Watch a video presentation of this article
Watch the interview with the author
Abbreviations
- BCS
Budd–Chiari syndrome
- PMN
polymorphonuclear cell
- SAAG
serum‐ascites albumin gradient
- WBC
white blood cell count
Prelude
The presence of ascites is a common indication for referral to specialists in gastroenterology and hepatology. The majority of patients will have ascites related to cirrhosis and portal hypertension; however, other causes of ascites are not uncommon. Careful and thoughtful evaluation of patients with ascites is critical to the proper management of these patients.
Causative Factors
Ascites is the accumulation of fluid within the peritoneal cavity. In the Western world, it is mainly caused by cirrhosis (∼75%), followed by peritoneal malignancy (12%), cardiac failure (5%), and peritoneal tuberculosis (2%).1 Alternative causes of ascites include hepatic outflow obstruction, nephrotic syndrome, and disruption of the pancreatic duct or lymph vessels. The underlying mechanism of development of ascites can include elevated hydrostatic pressure (e.g., cirrhosis and congestive heart failure), decreased oncotic pressure (nephrotic syndrome), increased peritoneal fluid production compared with resorption (neoplasms), or a combination all these factors.
History and Physical Examination
Patients with ascites report abdominal fullness, increased abdominal girth, weight gain, dyspnea, and early satiety. Fever, abdominal pain, and confusion may be a sign of infected fluid, although it may be absent in patients with cirrhosis because of a muted inflammatory response.2 Approximately 1500 mL fluid must be present before flank dullness is detected. If no flank dullness is present, the patient has less than a 10% chance of having ascites.2
Diagnosis Is Made by Peritoneal Fluid Analyses
In any patient with the new onset of ascites, a diagnostic paracentesis should be performed to determine the cause of the fluid.2 Abdominal imaging with an ultrasound is recommended before paracentesis. Diagnostic paracentesis is performed with a narrow‐gauge needle and is very safe, even in patients with coagulopathy. Technique and equipment have been described elsewhere.2, 3
In a study with 1100 large‐volume paracenteses, there were no reported hemorrhagic complications despite platelet counts as low as 19,000 cells/mm (19 × 10/L) (54% at <50,000) and international normalized ratios for prothrombin time as high as 8.7 (75% at >1.5 and 26.5% at >2.0).4 However, a systematic review reported a mortality rate of 0% to 1.2%, significant bleeding in 0% to 2.7%, ascitic fluid leak in 0% to 2.35%, perforation in 0.83%, and residual catheter tip fragment in 0.41%.5
Differential Diagnosis of Ascites: Fluid Albumin, Protein, and Differential Cell Count Are the Key for Diagnosis
Table 1 summarizes the key elements that are important in the differential diagnosis of ascites. The most important parameter to determine the cause of ascites is the serum‐ascites albumin gradient (SAAG). The SAAG correlates with the sinusoidal pressure,6 and a SAAG ≥1.1 g/dL (high SAAG ascites) indicates a hepatic vein–portal vein pressure gradient more than 11 mm Hg (i.e., portal hypertension). High SAAG ascites is almost always caused by a sinusoidal or postsinusoidal source of the ascites. A SAAG less than 1.1 g/dL suggests the cause of ascites is not related to portal hypertension. However, the presence of low SAAG in the clinical context of suspected cirrhosis should be repeated because up to 3.3% of patients with portal hypertension may have SAAG less than 1.1 g/dL.7 A repeat paracentesis will often reveal a high SAAG. When the SAAG is ≥1.1 g/dL and the total protein in the ascites is low (<2.5 g/dL), the cause of the ascites is undoubtedly cirrhosis and portal hypertension. When the SAAG is ≥1.1 g/dL and the total protein is high (≥2.5 g/dL), the cause of the ascites is usually right‐heart failure. Ascites albumin levels in patients with cirrhosis and portal hypertension are typically less than 1 g/dL7 (Figure 1).
Table 1.
