Watch a video presentation of this article
Watch the interview with the author
Abbreviations
- HCC
hepatocellular carcinoma
- HCV
hepatitis C virus
- NAFL
nonalcoholic fatty liver
- NAFLD
nonalcoholic fatty liver disease
- NASH
nonalcoholic steatohepatitis
Nonalcoholic Steatohepatitis
Together with nonalcoholic fatty liver (NAFL; hepatic steatosis without presence of significant inflammation), nonalcoholic steatohepatitis (NASH; a more serious form of hepatic steatosis associated with hepatic inflammation) represents a spectrum of liver pathology that resembles alcohol‐induced fatty liver damage but occurs in patients with no history of extreme alcohol consumption (i.e., nonalcoholic fatty liver disease [NAFLD]). NAFLD is strongly associated with obesity and the metabolic syndrome and is becoming similarly epidemic.1 The main causes for NAFLD are probably excess calorie intake from glucose or fructose and saturated fatty acids in combination with a lack of exercise and physical activity.2, 3 In the United States, studies report a prevalence rate of NAFLD up to 25% with biopsy‐ or aminotransferase‐based examinations, indicating a NASH prevalence rate of 3% to 8% (around 25% of those patients with NAFLD).4, 5, 6 Globally, the NAFLD prevalence rate is estimated to be around 25%, with up to 70% of patients with NAFLD affected by NASH.1 However, because biopsy‐based studies are problematic and noninvasive tests that reliably differentiate NASH from NAFLD are not established, it is not possible to assess the true prevalence and incidence rates. One study with a limited patient number using liver biopsy samples estimates that liver cirrhosis develops in about 25% of patients with NASH, suggesting that 1.5% to 2% of the US population suffers from cirrhosis caused by NAFLD (which is twice as high as cirrhosis related to chronic hepatitis C virus [HCV]).5 Thus, NASH also is predicted to become the leading indication for liver transplantation, surpassing chronic HCV in the near future.5 Finally, the overall long‐term mortality rate of 34% to 69% in Western patients with NAFLD (including patients with cirrhosis and/or liver cancer) in a 15‐year follow‐up is higher than in the general population of the same age and sex.7
Hepatocellular Carcinoma
HCC, the most common primary liver cancer, is currently considered the fifth most common cancer and the third leading cause of cancer‐related death in the United States.8 Its annual incidence (which is virtually identical to its mortality, underscoring the high case fatality rate) was at least 6 per 100,000 in the United States in 2010.8, 9 Currently, HCV is the most common risk factor for HCC within the Western countries, accounting for 30% to 50% of all cases, followed by alcohol‐related liver disease (10%‐20%) and hepatitis B (10%‐15%).10 HCC related to cryptogenic liver disease accounts for another 15% to 50% of HCC cases in the United States.10 NAFLD and NASH as increasingly recognized risk factors of HCC also have been proposed as underlying causes of many cases of cryptogenic cirrhosis (thus, the true prevalence rates of NAFLD/NASH‐related HCC might be underestimated in many studies) and are discussed in the following section.
HCC in NASH
The development and epidemiology of NAFLD/NASH‐associated HCC is depicted in Figure 1 demonstrating that patients with NAFLD/NASH are at an increased risk for HCC. In a 16‐year follow‐up study, the standardized incidence ratio of HCC in patients with NAFLD/NASH was 4.4.5 Consistently, the prevalence of HCC related to NAFLD/NASH is increasing worldwide; however, studies report different prevalence rates ranging between 4% and 22% in Western countries as reviewed by Michelotti et al.5 (Table 1). In another population‐based study in the United States, NAFLD accounted for 59% of HCC cases, with a cumulative incidence rate of 0.3% over a 6‐year follow‐up.11 For NASH, the annual incidence rate in a recent global meta‐analysis was 5.3 per 1000 person‐years.1 The mortality rates for HCC range from 0.25% to 2.3% over 8.3 and 13.7 years of follow‐up, respectively.7 Thus, NAFLD/NASH‐associated HCC is the leading cause of obesity‐related cancer deaths in middle‐aged