Watch a video presentation of this article
Answer questions and earn CME
Abbreviations
- HABR
hepatic arterial buffer response
- MELD
Model for End‐Stage Liver Disease
The liver is a highly vascular organ that receives approximately 25% of cardiac output and is prone to a spectrum of circulatory disturbances and vascular insult.1 Congestive hepatopathy describes the manifestations of chronic, passive congestion of the liver in the setting of heart failure or other cardiac defects that result in elevation of the central venous pressure.2 Circulatory impairment of the liver can also occur in the setting of a spectrum of primary vascular disorders that arise at different anatomic locations in the liver, including sinusoidal obstruction syndrome, portal vein thrombosis, Budd‐Chiari syndrome, and peliosis hepatitis.3, 4 This article focuses on the pathophysiology and clinical features of passive congestive disorders related to cardiac dysfunction.
Overview of Hepatic Circulation
Well‐oxygenated arterial blood comprises only about 25% of total hepatic blood flow. The remaining 75% of hepatic blood flow consists of deoxygenated blood supplied by the portal vein at venous pressure (approximately 6 mm Hg).5 The hepatic artery autoregulates blood flow via the hepatic arterial buffer response (HABR), whereby decreased portal flow instigates compensatory upregulation of hepatic arterial flow and vice versa.6 This regulatory response maintains hepatic oxygenation and clearance, and preserves a constant level of total hepatic blood flow.7, 8 It is estimated that the HABR can compensate for a 25% to 60% decrease in portal blood flow.6, 9 In contrast, portal venous flow is not autoregulated and is therefore dependent on mesenteric circulation and the gradient between portal and hepatic venous pressures.
Congestive Hepatopathy
Any cause of right ventricular heart failure may precipitate hepatic congestion, including constrictive pericarditis, tricuspid regurgitation, mitral stenosis, cardiomyopathy, and cor pulmonale. Several forms of congenital heart disease are associated with central venous hypertension and passive congestion, including single ventricular physiology after the Fontan procedure, Ebstein anomaly, and atrial and ventricular septal defects.10
Congestion predisposes to hepatic injury through three major pathogenetic mechanisms: (1) decreased hepatic blood flow, (2) decreased arterial oxygen saturation, and (3) increased hepatic venous pressures. Elevated central venous pressure transmits to the hepatic veins and sinusoids, and thereby decreases portal venous inflow.3, 10 Increased hepatic venous pressure also causes sinusoidal congestion, dilation of sinusoidal fenestrae, and exudation of protein and fluid into the space of Disse. Accumulation of exudate into the space of Disse then impairs diffusion of oxygen and nutrients to hepatocytes.3, 11 Decreased hepatic blood flow further increases susceptibility to injury in settings that compromise arterial flow, such as hypotension, arrhythmias, or left‐sided heart failure, which can precipitate ischemic hepatopathy.10
Grossly, the congested liver has been characterized as a “nutmeg liver,”12 with dark centrilobular zones reflecting sinusoidal congestion alternating with pale periportal zones with normal or fatty liver tissue (Fig. 1).12, 13 Histologically, passive congestion of the liver is reflected by sinusoidal dilation, congestion, and hepatocyte atrophy most prominent in zone 3 (Fig. 2).14, 15 Elevated hepatic venous pressures may precipitate extravasation of red blood cells into the space of Disse. The extent of necrosis, inflammation, and dilation has been correlated with right atrial and hepatic pressures,16 although ischemia may lead to findings of necrosis as well. Chronic congestion leads to perivenular fibrosis and, eventually, cirrhosis.14
Figure 1.

“Nutmeg liver” characteristic of congestive hepatopathy. Dark centrilobular zones reflecting sinusoidal congestion alternate with pale periportal zones.
Figure 2.
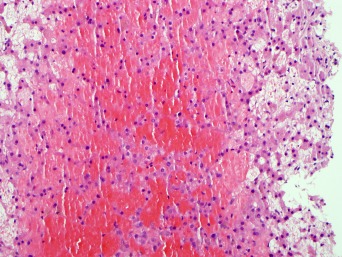
Characteristic histological changes reflective of congestive hepatopathy, including sinusoidal dilatation, congestion, hepatic cord atrophy, and extravasation of red blood cells into the hepatocytes.