Classification of Diagnostic Test in Ascitic Fluid Analysis
| Routine | Optional (indication) | Unusual (indication) | Unhelpful |
|---|---|---|---|
| Cell count and differential | Culture in blood culture bottles (infection) | AFB smear and culture (tuberculosis) | pH |
| Albumin | Glucose (infection) | Cytology (peritoneal carcinomatosis) | Lactate |
| Total protein | Lactate dehydrogenase (neoplasia, infection) | Triglyceride (chylous ascites if >110 mg/dL) | Cholesterol |
| Amylase (pancreatitis) | Bilirubin (suspicion for bile leak) | Fibronectin | |
| Gram stain (infection) | Glycosaminoglycans |
Adapted with permission from Hepatology.2 Copyright 2013, American Association for the Study of Liver Diseases.
Abbreviations: AFB, Acid‐fast bacillus.
Figure 1.
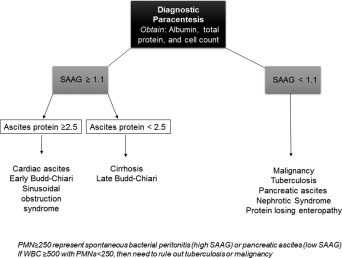
Diagnostic algorithm for patients with ascites. Abbreviation: WBC, white blood cell count.
Low SAAG ascites (<1.1 g/dL) is usually caused by peritoneal malignancies, chronic peritoneal infection (i.e., mycobacterium tuberculosis), and nephrotic syndrome. Cancers that spread to the omentum and result in ascites are typically of ovarian, gastric, or pancreatic origin. It is uncommon for hepatocellular carcinoma to cause malignant ascites.
Whenever ascites is sampled, a cell count should be performed. This is a critical test to determine whether spontaneous bacterial peritonitis is present. In patients with cirrhotic ascites, the presence of more than 250 polymorphonuclear cells (PMNs) is consistent with spontaneous bacterial peritonitis. The PMN count can also be elevated in pancreatic ascites, but the SAAG in these patients will be less than 1.1 g/dL. In patients with malignant‐related ascites and peritoneal carcinomatosis, cytology is positive in 96.7% of cases.8 However, in cases of hepatocellular carcinoma and cirrhosis, the yield of cytology for malignancy is extremely low and is not warranted.
In cases where chronic infection is suspected, positive cultures or peritoneal biopsy is required for the diagnosis. Ascites caused by chronic infections (e.g., tuberculosis and filariasis) is more common in the Far East and developing nations.9
Low serum oncotic pressure can also cause low SAAG ascites. Testing for nephrotic syndrome and protein‐losing enteropathy should be performed in patients with low SAAG ascites and a suspicion of either one of these conditions.
An ascites triglyceride level should be sent when ascites is cloudy or milky. An ascitic triglyceride level greater than 110 mg/dL is diagnostic of chylous ascites. Chylous ascites has been reported in up to 1% of patients with cirrhosis and is likely due to rupture of lymphatic channels in the setting of excessive lymph flow.9 Other causes of chylous ascites include inflammation (pancreatitis), abdominal surgery or traumatic injury, right‐heart failure, and abdominal radiation therapy.9 Patients with pancreatitis or abdominal trauma and disruption of the pancreatic ducts may present with ascites. In these patients, the amylase level of the ascites will be elevated (>100 mg/dL) and will have low SAAG ascites.
Budd–Chiari syndrome (BCS) can present with ascites. In early BCS, the SAAG will be ≥1.1 g/dL and the total protein will be greater than 2.5 g/dL. As BCS progresses to cirrhosis, the SAAG will remain elevated, but the total protein will decline to less than 2.5 g/dL.
Treatment Overview and Prognosis
Treatment of ascites caused by portal hypertension is sodium restriction, diuretics, therapeutic paracentesis, or shunt placement in refractory cases (Table 2), and this is reviewed elsewhere.2
Table 2.