men in the United States.5 The lower prevalences in Asia might reflect the fact that viral hepatitis remains endemic in those countries, causing the majority of HCC cases. Some studies also systematically ignore NAFLD/NASH‐related HCC cases because they attribute HCC to cryptogenic cirrhosis. Thus, the exact burden of HCC associated with NAFLD/NASH remains uncertain, but it seems clear that NAFLD and NASH are going to be the most common underlying causative risk factors for HCC globally, surpassing viral or alcohol‐related cirrhosis in the future.1, 7 However, etiological risk factors cannot be regarded separately because they might also affect the risk for HCC in other liver diseases. For example, in chronic HCV, the risk for HCC is up to 3‐fold higher in patients with coincident steatosis hepatis/NAFL than in those without. Opposite trends have been reported for steatosis hepatis/NAFL and HCC risk in patients with chronic hepatitis B.5 As expected, the HCC risk in patients with NAFLD depends on the severity of the underlying liver condition. Patients with NASH seem to have a much higher risk for HCC than individuals with simple steatosis hepatic/NAFL, with NASH itself as important risk factor.5, 11 Advanced fibrosis has been reported to increase the risk for HCC up to 25‐fold.5 Finally, individuals with NAFLD/NASH and cirrhosis have the highest risk for HCC up to 13% over 3 years compared with 0% to 3% over one to two decades in NAFLD cohorts without cirrhosis.5, 10 Thus, cirrhosis increases the risk but is clearly not required for HCC development during NAFLD.5, 12 Only approximately 45% to 50% of patients with NASH‐associated HCC exhibit cirrhosis.11, 12 Risk factors for HCC development in NASH are type 2 diabetes mellitus,13 which is also a predictor of mortality in NASH and HCV,11 whereas age or sex do not seem to affect HCC risk. In a large population‐based study, alcohol consumption was also identified as a risk factor for HCC in NASH.8 These findings suggest that NAFLD should no longer be seen as exclusion diagnosis but should be recognized as an entity based on metabolic injury to the liver. NAFLD can be present in parallel to other liver diseases, including HCV and significant alcohol consumption. Thus, when assessing HCC risk, multiple risk factors because of underlying causes of liver disease have to be considered.
Figure 1.
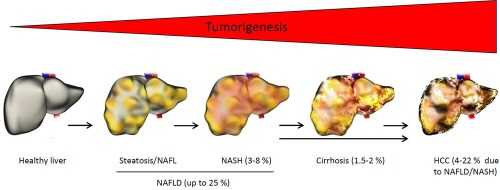
Pathogenesis and epidemiology of NAFLD/NASH‐related HCC. Prevalence rates are given for the population of the United States. HCC prevalence rates are related to patients with NAFLD/NASH (see Table 1). The long arrow indicates that HCC also can develop in patients with NAFLD/NASH who do not have cirrhosis.
Table 1.
Epidemiology of NAFLD/NASH‐Associated HCC
| Study (year) | Country | Patients with HCC, n | HCC Caused by NAFLD/NASH, % |
|---|---|---|---|
| Gonçalves et al. (2013)14 | Brazil | 1,516 | 4 |
| Yang et al. (2012)15 | United States | 47 | 11 |
| Tokushige et al. (2011)16 | Japan | 14,530 | 2 |
| Hucke et al. (2011)17 | Austria | 850 | 5 |
| Ertle et al. (2011)12 | Germany | 162 | 22 |
| Kawada et al. (2009)18 | Japan | 1,168 | 1 |
| Malik et al. (2009)19 | United States | 447 | 4 |
| Guzman et al. (2008)20 | United States | 50 | 10 |
| Marrero et al. (2002)21 | United States | 105 | 13 |
Adapted with permission from Nature Reviews Gastroenterology & Hepatology.5 Copyright 2013, Macmillan Publishers.
Summary
NAFLD and subsequently NASH affect a large proportion of the Western population, and their incidences and prevalences are increasing to epidemic proportions worldwide. Especially, but not only, because of cirrhosis, NAFLD/NASH increases the risk for liver cancer, a disease with poor clinical outcomes and limited therapeutic options. Consistently, the incidence and prevalence of HCC are also increasing. HCC is now a leading cause of obesity‐related cancer deaths, and NAFLD and NASH are predicted to be the most common underlying etiological risk factors for HCC and liver transplantation in the future.
This study was supported by grant D/107‐114400 (IFORES) to C.D.F.
Potential conflict of interest: The authors have no conflicts of interest.