Clinical Course
Many patients with congestive hepatopathy remain asymptomatic from their liver disease and are identified through abnormalities in routine laboratory evaluations. Characteristic laboratory abnormalities include mild elevations of serum aminotransferase levels to two to three times the upper limit of normal.2 Unconjugated hyperbilirubinemia may be present, although the total bilirubin level rarely exceeds 3 mg/dL. Hypoalbuminemia is present in 30% to 50% of patients and is generally mild. This finding does not correlate with histological liver damage and may be secondary to malnutrition or protein‐losing enteropathy in this population.3 When symptomatic, patients may experience dull right upper quadrant pain secondary to stretching of the liver capsule or, uncommonly, jaundice. Normal to minimal elevation of alkaline phosphatase can differentiate obstructive jaundice from a cardiac cause.3 Acute cardiac decompensation may instigate abrupt onset of jaundice and marked elevation of liver enzymes and bilirubin.
Clinical stigmata of portal hypertension or portosystemic shunts are generally absent until the development of cirrhosis.17 Physical examination may be remarkable for hepatomegaly and signs of right‐heart failure, including hepatojugular reflux and peripheral edema. The liver may be pulsatile in the setting of tricuspid regurgitation. Loss of this pulsatility suggests progression to cardiac cirrhosis.3 Although overt, clinically significant ascites is rare, the presence of ascites warrants diagnostic paracentesis. Because of preserved liver synthetic function, ascitic total protein content is high, usually more than 2.5 g/dL, with serum albumin‐ascites gradient greater than 1.1.
Congestive hepatopathy should be suspected in patients with liver enzyme abnormalities and right‐sided heart failure or other cause of elevated central pressures. Screening for viral and metabolic liver disease should be undertaken to rule out concomitant liver pathology, particularly those disorders associated with cardiomyopathy, such as amyloidosis and hemochromatosis.2
Treatment of congestive hepatopathy consists of management of the underlying cardiac condition with optimization of cardiac output. Diuresis can improve hepatic congestion but requires caution to avoid precipitating hepatic ischemia.2 Hemodynamic optimization may reverse the early changes of congestive hepatopathy. In severe cases refractory to medical management, improvement in liver injury has been noted after left ventricular assist device (LVAD) implantation or cardiac transplantation.18, 19 Liver function is an important variable when considering cardiac transplantation in patients with heart failure because studies suggest that patients with higher Model for End‐Stage Liver Disease (MELD) and modified MELD scores have worse outcomes 30 days after surgery and reduced 10‐year survival rates.20
Liver disease related to congestive hepatopathy is rarely responsible for significant morbidity or mortality. The underlying cardiac disease generally determines clinical outcome. Surprisingly, progression to cardiac cirrhosis has not been found to correlate with poorer prognosis and can demonstrate some reversibility with optimization of cardiac function. Although fulminant hepatic failure has been reported in the setting of heart failure,21 this is generally attributable to a superimposed ischemic insult.
Acknowledgment. The authors thank Dr. Vishal S. Chandan for providing Figures 1 and 2.
Potential conflict of interest: Nothing to report.