Treatment Options for Patients With Cirrhosis and Ascites
| First‐Line Treatment |
| Cessation of alcohol use, when present |
| Sodium‐restricted diet and diet education |
| Dual diuretics, usually spironolactone and furosemide, orally with single daily dosing |
| Discontinue nonsteroidal anti‐inflammatory drugs |
| Evaluation for liver transplantation |
| Second‐Line Treatment |
| Discontinue beta blockers, angiotensin‐converting enzyme inhibitors, and angiotensin receptor blockers |
| Consider adding midodrine especially in the profoundly hypotensive patient |
| Serial therapeutic paracenteses |
| Evaluation for liver transplantation |
| Transjugular intrahepatic portosystemic shunt |
| Third‐Line Treatment |
| Peritoneovenous shunt (e.g., LeVeen or Denver shunt; rarely performed because other options are superior with less complications and better outcomes) |
Adapted with permission from Hepatology.2 Copyright 2013, American Association for the Study of Liver Diseases.
Noncirrhotic ascites requires disease‐specific interventions. For example, acute BCS will require anticoagulation and consideration for transjugular intrahepatic portosystemic shunt. In nephrotic syndrome or ascites, or both, caused by heart failure, aggressive management of both renal and cardiac pathology will ameliorate ascites. In contrast with portal hypertension, diuretics targeting the renin‐angiotensin‐aldosterone system (spironolactone) are not useful in low SAAG ascites. In patients with poor life expectancy, where the priority is palliation of symptoms, an indwelling peritoneal drain may be useful to manage ascites. Family and patients should be informed that peritoneal drains may cause protein depletion and infection.
Summary
Ascites is a common indication for referral to gastroenterology and hepatology. Patients with ascites should undergo diagnostic paracentesis with fluid sent for albumin, total protein, and cell count. The SAAG should be calculated to differentiate between ascites caused by portal hypertension and ascites caused by local factors (Figure 1). These distinctions are critical for the management of this clinically important complication.
Potential conflict of interest: Nothing to report.
REFERENCES
- 1. Garcia‐Tsao G. Ascites In: Dooley JS, Lok ASF, Burroughs AK, eds. Sherlock's Diseases of the Liver and Biliary System. 12th ed Blackwell Publishing Ltd., Oxford, UK, 2011:210‐233. [Google Scholar]
- 2. Runyon BA. Introduction to the revised American Association for the Study of Liver Diseases Practice Guideline management of adult patients with ascites due to cirrhosis 2012. Hepatology 2013;57:1651‐1653. [DOI] [PubMed] [Google Scholar]
- 3. Thomsen TW, Shaffer RW, White B, Setnik GS. Videos in clinical medicine. Paracentesis. N Engl J Med 2006;355:e21. [DOI] [PubMed] [Google Scholar]
- 4. Grabau CM, Crago SF, Hoff LK, Simon JA, Melton CA, Ott BJ, et al. Performance standards for therapeutic abdominal paracentesis. Hepatology 2004;40:484‐488. [DOI] [PubMed] [Google Scholar]
- 5. Wong CL, Holroyd‐Leduc J, Thorpe KE, Straus SE. Does this patient have bacterial peritonitis or portal hypertension? How do I perform a paracentesis and analyze the results? JAMA 2008;299:1166‐1178. [DOI] [PubMed] [Google Scholar]
- 6. Hoefs JC. Serum protein concentration and portal pressure determine the ascitic fluid protein concentration in patients with chronic liver disease. J Lab Clin Med 1983;102:260‐273. [PubMed] [Google Scholar]
- 7. Runyon BA, Montano AA, Akriviadis EA, Antillon MR, Irving MA, McHutchison JG. The serum‐ascites albumin gradient is superior to the exudate‐transudate concept in the differential diagnosis of ascites. Ann Intern Med 1992;117:215‐220. [DOI] [PubMed] [Google Scholar]
- 8. Runyon BA, Hoefs JC, Morgan TR. Ascitic fluid analysis in malignancy‐related ascites. Hepatology 1988;8:1104‐1109. [DOI] [PubMed] [Google Scholar]
- 9. Cardenas A, Chopra S. Chylous ascites. Am J Gastroenterol 2002;97:1896‐1900. [DOI] [PubMed] [Google Scholar]


