider that statins differ in their potential for such drug–drug interactions, or even that ≥1 statin was available. Also, it appears that patients are not often given opportunity for discussion or input into the choice of a statin, nor “open” communication to discuss in subsequent provider visits any challenges they might face. This lack of “shared decision‐making” seemed to be far too common among current statin users, and it was even more common among past users.
The creation of an environment in which patients feel comfortable discussing concerns and asking questions about statin therapy before, during, and after treatment initiation may help with long‐term medication adherence. As a foundation for this, providers should ask their staff to obtain, from each statin‐taking patient, a list of all current prescription and over‐the‐counter medications as well as all dietary supplements. The following suggested provider statements might help facilitate provider‐patient communication:
At the beginning of statin treatment:
“What medications and supplements are you taking” (probably best done by clinic staff)
“What are your concerns or questions about taking a statin?”
“As we have discussed options among statin therapies, which statin appeals most to you? Why?”
Follow‐up after the initial prescription and later if a switch is needed:
“Most patients skip their statins a little or a lot. How often do you miss taking your statin?”
“Do you have any worries about, or problems with, the statin you're taking? If so, let's talk about it now.”
Better communication between providers and patients in general, and specifically more “shared decision‐making,” promises to enhance not only statin adherence and thus ASCVD event reduction, but also patient satisfaction and quality of life on statin therapy. More research is needed, however, to explore and assess methods and to verify outcomes of these enhanced efforts.
5.1. Conflicts of interest
Dr. Brinton has received honoraria related to speaking, consulting fees, and/or research grants from Akcea Therapeutics, Amarin, Amgen, Balchem, Boehringer Ingelheim, Kowa, Merck, Novo Nordisk, PTS Diagnostics, Regeneron, and Sanofi. The author declares no other potential conflicts of interest.
Supporting information
Table S1. Q1. Have you ever been diagnosed by a healthcare provider with any of the following health conditions? Please select all that apply.
Table S2. Q2. Which of the following types of prescription medication have you ever used to treat your high cholesterol? Please select all that apply.
Table S3. Q3. Which of the following types of prescription medication do you currently use to treat your high cholesterol? Please select all that apply.
Table S4. Q4. You mentioned that you are currently taking a statin. Are you taking a high‐Intensity statin? A high‐intensity statin is one that aims to lower your LDL‐C by 50% or more. For example, it includes 40–80 mg of atorvastatin or 20–40 mg of rosuvastatin daily.
Table S5. Q5. Which, if any, of the following prescription medications or types of medications are you currently taking in addition to your statin? Please select all that apply.
Table S6. Q6. In addition to your statin, how many prescription medications, over‐the‐counter medications, and non‐prescription supplements and vitamins are you currently taking? If you are not sure, please provide your best estimate.
Table S7. Q7. Would you say that in general your health is…?
Table S8. Q8. Now, we'd like to ask you some questions about your cholesterol levels. How concerned are you about your LDL‐C (“bad cholesterol”) level?
Table S9. Q9. Thinking about your LDL‐C (“bad cholesterol”) level, are you more, less, or equally concerned about each of the following? Patients are divided into 3 sub‐tables: (a) more concerned, (b) equally concerned, and (c) less concerned than about LDL‐C.
Table S10. Q10. You indicated earlier you [have previously treated/are currently treating] your high cholesterol with a statin. When you were first prescribed a statin, did your healthcare provider tell you any of the following? Please select all that apply.
Table S11. Q11. Which of the following did you do when you were first prescribed a statin? Please select all that apply.
Table S12. This question was asked only of those 89% in Table S11 who did not answer Q11 “I questioned my healthcare provider's statin recommendation.” Q12. You mentioned you did not question your healthcare provider's first statin recommendation. Why not?
Table S13. Q13. In total, how many different statin medications have you taken [in addition to the one you are currently taking,] since being diagnosed with high cholesterol?
Table S14. Q14. After you were diagnosed with high cholesterol, besides talking to your healthcare provider who diagnosed you, did you do any of the following to find out more about statin treatments? Please select all that apply.
Table S15. Q15. This question was asked only of those currently taking a statin and seeing an HCP. Thinking about the healthcare provider who helps you manage your high cholesterol now, which of the following are true for you? Please select all that apply.
Table S16. Q16. How much input did you have in choosing your [current/past] statin, compared to your healthcare provider?
Table S17. This question was asked only of those currently taking a statin and at least one other medication. Q17. How concerned are you about the possibility of the statin medication you are currently taking interacting with other medications or supplements?
Table S18. Summary of Strongly/Somewhat Agreed with the following questions. Q18. How much do you agree or disagree with each of the following statements?
Table S19. Summary of Extremely/Somewhat Important to Patients. Q19. How important is it that your healthcare provider does each of the following when recommending a statin to prescribe to you?