REFERENCES
- 1. Ford RM, Book W, Spivey JR. Liver disease related to the heart. Transplant Rev (Orlando) 2015;29:33‐37. [DOI] [PubMed] [Google Scholar]
- 2. Weisberg IS, Jacobson IM. Cardiovascular diseases and the liver. Clin Liver Dis 2011;15:1‐20. [DOI] [PubMed] [Google Scholar]
- 3. Giallourakis CC, Rosenberg PM, Friedman LS. The liver in heart failure. Clin Liver Dis 2002;6:947‐967, viii‐ix. [DOI] [PubMed] [Google Scholar]
- 4. DeLeve LD. Vascular liver diseases. Curr Gastroenterol Rep 2003;5:63‐70. [DOI] [PubMed] [Google Scholar]
- 5. Lautt WW. Hepatic Circulation: Physiology and Pathophysiology. San Rafael, CA: American Physiology Society, Bethesda, Maryland, USA; 2009. [PubMed] [Google Scholar]
- 6. Lautt WW. Mechanism and role of intrinsic regulation of hepatic arterial blood flow: hepatic arterial buffer response. Am J Physiol 1985;249:G549‐G556. [DOI] [PubMed] [Google Scholar]
- 7. Lautt WW. The hepatic artery: subservient to hepatic metabolism or guardian of normal hepatic clearance rates of humoral substances. Gen Pharmacol 1977;8:73‐78. [DOI] [PubMed] [Google Scholar]
- 8. Eipel C, Abshagen K, Vollmar B. Regulation of hepatic blood flow: the hepatic arterial buffer response revisited. World J Gastroenterol 2010;16:6046‐6057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lautt WW. Relationship between hepatic blood flow and overall metabolism: the hepatic arterial buffer response. Fed Proc 1983;42:1662‐1666. [PubMed] [Google Scholar]
- 10. Asrani SK, Asrani NS, Freese DK, Phillips SD, Warnes CA, Heimbach J, Kamath PS. Congenital heart disease and the liver. Hepatology 2012;56:1160‐1169. [DOI] [PubMed] [Google Scholar]
- 11. Safran AP, Schaffner F. Chronic passive congestion of the liver in man. Electron microscopic study of cell atrophy and intralobular fibrosis. Am J Pathol 1967;50:447‐463. [PMC free article] [PubMed] [Google Scholar]
- 12. Sherlock S. The liver in heart failure; relation of anatomical, functional, and circulatory changes. Br Heart J 1951;13:273‐293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lefkowitch JH, Mendez L. Morphologic features of hepatic injury in cardiac disease and shock. J Hepatol 1986;2:313‐327. [DOI] [PubMed] [Google Scholar]
- 14. Dai DF, Swanson PE, Krieger EV, Liou IW, Carithers RL, Yeh MM. Congestive hepatic fibrosis score: a novel histologic assessment of clinical severity. Mod Pathol 2014;27:1552‐1558. [DOI] [PubMed] [Google Scholar]
- 15. Arcidi JM Jr, Moore GW, Hutchins GM. Hepatic morphology in cardiac dysfunction: a clinicopathologic study of 1000 subjects at autopsy. Am J Pathol 1981;104:159‐166. [PMC free article] [PubMed] [Google Scholar]
- 16. Myers RP, Cerini R, Sayegh R, Moreau R, Degott C, Lebrec D, Lee SS. Cardiac hepatopathy: clinical, hemodynamic, and histologic characteristics and correlations. Hepatology 2003;37:393‐400. [DOI] [PubMed] [Google Scholar]
- 17. Naschitz JE, Slobodin G, Lewis RJ, Zuckerman E, Yeshurun D. Heart diseases affecting the liver and liver diseases affecting the heart. Am Heart J 2000;140:111‐120. [DOI] [PubMed] [Google Scholar]
- 18. Russell SD, Rogers JG, Milano CA, Dyke DB, Pagani FD, Aranda JM, et al.; HeartMate II Clinical Investigators . Renal and hepatic function improve in advanced heart failure patients during continuous‐flow support with the HeartMate II left ventricular assist device. Circulation 2009;120:2352‐2357. [DOI] [PubMed] [Google Scholar]
- 19. Dichtl W, Vogel W, Dunst KM, Grander W, Alber HF, Frick M, et al. Cardiac hepatopathy before and after heart transplantation. Transpl Int 2005;18:697‐702. [DOI] [PubMed] [Google Scholar]
- 20. Chokshi A, Cheema FH, Schaefle KJ, Jiang J, Collado E, Shahzad K, et al. Hepatic dysfunction and survival after orthotopic heart transplantation: application of the MELD scoring system for outcome prediction. J Heart Lung Transplant 2012;31:591‐600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kisloff B, Schaffer G. Fulminant hepatic failure secondary to congestive heart failure. Am J Dig Dis 1976;21:895‐900. [DOI] [PubMed] [Google Scholar]