REFERENCES
- 1. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease: meta‐analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016;64:73‐84. [DOI] [PubMed] [Google Scholar]
- 2. Mota M, Banini BA, Cazanave SC, Sanyal AJ. Molecular mechanisms of lipotoxicity and glucotoxicity in nonalcoholic fatty liver disease. Metabolism 2016;65:1049‐1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Keating SE, Hackett DA, George J, Johnson NA. Exercise and non‐alcoholic fatty liver disease: a systematic review and meta‐analysis. J Hepatol 2012;57:157‐166. [DOI] [PubMed] [Google Scholar]
- 4. Lazo M, Hernaez R, Eberhardt MS, Bonekamp S, Kamel I, Guallar E, et al. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition Examination Survey, 1988‐1994. Am J Epidemiol 2013;178:38‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nat Rev Gastroenterol Hepatol 2013;10:656‐665. [DOI] [PubMed] [Google Scholar]
- 6. Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle‐aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology 2011;140:124‐131. [DOI] [PubMed] [Google Scholar]
- 7. Marengo A, Jouness RIK, Bugianesi E. Progression and natural history of nonalcoholic fatty liver disease in adults. Clin Liver Dis 2016;20:313‐324. [DOI] [PubMed] [Google Scholar]
- 8. Ascha MS, Hanouneh IA, Lopez R, Tamimi TA‐R, Feldstein AF, Zein NN. The incidence and risk factors of hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. Hepatology 2010;51:1972‐1978. [DOI] [PubMed] [Google Scholar]
- 9. El‐Serag HB, Kanwal F. Epidemiology of hepatocellular carcinoma in the United States: where are we? Where do we go? Hepatology 2014;60:1767‐1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. White DL, Kanwal F, El‐Serag HB. Association between nonalcoholic fatty liver disease and risk for hepatocellular cancer, based on systematic review. Clin Gastroenterol Hepatol 2012;10:1342‐1359.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sanyal A, Poklepovic A, Moyneur E, Barghout V. Population‐based risk factors and resource utilization for HCC: US perspective. Curr Med Res Opin 2010;26:2183‐2191. [DOI] [PubMed] [Google Scholar]
- 12. Ertle J, Dechêne A, Sowa J‐P, Penndorf V, Herzer K, Kaiser G, et al. Non‐alcoholic fatty liver disease progresses to hepatocellular carcinoma in the absence of apparent cirrhosis. Int J Cancer 2011;128:2436‐2443. [DOI] [PubMed] [Google Scholar]
- 13. Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non‐alcoholic fatty liver disease and non‐alcoholic steatohepatitis in adults. Aliment Pharmacol Ther 2011;34:274‐285. [DOI] [PubMed] [Google Scholar]
- 14. PL Gonçalves, P Zago-Gomes Mda, CC Marques, AT Mendonça, CS Gonçalves, FE Pereira. Etiology of liver cirrhosis in Brazil: chronic alcoholism and hepatitis viruses in liver cirrhosis diagnosed in the state of Espírito Santo. Clinics (Sao Paulo) 2013;68:291‐295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. JD Yang, B Kim, SO Sanderson, JL St Sauver, BP Yawn, RA Pedersen, JJ Larson, TM Therneau, LR Roberts, WR Kim. Hepatocellular carcinoma in olmsted county, Minnesota, 1976-2008. Mayo Clin Proc 2012;87:9‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. K1 Tokushige, E Hashimoto, Y Horie, M Taniai, S Higuchi. Hepatocellular carcinoma in Japanese patients with nonalcoholic fatty liver disease, alcoholic liver disease, and chronic liver disease of unknown etiology: report of the nationwide survey. J Gastroenterol 2011;46(10):1230‐1237. doi: 10.1007/s00535-011-0431-9. [DOI] [PubMed] [Google Scholar]
- 17. F Hucke, W Sieghart, M Schöniger-Hekele, M Peck-Radosavljevic, C Müller. Clinical characteristics of patients with hepatocellular carcinoma in Austria - is there a need for a structured screening program? Wien Klin Wochenschr 2011;123:542‐551. [DOI] [PubMed] [Google Scholar]
- 18. N Kawada, K Imanaka, T Kawaguchi, C Tamai, R Ishihara, T Matsunaga, K Gotoh, T Yamada, Y Tomita. Hepatocellular carcinoma arising from non-cirrhotic nonalcoholic steatohepatitis. J Gastroenterol 2009;44:1190‐1194. [DOI] [PubMed] [Google Scholar]
- 19. SM1 Malik, PA Gupte, ME de Vera, J Ahmad. Liver transplantation in patients with nonalcoholic steatohepatitis-related hepatocellular carcinoma. Clin Gastroenterol Hepatol 2009;7:800‐806. doi: 10.1016/j.cgh.2009.02.025. [DOI] [PubMed] [Google Scholar]
- 20. G1 Guzman, EM Brunt, LM Petrovic, G Chejfec, TJ Layden, SJ Cotler. Does nonalcoholic fatty liver disease predispose patients to hepatocellular carcinoma in the absence of cirrhosis? Arch Pathol Lab Med 2008;132:1761‐1766. doi: 10.1043/1543-2165-132.11.1761. [DOI] [PubMed] [Google Scholar]
- 21. JA1 Marrero, RJ Fontana, GL Su, HS Conjeevaram, DM Emick, AS Lok. NAFLD may be a common underlying liver disease in patients with hepatocellular carcinoma in the United States. Hepatology 2002;36:1349‐1354. [DOI] [PubMed] [Google Scholar]