Table S20. Q20. Which, if any, of the following side effects have you experienced while taking your current statin? Please select all that apply.
Table S21. Among current statin users, this question was asked only of those who reported having taken more than 1 statin medication. Q21. Why did you [stop/switch from] the most recent statin medication you were taking? Please select all that apply.
Table S22. Q22. Among current statin users, this question was asked only of those who have taken more than 1 statin medication. Thinking again about the most recent time you stopped or switched your statin medication, which of the following happened? Please select all that apply.
Table S23. Q23. Some patients taking statins report that they delayed taking a statin after it was prescribed, sometimes miss a dose of their treatment, or do not take their treatment as prescribed by their healthcare provider. Have any of these things ever happened to you?
Table S24. Q24. Asked ONLY of those answering “yes” to Q23: You mentioned that you delayed taking a statin once it was prescribed to you, have missed a dose of your statin treatment or have not taken it as prescribed. Which of the following, if any, are reasons why? Please select all that apply.
Table S25. Q25. We have one final question for you about your experiences with statins. Have you ever done or experienced any of the following? Please select all that apply.
Table S26. Q26. Are you?
Table S27. Q27. Respondent Age.
Table S28. Q28. Racial Background/Ethnicity
Brinton EA. Understanding Patient Adherence and Concerns with STatins and MedicatION Discussions With Physicians (ACTION): A survey on the patient perspective of dialogue with healthcare providers regarding statin therapy. Clin Cardiol. 2018;41:710–720. 10.1002/clc.22975
Funding information The ACTION survey was funded by Kowa Pharmaceuticals America, Inc
REFERENCES
- 1. US Centers for Disease Control and Prevention . Heart disease statistics and maps. https://www.cdc.gov/heartdisease/facts.htm. Updated: November 28, 2017. Accessed March 15, 2018.
- 2. Mann DM, Woodward M, Muntner P, et al. Predictors of nonadherence to statins: a systematic review and meta‐analysis. Ann Pharmacother. 2010;44:1410–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Helin‐Salmivaara A, Lavikainen PT, Korhonen MJ, et al. Pattern of statin use among 10 cohorts of new users from 1995 to 2004: a register‐based nationwide study. Am J Manag Care. 2010;16:116–122. [PubMed] [Google Scholar]
- 4. Rublee DA, Chen SY, Mardekian J, et al. Evaluation of cardiovascular morbidity associated with adherence to atorvastatin therapy. Am J Ther. 2012;19:24–32. [DOI] [PubMed] [Google Scholar]
- 5. Blackburn DF, Dobson RT, Blackburn JL, et al. Cardiovascular morbidity associated with nonadherence to statin therapy. Pharmacotherapy. 2005;25:1035–1043. [DOI] [PubMed] [Google Scholar]
- 6. Raju SB, Varghese K, Madhu K. Management of statin intolerance. Indian J Endocrinol Metab. 2013;17:977–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. [DOI] [PubMed] [Google Scholar]
- 8. Cohen JD, Brinton EA, Ito MK, et al. Understanding Statin Use in America and Gaps in Patient Education (USAGE): an internet‐based survey of 10 138 current and former statin users. J Clin Lipidol. 2012;6:208–215. [DOI] [PubMed] [Google Scholar]
- 9. Wei MY, Ito MK, Cohen JD, et al. Predictors of statin adherence, switching and discontinuation in the USAGE survey: understanding the use of statins in America and gaps in patient education. J Clin Lipidol. 2013;7:472–483. [DOI] [PubMed] [Google Scholar]
- 10. Karalis DG, Wild RA, Maki KC, et al. Gender differences in side effects and attitudes regarding statin use in the Understanding Statin Use in America and Gaps in Patient Education (USAGE) study. J Clin Lipidol. 2016;10:833–841. [DOI] [PubMed] [Google Scholar]
- 11. Ito MK, Maki KC, Brinton EA, et al. Muscle symptoms in statin users, associations with cytochrome P450, and membrane transporter inhibitor use: a subanalysis of the USAGE study. J Clin Lipidol. 2014;8:69–76. [DOI] [PubMed] [Google Scholar]
- 12. Brinton EA, Maki KC, Jacobson TA, et al. Metabolic syndrome is associated with muscle symptoms among statin users. J Clin Lipidol. 2016;10:1022–1029. [DOI] [PubMed] [Google Scholar]
- 13. Jacobson TA, Khan A, Maki KC, et al. Provider recommendations for patient‐reported muscle symptoms on statin therapy: insights from the Understanding Statin Use in America and Gaps in Patient Education survey. J Clin Lipidol. 2018;12:78–88. [DOI] [PubMed] [Google Scholar]
- 14. Stone NJ, Robinson J, Lichtenstein AH, et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;01.cir.0000437738.63853.7a.
- 15. Jacobson TA. NLA Task Force on Statin Safety—2014 update. J Clin Lipidol. 2014;8(3 suppl):S1–S4. [DOI] [PubMed] [Google Scholar]
- 16. Jellinger PS, Handelsman Y, Rosenblit PD, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017;23(suppl 2):1–87. [DOI] [PubMed] [Google Scholar]
- 17. Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods J Multidiscip Healthc. 2016;9:211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Q1. Have you ever been diagnosed by a healthcare provider with any of the following health conditions? Please select all that apply.
Table S2. Q2. Which of the following types of prescription medication have you ever used to treat your high cholesterol? Please select all that apply.
Table S3. Q3. Which of the following types of prescription medication do you currently use to treat your high cholesterol? Please select all that apply.
Table S4. Q4. You mentioned that you are currently taking a statin. Are you taking a high‐Intensity statin? A high‐intensity statin is one that aims to lower your LDL‐C by 50% or more. For example, it includes 40–80 mg of atorvastatin or 20–40 mg of rosuvastatin daily.
Table S5. Q5. Which, if any, of the following prescription medications or types of medications are you currently taking in addition to your statin? Please select all that apply.
Table S6. Q6. In addition to your statin, how many prescription medications, over‐the‐counter medications, and non‐prescription supplements and vitamins are you currently taking? If you are not sure, please provide your best estimate.
Table S7. Q7. Would you say that in general your health is…?
Table S8. Q8. Now, we'd like to ask you some questions about your cholesterol levels. How concerned are you about your LDL‐C (“bad cholesterol”) level?
Table S9. Q9. Thinking about your LDL‐C (“bad cholesterol”) level, are you more, less, or equally concerned about each of the following? Patients are divided into 3 sub‐tables: (a) more concerned, (b) equally concerned, and (c) less concerned than about LDL‐C.
Table S10. Q10. You indicated earlier you [have previously treated/are currently treating] your high cholesterol with a statin. When you were first prescribed a statin, did your healthcare provider tell you any of the following? Please select all that apply.
Table S11. Q11. Which of the following did you do when you were first prescribed a statin? Please select all that apply.
Table S12. This question was asked only of those 89% in Table S11 who did not answer Q11 “I questioned my healthcare provider's statin recommendation.” Q12. You mentioned you did not question your healthcare provider's first statin recommendation. Why not?
Table S13. Q13. In total, how many different statin medications have you taken [in addition to the one you are currently taking,] since being diagnosed with high cholesterol?
Table S14. Q14. After you were diagnosed with high cholesterol, besides talking to your healthcare provider who diagnosed you, did you do any of the following to find out more about statin treatments? Please select all that apply.
Table S15. Q15. This question was asked only of those currently taking a statin and seeing an HCP. Thinking about the healthcare provider who helps you manage your high cholesterol now, which of the following are true for you? Please select all that apply.
Table S16. Q16. How much input did you have in choosing your [current/past] statin, compared to your healthcare provider?
Table S17. This question was asked only of those currently taking a statin and at least one other medication. Q17. How concerned are you about the possibility of the statin medication you are currently taking interacting with other medications or supplements?
Table S18. Summary of Strongly/Somewhat Agreed with the following questions. Q18. How much do you agree or disagree with each of the following statements?
Table S19. Summary of Extremely/Somewhat Important to Patients. Q19. How important is it that your healthcare provider does each of the following when recommending a statin to prescribe to you?
Table S20. Q20. Which, if any, of the following side effects have you experienced while taking your current statin? Please select all that apply.
Table S21. Among current statin users, this question was asked only of those who reported having taken more than 1 statin medication. Q21. Why did you [stop/switch from] the most recent statin medication you were taking? Please select all that apply.
Table S22. Q22. Among current statin users, this question was asked only of those who have taken more than 1 statin medication. Thinking again about the most recent time you stopped or switched your statin medication, which of the following happened? Please select all that apply.
Table S23. Q23. Some patients taking statins report that they delayed taking a statin after it was prescribed, sometimes miss a dose of their treatment, or do not take their treatment as prescribed by their healthcare provider. Have any of these things ever happened to you?
Table S24. Q24. Asked ONLY of those answering “yes” to Q23: You mentioned that you delayed taking a statin once it was prescribed to you, have missed a dose of your statin treatment or have not taken it as prescribed. Which of the following, if any, are reasons why? Please select all that apply.
Table S25. Q25. We have one final question for you about your experiences with statins. Have you ever done or experienced any of the following? Please select all that apply.
Table S26. Q26. Are you?
Table S27. Q27. Respondent Age.
Table S28. Q28. Racial Background/Ethnicity


